Mood Disorders & Suicide: Abnormal Psychology Chapter
advertisement

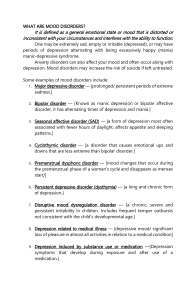
Abnormal Psychology ABPSY - 1st Sem (p.211-p.261) Chapter 7: MOOD DISORDERS AND SUICIDE Note: Feelings of depression (and joy) are universal, which makes it all the more difficult to understand disorders of mood —disorders that canbe so incapacitating that violent suicide may seem by far a better option than living. > The duration of manic episode, if untreated, is approximatelly 3-4 months. HYPOMANIC EPISODE - a less severe version of a manic episode that does not cause marked impairment in social or occupational functioning and need last only 4 days rather than a full week. > (Hypo means “below”; thus the episode is below the level of a manic episode.) Note: A hypomanic episode is not in itself necessarily problematic, but its presence does contribute to the definition of several mood disorders. 7.1: UNDERSTANDING AND DEFINING MOOD DISORDERS The disorders described in this chapter used to be categorized under several general labels, such as “depressive disorders,” “affective disorders,” or even “depressive neuroses.” These problems have been grouped under the heading mood disorders - because they are characterized by gross deviations in mood. MAJOR DEPRESSIVE EPISODE - most commonly diagnosed and most severe depression. > an extremely depressed mood state that lasts at least 2 weeks and includes cognitive symptoms (such as feeling or worthlessness and indeciveness) and disturbed physical functions (such as altered sleeping patterns, significant changes in appetite and weight, or a notable loss of energy) to the point that even the slightest activity or movement requires an overwhelming effort. > Most central indicators of a full major depressive episode are the physical changes (sometimes called somatic or vegetative symptoms) along with the behavioral and emotional “shutdown,” as reflected by low behavioral activation. > The duration of a major depressive episode, if untreated, is approximatelly 4-9 months. People with depression show dysfunctional reward processsing and anhedonia. ANHEDONIA - loss of energy and inability to engage in pleasurable activities or have any “fun.” second fundamental state of mood disorders: abnormally exaggerated elation, joy, or euphoria. MANIA - individuals find extreme pleasure in every activity; some patients compare their daily experience of mania with a continuous sexual orgasm. Speech is typically rapid and may become incoherent, because the individual is attempting to express so many exciting ideas at once; this feature is typically referred to as flight of ideas. > for a manic episode require a duration of only 1 week, less if the episode is severe enough to require hospitalization. THE STRUCTURES OF MOOD DISORDERS UNIPOLAR MOOD DISORDERS - individuals who experience either depression or mania. Their mood remains at one “pole” of the usual depression–mania continuum. > Most people with a unipolar mood disorder eventually develop depression. BIPOLAR MOOD DISORDER - someone who alternates between depression and mania. Traveling from one “pole” of the depression-elation continuum to the other and back again. MIXED FEATURES - An individual can experience manic symptoms but feel somewhat depressed or anxious at the same time or be depressed with a few symptoms of mania. requires specifying whether a predominantly manic or predominantly depressive episode is present and then noting if enough symptoms of the opposite polarity are present to meet the mixed features criteria. > DYSPHORIC - anxious or depressive features more commonly than was thought, and dysphoria can be severe. > FLIGHT OF IDEAS - racing thougts PREDOMINANT POLARITY - exists if one polarity occurs during at least two-thirds of the person’s lifetime. It is important to determine the course or temporal patterning of the depressive or manic episodes. For example, do they tend to recur? If they do, does the patient recover fully for at least 2 months between episodes (termed full remission) or only partially recover retaining some depressive symptoms (“partial remission”)? Do the depressive episodes alternate with manic or hypomanic episodes or not? All these patterns for mood disorders are important to note, since they contribute to decisions on which diagnosis is appropriate. The importance of temporal course (patterns of recurrence and remittance) makes the goals of treating mood disorders somewhat different from those for other psychological disorders. > chronic - almost continuous or nonchronic. > the two most important factors describe mood disorders are severity and chronicity. CLINICAL DESCRIPTION RECURRENT - If