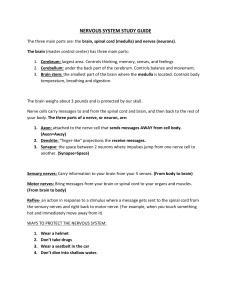
Pathophysiology Exam 1 Function of the Neurologic System Chapter 14 The Central Nervous System (CNS) consists of the brain and spinal cord; they are protected by the cranium and vertebrae The Peripheral Nervous System is composed of cranial nerves, spinal nerves and their ganglia o Afferent Pathways (ascending) carry sensory impulses towards the CNS o Efferent Pathways (descending) innervate skeletal muscle or effector organs – move motor impulses away from the CNS Somatic Nervous System have pathways which regulate voluntary motor control (skeletal muscle) Autonomic Nervous System is involved in regulation of body’s internal environment (viscera) through involuntary control of organ systems o Sympathetic and parasympathetic divisions Cells of the Nervous System o Neuron – primary cell of the nervous system, electrically excitable cell that transmits and receives information Structurally classified on basis of number of processes (projections) extending from cell body Unipolar neurons Pseudounipolar neurons Bipolar neurons Multipolar neurons o Functional classification of Neurons Sensory Neurons carry impulses from peripheral sensory receptors to CNS Associated Neurons (interneurons) transmit impulses from neuron to neuron Motor neurons transmit impulses away from CNS to effector (skeletal muscle, organs) with skeletal muscle: forms neuromuscular junction o They can work alone or in units – detecting environmental changes and initiating body responses to maintain homeostasis o Size and structure will vary and each has its own specialized functions o Cellular constituents: microtubules – transport within cell neurofibrils – supportive fibers microfilaments – transport of cellular products nissl substances – protein synthesis o There are 3 components: A cell body (soma) Dendrites (branching fibers of cell) Extensions that carry nerve impulses toward the body Axons (1 per neuron) Long, conductive projections that carry nerve impulses away from the cell body Axon hillock is a cone shaped process where axon leaves the cell body o Action potentials initiated at first part of axon hillock Myelin sheath membrane made from myelin, which may wrap axons o Interrupted at regular intervals, nodes of Ranvier o Myelin increases velocity of nerve impulses o Saltatory conduction: myelin acts as insulator, this allows action potentials to leap between segments rather than flow along entire length of membrane (increasing velocity) Axons TERMINATE with synaptic knobs – used in neurotransmission o Cell bodies for most are located in the Central Nervous System Those in the Peripheral Nervous System are found in groups called GANGLIA Neuroglial cells – provide structural support, protection, and nutrition for neurons, facilitate neurotransmission o “Nerve Glue” o Found both in the CNS and PNS o Comprises 50% of total brain and spinal cord volume o CNS cells Astrocytes Oligodendroglia (oligodendrocytes) Ependymal cells Microglia o PNS cells Schwann cells Nonmyelinating Schwann cells Satellite glial cells o All cells have different functions Nerve Injury and Regeneration o Mature nerve cells do not divide, injury causes permanent loss of function o Wallerian degeneration occurs when axon is severed, it is the portion cut off from the cell body o Distal to injury Swelling occurs Neurofilaments hypertrophy Myelin sheath shrinks and disintegrates Axon degenerates and disappears o Proximal to injury Swelling and dying by chromatolysis (dispersing the Nissl substance) or apoptosis Increased protein synthesis and mitochondrial activity by the cell (during repair) New terminal sprouts project from proximal segment o Process limited to myelinated fibers and occurs generally only in PNS o Nerve regeneration depends on many factors Location and type of injury Presence of inflammatory responses Process of scarring Nerve Impulse o Neurons generate and conduct electrical and chemical impulses Selectively changing the electrical potential of plasma membrane Influencing other nearby neurons by releasing chemicals (neurotransmitters) o Unexcited neuron: resting membrane potential When membrane potential sufficiently raised – action potential generated causing floe of nerve impulse to all parts of neurons Stimulus must be strong enough to initiate response if too weak, will not occur o All or none response o Synapses Regions between adjacent neurons Conducting neurons named whether they relay impulses Presynaptic neurons = proximal to synapse Postsynaptic neurons = distal to synapse Synapse composed of bulbous end of presynaptic neuron (knob) Separated from postsynaptic neuron by gap called synaptic cleft Impulses transmitted here through chemical and electrical conduction Synaptic bouton Where chemicals (neurotransmitters) are stored Neurotransmitters o Chemicals synthesized in the neuron and localized in the presynaptic terminal (bouton) Norepinephrine, acetylcholine, dopamine, histamine, serotonin o Released into synaptic cleft and bind to receptor site where they affect ion channels o They have more than one function o Neuromodulators chemical messengers released from neuron in CNS/PNS, affecting group of neurons that have receptors for that messenger