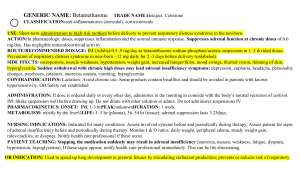
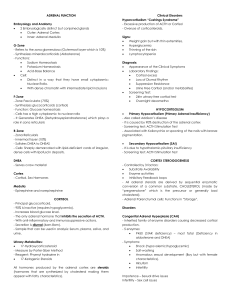
45 Adrenal Gland Disorders Devra K. Dang, Judy T. Chen, Frank Pucino, Jr, and Karim Anton Calis LEARNING OBJECTIVES Upon completion of the chapter, the reader will be able to: 1. Explain the regulation and physiologic roles of hormones produced by the adrenal glands. 2. Recognize the clinical presentation of adrenal insufficiency. 3. Describe the pharmacologic management of acute and chronic adrenal insufficiency. 4. Recommend therapy monitoring parameters for adrenal insufficiency. 5. Recognize the clinical presentation of Cushing syndrome and the physiologic consequences of cortisol excess. 6. Describe the pharmacologic and nonpharmacologic management of Cushing syndrome. 7. Recommend strategies to prevent the development of hypercortisolism and hypocortisolism. 8. Recommend therapy monitoring parameters for Cushing syndrome. INTRODUCTION T he adrenal glands are important in the synthesis and regulation of key human hormones. They play a crucial role in water and electrolyte homeostasis, as well as regulation of blood pressure, carbohydrate and fat metabolism, physiologic response to stress, and sexual development and differentiation. This chapter focuses on pharmacologic and nonpharmacologic management of the two most common conditions associated with adrenal gland dysfunction: glucocorticoid insufficiency (eg, Addison disease) and glucocorticoid excess (Cushing syndrome). Other adrenal disorders such as congenital adrenal hyperplasia, pheochromocytoma, hypoaldosteronism, and hyperaldosteronism are beyond the scope of this chapter. PHYSIOLOGY, ANATOMY, AND BIOCHEMISTRY OF THE ADRENAL GLAND The adrenal gland is located on the upper segment of the kidney. It consists of an outer cortex and an inner medulla. The adrenal medulla secretes the catecholamines epinephrine (also called adrenaline) and norepinephrine (also called noradrenaline), which are involved in the regulation of the sympathetic nervous system. The adrenal cortex consists of three histologically distinct zones: the outer zona glomerulosa, the zona fasciculata, and an innermost layer called the zona reticularis. Each zone is responsible for production of different hormones (Figure 45–1).1 The zona glomerulosa is responsible for the production of the mineralocorticoids aldosterone, 18-hydroxy-corticosterone, corticosterone, and deoxycorticosterone. Aldosterone promotes renal sodium retention and potassium excretion. Its synthesis and release are regulated by renin in response to decreased vascular volume and renal perfusion. Adrenal aldosterone production is regulated by the renin-angiotensin-aldosterone system. The zona fasciculata is the middle layer and produces the glucocorticoid hormone cortisol. Cortisol is responsible for maintaining homeostasis of carbohydrate, protein, and fat metabolism. Its secretion follows a circadian rhythm, generally beginning to rise at approximately 3 to 4 am and peaking around 6 to 8 am. Thereafter, cortisol levels decrease throughout the day, approach 50% of the peak value by 4 pm, and reach their nadir around midnight.2 The normal rate of cortisol production is approximately 8 to 15 mg/day.3 Cortisol plays a key role in the body’s response to stress. Its production increases markedly during physiologic stress, such as during acute illness, surgery, or trauma. In addition, certain conditions such as alcoholism, depression, anxiety disorder, obsessive-compulsive disorder, poorly controlled diabetes, morbid obesity, starvation, anorexia nervosa, and chronic renal failure are associated with increased cortisol levels. High total cortisol levels are also observed in the presence of increased cortisol binding globulin (the carrier protein for 80% of circulating cortisol molecules), which is seen in pregnancy or other high-estrogen states (eg, exogenous estrogen administration).2 Cortisol is converted in the liver to an inactive metabolite known as cortisone. The zona reticularis produces the androgens androstenedione, dehydroepiandrosterone (DHEA), and the sulfated form of dehydroepiandrosterone (DHEA-S). Only a small amount of testosterone and estrogen is produced in the adrenal glands. Androstenedione and DHEA are converted in the periphery, largely to testosterone and estrogen. Adrenal hormone production is controlled by the hypothalamus and pituitary. Corticotropin-releasing hormone (CRH) is secreted by the hypothalamus and stimulates secretion of adrenocorticotropic hormone (ACTH; also known as corticotropin) from the anterior pituitary. ACTH in turn stimulates the adrenal cortex to produce cortisol. When sufficient or excessive cortisol 695 696 SECTION 7 | ENDOCRINOLOGIC DISORDERS H3C H3C H3C H CH3 H H3C H H HO Cholesterol Glucocorticoid precursors CYP11A1 ADX O H3C H3C O CH3 H3C H3C H H O Progesterone H3C O CH3 H3C H H3C H H POR CYP17A1 H3C H3C O 17-Hydroxyprogesterone (17OHP) POR CYP17A1 H H H3C O Androstenedione DHEA PAPSS2 SULT2A1 O 11Deoxycortisol O H3C H3C H Adrenal androgen precursors O Testosterone H O HSD11B2 H3C H O OH Cortisone Zona Fasciculata Glucocorticoids H H SRD5A OH OH HSD11B1 Cortisol H3C O Aldosterone H H H6PDH H H HSD17B H3C O H3C H H ADX CYP11B1 H O OH OH H O H H HSD3B2 H3C H3C H3C H HO H O POR CYP21A2 H O O H3C H ADX CYP11B2 18OH-Corticosterone H3C HO H H O 17-Hydroxy- HSD3B2 pregnenolone H H 5-Dihydrotestosterone Zona Reticularis - Androgens H H HO H3C H H O OH OH OH H3C H ADX CYP11B2 Corticosterone O CHO HO OH H3C O H3C OH HO H H Deoxycorticosterone CYP11B1 H H H HO H CH3 H3C OH OH H ADX O CYP11B2 POR CYP17A1 POR CYP17A1 H3C POR O CYP21A2 HSD3B2 Pregnenolone OH O HO H3C HO H H O O H3C H H H HO O CH3 H3C H Zona Glomerulosa - Mineralcortocoids Mineralocorticoid precursors H DHEAS FIGURE 45–1. The adrenal cortex consists of three histologically distinct zones: the outer zona glomerulosa, the middle zona fasciculata, and an innermost layer called the zona reticularis. Each zone is responsible for production of different hormones. The zona glomerulosa is responsible for the production of mineralocorticoids such as aldosterone. The zona fasciculata produces cortisol and the zona reticularis produces androgens. ADX, adrenodoxin; CYP11A1, side chain cleavage enzyme; CYP17A1, 17-α-hydroxylase/17,20 lyase; CYP21A2, 21-hydroxylase; CYP11B1, 