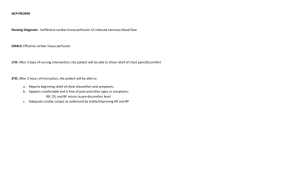
Coronary Artery Disease Virtually silent until the artery is approximately 40% blocked. Non-modifiable risk factors: Age, gender, ethnicity (Native and African Americans), family Hx, Genetics. Modifiable RF: Elevated serum lipids > 200 and triglyceride> 350., HTN, Smoking, inactivity, Obesity, DM, High stress, Metabolic syndrome, and Homocysteine level. Stable angina (fixed stenosis) - Chest pain or discomfort associated with physical activity. - R/t plaque accumulation - Predictable - Alleviated with rest/meds. Unstable angina (thrombus) - Chest pain at rest - Initial phase of Acute coronary syndrome (ACS) - Decrease in myocardial blood flow. - Precursor to MI - Emergency - ECG changes Prinzmetal’s, or variant, angina (vasospasm) - Coronary spasm - Occurs at rest and in clusters. - Usually at nighttime between midnight and 8 a.m. - Tx is a calcium channel blocker to prevent spasms. S/S radiation of pain to the left arm, back, neck, and jaw. SOB, fatigue, nausea, vomiting, diaphoresis, weakness, syncope, and epigastric, discomfort. Labs - Total cholesterol, triglyceride levels, LDL, high-density lipoprotein (HDL) - Cardiac-specific biomarkers: Creatine kinase (CK), creatine kinase–muscle/brain (CKMB), troponin (I or T) Electrocardiogram (ECG) - Initial test - ST-segment depression > 0.5 mm, flat T waves, inverted T waves: Ischemia Exercise stress test. - Assess heart function during exercise. Coronary angiography - Gold standard - Left-side catheterization to evaluate the coronary arteries for blockage. - Evaluate coronaries for blockage. - Medications aimed at MONA – pts with stable angina are treated with aspirin, nitro, antihypertensives, and antidiabetic agents. (a) stopping the aggregation of blood components to the injured endothelium - Aspirin – low dose daily to inhibit platelet aggregation and reduce risk of MI. - Plavix (b) controlling factors that led to damage to the endothelium - Calcium channel blockers - Statins - Beta-blockers (c) relieving symptoms and vasodilators - Nitro–patch, sublingual, topical, spray - Morphine - TABLE 30.2 MEDS Percutaneous transluminal coronary angioplasty (PTCA) - The most common and preferred procedure - The balloon and stent open the affected artery. FIGURE 30.3 Stent placement within the artery. Step 1: A catheter with a small balloon on its tip is advanced to the area with atherosclerotic plaque. Step 2: The balloon is inflated and deflated to open the lumen of the artery. Step 3: The stent is advanced to hold the artery open and maintain adequate blood flow. Coronary artery bypass grafting (CABG) more invasive surgical treatment - Open heart surgery - Coronary artery is bypassed from an artery in the chest, arm, or leg. Medical management-Lifestyle management. Maintain healthy body weight. Diet Physical activity Smoking cessation Screening and treatment for depression Refraining from excessive alcohol use. Cardiac rehabilitation Complications Myocardial Infraction Dysrhythmias Heart Failure. Nonspecific symptoms: Epigastric discomfort Nausea and vomiting Diaphoresis Syncope Shortness of breath (SOB) Pain between shoulders/jawline Decreased tissue perfusion related to inadequate blood flow secondary to the presence of plaque within the coronary arteries or microvascular dysfunction Vital signs – Tachycardia and tachypnea r/t cardiac ischemia Hypertension is a CAD risk factor Hypotension r/t nitro and morphine Pain assessment - pqrst Provoking factors Quality, region, radiation, severity, time Headache r/t nitro Electrocardiogram and continuous cardiac monitoring – ST depression, inverted T waves r/t ischemia ST elevation r/t acute injury Dysrhythmias r/t ischemia or infarction Non-ST elevated MI – T wave inversion, w/out Q wave, elevated cardiac marker, and depressed ST Physical assessment – Pallor, clamminess, nausea, vomiting, shortness of breath, diaphoresis r/t decreased perfusion Patient history – CAD risk factors Angina patterns Nondescript symptoms (e.g. nausea) Recreational drug use – It can cause vasospasm. Depression screening – Depression is common; it may increase morbidity and mortality. Laboratory values • Cardiac biomarkers: troponin, CK/CK-MB – Cardiac enzymes and troponin levels rise when the heart sustains an acute injury—can help differentiate between angina and MI pain. • Creatinine, blood urea nitrogen – Assess renal function. The contrast dye used during heart catheterization is nephrotoxic. • Glycosylated hemoglobin (HgbA1c) – Hyperglycemia