two or more major depressive episodes occurred and were separated by at least 2 months during which the individual was not depressed. > Recurrence is important in predicting the future course of the disorder, as well as in choosing appropriate treatments. UNIPOLAR DEPRESSION - is often a chronic condition that waxes and wanes over time but seldom disappears. > The median lifetime number of major depressive episodes is four to seven. > The median duration of recurrent major depressive episodes is 4 to 5 months. PERSISTENT DEPRESSIVE DISORDER (DYSTHYMIA) - shares many of the symptoms of major depressive disorder but differs in its course, but depression remains relatively unchanged over long periods, sometimes 20 or 30 years or more. > defined as depressed mood that continues at least 2 years, during which the patient cannot be symptom free for more than 2 months at a time even though they may not experience all of the symptoms of a major depressive episode. > more severe, higher rates of comorbidity, less responsive to treatment, and show slower rate of improvement over time. Chronicity is the most important distinction in diagnosing depression independent whether the symptom presentation meets criteria for a major depressive disorder. PURE DYSTHYMIC SYNDROME - people suffering from persistent depression with fewer symptoms; eventually experienced a major depressive episode. > meaning one has not met criteria for a major depressive episode in at least the preceding 2 years, “with persistent major depressive episode,” DOUBLE DEPRESSiON - Individuals who have major depressive episodes and persistent depression with fewer symptoms. (major depressive episode) SPECIFIERS - may or may not accompany a depressive disorder, but when they do, they are often helpful in determining the most effective treatment or likely course. Clinicians use eight basic specifiers to describe depressive disorders. These are (1) with psychotic features (mood-congruent or mood-incongruent), (2) with anxious distress (mild to severe), (3) with mixed features, (4) with melancholic features, (5) with atypical features, (6) with catatonic features, (7) with peripartum onset, and (8) with seasonal pattern. 1. PSYCHOTIC FEATURES SPECIFIER - Some individuals in the midst of a major depressive (or manic) episode may experience psychotic symptoms, specifically hallucinations (seeing or hearing things that aren’t there) and delusions (strongly held but inaccurate beliefs). Somatic (physical) delusions, believing, for example, that their bodies are rotting internally and deteriorating into nothingness. Some may hear voices telling them how evil and sinful they are (auditory hallucinations). MOOD CONGRUENT - hallucinations and delusions are called mood congruent because they seem directly related to the depression. MOOD-INCONGRUENT HALLUCINATION OR DELUSION - depressed indivuals might have other types of hallucinations/delusions such delusions of grandeur that do not seem consistent with the depressed mood; may progress to schizoprenia. DELUSIONS OF GRANDEUR - believing that they are supernatural or supremely gifted. Note: Delusions of grandeur accompanying a manic episode are mood congruent. > Psychotic features in general are associated with a poor response to treatment, greater impairment, and fewer weeks with minimal symptoms, compared with nonpsychotic depressed patients over a 10-year period. 2. ANXIOUS DISTRESS SPECIFIER - The presence and severity of accompanying anxiety, whether in the form of comorbid anxiety disorders (anxiety symptoms meeting the full criteria for an anxiety disorder) or anxiety symptoms that do not meet all the criteria for disorders. > makes suicidal thoughts and fatal suicide attempts more likely, and predicts a less effective outcome from treatment. 3. MIXED FEATURES SPECIFIER - Predominantly depressive episodes that have several (at least three) symptoms of mania, which applies to major depressive episodes both within major depressive disorder and persistent depressive disorder. 4. MELANCHOLIC FEATURES SPECIFIER - applies only if the full criteria for a major depressive episode have been met, whether in the context of a persistent depressive disorder or not. > Melancholic specifiers include some of the more severe somatic (physical) symptoms, 5. CATATONIC FEATURES SPECIFIER - can be applied to major depressive episodes whether they occur in the context of a persistent depressive order or not, and even to manic episodes, although it is rare—and rarer still in mania. CATALEPSY - This serious condition involves an absence of movement (a stuporous state) in which the muscles are waxy and semirigid, so a patient’s arms or legs remain in any position in which they are placed. > may also involve excessive but random or purposeless movement. > this response may be a common “end state” reaction to feelings of imminent doom and is found in many animals about to be attacked by a predator. 