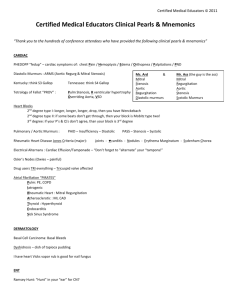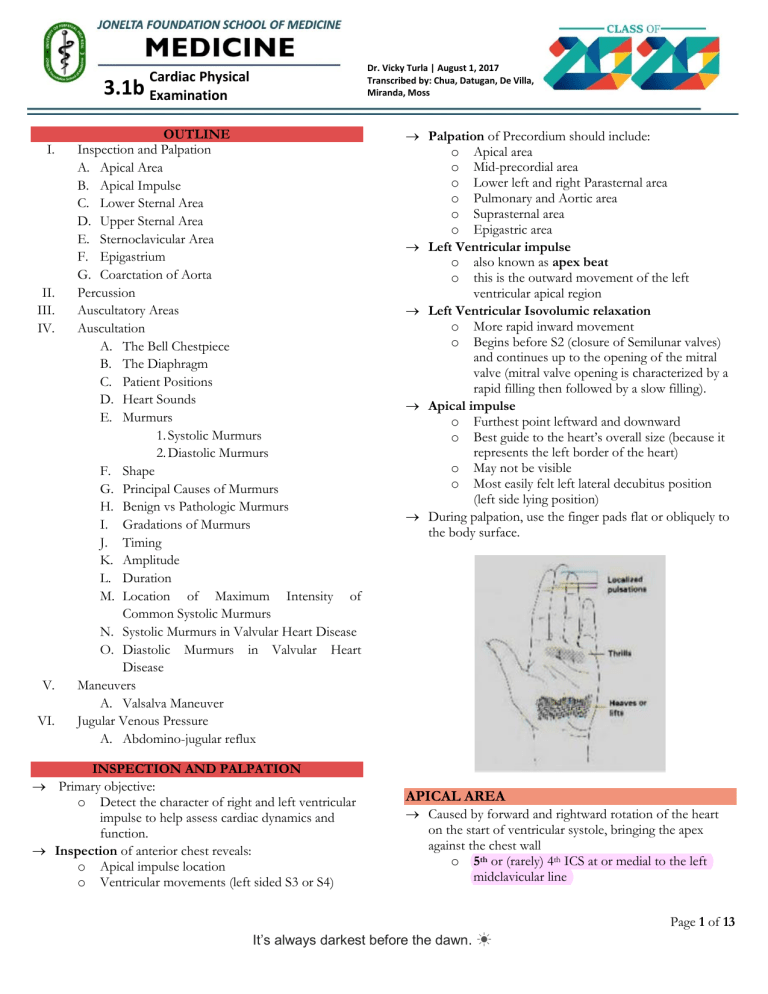
MEDICINE 1: CARDIAC PHYSICAL EXAMINATION Dr. Vicky Turla | August 1, 2017 Transcribed by: Chua, Datugan, De Villa, Miranda, Moss Cardiac Physical 3.1b Examination I. II. III. IV. V. VI. OUTLINE Inspection and Palpation A. Apical Area B. Apical Impulse C. Lower Sternal Area D. Upper Sternal Area E. Sternoclavicular Area F. Epigastrium G. Coarctation of Aorta Percussion Auscultatory Areas Auscultation A. The Bell Chestpiece B. The Diaphragm C. Patient Positions D. Heart Sounds E. Murmurs 1. Systolic Murmurs 2. Diastolic Murmurs F. Shape G. Principal Causes of Murmurs H. Benign vs Pathologic Murmurs I. Gradations of Murmurs J. Timing K. Amplitude L. Duration M. Location of Maximum Intensity of Common Systolic Murmurs N. Systolic Murmurs in Valvular Heart Disease O. Diastolic Murmurs in Valvular Heart Disease Maneuvers A. Valsalva Maneuver Jugular Venous Pressure A. Abdomino-jugular reflux INSPECTION AND PALPATION Primary objective: o Detect the character of right and left ventricular impulse to help assess cardiac dynamics and function. Inspection of anterior chest reveals: o Apical impulse location o Ventricular movements (left sided S3 or S4) Palpation of Precordium should include: o Apical area o Mid-precordial area o Lower left and right Parasternal area o Pulmonary and Aortic area o Suprasternal area o Epigastric area Left Ventricular impulse o also known as apex beat o this is the outward movement of the left ventricular apical region Left Ventricular Isovolumic relaxation o More rapid inward movement o Begins before S2 (closure of Semilunar valves) and continues up to the opening of the mitral valve (mitral valve opening is characterized by a rapid filling then followed by a slow filling). Apical impulse o Furthest point leftward and downward o Best guide to the heart’s overall size (because it represents the left border of the heart) o May not be visible o Most easily felt left lateral decubitus position (left side lying position) During palpation, use the finger pads flat or obliquely to the body surface. APICAL AREA Caused by forward and rightward rotation of the heart on the start of ventricular systole, bringing the apex against the chest wall o 5th or (rarely) 4th ICS at or medial to the left midclavicular line Page 1 of 13 It’s always darkest before the dawn. ☀ MEDICINE 1: CARDIAC PHYSICAL EXAMINATION <10cm from the midsternal line or 3.5 to 4 inches from the midclavicular line o May or may not be palpable in a normal person (depends on the thickness of chest wall and other factors) o Most readily seen in a left side lying position Certain conditions where the normal impulse is felt outside the midclavicular line: Pregnancy Obesity Ascites High left diaphragm Left ventricular hypertrophy Deformities of the thorax In young children, apex beat is often found in the 4th ICS (just outside the midclavicular line). o APICAL IMPULSE It measures < 2.5 cm and occupies only one interspace in a patient on supine position It is larger in left side lying position; however, a diameter >3cm indicates LV enlargement Cardiac pulsations that are seen lateral to the left midclavicular line often denotes cardiac enlargement Conditions that may cause Left cardiac displacement: o left pulmonary fibrosis o right-sided tension pneumothorax o massive pleural effusion o absent left pericardium o thoracic deformity LOWER STERNAL AREA Region where you can feel the right ventricle however any considerable outward movement in this area is usually due to RV enlargement. Normal RV does not produce a palpable thrust. Presence of palpable thrust may indicate: o mitral stenosis o