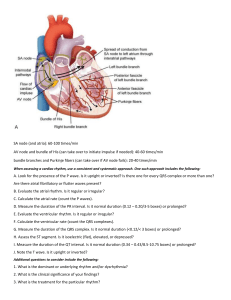
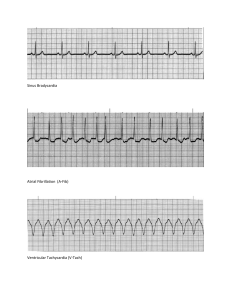
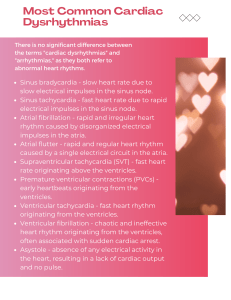
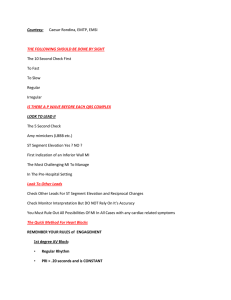
EKG INTERPRETATION Smitha Raju MSN, RN Adjunct Professor, Broward College Objectives of this 2 day Program • • • • • • • • • • Review of Cardiac Anatomy and Physiology Review the Conduction System of the Heart EKG Rhythm Analysis Sinus Rhythms Atrial Arrhythmias Junctional Arrhythmias Ventricular Arrhythmias AV Blocks Pacemaker Rhythms Myocardial Infarction Anatomy and Physiology 60 i00 gatekeeperDelays to impulsesfromsa venticual contractventricuals pacemaker five impulses myocardio cell fondract relax Depolarization Electrical Conduction polarization Electrical Impulses that Originate From: SA Node: 60-100bpm AV Node: 40-60bpm Bundle Branches: 20-40bpm Ventricular: 20-40bpm cardiac cycle one contraction one relaxation contra relax Electrocardiogram (EKG) Graphic record of the heart’s electrical activity, its conduction of impulses; a record of the electrical events that precede the contractions of the heart • Normal ECG is composed of the following: • P wave—represents depolarization of the atria • QRS complex—represents depolarization of the ventricles and repolarization of the atria • T wave—represents repolarization of the ventricles; may also have a • U wave that represents repolarization of the purkinji fibers. ECG Paper 6sec strip 30large boxes ECG Paper 1 Small Box 5 Small Boxes 15 Boxes of .20 30 Boxes of .20 = .04 sec = .20 sec = 3 sec = 6 sec ometric I ne ng p l ECG Waveforms P wave Represents depolarization of the atria SA node impulse usually causes a positive deflection on the ECG paper Above the Should be smooth and round Isometric line ECG Waveforms PR interval Represents time from beginning of P wave to beginning of QRS complex Normal measurement .12-.20 seconds( 3-5boxes) thetime it takes For SAnote tothe AUnode p rinterval ECG Waveforms QRS complex Represent depolarization of the ventricles Measured in time from the beginning of the ‘Q’ wave to the end of ’S’ wave see Imits- 0.12 secs) Normal measurement < 0.10seconds (0.8 (2-3 boxes) QRS > 0.12 sec is called a Bundle Branch Block ECG Waveforms T Wave Represents ventricular repolarization Absolute Refractory Period Watch OUT ECG Waveforms QT Interval Starts from the beginning of the ‘Q’ Wave to the end of the ‘T’ Wave Represents electrical depolarization and repolarization of the right and left ventricles Prolong ‘QT’ will lead to ventricular tachyarrythmias. Normal measurement 0.36 – 0.44 sec 812518 indicates point If Isometric Line MI if not Flatt ECG Interpretation 3 Methods are Used to Calculate Heart Rate 6 Second Method- Count the number of ‘R’ waves in a 6 second strip (30 large boxes) and multiply by 10. This method can be used for both regular and irregular rhythms Large Boxes Method- Count the number of large boxes between two consecutive ‘R’ waves and ÷ into 300 Sequence Method- Determine ventricular rate by selecting an ‘R’ wave that falls on dark vertical line. Number the next 6 dark lines: 300, 150, 100, 75, 60, 50. For regular H.R. For Irregular HR Sequence Method Find an R wave that peaks on a heavy black line and assign the numbers Follow the following steps in order to identify the Rhythm: Analyzing a Rhythm Strip • ‘P’ wave must be present: Look at the shape. • ‘P’ must be present for each QRS. • Rhythm Regular? R-R distance must be constant • Determine PR interval: Must be 0.12 0.20 sec • Determine QRS interval: Must be < or equal to 0.10 sec • Determine the Heart Rate: • Atrial Heart Rate: Count # of P waves and X 10 • Ventricular Rate: Count # of R waves and X 10 • Normal Heart Rate: 60 – 100 bpm Sinus Rhythms Normal Sinus Rhythm Sinus Arrhythmia Sinus Bradycardia Heart rate low r hythem normal Sinus Tachycardia Heart