6. ATYPICAL FEATURES SPECIFIER - This specifier applies to both depressive episodes, whether in the context of persistent depressive disorder or not. > individuals with this specifier consistently oversleep and overeat during their depression and therefore gain weight, leading to a higher incidence of diabetes. > although they also have considerable anxiety, they can react with interest or pleasure to some things, unlike most depressed individuals. > the atypical group also has more symptoms, more severe symptoms, more suicide attempts, and higher rates of comorbid disorders including alcohol use disorder. 7. PERIPARTUM ONSET SPECIFIER - Peri means “surrounding”—in this case, the period of time just before and just after the birth. > peripartum depression - giving birth > peripartum period - pregnancy and the 6-month period immediately following childbirth) > postpartum depression - after childbirth Note: The father and mother can try psychological interventions for paternal peripaturm depression. In general, guidelines for treating and preventing peripartum depression include CBT and interpersonal therapy. BABY BLUES - minor reactions in adjustment to childbirth, typically last a few days and occur in 40% to 80% of women between 1 and 5 days after delivery. > mothers may have an elevated corticotrophinreleasing hormone. 8. SEASONAL PATTERN SPECIFIER - This temporal specifier applies to recurrent major depressive disorder (and also to bipolar disorders). It accompanies episodes that occur during certain seasons (e.g., winter depression). SEASONAL AFFECTIVE DISORDER (SAD) - These episodes must have occurred for at least 2 years with no evidence of nonseasonal major depressive episodes occurring during that period of time. Emerging evidence suggests that SAD may be related to daily and seasonal changes in the production of melatonin, a hormone secreted by the pineal gland. PHASE SHIFT HYPOTHESIS - SAD is a result of phasedelayed circadian misalignment, meaning that the patient’s circadian rhythm is misaligned with the environmental day–night cycle. (according to this theory yung circadian rhythm though to have relationship with our mood.) PHOTOTHERAPY - a current treatment, most patients are exposed to 2 hours of bright light (2,500 lux) immediately on awakening. If the light exposure is effective, the patient begins to notice a lifting of mood within 3 to 4 days and a remission of winter depression in 1 to 2 weeks. U-SHAPED PATTERN - such that symptoms of depression were highest in young adults, decreased across middle adulthood, and then increased again in older age, with older people also experiencing an increase in distress associated with these symptoms. ACUTE GRIEF - the natural grieving process. After your initial reaction to the trauma, haveexperienced a number of depressive symptoms as well as anxiety, emotional numbness, and denial. > Usually, the natural grieving process has peaked within the first 6 months, although some people grieve for a year or longer. INTEGRATED GRIEF - The acute grief most of us would feel eventually evolves in which the finality of death and its consequences are acknowledged and the individual adjusts to the loss. For example, the very strong yearning in complicated grief seems to be associated with the activation of the dopamine neurotransmitter system. Brain-imaging studies indicate that areas of the brain associated with close relationships and attachment are active in grieving people, in addition to areas of the brain associated with more general emotional responding. OTHER DEPRESSIVE DISORDERS Premenstrual dysphoric disorder (PMDD) and disruptive mood dysregulation disorder, both depressive disorders, were added to DSM-5. PREMENSTRUAL DYSPHORIC DISORDER (PMDD) - As one can see, a combination of physical symptoms, severe mood swings, and anxiety are associated with incapacitation during this period of time. DISRUPTIVE MOOD DYSREGULATION DISORDER - A child’s mood is persistently negative between severe temper outbursts. EMIL KRAEPLIN - manic-depressive illness BIPOLAR DISORDERS - The key identifying feature of bipolar disorders is the tendency of manic episodes to alternate with major depressive episodes in an unending roller-coaster ride from the peaks of elation to the depths of despair. ONSET AND DURATION BIPOLAR II DISORDER - in which major depressive episodes alternate with hypomanic episodes rather than full manic episodes. > bipolar