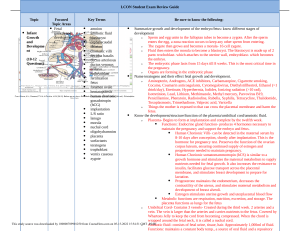
ANA 212 GENETICS AND GENERAL EMBRYOLOGY • Development of tissues and organ systems of the embryo, the chorionic and amniotic cavities. • Foetal membrane • Placental formation and functions • Our life begins as one cell (called zygote) formed by the union of the paternal and maternal germ cells called sperm and ovum. Human development is a continuous process that begins when an ovum is fertlised by a sperm. The zygote is the outcome of the process and it is the beginning of a new human being. Going down memory lane, development has two major phase. These are the prenatal and postnatal phases. The prenatal include from the term pre, it occurs before birth and it is the main developmental change. The prenatal development is divided into the embryonic (begins at birth to wk 8 of gestation) while fetal (begins at the beginning pof the 9wk and ends at birth). While the postnatal occurs after birth for example changes like teeth and breast development. Overview • After fertilisation, the fertilised oocyte (egg) splits (cleavage) into two cells of equal size; called blastomeres. After three more divisions(4, 8), there are 16 cells. At this point, the group of cells is referred to as the morula. Within the first week, the cells of the morula reorganise to form a cavity, known as the blastocyst cavity (blastocoel). From this point, the morula is known as the blastocyst.It is comprised of two different cell types: Outer cell mass (trophoblast) – contacts with the endometrium of the uterus to facilitate implantation and the formation of the placenta. • Inner cell mass (embryoblast) – responsible for the formation of the embryo itself. • During the second week, the trophoblast and embryoblast divide into increasingly specialised cell types. The trophoblast divides into the syncytiotrophoblast and cytotrophoblast. The embryoblast divides into the epiblastand hypoblast, forming a two-layered structure; the bilaminar disk. The amniotic cavity forms within the epiblast. • Implantation • After the initial rounds of cellular divisions, the embryo must implant into the endometrium of the uterus. • During this process, the syncytiotrophoblast becomes continuous with the uterus – such that maternal blood vessels (known as sinusoids) invade the spaces within the syncytiotrophoblast (known as lacunae). At this point, uteroplacental circulation has begun; and further embryonic development can occur. • Congenital Abn: In placenta praevia, implantation of the embryo occurs in the lower uterine segment (instead of in the normal position of the upper posterior uterine wall). Introduction • Week 3: Gastrulation • In the 3rd week of embryonic development, the cells of the bilaminar disk (epiblast and hypoblast) undergo a highly specialised process called gastrulation.During this process, the two cell layers become three germ cell layers, and the bodily axes observed in the mature adult are created. • Gastrulation is a process of cellular rearrangement which involves migration, invagination and differentiation of the epiblast. Itis largely controlled and orchestrated by the primitive streak. The primitive streak is a groove in the midline of the epiblast which appears during the third week. Within the primitive streak lies a primitive node at the cranial end, and within the primitive node lies the primitive pit. • Cells of the epiblast layer break off and migrate toward the primitive pit.Here, they detach and penetrate through the epiblast layer to form three new germ cell layers: ENDODERM, MESODERM AND ECTODERM • Upon arrival in the region of the streak, they become flask-shaped, detach from the epiblast, and slip beneath it. This inward movement is known as invagination. Once the cells have invaginated, some displace the hypoblast, creating the embryonic endoderm, and others come to lie between the epiblast and newly created endoderm to form mesoderm. Cells remaining in the epiblast then form ectoderm. Thus, the epiblast, through the process of gastrulation, is the source of all of the germ layers and cells in these layers will give rise to all of the tissues and organs in the embryo. As more and more cells move between the epiblast and hypoblast layers, they begin to spread laterally and cephalad. Gradually, • Gradually, they migrate beyond the margin of the disc and establish contact with the extraembryonic mesoderm covering the yolk sac and amnion. In the cephalic direction, they pass on each side of the prechordal plate. The prechordal plate itself forms between the tip of the notochord and the buccopharyngeal membrane and is derived from some of the first cells that migrate through the node in a cephalic direction. Later, the prechordal