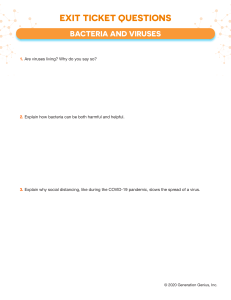
• • • • INTRODUCTORY MEDICAL MICROBIOLOGY CODE: MDID021 Medical Microbiology is a branch of medicine concerned primarily with the prevention, diagnosis and treatment of infectious diseases. Nutritional Microbiology is the study of microorganisms that contaminate food products and cause Food-Bourne diseases. What are infectious diseases? Communicable diseases? The profession of Medical Microbiology consists primarily of four major spheres of activity: • Scientific and administrative direction of a clinical microbiology laboratory. • The establishment and direction of a hospital infection control program. • Provision of clinical consultations on the investigation, diagnosis and treatment of patients suffering from infectious diseases. • Public Health and communicable disease prevention and epidemiology MICROORGANISM/MICROBES • Living organisms (such as bacteria, fungi, parasites and viruses) that are too small to be seen with naked eye but visible under a microscope and special staining techniques used to see them. BACTERIA • Microscopic, single-celled organisms, inhabit virtually all environments, including soil, water, organic matter, and the bodies of multicellular animals. • Bacteria are distinguished in part by their morphological and genetic features; for instance, they may have spherical, rod-like, or spiral shapes. • They also can be divided into two main groups, gram-positive or gramnegative, based on the structure of their cell wall and their reaction to the Gram stain. • Many bacteria swim by means of flagella (flagellum). • The DNA of most bacteria is found in a single circular chromosome and is distributed throughout the cytoplasm rather than contained within a membrane-enclosed nucleus. • Though some bacteria can cause food poisoning and infectious diseases in humans, most are harmless and many are beneficial. • They are used in various industrial processes, especially in the food industry (e.g., the production of yogurt, cheeses, and pickles). VIRUSES • A microorganism smaller than bacteria, which cannot grow or reproduce apart from a living cell. • They are acellular • A virus invades living cells and uses their chemical machinery to keep itself alive and to replicate itself. • It may reproduce with fidelity or with errors (mutations)-this ability to mutate is responsible for the ability of some viruses to change slightly in each infected person, making treatment more difficult. • Viruses may contain either DNA or RNA as their genetic material. • Herpes simplex virus and the hepatitisB virus are DNA viruses. • RNA viruses have an enzyme called reverse transcriptase that permits the usual sequence of DNA-to-RNA to be reversed so the virus can make a DNA version of itself. • RNA viruses include HIV and the hepatitis C virus. (even Corona virus) • Researchers have grouped viruses together into several major families, based on their shape, behavior, and other characteristics. • These include the herpesviruses, adenoviruses, papovaviruses (papilloma viruses), hepadnaviruses, poxviruses, and parvoviruses among the DNA viruses • On the RNA virus side, major families include the picornaviruses (including the rhinoviruses), calciviruses, paramyxoviruses, orthomyxoviruses, rhabdoviruses, filoviruses, bornaviruses, and retroviruses. • There are dozens of smaller virus families within these major classifications. Many viruses are hostspecific, causing disease in humans or specific animals only. THE STAGES OF THE LIFE CYCLE OF HUMAN IMMUNEDEFFECIENCY VIRUS (HIV-1) cause of ACQUIRED IMMUNODEFFICIENCY SYNDROME (AIDS) FUNGI • Any of about 80,000 known species of organisms belonging to the kingdom Fungi, including yeasts, rusts, smuts, molds, mushrooms, and mildews. • Though formerly classified as plants, fungi lack chlorophyll and the organized plant structures of stems, roots, and leaves. • The thallus, or body, of a typical fungus consists of a mycelium through which cytoplasm flows. • The mycelium generally reproduces by forming spores, either directly or in special fruiting bodies that make up the visible part of a fungus. • The soil provides an ideal habitat for many species, although fungi can also live in the air and water and on plants and animals. • Fungi are found in all regions of the world that have sufficient moisture to enable them to grow. • Lacking chlorophyll, fungi are unable to carry out photosynthesis and must obtain nutrients by secreting enzymes onto the surface on which they are growing. • These enzymes digest organic matter, forming solutions of nutrients that can be absorbed through