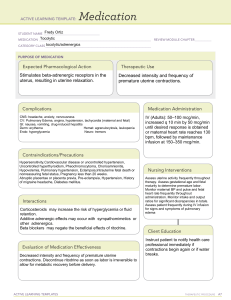
⚫DYSTOCIA a difficult labor which can arise from the POWER, the PASSAGEWAY, the PASSENGER, PSYCHE and medical interventions -labor that lasts >24 hours) COMMON CAUSES OF DYSFUNCTIONAL LABOR ⚫ Inappropriate use of analgesia (excessive or too early administration) ⚫ Pelvic bone contraction that has narrowed the pelvic diameter so that a fetus cannot pass (rickets) ⚫ Poor fetal position (posterior rather than anterior positions) ⚫ Extension rather than flexion of the fetal head ⚫ Overdistention of the uterus, as with multiple pregnancy, hydramnios, or an excessively oversized fetus ⚫ Cervical rigidity ( unripe) ⚫ Presence of a full rectum or urinary bladder that impedes fetal descent ⚫ Mother becomes exhausted from labor ⚫ Primigravida status COMPLICATIONS WITH THE POWER (FORCE OF LABOR) INERTIA- sluggishness of contractions, now known as DYSFUNCTIONAL LABOR ⚫ PRIMARY (occurring at the onset of labor) or ⚫ SECONDARY (occurring later in labor) UTERINE TONES NORMAL VALUES: RESTING TONE= 5-15 mm Hg MILD CONTRACTION= 15-30 mm Hg MODERATE CONTRACTION= 30-50 mm Hg STRONG CONTRACTION= 50-75 mm Hg INEFFECTIVE UTERINE FORCE HYPOTONIC CONTRACTIONS(2ary inertia)/HYPOTONIC UTERINE INERTIA ⚫ The number of contractions is low or infrequent ( not increasing beyond 2 or 3 in a 10-minute period ⚫ Resting tone of the uterus remains < 10 mm Hg, & strength of contractions does not rise above 25 mm Hg ⚫ Common in the ACTIVE PHASE ⚫ Increases length of labor & uterus does not contract effectively postpartally due to exhaustion, increasing chance for postpartal hemorrhage ⚫ Cervix is dilated for prolonged periods increasing risk for infection of mother & fetus Causes of Hypotonic Uterus ⚫ administration of analgesia when cervix is not dilated to 3 or 4 cm, ⚫ bowel or bladder distention- prevents descent or firm engagement, ⚫ multiple gestation, ⚫ LGA fetus, ⚫ hydramnios, ⚫ lax uterus due to grand multiparity Complications ⚫ Maternal/fetal infections- cervix is dilated for a prolonged time ⚫ Postpartum hemorrhage ⚫ Fetal distress and death ⚫ Maternal exhaustion Management of Hypotonic Uterus ⚫ UTZ to rule out CPD ⚫ Walking, if not contraindicated ⚫ OXYTOCIN to augment labor by strengthening contractions & making them effective ⚫ Amniotomy to speed up labor ⚫ 1st hour postpartum, palpate the uterus and assess lochia q 15 minutes to ensure that postpartl contractions are not also hypotonic & inadequate to halt bleeding OXYTOCIN for Hypotonic UI ⚫ Do not leave pt alone ⚫ Client must be in true labor- at least 3 cm ⚫ No obstruction, uterine overdistention, multiple gestation ⚫ Monitor VS esp BP( most impt bec oxytocin may cause hypo/hypertension ⚫ Assist w/ delivery: after failed trial labor of 6 hours ⚫ After delivery: observe for signs of injury & signs of poor bonding dt difficult delivery HYPERTONIC UTERUS( primary inertia) ⚫ Increase in resting tone to > 15 mm Hg, mostly seen in the LATENT PHASE ⚫Muscle fibers do not repolarize or relax after a contraction, thereby wiping it clean to receive a new pacemaker stimulus ⚫More painful because the myometrium becomes tender from constant lack of relaxation & the anoxia of uterine cells that results HYPERTONIC UTERUS ⚫Lack of relaxation between contractions may not allow uterine artery filling leading to fetal anoxia ⚫ **Any woman whose pain is out of proportion to the quality of her contractions should have both a uterine & fetal external monitor applied for at least 15 mins to make sure that the resting phase of contractions is adequate & that the fetal pattern is not showing late deceleration Management of Hypertonic Uterus ⚫ Rest & pain relief with a drug like morphine sulfate & sedatives ⚫ Change linen and client’s gown, darken the room lights, decrease noise & stimulation ⚫ If (+) for deceleration in FHR, abnormally long 1st stage of labor, or lack of progress