plate will be important for induction of the forebrain. The buccopharyngeal membrane at the cranial end of the disc consists of a small region of tightly adherent ectoderm and endoderm cells that represents the future opening of the oral cavity. • The embryonic period or period of organogenesis, occurs from the third to the eighth weeks of development and is the time when each of the three germ layers, ectoderm, mesoderm, and endoderm, gives rise to a number of specific tissues and organs • NOTE: Primitive streak is the primary organizer as it induces formation of notochord and intraembryonic mesoderm. Formation of notochord determines the cranio-caudal axis and right and left sides of embryo. • NOTE : Fate of primitive streak: It regresses at the end of 3rd week of development and completely disappears by 26th day. • NOTE: The period from the beginning of the ninth week to birth is known as the fetal period. It is characterized by maturation of tissues and organs and rapid growth of the body • NOTE: The obstetrician calculates the date of birth as 280 days or 40 weeks from the first day of the LNMP. In women with regular 28-day menstrual periods the method is fairly accurate, but when cycles are irregular, substantial miscalculations may be made • The ectoderm gives rise to cell lineages that differentiate to become the central and peripheral nervous systems, sensory organs, epidermis, hair, and nails. • Mesodermal cells ultimately become the skeleton, muscles, connective tissue, heart, blood vessels, and kidneys. • The endoderm goes on to form the epithelial lining of the gastrointestinal tract, liver, and pancreas, as well as the lungs. Fetal and placenta membranes • As the fetus grows, its demands nutrition. • Tissues or structures that develop from the zygote but do not form part of embryo proper are called fetal or extraembryonic membrane. • It is involved in nutrition, respiration, excretion, and protection of the developing offspring (within the uterus or the egg) • Fetal membranes are the membranes surrounding the embryo or fetus. These membranes are the amnion, the chorion, the allantois, and the yolk sac. • The placenta and fetal membranes separate the fetus from the endometrium—the inner layer of the uterine wall. An interchange of substances, such as nutrients and oxygen, occurs between the maternal and fetal bloodstreams through the placenta. The vessels in the umbilical cord connect the placental circulation with the fetal circulation. • Structure of the fetal membrane: • Trophoblast and chorion forming placenta • Amnion or ectodermal vesicle covering the embryo or fetus and filled with amniotic fluid • Yolk sac—Primary, secondary, tertiary • FUNCTIONS These are concerned with protection, nutrition • • Protection—Amniotic membrane and fluid • • Respiration—Placenta • • Excretion • • Nutrition—Amniotic fluid, placenta, umbilical cord • The chorion: It is the outermost extraembryonic membrane comprised of four layers, particularly the cellular layer, the reticular layer, the basement membrane, and the trophoblast layer. The trophoblast is the outermost layer. The chorion and the amnion form the amniotic sac. • Amnion : The amnion is a membrane that lies next to the chorion. It is a thin and tough membrane. It lines the amniotic cavity. It is comprised of two cell layers, i.e. the epiblast-derived extraembryonic ectodermal layer and the thin non-vascular extraembryonic mesoderm. provide shock absorption and facilitate movement of the foetus during development. The amniotic sac filled with a fluid referred to as amniotic fluid. The fluid serves as a cushion to the developing fetus. • The allantois is a sac-like or diverticulum from the ventral wall of the hindgut. It forms a part of conceptus (i.e. the embryo and its appendages or adjunct parts or associated membranes) of amniotes. The allantois helps in gas exchange and movement of liquid waste. • The yolk sac/Umbilical vesicle is a membrane formed by the hypoblast. It is associated with early embryonic blood supply and the formation of the primordial gut. It has a role in the transfer of nutrients to the embryo during the second and third weeks when the uteroplacental circulation is being established. The umbilical cord, surrounded by the amnion, contains (a) two umbilical arteries, (b) one umbilical vein, and (c) Wharton’s jelly, which serves as a protective cushion for the vessels. AMNIOTIC CAVITY • The amnion is a large sac containing amniotic fluid in which the fetus is suspended by its umbilical cord. The thin but tough amnion forms a fluid-filled, membranous sac that surrounds the embryo and later the fetus. The sac contains amniotic fluid. As the amnion enlarges, it gradually