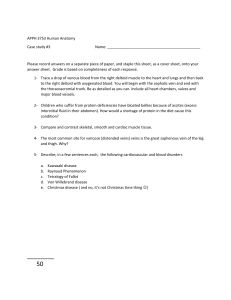
lOMoARcPSD|35970034 Prelim- Midterms Lessons PMLS 2 Lecture Medical Laboratory Science (Davao Doctors College) Scan to open on Studocu Studocu is not sponsored or endorsed by any college or university Downloaded by Makyxazo Premium (xonemo@pelagius.net) lOMoARcPSD|35970034 LESSON 1: PHLEBOTOMY UNDERSTANDING WHAT IS PHLEBOTOMY? ➢ The process of collecting blood. ➢ Phleb - vein ➢ Tomia (Greek) - cutting ➢ Temnien (Greek) - to cut ➢ Vena (Latin) - vein ➢ Sectio (Latin) - cutting MIDDLE AGE ➢ Dates back to early Egyptians: it was once thought that the practice would rid the body of diseases and provide a cure for almost all ailments. For thousands of years, medical practitioners clung to the belief that sickness was merely the result of a little “bad blood.” With this in mind, patients with a fever or other ailment were often diagnosed with an overabundance of blood. To restore bodily harmony, their doctor would simply cut open a vein and drain the blood. Picture a Roman gladiator bleeding from battle and would receive a treatment of further bleeding. The unfortunate result of the practice became one reason why it did not last very long. ➢ 12th century: blood letting was practiced by barbers (because of their skill with sharp instruments). Barbering was known as a barbersurgeon for 1000 years. They used to perform blood letting, surgery, extracting teeth and herb administration. Thus, the red and white poles. ➢ Dec 1799: George Washington, the first pres of US, had a severe throat infection. The cure that was used as an intervention was massive bleeding. He bled more than 9 pints of blood in less than 24 hours and died on Dec 14. after his death, the philosophy of bleeding as a cure to diseases changed. ➢ Mid 19th century: blood letting was no longer considered a cure of illness (man in picture right most is anton van leeuwenhoek) ➢ The discovery of microorganisms as the causative agent for many diseases started to change the way they treat diseases. Blood began to be examined for diagnostic purposes. ➢ Venesection - most common; a sharp lancet-like instrumtion that pulled blood to the capillaries under the cup. Then a spring-loaded box containing multiple blades cut the area to produce massive bleeding. Both methods produced much scarring ➢ Leeching (Hirudotherapy) - more modern method was to use leeches Ex. When a person’s finger is reattached after accidental amputation, the arteries and veins do not return to normal blood flow immediately. The blood tends to pool at the end of the finger, thereby causing pain and pressure. The leech is placed on the end of the finger to remove excess blood and relieve the symptoms. The only problem is that leeches get full fast so you need to change it after several hours. Bleeding of individuals to reduce the amt of blood does occur today to treat diseases like polycythemia vera and hereditary hemochromatosis. It is called “therapeutic phlebotomy”. Blood is still removed to cure the person, but it is primarily done to FIND a cure, not as the cure itself. Blood as changed from being therapeutic to being diagnostic. Thousands of different types of diagnostic tests are available. ➢ Fleams - are used to puncture vessels and then allow excess blood to drain out of the body. ➢ Bloodletting - medicine’s oldest practice. ➢ Over abundance of blood or plethora is known as the cause of illness. Centralized Phlebotomy (85% of hospitals) The phlebotomist is part of the laboratory team is dispatched to hospital units to be collected blood samples. Sample collection wherein the phlebo is part of the lab team and is dispatched to hospital units to collect blood samples rounds per hour then process samples. Decentralized Phlebotomy (15% of hospitals) Patient-focused care. The duties of the hospital revolve more than around the patient. it is easier to use the people who are already working. The nurse needs to learn phlebo and the phlebo needs to learn nursing duties; called “patientfocused care”, the duties of the hospital staff revolve more than around the patient; job is not restricted to one duty; “patient care technician”. Hybrid Phlebotomy Blend of centralized and decentralized. send lab-based phlebo to nursing units for blood collection and keep some phlebo available to help patient care technicians for diff draw. ANCILLARY HOSPITAL AREAS ● Administration - keeps the hospital in compliance ● Electrocardiography - monitors patients with cardiovascular disease ● Electroencephalography diagnosis of neurophysical disorders Downloaded by Makyxazo Premium (xonemo@pelagius.net) lOMoARcPSD|35970034 ● ● ● ● ● ● ● ● ● ● ● ● Environmental services - maintains a clean facility Food services - provides diets to patients GI lab - diagnosing gastrointestinal disorders Laboratory - provides testing of patient samples Medical records - maintains patient records Nursing - provides direct patient care Occupational Therapy - provides therapy to help maintain livings