Excitatory/inhibitory effects o Chemical synapses occur in one direction, action potentials along multineuronal pathway in one direction Neurotransmitters o Binding of neurotransmitter at receptor site changes permeability of postsynaptic neuron- changing membrane potential o Excitatory postsynaptic potentials where postsynaptic neuron becomes excited (depolarized) – reaching threshold and initiating action potential o Inhibitory postsynaptic potentials when plasma membrane is inhibited (hyperpolarized) – less likely to reach threshold potential – action potential inhibited o Summation Action potentials depends on number and frequency of potentials the postsynaptic neuron receives Temporal summation – time relationship: effects of successive, rapid impulses from single neuron at same synapse Spatial summation – spacing effect: combined effects of impulses from several neurons onto single neuron at same time Brain o Integrated circuit of millions of neurons o Enables person to reason, function intellectually, express personality and mood, perceive and interact with environment o Cerebrum Largest part of brain, contains gray and white matter Consists of forebrain, midbrain, and hindbrain (different functions) Forebrain (telencephalon) – consists of cerebral cortex (largest portion of brain) and basal ganglia o Contains outer layer of cell bodies of neurons (gray matter) o White matter lies beneath cerebral cortex and composed of myelinated nerve fibers o Lobes: 2 cerebral hemispheres that are separated by deep groove Frontal lobe goal oriented behavior (concentration), memory, thought, inhibits limbic, motor movements, eye movements Primary voluntary motor area corresponds between body region and area in brain Broca speech area – motor aspects of speech Parietal lobe somatic sensory input Occipital lobe primary visual cortex – receives input from retinas – visual interpretation Temporal lobe auditory cortex, Wernicke area (sensory speech area) – reception/ interpretation of speech o Basal Ganglia – group of nuclei includes caudate nucleus, putamen, and globus pallidus Responsible for dopamine synthesis, neurotransmitter, precursor of norepinephrine Important for voluntary movement and cognitive emotional functions (pleasure reward) Extrapyramidal system: part of motor control system that causes involuntary reflexes and coordinated movement with stabilizing effect on motor control o Limbic system – group of interconnected structures Composed of amygdala, hippocampus, fornix, hypothalamus, related autonomic nuclei involved in primitive behavioral responses: visceral reaction to emotion, motivation, mood, feeding behaviors, biologic rhythms, sense of smell mediates emotion and long term memory o Diencephalon (interbrain) Epithalamus, thalamus, hypothalamus, subthalamus Midbrain (mesencephalon) o Corpora quadrigemina 2 parts of superior colliculi and 2 pairs of inferior colliculi o Tegmentum Red nucleus, substantia nigra, basis pedunculi o BOTH TOGETHER ARE CALLED CEREBRAL PEDUNCLES o Voluntary and involuntary visual motor movements, auditory system, sensation Hindbrain (metencephalon) o Cerebellum is responsible for reflexive Involuntary fine tuning of motor control Maintaining balance and posture o Medulla and Pons o Myelencephalon: medulla oblongata, lowest portion of brain stem Reflex activities heart rate, respiration, blood pressure, coughing, sneezing, swallowing, and vomiting Contains nuclei of cranial nerves IX – XII Contralateral control when cerebral impulses control function on opposite side of body Sleep-wake cycles o Brainstem Comprised of midbrain, medulla, pons Connects hemispheres of brain, cerebellum, and spinal cord Reticular formation Collection of nerve cell bodies (nuclei): controls vital reflexes (CV function, respiration) Essential for maintaining wakefulness and attention, supports movements (balance, posture) Referred to as reticular activating system Spinal Cord o Portion of CNS that lies within the vertebral canal, surrounded and protect by vertebral column o Functions Connects brain and body Somatic and autonomic reflexes Motor pattern control Sensory and motor modulation o Spinal nerves continue from end of spinal cord and form a nerve bundle called cauda equine o Divided into vertebral sections 8 cervical, 12 thoracic, 5 lumbar, 5 sacral, 1 coccygeal o Cross section of spinal cord Butterfly shaped inner core of gray matter o Gray Matter Divided into 3 regions: posterior (dorsal horn), substantia gelatinosa, lateral horn o White Matter Surrounds gray matter – forms ascending and descending pathways called spinal tracts (carry sensory nerve impulses from spinal cord) o Central canal, filled with cerebrospinal fluid (CSF) o Motor Pathways Corticobulbar tract axons synapse on motor cranial nuclei and control muscles of face, head, and neck Lateral corticospinal project through nerves to specific muscles, involved in precise motor movement Reticulospinal modulates motor movement – inhibiting/exciting spinal activity Vestibulospinal tract causes extensor muscles of body to rapidly contract (witnessed when person falls back) Rubrospinal tract important for muscle movement and fine muscles control in upper extremities o Sensory Pathways Posterior (dorsal) column carries fine touch sensation, 2 point discrimination, proprioceptive information Anterior and Lateral spinothalamic tracts responsible for vague touch sensation, pain and temperature perception Protective structures o Cranium – consists of 8 cranial bones Occipital Temporal Parietal Frontal Sphenoid Ethmoid Galea aponeurotics Thick, fibrous band of tissue overlying cranium – adds protection to skull Subgaleal space Has venous connections with dural sinuses Increased ICP blood can be shunted to the space to reduce pressure in the intracranial cavity o Meninges Surrounding spinal cord and brain are 3 protective membranes Dura matter “hard mother” Composed of 2 layers o Periosteum (endosteal) layer of skull o Inner dura (meningeal) layer Arachnoid Spongy, web like structure Pia Matter Adheres to contours of brain and spinal cord Provides support for blood vessels serving brain tissue Subdural space Lies between dura and arachnoid With small bridging veins Subarachnoid space Lies between arachnoid and pia matter and contains CSF The spinal cord is anchored to the vertebrae by extension of meninges o Cerebrospinal Fluid Clear, colorless fluid like blood plasma and interstitial fluid 125 – 150 mL of CSF circulate in ventricles Produced in choroid plexuses – provided rich blood supply by blood vessels from pia matter Tight junctions limit barrier between CSF and blood functions similarly to BBB (blood brain barrier) CSF floe regulated by pressure gradient of arterial system/ and CSF filled cavities CSF is reabsorbed into venous circulation through arachnoid villi (one way valves) o Vertebral column Intervertebral disk – space between each interspace Nucleus pulposus at each center, pulpy mass with elastic fibers Disks absorb shock: prevent damage to vertebrae Blood supply to the brain o Brain receives 20% cardiac output 800-1,000 mL/ per minute o Autoregulated to maintain a stable flow during fluctuating perfusion pressures CO2 primary regulator for blood flow within the CNS o Arterial supply from 2 systems Internal carotid arteries and vertebral arteries Circle of Willis Provides an alternate route for blood flow when one of the contributing arteries is obstructed (collateral blood flow) Cerebral venous drainage does not parallel arterial supply Cerebral veins classified as superficial and deep veins Drain into venous plexuses, to dural sinuses, to join internal jugular veins at base of skull Venous outflow affects intracranial pressure Those with head injuries when allowing their heads to turn or fall to the side could occlude venous return, increasing intracranial pressure Blood Brain Barrier o Describes cellular structures that selectively inhibit certain potentially harmful substances in the blood from entering the interstitial spaces of brain or CSF o Endothelial cells in brain capillaries Intracellular tight junctions at BBB site Cell supporters: astrocytes, pericytes, microglia o Glucose, lipid soluble molecules, electrolytes and chemicals Cross into and out of brain facilitated by transport molecules Implications for drug therapy – certain drugs have a greater propensity for crossing this barrier Blood Supply to the Spinal Cord o Derives from branches off the vertebral arteries and from branches from various regions of the aorta Anterior and posterior spinal arteries o Venous drainage parallels the arterial supply closely Peripheral Nervous System (PNS) o Includes the nerves outside the CNS o Somatic nervous system part of the PNS controlling voluntary muscle movement (efferent nerves), and sensory information (afferent nerves) o Nerve composed of individual axons wrapped in myelin sheath arranged in bundles called fascicles o Spinal nerves (31 pairs) Named from vertebral level (cervical, thoracic, etc…) Contains both sensory and motor neurons called (mixed nerves) Structure of nerve like a tree: rootlets > roots > converge into trunk > divides into rami (branches) Anterior Rami form plexuses (networks of fibers) Posterior Rami innervate specific cutaneous areas called dermatomes o Cranial nerves: 12 pairs Arise from brain Sensory motor and mixed Autonomic Nervous System (ANS) o Coordinates and maintains a steady state among body organs o Regulates cardiac muscle, smooth muscle, and glands of body (involuntary system) o Considered part of the PNS o 2 divisions: promote antagonistic effect Sympathetic nervous system Parasympathetic nervous system o Neurons of ANS travel in spinal nerves and certain cranial nerves o CNS has cardiovascular and respiratory centers in reticular formation and both sympathetic/parasympathetic areas in hypothalamus Pathways intersect all these areas and project to autonomic areas in brain stem/spinal cord o Both divisions made up of efferent (motor)autonomic neurons which conduct impulses away from brainstem or spinal cord and down to autonomic effectors o 2 neuron system Preganglionic neurons (myelinated) Conduct impulses from the brainstem or spinal cord to an autonomic ganglion where they synapse with postganglionic neuron Postganglionic neurons (unmyelinated) Conducts impulses away from the ganglion to the effector Sympathetic Nervous System o Mobilizes energy stores in times of need Fight or flight (stress response) o