GI System Assessment: Structures, Functions, and Diagnostics
advertisement

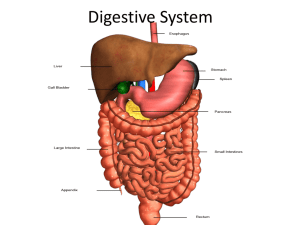
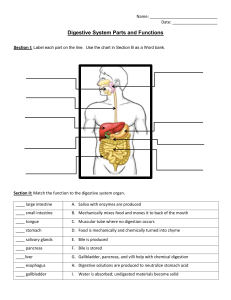
43: Assessment: Gastrointestinal System Structures and Functions of Gastrointestinal System The GI tract is essentially a tube composed of 4 layers. From the inside to the outside (1) Mucosa lining (2) Submucosa connective tissue, which contains glands, blood vessels, and lymph nodes; (3) Muscle (There are 3 smooth muscle layers: the oblique (inner) layer, circular (middle) layer, and longitudinal (outer) layer.) (4) Serosa. MSMS…my sis my sis GI Nervous system… ● The parasympathetic (cholinergic) system is mainly excitatory. The sympathetic (adrenergic) system is mainly inhibitory. For example… ● parasympathetic stimulation increases peristalsis, ● sympathetic stimulation decreases it. The GI tract has its own nervous system: the enteric nervous system (ENS) or intrinsic nervous system. ● ENS is composed of 2 networks: (1) Meissner plexus in the submucosa: The submucosal plexus controls secretion and is involved in many sensory functions. (Meissner plexus…Messyyyyyy plexus because is controls messy secretions and senses) (2) Auerbach (myenteric) plexus between the muscle layers :myenteric plexus is the major nerve supply to the GI tract and controls GI movements. ( myenteric plexus…Auerbach gets on MY nerves…because auerbach myenteric is a never supply to GI track) The main function of the GI system supply nutrients to body cells. …This is accomplished through the processes of (1) ingestion (taking in food) (2) digestion (breaking down food) (3) absorption (transferring food products into circulation). Elimination is the process of excreting the waste products of digestion. Ingestion -the intake of food and out appetite influences how much we eat -involves the mouth, pharynx, and esophagus -our appetite center is in our hypothalamus -Deglutition, or swallowing, is the mechanical portion of ingestion. The organs involved in deglutition are the mouth, pharynx, and esophagus. Factors that stimulate appetite ● hypoglycemia ● an empty stomach ● decrease in body temperature ● The hormone ghrelin released from the stomach mucosa plays a role in appetite stimulation. Factors that inhibit appetite ● Hormone Leptin ● Stomach distention ● illness (especially accompanied by fever) ● Hyperglycemia ● nausea and vomiting, and certain drugs (e.g., amphetamines) inhibit appetite. Digestion and absorption Digestion is the physical and chemical breakdown of food into absorbable substances. The timely movement of food through the GI tract and the secretion of specific enzymes promote digestion. These enzymes break down food to particles of appropriate size for absorption The process of digestion begins in the mouth, where food is chewed, mechanically broken down, and mixed with saliva. Saliva helps us swallow by lubricating food. Saliva contains amylase, which breaks down starches to maltose. Chewing and the sight, smell, thought, and taste of food stimulate the release of saliva. A person makes about 1 L of saliva each day. After swallowing, food moves through the esophagus to the stomach. No digestion or absorption occurs in the esophagus. -the small intestine takes nutrients from the gut lumen to the bloodstream.it is the longest portion of the GI tract Elimination(Large intestine) -Peristalsis is most active after first meal -The large intestine is a hollow, muscular tube around 5 to 6 ft (1.5 to 1.8 m) long and 2 in (5 cm) in diameter. -The most important functions of the large intestine are water and electrolyte absorption. -The large intestine also forms feces and serves as a reservoir for the fecal mass until defecation occurs. -The large intestine secretes mucus, which acts as a lubricant and protects the mucosa. The colon is the largest part of the large intestines…Microorganisms in the colon contribute to digestion by (1) producing vitamin K and some B vitamins and (2) breaking down proteins that are not digested or absorbed in the small intestine into amino acids. Liver, Biliary Tract, and Pancreas The liver performs many functions and is essential for life. It has metabolic, secretory, vascular, and storage functions VALSALVA MANEUVER-bearing down And leads to decreased HR, CO and BP -this is contraindicated in head injuries and eye surgery because you dont wanna add any extra pressure also heart issues, hemorrhoids, abdominal surgery, and liver cirrhosis w/portal hypertension For GI bleeds they are on fall risk because they are loosing blood and they bear down …double homicide Liver functions Function Description Metabolic Functions Blood clotting Synthesis of prothrombin (factor I), fibrinogen (factor II) and factors V, VII, IX, and X. Carbohydrate metabolism Performs glycogenesis (conversion of glucose to glycogen), glycogenolysis (process of breaking down glycogen to glucose), gluconeogenesis (formation of glucose from amino acids and fatty acids). Detoxification Inactivates drugs and harmful substances and excretes their breakdown products. Fat metabolism Synthesis of lipoproteins, breakdown of triglycerides into fatty acids and glycerol, formation of ketone bodies, synthesis of fatty acids from amino acids and glucose, synthesis and breakdown of cholesterol. Protein metabolism Synthesis of nonessential amino acids, synthesis of plasma proteins (except gamma globulin), synthesis of clotting factors. Bacteria in colon deaminate amino acids to form ammonia (NH3), which is then changed to urea (NH4). Secretory Functions Bile production Formation of bile, which contains bile salts, bile pigments (mainly bilirubin), and cholesterol. Bilirubin Conjugation and secretion of bilirubin. Vascular Functions Blood filtration Breakdown of old