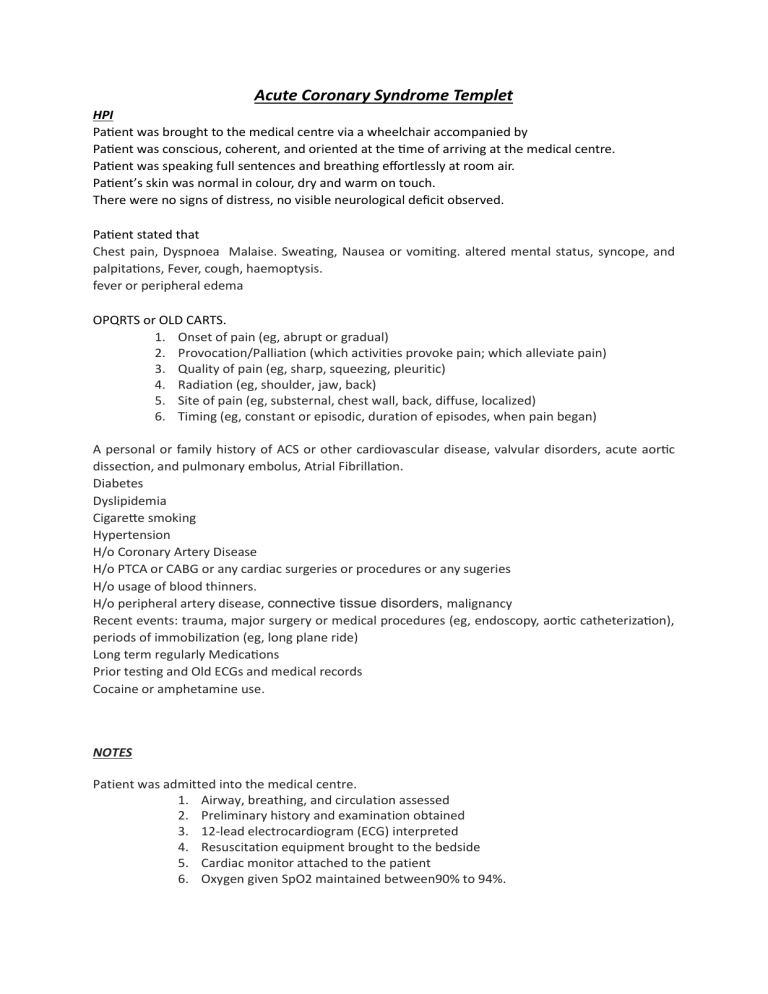
Acute Coronary Syndrome Templet HPI Patient was brought to the medical centre via a wheelchair accompanied by Patient was conscious, coherent, and oriented at the time of arriving at the medical centre. Patient was speaking full sentences and breathing effortlessly at room air. Patient’s skin was normal in colour, dry and warm on touch. There were no signs of distress, no visible neurological deficit observed. Patient stated that Chest pain, Dyspnoea Malaise. Sweating, Nausea or vomiting. altered mental status, syncope, and palpitations, Fever, cough, haemoptysis. fever or peripheral edema OPQRTS or OLD CARTS. 1. Onset of pain (eg, abrupt or gradual) 2. Provocation/Palliation (which activities provoke pain; which alleviate pain) 3. Quality of pain (eg, sharp, squeezing, pleuritic) 4. Radiation (eg, shoulder, jaw, back) 5. Site of pain (eg, substernal, chest wall, back, diffuse, localized) 6. Timing (eg, constant or episodic, duration of episodes, when pain began) A personal or family history of ACS or other cardiovascular disease, valvular disorders, acute aortic dissection, and pulmonary embolus, Atrial Fibrillation. Diabetes Dyslipidemia Cigarette smoking Hypertension H/o Coronary Artery Disease H/o PTCA or CABG or any cardiac surgeries or procedures or any sugeries H/o usage of blood thinners. H/o peripheral artery disease, connective tissue disorders, malignancy Recent events: trauma, major surgery or medical procedures (eg, endoscopy, aortic catheterization), periods of immobilization (eg, long plane ride) Long term regularly Medications Prior testing and Old ECGs and medical records Cocaine or amphetamine use. NOTES Patient was admitted into the medical centre. 1. Airway, breathing, and circulation assessed 2. Preliminary history and examination obtained 3. 12-lead electrocardiogram (ECG) interpreted 4. Resuscitation equipment brought to the bedside 5. Cardiac monitor attached to the patient 6. Oxygen given SpO2 maintained between90% to 94%. 7. Intravenous (IV) access secured and blood investigations- CBC, RFT, Serum Electrolytes, LFT, Cardiac markers, BN, D-dimer and ABG ordered. 8. Aspirin 162 to 325 mg given 9. Metaprolol 25 mg. 10. Nitrates given (contraindications to nitrates include severe aortic stenosis, hypertrophic cardiomyopathy, suspected right ventricular infarct, hypotension, marked bradycardia or tachycardia, and recent use of phosphodiesterase 5 inhibitor [eg, Viagr] were checked and excluded.) 11. Enoxaparin is given1 mg/kg subcutaneously every 12hours. 12. No h/o renal impairment 13. Clopidogrel 300 mg given 14. CXR -PA done. Causes of chest pain that pose an immediate threat to life including •Acute coronary syndrome (ACS) •Acute aortic dissection •Pulmonary embolism •Tension pneumothorax •Pericardial tamponade •Mediastinitis (eg, Esophageal rupture) were considered and rules out with clinical examination and available investigations. Evaluation for life-threatening conditions Shock Heart failure Aortic dissection Coagulopathy and/or thrombocytopenia Risk Stratification Use MDCal for HEART score. https://www.mdcalc.com/calc/1752/heart-score-major-cardiac-events.