skills Pharmacy - dispenses drugs and advises drug usage Physical Therapy - provides therapy to restore mobility Radiology - uses imaging for diagnosis and treatment Respiratory Therapy - provides therapy to evaluate the lungs Speech therapy - provides therapy to retore speech AREAS OF NURSING CARE ● Coronary Heart Unit - increased care of patient due to heart condition ● Emergency department - emergency treatment ● Geriatric - elderly patients ● Intensive Care Unit - increased care due to critical needs of the patient ● Neonatal - newborn care ● Nephropathy - patients on dialysis ● Obstetrics - patients in labor of childbirth ● Oncology - patients with cancer ● Orthopedic - patients with broken bones ● Pediatrics - infants and children ➢ Recovery - recovery treatment of patientsent pierced the veins and made them bleed ➢ Cupping - heated glass cup was placed on a person’s back. As the cup cooled, it created a suc LABORATORY SECTIONS 1. Administrative Office. Does the paper works, responds to calls, handles specimen collection requests. 2. Phlebotomy. Collect sample from patients and processes samples for testing and transport 3. Urinalysis. Study of urine and other body fluids. Performs quali and quanti chemical and microscopic exam of urine to detect UTI, diabetes, kidney or liver diseases. 4. Hematology. Studies blood in normal and diseased states. Usually limited to the study of cellular components and not the chemistry of blood. Studies blood cells and performs qualitative and quantitative analysis along w/ microscopic evaluations. Ex. CBC, RBC count, WBC count, Hemoglobin, Hematocrit, Platelet count, Sedimentation rate, Body fluid cells counts 5. Coagulation. Study of blood clotting mechanisms. Or hemostasis Usually the same area as hematology Study of the clotting of blood. Ex. PT, aPTT, factor VIII, Fibrinogen assay, Heparin level, vWF 6. Clinical Chemistry. Performs biochemical analysis of blood and body fluids. Works with the fluid portion of the blood (Serum/Plasma) or other body fluids. Performs biochemical analysis. In most procedures: Sample is added to various chemicals and a color or chemical change occurs. Ex. Metabollic panel, Hepatic panel, Renal panel, Iron studies, Glucose, Cholesterol, Enzymes, The intensity of color produced means the more glucose is in the blood 7. Microbiology. Cultures samples to determine if pathogenic organisms are present in a sample. Determines organism’s antibiotic susceptibility. 8. Immunology. Studies antigen and antibody to determine immunity or presence of disease. Antigens- substances that are foreign to the body Antibodies- proteins made by the body to combat antigens. Ex. HIV testing, Rubella, RPR, VDRL, Hepatitis testing 9. Blood Banking. Determines compatability of blood and blood products to be administered to the patient. Ex. Crossmatching, ABO blood typing, Rh typing, antibody panel testing 10. Cytogenetics. Study of deficiencies related to genetic diseases Ex. Chromosome analysis, prenatal chromosome screening 11. Molecular Diagnosis. Using PCR technologies to study the presence of various diseases and infections. Ex. MRSA infections, HIV testing 12. Histopathology. Examines tissues and cell smears for evidence of cancer, infection or other abnormalities. 13. STAT Requests. Emergency cases. Tested individually, not wait for batch processing. 14. Out Patient Department. Patients who are not admitted in the hospital. Lab aims to achieve the least turn around time. LABORATORY STAFF 1. Pathologist. Reads and interprets result. Examines tissues under microscope. Requires 5 years of training after graduating from medschool to be eligible to be a certified pathologist. 2. Medical Laboratory Scientist. Performing wide range of laboratory tests. Confirming and reporting laboratory tests. Holds a minimum of baccalaureate degree in MLS. - - varying job description from one health care facility to the other cross trained for: venipuncture, capillary collection, patient care, receptionist duties, sample processing and computer work traditional role of phlebotomist is only one job: TO Downloaded by Makyxazo Premium (xonemo@pelagius.net) lOMoARcPSD|35970034 COLLECT BLOOD SAMPLES 3. Medical Laboratory technician. Under the supervision of Med Lab Sci. Performs general tests. Cannot release result. Depends on board rating. Need special training aside from hs diploma. 