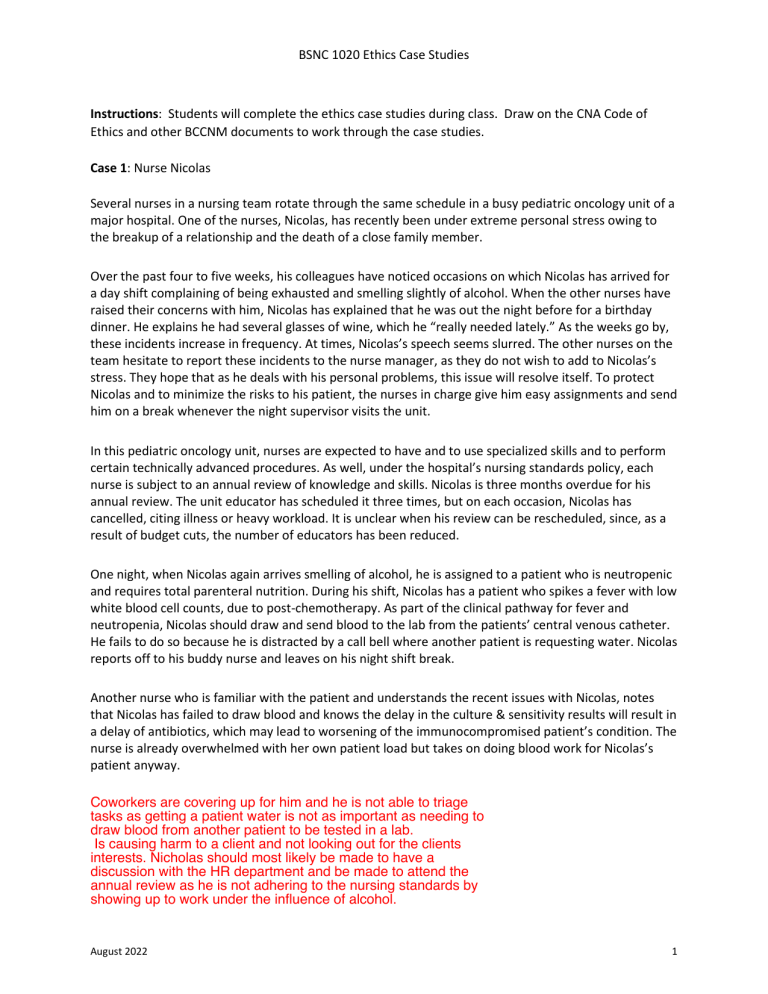
BSNC 1020 Ethics Case Studies Instructions: Students will complete the ethics case studies during class. Draw on the CNA Code of Ethics and other BCCNM documents to work through the case studies. Case 1: Nurse Nicolas Several nurses in a nursing team rotate through the same schedule in a busy pediatric oncology unit of a major hospital. One of the nurses, Nicolas, has recently been under extreme personal stress owing to the breakup of a relationship and the death of a close family member. Over the past four to five weeks, his colleagues have noticed occasions on which Nicolas has arrived for a day shift complaining of being exhausted and smelling slightly of alcohol. When the other nurses have raised their concerns with him, Nicolas has explained that he was out the night before for a birthday dinner. He explains he had several glasses of wine, which he “really needed lately.” As the weeks go by, these incidents increase in frequency. At times, Nicolas’s speech seems slurred. The other nurses on the team hesitate to report these incidents to the nurse manager, as they do not wish to add to Nicolas’s stress. They hope that as he deals with his personal problems, this issue will resolve itself. To protect Nicolas and to minimize the risks to his patient, the nurses in charge give him easy assignments and send him on a break whenever the night supervisor visits the unit. In this pediatric oncology unit, nurses are expected to have and to use specialized skills and to perform certain technically advanced procedures. As well, under the hospital’s nursing standards policy, each nurse is subject to an annual review of knowledge and skills. Nicolas is three months overdue for his annual review. The unit educator has scheduled it three times, but on each occasion, Nicolas has cancelled, citing illness or heavy workload. It is unclear when his review can be rescheduled, since, as a result of budget cuts, the number of educators has been reduced. One night, when Nicolas again arrives smelling of alcohol, he is assigned to a patient who is neutropenic and requires total parenteral nutrition. During his shift, Nicolas has a patient who spikes a fever with low white blood cell counts, due to post-chemotherapy. As part of the clinical pathway for fever and neutropenia, Nicolas should draw and send blood to the lab from the patients’ central venous catheter. He fails to do so because he is distracted by a call bell where another patient is requesting water. Nicolas reports off to his buddy nurse and leaves on his night shift break. Another nurse who is familiar with the patient and understands the recent issues with Nicolas, notes that Nicolas has failed to draw blood and knows the delay in the culture & sensitivity results will result in a delay of antibiotics, which may lead to worsening of the immunocompromised patient’s condition. The nurse is already overwhelmed with her own patient load but takes on doing blood work for Nicolas’s patient anyway. Coworkers are covering up for him and he is not able to triage tasks as getting a patient water is not as important as needing to draw blood from another patient to be tested in a lab. Is causing harm to a client and not looking out for the clients interests. Nicholas should most likely be made to have a discussion with the HR department and be made to attend the annual review as he is not adhering to the nursing standards by showing up to work under the influence of alcohol. August 2022 1 BSNC 1020 Ethics Case Studies Case 2: Nurse Kelly Kelly has been caring for Mr. Jones, a 58-year-old businessman who was admitted to a medical unit with a diagnosis