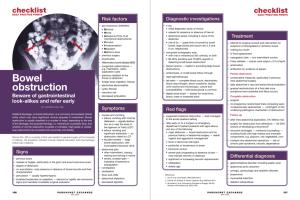
Conditions of the small bowel, the colon, rectum and anus Dr Ntakiyiruta Georges,Mmed,FCSECSA Lecturer Department of Surgery Faculty of Medicine National University of Rwanda • Meckel’s diverticulum • Typhoid • Tuberculosis • Small bowel obstruction • Appendicitis • Inflammatory bowel disease • Diverticular disease • Volvulus and large bowel obstruction • Anal conditions(haemorroids, rectal prolapse, perianal hematoma, fissure in ano, anorectal abscess, fistula-in-ano) Meckel’s diverticulum • It is a remnant of of the vitellointestinal duct of the embryo • Classically it occurs in 2% of patients, 2inches long, and 2feet from the ileocecal junction (‘rule of 2s’) • It occurs on the antimesenteric border of the terminal ileum Symptoms and signs • Symptomless • Incidental findings at laparotomy • Symptoms typical of acute appendicitis may occur • Rectal bleeding (ectopic gastric mucosa) • Rarely, umbilical discharge(fistula), intestinal obstruction(due to entrapment around the band from the apex of the diverticulum to the back of the umbilicus), small bowel volvulus, or intussusception(ileo-ileal) Investigations • Technetium scan for GI bleeding may show gastric mucosa in a Meckel’s • Laparotomy is required for complications of Meckel’s- the cause is not usually apparent until laparotomy is undertaken Treatment • Excision of the diverticulum Typhoid • Caused by salmonella typhi • It is endemic in Rwanda. • The organism enters the Peyer’s patches and may result in perforation or bleeding usually involving the ileum. • This usually occurs during the third week of the disease • The patient shows signs of perforation and generalized peritonitis • Surgical closure of the perforation is required Small bowel obstruction • Mechanical obstruction of the SB may be – simple(one point of obstruction) – Or closed loop(obstruction at 2 points enclosing a segment of bowel) • If the bowel is viable, the obstruction is termed non strangulating • If the blood supply is compromised, strangulating obstruction occurs with subsequent infarction of bowel. • Stranglation occurs when the obstructing mechanism cuts off the mesenteric arterial blood supply; e.g. the neck of the sac with a loop of bowel trapped in a hernial sac, or the twist of a volvulus • Mechanical obstruction is more common in the small bowel than in the large bowel Causes • In the lumen: gallstone ileus, food bolus(following pylorus destroying operations, i.e. pyloroplasty) • In the wall: congenital atresia, tumours, e.g. lymphoma or carcinoma • Outside the wall: herniae, adhesions, volvulus, intussusception Symptoms and signs • Colicky abdominal pain; Vomiting; Constipation; Abdominal distension • Symptoms depend on whether the obstruction is high or low. • High obstruction🡪early vomiting(bilious), and late constipation • Low obstruction🡪early constipation, and late vomiting(faeculent), and marked distension • Tympanitic abdomen • High-pitched tinkling bowel sounds • Hernial orifices should be carefully examined • Pyrexia, tachycardia, continuous pain and localized tenderness suggest actual or impending strangulation. Investigations • Hb; FBC; WCC with neutrophilia may indicate strangulation; U&Es; • AXR: distended loops of small bowel in central abdomen. Erect films show air fluid levels. Absent or diminished colonic gas. Dilated proximal small bowel shows lines close together (valvulae conniventes) crossing completely the lumen of the bowel. Look for gas in the biliary tree (gallstone ileus with cholecystoduodenal fistula) Treatment: conservative • Intravenous fluids and nasogastric aspiration • Nil orally • 2-hourly temperature and pulse • Abdominal examination 8-hourly Some cases of simple mechanical obstruction, e.g. due to adhesions, will settle on this regimen Treatment: indications for surgery • Strangulating obstruction, e.g. a tender irreducible hernia requires urgent surgery • If a conservative ”drip and suck”has been undertaken for obstruction, surgery is indicated for signs of incipient strangulation(pyrexia, tachycardia, localized