obliterates the chorionic cavity and forms the epithelial covering of the umbilical cord. • Amniotic fluid plays a major role in fetal growth and development. Initially, some amniotic fluid is secreted by cells of the amnion.The amniotic cavity is filled with a clear, watery fluid that is produced in part by amniotic cells but is derived primarily from maternal blood. The amount of fluid increases from approximately 30 ml at 10 weeks of gestation to 450 ml at 20 weeks to 800 to 1000 ml at 37 weeks. Amniotic fluid is swallowed by the fetus and absorbed by the fetus’s respiratory and digestive tracts. • Composition of Amniotic fluid:. It contains approximately equal portions of organic compounds and inorganic salts. Half of the organic constituents are protein; the other half consists of carbohydrates, fats, enzymes, hormones, and pigments. • Significance of Amniotic Fluid :The embryo, suspended in amniotic fluid by the umbilical cord, floats freely. Amniotic fluid has critical functions in the normal development of the fetus: • Permits symmetric external growth of the embryo and fetus • Acts as a barrier to infection • Permits normal fetal lung development • Prevents adherence of the amnion to the embryo and fetus • Cushions the embryo and fetus against injuries by distributing impacts the mother receives • Helps control the embryo’s body temperature by maintaining a relatively constant temperature. • Disorders of amniotic fluid volume: • Hydramnios or polyhydramnios is the term used to describe an excess of amniotic fluid (1500–2000 ml), whereas oligohydramnios refers to a decreased amount (less than 400 ml). Both conditions are associated with an increase in the incidence of birth defects • oligohydramnios : low volumes of amniotic fluid result in many cases from placental insufficiency with diminished placental blood flow. PLACENTA • Introduction: During pregnancy , fetal development and growth are sustained completely by the mother until birth. The placenta consists of a fetal side and a maternal side, and it provides a vascular communication between the mother and the fetus. This communication allows the mother to provide nutrients to the fetus and allows for removal of waste products from fetal blood. The placenta is also called “the fetal lung” because it allows for gas exchange between the maternal and fetal circulation . Diseases or defects in the placenta often have severe, and even fatal, complications. • The placenta is a highly-specialized organ that plays an essential role during pregnancy. It is responsible for providing nutrition and oxygen to the fetus as well as removing waste material and carbon dioxide. It is also responsible for creating a separation between the maternal and fetal circulation (known as placental barrier). Besides that, the placenta protects the fetus from infections and other maternal disorders, while also helping in the development of the fetal immune system. Additionally, this organ has an endocrine function as it secretes hormones (such as human chorionic gonadotropin) that affect the pregnancy, metabolism, fetal growth, and parturition. • The placenta is a fetomaternal organ. It connects growing embryo/fetus with the wall of pregnant uterus. It is the Primary site of nutrient and gas exchange between mother and embryo/fetus. STRUCTURE :It is a circular or disc-shaped organ of 500 g weight at term. It has two surfaces and two structural components. Fetal surface : The fetal surface of the placenta (or chorionic plate) is covered by the amnion, or amniotic membrane, which gives this surface a shiny appearance. Underlying the amnion is the chorion, a thicker membrane continuous with the lining of the uterine wall. The chorion contains the chorionic vessels which are continuous with the vessels of the umbilical cord. • The fetal part is contributed by chorionic frondosum that is seen as a plate called chorionic plate. From the chorionic plate 40–60 extensions (fetal cotyledons) arise and extend toward the decidua basalis. Each fetal cotyledon consists of a stem villus/ truncus chorii that show ramifications into number of branches (ramus chorii), each further subdivides (ramuli chorii) like the branches of a tree. Their terminal ramifications look like fingers and are called chorionic villi. The villi that are attached to decidua basalis are called anchoring villi. Others float in the maternal blood that flows in between the villi and are called floating villi • Maternal surface or basal: The maternal surface is rough and irregular. It emerges from the separation of the placenta from the uterine wall during delivery. This surface is composed of the decidua, the modified or specialized endometrium (or mucosal lining of