pulmonic stenosis/regurgitation o tricuspid stenosis/regurgitation o right to left shunts o pulmonary hypertension from any cause Hyperdynamic state of lower sternal area indicates: o Pregnancy o Anemia o Thyrotoxicosis o Fever o Anxiety UPPER STERNAL AREA Left Upper Sternal Border (LUSB) o Pulmonary area o Pulsations in this area are seen in or felt normally in children and thin chested adults o Abnormal pulsations may be due to: dilated pulmonary artery post stenotic dilatation(PS) Page 2 of 13 It’s always darkest before the dawn. ☀ MEDICINE 1: CARDIAC PHYSICAL EXAMINATION increased pulmonary flow (Atrial Septal Defect, Ventricular Septal Defect) pulmonary hypertension (LV failure, mitral stenosis, primary pulmonary hypertension) Right Upper Sternal Border (RUSB) o Aortic area o Seldom presents as obvious pulsations o Dilatation of the ascending aorta o Abnormal pulsations may be due to: Atherosclerosis post stenotic dilatation aortic regurgitation dissecting aneurysm COARCTATION OF THE AORTA STERNOCLAVICULAR AREA Not employed Palpation is used rather than percussion to estimate heart size rarely pulsate, but when they do, it is a sign of aortic disease like: o Dissecting aneurysm o tortuous innominate artery o right sided aorta o Aortic regurgitation o any form of aortic aneurysm Posterior intercostal arteries (enlarged arteries) may be visible and palpable. PERCUSSION AUSCULTATORY AREAS EPIGASTRIUM Pulsations felt in this area are either: o Aortic o Hepatic o Right ventricular Abdominal aortic pulsation is frequently visible over the epigastrium in: o Children o Persons with a scaphoid abdomen Abnormal pulsations may be due to: o Abdominal aneurysms o Aortic regurgitation o Right ventricular hypertrophy and dilation o Tricuspid regurgitation may cause liver pulsation in systole o Liver pulsation late in diastole may indicate: tricuspid stenosis severe RV failure pulmonary hypertension Erb’s point is the auscultation location for heart sounds and heart murmurs located at the third intercostal space and the left lower sternal border. Page 3 of 13 It’s always darkest before the dawn. ☀ MEDICINE 1: CARDIAC PHYSICAL EXAMINATION AUSCULTATION STETHOSCOPE: Ask the patient to sit up, lean forward, exhale completely and stop breathing in expiration Heart Sounds The Bell Chestpiece For low frequency sounds Ex. Diastolic murmurs through mitral and tricuspid valves, S3 and S4 o Q: How much pressure should be applied to the bell chestpiece? o A: Just enough to prevent room noise leak. Any more pressure tightens the skin and tends to damp out the low frequencies and make the bell function like a diaphragm The Diaphragm To damp low frequencies and unmask high frequencies Soft high frequency aortic and pulmonary blowing diastolic murmurs and soft mitral regurgitation murmurs, pericardial friction rubs, S1 and S2 Splitting of first and second heart sounds and nonejection clicks Patient Positions Listen to the precordium with the patient supine, turned on the left side and sitting upright Lying on the left side bringing the ventricle closer to the chest wall. Place the bell of your stethoscope lightly on the apical impulse Ventricular systole is defined by the interval between the first (S1) and second (S2) heart sounds The first heart sound (S1) includes mitral and tricuspid valve closure Normal splitting can be appreciated in young patients and those with right bundle branch block, in whom tricuspid valve closure is relatively delayed Aortic and pulmonic valve closure constitutes the second heart sound (S2) With normal or physiologic splitting, the A2–P2 interval increases with inspiration and narrows during expiration. The third heart sound (S3) occurs during the rapid filling phase of ventricular diastole o present in normal subjects up to the ages of 2030, they represent pathology in older patients A left-sided S3 is a low-pitched sound best heard over the left ventricular (LV) apex S3 - associated with left ventricular failure and is caused by blood from the left atrium slamming into an already overfilled ventricle during early diastolic filling A right-sided S3 is usually better heard over the lower left sternal border and becomes louder with inspiration The fourth heart sound (S4) occurs during the atrial filling phase of ventricular diastole and indicates LV presystolic expansion S4 - created by blood trying to enter a stiff, noncompliant left ventricle during atrial contraction. (left ventricular hypertrophy) Location of maximal intensity o Site where the murmur originates o Where you hear the murmur best Page 4 of 13 It’s always darkest before the dawn. ☀ MEDICINE 1: CARDIAC PHYSICAL EXAMINATION Radiation or transmission from the PMI o Reflects the site of origin, intensity of the murmur and direction of blood flow Intensity - Graded on a 6-point scale and expressed as a fraction Pitch – high, medium or low Quality – blowing, harsh, rumbling and musical Often related to blood flow across the semilunar valves Murmurs Holosystolic Starts with S1 and stops at S2 without a gap between heart murmur and heart sounds Often occur with regurgitant (backward) flow across the atrioventricular valves Heart murmurs - caused by audible vibrations that are due to increased turbulence from accelerated blood flow through normal or abnormal orifices, flow through a narrowed or irregular orifice into a dilated vessel or chamber, or backward flow through an incompetent valve or a congenital defect Timing within the cardiac cycle o Systolic murmurs begin with or after the first heart sound (S1) and terminate at or before the component (A2 or P2) of the second heart sound (S2) that corresponds to their site of origin (left or right, respectively). o Diastolic murmurs begin with or after the associated component of S2 and end at or before the subsequent S1. o Continuous murmurs are not confined to either phase of the cardiac cycle but instead begin in early systole and proceed through S2 into all or part of diastole The accurate timing of heart murmurs is the first step in their identification. The distinction between S1 and S2 and, therefore, systole and diastole is usually a straightforward process but can be difficult in the setting of a tachyarrhythmia, in which case the heart sounds can be distinguished by simultaneous palpation of the carotid upstroke which should closely follow S1. Late systolic murmur Starts in mid or late systole and persists up to S2 Murmur of mitral valve A. Systolic Murmurs B. Diastolic Murmurs Midsystolic murmur Begins after S1 and stops before S2 Brief gaps are heard between the murmur and heart sounds Early diastolic murmur Starts after S2 without a discernible gap and then fades before S1 Page 5 of 13 It’s always darkest before the dawn. ☀ MEDICINE 1: CARDIAC PHYSICAL EXAMINATION Shape determined by its intensity overtime Mid-diastolic murmur Starts a short time after S2 and then fade away Reflect turbulent flow across the atrioventricular valves Late diastolic (presystolic) murmur Starts late in diastole and continues up to S1 Reflect turbulent flow across the atrioventricular valves o Crescendo – grows louder (Ex. presystolic murmur of MS) o Decrescendo – grows softer (Ex. Early diastolic murmur of AR) o Crescendo-decrescendo – rise in intensity then falls (Ex. Midsystolic murmur of AS and innocent flow murmurs) o Plateau murmur – same intensity throughout (Ex. Pansystolic murmur of MR) Page 6 of 13 It’s always darkest before the dawn. ☀ MEDICINE 1: CARDIAC PHYSICAL EXAMINATION Principal Causes of Heart Murmurs Continuous murmurs can be: o Physiological- murmurs occurring only without any structural abnormality at that level (mammary soufflé heard during pregnancy or cervical venous hum most commonly heard in sitting position, in the supraclavicular fossa, in healthy children) o Pathological- secondary to changes that allow the passage of blood from a high pressure area into a low pressure area, or increased resistance in the arterial circulation by a severe fixed arterial stenosis Benign vs Pathologic Murmurs Benign Asymptomatic Benign murmurs have normal peripheral pulses, without evidence of palpable ventricular enlargement (heaves/lifts or a laterally displaced point of maximal impulse) or thrills Heart sounds are key: diagnosis of a benign murmur should be made in the context of normal splitting heart sounds, without gallops, clicks, or snaps early to mid-systolic Page 7 of 13 It’s always darkest before the dawn. ☀ MEDICINE 1: CARDIAC PHYSICAL EXAMINATION Gradations of Murmur GRADE I – very faint, may not be heard in all positions GRADE II – quiet, but heard immediately after placing the stethoscope on the chest GRADE III – moderately loud GRADE IV – loud with palpable thrill GRADE V – very loud, with thrill. Maybe heard with the stethoscope partly off the chest GRADE VI – very loud, with thrill. Maybe heard with the stethoscope entirely off the chest • • • • Duration • • • Timing hyperthyroidism severe anemia Pressure overload of the LV (aortic stenosis) volume overload of the LV (mitral regurgitation) Sustained high-amplitude impulse that is normally located suggests LVH from pressure overload Laterally displaced – volume overload Sustained low-amplitude – dilated heart of cardiomyopathy Sustained Low Amplitude Timing o Systolic murmur – falling between S1 and S2 o Diastolic murmur – falling between S2 and S1 o Murmurs that coincide with the carotid upstroke are systolic o Systolic murmurs - usually midsystolic or pansystolic May occur in normal hearts Location of Maximum Intensity of Common Systolic Murmurs Amplitude Small and feels like a gentle tap Increased amplitude: Page 8 of 13 It’s always darkest before the dawn. ☀ MEDICINE 1: CARDIAC PHYSICAL EXAMINATION YELLOW- Aortic stenosis PURPLE- Pulmonic Stenosis GREEN- Tricuspid Regurgitation RED-Mitral Regurgitation Diastolic Murmurs in Valvular Heart Disease Systolic Murmurs in Valvular Heart Disease AORTIC AREA= Aortic Regurgitation PULMONIC AREA= Pulmonic Regurgitation TRICUSPID AREA= Tricuspid Stenosis MITRAL AREA= Mitral Stenosis, Atrial Myoma MANEUVERS Changes in position, such as squatting, sudden standing, the valsalva maneuver, and hand gripping can all influence the aforementioned characteristics of a murmur by changing the preload, afterload, and chamber size This is an invaluable tool because murmur characteristics often overlap, and these maneuvers can result in predictable changes. Page 9 of 13 It’s always darkest before the dawn. ☀ MEDICINE 1: CARDIAC PHYSICAL EXAMINATION Inspiration can accentuate right-sided murmurs such as tricuspid regurgitation, but not left-sided murmurs A. Isometric handgrip (30 seconds) Increase afterload and preload; however, it appears as though afterload is increased proportionally more than preload. Hence, this maneuver is most useful for discerning mitral valve regurgitation from aortic stenosis. o This maneuver decreases the pressure gradient across the aortic valve, and thus decreases the intensity of the aortic stenosis murmur; similarly, a regurgitant mitral valve will see increased