Innervated by cell bodies located from thoracic (T1) through second lumbar (L2) regions in spinal cord Thoracolumbar division o Preganglionic axons form synapses in the sympathetic ganglia o Postganglionic neurons leave collateral ganglia and innervate the viscera below the diaphragm Parasympathetic Nervous system o Conserves and restores energy when a person is at rest o Innervated by nerve cell bodies located in the cranial nerve nuclei and in sacral region of spinal cord Craniosacral division o Preganglionic fibers are longer and travel close to organs they innervate before forming synapses with relatively short postganglionic neurons Autonomic Nervous System / Neurotransmitters and Neuroreceptors o Acetylcholine – released by sympathetic and parasympathetic preganglionic fibers Characterized by cholinergic transmission o Norepinephrine (norandrenaline) Released by most postganglionic sympathetic fibers Function by adrenergic transmission 2 types of adrenergic receptors (a & b) A1 – adrenergic – excitation or stimulation A2 – adrenergic – relaxation or inhibition B1 – adrenergic – facilitate HR and contractility, cause renin release from kidney B2 – adrenergic – all remaining effects of B- receptors o Primary response (focus) stimulation of a1, causes vasoconstriction Autonomic nervous system functions o 2 divisions causing opposite responses o Sympathetic stimulation Promotes responses for protection of the individual Increases blood glucose levels and temperature, increases HR and BP fight/flight o Parasympathetic Reduced HR and enhanced visceral functions (digestion) Aging and the Nervous System o Decrease in number of neurons o Decreased brain weight and size o Lipofuscin and neurofibrillary tangles o Slowing of neurologic responses Pain, temperature, sleep and Sensory Function Chapter 15 Pain o Unpleasant sensory and emotional experience associated with actual or potential tissue damage o Acute pain is protective and promotes withdrawal from painful stimuli, allows injured part to heal, and teaches avoidance of painful stimuli Neuroanatomy of Pain o 3 parts of nervous system responsible for sensation, perception, and response to pain o Afferent pathways begin in PNS and travel to spinal cord and brain o Interpretive pathways located in many parts of the brain o Efferent pathways descend from CNS back to spinal cord o Nociception Processing of potentially harmful stimuli through normally function nervous system o Nociceptors (pain receptors) Free nerve endings in skin, muscles, joints, arteries, and viscera in the afferent peripheral nervous system When stimulated by chemical, mechanical and thermal stimuli cause nociceptive pain 2 primary types transmitted to spinal cord, brainstem, thalamus, cortex A delta fiber – rapid transmit, well localized, “fast” pain sensations (causes withdrawal) C fibers – muscles, tendons, organs: slow, dull aching, burning sensations o Unmyelinated o 4 phases of Nociception Pain transduction nociceptors are activated by noxious stimuli Pain transmission conduction of pain impulses into dorsal horn and spinal cord Pain perception: Conscious awareness of pain 3 systems interact to produce perception of pain Sensory discriminative system o Character, location, intensity of pain Affective motivational system o Determines individuals conditioned avoidance behaviors and emotional responses to pain Cognitive evaluation system o Individual learned behavior concerning pain experience, modulating perception Pain threshold defined as lowest intensity of pain a person can recognize Pain tolerance defined as greatest intensity of pain that a person can endure Pain modulation involves many different mechanisms that increase or decrease the transmission of pain signals through the nervous system Can occur before, during, or after pain is perceived Neurotransmitters act to modulate control over transmission of pain impulses in periphery, spinal cord, and brain Excitatory neurotransmitters o Release by tissue injury/chronic inflammatory lesions o Glutamate, aspardate, substance P, and calcitonin o Sensitize nociceptors by reducing activation threshold Inhibitory neurotransmitters o Gamma aminobutyric acid (GABA), glycine, norepinephrine, and serotonin Endogenous opioids o Family of morphine like neuropeptides – inhibit transmission of pain impulses in periphery, spinal cord and brain o Bind with specific opioid receptors on neurons (mu, kappa, delta) o Widely distributed throughout body and responsible for general sensations of well-being and modulation of many physiological processes o Enkephalins – most prevalent Endorphins (endogenous morphine) – produced in the brain Dynorphins – most potent Endomorphins o Endocannabinoids Activate cannabinoid CB1 (in CNS), CB2 receptors (immune tissue) Modulates pain and other functions (memory, appetite, immune function, sleep, stress response, and addiction) Cannabis produces a resin containing cannabinoids Analgesia to humans – limited due to psychoactive and addictive properties o Descending inhibitory and faciliatory pathways: inhibit or facilitate pain Inhibitory pathways Activate opioid receptors Inhibit release of excitatory neurotransmitters Facilitate release of inhibitory neurotransmitters Stimulate