4. Phlebotomy technician. Collect blood samples 5. Histotechnologist. Prepares body tissue samples for microscopic evaluation of pathologist. PHASES OF SAMPLE PROCESSING Pre-examination ● Request form ● Patient identification and information ● Correct sample collection ● Correct use of all equipment ● Sample preparation and centrifugation ● Maintaining sample integrity until processing Examination ● Sample testing ● Maintaining testing equipment and reagents Post-examination ● Reporting of results ● Ensuring accuracy and reliablity of the delivery of the result ● Follow-up if repeat testing is needed or attend to other needs of the physician ● Storage of sample after processing LESSON 2: INFECTION CONTROL Downloaded by Makyxazo Premium (xonemo@pelagius.net) lOMoARcPSD|35970034 WHAT IS INFECTION CONTROL? ➢ Prevention of nosocomial or health care associated infections. Controlling the spread of disease and minimizing the number of healthcare-associated infections. ➢ Infection control is the discipline concerned with preventing nosocomial or healthcare-associated infections. It is about identifying and controlling the factors involved with the spread of these infections, whether from patient-to-patient, from patients to staff, from staff to patients, or among-staff. FACTORS ● Prevention ● Monitoring/Investigation ● Surveillance, Investigation and Management (Hand Hygiene, Contact Tracing, Asset Management, Medical Scope Management, Enviornmental Monitoring, Surgical Sterile Processing) NOSOCOMIAL VS. COMMUNITY ACQUIRED INFECTION Nosocomial Infection ➢ Infections contracted within hospital or those becoming clinically apparent til the discharge of the patient or infections contracted by the healthcare professionals as a result of their direct or indirect contact with the patients. ➢ The patient contracts the disease during the hospital stay. Community Acquired Infection ➢ Infections that are contracted outside the hospital or those who become clinically apparent within 48 hours from the hospital admission are community acquired infections. ➢ The disease is contracted by the patient before getting admitted to the hospital. CHAIN OF INFECTION ● Agent ● Reservoir ● Portal of Exit ● Mode of Transmission ● Portal of Entry ● Susceptible Host PERSONAL PROTECTIVE EQUIPMENT ● Lab Gown - Adds an additional layer of protection for skin. ● Gloves - Avoid direct contact to highly infectious agents. ● ● ● ● ● ● ● Mask - Required when drawing blood from patients with transmissible diseases. Goggles - Protects eyes from spills and splashes. Long hair must be tied back. Long pants that cover ankle. Shirts that cover your torso are required. Crop tops are not allowed. Natural fibers are recommended because they are fire resistant. Shoes completely enclose the foot and can be wiped clean. DIFFERENT TYPES OF MASKS ● N95 (Strongest protection) ● Surgical Mask (Medical use) ● FFP1 Mask (Filtere suspended particles) ● Activate Carbon (Stops odor) ● Cloth Mask (DIY) ● Sponge Mask (Fashion use) HAND HYGIENE 1. Before touching a patient 2. Before clean/aseptic procedure 3. After body fluid exposure risk 4. After touching a patient 5. After touching patient sorroundings ISOLATION Isolation precautions should be used for patients who are either known or suspected to have an infectious disease, are colonised or infected with a multi-resistant organism or who are particularly susceptible to infection. isolation procedures separate certain patients from others and limit tHeir contact with hospital personnel and visitors. It is important that standard precautions are implemented at all times and all patients must be assessed on admission to ensure that they are placed in appropriate isolation if necessary. 1. Source Isolation - when patients with contagious disease are placed into a room to protect other people from becoming infected. Isolation rooms are usually under negative pressure to prvent room air from entering the hallway. Air evacuated from the room passes through a HEPA filter. 2. Protective isolation protect an immunocompromised patient who is at high risk of acquiring microorganisms from either the environment or from other patients, staff or visitors. Positive room air pressure relative to corridors, along HEPA filtration of incoming air at >12 air changes per hour. Also recommended for allogeneic hematopoietic stem cell transplant Downloaded by Makyxazo Premium (xonemo@pelagius.net) lOMoARcPSD|35970034 patients. STANDARD PRECAUTIONS Are used in the care of all hospitalized persons regardless of their diagnosis or possible infection status. Tthey apply to blood, all body fluids, secretions and excretions, except sweat (whether or not blood is present or visible), broken skin, and mucous membranes. Designed to reduce the risk of transmission of microorganisms from recognized and unrecognized sources. TRANSMISSION-BASED PRECAUTIONS ● AIRBORNE PRECAUTIONS - designed to reduce the risk of infection that can be spread through the air transmission occurs when tiny droplets or dust containing the infected agent are suspended in the air for long periods. The agent can float in the air currents of the facility and can be inhaled by or deposited on a susceptible person. ● DROPLET PRECAUTIONS - designed to reduce the risk of infection that can be spread when the infected droplet contacts the eyes, nose or mouth of a susceptible person. These are large droplets and only travel a short distance before falling to the ground, usually about 3 feet. - the mask used for droplet precautions is for one time use and to be disposed of in the patient