with pushing (“2nd STAGE ARREST”), CS may be necessary HYPOTONIC vs HYPERTONIC CONTRACTIONS CRITERIA HYPERTONIC HYPOTONIC Phase of Labor Latent Active Symptoms Painful Painless Medication Oxytocin Unfavorable reaction Sedation Helpful Little value Favorable reaction CONTRACTION RING ⚫ It is a hard band that forms across the uterus at the junction of the upper and lower uterine segments and interferes with fetal descent. ⚫ BANDL’S RING or PATHOLOGIC RETRACTION RING- a type of contraction ring that usually appears at the 2nd stage of labor & can be palpated as a horizontal indentation across the abdomen. ⚫ It is a warning sign that severe dysfunctional labor is occurring as it is formed by excessive retraction of the upper uterine segment; the myometrium is much thicker above than below the ring. ⚫ It is caused by uncoordinated contractions due to CPD, manipulation or the use of oxytocin. ⚫ The fetus and the undelivered placenta are gripped by the retraction ring and cannot advance beyond this point. BANDL’s RING Management ⚫ Administration of IV morphine sulfate or inhalation of amyl nitrate ⚫ Tocolytics to halt the contractions ⚫ Cesarian birth to ensure safety of the fetus and manual removal of the placenta under general anesthesia Complications: ⚫Uterine rupture ⚫Neurologic damage to the fetus PRETERM/PREMATURE LABOR Definition: labor that occurs before the end of 37 weeks of gestation ⚫ Associated with: ⚫ Dehydration ⚫ Urinary tract infection ⚫ Periodontal disease ⚫ Chorioamnionitis ⚫ Large fetal size ⚫ Strenuous jobs during pregnancy ⚫ Shift work ⚫ Intimate partner violence and trauma Assessment ⚫ Persistent uterine contractions (4 contractions every 4 minutes or less) ⚫ Low abdominal cramping with or without diarrhea ⚫ Intermittent sensation of pelvic pressure, urinary frequency ⚫ Persistent, dull low backache ⚫ Increased vaginal discharge, may be pink-tinged ⚫ Leaking amniotic fluid ⚫ Cervical effacement > 80% & dilatation > 1 cm PTL Management ⚫Lab test to detect presence of fetal fibronectin to predict impending delivery; if absent, labor will not occur for at least 14 days ⚫UTZ of cervix to determine shortening ⚫Patient is admitted & placed in complete bed rest (preferably left side-lying) to relieve pressure of the fetus on the cervix Management cont’d ⚫ IV fluid to maintain hydration which may help stop contractions (dehydration stimulates PG to secrete oxytocin) ⚫ Vaginal, cervical & urine cultures to rule out infection ⚫ Increase fluid intake since a full bladder inhibits contractions ⚫ TOCOLYTICS- to halt labor ⚫ Discharge- once contractions have stopped and maternal and fetal conditions have stabilized ⚫ No MEPERIDINE(DEMEROL) TOCOLYTIC AGENTS to halt labor Drug Type/purpose Major side effects RITRODRINE (YUTOPAR) ß-adrenergic TERBUTALINE receptor agonist/tocolysis Maternal or fetal tachycardia, Nursing concerns shortness of breath, pulmonary edema, tremors, N/V,hyperglycemi a, (BRETHINE) ß-adrenergic/ tocolysis; antidote: PROPANOLOL SAME AS ABOVE SAME AS ABOVE hypokalemia Assess VS, breath sounds, FHR, contractions & maternal response Drug Type/purpose Major side effects Nursing concerns MgSO4 CNS Depressant/Tocol ysis BETAMETHASONE (CELESTONE) or Lethargy, heat sensation, 10-12 mg/dl) respiratory depression, Assess RR, DTR, hourly urinary depressed reflexes, cardiac output, serum Mg levels arrest if high serum levels (> DEXAMETHASONE infection & poor wound 48 hours before Corticosteroid/ healing, delivery to be stimulates fetal lung hypoglycemia, effective; commonly maturation by increased risk of used between 24 to 34 stimulating pulmonary edema when weeks AOG unless given with a fetal lung maturity can surfactant ß-adrenergic agent be documented production Increased risk of Must be given 24 to PRECIPITATE LABOR Definition: ⚫ it is a labor that is completed in < 3 hours ⚫ It occurs when uterine contractions