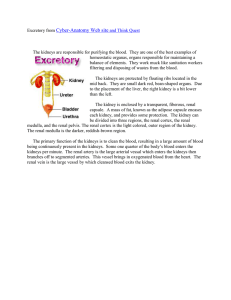
CHRONIC KIDNEY DISEASE a.k.a CHRONIC RENAL FAILURE - CKD is an umbrella term that describes kidney damage / ↓ in GFR for 3 or more mos. o GFR: bld test that checks how well kidneys are working estimates how much bld passes thru glomeruli each minute kidneys have glomeruli - - filters & helps remove wastes and excess fluids from bld o obtain bld sample let client fast for 8 hrs associated w/ ↓ quality of life, ↑ health care expenditures, premature death significant ↓ in renal fx; IRREVERSIBLE o (AKD – reversible) Untreated CKD = END-STAGE RENAL DSE (ESRD) - necessitate kidney replacement therapy o dialysis o kidney transplantation (last resort) - STAGE 1 to STAGE 5 PATHOPHYSIOLOGY 4 BASIC PROCESSES: FORMATION OF URINE 1. FILTRATION – mass movement of water and solutes from plasma to the renal tubule that occurs in the renal corpuscle. o 180 liters of fluid are filtered by the kidneys every day o entire plasma volume (about 3 liters) is filtered 60 times a day o primarily driven by hydraulic pressure (blood pressure) in the capillaries of the glomerulus. - kidneys filter much more fluid than the amount of urine that is actually excreted (about 1.5 liters per day). This is essential for the kidneys to rapidly remove waste and toxins from the plasma efficiently. 2. REABSORPTION - movement of water and solutes from the tubule back into the plasma (70% is reabsorbed) Reabsorption of water and specific solutes occurs to varying degrees over the entire length of the renal tubule. o many important solutes (glucose, amino acids, bicarbonate) are actively transported out of the proximal tubule such that their concentrations are normally extremely low in the remaining fluid. REGULATED REABSORPTION: hormones control the rate of transport of sodium and water depending on systemic conditions, takes place in the distal tubule and collecting duct. 3. SECRETION - Even after filtration has occured, the tubules continue to secrete additional substances into the tubular fluid. This enhances the kidney's ability to eliminate certain wastes and toxins (urea & crea). It is also essential to regulation of plasma potassium concentrations and pH. 4. EXCRETION - end result of the above three processes. last product is urine NEPHRONS kidneys have millions of nephrons nephrons have glomerulus - glomerulus: filters fluid & ions (electrolytes, bicarbs), waste products (urea – BUN, crea) o UREA – by product of protein breakdown from liver o CREATININE – waste product from breakdown of muscles o thus, we have your GFR Stage 1: (+) proteinuria (seen in U/A) Stage 2: mild loss of renal fx w/ proteinuria Stage 3: mild to severe loss of renal fx first 3 stages = asymptomatic however, s/sx will become more evident as dse progresses Stage 4: severe loss of renal fx Stage 5: ESRD - - - ASSESSMENT Subjective cues - Nausea - Loss of appetite - fatigue & weakness - sleep problems - anxiety - anorexia - paresthesia Objective cues - ↑ serum crea levels Glomerulus not functioning well = waste products (toxins, crea) are not being filtered and stays in the body - edema water is retained, hypervolemia, fluid overload - ↓ UO Malfunction of glomeruli = water is not excreted Oliguria: <400 ml/day Anuria: <100 mL/day - High BP Due to hypervolemia, pressure ↑ - abnormalities w/ Ca & P, & Mg ↓ Ca due to ↓ Vit. D - Anemia Kidney malfunctions = low erythropoietin (EPO – stimulates the production of RBC in bone marrow) - Metabolic acidosis Commonly found in px w/ CKD Causes: impaired ammonia excretion, reduced tubular bicarb reabsorption, insufficient renal bicarb production in relation to the amount of acids synthesised by the body and ingested with food. Pruritus – Uremic pruritus Aka KIDNEY-ASSOC. PRURITUS Due to elevated BUN Itching due to urea crystals on the skin --- white frost (uremic frost) in the skin Also caused by Ca phosphate crystals (accumulated in skin) Uremic – excessive urea in bld Occurs when both kidneys stop working Common problem to px w/ ESRD check K & Phosphate & Mg (↑) Ca is depleted due to phosphate bones become weak & brittle (+) proteinuria ---- hematuria (albumin – oncotic pressure) EPO = helps created RBC & bone marrow RENIN – increases BP - since there is less water, renin is stimulated to increase BP (HPN) Vit. D malabsorption: Hypocalcemia