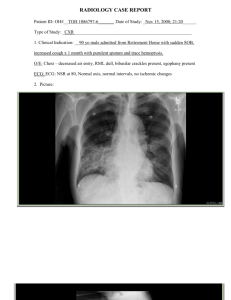
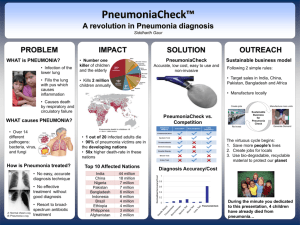
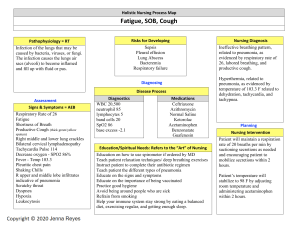
LOWER RESPIRATORY TRACT INFECTIONS PNEUMONIA - is an inflammatory condition of the alveoli of the lungs. the air sacs in the lungs are filled with fluid and pus can be caused by: a. bacteria b. Viruses c. Fungi Pic 1. Pneumonia Causes: 1. Bacterial Pneumonia o common bacterial pathogens include Streptococcus pneumoniae, Haemophilus influenza and Staphylococcus aureus. 2. Viral Pneumonia o Commonly cause by influenza viruses, respiratory syncytial virus (RSV), adenovirus, human metapneumovirus, and coronaviruses 3. Fungal Pneumonia o Pneumocystis jirovecii (common in immunocompromised individuals) 4. Aspiration Pneumonia o occurs when foreign materials, such as food, liquids, saliva, or vomitus, are entered into the lungs Classification of Pneumonia 1. Hospital acquired - Also known as nosocomial pneumonia - pneumonia contracted by the patient in a hospital at least 48- 72 hours during hospital stay 2. Community acquired - Acquired outside the hospital - Exposure in the community Signs and Symptoms 1. Fever- often high-grade, accompanied by chills. 2. Cough- may be dry or productive 3. rapid breathing (increased RR) 4. Lethargy 5. poor feeding 6. Crackles 7. Decreased breath sounds on auscultation 8. Decreased oxygen saturation < 92% 9. Sharp stabbing chest pain - worsened by deep breathing or coughing. 10. Sputum Production- Yellow, green, or bloody sputum in bacterial pneumonia; clear or white in viral pneumonia. Diagnostic Tests: 1. Physical Examination: Including auscultation of the lungs for crackles, decreased breath sounds, and dullness to percussion. 2. Chest X-ray: To visualize infiltrates, consolidation, or pleural effusion. Laboratory Tests 1. Complete blood count (CBC) 2. C-reactive protein (CRP)- to check for the presence of inflammation 3. blood cultures 4. sputum culture and gram stain. Other tests 1. Pulse Oximetry: To measure oxygen saturation. 2. Arterial Blood Gas (ABG): To assess oxygenation and acid-base balance. 3. Bronchoscopy: To obtain samples for culture and sensitivity in severe or complicated cases. Treatment 1. Antibiotics - depends on the suspected or identified causative organism, severity of illness, and risk factors for drug resistance. 2. Antiviral Drugs 3. Antifungal Agents - Such as trimethoprim-sulfamethoxazole 4. Corticosteroids 5. IV fluids 6. Supportive treatment - Oxygenation - Analgesia - Antipyretic WHO Recommendation for treatment of Pneumonia 1. Recommendation 1 • Children with fast breathing pneumonia with no chest indrawing or general danger sign should be treated with oral amoxicillin: at least 40mg/kg/dose twice daily (80mg/kg/day) for five days. In areas with low HIV prevalence, give amoxicillin for three days. • Children with fast-breathing pneumonia who fail on first-line treatment with amoxicillin should have the option of referral to a facility where there is appropriate second-line treatment. 2. Recommendation 2 • Children age 2–59 months with chest indrawing pneumonia should be treated with oral amoxicillin: at least 40mg/kg/dose twice daily for five days. 3. Recommendation 3 - Children aged 2–59 months with severe pneumonia should be treated with parenteral ampicillin (or penicillin) and gentamicin as a first-line treatment for at least five days 4. Ceftriaxone should be used as a second-line treatment in children with severe pneumonia having failed on the first-line treatment. BRONCHITIS - It is the inflammation or swelling of the bronchial tubes and mucosa increasing production of mucus, and narrowing of the airways. Pic 2. Bronchitis Types: 1. Acute Bronchitis o commonly caused by viral infections, such as the common cold or influenza viruses. o usually resolves on its own within a few weeks. 