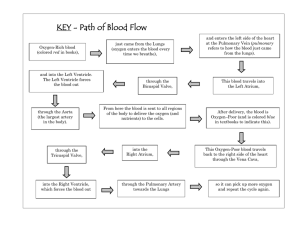
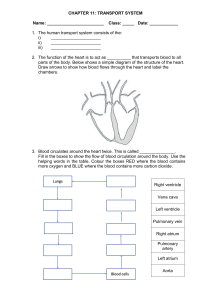
Blood from SVC & IVC Blood from SVC & IVC Blood from SVC & IVC Right Atrium Tricuspid Valve Blood from SVC & IVC Right Atrium Tricuspid Valve Right Ventricle Pulmonary Valve Blood from SVC & IVC Right Atrium Tricuspid Valve Right Ventricle Pulmonary Valve Main Pulmonary Artery, R& L Branch Pulmonary Arteries Blood from SVC & IVC Right Atrium Tricuspid Valve Right Ventricle Pulmonary Valve Main Pulmonary Artery, R& L Branch Pulmonary Arteries Lungs- Gas Exchange Lungs- Gas Exchange Pulmonary Vein Left Atrium Mitral Valve Left Ventricle Lungs- Gas Exchange Pulmonary Vein Left Atrium Mitral Valve Left Ventricle Aortic Valve Ascending Aorta, Descending Aorta 8 in 1000 infants- born with a congenital heart defect 25%- complex 1/3- will require surgical intervention 25%- have other associated congenital anomalies 90%- survive upto adulthood Increasing pulmonary blood flow Decreasing pulmonary blood flow Obstruction to systemic blood flow Left-to-Right Shunt ● Description—Abnormal opening between the atria, allowing blood from the higher pressure left atrium to flow into the lower pressure right atrium L atrial pressure > R atrial pressure • Blood flows from right to left ↑ oxygenated blood into the R side of the heart R ventricle tolerates flow of blood R atrial and ventricle enlargement • (although unusual) If unrepaired: • Pulmonary vascular changes occur after several decades Asymptomatic • if the defect is small • Many small ASDs will close spontaneously in the first few years of life Dysrhythmias • caused by atrial enlargement and stretching of conduction fibers Characteristic Murmur • Typically presents with a systolic ejection murmur, often described as a "flow murmur," due to increased blood flow across the pulmonary valve. • May also have a fixed split S2 (wide splitting of the second heart sound). Rales, congestion, tiring with activity, frequent RTI, or poor weight gain Dilation of the right atrium pulmonary vascular obstructive disease and emboli formation • pulmonary overcirculation, • increased blood volume • chronically increased pulmonary blood flow Asymptomatic Symptomatic • Not indicated for closure • Diuretics- attempted to allow the defect to close spontaneously Non-surgical: Amplatzer Septal Occluder via Cardiac Catheterization Post op- Low-dose aspirin for 6 months Surgical Treatment: Surgical patch closure (pericardial patch or Dacron patch) Description—Abnormal opening between the right and left ventricles Many VSDs (20%–60%) close spontaneously Spontaneous closure is most likely to occur during the first year of life in children having small or moderate defects. • Higher pressure L ventricle • Resistance: Systemic arterial circulation > Pulmonary circulation Left-to-right shunting ↑ pulmonary resistance Hypertrophy • R ventricles • R atrium Left heart dilatation Tachypnea, poor feeding, or failure to thrive • Increase in pulmonary blood flow • increased pulmonary blood flow Application of Dacron Patch with CPB A congenital heart defect characterized by abnormalities in the development of the septum between the atria and ventricles of the heart. In AVSD, septa are either partially or completely absent, resulting in a large opening between the atria and ventricles. ● AVSD is the most common type of CHD in children with trisomy 21 ● AVSD can involve various combinations of defects Left-to-right shunting • pulmonary blood flow increases Heart Failure Complete • with a large septal defect that includes both the atria and the ventricles, and a single atrioventricular valve Transitional • with a small or moderate-sized ventricular septal defect in addition to the atrial septal defect Partial • with an atrial septal defect but no ventricular septal defect, and the common AV valve separated into a right- and a left-sided AV valve Moderate to severe Heart Failure Murmur Mild cyanosis • rapid breathing, shortness of breath while eating, poor weight gain, failure to thrive, and diaphoresis by age 4 to 6 weeks • Loud systolic • Mixing of oxygen rich and oxygen poor blood, Increases with crying Medications • furosemide, digoxin, and an ACE inhibitor like captopril or enalapril Surgical Repair • consists of closing the ASD and VSD and repairing the mitral and tricuspid valves • Children with Down syndrome- less than 3 months of age • Children without Down syndrome – referred for repair by 5 or 6 months Manageent Pulmonary Artery Bands • is a band surgically placed around the pulmonary artery that constricts it to decrease some of the overall pulmonary blood flow and prevent too much pulmonary circulation and long-term pulmonary vascular changes. ● ● Description—Failure of the fetal ductus arteriosus (artery connecting the aorta and pulmonary artery) to close within the first weeks of life. left to right (from aorta to pulmonary artery) ● The ductus arteriosus is a normal connection between the pulmonary artery and aorta; it is necessary for proper fetal circulation. ● Two Mechanisms that Facilitate Closure: ○ the rise in PaO2 ○ decline in prostaglandin concentration left