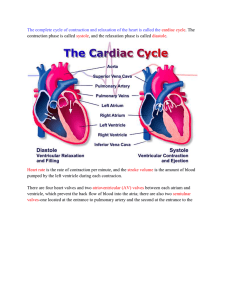
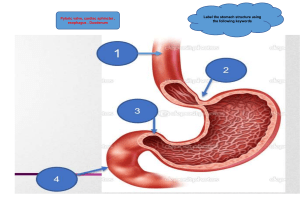
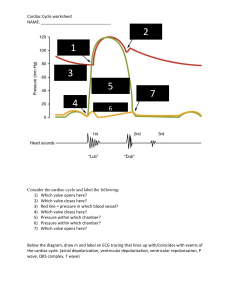
Heart Anatomy Layers of the Heart ● Endocardium: Innermost layer; lines inner chambers and valves. ● Myocardium: Actual contractile layer of the heart. ● Pericardium: Covers the outer surface of the heart, composed of two layers: ○ Visceral: Overlies the organ, closely adheres to the heart. ○ Parietal: Outermost tough fibrous layer. Heart Valves ● Tricuspid Valve: Three-pointed valve located between the right atrium (RA) and right ventricle (RV). ● Mitral/Bicuspid Valve: Two-pointed valve resembling a bishop's miter, located on the left side of the heart. ● Anchoring: Heart valves are anchored in the innermost layer (endocardium). Chambers of the Heart ● Atria: Receiving chambers that receive blood from the vena cava. ○ Right Atrium: Receives poorly oxygenated blood. ○ Left Atrium: Receives oxygen-rich blood from the lungs via pulmonary veins. ● Ventricles: Pumping chambers that receive blood from the atria. ○ Left Ventricle: Largest and most muscular; pumps oxygen-rich blood to the body. ○ Right Ventricle: Pumps blood to the pulmonary tree for oxygenation. Coronary Arteries and Cardiac Conduction Coronary Arteries ● Function: Responsible for delivering blood to the heart. ● Right Coronary Artery: Supplies blood to the right atrium, right ventricle, and other structures. ● Left Anterior Descending Artery: Supplies the anterior wall of the left ventricle and other areas. ● Left Circumflex Artery: Supplies the left atrium, lateral and posterior surfaces of the left ventricle. Cardiac Conduction System ● SA Node: Natural pacemaker of the heart with a firing rate of 60-100 bpm. ● AV Node: Delays the electrical signal to allow ventricles to fill with blood. ● Bundle of His and Purkinje Fibers: Transmit electrical signals to cause ventricular contraction. Cardiac Electrophysiology and Pathway Cardiac Electrophysiology ● Properties: Excitability, automaticity, conductivity, contractility, refractoriness. ● Depolarization: Stimulation followed by systole; Repolarization: Electrical relaxation. ● Systole and Diastole: Represent mechanical contraction and relaxation of the heart. Cardiac Electrical Stimulation Pathway ● SA Node: Initiates electrical signal; AV Node pauses signal for ventricular filling. ● Bundle of His and Purkinje Fibers: Transmit signals for ventricular contraction. ● Step-by-Step Process: SA node → Atria contraction → AV node delay → Ventricular contraction. Cardiac Output and Regulation Determinants of Cardiac Output ● Preload: Volume of blood entering the heart affecting contraction strength. ● Contractility: Ability of heart muscles to eject blood effectively. ● Afterload: Resistance the left ventricle must overcome to pump blood out. Regulation of Cardiac Function ● Intrinsic Factors: Venous return and preload within the heart. ● Extrinsic Factors: Hormonal (thyroid hormones, catecholamines) and nervous (SNS, PNS) regulation. Baroreceptors and Chemoreceptors Baroreceptors ● ● ● ● Location: Found in the aorta (aortic arch) and carotid arteries Function: Monitor the pressure of ejected blood High Pressure Response: Activates the Parasympathetic Nervous System (PNS) Low Pressure Response: Activates the Sympathetic Nervous System (SNS) Chemoreceptors ● ● ● ● Location: Coordinated in the Cardioregulatory Center in the medulla oblongata Monitor: Blood pH levels Acidosis Response: Activates the SNS Alkalosis Response: Activates the PNS Risk Factors for Cardiovascular Diseases Race ● Description: Black Americans have a higher incidence of hypertension ● Impact: Increased blood pressure leading to vessel wall thickening and potential complications like aneurysm Sex and Estrogen Effects ● Men vs. Women: Men have higher risk due to lifestyle factors; women's risk increases post-menopause ● Estrogen Effects: Cardioprotective effects include increasing HDL and decreasing LDL Lifestyle Factors ● Sedentary Lifestyle: Increases risk factors for cardiovascular diseases ● Faulty Diet: High intake of cholesterol and saturated fats contributes to the risk Other Risk Factors ● Age: Increased risk with aging and family history of coronary atherosclerosis ● Cigarette Smoking: Nicotine