disorders begin more acutely; that is, they develop more suddenly. BIPOLAR I DISORDER - are the same, except the individual experiences a full manic episode. The high during a manic state is so pleasurable that people may stop taking their medication during periods of distress or discouragement in an attempt to bring on a manic state again; this is a serious challenge to professionals. CYCLOTHYMIC DISORDER - A milder but more chronic version of bipolar disorder; chronic alternation of mood elevation and depression that does not reach the severity of manic or major depressive episodes. > Individuals with cyclothymic disorder tend to be in one mood state or the other for years with relatively few periods of neutral (or euthymic) mood. > This pattern must last for at least 2 years (1 year for children and adolescents) to meet criteria for the disorder. People with cyclothymia should be treated because of their increased risk to develop the more sever bipolar I or bipolar II disorder. CHRONICALLY FLUCTUATING MOOD STATES - by definition, substantial enough to interfere with functioning. There is one specifier that is unique to bipolar I and II disorders: RAPID-CYCLING SPECIFIER - Some people move quickly in and out of depressive or manic episodes. > An individual with bipolar disorder who experiences at least four manic or depressive episodes within a year is considered to have a rapid-cycling pattern, which appears to be a severe variety of bipolar disorder that does not respond well to standard treatments. RAPID SWITCHING OR RAPID MOOD SWITCHING - When this direct transition from one mood state to another happens, and is particularly treatment-resistant form of the disorder.’ ULTRA-RAPID CYCLE - lengths that only last for days to weeks. ULTRA-ULTRA-RAPID CYCLING - in cases where cycle lengths are less than 24 hours. > switches into depression occurred at night, and switches into mania occurred at daytime, suggesting that for patients with mood cycles of 48 hours or less, the switch process is closely linked to circadian aspects. > The average age of onset for bipolar I disorder is from 15 to 18 years and for bipolar II disorder from 19 and 22 years, although cases of both can begin in childhood. > people with bipolar II disorder will progress to full bipolar I disorder. > found that as many as 67.5% of patients with unipolar depression experienced some manic symptoms. SPECTRUM - These studies raise questions about the true distinction between unipolar depression and bipolar disorder and suggest they may be on a continuum. > cyclothymia is chronic and lifelong. > In one sample of cyclothymic patients, 60% were female, and the age of onset was often during the teenage years or before, with some data suggesting the most common age of onset to be 12 to 14 years. > disruptive mood dysregulation disorder - which can be diagnosed only up to 12 years of age. > As far as mania is concerned, children under the age of 9 seem to present with more irritability and emotional swings as compared with classic manic states, particularly irritability. EMOTIONAL SWING - oscillating manic states that are less distinct than in adults, may also be characteristic of children, as are brief or rapid-cycling manic episodes lasting only part of a day. EQUIFINALITY - same product resulting from possibly different causes. FAMILIAL AND GENETIC INFLUENCES > In family studies, we look at the prevalence of a given disorder in the first-degree relatives of an individual known to have the disorder (the proband). > Twin studies, in which we examine the frequency with which identical twins (with identical genes) have the disorder, compared with fraternal twins, who share only 50% of their genes (as do all first-degree relatives). “PERMISSIVE” HYPOTHESIS - when serotonin levels are low, other neurotransmitters are “permitted” to range more widely, become dysregulated, and contribute to mood irregularities, including depression. DOPAMINE - dopamine, particularly in relationship to manic episodes, atypical depression, or depression with psychotic features. DOPAMINE AGONIST L-DOPA - to produce hypomania in bipolar patients. HYPOTHALAMIC-PITUITARY-ADRENOCOTIRCAL AXIS (HPA) - produces stress hormones. > beginning in the hypothalamus and running through the pituitary gland, which coordinates the endocrine system. NEUROHORMONES - are an increasingly important focus of study in psychopathology. CORTICOL SECTION OF THE ADRENAL GLAND - which produces the stress hormone cortisol that completes the HPA axis. CORTISOL - called a stress hormone because it is elevated during stressful life events. DEXAMETHASONE SUPPRESSION TEST (DST) - is a glucocorticoid that suppresses cortisol