the mycelium. • Essential to many food and industrial processes, fungi are used in the production of enzymes, organic acids, vitamins, and antibiotics. • Parasitic fungi invade living organisms, often causing disease and death certain insects. PARASITES • An organism that lives on or in a different kind of organism (the host) from which it gets some or all of its nourishment. • Parasites are generally harmful to their hosts, although the damage they do ranges widely from minor inconvenience to debilitating or fatal disease. • A parasite that lives or feeds on the outer surface of the host's body, such as a louse, tick, or leech, is called Ectoparasites. • Ectoparasites do not usually cause disease themselves although they are frequently a vector of disease, as in the case of ticks, which can transmit the organisms that cause such diseases as Rocky Mountain spotted fever and Lyme disease. • A parasite that lives inside the body of its host is called an Endoparasite. • Endoparasites include organisms such as tapeworms, hookworms, and trypanosomes that live within the host's organs or tissues, as well as organisms such as sporozoans that invade the host's cells. Parasitic diseases include infections by protozoa, helminths, and arthropods: • Protozoa -- Malaria is caused by plasmodium, protozoa, a single-cell organism that can only divide within its host organism. • Helminths -- Schistosomiasis, another set of very important parasitic diseases, is caused by a helminth (a worm). • Arthropods -- The arthropods include insects and arachnids (spiders, etc.), a number of which can act as vectors (carriers) of parasitic diseases. BACTERIAL CLASSIFICATION IS BASED ON SEVERAL MAJOR PROPERTIES • • • • • • • Gram staining (and other stains). Morphology. Metabolic behaviour. Infection patterns. Intracellular vs extracellular. Antigenic composition. DNA sequence. Binomial (scientific) nomenclature Gives each microbe 2 names: Genus - noun, always capitalized species - adjective, lowercase Both italicized or underlined Staphylococcus aureus (S. aureus) Bacillus subtilis (B. subtilis) Escherichia coli (E. coli) BACTERIA: MORE ON MORPHOLOGY BACTERIAL SHAPES BRIEF HISTORY OF MICROBIOLOGY Old times… • Humans knew how to deal with germs before even • knowing about their existence. Discovery of Microorganisms • Antony van Leeuwenhoek Microbiology, a Dutchman. (1632-1723), the father of • A hobbyist microscopist microorganisms accurately. • Accurate shape, detailed movement. • Subjects were most possibly bacteria and protozoa and he called them “animalcules“, also reported spermatozoa, blood cells first to observe and describe The Conflict over Spontaneous Generation spontaneous generation living organisms can develop from nonliving or decomposing matter publically a common sense vision with social and cultural roots (almost 2000 years ago) Jan Baptista Van Helmont believed in spontaneous generation Louis Pasteur (1822-1895) was the founder of modern microbiology He developed methods for bacteria, and propagated the virus of rabies in animals • • • • Pasteur Refutes the Spontaneous Generation. Ambient germs are necessary for promoting growth. Principle of sterility and aseptic work is important. Specific aseptic techniques are employed to avoid microbial contamination (e.g., Pasteur's experiments. He developed Pasteurization (Method of prevention of spoilage of liquid foodstuffs (milk, wine, beer) which utilizes heating) Germ theory: Microorganisms Cause Disease There is a relationship between Microorganisms and Disease. • The germ theory of disease states that some diseases are caused by microorganisms. • These small organisms, too small to see without magnification, invade humans, animals, and other living hosts. • Their growth and reproduction within their hosts can cause a disease. • "Germ" may refer to not just a bacterium, but also a protist, fungus, virus, prion, or viroid. • Microorganisms that cause disease are called pathogens, and the diseases they cause are called infectious diseases. • Even when a pathogen is the principal cause of a disease, environmental and hereditary factors often influence the severity of the disease, and whether a particular host individual becomes infected when exposed to the pathogen. The germ theory was proposed by Girolamo Fracastoro in 1546, but scientific evidence in support of this accumulated slowly and, Galen's miasma theory remained dominant among scientists and doctors. A transitional period began in the late 1850s as the work of Louis Pasteur and Robert Koch provided convincing evidence; by 1880, miasma theory was still