to right (from aorta to pulmonary artery) Murmur • machinery-like murmur, second intercostal space, left upper sternal border, or out to the left clavicular area, rales, congestion, increased WOB, difficulty feeding, or • increased pulmonary circulation failure to thrive Left heart dilation Widened pulse pressure & bounding pulses • blood shunting to the lungs • runoff of blood from the aorta to the pulmonary artery cyclo-oxygenase (COX) inhibitor therapy (eg, indomethacin, ibuprofen lysine) for preterm infants • Given in three separate IV doses Increase Caloric intake- to help the child gain weight Furosemide, Fluid Restriction- manage increased blood flow Transcatheter closure: • the treatment of choice for PDA in children > 1 year IN SUMMARY ● ● ● ● Left-to-right shunt Increasing pulmonary blood flow ↑ pulmonary blood flow ○ Pulmonary edema (dyspnea) ○ Bronchopulmonary infections Heart Failure ○ Periorbital edema, weight gain, oliguria ○ hepatomegaly ● Description—Narrowing or stricture of the aortic valve, causing resistance to blood flow in the left ventricle, decreased cardiac output, left ventricular hypertrophy, and pulmonary vascular congestion Valvular Stenosis • Most common type, is usually caused by malformed cusps that result in a bicuspid rather than tricuspid valve or fusion of the cusps Supravalvular stenosis • occurs infrequently • stenosis occurs when there is narrowing or constriction of the aorta above the level of the aortic valve. Subvalvular stenosis • is a stricture caused by a fibrous ring below a normal valve Aortic Stenosis Left Ventricular Hypertrophy • prominent anatomic consequence Left Ventricular Failure Interferes with with coronary artery perfusion: myocardial infarction Increase in Left Atrial Pressure Pulmonary Vascular Congesti on Infant (critical) Child Systolic ejection murmur • decreased cardiac output with faint pulses, hypotension, tachycardia, and poor feeding • exercise intolerance, chest pain, and dizziness when standing for a long period • may or may not be present. Balloon Angioplasty • Narrowed valve is dilated • The first intervention Norwood procedure • For newborns with critical AS Aortic valve replacement • offers a good treatment option and may lead to normalization of left ventricular size and function ● Description—Narrowing at the entrance to the pulmonary artery. Resistance to blood flow causes right ventricular hypertrophy and decreased pulmonary blood flow. ● ● is the extreme form of PS in that there is total fusion of the commissures and no blood flows to the lungs. The right ventricle may be hypoplastic. Right ventricular Hypertrophy Pulmonary Stenosis •Right ventricular failure Increase Right Atrium Pressure Reopening of Foramen Ovale: shunting of unxygenated blood into the left atrium Right sided HF Asymptomatic • mild narrowing • Loud systolic ejection murmur Cyanosis or HF • At the upper left sternal border Cardiomegaly • Seen in chest radiography Balloon angioplasty • to dilate the valve Obstructive defects • impede blood flow out of the ventricles obstruction on the left side of the heart results in HF severe obstruction on the right side causes cyanosis ● Description—Localized narrowing near the insertion of the ductus arteriosus, which results in increased pressure proximal to the defect (head and upper extremities) and decreased pressure distal to the obstruction (body and lower extremities). proximal to the defect (upper extremities) ↑ pressure distal to the defect (lower extremities)↓ pressure Upper extremities • high blood pressure and bounding pulses in the arms Lower Extremities • weak or absent femoral pulses, and cool lower extremities with lower blood pressure systolic murmur • heard along the left sternal border and the left midscapular area. dizziness, headaches, fainting, • Older children and epistaxis Left ventricular hypertension and hypertrophy • As the narrowing increases the resistance to the left ventricle hypertension ruptured aorta aortic aneurysm stroke ● Description—The tricuspid valve fails to develop; consequently there is no communication from the right atrium to the right ventricle. ● Blood flows through an ASD or a patent foramen ovale to the left side of the heart and through a VSD to the right ventricle and out to the lungs ● There is complete mixing of unoxygenated and oxygenated blood in the left side of the heart, which results in systemic desaturation, and varying amounts of pulmonary obstruction, which causes decreased pulmonary blood flow. Continuous infusion of prostaglandin • For patients who depend on the patency of the ductus arteriosus Blalock-Taussig shunt (pulmonary–to– systemic artery anastomosis) Atrial septostomy Pulmonary artery banding ● Description—The classic form includes four defects: (1) ventricular septal defect (VSD), (2) pulmonic stenosis, (3) overriding aorta, and (4) right ventricular hypertrophy ● The alteration in hemodynamics varies widely, depending primarily on the degree of pulmonary stenosis, but also on the size of the VSD and the pulmonary and systemic resistance to flow. - VSD is usually big - RV pressure = LV pressure - Shunting will depend on: Pulmonary vs systemic vascular resistance Pulmonary vascular resistance > systemic resistance • Right-to-left shunt (RV Aorta) • ↓ Blood Flow to the Lungs Pulmonary vascular resistance < systemic resitance (Unrestricted VSD or Variable Pulmonary Stenosis) • Left-to-right shunt (LV to RV) • ↑ Blood flow to the lungs Cyanosis • progresses over the first year of life as the pulmonary stenosis worsens • Tet speels or blue spells (acute episodes of hypoxia) Murmur • Systolic ejection murmur due to pulmonary stenosis (harsh, crescendo-decrescendo, heard best at the upper left sternal border). May also have a holosystolic murmur from the associated VSD. ● Defects that cause decreased pulmonary blood flow result in cyanosis. Place infant in knee-chest position Employ a calm, comforting approach. Administer 100% oxygen by face mask. Give morphine subcutaneously or through existing intravenous line. Begin intravenous fluid replacement and volume expansion, if needed. •Repeat morphine administration. ● Description—The pulmonary artery leaves the left ventricle, and the aorta exits from the right ventricle, with no communication between the systemic and pulmonary circulations Associated defects such as must be present to permit blood to enter the systemic circulation or the pulmonary circulation for mixing of saturated and desaturated blood. Most common: foramen Ovale VSD increases the risk of heart failure (HF) large septal defects or a • less cyanosis but have symptoms of HF patent ductus arteriosus with minimum communication • Severe Cyanosis Tachypnea Murmur • may not be noted Management Intravenous prostaglandin E1 • At birth to maintain patency of the ductus arteriosus and encourage mixing of blood • SE: apnea ang hypotension (>2kg weight) • infant to remain on room air, spontaneously breathing • Prepare ventillatory support Balloon atrial septostomy • patent foramen ovale (PFO)the opening will be enlarged Jatene procedure • includes cutting both the pulmonary artery and aorta above their respective valves and switching the vessels to the appropriate location. • The final component of the surgical repair is removing the coronary arteries from the base of the original aorta and surgically placing them in an appropriate spot on the new aortic root, now arising from the left ventricle. Kawasaki disease (mucocutaneous lymph node syndrome) is defined as an acute febrile syndrome associated with generalized vasculitis (inflammation of blood vessels) affecting all blood vessels throughout the body, including the coronary arteries -unknown etiology ● ● ● ● ● There is a genetic predisposition Strong suggestion of an infectious precursor Occurs more commonly in winter and spring, with males affected more than females; 76% of children affected are less than 5 years old Diagnosis of exclusion ● ● ● ● ● ● ● Prolonged fever (higher than 100.4°F [39°C]) of 5 or more days Four or more of the following symptoms: Changes in hands and feet (erythema, edema, peeling) Polymorphous exanthema (diffuse maculopapular rash of the trunk and extremities) Bilateral conjunctivitis without exudates Changes in lips and mouth (erythema, strawberry tongue, dry, cracked lips) Cervical lymphadenopathy (larger than 1.5 cm in diameter, usually unilateral) Thrombocytosis leukocytosis, elevated liver enzymes, elevated ESR and CRP mild anemia. Acute Phase • children are very irritable and uncomfortable from the fever and • inflammatory process that causes joint pain Subacute Phase • 10 days after • Skin desquamates, particularly on the palms and soles. • ↑ platelet count: stroke risk • Aneurysm in a coronary artery: ischemia and infarction ● ● IV fluids/ Antipyretics high-dose intravenous immunoglobulin (IVIG) and highdose aspirin therapy ○ a reduction in the appearance of coronary artery irregularities and aneurysms due to their antiinflammatory properties ● One of the most important causes of cardiovascular ● Morbidity and mortality among socially and economically disadvantaged populations worldwide ● Rheumatic fever is an autoimmune disease that occurs as a reaction to a group A beta-hemolytic streptococcal infection, specifically, a pharyngitis. ● Inflammation from the immune response leads to inflammatory lesions in the heart, blood vessels, brain, and joints. ● Occurs as a reaction to a group A beta-hemolytic streptococcal infection (pharyngitis) ● Occurs most often in children 6 to 15 years of age, with a peak incidence at 8 years ● Genetically susceptible individuals ● The sensitized child will eventually have a group A betahemolytic streptococcal pharyngitis that sets off an unusually high antibody response Erythema marginatum Sydenham’s chorea elevated antistreptolysin-O (ASO) titer • recent streptococcal infection ESR and CRP • Inflammatory marker, elevated ECG and CXR • To evaluate the extent of cardiac involvement. • • • • • Intramuscular (IM) or oral penicillin is prescribed for a full 10-day course Oral nonsteroidal anti-inflammatory Phenobarbital and diazepam are both effective in Reducing the purposeless movements of the chorea Cardiologist consult for life