room. Do not reuse. ● CONTACT PRECAUTIONS - designed to reducethe transmission risk of epidemiologically important micro-organisms by direct or indirect contact. - contact involves dry or moist substances and physical transfer of microorganism from an inanimate object to a susceptible person. - when patient is in contact precautions: keep door closed, upon entering room don gloves and gown if you might have contact with patient or environment. - place in regular room to reduce the risk of infection that can be spread when the infected droplet contacts the eyes, nose or mouth of a susceptible person. These are large droplets and only travel a short distance before falling to the ground, usually about 3 feet. - The mask used for droplet precautions is for one time use and to be disposed of in the patient room. Do not reuse. LESSON 3: CIRCULATORY SYSTEM Downloaded by Makyxazo Premium (xonemo@pelagius.net) lOMoARcPSD|35970034 WHAT IS A CIRCULATORY SYSTEM? ➢ An organ system that permits blood to circulate and transports nutrient, oxygen, carbon dioxide, hormones, and blood cells to and from the cells in the body to provide nourishment and help in fighting diseases, stabilize temperature and pH, and maintain homeostasis. ➢ It includes the Pulmonary Circulation and Systemic Circulation. ➢ The circulatory system is centered on the HEART, a muscular organ that rhythmically pumps BLOOD around a complex network of BLOOD VESSELS extending to every part of the body. ➢ Blood carries the oxygen and nutrients needed to fuel the activities of the body’s tissues and organs, and it plays a vital role in removing the body’s waste products. An average-sized adult carries about 5 litres (9 pints) of blood. PULMONARY CIRCULATION A "loop" from the heart through the lungs where blood is oxygenated. Sends oxygen-depleted (deoxygenated) blood away from the heart through the pulmonary artery to the lungs and returns oxygenated blood to the heart through the pulmonary veins. RIGHT ATRIUM - the upper chamber of the right side of the heart. The blood that is returned to the right atrium is deoxygenated (poor in oxygen) and passed into the RIGHT VENTRICLE to be pumped through the PULMONARY ARTERY to the lungs for re-oxygenation and removal of carbon dioxide. PULMONARY ARTERY - this artery divides above the heart into two branches, to the right and left lungs, where the further subdivide into smaller and smaller branches until the capillaries in the pulmonary air sacs (alveoli) are reached. In the capillaries the blood takes up oxygen from the air breathed into the air sacs and releases carbon dioxide. It then flows into larger and larger vessels until the PULMONARY VEINS. PULMONARY VEINS usually four in number, each serving a whole lobe of the lung. The pulmonary veins open into the LEFT ATRIUM of the heart. LEFT ATRIUM - receives newly oxygenated blood from the lungs ● ● ● ● ● ● ● ● Right Atrium Right Ventricle Pulmonary Artery Pulmonary Arterioles Pulmonary Capillaries Pulmonary Ventricles Pulmonary Veins Left Atrium SYSTEMIC CIRCULATION Provides the functional blood supply to all body tissue. It carries oxygen and nutrients to the cells and picks up carbon dioxide and waste products. - network of veins, arteries and blood vessels that transports blood from heart, services the body's cells and then re-enters the heart. Blood is pumped from the LEFT VENTRICLE of the heart through the AORTA and arterial branches to the ARTERIOLES and through CAPILLARIES, where it reaches an equilibrium with the TISSUE FLUID, and then drains through the venules into the VEINS and returns, via the SUPERIOR AND INFERIOR VENAE CAVAE, to the RIGHT ATRIUM of the heart. ● ● ● ● ● ● ● Left Ventricle Aorta Arteries Tissues Veins Superior and Inferior Vena Cava Right Atrium VASCULAR SYSTEM ➢ Arteries. Oxygen-rich blood (bright red). have thick walls to withstand the pressure of ventricular contraction, which creates a pulse that can be felt, distinguishing them from veins. When arterial blood is collected by syringe, the pressure normally causes blood to “pump” or pulse into the syringe under its own power. ➢ Veins. Oxygen-poor blood (brick red). have thinner walls than the same-size arteries because blood in them is under less pressure. Consequently, they collapse more easily. Blood is kept moving through veins by skeletal muscle movement and the opening and closing of valves that line their inner walls. ➢ Capillaries. Allow the exchange of gases and other substances between the tissues and the blood.only one cell thick. The capillary bed in the skin can easily be punctured with a lancet to provide blood specimens for testing. PHLEBOTOMY-RELATED VASCULAR ANATOMY The major veins for venipuncture are in the antecubital fossa, the area of the arm in front of the elbow. Here, several large veins lie near the surface, making them easier to locate and draw blood from. Although exact locations vary slightly from person to person, two basic patterns in which the veins from the