11-β-hydroxylase; CYP11B2, aldosterone synthase; DHEA, dehydroepiandrosterone; DHEAS, dehydroepiandrosterone sulfate; H6PDH, hexose-6-phosphate dehydrogenase; HSD11B1, 11-β-hydroxysteroid dehydrogenase type 1; HSD11B2, 11-β-hydroxysteroid dehydrogenase type 2; HSD3B2, 3-β-hydroxysteroid dehydrogenase type 2; HSD17B, 17-β-hydroxysteroid dehydrogenase; PAPSS2, PAPS synthase type 2; POR, P450 oxidoreductase; SRD5A, 5-α-reductase; SULT2A1, DHEA sulfotransferase. Adapted, with permission, from Arlt W. Disorders of the adrenal cortex. In: Longo DL, Fauci AS, Kasper DL, et al., eds. Harrison’s Principles of Internal Medicine. New York: McGraw-Hill, 2011. levels are reached, a negative feedback is exerted on the secretion of CRH and ACTH, thereby decreasing overall cortisol production. The control of adrenal androgen synthesis also follows a similar negative feedback mechanism. Figure 46–1 depicts hormonal regulation with the hypothalamic-pituitary-adrenal (HPA) axis. ADRENAL INSUFFICIENCY Epidemiology and Etiology Adrenal insufficiency generally refers to the inability of the adrenal glands to produce adequate amounts of cortisol for normal physiologic functioning or in times of stress. The condition is usually classified as primary, secondary, or tertiary, depending on the etiology (Table 45–1).2,4–7 The estimated prevalence of primary adrenal insufficiency and secondary adrenal insufficiency is approximately 60 to 143 and 150 to 280 cases per 1 million persons, respectively. Whereas primary adrenal insufficiency is usually diagnosed in the third to fifth decade of life, secondary adrenal insufficiency is commonly detected during the sixth decade.2,8 Adrenal insufficiency is more prevalent in women than in men, with a ratio of 2.6:1.2 Chronic adrenal insufficiency is rare. CHAPTER 45 | ADRENAL GLAND DISORDERS 697 Table 45–1 Etiologies of Adrenal Insufficiency2,4–7 Primary Adrenal Insufficiency (Addison disease) •• Autoimmune—accounts for 70%–90% of all cases of primary adrenal insufficiency •• Infectious or granulomatous diseases •• Cytomegalovirus •• Fungal (histoplasmosis, coccidioidomycosis, cryptococcosis, Blastomyces dermatitidis infection) •• HIV (human immunodeficiency virus), AIDS (acquired immunodeficiency syndrome) •• Mycobacterial, cytomegaloviral, Pneumocystic jiroveci, and Toxoplasma gondii infection •• Sarcoidosis •• Tuberculosis •• Bilateral adrenal hemorrhage or infarction—usually due to anticoagulant therapy, coagulopathy, thromboembolic disease, or meningococcal infection. Causes acute adrenal insufficiency •• Adrenalectomy •• Adrenoleukodystrophy (in men) •• Adrenomyeloneuropathy •• Infiltrative disorders: amyloidosis, hemochromatosis •• Genetic causes •• Congenital adrenal hyperplasia •• Familial glucocorticoid deficiency and hypoplasia •• Metastatic malignancy Secondary Adrenal Insufficiency •• Cushing syndrome •• Panhypopituitarism •• Pituitary tumor •• Transsphenoidal pituitary microsurgery •• Pituitary irradiation •• Traumatic brain injury Tertiary Adrenal Insufficiency •• Hypothalamic dysfunction Drug-induced (most common cause of secondary and tertiary adrenal insufficiency) •• Chronic glucocorticoid administration at supraphysiologic doses •• Steroidogenesis inhibitors •• Megestrol acetate—has glucocorticoid-like activity •• Mifepristone (RU 486)—antagonizes glucocorticoid receptors •• Tyrosine kinase inhibitors •• Inducers of CYP450 enzymes that increase cortisol metabolism (2B1, 2B2, 3A4) CYP450, cytochrome P-450 Pathophysiology Primary adrenal insufficiency, also known as Addison disease, occurs when the adrenal glands are unable to produce cortisol. It occurs from destruction of the adrenal cortex, usually from an autoimmune process. In general, the clinical manifestations are observed when destruction of the cortex exceeds 90%.6 Signs and symptoms of adrenal insufficiency reflect the disturbance of normal physiologic carbohydrate, fat, and protein homeostasis caused by inadequate cortisol production and inadequate cortisol action. Primary adrenal insufficiency usually develops gradually. Patients may remain asymptomatic in the early stages with signs and symptoms present only during times of physiologic stress. Persistent signs and symptoms of hypocortisolism typically occur with disease progression. Additionally, Clinical Presentation and Diagnosis of Chronic Adrenal Insufficiency2,5,6,8 General •• Symptoms develop gradually, especially in the early stages, may be vague, and mimic other medical conditions. •• Patients with autoimmune adrenal insufficiency may have other autoimmune disorders such as type 1 diabetes mellitus or autoimmune thyroiditis. Symptoms (Percent Prevalence) •• Weakness and fatigue (99%) •• Anorexia, nausea, and diarrhea (56%–90%); may range from mild to severe with vomiting and abdominal pain •• Hypoglycemia may occur •• Amenorrhea may occur •• Salt craving occurs in approximately 22% with Addison disease due to aldosterone deficiency Signs •• Weight loss (97%) •• Hypotension (less than 110/70 mm Hg) and orthostasis (87%) •• Dehydration, hypovolemia, and hyperkalemia (in primary adrenal insufficiency only) due to aldosterone deficiency. •• Hyponatremia and hypochloridemia levels due to aldosterone deficiency. Hyponatremia can also be present in secondary insufficiency due to cortisol deficiency and increased antidiuretic hormone secretion leading to subsequent water retention. •• Increased serum blood urea nitrogen and creatinine due to dehydration. •• Hyperpigmentation of skin and mucous membranes (92%). Usually observed around creases, pressure areas, areolas, genitalia, and new scars. Dark freckles and patches of vitiligo may be present. Hyperpigmentation, due to increased ACTH levels, occurs in most patients with primary but not secondary or tertiary insufficiency. •• Personality changes (irritability and restlessness) due to cortisol deficiency. •• Loss of axillary and pubic hair in women due to decreased androgen production. •• Blood count abnormalities (normocytic, normochromic anemia, relative lymphocytosis, neutrophilia, eosinophilia) due to cortisol and androgen deficiency. Laboratory Tests (see Table 45–21,5,9,10) •• Decreased basal and stress-induced cortisol levels. •• Decreased aldosterone level (in primary insufficiency only). •• Lack of increase in cortisol and aldosterone level after ACTH stimulation. Other Diagnostic Tests •• Computed tomography (CT) scan or magnetic resonance imaging (MRI) of the adrenal glands, pituitary, and/or hypothalamus can aid in determining etiology. •• Presence of antiadrenal antibodies is suggestive of an autoimmune etiology. 