rate high rhythmnormal Sinus Arrest vythm pause Practice P Present : Yes P Before QRS: Yes Rhythm Regular: Yes PR Interval: 4 small boxes = 0.16sec Normal is .12 - .20sec QRS Interval: 2 small boxes = .08sec Normal is < or = .10sec Atrial Rate = 8 ‘P’ waves 8X10 = 80 Ventricular Rate = 8 ‘R’ waves 8X10 = 80 Normal HR is 60 – 100bpm Rhythm is NSR NSR Rhythm Sinus Bradycardia Rhythm Sinus Bradycardia - Normal in sleep; aerobically trained athlete Causes: Drug abuse, digoxin toxicity, CHF, hypothyroidism, hypothermia, hypokalemia/hyperkalemia SYMPTOMS Hypotension Pale, cool skin Weakness Angina Dizziness or syncope; shortness of breath Confusion or disorientation Shortness of breath Treatment- if symptomatic, atropine or pacer ppacemaker Sinus Tachycardia Rhythm SINUS TACHYCARDIA • Rate >100: Sinus Tachycardia 50 between •Causes-Anemia, bleeding, fever, dehydration, infection, anxiety, hypoxia, shock, pain, caffeine, drugs •Treatment-eliminate cause Sinus Dysrhythmias (Arrhythmia) (SA) Rate 60-100 Irregular rhythm- increases with inspiration, decreases with expiration P, QRS,T wave normal Cause- children, drugs (Morphine sulphate), MI Treatment- none Sinus Arrest •See pauses •May see ectopic beats (PAC s PVC s)*don t treat •Due to MI •Treatment Atropine Isoproterenol (Isuprel) Pacemaker Isoproterenol-synthetic sympathomimetic amine Analyzing a Rhythm Strip DON’T Treat the Monitor Treat the Patient!!! Assess patient: Symptomatic or Asymptomatic Is Heart Rate Brady or Tachy? Assess patient: Stable vs Unstable Treat Stable Patients with Meds Treat Unstable Patients with Electricity *******KNOW YOUR DRUGS!!!!! OR Practice Sinus sinus Taihy sinus ythias Sinus Brady Atrial Arrhythmias Premature Atrial Contraction (PAC) Supraventricular Tachycardia paroxysmal (SVT) atrial tachy Atrial Flutter Atrial Fibrillation Premature Atrial Contraction PAC P wave abnormally shaped-contraction originates from ectopic focus in atrium other than SA Node PR interval shorter-travels abnormal pathway (distorted P waves) QRS normal Cause-age, MI, CHF, stimulants, dig, electrolyte imbalance; valvular disease; hypoxia Treatment- remove stimulants; watch for SVT, depends upon cause; isolated not significant; B-adrenergic blockers Supraventricular Tachycardia No p waves SVT Toomoth impulses Pat waves together SVT/PSVT PSVT is Paroxysmal Supraventricular Tachycardia Rate is usually greater than 150bpm Causes: Alcohol or caffeine use, dig tox,hepatic failure, Hypokalemia, resp.illness V fib just give an electric 250 360jew in emerengy Treatment Vagal Maneuvers baredown cough kneeto chest Meds-Adenosine Iv 6mg Unstable Patient: Cardioversion reset the rhythm Shockduring Qrscomplex 20 150jewls wait 2 mins 12mg wait 2min 12mg much too Atriffing Atrial Fibrillation printed'd i 8 Pwaves now f waves Atrial Flutter more seriousthan A fiberate high fraternal regular gun Complication Atrial Fibrillation stroke PE Causes of Atrial Fibrillation: Hypertension Heart surgery Viral infections Stress due to pneumonia Sleep apnea Drugs: Stimulants controlthat Mt Lung diseases Heart Failure Abnormal Heart Valves Metabolic Imbalances Myocardial Infarction Heart Defects É carsonDrip j Treatment: Beta Blockers and Calcium Channel Blockers É Unstable Patient: Cardioversion Anticoagulants bc of clots Heprin drip blood gets Drwill get clots cause Atrium May in trapped you a target goal for the heart rate TED Practice scope to the O to see if thereis any clots inthere A fib SVT A flutter Supraventricular Rhythm • • • Junctional Rhythm (40-60bpm) Accelerated Junctional Rhythm(>60-100bpm Junctional Tachycardia(>100BPM) Junctional Rhythm (Supraventricular Rhythm) Dysrhythmia that originates in area of AV node AV node is pacemaker- slow rhythm (40-60) but regular impulse goes to atria from AV nodebackward); SA node failed to fire