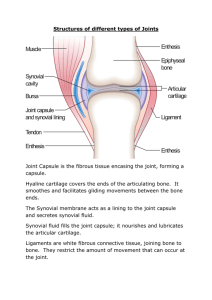
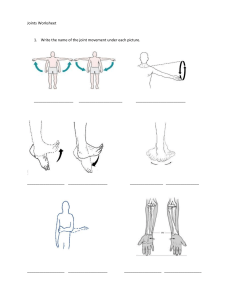
PART A QUESTION 1 (a) Cells in the human body perform a multitude of functions, each vital for the overall health and functioning of the organism. Here are five key functions: i. Energy Production (Metabolism): Cells generate energy through various metabolic processes, primarily through the production of adenosine triphosphate (ATP) in organelles like mitochondria. This energy is essential for powering cellular activities, including muscle contraction, nerve impulse transmission, and biochemical reactions. ii. Cellular Communication: Cells communicate with one another through chemical signals, allowing for coordinated responses and the regulation of various physiological processes. This communication occurs via signaling molecules such as hormones, neurotransmitters, and cytokines, which bind to receptors on the cell surface or within the cell to initiate specific responses. iii. Homeostasis Maintenance: Cells maintain internal balance, or homeostasis, by regulating the concentration of ions, nutrients, and other molecules within their cytoplasm. They also participate in processes like osmoregulation, pH regulation, and temperature control to ensure optimal conditions for cellular function. iv. Cell Growth, Repair, and Reproduction: Cells undergo growth, division, and repair to replace damaged or old cells and to support tissue growth and regeneration. This includes processes such as cell cycle regulation, DNA replication, and cell differentiation, which enable cells to perform specialized functions in various tissues and organs. v. Defense and Immunity: Cells play critical roles in the body's defense against pathogens and foreign substances. Immune cells such as white blood cells, macrophages, and lymphocytes detect and neutralize pathogens through phagocytosis, antibody production, and cell-mediated immunity. Additionally, cells produce molecules like interferons and cytokines to coordinate immune responses and inflammation. (b) A cell’s basic characteristics are fundamental to their structure and function: i. Plasma Membrane: This membrane serves as a barrier that regulates the passage of substances into and out of the cell, maintaining internal homeostasis. ii. Genetic Material: Cells contain genetic material in the form of deoxyribonucleic acid (DNA), which carries the instructions for the cell's structure, function, and development. iii. Cytoplasm: The cytoplasm is the gel-like substance that fills the interior of the cell, surrounding organelles and other cellular structures. It consists of water, salts, and various organic molecules, providing a medium for metabolic reactions and cellular processes. iv. Organelles: Cells contain various organelles, each with specific roles in cellular processes. For example, mitochondria. Centrioles, Cilia, Flagella, Microvilli, spindle fibers, ribosomes, and rough endoplasmic reticulum (RER). (c) List and describe the component of the nucleus: The nucleus consists of several components, each with specific functions: i. Nuclear Envelope/Membrane: The nuclear envelope is a double membrane structure that surrounds the nucleus, separating its contents from the cytoplasm. It consists of an outer nuclear membrane and an inner nuclear membrane, which are fused at various points to form nuclear pores ii. Nuclear Pores: Nuclear pores are protein-lined channels that span the nuclear envelope, facilitating the exchange of molecules between the nucleus and the cytoplasm. iii. Nucleoplasm: The nucleoplasm, also known as the nuclear matrix or karyoplasm, is the gel-like substance that fills the interior of the nucleus. iv. Chromatin: Chromatin is the complex of DNA and proteins found within the nucleus, representing the cell's genetic material. v. Nucleolus (Plural: Nucleoli): The nucleolus is a distinct structure within the nucleus responsible for the synthesis and assembly of ribosomal RNA (rRNA) and ribosomal subunits. It appears as a dark-staining region and is composed of proteins, RNA, and DNA. vi. Nuclear Lamina: The nuclear lamina is a protein meshwork that lines the inner surface of the nuclear envelope, providing structural support and stability to the nucleus. It helps maintain the shape of the nucleus and anchors chromatin and nuclear pore complexes to the nuclear envelope. QUESTION 2 (a) The skeletal system is a complex network of bones, cartilage, and connective tissues that provides structural support, protects vital organs, facilitates movement, produces