698 SECTION 7 | ENDOCRINOLOGIC DISORDERS Table 45–2 Tests for Diagnosing Adrenal Insufficiency1,2,5,10 Test Procedure Rationale Screening and Diagnostic Tests for Adrenal Insufficiency Unstimulated Measure serum Serum cortisol level peaks serum cortisol cortisol at 6–8 am in the early morning measurement Rapid ACTH stimulation test (also called cosyntropin stimulation test) Measure serum cortisol 30–60 minutes after administering cosyntropin 250 mcg IM or IV Insulin tolerance test Administer insulin (insulin-induced IV to induce hypoglycemia test) hypoglycemia then measure serum cortisol during symptomatic hypoglycemia (confirm that blood glucose is < 40 mg/dL [2.2 mmol/L]) Overnight metyrapone test Administer metyrapone at midnight then measure serum cortisol at 8 am the next day Finding in Adrenal Insufficiency Serum cortisol < 3 mcg/dL (83 nmol/L) Increased cortisol secretion Serum cortisol in normal individuals concentration in response to ACTH < 18–20 mcg/dL stimulation but not in (497–552 nmol/L) adrenal insufficiency Evaluates ability of entire HPA axis to respond to stress (hypoglycemia) Serum cortisol concentration < 18 mcg/dL (497 nmol/L) is indicative of secondary adrenal insufficiency Comments •• Evaluate result in context of those from other test(s) •• Can be performed in conjunction with the rapid ACTH stimulation test (measure baseline serum cortisol before administering 250 mcg of cosyntropin) •• Used as gold standard test for diagnosing primary adrenal insufficiency •• False negative results may occur if ACTH deficiency is of recent onset (< 1 month) •• If measured serum cortisol concentration is low, measure plasma ACTH, aldosterone, and renin concentrations to differentiate between primary and secondary or tertiary adrenal insufficiency (see below) •• A normal response does not exclude mild secondary adrenal insufficiency or recent onset ACTH deficiency. Additional testing (eg, insulin tolerance or metyrapone test) may be required •• If the result of the rapid ACTH stimulation test is normal, either this or the overnight metyrapone test is still needed to evaluate for secondary adrenal insufficiency. The insulin tolerance test is considered the gold standard •• Contraindicated in patients with a seizure history, older than 60 years, or with cardiovascular or cerebrovascular disease •• Requires close medical supervision •• Contraindicated in adrenal crisis and primary adrenal insufficiency •• Distinguishes between normal individuals and patients with secondary adrenal insufficiency •• Contraindicated in adrenal crisis and primary adrenal insufficiency Metyrapone inhibits Normal response is a cortisol synthesis. Its decrease in serum administration leads to cortisol to < 5 mcg/dL rise in levels of ACTH and (138 nmol/L) and the precursor of cortisol, an increase in 11-deoxycortisol. Patients 11-deoxycortisol to with adrenal insufficiency > 7 mcg/dL (202 nmol/L). do not exhibit this Response not seen in secondary adrenal insufficiency Tests for Differential Diagnosis of Primary, Secondary, and Tertiary Adrenal Insufficiency Plasma ACTH Measure plasma In primary adrenal •• Primary adrenal •• Evaluate result of test in combination concentration ACTH insufficiency, insufficiency: elevated with those from the plasma hypocortisolism leads to plasma ACTH. aldosterone and plasma renin tests elevated plasma ACTH •• Secondary or tertiary concentration via positive adrenal insufficiency: HPA axis feedback plasma ACTH low or inappropriately normal (Continued) CHAPTER 45 | ADRENAL GLAND DISORDERS 699 Table 45–2 Tests for Diagnosing Adrenal Insufficiency1,2,5,10 (Continued) Test Plasma aldosterone concentration Plasma renin concentration or activity Finding in Adrenal Procedure Rationale Insufficiency Comments Measure plasma Patients with primary •• Primary adrenal •• Evaluate result of test in combination aldosterone adrenal insufficiency may insufficiency: low plasma with those from plasma ACTH and from same blood experience a reduction in aldosterone plasma renin tests samples as those aldosterone production •• Secondary or tertiary used in ACTH adrenal insufficiency: stimulation test aldosterone concentration is usually normal (≥ 5 ng/dL [139 pmol/L]) Measure Mineralocorticoid •• Primary adrenal •• Evaluate result of test in combination plasma renin deficiency occurs insufficiency: elevated with those from plasma ACTH and concentration or in primary adrenal plasma renin plasma aldosterone concentration activity insufficiency but is usually •• Secondary or tertiary tests not present in secondary adrenal insufficiency: or tertiary adrenal plasma renin insufficiency concentration or activity is usually normal ACTH, adrenocorticotropic hormone or corticotropin; HPA, hypothalamic-pituitary-adrenal; IM, intramuscularly; IV, intravenously primary adrenal insufficiency may be accompanied by a reduction in aldosterone and androgen production. Secondary adrenal insufficiency occurs as a result of pituitary gland dysfunction, whereby decreased production and secretion of ACTH leads to a decrease in cortisol synthesis. Tertiary adrenal insufficiency is a disorder of the hypothalamus that results in decreased production and release of CRH, which in turn decreases pituitary ACTH production and release. In contrast to Addison disease, aldosterone production is unaffected in the secondary and tertiary forms of the disease. Chronic adrenal insufficiency often has a good prognosis if diagnosed early and treated appropriately. Acute adrenal insufficiency (ie, adrenal crisis) results from the body’s inability to sufficiently increase endogenous cortisol during periods of excessive physiologic stress. Adrenal crisis can occur when patients with chronic adrenal insufficiency do not receive adequate glucocorticoid replacement during stressful conditions such as those experienced during surgery, infection, fever, acute illness, invasive medical procedures, or trauma. Acute adrenal insufficiency can also result from bilateral adrenal infarction due to hemorrhage, embolus, sepsis, or adrenal