backward blood flow because of the increased forward resistance encountered by the pumping left ventricle, and so its intensity will increase B. Sudden standing from a supine position Gravity will decrease venous return to the heart (decreases preload -- decrease in diastolic and stroke volumes - decrease in blood pressure) (blood pressure = heart rate x stroke volume x systemic vascular resistance). The heart compensates by increasing the heart rate to maintain blood pressure. There are more heartbeats, but less blood flow per beat, and thus most systolic murmurs will decrease in intensity The important exception is hypertrophic cardiomyopathy, where the murmur increases in intensity - because the murmur is due to the narrowing of the left ventricular outflow tract C. Squatting from an erect/standing position The muscle contractions caused by squatting literally squeeze venous blood to the heart, thus increasing preload Muscle contractions also compress arterioles and thus increase systemic vascular resistance (afterload) In this case, most systolic murmurs will increase in intensity because the ventricles will have a higher diastolic and stroke volume. Hypertrophic cardiomyopathy - decrease in intensity because the outflow tract becomes wider Murmur of aortic stenosis may not become accentuated because squatting may increase afterload more so than preload, thereby dissipating its transvalvular pressure gradient Tetralogy of fallot, an increased venous return will cause an increased pressure gradient through the pulmonary valve, increasing the intensity of its pulmonary stenosis murmur VALSALVA MANEUVER Straining phase of the valsalva - best for analyzing murmur Raises intrathoracic pressure, which compresses the caval veins and decreases venous return to the heart, and thus decreases stroke volume. This in turn leads to a compensatory increase in heart rate. This causes similar findings to sudden standing from a supine position Patient in the lateral decubitus position (tends to accentuate mitral murmurs because it brings the left ventricle closer to the stethoscope) Exercise can accentuate holosystolic murmurs such as mitral regurgitation and VSD, but not tricuspid regurgitation Palpating continuous murmurs: a venous hum disappears with compression of the internal jugular vein; a mammary soufflé murmur disappears with pressure from a stethoscope. ** SEE ADDENDUM FOR THE TABLE A diastolic murmur is never benign The higher the intensity (i.e. grade 4 or more) the more likely it is pathological Benign murmurs change significantly with different patient positions Finally, if investigations are performed they should reveal no abnormalities on ECG, CXR, echocardiogram, or other imaging modalities Page 10 of 13 It’s always darkest before the dawn. ☀ MEDICINE 1: CARDIAC PHYSICAL EXAMINATION JUGULAR VENOUS PRESSURE JVP is the single most important bedside measurement from which to estimate the volume status Internal jugular vein is preferred because the external jugular vein is valved and not directly in line with the superior vena cava and right atrium. Venous pressure traditionally has been measured as the vertical distance between the top of the jugular venous pulsation and the sternal inflection point (angle of Louis) A distance >4.5 cm at 30° elevation is considered abnormal Normally, JVP falls with inspiration due to reduced pressure in the expanding thoracic cavity and the increased volume afforded to right ventricular expansion during diastole Kussmaul sign suggests impaired filling of the right ventricle due to either fluid in the pericardial space or a poorly compliant myocardium or pericardium. This impaired filling causes the