shape of either an H or an M are seen most often. Downloaded by Makyxazo Premium (xonemo@pelagius.net) lOMoARcPSD|35970034 H PATTERN (displayed approximately 70% of the population) ● Medican Cubital Vein - preferred vein for venipuncture in the H pattern because it is typically large, closer to the surface, and the most stationary, making it the easiest and least painful to puncture and the least likely to bruise. - Near the center of the antecubital fossa. - Preferred vein for venicpuncture. ● Cephalic Vein - second-choice vein - although often harder to palpate(feel) than the median cubital, it is fairly well anchored and often the only vein that can be felt in obese patients - Laspect of the antecubutal fossa. ● Basilic Vein - last choice vein - although normally large and easy to feel, it is not well anchored and rolls easily, increasing risk of puncturing a median cutaneous nerve branch or the brachial artery that is nearby - Medial site of the antecubital fossa. venipuncture. Veins on the underside of the wrist, however, should NEVER be used for venipuncture. Leg, ankle, and foot veins are sometimes used but not without permission of the patient’s physician, due to a potential for significant medical condition. M PATTERN ● Median Vein - Center-most vein. - it is the first-choice vein in the M pattern because it is well anchored, tends to be less painful, and is not as close to major nerves or arteries as the others, making it generally safest to puncture. ● Median Cephalic vein - Branches from the medin vein to the lateral aspect of the arm. - it is the second choice M-pattern vein because it is accessible, unlikely to roll, less painful, located far enough away from major nerves or arteries, and generally safe to puncture. ● Median Basilic vein - Branches fromt the median to the medial aspect of the arm. - it is the 3rd choice in the M pattern because, although it may appear more accessible, it is located near the anterior and posterior branches of the median cutaneous nerve Although antecubital veins are used most frequently, veins on the back of the hand and wrist may also be used for LESSON 4: REQUIREMENTS Downloaded by Makyxazo Premium (xonemo@pelagius.net) PHLEBOTOMY lOMoARcPSD|35970034 EQUIPMENTS All methods of venipuncture require an invasive procedure of entering a vein to obtain a blood sample. The syringe and needle method is one of the oldest methods known that does not destroy the integrity of the vein. Syringes are made of glass or plastic (mostly plastic). How to use: 1. Pull the plunger to create a vacuum within the barrel (The plunger on a syringe is often hard to pull. A technique called breathing the syringe needs to be done before it is used. Pull the plunger midway then push it back to make the plunger pull smoothly). 2. The vacuum created while pulling the plunger while a needle is in a patient’s vein fills the syringe with blood (the larger the syringe, the greater blood). A too large vacuum has the tendency to pull too hard on the vein and collapse it. pull the plunger slowly. Syringes are used for difficult to draw veins such as fragile, thin and rolly veins. Needle gauge and needle use: 27: skin tests 25: intramuscular injections (cannot be used for veni bc RBCs will be destroyed when the blood is pulled thru the bore) 23: butterfly or syringe collection (most common for children) 22-20: syringe or ETS collection (21 most common for adults) 18-16: IVs or blood donation A tube with a vacuum already in it attaches to the needle and the tube’s vacuum is replaced by blood. Needle used on a syringe consists of a hub, cannula (shaft) and a bevel. Hub: attached to a syringe (screw the hub) Recommended length of a needle: 1- 1 ½ inch. The gauge of the needle is determined by the diameter of the lumen or opening. Needle gauge is inversely proportional to the needle bore. The bevel must always be facing upward, the opening of the needle should be visible. Parts: 1. Double pointed needle ➢ The needle is a straight hollow type with double points and a screw hub near the center ➢ The needle outside the holder punctures the skin while the needle inside the holder pierces the ➢ rubber stopper of an evacuated tube ➢ The bevel must always be facing upward, the opening of the needle should be visible ➢ The bevel is cut at an angle so as to ensure maximum blood flow thru the needle ➢ Needle should be inserted at 15-30 degree angle ➢ The deeper the vein, the greater angle you will use (superficial vein: 15° deep vein: 30°) 2. Adapter (holder) ➢ Where the phlebo holds 3. Vacuum tubes Downloaded by Makyxazo Premium (xonemo@pelagius.net) lOMoARcPSD|35970034 SPS: allows bacteria to grow so that they can be cultured SERUM: liquid portion of coagulated or clotted blood; fibrinogen and other clotting factors are not present since it is being used up during clotting. PLASMA: liquid portion of anticoagulated blood; fibrinogen and other clotting factors are present since it is not used up because of the presence of an anticoagulant. The liquid portion contains water, proteins (including enzymes and some hormones) and others. RED TOP (plastic): no anticoag but contains silica particles as clot activator RED TOP (glass): no anticoag and additive bc the glass itself serves as a clot activator GOLD TOP: aka serum separator tube; no anticoag but contains a separator gel (thixotropic gel)→ principle: upon centrifugation, the di昀昀erent speci昀椀c gravity will separate the components topmost: serum then gel then formed elements GREEN TOP: heparin is the anticoagulant naturally found in the body, thus, it has the least effect on chemistry tests. Preferred anticoagulant for CC; best for blood gas studies, electrolyte studies. 