occurs with diabetes and is a risk factor for CAD. • Lipid profiles: cholesterol, triglycerides, LDL, HDL – Assess for hyperlipidemia, a risk factor for CAD development. Nursing Interventions Action Administer oxygen to keep oxygen saturation greater than 93% – Supplemental oxygen optimizes oxygen delivery to the myocardium. Cardiac dysrhythmias, especially tachycardia, and anxiety increase myocardial oxygen consumption. Obtain ECG with the occurrence of chest pain – Evaluate new anginal episode for evidence of ischemia or injury. In cases of acute chest pain, an ECG within 10 minutes is THE GOLD STANDARD Administer nitroglycerin as ordered – Dilates the coronary arteries to improve flow to the heart and relieve pain. Administer aspirin as ordered – Prevents platelet aggregation. Administer morphine as ordered if nitroglycerin does not relieve pain – Minimizes pain and decreases the workload on the heart. Monitor for adverse effects of hypotension, nausea, vomiting, and respiratory depression. Administer beta blockers/calcium channel blockers as ordered – Inhibit cardiac response to physical activity, decrease oxygen consumption; may consider holding before exercise test. Administer statin medications as ordered – Reduce cholesterol level and decrease the risk of increased plaque formation. Nursing interventions – Actions after PCI Perform cardiac catheterization care. Report and treat chest pain immediately – Reclusions, vasospasm, or stenosis can result in ischemia and require prompt intervention. Administer additional anticoagulants – Prevents vessel occlusion by thrombus. Maintain fluids through catheterization sheaths if left in place – Allows for immediate coronary access if return to catheterization lab is needed. Maintaining bedrest and compression devices at the catheter insertion site – Promotes hemostasis and prevents bleeding. NI – Teaching Medication regimen – Medication adherence lowers mortality and the risk of hospitalization and MI. Angina management – If angina occurs during activity, stop the activity and rest. Take a dose of nitroglycerin. Tabs can cause tingling or taste bitter when placed under the tongue. Not to exceed three doses 5 minutes apart. Caution patient about the use of the medication in the setting of light-headedness or dizziness because this can be indicative of hypotension. Bleeding precautions if on anticoagulants – Avoiding activities that have a high injury or fall risk, using a soft toothbrush and electric razor, and using caution with sharp objects reduce bleeding risk. Risk factor reduction strategies: physical activity, blood pressure management, healthy diet/weight loss, smoking cessation, decreased alcohol consumption, control of glucose – Risk factor reduction can prevent primary disease and limit the progression of CAD. When to call providers or emergency services – Unrelieved chest pain—chest pain at rest requires early intervention. For PCI patients: uncontrolled bleeding, swelling, redness, purulent discharge, and pain at insertion site or fever need prompt treatment. Encourage participation in cardiac rehabilitation for ACS patients after PCI or CABG. Reduces morbidity and mortality. Infective Endocarditis Infective Endocarditis – damage or endothelium of the inner lining of the heart and its valves. The Tricuspid and Mitral are at risk for infection. Risk Factors: IV drug abusers, DM, Prosthetic heart valves, Systemic infections, Structural Cardiac defects, and imported Cath. Symptoms: strokes, heart failure, and dysrhythmias. Assessment cues: Murmur, HF, Osler’s nodes, Janeway lesions, Neurological changes, Petechiae, splinter hemorrhages, fever. Diagnosis Assessment: Positive blood cultures, New regurgitant murmur, evidence of endocardial involvement by echocardiography, elevated WBC. Medical management medications: IV antibiotic therapy. Non-surgical: Antimicrobials, activities balanced with adequate rest. Surgical management: repair or replacement of the valves. Nursing Management Interventions (VS/ Actions/ Diagnosis) Infection-related to an invading organism secondary to IE Ineffective tissue perfusion related to emboli. Decreased cardiac output related to valve dysfunction, altered rhythm, and/or altered stroke volume Vital signs – Fever is indicative of ongoing acute infection. Hypotension, tachycardia, tachypnea, and low SpO2 can be signs of sepsis or heart failure. Auscultate breath sounds. Crackles may be a sign of heart failure related to valve dysfunction. Auscultate heart sounds. A new