vein thrombosis. Patients who are critically ill may also experience impaired HPA axis function, with an overall prevalence rate of 10% to 20%, and as high as 60% in those experiencing septic Clinical Presentation and Diagnosis of Acute Adrenal Insufficiency (Adrenal Crisis)2,6,8 General •• Onset of symptoms is acute and precipitated by excessive physiologic stress or abrupt discontinuation of supraphysiologic doses of chronic glucocorticoid. Symptoms •• Severe weakness and fatigue •• Abdominal or flank pain Signs •• Severe dehydration leading to hypotension and shock (circulatory collapse). Hypovolemia may not be responsive to intravenous (IV) hydration and may require the use of vasopressors. •• Tachycardia •• Nausea, vomiting •• Fever •• Confusion •• Hypoglycemia •• Laboratory abnormalities are similar to those observed in chronic adrenal insufficiency. Laboratory Tests •• The unstimulated serum cortisol and rapid ACTH stimulation tests are useful in diagnosis (see Table 45–2). The insulin tolerance test is contraindicated due to preexisting hypoglycemia. The metyrapone test is also contraindicated since metyrapone inhibits cortisol production. Note: Due to the life-threatening nature of this condition, empiric treatment should be started before laboratory confirmation in patients who present with the clinical picture of acute adrenal crisis. 700 SECTION 7 | ENDOCRINOLOGIC DISORDERS shock. These patients are also at risk for the life-threatening consequences of an adrenal crisis. To better recognize this condition, the term critical illness–related corticosteroid insufficiency was coined by the American College of Critical Care Medicine Task Force.9 Additionally, abrupt discontinuation or rapid tapering of glucocorticoids, given chronically in supraphysiologic doses, may lead to adrenal crisis. This condition results from prolonged suppression of the HPA axis and subsequent adrenal gland atrophy and hypocortisolemia. Other drugs associated with adrenal insufficiency include those that inhibit production (eg, ketoconazole) or increase metabolism (eg, the cytochrome P-450 3A4 inducer rifampin) of cortisol.6 Regardless of the etiology, patients experiencing an adrenal crisis require immediate glucocorticoid treatment since manifestations such as circulatory collapse can lead to life-threatening sequelae. Treatment and Outcome Evaluation »» Chronic Adrenal Insufficiency The general goals of treatment are to manage symptoms and prevent development of adrenal crisis. Lifelong glucocorticoid replacement therapy may be necessary for patients with adrenal insufficiency, and mineralocorticoid replacement therapy is usually required for those with Addison disease. Glucocorticoids with sufficient mineralocorticoid activity are generally required. However, the addition of a potent mineralocorticoid such as fludrocortisone, along with adequate salt intake, is sometimes needed to prevent sodium loss, hyperkalemia, and intravascular volume depletion. Mineralocorticoid supplementation typically is not indicated for the treatment of secondary or tertiary adrenal insufficiency because aldosterone production is often unaffected. Moreover, patients with secondary or tertiary adrenal insufficiency may only require replacement therapy until the HPA axis recovers. Hydrocortisone is often prescribed because it most closely resembles endogenous cortisol with its relatively high mineralocorticoid activity and short halflife, and allows the design of regimens that simulate the normal circadian cycle.5 Other glucocorticoids, however, can be used. Table 45–3 lists the pharmacologic characteristics of commonly used glucocorticoids.11 Because patients with primary adrenal insufficiency can experience DHEA deficiency, DHEA replacement has also been tried. Several small clinical studies, consisting mostly of women, suggest that treatment with DHEA can improve mood and fatigue and provide a general sense of well-being.12–14 However, a recent meta-analysis of 10 studies found that DHEA use in women only slightly improved health-related quality of life and depression but did not affect anxiety or sexual well-being; it concluded that the totality of available data does not support routine supplementation with DHEA.15 The use of DHEA remains controversial and requires further study. Management strategies for chronic adrenal insufficiency are outlined below:2,4,5,8,16 •• For the treatment of primary adrenal insufficiency (Addison disease) in adults, 15–25 mg/day of oral hydrocortisone is typically administered in two divided doses, with two-thirds of the dose given in the morning upon awakening to mimic the early morning rise in endogenous cortisol, and the remaining one-third of the dose given in the late afternoon to avoid insomnia and allow for the lowest concentration in the blood at around midnight. Hydrocortisone may also be given in three doses but this may decrease adherence. The longeracting glucocorticoids (eg, prednisone, dexamethasone) may provide a more prolonged clinical response thereby avoiding symptom recurrence that can occur at the end of the dosing interval with short-acting agents such as hydrocortisone. Longer-acting agents also may improve adherence in some patients. Monitor the patient’s weight, blood pressure, and serum electrolytes along with symptom resolution and general well-being; adjust dosages accordingly as needed. Doses of hydrocortisone, dexamethasone, prednisone, and other glucocorticoids may need to be increased or decreased in patients taking cytochrome P-450 (CYP450) 3A4 inducers or inhibitors, respectively. Monitor for adverse drug reactions related to glucocorticoid administration. Glucocorticoid therapy at physiologic replacement doses should not lead to development of Cushing syndrome; Table 45–3 Pharmacologic Characteristics of Major Corticosteroids11 Corticosteroid Glucocorticoid Cortisol Cortisone Prednisone Prednisolone Methylprednisolone Triamcinolone Betamethasone Dexamethasone Mineralocorticoid Fludrocortisone Glucocorticoid (AntiInflammatory) Potency Mineralocorticoid (Sodium-Retaining) Potency 1 0.8 4 4 5 5 25 25 1 0.8 0.8 0.8 0.5 0 0 0 S S I I I I L L 20 25 5 5 4 4 0.75 0.75 10 125 I c Duration of Actiona Equivalent Dose (mg)b S, short (ie, 8–12 hour biological t1/2); I, intermediate (ie, 12–36 hour biological t1/2); L, long (ie, 