3 forms of heparin: lithium, sodium and ammonium heparin LIGHT GREEN TOP: aka plasma separator tube LIGHT BLUE TOP: 2 concentrations: 3.2% (0.105M) (preferred) and 3.8% (0.129M). Chelates calcium means that it binds to calcium or forms calcium salts to remove calcium Tube must strictly be filled 100%; blood to anticoagulant ratio is 9:1, if the ratio is not achieved, the results will be invalid. BLACK TOP: blood to anticoagulant ratio is 4:1. Downloaded by Makyxazo Premium (xonemo@pelagius.net) lOMoARcPSD|35970034 LAVENDER TOP: has 3 concentrations ● Plastic (spray-dried): K2 EDTA or dipotassium EDTA (recommended bc it preserves the cell morphology and provides stable microhct result) ● Glass (liquid): K3 EDTA or tripotassium EDTA (commercial name: sequestrene) ● NA2 EDTA or disodium EDTA (commercial name: versene) ● GRAY TOP: also contains an antiglycolytic agent: Sodium fluoride (if not available, iodoacetate can be used as an alternative antiglyco agent) veins are near the skin surface, the winged needle is inserted at a 5 degree angle instead of the usual 15-30 in. ● ● ● ● Other uncommon tubes WHITE TOP OR PEARL TOP: helpful in HIV testing ORANGE TOP: thrombin is the most potent clot activator; used in STAT chemistries bc the optimum clotting time is 510 min. ● ● Applied tight enough to slow the flow of blood in the veins but not prevent the flow of blood in the arteries Modern: do not use latex tourniquets as to avoid latex exposure and allergy Patient should close his or her hand to make the vein prominent (dili mangusog dapat) Palpating vein (one of the most difficult skills to learn): using the finger to press down on top of the vein to feel the “bounce” or running the finger across the arm to feel the “speed bump” Should not be on the arm for more than 1 min; can cause hemoconcentration: increased concentration of cellular compponents in the sample Blood pressure cuff (sphygmomanometer) can be used as an alternative (can be used for obese, pediatric or geriatric px) BUTTERFLY or winged infusion set COLLECTION SYSTEM Holding the plastic wings provide easy access into small surface veins on the back of the hand, the arm or foot. 3-12 inch tubing leads from the needle to a hub that could be attached to either a syringe barrel or evacuated tube needle adapter called luer adapter. When disposing in sharps container, hold the plastic wing and drop the tubing next (so as to prevent needle stick injury bc of the tubing) Since these Downloaded by Makyxazo Premium (xonemo@pelagius.net) lOMoARcPSD|35970034 Cleansing Agents ● Disinfectant - removes or kills micoorganisms and instruments - 10% sodium hypochlorite (best) ● Antiseptic - prevents microorganisms and their toxins from infecting the blood - 70% isopropyl alcohol (most common and best) ● Hand Sanitizer - Alcohol-based rinses, gels and foams - Can replace handwashing if hands are not visibly soiled Microcollect equipment ● Non-spring loaded lancets ● Spring loaded lancets LESSON 1: PROCEDURES VENIPUNCTURE STEPS IN BLOOD COLLECTION: STEP 1: Preparation request form the patient. ● Patient’s complete name ● Age ● Date of birth ● Patient identification number ● Type of test to be collected ● Date and time the sample is to be obtained ● Department or location of the patient ● Clinical impression/diagnosis ● Physician’s name Downloaded by Makyxazo Premium (xonemo@pelagius.net) lOMoARcPSD|35970034 STEP 2: Greet and identify the patient. ● Conscious Patients (out-patient) ● Ask patient to give their full name and spell their last name ● Compare the information on the request form ● ● ● ● ● ● ● Conscious patients (in-patient) ● Ask patient to give their full name and spell their last name ● Compare the information on their identification bracelet and request form ● Sleeping patient ● Awaken a sleeping patient before attempting venipuncture ● If the patient is already awake, do the same steps as conscious patients. ● Semi-conscious or comatose patients ● Ask the watcher or nurse, if no nurse is around to identify the patient ● Compare the information on the identification bracelet and request form ● Too young, mentally incompetent or do not speak the language of a phlebotomist ● Ask the watcher or nurse, if no nurse is around to identify the patient ● Compare