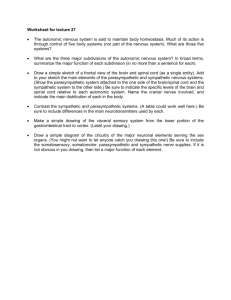
Jimma University Institute of Technology Department of Biomedical Engineering Course Title : Physiology Section : 2 Group : 5 No Name of group members Id number 1 Dawit Girma RU 0602/15 2 Elias Sultan RU 0701/15 3 Fraol Zawude RU 0840/15 4 Henok Girma RU 0981/15 5 Hamelmal Behailu RU 1058/15 1 1. You’ve been to the “all-you-can-eat” buffet and have consumed large amounts of food. After returning home, you recline on the couch to watch television. Which division of the nervous system will be handling your body’s after-dinner activities? List several organs involved, the major nerve supply to each organ, and the effects of the nervous system on their functions. The division of the nervous system responsible for handling the body’s after dinner-activities is the autonomic nervous system. the autonomic nervous system controls many of the organs in our body, including the heart, stomach, and intestine. In most situations, we are not aware that our nervous system is doing anything because it happens automatically. However, sometimes we become aware of these organs and the way our nervous system regulates them, like when we get scared or feel like we are in danger, and also It is further divided into the sympathetic and parasympathetic nervous systems. After eating, the autonomic nerve system (ANS) is essential for digestion. Particularly, the post-meal rest and digest processes are carried out by the parasympathetic nerve system (PSNS), a division of the autonomic nervous system (ANS). When we eat, the brain integrates signals about what we are eating from the gut and the hepatoportal area, among other sources. This results in an increase in peripheral sympathetic outflow. Organs that involved in the activities and the effects of nervous system on their functions Stomach: the stomach is an essential organ for both chemical and mechanical food digestion. the vagus nerve, which is parasympathetic, and the splanchnic nerve, which is sympathetic, are the main nerve supplies that supply the stomach. while sympathetic stimulation reduces these processes, parasympathetic stimulation enhances stomach motility and the release of digestive enzymes. Pancreas: the pancreas secretes hormones such as glucagon and insulin as well as digestive enzymes. The pancreas is innervated by the parasympathetic vagus 2 nerve and the sympathetic splanchnic nerve. enzyme secretion is stimulated by parasympathetic activity and inhibited by sympathetic activity. Liver: nutrients ingested from the intestines are processed by the liver. Both the sympathetic (splanchnic nerves) and parasympathetic (vagus nerve) innervate it. Bile production is increased by parasympathetic stimulation and decreased by sympathetic activation. Intestine : small and large intestines are in charge of taking up water and nutrients from food that has been digested. Both the sympathetic and parasympathetic vagus and splanchnic nerves innervate them. Sympathetic activity hinders peristalsis and the absorption of nutrients, whereas parasympathetic activity promotes these functions. 2. Define arterial blood pressure and its measurement procedures. Describe the regulation of arterial blood pressure. Definition of arterial blood and its measurement procedure Arterial blood pressure is the measure of the force exerted by the blood on the walls of the arteries in the body, usually determined with the help of a device called a sphygmomanometer. This measurement is also known as systemic pressure or blood pressure and represents one of the main vital signs to determine the state of health of a person at a defined moment. Blood pressure reaches its maximum values in the larger vessels that connect directly to the heart, for example, the aorta. The pressure of the blood decreases the further it travels from the heart and is lowest in the outermost vessels such as extremity arteries, arterioles, capillaries, and veins. Typical arterial blood pressure values in a healthy adult human, at rest, are about 120 mmHg for systolic pressure (ventricular contraction phase), and 80 mmHg for diastolic pressure (ventricular relaxation phase). These values can vary between individuals and are determined by a wide variety of factors. There are two methods to measurement of ABP: 1- Direct method:- A cannula or needle filled with anticoagulant is inserted in artery. Then it is connected to the manometer. 2- Indirect method: A) Palpatory method: The SBP can be determined by inflating an arm cuff and then letting the pressure fall and determining the pressure at which the radial pulse first becomes palpable. B) Auscultatory method: It is standard method of taking a patient blood pressure by use technique developed by Korotkoff in 1905. The arterial pressure in human is 3 routinely measured by this method by using instrument which is called a sphygmomanometer. Inflate the bag of instrument by means of a rubber squeeze bulb to pressure above the expected systolic pressure so no sound is heard with the stethoscope. The pressure in the cuff is then lowered slowly by open release valve. When the inflation pressure falls, the small spurt of blood escapes through the cuff and slight tapping sound heard. The pressure at which the sound is first heard (phase 1 of korotkoff sound) represents the systolic blood pressure (SBP). The sounds become louder, then dull, muffled and finally they disappear. The point at which the sound becomes muffled is taken as the diastolic pressure in pregnancy, children, and adult after exercise. This is also true in diseases such hyperthyroidism and aortic insufficiency. Diastolic pressure in resting adult correlates best with the pressure at which the sound disappears. Korotkoff sounds are: 1. Phase 1: tapping sound. 2. Phase 2: louder sound. 