increased blood flow to back up into the venous system, causing the jugular vein distension (JVD) and is seen clinically in the internal jugular veins becoming more readily visible Kussmaul’s sign - either a rise or a lack of fall of the JVP with inspiration and is classically associated with constrictive pericarditis Also reported in patients 1. restrictive cardiomyopathy, massive pulmonary embolism, right ventricular infarction, and advanced left ventricular systolic heart failure Pulsus paradoxus is measured by noting the difference between the systolic pressure at which the Korotkoff sounds are first heard (during expiration) and the systolic pressure at which the Korotkoff sounds are heard with each heartbeat, independent of the respiratory phase Pulsus paradoxus - refers to a fall in systolic pressure >10 mmHg with inspiration that is seen in patients with pericardial tamponade but also is described in those with massive pulmonary embolism, hemorrhagic shock, severe obstructive lung disease, and tension pneumothorax Page 11 of 13 It’s always darkest before the dawn. ☀ MEDICINE 1: CARDIAC PHYSICAL EXAMINATION Abdomino-Jugular Reflux Normally the jugular venous pressure rises with expiration and falls with inspiration as the negative intrathoracic pressure increases Paradoxical venous filling or Kussmaul sign – veins fill with inspiration and empty with exhalation. In normal persons, jugular venous pressure rises less than 3 cm H2O and only transiently while abdominal pressure is continued, whereas in right or left ventricular failure or tricuspid regurgitation the jugular venous pressure remains elevated Occurs in: cardiac failure, cardiac tamponade from pericardial effusion, hemopericardium a heartbeat or two, before returning to normal. This negative result would be indicated by a lack of swelling of the jugular vein. References Dra. Vicky Turla’s Lecture and PowerPoint Bates’ Guide to Physical Examination and History Taking 12th Edition Braunwald: Heart Disease: A Textbook of Cardiovascular Medicine, 6th ed. Harrison’s Principle of Internal Medicine 19th ed. Batch 2019’s Transcription Technique for Examining Hepatojugular Reflux (HJR) Hepatojugular reflux is the distention of the neck veins precipitated by the maneuver of firm pressure over the liver. It is seen in tricuspid regurgitation, heart failure due to other non-valvular causes, and other conditions including constrictive pericarditis, cardiac tamponade, and inferior vena cava obstruction. The HJR maneuver may be performed as follows: 1. The patient is positioned supine with an elevation of the head at 45 degrees. 2. Look at the jugular pulsations during quiet respirations. (baseline JVP) 3. Apply gentle pressure (30-40 mmHg) over the right upper quadrant or middle abdomen for atleast 10 seconds. 4. Repeat the JVP. 5. An increase in JVP of >3cm is a positive HJR Test. NOTE: Normal subjects will have a decrease in JVP with this maneuver since venous return to heart is reduced. The jugulars venous pressure may transiently rise then return to normal or decease within 10 seconds. The clinician presses firmly over either the right upper quadrant of the abdomen or over the center of the abdomen for 10 seconds with a pressure of 20 to 35 mm Hg while observing the swelling of the internal jugular vein in the neck and also observing to be sure the patient does not perform a Valsalva maneuver On an otherwise healthy individual, the jugular venous pressure remains constant or temporarily rises for Page 12 of 13 It’s always darkest before the dawn. ☀ MEDICINE 1: CARDIAC PHYSICAL EXAMINATION ADDENDUM Diagram of Principal Heart Murmurs Page 13 of 13 It’s always darkest before the dawn. ☀