secretion in normal participants. ADRENAL CORTEX - secreted enough cortisol to overwhelm the suppressive effects of dexamethasone. > This theory was heralded as important because it promised the first biological laboratory test for a psychological disorder. HIPPOCAMPUS - individuals experiencing heightened levels of stress hormones over a long period undergo some shrinkage of a brain structure. > individuals experiencing heightened levels of stress hormones over a long period undergo some shrinkage of a brain structure. NEUROGENESIS - organisms ability to develop new neurons. GUT MICROBIOTA - which are the bacteria and other microorganisms residing in the human intestines. REM SLEEP - when the brain arouses, and we begin to dream. SLOW-WAVE SLEEP - REM activity that is more intense, and the stages of deepest sleep. > Most mammals are exquisitely sensitive to day length at the latitudes at which they live, and this “biological clock” controls eating, sleeping, and weight changes. ALPHA WAVES - indicate calm, positive feelings. > depressed individuals exhibit greater right-sided anterior activation of their brains, particularly in the prefrontal cortex (and less left-sided activation and, correspondingly, less alpha wave activity) than nondepressed individuals. BIPOLAR SPECTRUM PATIENTS - (individuals with subthreshold swings in mood) show elevated rather than diminished relative left-frontal EEG activity and that this brain activity predicts the onset of a full bipolar I disorder. > endocrine system, sleep and circadian rhythms, and relative activity in certain areas of the brain associated with depression. DIATHESIS-STESS MODEL - which describes possible genetic and psychological vulnerabilities. PROSPECTIVELY - to determine more accurately the precise nature of events and their relation to subsequent psychopathology. RECURRENT DEPRESSION - the clear occurrence of a severe life stress before or early in the latest episode predicts a poorer response to treatment and a longer time before remission. GENE-ENVIRONMENT CORRELATION MODEL - our genetic endowment might increase the probability that we will experience stressful life events. STRESS AND BIPOLAR DISORDER > First, typically negative stressful life events trigger depression, but a somewhat different, more positive, set of stressful life events seems to trigger mania. > Second, stress seems to initially trigger mania and depression, but as the disorder progresses, these episodes seem to develop a life of their own. > Third, some precipitants of manic episodes seem related to loss of sleep, as in the postpartum period. JET LAG - disturbed circadian rhythms. > Finally, although almost everyone who develops a mood disorder has experienced a significant stressful event, most people who experience such events do not develop mood disorders. LEARNED HELPLESSNESS THEORY OF DEPRESSION > (1) internal, in that the individual attributes negative events to personal failings (“it is all my fault”); (2) stable, in that, even after a particular negative event passes, the attribution that “additional bad things will always be my fault” remains; and (3) global, in that the attributions extend across a variety of issues. > people with depression make the worst of everything; for them, the smallest setbacks are major catastrophes. ARBITRARY INFERENCE - is evident when a depressed individual emphasizes the negative rather than the positive aspects of a situation. OVERGENERALIZATION - You are overgeneralizing from one small remark. DEPRESSIVE COGNITIVE TRIAD - They make cognitive errors in thinking negatively about themselves, their immediate world, and their future, three areas that together. NEGATIVE SCHEMA - an enduring negative cognitive belief system about some aspect of life. SELF-BLAME SCHEMA - individuals feel personally responsible for every bad thing that happens. NEGATIVE SELF-EVALUTION SCHEMA - they believe they can never do anything correctly. COGNITIVE TRIAD - the self, the world, and the future. NEGATIVE OUTLOOK - dysfunctional attributes. DOMAINS OF RACISIM - (structural racism, cultural racism, and individual-level discrimination) ACTIVATING - getting them (patient/participants) busy doing something. PSYCHOLOGICAL VULNERABILITY - experienced as feelings of inadequacy for coping with the difficulties confronting them as well as depressive cognitive styles. ACUTE TRYPTOPHAN DEPLETION (ATD) - had the effect of temporarily lowering levels of serotonin. ELECTROCONVULSIVE THERAPY (ECT) - dramatically affect brain chemistry. MEDICATIONS > selective-serotonin reuptake inhibitors (SSRIs), mixed reuptake inhibitors, tricyclic antidepressants, and monoamine oxidase (MAO) inhibitors. SELECTIVE-SEROTONIN REUPTAKE INHIBITORS (SSRIs) - specifically block the presynaptic reuptake of serotonin. > This temporarily increases levels of serotonin at the receptor site, but again the precise long-term mechanism of action is unknown, although levels of serotonin are eventually increased. MIXED REUPTAKE INHIBITORS - seem to have somewhat different mechanisms of neurobiological action. VENLAFAXINE (EFFEXOR) - blocking reuptake of norepinephrine as well as serotonin. > side effects remain, including nausea and sexual dysfunction. MONOMINE OXIDASE (MAO) INHIBITOR - they block the enzyme MAO that breaks down such neurotransmitters as norepinephrine and serotonin. > MAO inhibitors are usually prescribed only when other antidepressants are not effective. TRYCYCLIC ANTIDEPRESSANTS - were the most widely used treatments for depression before the introduction of SSRIs but are now used less commonly. > seem to have their greatest effect by down-regulating norepinephrine, although other neurotransmitter systems, particularly serotonin, are also affected. SELF-BLAME SCHEMA - individuals feel personally re systems, particularly serotonin, are also affected. > Side effects include blurred vision, dry mouth, constipation, difficulty urinating, drowsiness, weight gain (at least 13 pounds on average), and sometimes sexual dysfunction. Trycyclics are lethal if taken in excessive doses. ST. JOHN’S WORT - produces few side effects and is relatively easy to produce. REMISSION - Because the SSRIs and other drugs relieve symptoms of depression to some extent in about 50% of all patients treated but eliminate depression or come close to it in only 25% to 30% of all patients treated. TREATMENT-RESISTANT DEPRESSION - when depression does not respond adequately to drug treatment. SEQUENCES TREATMENT ALTERNATIVE DEPRESSION - examined whether it is useful to offer those individuals who did notachieve remission the alternatives of either adding a second drug or switching to a second drug. DEPRESSION CARE MANAGER - office of their primary medical care doctor including encouraging compliance with drug taking, monitoring side effects unique to older adults, and delivering a bit of psychotherapy was more effective than usual care > it is recommended that drug treatment go well beyond the termination of a depressive episode, continuing perhaps 6 to 12 months after the episode is over, or even longer. APGAR SCORE - (a measure of infant health immediately after birth that predicts IQ scores, performance in school, as well as neurological disability including cerebral palsy, epilepsy, and cognitive impairment lasting for many years after birth). LITHUIM CARBONATE (MOOD STABILIZING DRUG) - is a common salt widely available in the natural environment; It is also often effective in preventing and treating manic episodes. > anyone with recurrent manic episodes, maintenance on lithium or a related drug is recommended to prevent relapse. TRANSCRANIAL MAGNETIC STIMULATION (TMS) - it works by placing a magnetic coil over the individual’s head to generate a precisely localized electromagnetic pulse. VAGUS NERVE STIMULATION - pulses to the vagus nerve in the neck, which, in turn, is thought to influence neurotransmitter production in the brain stem and limbic system. DEEP BRAIN STIMULATION - has been used with a few severely depressed patients. In this procedure, electrodes are surgically implanted in the limbic system (the emotional brain). These electrodes are also connected to a pacemaker-like device. COGNITIVE BEHAVIORAL APPROACH Aaron T. Beck - founder of cognitive therapy Myrna Weissman and Gerald Klerman - interpersonal psychotherapy. COGNITVE-BEHAVIORAL ANALYSIS SYSTEM OF PSYCHOTHERAPY (CBASP) - which integrates cognitive, behavioral, and interpersonal strategies and focuses on problem-solving skills, particularly in the context of important relationships. MINDFULNESS-BASED THERAPY - therapy has been found to be effective for treating depression and preventing future depressive relapse and recurrence. NEUROGENESIS - in the hippocampus, which is known to be associated with resilience to depression. INTERPERSONAL PSYCHOTHERAPY (IPT) - focuses on resolving problems in existing relationships and learning to form important new interpersonal relationships. INTERPERSONAL ISSUES - dealing with interpersonal role disputes, such as marital conflict; adjusting to the loss of a relationship, such as grief over the death of a loved one; acquiring new relationships, such as getting married or establishing professional relationships; and identifying and correcting deficits in social skills that prevent the person from initiating or maintaining important relationships. Therapist first job is to identify and define an interpersonal dispute. After helping identify the dispute, the next step is to bring it to a resolution. First, the therapist helps the patient determine the stage of the dispute. 