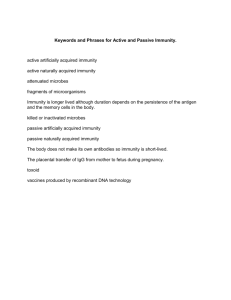
IMMUNITY The word immunity is derived from Latin word “Immunis”, means exempt. “It is the natural and acquired resistance of the body to certain disease and pathogenic microorganisms” Lines of Defenses I. II. III. First line of defense Second line of defense Third line of defense I. First line of defense This line of defense is provided by certain mechanical and chemical barriers. The mechanical barriers include skin and mucous membranes. The chemical barriers include the acidity of stomach and vagina, lysozymes also known as muramidase (rich in saliva, tears, and human milk), interferon (proteins) and complement proteins. Page 1 of 9 II. Second line of defense Once the microorganisms succeed in passing first line of defense and enter the deeper tissues, they are then attacked by the specific cells of body which may ingest them and destroy them. These cells are called phagocytes and form the second line of defense. These include cells such as Mast cells, basophils, eosinophils and phagocytes: neutrophils, macrophages, and dendritic cells. III. Third line of defense: it is provided by the antibodies and the T -cells (T helper and Cytotoxic T cells). Antibodies are produced by B-lymphocytes. Types of Immunity: 1. Natural/Non-specific Immunity: It is the natural resistance of body against the infections of a number of mechanical and chemical stimulus. It is called as non-specific because it exists in all humans and present from the earliest time of life. Lack of such type of immunity is knowns as susceptibility. 2. Acquired Immunity: It is an acquired resistance of body against infection. It involves the action of anti-bodies and immuno-competent cells (helper T cells and cytotoxic T-cells) as a result of stimulation by foreign particle known as antigen. It is specific and provide specific resistance. It is of two types I. Acquired Active immunity II. Acquired Passive immunity I. Acquired Active immunity: It is produced by introduction of antigenic substances from outside to stimulate the activation of T and B lymphocytes and antibody production. Acquired active immunity is further of two types: a) Naturally acquired active immunity b) Artificially acquired active immunity a) Naturally acquired active immunity It occurs when exposure to antigen is unintentional. It often follows the diseases like mumps, polio etc. b) Artificially acquired active immunity (Induced active immunity) It occurs when exposure to antigen is intentional. It is often followed by an immune response (antibody formation). For example, vaccines and toxoids produce such type of response. II. Acquired Passive immunity It is provided by injecting pre-formed antibodies from external to the body. It is further of two types: a) Naturally acquired passive immunity Also called Maternal immunity or Congenital immunity. It occurs when antibodies pass into fetal circulations from mother through placenta or milk unintentionally. E.g., IgA from milk and IgG thru placenta. b) Artificially acquired passive immunity (Induced passive immunity) It develops from the intentional injection of antibody rich serum into the circulation. Page 2 of 9 Example: Rabies anti-serum, Diphtheria anti-toxins Innate Immunity (Natural /Non-Specific Immunity) Innate defenses can be categorized into 3 major categories. 1) Physical & Chemical Barrier: Such as intact skin and mucous 2) Cell of innate immunity: Such as neutrophils, macrophages and natural killer cell 3) Proteins: Such as complement proteins, lysozymes, interferon. Intact skin and mucous membrane: ⮚ Intact skin is the first line of defense. In addition to the physical barrier present on skin the fatty acid (oleic acid) secreted by sebaceous glands have antibacterial and antifungal activity. The low pH of skin i.e., 3-5 is due to these fatty acids. ⮚ Keratin is first barrier. Keratin is undigested by microorganism, so they cannot cross. ⮚ A second most important defense is mucous membrane of respiratory tract, which is lined with cilia and covered with mucous (thread like projections called cilia). The apparatus is called “muco-ciliary apparatus”. The coordinating beating of cilia derives the mucous up to nose and mouth where the trapped bacteria can be expelled. This muco-ciliary apparatus or ciliary escalator can be damaged by alcohol, smoking and viruses. ⮚ Other protective mechanisms of respiratory tract involve alveolar macrophages, lysozymes, mucous, hair in the nose and cough reflex which prevent aspiration into the lungs. ⮚ The non-specific protections in the GIT includes hydrolytic enzymes in the saliva, enzymes in the stomach and various degradative enzymes and macrophages in the small intestine. The vagina of adult human is protective due to low pH (3.8-4.5) generated by Lactobacilli which is a part of normal flora. Cells of innate immunity 1) Phagocytes (i) neutrophils (ii) macrophages Page 3 of 9 (iii) dendritic cells 2) Natural Killer Cells (NK Cells) 3) Mast