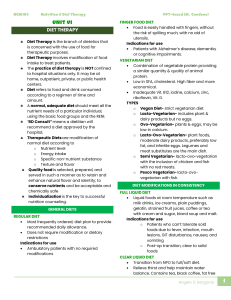
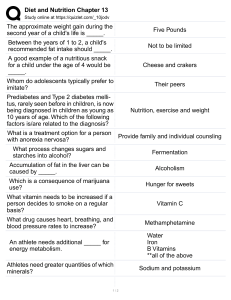
BACHELOR OF SCIENCE IN NURSING: NUTRITION AND DIET THERAPY COURSE MODULE COURSE UNIT WEEK 2 9 10 Nutrition Education and Counseling Read course and unit objectives Read study guide prior to class attendance Read required learning resources; refer to unit terminologies for jargons Proactively participate in classroom discussions Participate in weekly discussion board (Canvas) Answer and submit course unit tasks At the end of this unit, the students are expected to: Cognitive 1. Describe the need for and the factors to consider in planning for a therapeutic diet. 2. Differentiate the types of dietary modification. A. General Diets B. Diets modified in consistency C. Diets modified in composition D. Liquid Diets E. Soft Diets F. Test Meals 2.1. Good Tray Service 3. Determine the appropriate therapeutic diet specific to a patient’s health condition. A. Obesity and Weight Control B. Diabetes Mellitus C. Diseases of the Gastrointestinal Tract D. Diseases of the Lliver, Gallbladder, and Pancreas E. Cardiovascular Diseases F.Diseases of the Kidneys G. Cancers H. Immune Deficiency Syndrome 4. Deduce the role of the nurse in nutritional care. 5. Discuss the patient’s (individual and/or the family) need for nutrition education. 6. Describe the nutrition education process. 7.Utilize selected behavioral theories as guide in the teaching-learning process. A. Health Belief Model B. Self- Efficacy Theory C. Stages of Change Model D. Theory of Reasoned Action and Theory of Planned Behavior E. Therapeutic Alliance Model 8. Determine the patient’s (individual and family) need for nutritional counseling. 10. Refer patients (individual and/or the family) to the appropriate agency for their needs related to nutrition as needed. Affective 1.Express the necessity of the nurse to conscientiously monitor patients’ progress. 2. Demonstrate diligence in preparing and presenting nutrition education and nutritional counseling. 3. Display warmth to patients during the nurse-patient interaction. 4.Utilize the therapeutictechniques in communication during the nurse-patient interaction. 5. Follow standards in documenting and reporting nutrition care process/nutritional Counseling implemented. Psychomotor 1. Draft a teaching plan for the nutritional education of a given patient, using the following: A. Goal B. Objectives C. Content D. Methodology E. Resources needed F. Indicators 2. Plan a Counseling Session for a patient with specific nutritional need. I.Modified Diets Illness affects numerous bodily processes, including how one nutrients are being processed; A sick person’s usual interest in food may change and the disease process may put limitations to his/her food choices and thus, food acceptance. Patients are affected by the dynamics of Illness and food acceptance - thus the need to modify the diet. Nutrients are required to control illness and sustain life. The nurse will play specific roles in the patient’s and/or the family’s nutritional care. Diet Therapy may be a specific treatment of a disease or a supplement of other modes of treatment that a patient may go through. Included in its purposes are maintenance of normal nutrition; correction of nutritional deficiency, changes in body weight and adjusting the body’s ability to use one or more nutrients. Normal Diet (also known as regular, general or house diet) is the foundation on which therapeutic diet modifications are based. Regardless of the type of diet prescribed, the purpose of the diet is to supply needed nutrients to the body in a form it can handle. Modification of this diet include: a. consistency and texture b. flavor c. energy value d. nutrient level e. food category Standard hospital diets are: A. Liquid diets a. Clear Liquid Diet : indicated for patients experiencing acute vomiting, diarrhea or surgery; the diet is used for 24-48 hours; it allows tea, coffee or coffee substitute and fat-free broth. b. Full Liquid Diet: used for acute infections and fever of short duration; patients who’ are too ill to chew. It consists of liquids and foods that liquefy at body temperature, generally offered in 6 feedings or more. B. Soft diets These diet is often used immediately between full fluid diet and the regular diet following surgery, acute infections and fevers, and in GI disturbances. It has reduced fiber content, bland flavor and soft consistency. Modifications are done by having the meat and poultry being minced or ground; Vegetables are diced, chopped or cooked longer than usual; the use of soft raw fruits and the use of soft rolls, breads or biscuits. C. Test Meals : used for specific diagnostic tests such as a. Fecal Fat Determination – to measure fat globules to detect fat absorption. b. Meat-free Test – to determine GIT bleeding . c. Calcium Test – to determine urinary calcium excretion. d. Serotonin Test – to detect calcinoid tumors of the intestinal tract. I.2.Good Tray Service Tray service is a style of service that makes use of a tray and does not make use of the usual dining table; dishes and utensils are arranged in a tray and brought to the patient in his/her room.Essentials of good tray service are as follows: 1. Sufficient size of the tray for un crowded arrangement. 2. Clean, unwrinkled tray cover and napkin or good quality paper. 3. Attractive pattern of spotless chinaware without chips or cracks; clean glassware and shining silverware. 