2. Chronic Bronchitis - a type of chronic obstructive pulmonary disease (COPD) characterized by persistent inflammation of the bronchial tubes and excessive mucus production - is often associated with long-term exposure to irritants such as cigarette smoke or air pollution. Risk Factors Smoking/ exposure to 2nd hand smoke Exposure to Respiratory Irritants Viral Infections Age o Young children and older adults are more susceptible to bronchitis due to weaker immune systems and other factors. 5. Chronic Respiratory Conditions o Individuals with asthma, COPD, or other chronic respiratory conditions are prone to recurrent episodes of bronchitis. 6. Weakened immune systems 1. 2. 3. 4. Causes: 1. Viral Infections - most commonly caused by viruses, including rhinovirus (common cold), influenza virus, respiratory syncytial virus (RSV), and adenovirus. 2. Bacterial Infections - Streptococcus pneumoniae, Haemophilus influenzae, 3. Environmental Irritants 4. Allergens - pollen, mold, pet dander, or other allergens Signs and Symptoms 1. Cough: Initially dry and irritating, may progress to productive cough with clear, yellow, or green sputum. 2. Chest tightness when coughing. 3. Dyspnea on exertion. 4. Fatigue 5. Low-grade Fever Diagnostic or Lab Tests: 1. Physical Examination - Auscultation 2. Chest X-ray 3. Sputum Culture and Sensitivity 4. Pulmonary Function Tests (PFTs) 5. Blood Tests a. Complete blood count (CBC) b. C-reactive protein (CRP) Treatment 1. Symptomatic Relief - Throat lozenges for sore throat - Analgesics for fever - Cough suppressants for coughing 2. Fluids and Rest - adequate hydration and rest 3. Bronchodilators - Inhaled bronchodilators to relieve bronchospasm and improve airflow 4. Antibiotics/ antiviral - Depending on the cause 5. Avoidance of Irritants NOTE: The goal of treatment for bronchitis is to relieve symptoms, support the body's immune response, prevent complications, and promote recovery. PRIMARY COMPLEX (CHILDHOOD TUBERCULOSIS) - refers to the initial stage of infection with Mycobacterium tuberculosis. It occurs when M. tuberculosis enters the body and establishes a localized infection, typically in the lungs, although it can affect other organs as well. Mode of Transmission: Droplet Infection Incubation Period: 2-6 weeks after initial infection Cause: Mycobacterium tuberculosis. Risk Factors 1. 2. 3. 4. Close Contact: Exposure to individuals with active tuberculosis Immunocompromised Status: Weakened immune systems Crowded or Poorly Ventilated place Substance and alcohol abuse 5. Malnutrition 6. Age - Infants, young children, and older adults are at increased risk of TB infection and progression to active disease. 7. Travel to Endemic Areas Diagnostic and Laboratory Tests 1. Tuberculin Skin Test (TST) a. A purified protein derivative (PPD) solution containing TB antigens is injected into the skin, and the reaction is assessed after 48-72 hours. - A positive reaction indicates exposure to TB antigens b. Mantoux Test 2. Chest X-ray - pulmonary infiltrates, or pleural effusion suggestive of TB infection or disease. 3. Sputum Culture and Acid-Fast Bacilli (AFB) Smear: Medications and Treatment Goal of Treatment of TB in children: 1. 2. 3. 4. 5. 6. Cure TB patient Prevent death form TB disease Prevent complications Prevent relapse of the disease Prevent DR TB and transmission Reduce transmission to others Doses of Anti TB Drugs: - 4-month treatment regimen (2HRZ(E)/2HR) o 2 months H- isoniazid, R- Rifampicin , Z- Pyrazinamide , E- ethambutol o 2 months H- isoniazid, R- Rifampicin Drug Suggested daily dose Isoniazid 10 (7-15) mg/kg/d Rifampicin 15 (10-20) mg/kg/d Pyrazinamide 35 (30-40) mg/kg/d Ethambutol 20 (15–25) mg/kg/d