1. Negotiation stage. Both partners are aware it is a dispute, and they are trying to renegotiate it. 2. Impasse stage. The dispute smolders beneath the surface and results in low-level resentment, but no attempts are made to resolve it. 3. Resolution stage. The partners are taking some action, such as divorce, separation, or recommitting to the marriage. INSTITUTE OF MEDICINE (IOM) delineated three types of programs: universal programs, which are applied to everyone; selected interventions, which target individuals at risk for depression because of factors such as divorce, a family history of alcohol use disorder, and so on; and indicated interventions, in which the individual is already showing mild symptoms of depression ACUTE PHASE - has an enduring effect that protects some patients against relapse and others from recurrence following treatment termination. SEQUENTIAL STRATEGY - in which you start with one treatment (maybe the one the patient prefers or the one that’s most convenient) and then switch to the other only if the first choice is not entirely satisfactory. MAINTENANCE TREATMENT - to prevent relapse or recurrence over the long term. PERFECT ADHERENCE - should have received maximum benefit from the drugs. INTERPERSONAL AND SOCIAL RHYTHM THERAPY (IPSRT) - patients receiving IPSRT survived longer without a new manic or depressive episode compared with patients undergoing standard, intensive clinical management. SUICIDE SUICIDAL IDEATION - thinking seriously about suicide. SUICIDAL PLANS - the formulation of a specific method for killing oneself, (NONFATAL) SUICIDAL ATTEMPTS - the person survives. THOUGHTS - a serious contemplation of the act. The first step down the dangerous road to suicide is thinking about it. FORMALIZED SUICIDES - suicides that were approved of, such as the ancient custom in Japan of hara-kiri (lit. stomach-cut), in which individuals slit open their stomach and another person beheaded them. The purpose of hara-kiri, or seppuku, was to preserve one’s honor. > ALTRUISTIC SUICIDE - Durkheim referred to this as altruistic suicide. Durkheim also recognized the loss of social supports as an important provocation for suicide; he called this egoistic suicide. ANOMIC SUICIDES - are the result of marked disruptions, such as the sudden loss of a highprestige job. FATALISTIC SUICIDES - result from a loss of control over one’s own destiny. Sigmund Freud believed that suicide (and depression, to some extent) indicated unconscious hostility directed inward to the self rather than outward to the person or situation causing the anger. PSYCHOLOGICAL AUTOSPY - The psychological profile of the person who died by suicide is reconstructed through extensive interviews with friends and family members who are likely to know what the individual was thinking and doing in the period before death. low levels of serotonin are associated with impulsivity, instability, and the tendency to over-react to situations. HOPELESSNESS - predicts suicide among individuals whose primary mental health problem is not depression. INTERPERSONAL THEORY OF SUICIDE - cites a perception of oneself as a burden on others and a diminished sense of belonging as powerful predictors of hopelessness and subsequently suicide. SENSATION-SEEKING - predicts teenage suicidal behavior as well, above and beyond its relationship with depression and substance use. BORDERLINE PERSOALITY DISORDER - Individuals with this disorder, known for making manipulative and impulsive suicidal gestures without necessarily wanting to destroy themselves, sometimes kill themselves by mistake in as many as 10% of the cases. WERTHER EFFECT - Suicides as imitations of other suicides. PAPAGENO EFFECT - However, other media content can be associated with a decrease in suicide. STROOP TEST - people who demonstrated an implicit association between the words death/suicide and self, even if they weren’t aware of it, were six times more likely to make a suicide attempt in the next 6 months than those without this specific association. The clinician must assess for: (1) suicidal desire (ideation, hopelessness, burdensomeness, feeling trapped); (2) suicidal capability (past attempts, high anxiety and/or rage, available means); and (3) suicidal intent (available plan,expressed intent to die, preparatory behavior). NO SUICIDE CONTRACT - includes a promise not to do anything remotely connected with suicide without contacting the mental health professional first.