4. An orderly arrangement of all items on the tray. 5. Food portions are suitable for the patient’s appetite. 6. Foods are attractively arranged with the appropriate garnishing. 7. Meals are served on time; Hot foods served warm and cold foods served chilled. 8. Trays are served promptly to the patient. II. Therapeutic Diets A.Nutrition Therapy for Obesity and Weight Control Obesity is said to be a state of adiposity in which body fat is above the ideal weight. Assessment will show a body mass index of 30 – 39.9.Whereas, being overweight is having a body mass index of 25 – 29.9 or greater. Often this results from an imbalance of the complex system of neural, hormonal and chemical mechanisms that keeps the balance between energy intake and energy expenditure. There are reasons why an individual may have an excessive intake of calorie; but obesity can be prevented and the intention to lose weight is planned. A Low calorie Diet and exercise may help in weight control. B.Nutrition Therapy for Diabetes Mellitus Diabetes Mellitus is a condition that results from the lack of insulin produced by the Body. This metabolic problem affects the use of carbohydrates and fats by the body. Hyperglycemia or hypoglycemia often occur. These signs along with the excess in weight can be prevented by controlling the amount of food and their distribution in meals in a day to day basis. Patients may initially be placed on a low calorie diet; those with normal weight are given sufficient calories to maintain their weight. Protein of about 11/2 per kg body weight may be allowed ; the same may be given to the amount of fat allowed. The amount of carbohydrate is roughly twice the number of protein. Menu Plan follows the recommended Food Exchange List. C.Nutrition Therapy for Diseases of the Gastrointestinal Tract Dietary modifications in disorders of the intestinal tract are designed to alleviate symptoms , correct nutrient deficiencies, and where possible, address the primary cause of the difficulty. The nature of the modification will depend on the medical condition that the patient has. Bland diet may be prescribed to manage Peptic ulcer. This diet must meet nutritive adequacy, bland flavor and soft consistency, and mechanically and chemically non-stimulating. Long term use is not recommended as this may lead to the patient becoming malnourished. Management of Diverticular diseases may include the increase of fiber in the diet, with Bran, whole grains and cellulose foods to reduce muscle contractions and facilitate normal muscle tone. Celiac sprue and Non-tropical sprue will show intolerance for gluten; thus food sources containing gluten are removed from the diet. A high-protein diet is usually necessary, along with supplements of minerals and vitamins. A diagnosis of Ulcerative colitis – where there is an inflammation of the colon and the rectum - implies a diet with high calorie, high protein, high vitamins and mineral. In its acute stages, the patient is placed on a Low-residue diet , avoiding heavy roughage to prevent irritation. Lactose intolerance is a condition brought about by a deficiency in the enzyme lactase; the lactose (sugar in milk) then, cannot be hydrolyzed. A lactoserestricted diet is prescribed. Milk, milk-products, foods containing whey and casein are avoided. Patients suffering from diarrhea may initially be placed on NPO for 12 hours with IVT support; as the condition improves, Oral fluids may be given liberally to prevent Dehydration. Broths and rehydration solutions are given to replace the electrolytes lost as well as foods rich in pectin. Constipation is also a problem that is commonly experienced. It may have a variety of Causes but the management often includes high –fiber diet and liberal fluid intake. Intestinal gas is controlled by excluding gas-producing foods; the patient is advised to take small frequent meals and to chew food thoroughly. Hemorrhoids are managed with intake of high –fiber diet, liberal fluids and avoidance of highly-seasoned foods and relishes. Gastroesophageal reflux disease, hiatal hernia and esophagitis is a condition that takes place 1 to 4 hours after a meal when a decrease in sphincter pressure happens. Maintaining the ideal body weight is recommended; Dietary management includes avoiding foods high in fat and eating of large meals. Protein and carbohydrate foods with low-fat content are preferred as these do not affect the lower esophageal sphincter pressure. D. Nutrition Therapy Diseases of the Lliver, Gallbladder, and Pancreas Hepatitis is the inflammation of the liver. Diet Therapy includes protein coming from animal sources as these are considered to have a superior quality. Additional serving of foods rich in protein is recommended – like an additional milk, an extra egg, as well as meat, fish and cheese. Caloric intake must also be adjusted to meet the body’s energy needs. Patients with fever may have 2,500 to 4,000 calories per day. Fat should be taken in moderation. The foods added to the diet are sufficient to meet the daily requirements for minerals and vitamins. Protein is often depleted in patients with cirrhosis. Often a 100 g protein is given, with Sodium restriction to 250 mg a day; and a 1,800 calorie diet is recommended. Fat restriction is not necessary. Patients with hepatic coma are prescribed with a high calorie diet. Cholecystitis