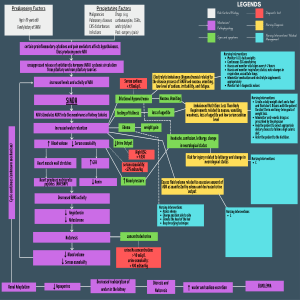
EMORY INTERNAL MEDICINE RESIDENCY: INTERN GUIDEBOOK VISUAL SERIES Sodium Hyponatremia Hyponatremia is usually caused by the inability to excrete water normally. In the vast majority of cases, ADH (appropriately or inappropriately secreted) is the culprit. Always start with a good history and exam, paying particular attention to volume status. Then, ask 3 questions to work through a physiologic approach to the differential! 1 Is it hypotonic? Calculate serum osmolality! Serum osmolality = (2 x [Na]) + ([BUN] / 2.8) + ([Glucose] / 18) Hypotonic Isotonic Hypertonic serum Osm <275 serum Osm 275-295 serum Osm >295 True hypoNa Go to step 2! ↑ Lipids (TGs) Paraproteinemia Mannitol Pseudohyponatremia Glucose Correction standard assays to measure [Na], resulting in a falsely low [Na] When [Glu] is ↑, add ~2 mEq/L to [Na] for every 100 mg/dL of glucose over 100 ↑ lipids/proteins in serum interfere with 2 Glucose Is ADH elevated? Measure urine osmolality! Urine osm is the best marker of ADH activity. However, because hypoNa is often multifactorial in etiology and treatment commonly administered prior to complete workup, most patients will have urine osm >100. Dx Often a UA can estimate urine osm - multiply SG decimals by 30,000 (SG = 1.010: 0.010*30000 = 300 osm)! Urine osm can also be helpful to monitor response to treatment as a decrease indicates suppression of ADH. 3 ↓ ADH ↑ ADH urine osm <100 urine osm >100 Iatrogenic Abnormal Intake hypotonic IVF surgery (e.g., hypotonic fluids from hysteroscopy/cystoscopy) ↑ water (polydipsia) ↓ solute (tea & toast, beer potomania) Go to step 3! Is it appropriate? Assess volume status (EABV)! While the volume status exam is vital, it can be challenging in patients who are not overtly hyper/hypovolemic. Recall ↓ EABV (real or perceived) often drives the process, so it is helpful to augment the exam with lab signs of ↓ EABV: ↓ GFR (↑ BUN, Cr, serum uric acid), ↑ aldosterone (↓ urine Na), hemoconcentration (↑ Alb, Ca, Hct). In patients not on diuretics, ↓ urine Na (<20) indicates ↓ EABV (real or perceived). In the case of diuretic use, uric acid is helpful as ↓ serum uric acid and ↑ urine uric acid points away from ↓ EABV and towards SIADH! Hypovolemic Euvolemic Hypervolemic ↓ EABV Appropriate ↑ ADH Normal EABV Inappropriate ↑ ADH Perceived ↓ EABV Appropriate ↑ ADH GI loss Renal loss Insensible Hypothyroidism Adrenal insufficiency SIADH Heart failure Liver failure Renal failure Common causes of SIADH include drugs (e.g., SSRIs), surgery, CNS disturbances, and pulmonary disease. Volume resuscitation & tx underlying cause Tx Fluid restriction & tx underlying cause Diuresis & tx underlying cause Treatment of hyponatremia is a complex issue which varies based on chronicity and severity. Generally, treat the underlying cause and avoid rapid correction (max rate of correction 8 mEq/L/day) Rapid correction of chronic hyponatremia puts patients at risk for osmotic demyelination syndrome. 3% saline can be administered (through a peripheral IV!) in 100 mL boluses over 10 minutes up to 3x in the setting of symptomatic (seizures, obtundation, coma, respiratory arrest) hyponatremia. Other options for severe/refractory hypoNa include vaptans (HF/liver dz) and augmentation with DDAVP may be required.* Hypernatremia Hypernatremia is almost always due to unreplaced water loss (free water deficit). The differential can be broadly placed into 4 categories. Diagnosis is primarily based on history, exam, and urine osm (in DI; high dilute urine output is a clue). Dx 1 2 3 4 ↓ Water Intake Dehydration Osmotic Diuresis Diabetes Insipidus ↑ Salt Intake neurologic dz water unavailable HHS postobstructive neurogenic nephrogenic salt water hyper/isotonic saline Note that dehydration and hypovolemia are distinct phenonema. Dehydration refers to the loss of pure water, which is lost evenly from all body compartments freely permeable to water. Hypovolemia refers to the loss of ECF volume. It implies the loss of sodium, in addition to water and consequently poses a greater risk of circulatory compromise than dehydration. Tx Treatment of hypernatremia can also be complex and varies with chronicity and severity. Start by calculating the free water deficit (FWD) = Total Body Water (TBW) x (([Na] / 140) - 1) Total body water is 50-60% of patient weight (e.g., 0.5-0.6 x pt weight). Generally, the treatment will involve resuscitation with isotonic fluids followed by free water. Free water can be delivered with D5 fluids or enteral free water flushes. Rapid correction of chronic hypernatremia puts patients at risk for cerebral edema and herniation. The maximum rate of correction should not exceed 12 mEq/L in a 24-hour period. Created by: David Rink, MS4 (@de_Rink) Meredith Greer, MD (@EmmGeezee) Kerryn Roome, MS4 (@KerrynRoome) Caroline Coleman, MD (@cg_coleman) References: Chung HM, Kluge R, Schrier RW, Anderson RJ. Am J Med. 1987 Nov;83(5):905-8. Hoorn EJ, Lindemans J, Zietse R. Nephrol Dial Transplant. 2006 Jan;21(1):70-6. Milionis HJ, Liamis GL, Elisaf MS. CMAJ. 2002;166(8):1056-1062. Decaux G, Dumont I, Waterlot Y, Hanson B. Nephron. 1985;39(3):164-8. *https://emcrit.org/ibcc/hyponatremia/#rapidly_reversible_cause_-_DDAVP_clamp