competing with the germ theory of disease. Eventually, a "golden era" of bacteriology ensued, in which the theory quickly led to the identification of the actual organisms that cause many diseases. • Viruses were discovered in the 1890s. Louis Pasteur (1860s), a noted chemist, took up the challenge and utilized broths allowing air but disallowing microbes. Grew broths at different altitudes and in a dusty cellar. Used broths with cotton to show the germs accumulated on cotton. Did the Swan neck Pasteur went to work on chicken cholera and discovered one could attenuate cultures and produce artificial vaccines. Pasteur solved the riddle of rancid wines in France's vinyards. Recommended sterile technique and Pasteurization (applied to milk and became a central method for controling TB, Diptheria, and other diseases). Pasteur wanted to isolate a bacterium in pure culture that caused disease. Began working with Anthrax. Anti-spontaneous generation experiments: Pasteur definitively demonstrated that microorganisms are present in air but not created by air. Vaccine discoverer. Pasteurization. Semmelweis, Ignaz (1840s) • Hand washing/childbirth fever: • Demonstrated that hand washing prevented the spread of childbirth fever. • Ignaz Semmelweis, an eastern European physician working in a Vienna Hospital, noticed the wards where delivery occurred by midwives had 10X less Puerperal Fever and deaths than those tended to by doctors. • He showed he could dramatically decrease "Childbed Fever" by having doctors wash hands in chlorine water after dissection of cadavers and between patients. • Was fired for blaming deaths on doctors who didn't wash hands. • Oliver Wendel Holmes wrote on the Contagiousness of Puerperal Fever". Author, Physician, and Anatomy Professor. Late 19th Century. Lister, Joseph (1860s) • Chemical inhibition of infection: • Connected and applied Semmelweis' and Pasteur's work to develop and popularize the chemical inhibition of infection during surgery. • Washed surgical wounds with phenol (a.k.a., carbolic acid) • Lister is considered to be the father of antiseptic surgery. Koch, Robert (1870s) • Developed Koch's Postulates which are a sequence of experimental steps for directly relating a specific microbe to a specific disease. • Koch discovered: i. Bacillus anthracis ii. Mycobacterium tuberculosis iii.Vibrio cholera • Technique developer: • In addition to Koch's postulates, Koch played an important role in the development of the use of agar as solid medium. • Louis Pasteur along with Robert Koch developed the germ theory of disease which states that "a specific disease is caused by a specific type of microorganism." • In 1876, Robert Koch established an experimental procedure to prove the germ theory of disease. This scientific procedure is known as Koch's postulates. • Koch’s postulates not only proved the germ theory but also gave a tremendous boost to the development of microbiology by stressing a laboratory culture and identification of microorganisms. Koch's postulates: The causative agent must be present in every case of the disease and must not be present in healthy animals. The pathogen must be isolated from the diseased host animal and must be grown in pure culture. The same disease must be produced when microbes from the pure culture are inoculated into healthy susceptible animals. The same pathogen must be recoverable once again from this artificially infected animal and it must be able to be grown in pure culture. Koch’s postulates not only proved the germ theory but also gave a tremendous boost to the development of microbiology by stressing a laboratory culture and identification of microorganisms. • • • • Fleming, Alexander (1920s) Penicillin/first antibiotic: Fleming discovered that a mould accidentally growing on one of his petri dishes had antibacterial activity. The mould was producing penicillin. This was the first antibiotic discovered. Microbial diseases changed history • 14th century: Bubonic plague (Black death) caused by Yersinia pestis in Europe. • 19th century: Tuberculosis caused by Mycobacterium tuberculosis • Today: AIDS by the human immunodeficiency virus (HIV). THE NORMAL BACTERIAL FLORA OF HUMANS • In a healthy animal, the internal tissues, e.g. blood, brain, muscle, etc., are normally free of microorganisms. • However, the surface tissues, i.e., skin and mucous membranes, are constantly in contact with environmental organisms and become readily colonized by various microbial species. • The mixture of organisms regularly found at any anatomical site is referred to as the normal flora, except by researchers