blood cells, and stores minerals. Its main functions include: i. Support and Structure: The skeletal system provides the structural framework for the body, supporting and maintaining its shape. ii. Protection of Vital Organs: The skeletal system protects vital organs from injury and damage. iii. Facilitation of Movement: Bones, in conjunction with muscles and joints, enable movement and locomotion. iv. Blood Cell Production (Hematopoiesis): Within certain bones, such as the marrow cavities of long bones and the spongy bone tissue of flat bones, hematopoiesis occurs. v. Mineral Storage and Homeostasis: Bones serve as reservoirs for essential minerals, primarily calcium and phosphorus. (b) Phases involved in bone repair are hematoma formation, callus formation, callus ossification, and bone remodeling, respectively. i. Hematoma formation is the initial response to a bone injury, such as a fracture. When a bone is fractured, blood vessels within the bone and surrounding tissues are damaged, leading to bleeding. As blood leaks out of the damaged vessels, it accumulates in the fractured area, forming a hematoma (blood clot). The hematoma serves as a temporary scaffold and provides a source of nutrients and signaling molecules for the subsequent repair processes. ii. During callus formation phase, After the formation of the hematoma, the body initiates the repair process by forming a callus. The callus is a mass of tissue that stabilizes the fractured bone and bridges the gap between the broken ends. Initially, fibroblasts from surrounding tissues and periosteum (the outer membrane of bone) migrate to the fracture site. These fibroblasts produce collagen fibers, which form a fibrous tissue matrix, and chondroblasts, which produce cartilage matrix. The combined action of fibroblasts and chondroblasts results in the formation of a soft callus (fibrocartilaginous callus) that stabilizes the fracture and provides structural support. iii. Callus ossification is when the soft callus undergoes a process called ossification, during which it is gradually replaced by bone tissue. Osteogenic cells (osteoblasts) within the soft callus differentiate into bone-forming cells. These osteoblasts deposit new bone matrix (osteoid) onto the surface of the soft callus. Over time, the osteoid mineralizes, forming immature woven bone tissue. This process transforms the soft callus into a hard callus (bony callus) composed of immature bone tissue. iv. The final phase of bone repair is bone remodeling, during which the bony callus is reshaped and strengthened to restore the bone's original structure and function. Osteoclasts, specialized cells that break down bone tissue, resorb excess bone material from the callus. Concurrently, osteoblasts deposit new bone matrix in a more organized manner, replacing the woven bone with lamellar (mature) bone tissue. The remodeling process continues over months to years, during which the bone gradually regains its pre-injury structure and strength. It is influenced by mechanical stresses and hormonal factors, ensuring that the healed bone adapts to its functional requirements. (c) Synovial and fibrous joints are two types of structural classifications of joints in the human body. Here are the key differences between them along with examples of each: i. Structure: i. Synovial Joints: Synovial joints are characterized by the presence of a synovial cavity, which is filled with synovial fluid. The articulating surfaces of the bones are covered with articular cartilage, and the joint is surrounded by a joint capsule composed of dense connective tissue. ii. Fibrous Joints: Fibrous joints are connected by fibrous tissue and lack a synovial cavity. The bones in fibrous joints are held together by fibrous connective tissue, which may be dense regular connective tissue or fibrocartilage. ii. Movement: i. Synovial Joints: Synovial joints are highly mobile and allow a wide range of movements, including flexion, extension, abduction, adduction, rotation, and circumduction. The mobility of synovial joints depends on their specific structure and the arrangement of their ligaments. ii. Fibrous Joints: Fibrous joints are typically immobile or have limited mobility. The degree of movement in fibrous joints depends on the length and flexibility of the fibrous connective tissue that binds the bones together. iii. Examples: i. Synovial Joints: Examples of synovial joints include the ball-andsocket joint (e.g., shoulder and hip joints), hinge joint (e.g., elbow and knee joints), pivot