RBCs, WBCs, bacteria, and other particles. Breakdown of hemoglobin from old RBCs to bilirubin and biliverdin. Blood reservoir Serves as temporary storage for blood within general circulation. Storage Functions Storage Stores glucose in form of glycogen; vitamins, including fat-soluble (A, D, E, K) and water-soluble (B1, B2, cobalamin, folic acid); fatty acids; minerals (iron, copper); and amino acids in form of albumin and β-globulins. Biliary tract -The biliary tract consists of the gallbladder and ducts that connect the liver, gallbladder, and duodenum. The gallbladder is a pear-shaped sac found below the liver. Its function is to concentrate and store bile. It holds around 45 mL of bile. The presence of fat in the upper duodenum triggers the release of cholecystokinin, which causes the gallbladder to contract and release bile. Pancreas -The pancreas is a long, slender gland lying behind the stomach and in front of the first and second lumbar vertebrae. It consists of a head, body, and tail - The exocrine function of the pancreas contributes to digestion. Theendocrine function occurs in the islets of Langerhans, whose cells secrete insulin, cells secrete glucagon, and cells secrete somatostatin. Gerontologic Considerations: Effects of Aging on GI System ● Aging changes the functional ability of the GI system. ● Many factors can lead to a decrease in appetite and make eating less pleasurable, including caries and periodontal disease, fewer taste buds, a lessened sense of smell, and decreased saliva production. ● The liver size decreases after 50 years of age, but liver function tests stay within normal ranges. ● The ability to metabolize drugs and hormones decreases. ● Risk for decreased food intake and ability to obtai Structures Located in Abdominal Regions Right Upper Quadrant • Liver and gallbladder • Pylorus • Duodenum • Head of pancreas • Right adrenal gland • Portion of right kidney • Hepatic flexure of colon • Portion of ascending and transverse colon Left Upper Quadrant • Left lobe of liver • Spleen • Stomach • Body of pancreas • Left adrenal gland • Portion of left kidney • Splenic flexure of colon • Portion of transverse and descending colon Right Lower Quadrant • Lower pole of right kidney • Cecum and appendix • Portion of ascending colon • Bladder (if distended) • Right ovary and fallopian tube • Uterus (if enlarged) • Right spermatic cord • Right ureter Left Lower Quadrant • Lower pole of left kidney • Sigmoid flexure • Part of descending colon • Bladder (if distended) • Left ovary and fallopian tube • Uterus (if enlarged) • Left spermatic cord • Left ureter Normal assessment of GI system Mouth • Moist and pink lips • Pink and moist buccal mucosa and gingivae without plaques or lesions • Teeth in good repair • Protrusion of tongue in midline without deviation or twitches • Pink uvula (in midline), soft palate, tonsils, and posterior pharynx • Swallows smoothly without coughing or gagging Abdomen • Flat without masses or scars. No bruises • Bowel sounds in all quadrants • No abdominal tenderness; nonpalpable liver and spleen • Liver 10 cm in right midclavicular line ( The liver edge should feel firm, sharp, and smooth) • Generalized tympany Anus • Absence of lesions, fissures, and hemorrhoids • Good sphincter tone • Rectal walls smooth and soft • No masses • Stool soft, brown, and heme negative Look at table 43.10 for abnormal findings Diagnostic Studies- table 43.11 DIAGNOSTIC STUDIES OF GASTROINTESTINAL SYSTEM ● Many of the diagnostic procedures of the GI system require measures to cleanse the GI tract, as well as the use of a contrast medium or a radiopaque tracer. ● An upper GI series with small bowel follow through provides visualization of the esophagus, stomach, and small intestine. ● A lower GI series (barium enema) x-ray examination is done to detect abnormalities in the colon. ● Ultrasonography shows the size and configuration of solid organs. ● Virtual colonoscopy combines computed tomography (CT) scanning or magnetic resonance imaging (MRI) to produce images of the colon and rectum. ● GI structures that can be examined by endoscopy include the esophagus, stomach, duodenum, and colon. Retrograde cholangiopancreatography (ERCP) is an endoscopic procedure that visualizes the pancreatic, hepatic, and common bile ducts. ● Capsule endoscopy is a noninvasive approach to visualize the GI tract. ● Liver biopsy is done to obtain tissue for diagnosing cancer and staging of fibrosis. ● Liver function tests reflect hepatic disease and function. - Test Reference Interval Description and Purpose Blood Studies Amylase 60–120 U/L (30–220 U/L) Enzyme secreted by pancreas. Important in diagnosing acute pancreatitis. Level peaks in 24 hr and then returns to normal in 48–72 hr Gastrin 25–100 pg/mL when fasting Hormone secreted by cells of the antrum of the stomach, the duodenum, and the pancreatic islets of Langerhans Lipase 0–160 U/L Enzyme secreted by pancreas. Important in diagnosing pancreatitis. Level stays higher longer than serum amylase in acute pancreatitis Fecal analysis Note form, consistency, and color. Specimen examined for mucus, blood, pus, parasites, and fat content Teach patient to keep diet free of red meat for 24–48 hr before occult blood test Fecal DNA testing Negative Detects shredded cell debris from polyps, adenomas, and cancers Fecal occult blood Negative Detects blood in stool related to the presence of inflammatory bowel disease, diverticulosis, ulcers, cancer, and other GI problems Stool culture Normal intestinal flora Tests for the presence of bacteria, including Clostridium difficile Fecal Tests For liver function tests look at chart 43.13 A Lot of people with gastric problems complain of left arm pain Avoid using straws because of extra air LOOK AT QUESTION AT END OF CHAPTER