36–72 hour biological t1/2). These dose relationships apply only to oral or intravenous administration, as glucocorticoid potencies may differ greatly following intramuscular or intraarticular administration. c This agent is not used for glucocorticoid effects. Adapted, with permission, from Shimmer BP, Funder JW. ACTH, adrenal steroids, and pharmacology of the adrenal cortex. In: Brunton LL, Chabner BA, Knollmann BC, eds. Pharmacological Basis of Therapeutics, 12th ed. New York: McGraw-Hill, 2011: Figure 42–2. a b CHAPTER 45 | ADRENAL GLAND DISORDERS 701 Patient Encounter 1, Part 1: Presentation and Medical History A 48-year-old woman presents to the primary care clinic with complaints of fatigue and asking for a prescription for “vitamin injections.” She states that she has been feeling very tired for the past year. Upon further questioning, she also complains of dizziness, especially with positional changes, and intermittent nausea, abdominal pain, and diarrhea. PMH: Tuberculosis—completed treatment course; history of candidal vulvovaginitis; depression FH: Mother with type 1 diabetes SH: Denies smoking, alcohol use or illicit drug use Current Meds: Sertraline 100 mg once daily; loperamide 2 mg as needed for diarrhea (nonprescription) PE: VS: Sitting BP 106/68 mm Hg, P 74 beats/min, standing BP 96/68 mm Hg, RR 14 breaths/min, Wt 130 pounds (59 kg)— 5 pound (2.3 kg) loss in last 6 months, Ht 5′2″(157 cm) however, careful monitoring should still be performed, and the smallest effective dose used. Educate patients regarding the need for increased glucocorticoid dosage during excessive physiologic stress. In addition, administer oral fludrocortisone at a daily dose of approximately 0.05 to 0.2 mg in the morning. Monitor for resolution of hypotension, dizziness, dehydration, hyponatremia, and hyperkalemia; and increase the dose if needed. Conversely, consider decreasing the dose if adverse reactions from mineralocorticoid administration such as hypertension, hypokalemia, fluid retention, and other significant adverse events occur. In patients receiving hydrocortisone, it should be noted that this drug also possesses mineralocorticoid activity. All patients with Addison disease should also maintain adequate sodium intake. Lastly, although controversial, consider giving DHEA 25–50 mg/day (in the morning) to female patients who do not experience an improvement in mood and well-being even with adequate glucocorticoid and mineralocorticoid replacement. In these patients, monitor serum DHEA-S (aim for the middle range of normal levels in healthy young people) and free testosterone level. •• Patients with secondary and tertiary adrenal insufficiency are treated with oral hydrocortisone or a longer-acting glucocorticoid as described for primary adrenal insufficiency. Patient Encounter 1, Part 2: Treatment After appropriate laboratory and diagnostic tests are performed, the patient is diagnosed with Addison disease. How should her chronic primary adrenal insufficiency be treated? What monitoring parameters (therapeutic and toxic) should be implemented? Skin: Hyperpigmentation in creases of palms CV: RRR, normal S1, S2; no murmurs, rubs, or gallops Labs (fasting): Serum electrolytes: sodium 133 mEq/L (133 mmol/L), potassium 5.2 mEq/L (5.2 mmol/L), chloride 98 mEq/L (98 mmol/L), bicarb 30 mEq/L (30 mmol/L), blood urea nitrogen (BUN) 25 mg/dL (8.9 mmol/L), serum creatinine 1.2 mg/dL (106 μmol/L), glucose 60 mg/dL (3.3 mmol/L). Which signs or symptoms of adrenal insufficiency does the patient exhibit? Does her presentation offer any clues as to etiology or classification of adrenal insufficiency? Which tests would be most useful for determining etiology and confirming diagnosis of adrenal insufficiency? However, patients with secondary and tertiary adrenal insufficiency may require a lower dose. Some patients (eg, patients with drug-induced adrenal insufficiency or adrenal insufficiency following treatment for Cushing syndrome) will only require glucocorticoid replacement temporarily, which can be discontinued after recovery of the HPA axis. Monitor for progression of the underlying etiology of adrenal insufficiency. Fludrocortisone therapy is generally not needed. »» Acute Adrenal Insufficiency During an acute adrenal crisis, the immediate treatment goals are to correct volume depletion, manage hypoglycemia, and provide glucocorticoid replacement. Volume depletion and hypoglycemia can be corrected by giving large volumes (~ 2–3 L) of IV normal saline and 5% dextrose solution.2 Glucocorticoid replacement can be accomplished by administering IV hydrocortisone, starting at a dose of 100 mg every 6 hours for 24 hours, decreasing to 50 mg every 6 hours on the second day after achieving hemodynamic stability, and thereafter be tapered to a lower maintenance dose by the fourth or fifth day and fludrocortisone can be added if needed. The dose can be increased to 200 to 400 mg/day if complications.2 For the treatment of patients with critical illness-related corticosteroid insufficiency, see the 2008 consensus statements from the American College of Critical Care Medicine Task Force.9 Patients with known adrenal insufficiency should be educated about the need for additional glucocorticoid replacement and prompt medical attention during periods of physiologic stress. Although the dosage of glucocorticoid is generally individualized, a common recommendation is to double the maintenance dose of hydrocortisone if the patient experiences fever or undergoes invasive dental or diagnostic procedures.5 Patients who experience vomiting or diarrhea may not adequately absorb oral glucocorticoids and may benefit from parenteral therapy until symptoms resolve. Prior to surgery, additional glucocorticoid replacement (higher dose and parenteral route) must be given to prevent adrenal crisis. The dose and protocol varies depending 702 SECTION 7 | ENDOCRINOLOGIC DISORDERS Patient Care Process: Adrenal Insufficiency on the type of surgery (eg, larger doses for major surgery compared to minor surgery). Patient Assessment: •• Evaluate for typical clinical manifestations of chronic or acute adrenal insufficiency. Clinical presentation can differentiate between chronic primary and secondary/ tertiary adrenal insufficiency. •• Review medical and medication history to determine if the