joint (e.g., between the atlas and axis vertebrae), condyloid joint (e.g., between metacarpals and phalanges), saddle joint (e.g., between the carpal and metacarpal of the thumb), and gliding joint (e.g., between the carpal bones of the wrist). ii. Fibrous Joints: Examples of fibrous joints include the sutures of the skull (e.g., sagittal suture, coronal suture), syndesmoses (e.g., distal tibiofibular joint, interosseous membrane between radius and ulna), and gomphoses (e.g., teeth held in sockets of the maxilla and mandible by periodontal ligaments). QUESTION 3 (a) The anterior pituitary gland, also known as adenohypophysis, secretes several important hormones that regulate various physiological processes throughout the body. Here are the hormones released by the anterior pituitary gland and their sites of action: i. Adrenocorticotropic Hormone (ACTH): i. ACTH stimulates the adrenal cortex (the outer layer of the adrenal glands) to produce and release cortisol, a stress hormone. ii. Thyroid-Stimulating Hormone (TSH): i. TSH stimulates the thyroid gland to produce and release thyroid hormones, primarily thyroxine (T4) and triiodothyronine (T3). iii. Follicle-Stimulating Hormone (FSH): i. FSH plays a key role in regulating the growth and development of ovarian follicles in females and spermatogenesis (sperm production) in males. iv. Luteinizing Hormone (LH): i. LH works in conjunction with FSH to regulate reproductive function in both males and females. v. Prolactin (PRL): i. Prolactin primarily regulates lactation (milk production) in mammary glands following childbirth. vi. Growth Hormone (GH): i. GH, also known as somatotropin, plays a crucial role in growth, development, and metabolism. (b) Thyroid hormones, primarily thyroxine (T4) and triiodothyronine (T3), play a crucial role in modulating basal metabolic rate (BMR), which is the amount of energy expended by the body at rest to maintain basic physiological functions such as breathing, circulation, and cell maintenance. Thyroid hormones play a central role in regulating basal metabolic rate by influencing cellular metabolism, oxygen consumption, thermogenesis, and the metabolism of carbohydrates, fats, and proteins. Dysfunction of the thyroid gland, such as hypothyroidism or hyperthyroidism, can disrupt metabolic homeostasis and lead to alterations in BMR, resulting in metabolic disorders and related symptoms. (c) The pancreas plays a crucial role in the regulation of blood sugar levels through the release of two key hormones: insulin and glucagon. These hormones work in tandem to maintain blood glucose within a narrow physiological range. Here's how their action mechanisms contribute to blood sugar control: i. Insulin: i. Secretion: Insulin is produced and released by beta cells located in the islets of Langerhans within the pancreas in response to elevated blood glucose levels. ii. Action Mechanism: 1. When blood glucose levels rise, insulin is secreted into the bloodstream. 2. Insulin binds to specific receptors on target cells, such as muscle, adipose tissue, and liver cells. 3. Binding of insulin to its receptors triggers a series of intracellular signaling pathways, leading to the translocation of glucose transporter proteins (GLUT4) from intracellular vesicles to the cell membrane. 4. The translocation of GLUT4 proteins facilitates the uptake of glucose from the bloodstream into target cells, promoting glucose utilization for energy production, glycogen synthesis, and lipid synthesis. 5. Insulin also inhibits the breakdown of glycogen (glycogenolysis) in the liver and the production of glucose from non-carbohydrate sources (gluconeogenesis), further reducing blood glucose levels. iii. Overall Effect: Insulin promotes the storage of glucose, fatty acids, and amino acids while lowering blood glucose levels, thus counteracting hyperglycemia. ii. Glucagon: i. Secretion: Glucagon is produced and released by alpha cells in the pancreatic islets in response to low blood glucose levels. ii. Action Mechanism: 1. When blood glucose levels decrease, glucagon secretion is stimulated. 2. Glucagon binds to specific receptors on target cells, primarily hepatocytes (liver cells). 3. Binding of glucagon to its receptors activates adenylate cyclase, leading to the production of cyclic AMP (cAMP). 4. Increased cAMP levels activate protein kinase A (PKA), which phosphorylates enzymes involved in glycogen breakdown (glycogenolysis) and gluconeogenesis. 