impacts blood pressure, heart rate, and platelet activation ● Type A Personality, Obesity, Diabetes Mellitus, and Stress: Each factor contributes to cardiovascular risk through various mechanisms Assessment Findings and Detailed Assessment Symptoms and Associated Conditions ● ● ● ● ● ● Chest Pain: Indicates myocardial ischemia Cyanosis: Linked to decreased cardiac output or congenital conditions Fatigue: Result of poor circulation affecting energy levels Syncope: Fainting due to low perfusion Dyspnea: Difficulty in breathing, a common symptom in cardiac issues Palpitations: Awareness of irregular heartbeats Detailed Assessment Techniques ● Observation: Includes assessing appearance, pillow use, facial expressions, skin color, and cognitive status ● Weight Management: Sudden weight gain may indicate fluid retention ● Eye and Skin Assessments: Arcus Senilis and Xanthelasma are indicative of high cholesterol levels ● Tests: Include the Blanch Test, Schamroth Test, and assessment of skin turgor for elasticity Cardiac Assessment Techniques ● Carotid Arteries: Caution against assessing both simultaneously to avoid vagal stimulation ● Jugular Vein Distention (JVD) Assessment: Use of rulers to measure venous pressure ● Precordium Landmarks & Heart Sounds: Description of normal and abnormal heart sounds and their locations Lungs and Abdomen Assessment ● Lungs Assessment: Includes findings like tachypnea, crackles, and Cheyne-Stokes Respirations ● Abdomen Assessment: Observations related to obesity, ascites, hepatomegaly, and auscultation Diseases Affecting Cardiac Function Mechanisms of Compensation ● SNS Activation, Cardiac Dilation, and RAAS Activation: Responses to decreased cardiac output ● Aldosterone Role: Promotes sodium retention to improve blood volume and perfusion adequacy Symptom Analysis for Chest Pain ● Causes: Lactic acid buildup during myocardial ischemia, Angina Pectoris, and other potential origins of chest pain Esophageal Disorders and Musculoskeletal Issues Esophageal Disorders ● Hiatal Hernia or Reflux Esophagitis: Characterized by epigastric burning sensation. ● Anxiety and Panic Disorders: Often manifest as burning sensations, triggered by emotions like anger, depression, and anxiety. Musculoskeletal Problems ● Costochondritis: Inflammation of rib connective tissues causing tenderness upon movement. Respiratory Manifestations and Cardiovascular Conditions Respiratory Manifestations ● Dyspnea: Difficulty breathing. ● Exertional Dyspnea: Breathing difficulty during exertion, assessed by the ability to complete sentences. ● Orthopnea: Severe dyspnea requiring a 3-point position due to increased blood return to the heart and lungs when supine. ● Paroxysmal Nocturnal Dyspnea (PND): Sudden nighttime breathing difficulty linked to left-sided heart failure. Cardiovascular Conditions ● ● ● ● Irregular Heart Rhythm (Dysrhythmias) Syncope: Fainting due to poor cerebral perfusion. Nape Pain: Associated with hypertension. Weight Gain: Linked to conditions like edema and dependent edema. Valvular Defects and Congenital Heart Conditions Mitral Valve and Valvular Assessment ● Mitral Valve: An atrioventricular valve prone to regurgitation, causing backflow. ● Murmur: Audible in affected valves like aortic, pulmonic, tricuspid, and mitral valves. ● Valvular Defect Assessment: Specific landmarks for auscultation of aortic, pulmonic, tricuspid, and mitral valves. Congenital Heart Defects ● Atrial Septal Defect: Abnormal opening between atria, leading to increased pulmonary blood flow. ● Ventricular Septal Defect: Increased pulmonary blood flow with backflow into the right ventricle. ● Patent Ductus Arteriosus: Failure of fetal artery closure, causing abnormal blood flow. ● Coarctation of the Aorta: Narrowing leading to blood flow obstruction. ● Tetralogy of Fallot: Combination of four defects causing cyanosis. ● Transposition of Great Arteries (TOGA): Abnormal positioning of pulmonary artery and aorta causing cyanosis. Laboratory Examinations and Diagnostic Tests Cardiac Enzymes & Markers ● ● ● ● CK-MB: Early marker for myocardial infarction. Troponin I and T: Indicators of cardiac damage. Lactate Dehydrogenase: Enzyme showing cardiac injury over time. Myoglobin: Early diagnostic marker for cardiac issues.