or worsening murmur may occur due to valve damage. Assess neurological function. Neurological changes or deficits in pupils, grips, foot pushes, facial droop, and speech may be signs of CNS embolization. Assess extremities. Cyanosis or pallor, delayed capillary refill, and decreased peripheral pulses may indicate peripheral embolization. Edema could be a sign of heart failure related to valve dysfunction. Skin assessment – Osler’s nodes, Janeway lesions, and splinter hemorrhages are indicative of IE. Monitor diagnostic test results. Repeated culture reports are used to evaluate the effective treatment of IE. White blood cell (WBC) counts can indicate responsiveness to infection. Echocardiograms can evaluate the size of vegetation and valve function and can be used to predict the risk of complications. History of drug use, invasive procedures, implanted vascular or cardiac devices, or valve replacement surgery Administer antibiotics as prescribed – Treatment for IE is long-term IV antibiotic treatment. Maintain IV access for antibiotic administrations – Intravenous access is essential for antibiotic administration. Long-term venous access, such as a peripherally inserted central catheter (PICC), may be considered. Administer heart failure medications as needed – Heart failure treatment optimizes cardiac output and tissue perfusion. Provide social support during prolonged hospitalization – Social isolation due to hospitalization may contribute to depression, anxiety, and anger. Refer patient to addiction counseling services if drug use has caused the disease – Stopping recreational IV drug use may help limit the recurrence of IE and lead to a better quality of life. Myocarditis – Inflammation of the myocardium Men and young persons are the most affected. The third leading cause of cardiac death in young athletes. COVID-19 and the vaccines are possible causes. The AHA says…An international study published in April 2022 found about 3 in every 1,000 patients hospitalized due to a COVID-19 infection developed acute myocarditis. The study used data from the first 15 months of the pandemic before COVID-19 vaccines were widely available. Among those hospitalized for COVID-19 and diagnosed with myocarditis, those who also developed pneumonia were more likely to need a ventilator to breathe and had an increased risk of death. Myocarditis was reported at a higher rate than expected among some people who received the Pfizer or Moderna vaccines, according to a July 2021 study. Most of the suspected myocarditis cases in that study developed after the second dose and were among males between 12 and 39 years old. Despite these cases, the study stated that the benefits of the COVID-19 vaccine outweigh the rare risk of myocarditis (AHA). Clinical Manifestations: HF, Cardiogenic shock, chest pain, dysrhythmia, dyspnea, palpitations, syncope. Complications: Labs, Echocardiogram, MRI, and Myocardial biopsy. Treatment is dependent on clinical manifestations/complications. It is focused on managing complications, such as heart failure, dysrhythmias, and sudden cardiac death, and involves medications geared toward managing these individual problems—there is no definitive treatment specifically for myocarditis. Sudden cardiac death especially common in young athletes Vital signs – Hypotension, hypertension, tachycardia, tachypnea, and hypoxia are signs of heart failure. Fever is indicative of infection. Cardiac rhythm – Dysrhythmias are a common and dangerous clinical manifestation and must be identified and treated promptly. Assess for crackles, edema, jugular vein distention (JVD), weight gain, and decreased urine output. These are evidence of the weakened heart muscle seen with heart failure. Administer antivirals, antimicrobials, immunosuppressives, and immunoglobulins as ordered – Medications are administered depending on the cause of myocarditis. Administer heart failure medications as needed – Heart failure is a common manifestation and must be treated to optimize cardiac output and tissue perfusion. Provide emotional support – The diagnosis of myocarditis can cause fear and anxiety. Complete the full medication treatment regimen – Patients should continue to take medications as directed even if feeling better to ensure an effective/positive result. Avoid strenuous activities – Athletes should not participate in competitive sports while inflammation is present and need to be reevaluated in no less than 3 to 6 months before resuming sport. Activity restrictions may reduce