inhibitory interneurons Afferent stimulation Inhibit ascending pain signals at the dorsal horn o Segmental pain inhibition When A-beta fibers are stimulated – inhibit interneuron and decrease pain transmission Rubbing injured area to relieve pain Diffuse noxious inhibitory control (DNIC) Inhibitory pain system – pain relieved when 2 noxious or painful stimuli occur at same time from different sites o Acupuncture, deep massage, intense cold/heat Expectancy related cortical activation (placebo effect) Can exert control over analgesic systems to attenuate or intensity pain Cognitive expectations cause physiologic effects Descriptions of Pain ACUTE PAIN o Normal protective mechanism alerting individual to condition or experience that is harmful to body and mobilizes individual to take prompt action to relieve it o Transient, lasting seconds to days at times up to 3 months o Occurs suddenly and relieved after chemical mediators (inflammatory) that cause pain are removed o Physical manifestations Increased HR, HTN, diaphoresis (sweating), dilated pupils o Somatic pain arises from the skin (abrasion/laceration), joints (arthritis), muscles (strain) o Visceral pain pain in internal organs and lining of body cavities Poorly localized – aching, gnawing, throbbing, intermittent cramping quality Associated with N/V, hypotension Often radiates (spreads away from site of pain)/ referred (gallstones, pancreatitis, kidney stones, appendicitis) o Referred pain felt in an area removed or distant from its point of origin, the area of referred pain is supplied by same spinal segment as actual site of pain Can be acute or chronic Chronic or Persistent pain o pain lasting longer than 3-6 months, well beyond expected normal healing time o ongoing or intermittent o Changes in PNS and CNS that cause dysregulation of nociception and pain modulation processes are thought to lead to chronic pain o Chronic pain thought to be due to stress and coping o Persistent pain allows for physiologic adaptation (normal HR, BP) Neuropathic Pain o Chronic pain initiated or caused by primary lesion of dysfunction in nervous system o Leads to long term changes in pain pathway structures and abnormal processing of sensory information o Described as burning, shooting, shock like, or painful/nonpainful stimuli o Classified by Peripheral neuropathic pain; peripheral lesions Central neuropathic pain; by a lesion or dysfunction in brain/spinal cord Temperature Regulation o Thermoregulation maintained through Heat production, heat conservation, heat loss Normal 96.2 – 99.4 F varies in response location, activity, environment, circulation, rhythm, gender Mediated by hypothalamus and endocrine system Peripheral thermoreceptors Skin, liver, skeletal muscle Central thermoreceptors Hypothalamus, spinal cord, viscera Body heat produced by chemical reactions of metabolism and skeletal muscle tone and contraction Heat producing mechanism (chemical/non-shivering thermogenesis) initiated hypothalamic thyrotropin releasing hormone (TRH) to act on thyroid gland to stimulate release of thyroxine Thyroxin = acts on adrenal medulla to release epinephrine and cause increased metabolic rate (increases body heat) Norepinephrine and thyroxine activate brown fat thermogenesis where energy is released as heat (non-shivering thermogenesis) rather than use of ATP Heat conservation performed by the SNS (somatic nervous system) being stimulated by the hypothalamus Increases skeletal muscle tone, initiates shiver response and produces vasoconstriction Peripheral constriction of blood vessels occurs, blood shunted to core of body to maintain heat Voluntary responses such as bundling up, keeping moving to keep warm will ensue Heat loss occurs through Radiation, conduction, convection, vasodilation, evaporation (sweating), decreased muscle tone, increased respiration, voluntary measures, adaptation to warmer climates o Infants Produce sufficient body heat however are unable to conserve heat produced due to small body size Greater ratio of body surface to body weight = inability to shiver Little subcutaneous fat (not well insulated) o Elderly Respond poorly to environmental temperature extremes due to slowed blood circulation, structural and functional skin changes, decreased heat producing activities, presence of disease Decreased shivering response, slowed metabolic rate, decreased vasoconstrictor response, diminished/absent ability to sweat, decreased peripheral sensation, decreased perception of heat and cold, decreased thirst, decreased adipose tissue Fever o Temporary resetting of hypothalamic thermostat to higher level in response to exogenous or endogenous pyrogens Exogenous pyrogens Endotoxins produced by pathogens stimulate release of endogenous pyrogens, which raise thermal set point Integrated response occurs to increase heat production as well as conserve heat by the person feeling colder and dressing more warmly, decreases surface area by curling up. Fever of unknown origin Body temperature > 101 F for longer than 3 weeks that remains undiagnosed o Benefits of a Fever Moderate fever helps body respond to infectious processes Raising temperature kills many microorganisms – affects growth/replication Higher temperatures decrease