the uterus) that forms in preparation for pregnancy. The decidua has several parts: • Decidua basalis - forms the portion of placenta; • Decidua capsularis - overlies the embryo; • Parietal decidua - the rest of the decidual tissue. • Also seen are slightly elevated regions called lobes or maternal cotyledons (approximately 10 to 40 ) which are separated by grooves or sulci. • PARTS: • Maternal part: This is contributed by decidua basalis or decidual plate of endometrium. • Fetal part: This is contributed by chorion frondosum or chorionic plate. This surface is covered by the fetal membrane amnion and the umbilical cord is attached near the center of this surface. Development of the placenta • The development of the placenta begins during implantation of the blastocyst. • The 32-64 cell blastocyst contains two distinct differentiated embryonic cell types: the outer trophoblast cells and the inner cell mass. The trophoblast cells form the placenta. The inner cell mass forms the foetus and foetal membranes. • The trophoblast has the tendency to stick to the structure with which it comes in contact. Once the zona pellucida disappears, the cells of the trophoblast stick to the uterine endometrium. This is called the beginning of the process of implantation and it takes place on 6th day after fertilization. • Early placental development is characterized by the rapid proliferation of the trophoblast and development of the chorionic sac and chorionic villi. By the end of the third week, the anatomic arrangements necessary for physiologic exchanges between the mother and embryo are established. A complex vascular network is established in the placenta by the end of the fourth week, which facilitates maternal-embryonic exchanges of gases, nutrients, and metabolic waste products. • The uterus, chorionic sac, and placenta enlarge as the fetus grows. Growth in the size and thickness of the placenta continues rapidly until the fetus is approximately 18 weeks old. The fully developed placenta covers 15% to 30% of the decidua and weighs approximately one sixth that of the fetus. • Implantation • On the 6 day, as the zona pellucida disintegrates, the blastocyst “hatches”, allowing implantation to take place. th • The trophoblast cells interact with the endometrial decidual epithelia to enable the invasion into the maternal uterine cells. • The embryo then secretes proteases to allow deep invasion into the uterine stroma. Implantation is interstitial. Normal implantation occurs on the anterior or posterior wall of the body of the uterus. The most common ectopic implantation site is in the ampulla of the Fallopian tube. • On the 8 day of development, the trophoblast cells differentiate into the outer multinucleated syncytiotrophoblast, which erodes maternal tissues by sending out projections, and the inner mononucleated cytotrophoblast, which is actively proliferating. • The syncytiotrophoblast is responsible for producing hormones such as Human Chorionic Gonadotropin (hCG) by the second week, which is used in pregnancy testing. th • Post implantation: • On day 9, lacunae or spaces form within the syncytiotrophoblast. The syncytiotrophoblast also erodes maternal tissues allowing maternal blood from uterine spiral arteries to enter the lacunar network. Thus early uteroplacental circulation is established by the end of week 2. • Meanwhile, the cytotrophoblast begins to form primary chorionic villi (finger-like projections) which penetrate and expand into the surrounding syncytiotrophoblast. In the 3 week, extra-embryonic mesoderm grows into these villi, forming a core of loose connective tissue, at which point these structures are called secondary chorionic villi. • By the end of the third week, embryonic vessels begin to form in the embryonic mesoderm of the secondary chorionic villi, making them tertiary chorionic villi. • The cytotrophoblast cells from the tertiary villi grow towards the decidua basalis of the maternal uterus and spread across it to form a cytotrophoblastic shell. The villi that are connected to the decidua basalis through the cytotrophoblastic shell are known as anchoring villi. • Villi growing outward within the intervillous space from the stem (anchoring) villi are called branching villi and provide surface area for exchange of metabolites between mother and fetus. Imagining the villi as tree-like projections can help visualise their structure. rd • The final form is a placenta made up of bunches of villi (cotyledons) that are partially separated from each other. At full term the placenta is discoid in shape with a diameter of 15-25cm, approximately 3 cm thick and weighs about 500-600g. At birth, it is torn from the uterine wall and around 30 minutes