the risk of sudden cardiac death. Pericarditis - Inflammation of the pericardium. Just pericarditis can be very benign and self-limiting, though very painful, however, depending on the cause… Pericarditis can lead to pericardial effusion—fluid accumulation within the pericardial sac, which can build up and cause cardiac tamponade (severe restriction of the heart muscle) and severely reduced cardiac output. Pleuritic chest pain 85% to 90% of cases Relieved by sitting up and leaning forward (different from MI) Friction rubs 30% of cases New or worsening pericardial effusion 60% of cases ECG changes: diffuse ST-segment elevations or PR depression 60% of cases Fever Cardiomegaly ECG and cardiac markers to r/o MI Cardiac tamponade – life-threatening emergency (PEA arrest) because of pericardial effusion Chest pain related to swelling and inflammation secondary to pericarditis. Risk for decreased cardiac output related to cardiac structure compression. Valvular Disease First: Murmur is “Lub” Then, they resemble those of HF due to decreased cardiac output. SOB, dyspnea, orthopnea. Crackles Angina Syncope, dizziness Dysrhythmias Palpitations Fatigue Weight gain Edema Cool, pale extremities with weak pulses Diagnostic tests used to diagnose valvular disease include: Echocardiogram to identify valve abnormalities and ejection fraction Chest x-ray to identify left or right heart hypertrophy and pulmonary edema Stress testing to identify functional capacity Heart catheterization as a definitive test for stenosis done before corrective surgery CT or MRI Angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), or angiotensin receptor–neurolysin inhibitors (ARNIs) with beta-blockers - Reduce heart rate and blood pressure. Diuretics to decrease preload and pulmonary congestion. Valve repair has better outcomes than replacement. Vital signs – Hypertension, tachycardia, and tachypnea are indicative of HF due to increased resistance to flow and backflow of blood to the pulmonary system. Tachycardia occurs as a compensatory mechanism to increase cardiac output and oxygenation. Fever is indicative of infection and increases metabolic demands. Decreased SpO2 occurs with pulmonary congestion. Pain assessment – Chest pain and palpitations may occur with some murmurs. Monitoring for irregular heart rhythm – Dysrhythmias, specifically atrial fibrillation, are common in valve disease. Peripheral vascular assessment – Poor color, cool extremities, weak peripheral pulses, delayed capillary refill, and edema can indicate inadequate cardiac output. Breath sounds – Crackles and orthopnea indicate pulmonary congestion. Activity tolerance – Dyspnea on exertion, weakness, and fatigue indicate worsening HF. Auscultate heart sounds. Murmurs are typically the initial manifestation of valvular disease. Daily weights, intake, and output – Weight increases and intake greater than output can indicate HF. Monitor international normalized ratio (INR). Patients with valve replacements on warfarin need to maintain an INR that is two to three times normal. Provide supplemental oxygen and elevate the head of the bed – Oxygen and positioning increase oxygenation and ventilation. Administer medications as ordered. Restrict sodium and fluids – To decrease fluid overload and reduce HF symptoms. Medication teaching – Understanding and adhering to the medication treatment plan are essential for effective medication treatment. Consider prophylactic antimicrobials for dental procedures only for patients at high risk – Prevent (re)occurrence of infectious valvular disease. Strict adherence to anticoagulation regimen if prosthetic valve – Prevent thrombotic/embolic events (i.e., stroke) Anticoagulation precautions: avoid activities/sports that have a high risk for injury, report any injuries or falls to your provider, report anticoagulant use before any procedure, take care with shaving (electric razor preferred), take care with flossing to avoid bleeding, and limit alcohol consumption – Avoid activities/actions that increase bleeding risk. Maintain consistent intake of green leafy vegetables if taking warfarin – Green leafy vegetables impair the effectiveness of the anticoagulant warfarin. Immunizations: Patients at higher risk of infections. Heart Failure (4 stages): it is a progressive disease characterized by myocardial cell dysfunction – the inability of the heart to pump effectively. It can be left-sided or right-sided. The contractility of the myocardial muscle is not working effectively. HF starts