are so strong that the woman gives birth with only a few, rapidly occurring contractions. Causes: grand multiparity, induction of labor by OXYTOCIN or AMNIOTOMY PRECIPITATE LABOR Causes: ⚫ grand multiparity, ⚫Large pelvis ⚫ Small fetus ⚫ induction of labor by OXYTOCIN or ⚫ AMNIOTOMY PRECIPITATE LABOR Symptoms: ⚫ rate of dilatation in the active phase: ⚫ > 5 cm/hr (1 cm/12 mins) in a nullipara ⚫ 10 cm/hr (1 cm/6 mins) in a multipara; ⚫ tocolytics may be administered PRECIPITATE LABOR Maternal Complications: ⚫ premature separation of the placenta leading to hemorrhage, ⚫ infection ⚫ lacerations on the birth canal ⚫ Uterine rupture ⚫ Amniotic fluid embolism Fetal Complications ⚫ Fetal hypoxia, anoxia ⚫ Erb-Duchenne palsy ⚫ Injuries like falling to the floor in unattended childbirth ⚫ Subdural hemorrhage on the fetus due to sudden release of pressure on the head, ⚫ hemorrhage PRECIPITATE LABOR Management: ⚫TOCOLYTICS ⚫ In multiparous women with history of a brief past labor, advise to prepare for appropriately timed transport starting on her 28th week of gestation(BIRTH PLAN) ⚫ Never leave client ⚫ Monitor FHT q15 min ⚫ Provide emotional support: inform client of what is happening ⚫ Assist with the delivery, advising the client to pant or blow and NOT to push ⚫ Never hold the baby back ⚫ Support the perineum with a towel to prevent lacerations and also subdural hemorrhage(MODIFIED RITGEN’S MANEUVER) ⚫ Deliver baby in-between contractions ⚫ Inspect the perineum for possible lacerations INVERSION OF THE UTERUS Definition: ⚫turning inside out of the uterus with either birth of the fetus or the delivery of the placenta INVERSION OF THE UTERUS Predisposing Factors ⚫ Pulling or traction on the umbilical cord to remove the placenta ⚫ Vigorous pressure is applied to the fundus while the uterus is not contracted ⚫ The placenta is attached at the fundus and the passage of the fetus during birth pulls it down INVERSION OF THE UTERUS Types of Inversion ⚫ 1. Complete or Total Inversion ⚫ The uterus is visible outside the vaginal introitus ⚫ Life threatening because of severe hemorrhage & shock ⚫ 2. Partial Inversion ⚫ The inverted fundus may lie within the uterine cavity ⚫ It is not visible but may be palpated ⚫ It hampers or impedes contractions & control of hemorrhage INVERSION OF THE UTERUS Assessment ⚫ Sudden gushing of blood from the vagina ⚫ Signs of blood loss: hypotension, dizziness, paleness or diaphoresis ⚫Because bleeding is continuous, exsanguination could occur within 10 minutes INVERSION OF THE UTERUS Management ⚫ Never attempt to replace an inversion since handling of the uterus will worsen the hemorrhage ⚫ Never attempt to remove the placenta if it is still attached ⚫ Oxytocic drugs makes the uterus more tense thus, more difficult to replace ⚫ Start an IV line (use a large-gauge needle to be used in BT) & open it to achieve optimal flow to restore fluid volume Management cont’d ⚫Administer O2 by mask ⚫Assess VS ⚫Prepare to administer CPR ⚫General anesthesia, nitroglycerin or a tocolytic is administered to relax the uterus ⚫Physician or midwife will then replace the fundus manually ⚫After replacement, administer Oxytocin ⚫Antibiotic therapy to prevent infection ⚫CS is recommended for succeeding pregnancies PROBLEMS WITH THE PASSENGER PROLAPSE OF THE UMBILICAL CORD Definition ⚫A loop of the umbilical cord slips down in front of the presenting fetal part ⚫ It may occur any time after the membranes have ruptured if the presenting part is not fitted firmly into the cervix Cord Prolapse Predisposing Factors ⚫ Premature rupture of membranes ⚫ Fetal presentation other than cephalic ⚫ Placenta previa ⚫ Intrauterine tumors preventing the presenting part from engaging ⚫ A small fetus ⚫ CPD preventing firm engagement ⚫ Hydramnios ⚫ Multiple gestation CORD COMPRESSION Cord Prolapse Assessment ⚫ The cord may be felt as the presenting part on