or impulse delayed or blocked at AV node P wave patterns Absent or hidden; Short < .0.12 or negative or PR interval; P wave precedes QRS inverted in II, III, and AVF or P wave hidden in QRS or P wave follows QRS QRS normal . Junctional Dysrhythmias Accelerated Junctional Rhythm Rate is 60-100 Junctional Tachycardia Rate is Greater Than 100bpm Junctional Dysrhythmia Cause: Digitalis/Digoxin toxicity-Digibind MI Cardiac Surgery(Valve Replacement) Treatment Treat underlying cause Accelerated junctional rhythm and junctional tachycardia caused by digoxin toxicity; digoxin is held b- blockers, calcium channel blockers, and amiodarone for rate control for junctional tachycardia not caused by digoxin toxicity Cardioversion is contraindicated 49 Types of Heart Blocks First Degree AV Block Second-Degree AV Block (Mobitz Type I) or Wenckebach Second-Degree AV Block (Mobitz Type II) Third Degree AV Block (Complete) reflex in the PR inteval more than 0.2sec largebox First Degree AV Block First Degree AV Block Cause-dig toxicity, MI, CAD, vagal stimulation; hyperthyroidism, beta- adrenergic drugs; calcium channel blockers Usually asymptomatic Treatment none but watch for further blockage Check medications. Continue to monitor. Second-Degree AV Block (Mobitz Type I) or Wenckebach Second Degree AV Block more P s than QRS s • A. Mobitz I (Wenckebach) • Cause- MI, drug toxicity • Treatment- watch for type II and 3rd degree Second-Degree AV Block (Mobitz Type II) Second-Degree AV Block, Type 2 (Mobitz II) • Clinical significance • Often progresses to third-degree AV block ; associated with poor prognosis • Reduced HR often results in dec. CO with subsequent hypotension and myocardial ischemia Second-Degree AV Block, Type 2 (Mobitz II) Clinical associations Rheumatic heart disease CAD Anterior MI Digitalis toxicity Treatment If symptomatic (e.g., hypotension, angina) before permanent pacemaker can be inserted, temporary transvenous or transcutaneous pacemaker Permanent pacemaker Copyright © 2011, 2007 by Mosby, Inc., an affiliate of Elsevier Inc. 60 Third Degree AV Block (Complete) 3rd Degree AV Block • Atria and ventricles beat independently (ventricular rhythm is escape rhythm • Atrial rate- 60-100 • Slow ventricular rate 20-40 • No PR interval • Wide or normal QRS (depends on where block is) • Cause- severe heart disease, systemic diseases; meds as digoxin, beta-adrenergic blockers, calcium channels blockers • Complications- dec. CO, ischemia, HF, shock, bradycardia, syncope, possible asystole Third-Degree AV Heart Block (Complete Heart Block) • Treatment • If symptomatic, transcutaneous pacemaker until a temporary transvenous pacemaker can be inserted • Drugs (e.g., atropine, epinephrine): Temporary measure to increase HR and support BP until temporary pacing is initiated • Permanent pacemaker as soon as possible 64 PRACTICE QUESTION PRACTICE QUESTION SECOND DEGREE AV BLOCK, TYPE I WENCKEBACH FIRST DEGREE AV BLOCK Second degree AV Block MOBITZ II THIRD DEGREE AV BLOCK SECOND DEGREE AV BLOCK, TYPE I WENCKEBACH THIRD DEGREE AV BLOCK Second degree AV Block MOBITZ II First degree AV Block Bundle Branch Blocks • Left BBB • Right BBB • QRS.12 or greater • Rabbit ears- RR - Right bundle branch block • Devil’s ear-RR- LBB Block • No change in rhythm Types of Ventricular Rhythms most Dangerous Premature Ventricular Complexes Ventricular Tachycardia Torsades de Pointes Ventricular Fibrillation Asystole Pulseless Electrical Activity (PEA) expat Premature Ventricular Complexes (PVCs) 00 extrawfoutpwave Premature Ventricular Contractions (PVC s)-ectopic • Cause- 90% with MI, stimulants, dig, electrolyte imbalance • Treatment- O2, lidocaine, procainamide (Pronestyl), *amiodarone, *abalation side warning elegygyatences for jaded Definitions Bigeminy- (PVC) every other complex Trigeminy-(PVC) every 