with the left side and then moves to the right. Left-sided HF: the weak contraction results in poor peripheral perfusion that leads to backflow into the lungs. S/S are SOB, crackles, pale color, weak pulses, cool temperature in extremities, delayed cap refills, and fatigue. Right-sided HF: back up into the right atrium and venous circulation. S/S are JVD distention, Dependent edema (swollen ankles), ascites, and hepatomegaly. Lifestyle, lifestyle, lifestyle!! Though there are some hereditary associations Risk Factors: CAD, Hypertension, Diabetes mellitus, Metabolic syndrome, Obesity, Smoking, High sodium dietary intake, Sleep apnea. Other factors are: - Valvular dysfunction - Cardiomyopathies - Infectious/inflammatory heart disorders - Dysrhythmias - Cardiotoxic substances Dx – physical assessment. Chest x-ray – Assess heart structure. Echocardiogram- Visualize chambers and valves, and measure EF. ECG – Identify dysrhythmias. Picks up the electrical flow and the heart can shift. Cardiac biomarkers – r/o MI, pro-BNP diagnostic for HF. Serum electrolytes – Renal impairment, diuretic therapy H&H – Decreased erythropoietin leads to anemia. Tx – HF Ejection Fraction (65% – 70 %) Treatment of the underlying cause Blood pressure control Diuretics for fluid volume overload Symptom management Reduction of risk factors Manipulation of the critical components of cardiac output (preload, afterload, and contractility) Control of the compensatory mechanisms Blood pressure and glucose control, weight loss, optimizing serum lipids, smoking cessation. Beta-blockers - Control SNS compensatory response. - Decrease cardiac workload. Aldosterone antagonist diuretics, loop diuretics - Decrease preload. - Watch renal function and electrolytes. ACE inhibitors, vasodilators - Reduce afterload. Digoxin (inotropic) - Improve contractility. Automatic internal cardiac defibrillator (ICD) and a pacemaker - Dysrhythmia control and ventricular resynchronization (CRT) VAD - Mechanical circulatory support acts like the heart. Symptom monitoring - Daily weights are taken at about the same time. Medication adherence Lifestyle - Restrict sodium. About 1500 mg/day - Maintain weight. Weight gain indicates fluid retention. 1kg in a day or 2ky in a week may be significant. - Nutrition The clinical manifestations of HF are due to weakened myocardial contraction resulting in decreased cardiac output, a backup of blood, and poor peripheral perfusion. Common findings include: Poor mentation Anorexia Exercise intolerance. SOB, orthopnea JVD Dependent peripheral edema Weak peripheral pulses, cool extremities, delayed capillary refill Cardiac cachexia or generalized body wasting Renal Failure happens as a result is damage to the kidneys. Impaired oxygenation related to the accumulation of fluid in the lungs secondary to HF Decreased cardiac output related to altered preload, afterload, and contractility Ineffective peripheral perfusion related to decreased cardiac output secondary to HF Vital signs – Hypertension is present because of the increased afterload. Hypotension may be caused by acute heart failure or be an adverse effect of medications. Tachycardia can be present as the heart attempts to compensate for decreased cardiac output. Tachypnea and decreased oxygen saturation may be present when fluid accumulates in the lungs because of left-sided HF. Breath sounds – Crackles indicate pulmonary congestion. Monitoring for irregular heart rhythm or dysrhythmias. Dysrhythmias are a common adverse effect of HF and medications used to treat HF. Skin color, temperature, peripheral pulses, and capillary refill time Pale or cyanotic color, cool extremities, weak peripheral pulses, and sluggish refill time result from inadequate cardiac output. Dry, persistent cough – Common complication of ACE inhibitors Activity tolerance – Dyspnea on exertion, weakness, and fatigue indicate decreased cardiac output and worsening heart failure. Urine output – Output may be reduced with decreased renal perfusion and also can be used to assess the effectiveness of diuretic therapy. Less than 30 mL/hr should be reported to the provider. Daily weight – same scale, same clothing with each weighing of pt. To evaluate fluid retention and the effectiveness of diuresis Laboratory data – Elevated BNP and NT-proBNP indicate overstretching of heart tissue. Elevated creatinine and BUN may be indicative of prerenal failure due to decreased cardiac output or over-diuresis. Elevated hepatic enzymes can be indicative of hepatomegaly; hypokalemia