MEDICAL MANAGEMENT SPECIAL NOTATION 1. The mgt of px w/ CKD includes tx of the underlying causes 2. Nutritional therapy 3. Renal replacement therapy (dialysis, kidney transplant) 4. Measures to treat hyperlipidemia 5. Measures to lower K Laboratory/Diagnostic Examination Hx & PE - Identification of reversible kidney dse - Renal UTZ - Renal scan - CT scan - renal biopsy - BUN, serum creatinine, creatinine clearance levels – bld often a blood sample may also be taken to measure crea, serum protein levels, & BUN, esp. when 24-hour urine has been ordered - - Serum electrolytes Lipid profile Protein-to-creatinine ratio i1st morning voided specimen Urine is collected in a container The collection process generally begins first thing in the morning For a 24-hour urine collection, the process generally begins by discarding the first morning void and then collecting all of the urine for the remaining 24-hour period. --send to lab, refrigerated, no preservatives in the container Occasionally, a split 24-hour sample w/ a night collection, 11-7, separated form the collection of morning (7-11) may be used Assoc. w/ 24-hour total protein excretion Urinalysis (proteinuria) Hematocrit & hemoglobin levels Underlying causes: - high BP - DM MEDICATIONS: - Erythropoietin therapy o so anemia would not occur o expensive o also used in cancer px esp. if hemoglobin is ↓ - Ca supplementation, phosphate binders (Ca carbonate) o used for tx of hyperphosphatemia o ex. Ca acetate - Antihypertensive therapy o ACE (-pril) or ARBs (-sartan) o slows the process of renal dse in px. w/ diabetes by interfering w. reninangiotensin system; o reduce intraglomerular pressure by inhibiting angiotensin II ̶ mediated efferent arteriolar vasoconstriction. - Adjustment of drug dosages to degree of renal fx IV FLUIDS: - correction of extracellular fluid volume overload / deficit During ESRD: px will experience - hypovolemia - anemia - electrolyte imbalance - waste product retention - low UO focus interventions on s/sx of hyperkalemia: muscle weakness, palpitations, urine abnormalities, dysrhythmias 1. 2. 3. 4. 5. 6. 7. 8. NURSING INTERVENTIONS Assess fluid status & identify potential sources of imbalance Nutritional intake: Implement a dietary program to ensure proper nutritional intake w/in limits of the tx regimen Independence: Promote positive self feelings by encouraging increased self-care & greater independence Protein: Promote intake of high-biologic-value protein foods: eggs, dairy products, meats a. minimize protein, needs some to prevent muscle wasting but not as madami kasi may sir ana sa kidney Medication: Alter sched of meds so that they are not given immediately before meals Rest: Encourage alternating activity w/ rest S/SX of electrolyte imbalance, esp. high K a. N: 3.5 – 5 mEq/L b. hyperkalemia: Tall, tinted T wave, widened QRS, long PR interval c. restrict K-rich foods: potatoes, avocadoes, strawberries d. KAYEXALATE as ordered (orally / rectally) to decrease K Alternative ways of reducing thirst, such that sucking on ice cubes, lemon, hard candy Report any of the following: - Weight gain >4 lb (2kg) - Increasing BP - Shortness of breath (due to fluid accumulation in lungs) - Edema - Increasing fatigue / weakness - Confusion / lethargy o due to accumulation of toxic wastes (ammonia, urea, crea) o promote safety Need changes, living w/ a chronic illness, and decisions about type of dialysis or transplantation CAUSES - DM o - - uncontrolled hyperlgycemia casues glucose to stick to artery walls --damage to blood supply to kidneys HPN o high pressure on artery walls to kidneys -- less blood supply to nephrons --- less O2 others: Acute kidney injury, polycystic kidney dse, infection, nephrotoxic drugs (NSAIDS – paracetamol, acetaminophen, abx – aminoglycosides, chemotherapeutic drugs, contrast dyes) TX 1. control BP and glucose a. meds (ACE inhibitors, ARBs) 2. monitor GFR and BP regularly 3. Dialysis 4. Kidney transplant NSG MGT: Uremia – increased waste in bld (esp. BUN) pH is usually less that 7.35 = metabolic acidosis - kussmaul’s breathing (deep rapid breathing) - check lung sounds: crackles – pulmonary edema Anemia - pale, tired, shortness of breath, confusion - iron supplement - EPO SC - blood transfu Low UO - monitor I&O - daily weight Some doctors restrict fluid & low Na diet and CHON