an initial vaginal examination during labor ⚫ UTZ evidence ( a CS is necessary before rupture of membranes) ⚫ variable deceleration pattern becomes apparent ⚫ The cord may be visible at the vulva ⚫ To r/o prolapse, assess FHR immediately after rupture of membranes Management ⚫ cord prolapse will lead to cord compression because the presenting part will press against the cord at the pelvic brim ⚫ Place the mother’s hips higher than her head: knee-chest position ⚫ Trendelenberg position Management ⚫ Amnioinfusion-to reduce compression on the cord with infusion of 5ooml warmed NSS. ⚫ Used for only a short time until the cervix is fully dilated or a cesarean birth can be arranged. ⚫ Can also be performed for women with oligohydramnios ⚫ Nursing Consideration ⚫ Monitor FHR and uterine contractions continuously. ⚫ Monitor maternal temp every hour ⚫ Placed the bag of fluid in a radian warmer to prevent chilling Management 1. Prevention: ⚫Always assess FHT after membranes rupture ⚫Place woman on bed rest after membranes rupture 2. Reduce pressure on the cord by: ⚫Place in Knee-chest or Trendelenburg position, or place folded towel under the hips ⚫Put on sterile gloves and insert 2 fingers into the vagina, then push presenting part upward 3. If cord is exposed to air, cover with saline moistened sterile compress to prevent drying. ⚫Drying of cord leads to atrophy & constriction of BV Management 4. Never replace the cord back into the vagina as it may result in kinking and knotting obstructing blood flow 5. Administer O2 at 10 LPM to improve O2 supply to fetus 6. Deliver baby ASAP: ⚫Vaginal delivery if cervix is fully dilated & no fetal distress ⚫CS if cervix is not fully dilated & if fetal distress is present Cesarean Section Management ⚫ Place a gloved hand in the vagina and manually lift the fetal head off the cord ⚫ Administer O2 at 10 LPM by face mask to the mother to increase oxygenation to the fetus ⚫ Tocolytic agent may be administered to reduce uterine activity & pressure on the fetus ⚫ Maintain continuous electronic fetal monitoring ⚫ Prepare for rapid delivery vaginally or by CS FETAL MALPOSITION ⚫The ideal position is flexed with the occiput in the R or L Anterior quadrant (ROA/LOA) Types of Malposition 1. OCCIPITOPOSTERIOR POSITION ⚫ It occurs in 1/10 of all labors and during internal rotation the head must rotate through 135 degrees instead of 90 degrees ⚫Failure to rotate is termed PERSISTENT OCCIPUT POSTERIOR ⚫Common in women with android, anthropoid or contracted pelves OCCIPITOPOSTERIOR Occipitoposterior Position Symptoms: ⚫ prolonged active phase, ⚫ arrested descent, ⚫ FHT heard best at the lateral sides of the abdomen, ⚫ intense back pain during labor ROP/LOP ⚫Maternal risks: prolonged labor, potential for CS birth, 3rd or 4th degree lacerations ⚫Fetal risks: umbilical cord prolapse, increased molding, caput formation 2. OCCIPUT TRANSVERSE POSITION ⚫Due to ineffective contractions or a flattened bony pelvis ⚫Vaginal delivery is possible with oxytocin administration and application of forceps for delivery Management: ⚫Encourage mother to lie on her opposite side from the fetal back which may help with rotation ⚫Other positions: Hands and knees position, squatting, pelvic rocking Management ⚫Apply sacral counter-pressure with the heel of the hand or do back rubs to relieve back pain ⚫Apply heat or cold, as desired by the patient Occipitotransverse ⚫ Encourage voiding every 2 hours ⚫ In prolonged labor, provide sports drink or IV glucose to replenish glucose stores ⚫ Provide constant encouragement and inform the client & family of progress ⚫ Prepare for a forceps delivery FETAL MALPRESENTATION 1. BREECH PRESENTATION 2. VERTEX MALPRESENTATIONS a. FACE PRESENTATION b. BROW PRESENTATION c. SINCIPITAL PRESENTATION (MILITARY ATTITUDE) FETAL MALPRESENTATIONS 3. SHOULDER PRESENTATION (TRANSVERSE LIE) 4. COMPOUND PRESENTATION