serum iron, zinc, copper needed for bacterial replication Causes lysosomal breakdown and auto destruction of cells, preventing viral replication in infected cells Increased lymphocytic transformation and motility of polymorphonuclear neutrophils – facilitates immune response Enhances phagocytosis and production of antiviral interferon o Hyperthermia Elevation of the body temperature without increase in hypothalamic set point Can produce nerve damage, coagulation of cell proteins and death At or higher than 105.8F can produce convulsions/seizures – death at 109.4 F May be associated with stroke or head trauma Therapeutic hyperthermia Form of local regional or whole body hyperthermia used to destroy pathologic microorganisms or tumor cells o Accidental hyperthermia Heat cramps severe spasmodic cramps in abdomen and extremities that follow prolonged sweating and sodium loss (strenuous exercise) Heat exhaustion prolonged high core or environmental temperatures cause profound vasodilation and profuse sweating leading to dehydration Heat stroke overstress thermoregulatory center leads to impaired/failed physiologic mechanisms with temperatures at or over 104F Malignant hyperthermia hypermetabolic complication of rare inherited muscle disorder that is triggered by inhaled aesthetics and depolarizing muscle relaxants Involved hypermetabolism – increased level of lactic acid causing acidosis and increased body temperature o Hypothermia core body temperature less than 95 F Produces Depression of the CNS and respiratory system Vasoconstriction, and changes in microcirculation/coagulation Ischemic tissue damage Severe – ice crystals form inside of cells, causing rupture and death of cell Tissue hypothermia Slows cell metabolism, increases blood viscosity, slows microcirculatory blood flow, facilitates blood coagulation, stimulates profound vasoconstriction Therapeutic hypothermia Used to slow metabolism and preserve ischemic tissue during surgery or limb reimplantation Accidental hypothermia Results from immersion in cold water, prolonged exposure to cold, or altered thermoregulation Trauma & Temperature o CNS trauma leads to central fever Inflammation, increased intracranial pressure, intracranial bleeding Does not induce sweating Resistant to antipyretic therapy o Other trauma that alters temperature Accidental injuries Hemorrhagic shock Major surgery Thermal burns Sleep o Active multiphase process that provides restorative functions and promotes memory consolidation o Hypothalamus – major sleep center control timing of sleep wake cycle coordinate with circadian rhythms (24 rhythm cycles) hypocretins (orexins), acetylcholine, glutamate promote wakefulness Prostaglandin D2, adenosine, melatonin, serotonin, GABA, growth factors Promote wakefulness o Normal sleep has 2 primary alternating phases o Rapid eye movement (REM) sleep 20-25% of sleep time Occurs every 90 min beginning 1-2 hours after non-REM sleep begins Paradoxical sleep – ECG pattern is like normal awake pattern, brain is very active with dreaming Noted changes – increased parasympathetic activity, variable sympathetic activity Muscle relaxation, loss of temperature, regulation, altered HR, BP, and respiration, memorable dreams o Non-REM sleep 75-80% of sleep time Sympathetic tone decreased, increased parasympathetic activity Decreased metabolic rate, decreased temperature, HR, BP, and muscle tone o Sleep disorders 6 classifications Insomnia o Inability to fall or stay asleep, accompanied by fatigue, malaise, and difficulty with performance during wakefulness o mild, moderate, severe o transient/chronic o poor sleep hygiene, drug abuse, pain, modo disorders, genetics Sleep related breathing disorders Central disorders oh hypersomnolence Circadian rhythm sleep awake disorders Parasomnias Sleep related movement disorders Dyssomnias o Include insomnia o Obstructive sleep apnea syndrome (OSA) Most diagnosed sleep disorder Risks: Obesity, male sex, older age, postmenopausal status, increased adenoidal/tonsillar tissue Results from partial or total upper airway obstruction to airflow recurring during sleep with excessive loud snoring, gasping, multiple apneic episodes lasting 10 seconds or longer Periodic breathing interrupts sleep cycle, reducing sleep time and producing sleep and REM deprivations Produces hypercapnia, low O2 concentration, leading to polycythemia, pulmonary HTN, systemic HTN, stroke, right sided heart failure, liver congestion, edema Hypersomnia noted, diagnosed by polysomnography Dyssomnias narcolepsy o Hypersomnia excessive daytime sleepiness. Individuals may fall asleep while driving a car, working, while conversing Impaired mood, cognitive function with impaired attention, episodic memory o Primary hypersomnia disruption of sleep-wake cycles characterized by hallucinations, sleep paralysis Usually sporadic or occurring in families Associated with immune mediated destruction of hypocretin (orexin) secreting cells in hypothalamus Dyssomnias Circadian Rhythm Sleep Disorders o Common disorders of 24 hour sleep wake schedule which desynchronize circadian rhythm o Extrinsic causes Rapid time zone changes (jet lag) Alternating sleep schedule (rotating work shifts) Changing total sleep time from day to