may be managed with a low-fat diet, to avoid stimulating the gallbladder. Spices and high-residue foods are avoided as these can cause distention and increase in peristalsis. Selection of food items must be carefully done as these may either be restricted or limited. There also items to be excluded from food preparation such as the use of butter, margarine and sauces as vegetable dressing; instead, lemon juice vinegar or low-calorie, fat-free dressings are used. Patients with pancreatitis are placed on low-fat, low-elemental formulas when enteral feeding is appropriate. During acute attacks, the patient may be placed on NPO for 48 hours. In chronic cases, the diet is high calorie, moderate protein and low to moderate fat. On the other hand, patients with cystic fibrosis are given high-protein diet to compensate for fecal losses, with liberal fat intake. Calories are often according to the need for growth. E. Nutrition Therapy for Cardiovascular Diseases Atherosclerosis is caused by the accumulation of fatty materials including a high proportion of cholesterol and other substances in the blood vessel, causing it to narrow. Thus Dietary management is low-fat, low in saturated fat and cholesterol (300 mg/day). Increase in monounsaturated fatty acid, polyunsaturated fats, omega-6 and omega-3 fatty acids – with at least 2 servings per week are recommended to decrease plasma cholesterol levels. Simple sugars are restricted. Complex carbohydrates and dietary fiber are increased to 25-30 g/day and restriction of carbohydrates are also done. Congestive heart failure is managed by restricting sodium in the diet. Depending on the severity of the condition, sodium restriction may range from mild (2-3 g) to severe (250 mg) restriction. Low-fat diet with emphasis on unsaturated oils is recommended. Diet for patients with Myocardial infarction (MI) are designed to help reduce the work load of the heart. Small frequent meals are done; Liquid diet is used on the initial stages gradually progressing as the condition of the patient improves. Among the food items restricted are caffeine-containing beverages, sodium, cholesterol, fat and calorie. Consumption of omga-3 fatty acid-rich foods may be done to reduce blood clots. F. Nutrition Therapy for Diseases of the Kidneys Acute glomerulonephritis is a condition consequent to an antigen-antibody complex in which some of the complexes become ensnared in the glomeruli leading it to swell. Emphasis of nutritional care is the overall nutritional needs of the patient rather than the Restriction in protein; restriction in sodium is done only when edema is present. High Calorie from carbohydrates is recommended. Malnutrition may result from Nephrotic syndrome, as lesions in the nephrons can effect massive albuminuria and protein losses. Thus, recommended is a diet high calorie, and high protein, low sodium. In contrast, Acute renal failure patients are given high calorie, low to moderate protein and moderate fat diet. Adequate caloric intake prevents tissue break down; Potassium and sodium are controlled according to the patient’s capacity to excrete them. Water intake is also restricted to a liter a day and is carefully monitored. Renal calculi requires a large intake of fluids to dilute the urine and prevent concentration of stones. The type of stone present influence the nature of the diet. Such that: a. Calcium oxalate stones – low calcium, low phosphate or oxalate –according to the Calcium compound, acid ash. Calcium-rich foods are Eliminated; alkaline foods are controlled; potassium-rich Foods are increased. b. Uric acid stones – low purine; limited protein with emphasis of milk, fruits and Decreased intake of bread products. c. Cystine stones – High fluid intake, controlled intake of meat, milk, egg and cheese. G. Nutrition Therapy for Cancers Cancer is a group of many dissimilar diseases categorized by unfettered replication of Cells. The clinical status of the patient also warrants the appropriate route of feeding. Oral nutrition is high calorie, high protein. Tube feedings may range from complete products – meal replacements that require digestion and absorption; chemicallydefined products – minimal or no digestion – or Specialty products – which may vary in terms of amino acid, carbohydrate or fat content. Total parenteral nutrition may also be done when the digestive tract is not functioning well. H. Nutrition Therapy for Human Immune Deficiency Syndrome (HIV/AIDS) HIV/AIDS is an infection that is transmitted via sexual contact, transfusion of contaminated blood, sharing of contaminated needles and mother to child during pregnancy, childbirth or breast feeding. Nutritional management for patients with HIV/AIDS include Energy of 35 – 45 kcal/kg BW; Protein 2 – 2.5 g/kg BW ; Fats – increase in omega-3 sources and decrease in saturated fats in the diet; Vitamins and minerals - an increase to be recommended in case of altered metabolism. III. Nutrition Education and Counseling: Behavioral Change Patient education is a process of assisting people to learn health-related behaviors that can be used in their everyday life and achieve optimal health. It aims to increase the competence and confidence of clients for self-management; increasing the responsibility and independence of clients for self-care. A partnership approach can provide clients with opportunities to explore and expand their self-care abilities as they transition from being passive to active participants of their care. Behavioral Models that the nurse may use as guide include the following: 1. Health Belief Model : it explains and predicts health behaviors based on the Patient’s beliefs about the health problem and the health behavior. Its subcomponents include the individual’s perceptions, modifying factors and the likelihood of action. 