3rd complex Couplet- pair of abnormal beats Treat if: • >5 PVC s a minute II It if code we Ventricular Tachycardia • V-tach is caused by a disruption in the normal electrical impulses that control the ventricular contraction • Abnormal electrical signals in the ventricles cause the heart to beat faster than normal Symptoms • Palpitation/chest pain • Syncope/Dizziness • Weak/no pulse • Shortness of breath Ventricular Tachycardia Ventricular Tachycardia (VT) • Can be stable- pulse or unstable –no pulse • Cause- electrolyte imbalance, MI, CAD, dig • Life- threatening, decreased CO, watch for V-fib • Symptomatic or Asymptomatic Sustained VT must be treated! Or It will lead to Ventricular Fibrillation • Treatment: • Stable with a pulse = Meds • Unstable with a pulse = Cardioversion • Unstable without a pulse = Defibrillate Remember VT without a pulse is a life-threatening situation. • Cardiopulmonary resuscitation (CPR) and rapid defibrillation • Epinephrine if defibrillation is unsuccessful Polymorphic Ventricular Tachycardia- Torsades de Pointes French term that signifies the “twisting of the points”. May wax and wane in amplitude and may “flip” or “twist” on its electrical axes. Similar to ventricular tachycardia Caused by hypomagnesemia or by antiarrhythmic drugs Alchot intoxicated r wing up alot e y s imbalances Torsades de Pointes Magni un Polymorphic Ventricular Tachycardia- Torsades de Pointes ( twisting around a point ) Causes : hypo/hyperkalemia, HYPOMAGNESEMIA, TCA OD, and some antidysrhythmic medications. Treatment – Defibrillation at 200j, Mg 2gm IVP rapidly/drip 3mg/min, antiarrhythmic drug, pacing Ventricular Rhythms Idioventricular Rhythm When gross damage above the ventricles The ventricular cells are generating the impulses Rate-20- 40 When is very slow is called Agonal Rhythm Poor Cardiac Output TX: Transcutaneous Pacing Epinephrine, Dopamine, Idioventricular Rhythm Idioventricular Rhythm Accelerated Idioventricular Rhythm V. Fibrillation tiffin course fir Ventricular Fibrillation • No P s • No QRS s • No CO • Cause-MI, CAD, CMP, shock, altered K+, hypoxia, acidosis, and drugs • Treatment- code situation, ACLS, CPR, **defibrillate *cannot cardiovert…no rhythm to cardiovert Pulseless Electrical Activity(PEA) NO PULSE Treatment: Find the Cause: Find the H’s & T’s Hypovolemia Toxins Tamponade Hypoxia Tension Pneumothorax Hydrogen ion (acidosis) Thrombosis Hyper-/hypokalemia (Coronary or Pulmonary) Hypothermia. Asystole Asystole • Clinical significance • Unresponsive, pulseless, and apneic state • Prognosis for asystole is extremely poor. • Treatment • CPR with initiation of ACLS measures (e.g., intubation, transcutaneous pacing, IV therapy with epinephrine and atropine) 100 Pacemaker Rhythms Pacemaker Rhythms Atrial Pacemaker Spike before P wave 0 before Spike QRS Pacemaker Rhythms Ventricular Pacemakercomplex EI pwave before Spike a QRS Pacemaker Rhythms AV Sequential Pacer 00 Myocardia Infarction (MI) • An Myocardial Infarction or (MI) can be defined as irreversible myocardial damage. It is caused by a blockage or narrowing of one or more coronary arteries. • Lack of Oxygen to the heart leads to myocardial death. • 12-Lead EKG is used to identify the area of myocardial damage as well as heart disease STDMI (MYOCARDIAL ISCHEMIA) 12 Lead EKG •A 12-lead electrocardiogram or EKG shows the representation of the heart's electrical activity recorded from electrodes on the body surface. •Bipolar Limb Leads - (I, II, III) •Augmented Limb Leads – (aVR, aVL, aVF) •Chest Leads – (V1 – V6) White Right Arm Blaik Bipolar Leads Lead I, II & III e i n m Green Right Leg red Left leg Brown Chest Augmented Leads AUGMENTED OR UNIPOLAR LEADS, AVR, AVL,AVF Chest Leads CHEST PRECORDIALS: V1-V6 Normal 12-Lead EKG Go to Website and Practice https://www.practicalclinicalskills.com/