in the field who prefer the term "indigenous microbiota". THE NORMAL BODY FLORA • Normal Flora: Also called normal biota, normal microflora, and normal microbiota. • Hundreds of species of bacteria and fungi live symbiotically on the human body. • The Normal flora, are bacteria, fungi, and protozoa that live on or within the bodies of animals and plants. • These organisms are present on external surfaces (skin and conjunctiva of the eye) and internal surfaces (linings of the respiratory, digestive and urogenital systems) of the body. • Internal structures and organs (for example, bone, heart, liver, kidneys) are normally sterile Normal microflora may be harmless, beneficial or disease causing. • The spectrum of microorganisms changes with growth and development of the individual. • The womb provides a sterile environment for the developing fetus. Upon birth, the newborn is colonized with numerous different bacteria and fungi. • During growth and maturation, different microorganisms predominate at various sites on the body. Normal flora [normal microbiota] Not disease-causing: • Normal flora are those not-typically-diseasecausing microorganisms normally found in and on healthy individuals. • Also known as normal microbiota. Very abundant: • Normal flora are extremely abundant in terms of absolute numbers. • A normal human has approximately 1013 body cells and 1014 individual normal flora! All found externally: • Normal flora are found mostly: – – – – – – – – on the skin in the eyes in the nose in the mouth in the upper throat in the lower urethra in the lower intestine especially in the large intestine • Note that this list basically includes all of the body surfaces exposed to the external environment. SIGNIFICANCE OF THE NORMAL FLORA We are covered in microorganisms – 10 times as many prokaryotic cell (mainly bacteria) associate with our bodies. The normal flora substantially influences the well-being of the host. Although the foregoing indicates that bacterial flora may be undesirable, studies with antibiotic treated animals suggest that the flora protects individuals from pathogens. The normal flora in humans usually develops in an orderly sequence, or succession, after birth, leading to the stable populations of bacteria that make up the normal adult flora. For example, an infant begins to contact organisms as it moves through the birth canal. A Gram-positive population (bifidobacteria arid lactobacilli) predominates in the gastrointestinal tract early in life if the infant is breast-fed. This bacterial population is reduced and displaced somewhat by a Gram-negative flora (Enterobacteriaceae) when the baby is bottle-fed. The type of liquid diet provided to the infant is the principal instrument of this flora control; immunoglobulins and, perhaps, other elements in breast milk may also be important. What, then, is the significance of the normal flora? Animal and some human studies suggest that the flora influences human anatomy, physiology, lifespan, and, ultimately, cause of death. The human body provides many unique environments for different bacterial communities to live and is referred to as the host. A positive host-microbe relationship is usually described as either mutualistic or commensalistic. In mutualism both the host and the microbe benefit. Which is in contract to commensalisms, where one partner of the relationship benefits (usually the microbe) and the other partner (usually the host) is neither benefited nor harmed. The benefits of normal flora Normal flora synthesize and excrete vitamins in excess of their own needs, which can be absorbed as nutrients in the host. For example, E. coli secretes Vitamin K and certain Bvitamins. The normal flora prevent colonization by pathogens by competing for attachment sites or for essential nutrients. The normal flora may antagonize other bacteria through the production of substances which inhibit or kill nonindigenous species. The normal flora stimulate the development of certain tissues, i.e., the caecum and certain lymphatic tissues in the GI tract. The normal flora stimulate the production of cross-reactive antibodies. It is known that the normal flora behave as antigens in an animal and therefore induce immunological responses. Harmful Effects Of Normal Flora Clinical problems from normal flora arise in the following conditions: When the organisms are displaced from their normal site in the body to an abnormal site, for e.g. the introduction of the normal skin bacterium S. epidermidis into the blood stream where it can colonize catheters and heart valves. When potential pathogens gain