5. As a result, glycogen stored in the liver is broken down into glucose (glycogenolysis), and glucose is synthesized from non-carbohydrate precursors (gluconeogenesis). iii. Overall Effect: Glucagon promotes the release of glucose from liver glycogen stores and increases blood glucose levels, thus counteracting hypoglycemia. Together, insulin and glucagon play complementary roles in the regulation of blood sugar levels, ensuring that glucose is available to meet the energy needs of cells throughout the body. This dynamic interplay between insulin and glucagon maintains blood glucose homeostasis, preventing hyperglycemia (high blood sugar) or hypoglycemia (low blood sugar) and supporting overall metabolic health. Dysregulation of insulin and glucagon secretion or action can lead to metabolic disorders such as diabetes mellitus. Part B QUESTION 1 Carbohydrate metabolism in the gastrointestinal (GI) system is a complex process involving several organs and enzymes. Here's a breakdown of the process: Mouth Stomach Small Intestine Liver Large Intestine •The digestion of carbohydrates begins in the mouth with the action of salivary amylase. •This enzyme starts breaking down complex carbohydrates like starch into simpler sugars like maltose. •Carbohydrate digestion is briefly paused in the stomach due to the acidic environment, which inhibits salivary amylase. •However, some digestion continues due to the action of lingual amylase until the food bolus is further broken down into chyme. •The majority of carbohydrate digestion and absorption occur in the small intestine. •Pancreatic amylase, released from the pancreas, further breaks down complex carbohydrates into disaccharides like maltose, sucrose, and lactose. •Disaccharidases, located in the brush border of the small intestine, break down disaccharides into monosaccharides (glucose, fructose, and galactose) that can be absorbed into the bloodstream. •Glucose and galactose are absorbed via active transport, while fructose is absorbed via facilitated diffusion. •Once absorbed, monosaccharides travel to the liver via the portal vein. •The liver metabolizes galactose and fructose into glucose. •Glucose is either stored as glycogen, converted into fat for storage, or released into the bloodstream to provide energy to cells throughout the body. •Any undigested carbohydrates, as well as fibers, reach the large intestine where they undergo fermentation by the gut microbiota. •Fermentation produces short-chain fatty acids (SCFAs) and gases like carbon dioxide, hydrogen, and methane. •SCFAs can be absorbed and used as an energy source by the body. 2. Below is a diagram illustrating the role of female sex hormones in synchronizing the ovarian and uterine (menstrual) cycles: i. Follicular Phase: a. Ovarian Cycle: During this phase, follicle-stimulating hormone (FSH) from the anterior pituitary stimulates the growth and maturation of ovarian follicles. As the follicles develop, they produce estrogen. b. Uterine Cycle: Estrogen released from the developing follicles stimulates the proliferation of the endometrial lining in the uterus. This phase prepares the uterus for potential implantation of a fertilized egg. ii. Ovulation: a. Ovarian Cycle: A surge in luteinizing hormone (LH), triggered by rising estrogen levels, induces ovulation. The mature follicle ruptures, releasing the egg into the fallopian tube. b. Uterine Cycle: There is no significant change in the uterine cycle during ovulation. iii. Luteal Phase: a. Ovarian Cycle: After ovulation, the remaining follicular cells transform into the corpus luteum, which secretes progesterone and estrogen. These hormones prepare the uterine lining for potential implantation and maintain the pregnancy if fertilization occurs. b. Uterine Cycle: Progesterone from the corpus luteum stimulates the secretory phase in the uterus, where the endometrial lining becomes more vascularized and glandular, ready to support implantation. iv. Menstrual Phase: a. Ovarian Cycle: If fertilization does not occur, the corpus luteum degenerates, leading to a decrease in progesterone and estrogen levels. b. Uterine Cycle: With the decline in hormone levels, the endometrial lining is shed, resulting in menstrual bleeding. The interplay of estrogen and progesterone, along with the feedback loops involving FSH and LH, regulates the ovarian and uterine cycles. This synchronization ensures proper preparation of the reproductive system for potential fertilization and pregnancy. Any disruptions in hormone levels or feedback mechanisms can lead to irregular menstrual cycles or fertility issues.