after the birth of the child it is expelled from the uterine cavity. • The maternal side will have 15-20 bulging areas which are the cotyledons, covered by a thin layer of decidua basalis. The fully grown placenta contains intervillious lakes. These structures will hold approximately 150 mL of maternal blood. This is renewed 3-4 times per minute. • PLACENTA MEMBRANE/BARRIER • Placental membrane is the composite structure that consists of several extra fetal tissues separating the maternal and fetal blood • In the placenta, maternal blood circulates through the intervillous space and fetal blood circulates through blood vessels in the villi. Though the maternal and fetal bloods are flowing side by side and in opposite directions they do not mix with each other. They are separated by a membrane, made up of the layers of the wall of the villus. Tissues intervening between fetal blood in chorionic villi and maternal blood in intervillous space constitute the placental membrane or barrier. All interchanges of oxygen, nutrition and waste products take place through this membrane. • The placental membrane, which separates maternal and fetal blood, is initially composed of four layers: (a) the endothelial lining of fetal vessels; (b) the connective tissue in the villus core; (c) the cytotrophoblastic layer; and (d) the syncytium (Fig. 6.8C ). From the fourth month on, however, the placental membrane thins, since the endothelial lining of the vessels comes in intimate contact with the syncytial membrane, greatly increasing the rate of exchange • NOTE: maternal whole blood (cells and plasma) flow to placenta via converted spiral arteries • The constituent structures forming the placental barrier or maternal fetal barrier are as follows: • In the early part of pregnancy, the barrier presents the following layers - Endothelium of fetal blood vessels, and its basement membrane, Surrounding mesoderm (connective tissue), Cytotrophoblast and its basement membrane, Syncytiotrophoblast. • In the later part of pregnancy, the efficiency of the membrane is increased due to the reduction in its thickness by • - Disappearance of cytotrophoblast Thinning of syncytiotrophoblast, Edematous stroma, Peripheral migration of fetal blood vessels, It presents endothelium of fetal capillaries resting on basement membrane and syncytiotrophoblast only. Functions of the placenta • Main functions of the placenta are (a) exchange of metabolic and gaseous products between maternal and fetal bloodstreams and (b) production of hormones. • 1. It acts as a temporary organ that allows transport of oxygen, water, electrolytes and nutrients (in the form of carbohydrates, lipids, polypeptides, amino acids and vitamins) from maternal to fetal blood and thus maintains the nutrition of the fetus. A full term fetus takes up about 25 mL of oxygen per minute from maternal blood. Even a short interruption of oxygen supply is fatal for the fetus. • 2. It eliminates excretion of carbon dioxide, urea and other Classification of Placenta waste products produced by the fetus into the maternal blood. • Maternal antibodies [immunoglobulin G (IgG), gamma globulins or immunoglobulins] reaching the fetus through the placenta give the fetus immunity against some infections (e.g. diphtheria and measles). • • The placenta acts as a barrier and prevents many bacteria and other harmful substances from reaching the fetus. However, most viruses (including poliomyelitis, measles and rubella) and some bacteria can pass across it. • • Drugs taken by the mother may also enter the fetal circulation and can produce congenital malformations. As a rule, maternal hormones do not reach the fetus. However, synthetic progestins and synthetic estrogens (e.g. diethylstilboestrol) easily cross the placenta and can have adverse effects on the fetus (including carcinoma in later life). • • While permitting the exchange of several substances between the maternal and fetal blood, it keeps these blood streams separate, thereby preventing antigenic reactions between them. • • The placenta synthesizes several hormones. These are probably produced in the syncytiotrophoblast. Progesterone secreted by the placenta is essential for maintenance of pregnancy after the 4th month (when the corpus luteum degenerates). Estrogens (mainly estriol) produced by the placenta reach maternal blood and promote uterine growth and development of the mammary gland. Clinical anatomy • placenta previa, which is the implantation of the placenta over the cervical os. This condition usually presents as painless vaginal bleeding in the third trimester. • Placenta previa is when a pregnant woman's placenta blocks the opening to the cervix that allows the baby to be born.