is a common complication of diuretic administration. Anemia can be caused by reduced kidney perfusion. Depression screening and mood – High rates of depression and anxiety are noted in the HF population. These can impact self-management. Social support – Social isolation is an independent predictor of mortality among HF patients. Nursing Intervention (Action and Teaching) Oxygen therapy – To maintain adequate oxygenation Elevate the head of the bed and provide a fan for dyspnea – Maximize oxygenation and promote comfort Medication administration as ordered: • Administer diuretics – Diuretics decrease volume, thus preload. Hydrochlorothiazide, Furosemide, • Administer ACE inhibitors, ARBs, ARNIs, and vasodilators – Angiotensin-converting enzyme inhibitors, ARBs, ARNIs, and vasodilators decrease afterload, which helps to decrease the workload on the heart and decrease myocardial oxygen consumption. Lisinopril, • Administer beta blockers – Beta blockers decrease the sympathetic response (decreases heart rate so the heart can fill), thus reducing myocardial oxygen consumption--Metoprolol • Administer positive inotropic agents – Enhance contractility--Digoxin Fluid and sodium restriction – To prevent fluid overload. Teaching Medication management – Understanding and adhering to the medication treatment plan are essential for effective medication treatment. Maintain activity as tolerated. Alternate rest and activity periods – To reduce muscle wasting and functional losses; to decrease workload on the heart. Low-salt diet – cardiac diet. To prevent fluid retention and exacerbation of HF. Daily weight at home at the same time each day, preferably in the morning after voiding – Evaluate fluid retention and call the provider. Cardiac rehabilitation – Cardiac rehabilitation reduces mortality, improves functional status, reduces hospitalization, and improves quality of life. Signs and symptoms of worsening HF checklist (edema, SOB, fatigue, and orthopnea) – Knowing the symptoms can expedite treatment and reduce hospitalizations. Myocardial Infraction Blockage in the blood vessels to the heart. Risk factors: elevated catecholamines, smoking, diabetes, lack of sleep, and obesity. What is a “silent MI” and what patient populations are at the greatest risk of having them? Patho… The most common cause is atherosclerosis. Plaque in artery > rupture of plaque > thrombus formation > obstruction of blood flow FIGURE 32.8 Acute coronary syndrome: unstable angina, non-ST elevation myocardial infarction, and ST elevation myocardial infarction. Not all MIs present as chest pain, diaphoresis, and SOB. Some patient populations present with more obscure s/sx, such as… Jaw and tooth pain, shoulder blade pain, upper back pain, shortness of breath, nausea and vomiting, sweating, syncope, confusion, arm pain, and generalized fatigue Females – heartburn, fatigue, neck and jaw pain, nausea and vomiting, and abdominal pain. Adults – syncope, dyspnea, weakness, confusion. Dx: Labs Troponin—the gold standard, creatine kinase (CK), CK-MBEKG, TIMELY, is critical. End-organ compromise – CMP, CBC, coagulation studies, and ABG. EKG - ST-segment depression or elevation. A pathological Q-wave indicates damage. Medical Management: Goal: Increase blood flow to cardiac tissue, or reperfusion therapy. O2 – All patients receive this. Nitro – Dilates coronary arteries and venous system, increases cerebral blood flow and controls pain. Pt can become allergic to nitro, so it is important to have IV access. Aspirin – Anti-platelet to prevent clots from growing. Morphine – Pain control, also dilates coronary arteries and venous system, but may mask change in condition. “MONA” (but not in that order) You may also see providers order calcium channel blockers, especially if Morphine and or Nitro are contra-indicated, as they also help dilate vessels and reduce workload and O2 consumption of the heart, which helps reduce pain. Definitive Treatment: Three basic approaches PCI Gold Standard within 30 mins. Fibrinolytic within 6 hours; mortality 38% vs 70% without revascularization CABG—often used for multiple-vessel disease. PCI – Interventional Cath lab with stent deployment to open coronary vessel and revascularize tissue distal to clot Fibrinolytic – Used if PCI is not available. Surgical infarction – Revascularization intervention that bypasses blockages in the coronary arteries causing the myocardial muscle damage. Complications, assessment, and diagnoses. Decreased heart function r/t myocardial