day o Intrinsic Advanced sleep phase disorder (early morning waking, early evening sleeping Delayed sleep phase disorder (late morning waking – late night to early morning sleeping) o These changes desynchronize circadian rhythm Depress vigilance, performance of psychomotor tasks, arousal o Can influence many health problems Cognitive deficits, difficulty concentrating, depression, anxiety, CV disease Parasomnia o Unusual behaviors occurring during non-REM stage 3 sleep Sleep walking Night terrors Rearranging furniture Eating food Exhibiting sleep sex Violent behavior Restless leg syndrome Special senses o Olfaction (smell) – cranial nerves I and V o Taste (gustation) – crania nerves (VII and IX) Eye o 3 layers Sclera thick white, outermost layer becomes transparent at the cornea Central anterior region allowing light to enter eye Choroid deep pigmented middle layer –prevents light from scattering inside eye Iris – round opening (pupil) through which light passes, adjusts to bright or dim light and close or distant vision Retina Innermost layer, contains rods (peripheral/dim light) and cones (color, detail receptors) o Nerve impulses pass through the optic nerves to optic chiasm Synapses travel to primary visual cortex in occipital lobe of brain o Light entering eye focused on retina by lens – flexible biconcave structure Flexibility allows changes in lens known as accommodation, allowing eye to focus on objects at different distances o Lens divides anterior chamber into Aqueous chamber – filled with aqueous humor which maintains pressure inside eye, and provides nutrients to structures in eye Secreted by ciliary processes and reabsorbed at canal of Schlemm Vitreous chamber – filled with vitreous humor, a gel like substance Cannot regenerate, and helps eyeball from collapsing inward Visual Dysfunction Alterations in Ocular Movements o Strabismus – one eye deviates from the other when the person is looking at an object Caused by a weak or hypertonic muscle in one eye Early correction important in affected eye caused by cerebral blockage of the visual stimuli Amblyopia – reduced vision in affected eye caused cerebral blockage of the visual stimuli Diplopia (double vision) – primary symptom o Nystagmus Involuntary unilateral or bilateral rhythmic movements of eyes Pendular Characterized by back and forth movements of the eyes Jerk One phase of eye movement is faster than the other o Paralysis of specific extraocular muscles may cause limited abduction, abnormal closure of eyelid, ptosis (drooping of eyelid), diplopia (double vision) Visual Dysfunction Alterations in Visual Acuity o Visual acuity is the ability to see objects in sharp detail o Aging causes lens of eye to become less flexible and adjusts more slowly and altered refraction of light by cornea and lens o Visual acuity declines with age Amblyopia – reduced or dimmed vision, scotoma (blind spot), decreased dark adaptation Cataracts – cloudy/opaque area in lens Papilledema – edema of optic nerve, retinal detachment (tear or break in retina with accumulation of fluid Glaucoma – second leading cause of blindness; increased intraocular pressures Open angle outflow obstruction of aqueous humor (canal of Schlemm) Angle closure/narrow angle displacement of iris toward cornea causes obstruction of outflow of aqueous humor (medical emergency) Age related macular degeneration Atrophic – dry, nonexudative, more common, slowly progressive w/ inflammation and accumulation of lipotuscin (lysosomal pigment residue) and drusen (photoreceptor waste products) in retina Neurovascular – wet, exudative, accumulation of drusen and lipofuscin, abnormal choroid blood vessel growth, leakage of blood or serum, and retinal detachment, fibrovascular scarring, loss of photoreceptors, severe, central vision loss Visual Dysfunction Alterations in Accomodation o Accommodation refers to changes in shape of lens and allow for change of focus from distant to near images Mediated through oculomotor nerve o May be altered causing Diplopia Blurred vision Headache o Presbyopia Term used for loss of accommodation with age Ocular lens become larger, firmer, less elastic Visual Dysfunction Alterations in Refraction o Most common visual problems o Common causes include irregularities in Corneal curvature Power of the lens Length of the eye o Myopia: nearsightedness Light rays are focused in front of the retina when the person is looking at a distant point o Hyperopia: farsightedness Light rays are focused behind the retina when a person is looking at a near object o Astigmatism: unequal curvature of the cornea Light rays are bent unevenly and do not come to a single focus on the retina May coexist with those above Visual Dysfunction Alterations in Color Vision o Sensitivity to color diminishes with age Age related yellowing of lens All colors become less intense o Color blindness X linked genetic trait Commonly red-green most common form o Acquired color vision deficiency occurs with ocular, neurologic, or systemic disease Neurologic Disorders causing Visual Dysfunction o Vision may be disrupted at points along the visual pathway Causing defect along visual field Visual changes may cause defects or blindness in entire visual field or in half a visual