patient has any etiologies of adrenal insufficiency. •• Perform the rapid ACTH stimulation test to assess for presence of adrenal insufficiency (see Table 45–2). •• After diagnosis is confirmed, perform further testing to differentiate between primary, secondary, and tertiary adrenal insufficiency (see Table 45–2). HYPERCORTISOLISM (CUSHING SYNDROME) Therapy Evaluation: •• Determine whether patient will require mineralocorticoid replacement therapy in addition to glucocorticoid supplementation. Cushing syndrome can be classified as ACTH-dependent or ACTH-independent (Table 45–4).1,18–20 ACTH-dependent Cushing syndrome results from ACTH-secreting (or rarely CRH-secreting) adenomas. The term Cushing disease refers specifically to Cushing syndrome from an ACTH-secreting pituitary adenoma. ACTH-independent Cushing syndrome is due either to excessive cortisol secretion by the adrenal glands (independent of ACTH stimulation) or to exogenous glucocorticoid administration. The plasma ACTH concentration is elevated in ACTH-dependent conditions but not in ACTH-independent conditions because elevated cortisol concentrations suppress pituitary ACTH secretion via negative feedback. ACTH and cortisol concentrations are elevated episodically in ACTH-dependent Care Plan Development: •• In patients presenting with acute adrenal crisis not previously diagnosed with adrenal insufficiency, immediate treatment with injectable hydrocortisone and IV saline and dextrose solutions should be initiated prior to confirmation of diagnosis because of the life-threatening nature of this condition. Determine and correct the underlying cause of the acute adrenal crisis (eg, infection). •• In patients with chronic adrenal insufficiency, devise a strategy to give supplemental doses of glucocorticoid when varying degrees of physiologic stress are experienced (eg, minor infection, pending surgery). Monitor patient for signs of an acute adrenal crisis and develop a plan to treat this emergency condition. •• Educate both patient and family members/caregiver regarding: •• Causes of adrenal insufficiency, including drug-induced etiologies. •• How to recognize clinical manifestations. •• How to prevent an acute adrenal crisis: adhere to therapy; do not abruptly stop glucocorticoid treatment; increase glucocorticoid dose during different severity levels of physiologic stress including childbirth. •• When to self-administer parenteral glucocorticoid and seek emergency care. •• Need to notify all health care providers of condition. •• Wearing or carrying a medical alert (eg, bracelet, card). •• Dietary and pharmacologic therapy, including duration of treatment and potential adverse consequences of glucocorticoid and mineralocorticoid replacement. Follow-Up Evaluation: •• Monitor for adequacy of treatment and adverse reactions from glucocorticoid and/or mineralocorticoid therapy. •• Determine duration of treatment for patients with secondary and tertiary adrenal insufficiency. Epidemiology and Etiology Cushing syndrome refers to the pathophysiologic changes associated with exposure to supraphysiologic cortisol concentrations (endogenous hypercortisolism) or pharmacologic doses of glucocorticoids (exogenous hypercortisolism). Cushing syndrome from endogenous causes is a rare condition, with an estimated incidence of two to five cases per 1 million persons per year.17 Patients receiving chronic supraphysiologic doses of glucocorticoids, such as those with rheumatologic disorders, are at high risk of developing Cushing syndrome. Pathophysiology Table 45–4 Etiologies of Cushing Syndrome2,18–20 ACTH-Dependent •• ACTH-secreting pituitary tumor (Cushing disease)—70% of endogenous cases •• ACTH-secreting nonpituitary tumors (ectopic ACTH syndrome)—15% of endogenous cases; usually from small cell lung carcinoma and bronchial carcinoids; also from pheochromocytoma, or from thymus, pancreatic, ovarian, or thyroid tumor. The tumor is usually disseminated (difficult to localize). •• CRH-secreting nonpituitary tumors (ectopic CRH syndrome)—rare ACTH-Independent—15% of endogenous cases •• Unilateral adrenal adenoma •• Adrenal carcinoma •• Bilateral nodular adrenal hyperplasia—rare (< 1%) Drug-Induced Cushing Syndrome (ACTH-independent)—most common cause of Cushing syndrome •• Prescription glucocorticoid preparations (most routes of administration) •• Nonprescription and herbal products with glucocorticoid activity (eg, nonprescription anti-itch products with hydrocortisone, herbal products with magnolia bark or those claiming to contain adrenal cortex extracts or other by-products) •• Other drugs with glucocorticoid activity (eg, megestrol acetate, medroxyprogesterone) ACTH, adrenocorticotropic hormone or corticotropin; CRH, corticotropin-releasing hormone CHAPTER 45 | ADRENAL GLAND DISORDERS 703 Clinical Presentation and Diagnosis of Cushing Syndrome2,17,18,24 General •• Onset of signs and symptoms range from gradual to rapid, depending on etiology. •• Differential diagnoses include diabetes mellitus and the metabolic syndrome because these conditions share several similar characteristics with Cushing syndrome (eg, obesity, hypertension, hyperlipidemia, hyperglycemia, and insulin resistance). In women, the presentations of hirsutism, menstrual abnormalities, and insulin resistance are similar to those of polycystic ovary syndrome. Cushing syndrome can be differentiated from these conditions by identifying the classic signs and symptoms described below. •• True Cushing syndrome also must be distinguished from other conditions that share some clinical presentations (as well as elevated plasma cortisol concentrations) such as depression, anxiety disorder, obsessive-compulsive disorder, alcoholism, obesity, uncontrolled diabetes, eating disorders, and physiologic stress—the so-called pseudo-Cushing states. Signs and Symptoms (Percent Prevalence) General appearance •• Weight gain and obesity, manifesting as truncal obesity (90%) •• Rounded and puffy face (“moon facies”) (75%) •• Dorsocervical (“buffalo hump”) and supraclavicular fat accumulation •• Hirsutism (75%) Skin changes from atrophy of dermis and connective tissue •• Thin skin •• Facial plethora (70%) •• Skin striae (“stretch marks” that are usually red or purple in appearance and greater than 1 cm) (50%)—not common in patients older than 40 years of