of liver cirrhosis. He is currently going through alcohol withdrawal. For the past hour, he has been confused, combative, and using profanity and inappropriate sexual language. He has just now struck Kelly in the chest, and the injury is painful. Kelly informs the charge nurse (CN) and then phones the physician to report on the patient’s condition and ask that he assess the patient. Because Kelly needs to be examined by an ER physician and complete a Workers Compensation form, the CN relieves Kelly from duty and assigns another RN as her replacement. She also places the patient on 1-1 observation and assigns this to an LPN. After Kelly gives report to the RN and LPN, she decides that, despite the pain in her chest, she is able to complete her charting before leaving the unit. Just before she leaves for the ER, the CN informs Kelly that the patient has fallen out of bed and may have fractured his wrist. The LPN was in the room at the time but was unable to arrest his fall. Fortunately, there was no permanent injury caused by Mr. Jones striking Kelly in the chest yesterday. Today Kelly is back at work and assigned to Mr. Jones. Kelly finds him to be lucid this morning, and no longer exhibiting restlessness, agitation, or using profanity. However, when Kelly begins her initial assessment, Mr. Jones becomes visibly angry and accuses Kelly of causing his fall and fractured wrist. He states that the replacement nurse “didn’t know what she was doing” and that he should never have been left with such an incompetent nurse. Mr. Jones says that when he gets home, he is going to have his lawyer sue Kelly, the other nurse, and the hospital. Kelly realizes her relationship with Mr. Jones is no longer therapeutic, and so she asks the Charge Nurse to assign him to a different RN. The CN says “sure, you can have Mrs. Blair and Cindy (Mrs. Blair’s nurse) can look after Mr. Jones. She just left for coffee, but I’ll tell her when she gets back”. She then turns to the Resident to discuss an issue about another patient. The nurse should be able to distinguish between what is good and bad and not make decisions which negatively impact the client. In this case the client showed violent behaviour which effected the nurse and the next day the same nurse was asked to take care of the patient. August 2022 2 BSNC 1020 Ethics Case Studies Case 3: New mother Sally Sally is a Registered Nurse (RN) and she just delivered her second baby this morning by c-section. She is recovering in hospital with her new baby and her partner. The night nurse comes in to assess Sally around 21:30 hours. While completing her assessment, the nurse stands at the door to the room, asks a couple of questions about Sally and the baby, inquires about pain, and then leaves the room. The nurse does not return to Sally’s room for the rest of the shift. Around 04:00, Sally’s baby experiences difficulty breathing and needs help to clear some mucous from his lungs. Sally brings the baby to the nurse’s station in a rush, and the nurse helps the baby clear his airways. At the same time, Sally experiences some heavy bleeding, which Sally reports to the nurse after the baby is safe. The nurse advises Sally to go back to her room and that she would return to the room to assess her again. The nurse does not return to assess Sally. The following morning, Sally asks the day nurse if the night nurse had documented any care and if so what was documented. The day nurse summarizes the documentation. Sally informs the day nurse about the lack of care provided, indicating that the nurse did not complete an assessment of the mother, and only assessed the baby when he was in distress. August 2022 3