the information on the identification bracelet and request form ● Unidentified Emergency patient. ● Upon admission, a temporary identification number will be assigned to the patient. Use this ID number on all tests. ● When a permanent number or when the patient has already been identified crossreference it with the temporary number. STEP 3: Verify diet restriction, latex sensitivity, and other allergies. STEP 4: Sanitize hands and position the patient properly. STEP 5: Assemble equipment and supplies. STEP 6: Apply tourniquet. Ask the patient to make a fist without vigorous hand pumping. Select a suitable vein for puncture. Burns, scars or tattoos Damaged veins - springy feel when vein is palpated/touched. Edema Hematoma - causes hemolysis. Mastectomy - breast cancer (prone to infection and swelling) IV line, Cannula, Fistula Tourniquet: should be 3-4 inches above the site. Vigorous hand pumping will have effects in some tests Burns, scars or tattoos: impaired circulation, hard to palpate and draw from Damaged veins: Sclerosed (hardened), thrombosed (clotted) Edema (swelling/high tissue fluid): veins are not prominent and hard to locate; tourniquet will be ineffective due to swelling Hematoma (leakage of blood in surrounding tissues): painful and erroneous test results Mastectomy (lymph node removal): susceptible to swelling and infection IV line, cannula, fistula: draw on the opposite arm. Cannula: a thin tube inserted into a vein or body cavity to administer medicine, drain off fluid, or insert a surgical instrument IV line: If both arms have IV lines and no other vein is available, ask the nurse to turn off the IV fluid for 5 minutes, discard the first 5ml of blood then collect the desired sample. Ask the nurse to turn the IV fluid back on. STEP 7: Put on gloves. Cleanse the venipuncture site with 70% isopropyl alcohol. Allow the area to air dry. STEP 8: Anchor the vein firmly. STEP 9: Enter the skin with a needle at approximately 30degree angle, bevel up. ● If using a syringe, pull back on the barrel with a slow, even tension up to the desired volume of blood. ● If using ETS, as soon as the needle is in the vein, ease the tube forward as far as it will go. - When the tube is filled, remove and invert the tube gently. ORDER OF DRAW: ● Blood culture bottles (sterile procedure) ● Coagulation tubes ● Serum tubes with or without clot activator or gel serum separator ● EDTA tubes ● Oxalate/fluoride, glycolytic inhibitor tubes SITES TO BE AVOIDED: Downloaded by Makyxazo Premium (xonemo@pelagius.net) lOMoARcPSD|35970034 STEP 10: Release the tourniquet. Never withdraw the needle without removing the tourniquet. STEP 11: Place gauze, withdraw needle, and apply pressure. STEP 12: Properly recap the needle using “fishing out” technique. STEP 13: Check the condition of the patient. STEP 14: Dispose contaminated material (needle and holder, and syringe) in designated containers using universal precautions STEP 15: Label tubes at patient’s side. ● Place label directly under the cap ● Name at the top ● Barcode straight ● Collector’s user id ● Leave visible window to be seen ● Patient first and last name, date and time of collection, identification number, and initials of phlebotomist LESSON 2: PROBLEMS ENCOUNTERED IN VENIPUNCTURE PAIN Most common patient reaction. Px may indicate that the venipuncture is painful. Releasing the tourniquet (it may be pinching the arm and causing pain rather than the needle) Discontinue the venipuncture if the px idicates sharp, piercing pain. Avoid deep, probing or fishing venipuncture esp in the area of basilic vein. ● Reposition the needle ● Release the tourniquet ● Discontinue venipuncture ● Avoid deep, probing venipunctures NERVE DAMAGE Caused by deep, probing or fishing out veni esp in the area Downloaded by Makyxazo Premium (xonemo@pelagius.net) lOMoARcPSD|35970034 of basilic vein. First felt by a tingling or numbing of arm or hand may result in legal issues. Avoid probing venipunctures and puncture only veins that can be felt. Deep punctures can also result in puncturing an artery. ● If the nerve is only touched, not damaged, it may be gone in a few hours or days. ● If damaged, numbness could be permanent ● Discontinue venipuncture NAUSEA ● Make the patient as comfy as possible ● Instruct him/her to breathe slowly ● Apply cold compress if necessary ● Give waste basket or container and have tissues and water ready SYNCOPE ● Warning signs: perspiration beads on the forehead, hyperventilation, loss of color ● Vasovagal syncope - fainting due to abrupt pain or trauma ● Discontinue venipuncture ● Lower the head and arms DIABETIC SHOCK ● Experience hypoglycemia because they fasted ● If conscious, let them drink a glass of orange juice or cola will temporary help ● If unconscious, call a physician CONVULSIONS ● Patient become unconscious and exhibit mild to violent uncontrollable movements ● Do not restrain the patient ● Move objects out of the way; protect the head ● Patient will usually