age •• Acne (35%) •• Easy bruising (40%) •• Hyperpigmentation—typically with ectopic ACTH syndrome Metabolic •• Hyperglycemia that can range from impaired glucose tolerance (75%) to diabetes mellitus (20%–50%) •• Hyperlipidemia (70%) •• Polyuria (30%) disease due to random hypersecretion of ACTH.6 In general, patients with Cushing syndrome due to endogenous or exogenous glucocorticoid excess present with similar clinical manifestations. However, patients with ectopic ACTH syndrome may not exhibit the typical signs and symptoms of hypercortisolism due to the acute onset nature of the underlying disease process.2 Cushing disease and adrenal carcinomas cause adrenal androgen hypersecretion in high enough concentrations to result in signs of androgen excess such as acne, menstrual irregularities, and hirsutism, and cause virilization in women.6 Drug-induced Cushing syndrome from glucocorticoid administration occurs most commonly in patients receiving oral therapy, but other •• Kidney stones (15%–50%) •• Hypokalemic alkalosis (from mineralocorticoid effect of cortisol) Cardiovascular •• Hypertension (from mineralocorticoid effect of cortisol) (85%) •• Peripheral edema Genitourinary •• Menstrual irregularities (typically amenorrhea) (70%) •• Erectile dysfunction (85%) Other •• Psychiatric changes such as depression, emotional lability, psychosis, euphoria, anxiety, and decreased cognition (85%) •• Sleep disturbances •• Osteopenia (80%) and osteoporosis—usually affecting trabecular bone •• Linear growth impairment in children •• Proximal muscle weakness (65%) •• Avascular necrosis (more common in iatrogenic cases) •• Glaucoma, cataracts •• Impaired wound healing and susceptibility to opportunistic infections •• Hypothyroidism Laboratory tests •• Diagnosis is often complex and generally requires the involvement of endocrinologists and specialized testing centers. •• Initial screening tests are listed in Table 45–5.2,24 Typically, a combination of two screening tests is used to establish the preliminary diagnosis. •• After the diagnosis is confirmed, additional tests (eg, midnight serum cortisol or combined dexamethasone suppression plus CRH test) can be performed to determine the etiology or rule out false positive/negative results. Other diagnostic tests Imaging studies and inferior petrosal sinus sampling may be needed to distinguish between pituitary, ectopic, and adrenal tumors. routes such as inhalation, dermal, nasal, and intraarticular have also been implicated.18 Over-the-counter products, including dietary supplements, should also be evaluated since they may contain corticosteroids. Drug-induced Cushing syndrome has been reported with the use of Chinese herbal products adulterated with corticosteroids.21,22 The risk of glucocorticoid-induced Cushing syndrome appears to increase with higher doses and/or longer treatment durations.18 Left untreated, patients with Cushing syndrome may experience severe complications of hypercortisolism, resulting in up to a nearly four-fold increase in mortality.23 Mortality in patients with Cushing is mostly attributed to cardiovascular disease. 704 SECTION 7 | ENDOCRINOLOGIC DISORDERS Table 45–5 First-Line Screening Tests in Patients with Characteristics of Cushing Syndrome2,24 Test Procedure and Measurement Rationale 24-hour urinary free cortisol Collect urine over 24 hours and measure unbound cortisol excreted by kidneys Urinary cortisol is elevated in hypercortisolic states Overnight dexamethasone suppression test (DST) Give 1 mg oral dexamethasone at 11 pm, then measure plasma cortisol at 8–9 am the next morning Late-night salivary cortisol Collect salivary cortisol concentration at 11 pm Test Typical Finding in Cushing Syndrome Comments Elevated urinary •• Easy to perform but should not be used free cortisol (value alone since sensitivity and specificity depends on the assay depend on assay used used) •• To exclude periodic hypercortisolism, two or more samples should be obtained (with urinary creatinine measurement to assess completeness of collection) •• Distinguishes the effects of Cushing syndrome (elevation) from obesity (no elevation). However, false positive in other pseudo-Cushing states, physiologic stress, if fluid intake ≥ 5 L/day, or taking carbamazepine or fenofibrate (if measured by HPLC) •• False negative if moderate to severe renal function, or subclinical hypercortisolism Dexamethasone Plasma cortisol < 1.8 •• Simple to perform and inexpensive administration μg/dL (50 nmol/L) •• Can be used in conjunction with, or suppresses morning is not suggestive of instead of, the urinary free cortisol test plasma cortisol in Cushing syndrome •• False positive if pseudo-Cushing normal individuals states, physiologic stress, pregnancy, estrogen treatment (including contraceptives), uremia, taking inducers of dexamethasone metabolism (phenytoin, alcohol, etc), or decreased dexamethasone absorption •• False negative if subclinical hypercortisolism, slow metabolism of dexamethasone (eg, CYP3A4 inhibitors), or liver or renal impairment •• In pseudo-Cushing states, the 48-hour 2-mg DST (administer 0.5 mg dexamethasone every 6 hours for 48 hours then measure serum cortisol at 8 or 9 am after the last dose) is preferred Loss of circadian Elevated late-night •• Easiest screening test to perform rhythm of cortisol salivary cortisol (sample can be collected at home by secretion (no nadir patient) at night) in Cushing •• To exclude periodic hypercortisolism, syndrome but not two or more samples (on two separate in pseudo-Cushing evenings) should be obtained states •• False positive possible with cigarette smoking, chewing tobacco, licorice ingestion, in pseudo-Cushing states •• Adjust collection time in shift workers and others with bedtime significantly after midnight CYP, cytochrome P-450; HPLC, high-performance liquid chromatography Hypertension, hyperglycemia, and hyperlipidemia are common findings and can be associated with cardiac hypertrophy, atherosclerosis, and hypercoagulability. Osteopenia, osteoporosis, and increased fractures also have been reported.23 Prevention and management of these conditions are discussed elsewhere in this text. Children may experience linear growth retardation from reduced growth hormone secretion and inhibition of epiphyseal cartilage development in long bones.17,23 Treatment