field (hemianopia) o Damage to optic nerve Same sided blindness o Damage to optic chiasm (x shaped crossing of optic nerves) Depends on location External Eye Disorders o Blepharitis – inflammation of eyelids caused by staphylococcus o Hordeolum (stye) – infection (staphylococcal) of sebaceous glands of eyelids o Chalazion – noninfectious lipogranuloma of oil secreting Meibomian gland, occurs with hordeolum o Entropion – lid margin turns inward against eyeball o Conjunctivitis – inflammation of conjunctiva (mucous membrane covering eyeball) Bacterial (pinkeye) – highly contagious; staphylococcus Viral – caused by adenovirus Allergic – antigen related/ pollens Trachoma – chlamydial o Keratitis – infection of cornea by bacteria or viruses The Ear o External Ear Comprised of pinna (auricle) visual portion of ear External auditory canal connects to middle ear Air filled sinuses promote conduction of sound Tympanic membrane (eardrum) Separates external ear from middle ear Sound waves entering external auditory can hit tympanic membrane causing it to vibrate o Middle ear Composed of tympanic cavity: houses three ossicles- malleus (hammer), incus (anvil), stapes (stirrup) Transmits vibration to inner ear Eustachian tube (pharyngotympanic) tube Connects middle ear with the thorax, opens when person swallows/yawn – equalizes pressure in middle ear o Inner ear System of osseous labyrinths (bony, fluid mazelike chambers) – perilymph Cochlea (organ of Corti (hair cells w/ hearing receptors), vestibule, and serricircular canals (equilibrium receptors) o Hair cells stimulate cochlear nerve to auditory cortex of temporal lobe of brain = interpretation of sound o Canal equilibrium receptors respond to changes in direction of movement o In each canal: receptor regions known as crista ampullaris: tufts of hair cells Vestibule o Contain maculae: receptors essential to body’s sense of static equilibrium o Otaliths (calcium salts) move in gel like material responding to changes in pull of gravity o Otaliths pull on gel which then pulls on hair cells in maculae Auditory dysfunction o Conductive hearing loss Occurs when change in outer or middle ear impairs conduction of sound from outer to inner ear o Sensorineural hearing loss Caused by impairment of organ of corti or central connections Congenital, noise exposure, aging, ototoxicity (medications antibiotics/diuretics), systemic disease, autoimmunity Presbycusis - most common form: age related hearing loss Tinnitus (ringing) – in ear initial symptom with medications – followed by progressive high tone hearing loss that is permanent o Meniere disease Endolymphatic hydrops Episodic chronic disorder of middle ear with unknown etiology Noted to have excessive endolymph and pressure in the membranous labyrinth which disrupts vestibular and hearing functions Vertigo, ear fullness, tinnitus, hearing loss Ear Infections o Otitis Externa – inflammation of outer ear; infectious: pseudomonas, staphylococcus: following prolonged exposure to moisture (swimmers ear) o Otitis media – common infection of infants/children, streptococcus, associated with ear pain, fever, irritability, inflamed tympanic membrane, fluid in middle ear o Otitis media with effusion – presence of fluid in middle ear without symptoms of acute infection Olfaction (smell) o Function of cranial nerve I o Strong relationship between taste and smell Creates sensation of flavor Both influenced by hormones within sensory cells Dysfunction may be in one or both, one may alter the other o Olfactory stimulants Camphoraceous, musky, floral, peppermint, ethereal, pungent, putrid o Sensitivity to odors declines steadily with aging Olfactory dysfunction o Hyposmia – impaired sense of smell o Anosmia – complete loss of smell o Olfactory hallucinations – smelling odors that are not present o Parosmia – abnormal or perverted sense of smell Taste (Gustation) o Function of multiple nerves in tongue, soft palate, uvula, pharynx Cranial nerves VII and IX o Taste sensations sour, salty, sweet, bitter, umami (savoriness) taste buds located in specific areas of mouth and tongue Taste dysfunction o Hypogeusia – decrease in taste sensation o Ageusia – absence of sense of taste o Both due to cranial nerve injuries o Dysgeusia – perversion of taste in which substances possess an unpleasant flavor (metallic) Somatosensory o Touch Involves 4 afferent fibers types that mediate tactile sensation Receptors are in skin Meissner and pacinican corpuscles o Sense movement across skin and vibration Merkel discks o Sense sustained light touch Ruffini endings o Respond to deep sustain pressure, stretch, and joint position Gradual decline in tactile discrimination with advancing age Places person at risk for trauma Somatosensory Function o Proprioception – awareness of the position of the body and its parts Depends on inner ear impulses and from receptors in joints and ligaments Progressive loss has been noted in elderly persons o Dysfunction Vestibular nystagmus – constant, involuntary movement of eyeball, develops when semicircular canal system is overstimulated Vertigo – sensation of spinning that occurs with inflammation of semicircular canals in ear (world is revolving) Meniere disease Peripheral neorpathies