Cells and Basophils 4) Eosinophils 1) Phagocytes i) Neutrophils: Neutrophils are the most abundant type of WBCs and form an essential part of immune system. Neutrophils are 62% of total WBCs. They are formed from stem cells in the bone marrow. Neutrophils are the types of phagocytosis that are normally found in blood stream. During the acute phase of inflammation particularly as a result of bacterial infection, neutrophils are one of the first responders of inflammatory cells to migrate towards the site of inflammation. Neutrophils are mature cells that can attack and destroy bacteria and virus even in the circulating blood. ii) Macrophages: Monocytes are called immature cells because they have very little ability to fight infectious agent. Monocytes enter in the tissue and change into macrophages which are capable of combating diseased agents. The macrophages may be mobile (circulating in the mobile) and fixed. Fixed macrophages are those which are fixed to some tissue or organ e.g., histocytes (macrophages fixed in skin tissue), Kupffer cells (fixed macrophages in liver cells), microglia (in brain and spinal cord). (i) Dendritic cell Dendritic cell is derived from bone marrow and are found in tissues that have direct contact with the external environment such as skin and in the inner linings –of nose, lungs, stomach and intestine. E.g., Langerhans cells in skin. Immature forms are also found in blood. Once activated and mature they migrated to the lymph nodes where they interact with the T cells to initiate and shape the adaptive immune response. At certain development stages, they grow into branched projections i.e., dendrites that give the cells its name. Greek word ‘’Dendron ‘’ means ‘tree’. 2. Natural killer cells NK cells are the type of lymphocytes and are the component of innate immune response. They are specialized in killing virus-infected cells and tumor cells. NKC are cytotoxic and small granules in their cytoplasm contain special proteins such as perforins and proteases (granzymes). NKC release perforins in close proximity of infected cells which form pores in the cell membrane of the target cells through which the granzymes can enter to induce apoptosis. (programmed cell death) 3. Mast cells and Basophils A mast cell is derived from the myeloid stem cells in bone marrow. It is a part of immune system and contain many granules such as histamine and heparin. Mast cells play an important protective role. They discharge granules when they are stimulated, and the granule contents can contribute the triggering of local inflammation. Basophiles are WBCs with cytoplasmic granules that appear blue when stained with Wright stain. The blue color is caused by positively charged methylene blue dye binding to several negatively charged molecules in the granules. The mast cells are similar in both appearance and functions to basophils. They differ in that mast cells are tissue residents specially under the skin and in the mucosa of the respiratory and GI tract. Page 4 of 9 4. Eosinophils: Eosinophils are WBCS with cytoplasmic granules that appear red when stained with the wright stain. The red color is caused by negatively charged Eosin dye binding to the positively charged basic protein in the granules. Wright stain has been divided into two types. ● Eosin ● Methylene blue Eosin stain: It is an anionic (negatively charged) acidic dye. It combines with the positively charged granules of eosinophils and forms red color dye. Methylene blue stain: It is a cationic (positively charged) basic dye. It combines with the negatively charged granules of basophils and forms blue violet color dye. On the other hand, neutrophils contain both positively and negatively charged granules and forms pink color, with both eosin and methylene blue stain. Elevation of Eosinophil count: Eosinophil count is elevated in two medically important conditions: ● In parasitic diseases specially caused by nematodes. ● Hypersensitivity diseases such as asthma and Serum sickness. Functions of Eosinophils: The function of Eosinophils has not been clearly established. It seems likely that their main function is to defend against the larvae of nematodes. As they attach to the surface of the larvae end discharge the contents of their granules, which in turn damages the cuticle of larvae. Another function of Eosinophils is to mitigate the effects of immediate hypersensitivity reactions because the granules of Eosinophils contain histaminase, an enzyme that degrades histamine, which is an important mediator of immediate reactions. Page 5 of 9 Inflammatory response and phagocytosis ⮚ The presence of foreign bodies, such as bacteria within the body provokes a protective inflammatory response. ⮚ This response is characterized by clinical findings of redness, swelling, warmth and pain at the site of ⮚ inflammation. These signs are due to increased blood flow, increased capillary permeability and escape of fluid from cells into tissue spaces. ⮚ The