a competitive advantage due to diminished populations of harmless competitors for e.g. when normal bowel flora is depleted by antibiotic therapy. When harmless commonly ingested food substances are converted into carcinogenic derivatives by bacteria in the colon. When an individual is immunocompromised normal flora can overgrow and become pathogenic. Their metabolism allows them to attack a broad variety of compounds in our diets, some of which they can convert to compounds that are harmful to us They can be opportunistic pathogens whenever luck or injury allows them into regions of the bodies where they are not wanted. Opportunistic infection: Clinically apparent infection with a microorganism that usually causes in apparent infection or no infection at all. When someone is weakened by illness, injury, malnutrition, or other factors, opportunistic infections may occur. Individuals with decreased resistance to infection are called compromised hosts Nosocomial infection: infections caused by medical treatment, usually in a hospital or clinic. Hospitals are full of sick people, many of whom are compromised hosts. These people often acquire opportunistic infections from hospital personnel or medical equipment. HOST DEFENCES • Host defences include both physiologic barriers and immunological responses. • Some defences are non-specific; others are highly specific. • Host defences can vary considerably due to many factors including alcohol, drugs, nutrition, immunologic disorders, etc. Skin and mucous membranes provide the first line of defence through: • Mechanical factors: physical barrier to penetration. • Chemical factors: gastric acidity, unsaturated fatty acids, lysozyme. • Microbial factors: antagonism by normal flora. Phagocytic cells provide a secondary line of defense by consuming invaders and secreting substance that produce immune responses: • Mononuclear cells: monocytes (blood) and macrophages (tissue). • Neutrophils: polymorphonuclear (PMN) granulocytes. P.T.O • Inflammation: immune response producing dilation of blood vessels, increased vascular permeability and diapedesis of monocytes. • Phagocytosis: cells destroy invaders by i) utilizing specific membrane receptors for attachment (e.g. immunoglobulin Fc and complement C3b receptors) and ii) ingesting invaders into phagocytic vacuoles, leading to intracellular killing by fusion with lysosome-like granules containing lowered pH, peroxide, enzymes, etc. Humoral factors: antibody mediated defences include: • Antitoxins: specific antibodies that bind certain exotoxins. • Bacteriolytic antibodies: antibodies plus complement can directly lyse Gram-negative cells. • Opsonizing antibodies: coat cell surface and enhance phagocytosis (Fc receptors). Cell-mediated factors: cellmediated defences include: • Cytotoxic T-lymphocytes: specific cells capable of destroying altered host cells. • K and NK cells: lyse altered or transplanted host cells. • Activated macrophages: phagocytes that possess a greatly enhanced capacity for intracellular destruction of ingested microorganisms. TRANSMISSION OF DISEASE Communicability: infectious disease can be transmitted either directly (e.g. person to person) or indirectly (e.g. contaminated water). Factors involved in the communicability of an infectious agent include: • Source, including dormant or latent infections (carriers). • Number of infectious agents released from a host. • Capability of surviving transit from host to host. • Percentage of the host population that is susceptible to the agent MECHANISMS OF PATHOGENESIS • Pathogenic properties of bacteria: microorganisms cause disease by two basic mechanisms: 1) invasion of tissue and 2) production of toxins. Invasiveness: the ability to invade host tissues. Toxigenicity: the production of toxins. Virulence: the combination of invasiveness and Toxigenicity producing the ability to overcome host defences. CONTROL OF MICROORGANISMS The control of microorganisms is desirable in several environments including: • Microbiology for prevention of contamination by extraneous organisms. • In surgery for maintenance of asepsis (absence of bacteria, viruses, other microorganisms). • In food and drug manufacture for ensuring safety from contaminating organisms. • Decontamination is the process of cleansing an object or substance to remove contaminants such as microorganisms or hazardous materials, including chemicals, radioactive substances, and infectious diseases. • The control of microorganisms is achieved through the decontamination processes of Disinfection and Sterilization. • Disinfection: It is a process in