The goal of treatment in patients with Cushing syndrome is reversal of hypercortisolism and management of the associated comorbidities, including the potential for long-term sequelae such as cardiac hypertrophy. Surgical resection is considered the treatment of choice for Cushing syndrome from endogenous causes if the tumor can be localized and if there are CHAPTER 45 | ADRENAL GLAND DISORDERS 705 no contraindications. The treatment of choice for Cushing syndrome from exogenous causes is gradual discontinuation of the offending agent. »» Nonpharmacologic Therapy Transsphenoidal pituitary microsurgery is the treatment of choice for Cushing disease. Removal of the pituitary tumor can bring about complete remission or cure in 78% to 97% of cases. HPA axis suppression associated with chronic hypercortisolism can result in prolonged adrenal insufficiency lasting for months after surgery and requiring exogenous glucocorticoid administration. Pituitary irradiation or bilateral adrenalectomy is usually reserved for patients who are not surgical candidates or for those who relapse or do not achieve complete remission following pituitary surgery. Because the response to pituitary irradiation can be delayed (several months to years), concomitant treatment with cortisol-lowering medication may be necessary. Bilateral adrenalectomy is also used for management of adrenal carcinoma and in patients with poorly controlled ectopic Cushing disease in whom the ACTH-producing lesion cannot be localized. Bilateral laparoscopic adrenalectomy achieves an immediate and total remission (nearly 100% cure rate), but these patients will require lifelong glucocorticoid and mineralocorticoid supplementation.7,25 Nelson syndrome may develop in nearly 20% to 50% of patients who undergo bilateral adrenalectomy without pituitary irradiation. This condition presumably results from persistent hypersecretion of ACTH by the intact pituitary adenoma, which continues to grow because of the loss of feedback inhibition by cortisol. Treatment of Nelson syndrome may involve pituitary irradiation or surgery.6 The treatment of choice in patients with adrenal adenomas is unilateral laparoscopic adrenalectomy. These patients require glucocorticoid supplementation during and after surgery due to atrophy of the contralateral adrenal gland and suppression of the HPA axis. Glucocorticoid therapy is continued until recovery of the remaining adrenal gland is achieved. Patients with adrenal carcinomas have a poor prognosis, with a 5-year survival of 20% to 58%, because of the advanced nature of the condition (metastatic disease). Surgical resection to reduce tumor burden and size, pharmacologic therapy, or bilateral laparoscopic adrenalectomy are the treatment options commonly utilized to manage this condition.2,7 »» Pharmacologic Therapy Pharmacotherapy is indicated when the ectopic ACTHsecreting tumor cannot be localized; to control hypercortisolism to prepare for surgery; and in patients who: (1) are not surgical candidates; (2) have failed surgery or had a relapse after surgery; or (3) have Cushing disease awaiting the onset of effect of pituitary radiation.26 The drugs used are classified according to their mechanism and site of action (Table 45–625–31). The most widely used therapeutic class is the adrenal steroidogenesis inhibitors, which can improve hypercortisolism by inhibiting enzymes involved in the biosynthesis of cortisol.26 Because of their potential to cause adrenal suppression, temporary glucocorticoid replacement, and in some cases mineralocorticoid supplementation, may be needed during and after treatment. In drug-induced Cushing syndrome, discontinuation of the offending agent is the best management option. However, abrupt withdrawal of the glucocorticoid can result in adrenal insufficiency or exacerbation of the underlying disease.18 Glucocorticoid doses less than 7.5 mg/day of prednisone or its equivalent for less than 3 weeks generally would not be expected to lead to suppression of the HPA axis.3,7 However, in patients receiving pharmacologic doses of glucocorticoids for prolonged periods, gradual tapering to near physiologic levels (5–7.5 mg/ day of prednisone or its equivalent) should precede drug discontinuation. Administration of a short-acting glucocorticoid in the morning and use of alternate-day dosing may reduce the risk of adrenal suppression. Testing of the HPA axis may be useful in assessing adrenal reserve. In some cases, supplemental glucocorticoid administration during excessive physiologic stress may be needed for up to 1 year after glucocorticoid discontinuation.18 Table 45–7 lists strategies to prevent the development of hypercortisolism and hypocortisolism. Outcome Evaluation •• Monitor patients receiving surgical, medical, or radiation therapy for resolution of the clinical manifestations of hypercortisolism. Symptoms often improve immediately after surgery and soon after initiation of drug therapy. However, it may take months for symptoms to resolve following radiation therapy. •• Monitor for normalization of serum cortisol concentrations. •• Patient Care Process discusses additional evaluation strategies. Patient Encounter 2 A 61-year-old man presents to a clinical pharmacist for diabetes education. He was recently diagnosed with type 2 diabetes. He also has a diagnosis of hypertension, atrial fibrillation, dyslipidemia, chronic obstructive pulmonary disease (COPD), and depression. He complains of thirst, polyuria, and fatigue. Physical exam reveals an obese (BMI 37 kg/m2) gentleman with truncal obesity, dorsocervical fat, several small bruises on abdomen and extremities, and facial plethora. His current medications include metformin, lisinopril, hydrochlorothiazide, warfarin, atorvastatin, fluticasone/salmeterol, tiotropium, albuterol, and fluoxetine. He has been treated several times this year with high-dose prednisone therapy for frequent COPD exacerbations. The clinical pharmacist suggests evaluation for possible Cushing syndrome. Which findings are suggestive of Cushing syndrome? Aside from Cushing syndrome, what are some major differential diagnoses for clinical presentation? The patient is diagnosed with drug-induced Cushing syndrome after evaluation and diagnostic testing by the endocrinologist. What patient education points should be provided?