increased permeability is due to the several chemical mediators of which histamine, prostaglandins and ⮚ leukotrienes are most important. Bradykinin is an important mediator of pain and fever. The cells that appear at the site, neutrophils and macrophage both of which perform phagocytic function arrive early. Neutrophils and macrophage are attracted to the site of infection by small polypeptides known as chemokines. Chemotaxis: Many different chemical substances (Chemokines) in the tissues cause both neutrophils and macrophages to move towards the source of chemicals. This phenomenon is known as chemotaxis. Acute phase response: Certain proteins collectively known as acute phase response proteins, are also produced early in the inflammation mainly by the liver. The best known of these are C-Reactive proteins and MBL (Mannose binding lectin) protein, which bind to the surface of bacteria and enhance the activation of compliment system. Phagocytosis: As part of inflammatory response, bacteria engulfed by neutrophils and macrophages. Process of phagocytosis can be divided into three steps: ● Migration ● Ingestion ● Killing Page 6 of 9 1. Migration: ⮚ Migration of neutrophils and macrophages to the site of infection is due to chemokines such as Interleukin-8 and complement component C5a. 2. Ingestion: ⮚ The bacteria are ingested by the invagination of phagocytic cell membrane around the bacteria to form a vacuole known as phagosome. ⮚ At the time of engulfment, a new metabolic pathway known as respiratory burst is triggered. This results in the production of two microbicidal agents, the superoxide radicle (O2._) and hydrogen peroxide. These highly reactive compounds are generated by the following reactions. ⮚ In the first reaction molecular oxygen is reduced by an electron to form superoxide which is weak bactericidal agent. O2 + 1e- → O2._ ⮚ In the next step the enzyme superoxide dismutase catalyzes the formation of Hydrogen peroxide from the superoxide radicle. 2O2.- + 2H+ → H2O2 + O2 3. Killing: ⮚ The killing of microorganisms within the phagosome is a two-step process that consists of degranulation followed by the production of hypochlorite ions which are probably the most important microbicidal agents. ⮚ In degranulation, the two types of granules in the cytoplasm of neutrophils fuse with the phagosome (Now known as phagolysosome), emptying the contents in this process. These granules are lysosomes that contain a variety of enzymes essential to the killing and degradation. ● ● The larger lysosomal granules which constitute about 15% of the total contain an important enzyme myeloperoxidase as well as lysozyme and several other degradative enzymes. Myeloperoxidase which is green in color makes major contribution to the color of the pus. The smaller granules which make up remaining 85% contain lactoferrin and other degradative enzymes such as proteases, nucleases and lipases. Page 7 of 9 ⮚ The actual killing of microorganisms occurs by variety of mechanisms which fall into two categories: oxygen dependent and oxygen independent. ● Oxygen independent mechanism involve the activation of hydrolytic enzymes and the action of antimicrobial peptides. ● But, much of killing occurs by variety of oxidative enzymes, of them the most important is the production of highly reactive hypochlorite ion by Myeloperoxidase according to the following reaction. Cl- + H2O2 HOCl ● HOCl (Hypochlorous acid) + H2O H+ + OCl- (Hypochlorite ion) Hypochlorite itself damages the cell wall but can also react with the hydrogen peroxide to produce singlet oxygen which damages the cell by reacting with the double bonds in fatty acids of membrane lipids. ❖ Macrophages also migrate, engulf and kill bacteria, by using the same process as neutrophils, but they don't produce myeloperoxidase, therefore they can't make hypochlorite ion. However, in macrophages, the hydrogen peroxide and superoxide free radicals are produced to kill the microbe. Proteins Interferon Word Derived from” interfere” interfere with viral replication They are proteins which interfere with the viral replication. They're basically signaling proteins by macrophages, lymphocytes, and infected cells. Page 8 of 9 Interferon are a group of protein made and released by host cells in response to the presence of several pathogens such as virus, bacteria, parasites, and also tumor cells. Interferon was named for its ability to interfere with viral replication. General Mechanism of Action Interferons are small proteins or glycoproteins released by macrophages, lymphocytes and tissue cells infected with virus. It releases interferon. Interferon will diffuse into the surrounding cells when it binds to the receptors, on the surface of those adjacent cells, they begin the production of proteins that interfere with the synthesis of viral proteins. This prevents the spread of virus throughout the body. There are mainly Three types of interference named alpha beta and gamma interferons. Page 9 of 9