which most or nearly all microorganisms (not including their spores) capable of giving rise to infection are eliminated. • Sterilization: It is a process by which objects are freed of all microorganisms (harmful or not) both vegetative and spore state. • Sanitation: Reduction of the microbial population to levels considered safe by public health standards • Antiseptic: A mild disinfectant agent suitable for use on skin surfaces • -cidal: A suffix meaning that “the agent kills.” For example, a bactericidal agent kills bacteria and fungicidal kills fungi. • -static: A suffix that means “the agent inhibits growth.” For example, a fungistatic agent inhibits the growth of fungi, but doesn’t necessarily kill it and bacteriostatic inhibits bacteria growth, but doesn’t necessarily kill.it. Basically two Methods of Sterilization: Physical Methods and Chemical Methods PHYSICAL METHODS 1. Heat: • most reliable and preferred method • is non-selective (all organisms are susceptible including spores). • Is able to reach organisms protected from action of chemicals and radiation. • Lethal action of heat is due to denaturation of proteins and nucleic acid (DNA and RNA). • There is variation in heat resistance in different microbes. Moist Heat sterilization • Is more rapidly lethal than dry heat. • Requires lower working temperature and shorter periods of exposure. • Mechanism of killing is a combination of protein/nucleic acid denaturation and membrane disruption. Measurements of killing by Moist Heat: • Thermal death point (TDP): refers to the lowest temperature at which a microbial suspension is killed in 10 minutes at pH 7. • Thermal death time (TDT): Shortest time needed to kill all organisms in a suspension at a specified temperature under specific conditions. • Decimal reduction time (D value): Time required reducing a bacterial population by 90% (a 10-fold, or one decimal, reduction) at a specified temperature and specified conditions. • Z-value: The change in temperature, in “oC”, necessary to cause a 10-fold change in the D value of an organism under specified conditions. • F-value: The time in minutes at a specified temperature (usually 121.1oC) needed to kill a population of cells or spores. • Example of calculations using D value: • Given that the Clostridium botulinum spores are suspended in phosphate buffer, and the D121=0.204 minutes (Note 121oC). • How long would it take to reduce a population of C. botulinum spores in phosphate buffer from 1012 spores to 100 spores (1 spore) at 121oC? • Answer: Since 1012 to 100 is 12 decimal reductions, then the time required is 12x0.204minutes = 2.45minutes Methods of Moist Heat: Boiling method (100oC) • Kills vegetative forms of bacteria, fungi, and many viruses within 10 minutes. • However, bacterial spores and some viruses can survive. • • • • Autoclaving/ pressure canning Most effective method of moist heat sterilization. Is carried out in an autoclave where steam under pressure is used. Most procedures use 121.1 oC, achieved at approximately 15psi pressure, with 1530minutes autoclave time to ensure sterilization. Sterilization in autoclave in biomedical or clinical laboratory must periodically validated by testing with spores of Clostridium or Bacillus stearothemophilus. An example of an Autoclave Pasteurization • Used to reduce microbial numbers in milk and other beverages while retaining flavour and food quality of the beverage. • Retards spoilage but does not sterilize. • Traditional treatment of milk, 63oC for 30 minutes. • Flash pasteurization (high-temperature short term pasteurization); quick heating to about 720C for 15 seconds, then rapidly cooling. Ultrahigh-temperature (UHT) sterilization • Milk and similar products heated to 140-150oC for 1-3 seconds. • Very quickly sterilizes the milk while keeping its flavour and quality. • Used to produce the packaged “shelf milk” that does not require refrigeration. Dry Heat Sterilization Incineration • Burner flames: direct flaming of inoculating loop. • Electric loop incinerators. • Incineration of infected carcasses, laboratory animals and infected material using controlled air, excess air or rotary kiln incinerators. Hot air oven sterilization • Hot air oven sterilization • Used to sterilize glassware and heatresistant metal equipment. • Objects are exposed for 2 hours at 160oC–180oC in an electric or gas oven. • Treatment denatures proteins and cell membranes desiccate cytoplasm and oxidize cellular components. 