tenderness) • Surgery is also required for simple obstruction which fails to settle, e.g. adhesions • At surgery the affected bowel is inspected for viability. • Indications of non-viability include: – Absence of peristalsis – Loss of normal sheen – Loss of pulsation in bowel mesentry – Colour: green or black bowel is non-viable and resection is required. Plum-coloured bowel may respond to wrapping for a few minutes in warm saline-soaked packs. If colour returns and transmission of peristaltic wave, it is viable. Prognosis • Small bowel obstruction has a very low mortality rate if it is simple. • Strngulating obstruction increases the mortality and if small bowel resection is required, esp. in the elderly, the mortality rate may reach 25% Appendicitis • When there is an obstruction in the lumen of the appendix either by a faecolith or foreign body or by enlargement of lymphoid follicles in its wall. • Most often children, teenagers and young adults. • Rare in the extremes of life. • Rare causes include carcinomas of the caecum obstructing the appendiceal lumen, carcinoid tumours and obstructing fibrous bands Symptoms and signs • Central abdominal cramping or colicky pain • Nausea. Vomiting is uncommon. • Occasionally the patient may pass a loose stool • Central abdominal pain lasts approximately 8hours • It is followed by the development of a sharp, stabbing somatic type of pain in the RIF made worse by coughing or moving • Low grade pyrexia(37.2-37.8C) • White furred tongue • Tachycardia • Tender with guarding in RIF over McBurney’s point • PR examination: tender anteriorly in the rectovesical or rectouterine pouch • In infants diarrhoea and vomiting may be the only symptoms. This may lead to difficulty in diagnosis and confusion with gastroenteritis. • In elderly patients there may be confusion and later shock may develop. Investigations • WCC: usually > 10X109/L with neutrophil leukocytosis • USS: may show a mass or abscess; not useful in early appendicitis DD: DD • In the classical case: mesenteric adenitis, Meckel’s diverticulitis, Crohn’s disease(regional ileitis);mesenteric embolus and right sided colonic diverticulitis • In the atypical case, other causes of intra-abdominal pathology, urinary tract disease, gynecological problems and extra-abdominal conditions must considered. • Abdominal disease: cholecystitis, gastroenteritis, pancreatitis, perforated DU, intestinal obstruction, diverticulitis, non-specific abdominal pain • Urinary tract: acute pyelonephritis, renal colic, cystitis, • Gynecological causes: salpingitis, ectopic pregnancy, degeneration of a fibroid, Mittelschmerz. Pelvic inflammatory disease • Extra-abdominal causes: referred pain from nerve roots, e.g. herpes zoster; right lower lobar pneumonia, right-sided testicular torsion • The treatment of acute appendicitis is Appendicectomy. Prophylactic metronidazole should be given 1hour preoperatively to reduce the risk of wound infection. Complications • It may resolve spontaneously • It may give rise to an Appendix mass • It may perforate giving rise to generalized peritonitis or it may perforate amidst of local adhesions giving rise to an Appendix abscess • if the symptoms have been there for 48hours(48hour rule) and the dx is truly appendicitis, then the patient should either have developed an appendix mass or generalzed peritonitis • If neither, then the DX should be reviewed Appendix mass • Omentum and small bowel adhere to the inflamed appendix • 2-5days after onset of initial symptoms • This should be initially treated conservatively. Mark out the site of the mass, IV fluids, analgesia and antibiotics • If the mass resolves, interval appendicectomy after 3months • If it gets bigger, it is likely that an abscess is forming Appendix abscess • The appendix mass enlarges and the temperature fails to settle • Patient may appear toxic with tachycardia • Either surgical drainage or appendicectomy, or percutaneous insertion of a drain under USS control. Interval appendicectomy requored later. • Other complications: subphrenic abscess, paralytic ileus, septicaemia, portal