tissue death. Asystole, symptomatic bradycardia, heart block, and ventricular arrhythmias; may need a temp pacemaker. Decreased CO related to poor cardiac contractility secondary to MI Pain related to inadequate blood supply by the heart. Nursing Intervention – assessments-initial and ongoing Vital signs and pulse oximetry — Tachycardia with a borderline low BP and decreased oxygen saturation is a sign of inadequate CO and oxygen delivery. Assess characteristics of pain including location, radiation, duration, intensity, precipitating or alleviating factors; use a 1 to 10 pain scale — Chest pain is an indication of MI. Continued or changing pain characteristics can be indicative of a worsening condition. Remember the OPQRST mnemonic! Onset—What time did this pain start? Provokes/Palliates—what provokes the pain or makes it better? Quality—have the pt describe the pain—is it dull, aching, piercing, throbbing, burning, etc.? Radiation—Does it radiate or travel? Severity—Scale of 0-10 Time—does it come and go, or is it constant? Assess ECG changes — ST-segment depression is indicative of ischemia. ST-segment elevation is indicative of injury. If present, a Q wave is diagnostic for MI. Assess for restlessness — Restlessness may be found in the early stages, but progression to severe anxiety and a sense of doom is a late-stage symptom. Assess skin color and temperature, peripheral pulses, and diaphoresis — Decreased pulses and cold, clammy, pale skin are signs of inadequate tissue perfusion and inadequate CO. Activation of the sympathetic system with low CO will stimulate diaphoresis. Monitor urine output — Decreased or absent urine output is a sign of decreased renal perfusion related to decreased CO. What is the minimum UO for adults? ML/HR? Assess troponin and CK, CK/MB levels — Troponin (Gold Standard) is a protein released from damaged cardiac muscle. It elevates within 4 hours and can stay elevated for days. CK/MB, the CK isoenzyme marker specific to cardiac tissue, is released from the cells with cardiac muscle damage. Increased levels can be seen at 3 hours and remain elevated for as long as 36 hours. Post-CABG Monitor heart rate and BP continuously with an arterial catheter at least every 15 minutes initially and then every 4 hours when the patient is stable — Tachycardia, bradycardia, hypotension, and hypertension may be signs of decreased cardiac output or compensatory mechanisms. Hemodynamic monitoring — Decreased preload (CVP, PAOP), SvO2 may indicate a decreased cardiac output leading to poor tissue perfusion Continuous cardiac monitoring — Dysrhythmias are common after CABG. Assess heart tones — Muffled heart tones may indicate tamponade. S3, S4, and crackles may indicate heart failure. Monitor breath sounds and continuous oxygen saturation monitoring — Decreasing saturation may indicate pulmonary complications. Diminished or unilateral absent breath sounds may indicate atelectasis, pleural effusions, or pneumothorax. Monitor core temperature hourly — Hypothermia during surgery reduces metabolic rate and risk of organ ischemia. Rewarming may produce hypotension from vasodilation. Core temperatures are the most reliable. Assess the level of consciousness, pupils, and responsiveness — Assesses effectiveness of sedation and evaluates neurological function. Hourly intake and output. Notify the provider for output less than 30 ml/hr for 2 hours — Decreased urine output may be a sign of renal damage or decreased cardiac output. Assess skin color and temperature, pulses, edema, and capillary refill — Pale, cool skin with delayed capillary refill and weak pulses may indicate decreased cardiac output. Edema can be an expected response after CABG due to fluid resuscitation during surgery. Monitor chest tube output, color, and volume hourly — Sudden increases in output greater than 100 to 200 ml not associated with position changes or increased bright red drainage may indicate hemorrhage and the need to return to the operating room. Assess hemoglobin, hematocrit, electrolytes, creatinine blood urea nitrogen, and glucose — Changes may indicate bleeding, fluid shifts, and renal dysfunction. Tight glucose control is associated with improved outcomes. Assess incisions for drainage, warmth, redness, and swelling — Redness, warmth, swelling, and purulent drainage may indicate infection. Nursing Intervention/Teaching/Outcomes Administer oxygen — Oxygen consumption and demand increase; therefore, oxygen supply should be increased. Insert two large-bore IVs — IV access is essential for medication delivery and fluid resuscitation. Administer medications as ordered — Medications are essential to be given promptly: • Aspirin and heparin — Aspirin and heparin are given to prevent new clot formation. • Nitroglycerin SL — Nitroglycerin dilates the coronary arteries, increasing blood flow and decreasing pain. • Morphine — Morphine is a narcotic given for pain relief if nitroglycerin is not effective. • Beta blockers — Beta blockers decrease the sympathetic response to an MI, decreasing cardiac workload and oxygen consumption. • Fibrinolytics — Fibrinolytics work to dissolve clots. Continuous ECG monitoring — Electrocardiogram monitoring is essential to evaluate the evolution of MI and the effectiveness of treatment and to monitor for dangerous dysrhythmias that can occur. Bed rest — The patient may require bed rest as well as emotional rest to decrease oxygen and cardiac demands Maintain tight BP control — Hypotension may result in graft collapse; hypertension may result in bleeding. Administer fluids and medications (vasodilators, vasoconstrictors, inotropes, and diuretics) as ordered — Maintains hemodynamic stability Rewarm the patient slowly with warm fluids, blankets, or air flow devices. Prevent shivering — Rapid rewarming may cause dysrhythmias and/or hypotension due to vasodilation. Shivering increases oxygen needs. Administer pain medication and continuous sedation medications — Maintains effective sedation and analgesia to decrease anxiety and pain which may potentially increase cardiac workload. Pulmonary hygiene while intubated: Reposition frequently, suction as needed. Oral care every 4 hours. Pulmonary hygiene after extubation; Incentive spirometry (IS), cough, and deep breathing (C&DB) every 1 to 2 hours while awake, encourage chest splinting when coughing — Helps with weaning toward extubation, oral care helps prevent ventilator-associated pneumonia, IS and C&BD reduce the risk of hospital-acquired pneumonia, and improves oxygenation. Plan for and initiate early mobility or ambulation — Reduces complications related to immobility: deep venous thrombosis, pneumonia, constipation, skin breakdown Wound care: Initial dressing to be removed or changed by provider, then change daily or as needed — Helps prevent wound infection and promotes healing Nursing Teaching Immediately report signs and symptoms of MI such as chest pain chest discomfort or increased shortness of breath — Understanding of the signs and symptoms of MI allows the patient to have earlier intervention, thus decreasing the complications and severity of present or future MIs. Purpose, dose, and side effects of medications — Prescribed medications are to treat the effects of MI and prevent future MIs. The American Heart Association “Life’s Simple 7”: 1. No smoking of cigarettes or other tobacco products 2. Maintain a normal body weight 3. Exercise for at least 150 minutes with moderate-intensity activity, 75 minutes of vigorous-intensity activity, or a combination of each per week 4. Eat a healthy diet that follows the current American Heart Association recommendations. 5. Maintain a total cholesterol level of less than 200 mg/dL 6. Keep BP less than 120/79 mm Hg 7. Keep fasting blood glucose less than 100 mg/dL Signs of infection — Wound infection requires prompt intervention to promote healing. Sternal precautions: do not lift weights over 10 lbs, raise arms overhead, bend at the waist, or participate in vigorous activity until cleared by a physician — These activities may interfere with sternal wound healing. Cardiomyopathy It is a disorder in which the heart muscle becomes weak – genetics, COVID-19. Males > females 2x more in Blacks Measure of function: Ejection fraction (EF) EF is the percentage of blood ejected from the ventricle with each contraction. Normal EF is approximately 55% to 65% < 45% means weakness. <30% means a severe decrease in function. Complications/ Nursing Management – assessment and diagnoses. Heart failure is the inability of the heart to produce enough cardiac output CO to meet the body’s metabolic demands. Problems with filling or contraction Dysrhythmias are a common complication of cardiomyopathy: Atrial fibrillation and more lethal rhythms such as ventricular tachycardia (V-tach) and ventricular fibrillation (V-fib) Thrombosis, or clot formation, is a risk due to the sluggish forward flow of blood leading to stasis. Decreased Cardiac Output related to ineffective cardiac pumping secondary to cardiomyopathy.