2. Self-efficacy theory : this theory is based on a person’s expectations relative to a specific course of action. It deals with the belief that one is competent and capable of accomplishing a specific behavior. The behavior-specific predictions of this theory can be used for understanding the likelihood of individuals participating in existing or a planned educational program. 3. Stages of Change Model: This theory is useful in staging the client’s intentions and behaviors for change as well as to determine the strategies that will enable completion of a specific stage. The six stages that the authors used begins with 1.)Precontemplation 2.)Contemplation 3.)Preparation 4.)Action 5.) Maintenance 6.)Termination. Among its current applications are in health promotion and the processes by which people decide to change. 4.Theory of Reasoned Action and Theory of Planned Behavior: the premise of this theory is that humans behave in a rational way that is consistent with their beliefs; suggesting that a person’s behavior can be predicted by examining the individual’s attitudes about the behavior as well as the individual’s beliefs about how others might respond to the behavior. In designing the educational program for patients, nurses as educators need to take beliefs, attitudinal factors and subjective norms into consideration. 5.Therapeutic Alliance Model: Fundamental to this model is the shift toward selfdetermination and control over one’s own life. This model views the client as active and responsible, with an outcome expectation of self-care. The therapeutic alliance is formed when the nurse and patient views each other as having equal power. The therapeutic is significant as it relates to the patient’s adherence to therapeutic interventions and achievement of set goals. Counseling for change: When a person makes a lifestyle change, he or she is giving up something; adapting new behaviors entails “costs” and “benefits”. In communities where individual health care providers and mass media promote healthy habits, there may be more motivation for people to make changes. By using motivational interviewing techniques, the counselor can help the patient move through the stages of change. The goal is to increase the client’s intrinsic motivation so that he or she can express the rationale for the changes. Persuasion and support are key elements in counseling. Community Resources: Basic in communities are the availability of wellness centers where patients may be referred to for assistance. The Barangay Nutrition Scholar is tasked to do preliminary assessment , monitoring and ensuring availability of food supplements for children who may be suffering from Vit A Deficiency, Iron Deficiency Anemia, malnutrition or Iodine deficiency. Available from the Web are various literatures and sites that may be used for specific nutritional needs and support groups, such as Overeaters Anonymous, glutenfreediet.com and thelike. Modified Diet refers to changes in texture and composition being made from a regular diet (normal diet) to meet a patient’s nutritional need. Therapeutic Diets is a form of a diet prescribed , specifying the type, amount and frequency of feeding based on the patient’s disease process and management goals. It specifies the caloric level, restrictions or increase in various components of the diet such as the carbohydrate, protein, fat, specific vitamins, minerals, fiber or water. Pelletier, D., Porter,C. et al. Expanding the Frontiers of Nutrition Research: New Questions, New Methods, and New Approaches.January 2013.Advances in Nutrition 4(1):92-114 Prepare a one-hour teaching plan or a counseling session as needed for these patients: Patient 1: Pam Age: 40 y/o/Single Ht: 5 ft 4 in. Wt: 80kg (lowest weight she had was 55kg about 3 years ago) BP: 160/90 claims to take some antihypertensive meds; none of which she can remember. She has followed strict diets and has never exercised in her previous weight-loss attempts. Her favorite foods include fried foods, fruits, kakanins and soda – which helps digest her food faster. Her hectic schedule often mean eating out or buying to go from a convenience store near where she lives. Patient 2: Rene Age: 26y/o/Male Ht:5 ft 9 inches Wt: 70 Kg He claims to have problems maintaining his weight; he cycles for an hour, three times a week and goes to the Gymn twice a week. He works as a hair stylist and is on his feet most of the day. Busy days will mean skipping lunch. On weekends, he works late and when he gets home, he would be too tired to prepare his dinner. To date, he is not aware of any medical problems present. Caudal, Maria Lourdes C. (2019). Basic nutrition and diet therapy : textbook for nursing students 2nd Edition. QC: C&E. F 613.2 C31 2019 Caudal, Maria Lourdes C. (2019). Basic nutrition and diet therapy : laboratory manual for nursing students. QC: C&E. F 613.2078 C31 2019 Bastable, S. (2019) Nurse as Educator: principles of teaching and learning for nursing practice. 5th Ed.