pyaemia Appendicitis in pregnancy • No commoner than at other times • Pain and tenderness are higher because of displacement of the appendix by the enlarging uterus • Prompt assessment and interventionare essential • Risk of abortion in the first trimester but if treatment is delayed until perforation occurs, the risk is considerably higher ~ 25% Volvulus • This a twisting of a loop of bowel around its mesenteric axis. Partial or complete obstruction may result. • Occlusion of the arteries at the base of the involved mesentery leads to gangrene and perforation Sigmoid volvulus • Middle-aged and elderly males are more often affected. • A large redundant sigmoid colon and constipation are predisposing factors Symptoms and signs • Sudden onset of lower abdominal colicky pain associated with gross abdominal distension • Distended tympanic abdomen • Investigations: AXR, distended loop of bowel the shape of a coffee bean arising out of the pelvis ; barium enema: the barium column resembles a bird’s beak. Treatment • Decompression by sigmoidoscopy. A rectal flatus tube should be left in situ for 48hours. • If the patient is fit, elective resection of the sigmoid is carried out at a later date • If decompression not successful, laparotomy with resection; • If decompression is not successful or signs of gangrene or perforation, laparotomy with resection, the two ends are brought out as a double-barreled colostomy(Paul Mickulicz procedure) Caecal volvulus • When caecum and ascending colon are excessively mobile(the caecum has retained its mesentery) • Sudden onset of abdominal pain, vomiting and constipation. Tympanitic mass in LUQ • Investigations: AXR🡪dilated caecum in LUQ • R/ Laparotomy. – If the bowel is viable, untwisting and caecostomy. Right hemicolectomy may be the best option as high recurrence rate – If gangrenous bowel, right hemicolectomy is required Large bowel obstruction • Major causes: carcinoma, diverticular disease and sigmoid colon • In 20%, the ileocaecal valve is competent and decompression into small bowel does not occur. Closed-loop obstruction therefore occurs with progressive distension of the caecum. Ischaemia and perforation of the caecum may occur. S&S • Colicky abdominal pain,constipation and vomiting(late) • Constant severe pain suggests ischemic bowel • Distended tympanitic abdomen • Obstructed bowel sounds • Rectum may be empty on PR Investigations • Sigmoidoscopy: rectosigmoid lesions may be seen • AXR: distended large bowel with air/fluid levels surrounding the abdomen • Limited barium enema 🡪”apple core” lesion Treatment • Drip and suck. Correct electrolyte imbalance • A caecum 10cm or > in diameter on radiograph is urgent indication for surgery • Laparotomy with decompression of the obstruction • Right sided lesions: right hemicolectomy; left sided lesions by left hemicolectomy with covering colostomy • Low left-sided lesions: resection of the tumour with Hartmann’s procedure Anal conditions • Haemorroids • Rectal prolapse • Perianal haematoma • Fissure-in-ano • Ano-rectal abscesses • Fistula-in-ano • Pruritus ani Haemorroids • Enlarged vascular cushions in the lower rectum and anal canal • They are not simply varicosities. At least 10% of the population have symptomatic haemorroids at some time in life • The classical position corresponds to branches of superior haemorroidal artery occurring at the 3 o’clock, 7 o’clock and 11 o’clock positions with the patient in lithotomy position S&S • Asymptomatic, Rectal bleeding, Prolapse, Itching • Piles are not painful unless they thrombose • 1st degree piles remain in the rectum • 2nd degree piles prolapse on defaecation but reduce spontaneously • 3rd degree piles prolapse and require manual reduction Investigations • Sigmoidoscopy • Proctoscopy • Barium enema (if any doubt as to the cause of bleeding) Treatment • Injection treatment: 2-3ml of phenol in almond oil into the submucosa above the pile • Other non-operative approaches: rubber band ligation, cryosurgery and photocoagulation • Large 2nd and 3rd degree piles: haemorroidectomy • Thrombosed piles: bed rest, analgesia, ice packs or emergency hemorroidectomy • Regulation of bowel habits with high-fibre diet Complications of haemorroidectomy • Acute retention of urine • Haemorrrhage • Stricture Rectal prolapse • May be partial or complete • Partial 🡪 mucosa alone; no more than a few cm • Complete 🡪 all layers of the rectal wall • S &S: protruding mass from anus esp. during defaecation. May reduce spontaneously. May need manual reduction and eventually becomes difficult to reduce. Blood and mucus PR from ulceration of exposed mucosa • Differential Dx: prolapsing hemorroids, polyps, intussusception • Treatment – Mucosal prolapse: sclerosants (as for piles) – Complete prolapse: abdominal rectopexy (Ripstein’s procedure). Other procedures are Delorme procedure or Thiersch wire Peri-anal haematoma • Acute peri-anal pain. Worse on sitting, walking and defaecation. • Tense, smooth, tender blue lump at anal verge • R/ – symptoms may subside spontaneously after 2-3 days during which analgesia is given – If patient presents in acute phase, incision under LA Fissure-in-ano • A tear at the anal margin due to passage of a constipated stool • It is usually in the midline posteriorly but may be occasionally anterior • Multiple fissures --? Crohn’s disease • S&S: acute anal pain, severe on defaecation. Blood on toilet paper. Part the buttocks and they may be apparent. Acute sphincter spasm. Examination PR is impossible. Occasionally “sentinel” pile. • Differential Dx: trauma, carcinoma, TB, herpes, Crohn’s disease, syphilis • Treatment – Conservative if mild symptoms: • LA gel or suppository(1/2hr before defaecation); stool softening laxative and high-fibre diet • Apply 0.2% GTN ointment locally bid x 6weeks 🡪relax internal sphincter – Surgical: a lateral subcutaneous internal sphincterotomy to relieve spasm. Laxative and high-fibre diet. Recurrent fissure should be excised and sent for histology Anorectal abscess • These develop in tissue spaces adjacent to the anorectal area. • They may be – Perianal (in a hair follicle, sebaceous gland or perianal haematoma) – Ischio-rectal (in the ischio rectal fossa) – Intermuscular (between internal and external sphincters) – Pelvirectal (from a pelvic abscess) • S& S: constant, throbbing, perianal pain worse on sitting. Lower abdominal pain with pelvirectal abscess. Indurated tender mass perianally. Boggy mass on examination PR. Fever. • Treatment: prompt surgical drainage to prevent fistula formation. No role of antibiotics except in Diabetics and Immunocompromised. Fistula-in-ano • A fistula is abnormal communication between two epithelial surfaces. • There is internal opening in the anal canal and one or more external openings on the perianal skin • The majority arise from delay in treatment or inadequate treatment of anorectal abscesses • Rare causes: TB, Crohn’s disease, carcinoma Goodsall’s law • It may be difficult to locate the internal opening. • If the external opening lies anterior to a line drawn transversely through the center of the anus, the track passes radially through a straight line towards the internal opening. If the external opening is behind this line the track curves in a horseshoe manner to open into the midline posteriorly. Classification • Subcutaneous • Submucous • Low anal(below pubo rectalis) • High anal(opening in close relation to the anorectal junction) • Pelvirectal(penetrating levator ani) Symptoms and signs • History of abscess which drains spontaneously or was surgically drained • Persistent drainage of pus, mucus, blood or faecal matter associated with perianal irritation and discomfort • Drainage may be intermittent • Single opening near the anus • examinationPR: indurated track, pressure on which may cause discharge • Proctoscopy or sigmoidoscopy to define internal openings Treatment • The track is identified by probing and laid open under GA, so that it heals by granulation tissue from the base • With high fistulae, there is a danger to puborectalis when opening the track. Incontinence may result. They require specialist treatment often by a two-staged operation