2. Filtration Method • Used for physically removing microbes and dust particles of heat labile liquids e.g. urea, vitamin. • Liquid is filtered through sterile membrane filters capable of retaining microbes e.g. 0.45µm; 0.22 µm pore diameter. • Examples of filters: • Membrane filters e.g. Nitrocellulose nylon, polyvinylidene difluoride. • HEPA filters: High efficiency particulate air filters used in laminar flow biological safety cabinets 3. Radiation Method • Has varying effects on cells depending on its wavelength, intensity and duration. a) Ionizing Radiation • Example: x-rays (0.001-0.1nanometre (nm): Gamma rays (0.12-100nm) b) Non-Ionizing Radiation • Example: Ultraviolet (UV) radiation (10- about 400nm). 4. Low Temperatures a) Refrigerator: • around 4°C • inhibits growth of mesophiles or thermophiles; psychrophiles will grow b) Freezer: • ordinary” freezer around -10 to -20°C • “ultra cold” laboratory freezer typically 80°C • Generally, inhibits all growth; many bacteria and other microbes may survive freezing temperatures CHEMICAL METHODS • Chemical agents are used to sterilize body surfaces and inanimate objects. • Most do not achieve sterility but reduce microbial population to safe levels. Characteristics of an ideal Disinfectant: • Acts quickly. • Attack all or wide range of microbes. • Is able to penetrate thoroughly the material that is contaminated. • Readily mixes with water to form a stable solution. • Is not hampered (reduced activity) by organic matter on the substance that is to be disinfected. • Is not likely to decompose and lose its activity after exposure to light, heat or unfavorable weather. • Does not stain, corrode, or destroy the object being disinfected. • Is not toxic to man and animals if it is to be used as an antiseptic. Types of Chemical agents • • • • • • • Phenols and Phenolics Alcohols Halogens Aldehydes Sterilizing Gases Heavy metals and their compounds Antimicrobial Chemotherapeutic agents Antimicrobial Chemotherapeutic agents These are drugs which have lethal (Bactericidal) or inhibitory effects (bacteriostatic) on the microbes. Ideal characteristics of antimicrobial drugs: • Should have selective toxicity i.e. should be toxic for the microorganism and not for the host. • Should not produce hypersensitivity in most host e.g.. Sensitivity to penicillin in form of skin rash. • Must have solubility in body fluids so that it can readily or rapidly penetrate body tissues. • Should not readily lead to development of drug resistance by microorganisms. • The drug should not eliminate the normal flora of the host where opportunistic pathogen e.g. Pseudomonas, Candida albicans cause superinfections. • Should have broad spectrum activity i.e. being effective against a large number of Gram positive and Gram negative species of bacteria. However, the problem is that broad spectrum drugs can also kill normal flora. Four categories of antimicrobial drugs namely: • Antibacterial • Antiviral • Antiparasitic • Antifungal i) Antibacterial/antibiotic drugs Classes of Antibiotics target organisms Penicillins: penicillin G, ampicillin, methicillin, Gram +ve bacteria oxacillin, carbenicillin Cephalosporins: cephalothin,cefazolin, cefuroxime, Gram +ve bacteria ceftriaxone, ceftazidine Moderate against gram –ve bacteria Aminoglycosides: streptomycin, neomycin, Gram -ve bacteria kanamycin, gentamycin. doxycycline Gram +ve and Gram -ve bacteria; rickettsia, chlamydias Erythromycins/Macrolides: erythromycin, Gram +ve bacteria Tetracyclines: tetracycline, chlortetracycline, spiramycin, clindamycin Polypeptides: bacitracin, polymyxin Gram +ve bacteria Some Gram -ve bacteria MODE OF ACTION OF ANTIBIOTICS They interfere chemically with synthesis of function of vital components of microorganisms. Cellular structures and functions of prokaryotic cells (bacteria) differ from those of eukaryotic cells of human body and provides basis for selective toxicity. Inhibition of cell wall synthesis • Drug prevents formation of peptide cross bridges in actively growing bacteria resulting in weakened cell wall and cell lyses. • Examples of drugs: Penicillin, ampicillin, methicillin, oxacillin- effective against gram positive organisms. Inhibition of Protein synthesis • Antibiotics combine with either 50s or 30s subunits of 70s ribosomes where they inhibit peptide bond formation in growing polypeptide chain of protein. • Examples of drugs: chloramphenicol, erythromycin, tetracycline Injury to cytoplasmic membrane • Polypeptide antibiotics attach to cytoplasmic membrane where they change its permeability resulting in loss of metabolites from microbial. These antibiotics are toxic to host tissue and have limited use in chemotherapy • Example: Polymyxin B. Inhibition of nucleic acid synthesis • Antibiotics also toxic to host cells due to similarities in microbial and host cell DNA and RNA metabolism. Have limited clinical use • Example: Trimethoprim Inhibition of enzymatic activity • Drugs bind to enzyme in organism preventing its activity e.g.. Enzyme involved in folic acid synthesis in bacteria. • Example: Sulfonamides Mechanisms of antibacterial resistance During treatment with drugs, bacteria may acquire resistance towards them. The following are various mechanisms by which bacteria can acquire drug resistance: Accumulation barriers • Cell wall and membrane provide barriers to drugs. • Outer membrane of Gram negative bacteria provides a formidable barrier for access to the interior of the cell. • Some bacteria have energy dependent efflux mechanisms that pump drugs from the cell. Altered target • Once in the cell; drugs act by binding and inactivating their targets which is typically a crucial enzyme or ribosomal site. • If the target is altered by substitution of a single amino acid at a certain location in a protein, then it alters its binding affinity to the drug without affecting its function in the bacterial cell. Enzymatic inactivation • Enzymes produced by resistant bacteria may inactivate the drug in the cell; in periplasmic space or outside cell. • They may act by disrupting the structure of the drug. • For example, B-lactamases may break open the B-lactam ring of Penicillin and inactivate the drug. • Some enzymes produced modify the drug by phosphorylating the amino group on aminoglycosides (e.g.. Streptomycin, neomycin, kanamycin, gentamicin) rendering them ineffective. Chromosomal resistance • Develops as a result of mutation on chromosome. • Presence of drug serves as selecting mechanism to suppress susceptible microorganisms and favor growth of resistant mutant. Extrachromosomal resistance • Plasmids e.g. R-factor carry genes for resistance to one or several antimicrobial drugs. • Plasmids code for enzymes that destroy antimicrobial drug. Antiviral drugs Mode of action of antivirals Inhibition of cell penetration and uncoating • Inhibits several early steps in viral replication including viral uncoating. • Examples: Amantadine; rimantadine • • • • Inhibition of reverse transcriptase enzyme (Nucleoside analogue of Thymidine) Inhibits the reverse transcriptase enzyme of RNA containing viruses e.g. HIV All terminates the elongation of the chain that is initially synthesized to initiate replication of viral genome. Toxicity frequently occurs. Examples: Lamivudine, Stavudine, Inhibition of reverse transcriptase enzyme (Non-Nucleoside analogue) • Also inhibits reverse transcriptase enzyme in RNA viruses e.g. HIV • Relatively non-toxic. • Examples: Nevirapine; Efavirenz Inhibition of protease enzyme • These block the action of viral coded enzyme protease. • Protease is responsible for cleaving polypeptides to produce structural proteins. • Inhibition of this enzyme leads to blockage of viral assembly and release. • Causes hepatotoxicity. • Examples; Saquinavir, ritonavir, indinavir, nelfinavir Mechanisms of antiviral resistance • Resistance is largely due to mutations in genes that code for production of enzymes. Antifungal drugs • These act against fungi. Mode of action of antifungals P.T.O • Azoles act by inhibiting the action of cytochrome P450 dependent sterol 14αdemethylase enzyme with resulting in cooperation of 14-methyl sterol which is thought to disrupt membrane structure and function thereby inhibiting fungal growth. Examples: Ketoconazole, miconazole, Itraconazole, clotrimazole • Polyenes acts by binding to ergosterol leading to distortion and damage of normal membrane permeability. Results in leakage of intracellular constituents and cell death. Examples: amphotericin B; Nystatin Mechanisms of antifungal resistance • Secretion of some cellular enzymes to extracellular medium which degrade drug. • The drug is pumped out by an efflux pump. • The drug target is altered so that the drug cannot bind to the target. • The target enzyme is overproduced so that the drug does not inhibit biochemical reactions completely. • The cell develops a bypass route for production of drug target. Antiparasitic drugs These drugs act on parasites. • Mode of action of antiparasitic drugs • Quinolones block nucleic acid synthesis by intercalation into double stranded DNA. • Example: chloroquine • Quinones blocks pyrimidine biosynthesis and inhibition of parasites mitochondrial electron transport chain. • Example: Atovaquone • Praziquantel induces loss of intracellular calcium, titanic muscular contraction and destruction of the tegument.