3. Phase 3: dull sound. 4. Phase 4: muffled sound. 5. Phase 5: disappeared sound. The ausculatory method is accurate when used properly, because of the difficulty in determining exactly when the first beat is felt. Pressure by palpatory method is sually 2– 5 mmHg. lower than those measured by the ausculatory method. Regulation of arterial blood pressure There are several mechanisms through which the body regulates arterial pressure. Baroreceptor Reflex In response to acute changes in blood pressure, the body responds through the baroreceptors located within blood vessels. Baroreceptors are a form of mechanoreceptor that become activated by the stretching of the vessel. This sensory information is conveyed to the central nervous system and used to influence peripheral vascular resistance and cardiac output. There are two forms of baroreceptors : 1. High-Pressure Baroreceptors Two baroreceptors are located within the high-pressure arterial system. The carotid baroreceptor responds to both increases and decreases in blood pressure and sends afferent signals via the glossopharyngeal nerve (CN IX). 4 The aortic arch baroreceptor responds only to increases in blood pressure, sending its signals through the vagus nerve (CN X). These both send signals in response to the physical distortion of the vessel. The stretch of the vessel leads to an increase in action potential relayed from the sensory endings located in the tunica adventitia of the artery. These action potentials get transmitted to the solitary nucleus that signals to autonomic neurons secrete hormones to affect the cardiovascular system. Activation of the aortic baroreceptor during increases in blood pressure effectively inhibits the efferent sympathetic nerve response. On the other hand, if an individual’s blood pressure were to fall such as in hypovolemic shock, the rate of action potential from the baroreceptors would be decreased due to reduced depolarization; this would lead to reduced inhibition of sympathetic activity, resulting in a reflex to increase pressure. 2. Low-Pressure Baroreceptors These baroreceptors are present within the low-pressure venous system. They exist within large veins, pulmonary vessels, and within the walls of the right atrium and ventricle. The venous system has compliance approximately 30 times greater than that of the arterial system . Changes in volume largely influence the baroreceptors in the venous system. Decreased frequency in action potentials in low-pressure scenarios leads to the secretion of antidiuretic hormone, renin, and aldosterone. These lead to a downstream effect to regulate arterial pressure. Antidiuretic Hormone Antidiuretic hormone (ADH), also known as vasopressin, is a hormone synthesized in the magnocellular neurosecretory cells within the paraventricular nucleus and supraoptic nucleus of the hypothalamus. ADH is synthesized and released in response to multiple triggers which are: High serum osmolarity, which acts on osmoreceptors in the hypothalamus Low blood volume causes a decreased stretch in the low-pressure baroreceptors, leading to the production of ADH Decreased blood pressure causes decreased stretch in the high-pressure baroreceptors, also leading to the production of ADH Angiotensin II The antidiuretic hormone produced in the hypothalamus makes its way down the pituitary stalk to the posterior pituitary where it is kept in reserve for release in response to the above-listed triggers. ADH mainly functions to increase free water reabsorption in the collecting duct of the nephrons within the kidney, causing an increase in plasma volume and arterial pressure. ADH in high concentrations has also been shown to cause moderate vasoconstriction, increasing peripheral resistance, and arterial pressure. Renin-Angiotensin-Aldosterone System (RAAS) 5 The renin-angiotensin-aldosterone system is an essential regulator of arterial blood pressure. The system relies on several hormones that act to increase blood volume and peripheral resistance. It begins with the production and release of renin from juxtaglomerular cells of the kidney. They respond to decreased blood pressure, sympathetic nervous system activity, and reduced sodium levels within the distal convoluted tubules of the nephrons. In response to these triggers, renin is released from the juxtaglomerular cells and enters the blood where it comes in contact with angiotensinogen which is produced continuously by the liver. The angiotensinogen is converted into angiotensin I by renin. The angiotensin I then make its way to the pulmonary vessels, where the endothelium produces the angiotensin-converting enzyme (ACE). Angiotensin I is then converted to angiotensin II by ACE. Angiotensin II has many functions to increase arterial pressure, including: - Potent vasoconstriction of arterioles throughout the body. - Vasoconstriction of the efferent arterioles within the glomerulus of the kidney, resulting in the maintenance of glomerular filtration rate. - Increased sodium reabsorption within the kidney tubules - the increased sodium reabsorption from the kidney tubules results in passive reabsorption of water through osmosis; this causes an increase in blood volume and arterial pressure. - The release of antidiuretic hormone (ADH) release from the posterior pituitary gland. - The release of aldosterone from the zona glomerulosa of the adrenal cortex within the adrenal gland. Aldosterone functions to increase the arterial pressure through the upregulation of Na+/K+ pumps of the distal convoluted tubule and collecting duct within the nephron. This activity is the distal convoluted tubule leads to increased reabsorption of sodium, as well as increased secretion of potassium. The increase in sodium reabsorption leads to passive reabsorption of water and an increase in blood pressure 6