recover after a few minute CARDIAC ARREST ● Patient will fall into unconsciousness, no pulse or respiration, dilated eyes and pale skin ● Immediate CPR CONTINUOUS BLEEDING ● Some patients take more than 5 minutes for the site to stop bleeding ● Continue to wrap an elastic gauze around the arm with a pad ● Leave it on for 15 minutes or until the bleeding stops SKIN ALLERGIES ● Some patient are allergic to latex, tape or iodine ● Use hypoallergenic tape and non-latex wrap HEMATOMA ● Discontinue venipuncture and apply heavy pressure on the site of puncture. ● Leakage of blood under the skin at the site of venipunctureat the first sign of hematoma, Discontinue venipuncture and apply heavy pressure ● Petechiae: small red dots that are indications of small amounts of bleeding under the skin surface often a result of low plt count or coagulation problems ● The puncture should not be too deep to pass through the top and bottom walls of the vein (“through and through”) UNUSUAL BLOOD SAMPLES: ● Icteric sample - serum/plasma that contains large amounts of bilirubin. - Patient presents with jaundice ● Lipemic sample - milky and cloudy, serum/plasma contains large amounts of fats and lipids. - May be due to patient not fasting ● Hemolyzed sample - serum/plasma contaminated with RBC contents. CAUSES OF HEMOLYSIS: a. Drawing from a hematoma b. Rupturing of RBCs by using a needle that is too small c. Alcohol on the site of venipuncture that entered the blood sample d. Pulling the plunger too forcibly e. Fast drip/expelling blood vigorously as it is transferred to the tube f. Redirecting g. Mixing tubes vigorously POSSIBLE CAUSES FOR FAILED VENIPUNCTURE: ● Vacuum in tube is not working ● Bevel against the vein wall ● Bevel inserted too far ● Needle partially inserted ● Needle slipped beside the vein ● Collapsed vein ● Undetermined needle position TECHNIQUES TO ENHANCE VEIN AND RECOVER A FAILED VENIPUNCTURE: ● Retie the tourniquet ● Use a blood pressure cuff in place of a tourniquet ● Massage the arm or warm the location ● Lower patient’s arm ● Reseat the tube holder Downloaded by Makyxazo Premium (xonemo@pelagius.net) lOMoARcPSD|35970034 ● ● ● ● ● Use a different tube Place your finger below the venipuncture site and stretch the vein slightly Pull back or advance the needle slightly Rotate the needle one quarter to one half turn. Make sure to pull a little backward before redirecting Venipuncture attempts should be upto 2 tries only. Ask someone else to do it (endorse to another staff) COMMON ERRORS IN SPECIMEN COLLECTION: ● Misidentification of patient ● Mislabeling of the patient ● Short draws/wrong AC/blood ratio ● Mixing problems/clots ● Hemolysis/lipemia ● Hemoconcentration from prolonged tourniquet time ● Exposure to light/extreme temperatures ● Improperly tied specimen/delayed delivery to the laboratory ● Processing errors: incomplete centrifugation, improper storage SPECIMEN CONSIDERATIONS ADDITIONAL: Position or posture - changes in posture result to efflux of filterable substances from the intravascular space to the interstitial fluid spaces - non filterable substances increases in concentration Tourniquet application ● Hemoconcentration: blood pooling at the venipuncture site. If the phlebotomist takes longer than one minute to assess and locate vein of choice for venipuncture, it is best practice to release the tourniquet, assemble supplies and reapply tourniquet immediately before needle insertion. Smoking ● Acute exposure to cigarette smoking affects hematological indexes and oxidative stress biomarkers negatively. ● Increase in hemoglobin because your body requires increased oxygen-carrying capacity because you smoke. red blood cell production naturally increases to compensate for the lower oxygen supply. ● Wbc count increases due to inflammation on respiratory tree due to the irritant effect of cigarette smoke Drugs First pass: All drugs pass thru the liver PATIENT INTERACTION ● Appearance ● ● ● - image projected professional Communication skills Bedside Manner Attitude portrays a trustworthy Attitude ● Integrity or honest – doing what is right regardless of the circumstances ● Compassion – a deep awareness of the distress of others and a desire to alleviate it ● Motivation – having a drive to meet a need ● Dependability and work ethic – able to be relied upon. ● Diplomacy – skill on handling situation without hostility ● Ethical behavior – conforming to a standard of right and wrong IMPLIED CONSENT: example px holds put an arm after being told to draw blood FOR MINORS: if health care prof did not get a parent or guardian consent, may be liable for assault or battery LESSON 1: CAPILLARY PUNCTURE CAPILLARY/SKIN/DERMAL PUNCTURE Severely Burned - blood with tissue fluid Cancer patients - veins are inaccessible or very fragile POCT - in healthcare facility Test on themselves - Ex. Home glucose monitoring Special procedure - Ex. Malarial Smears DEHYDRATED - cannot produce adequate capillary Downloaded by Makyxazo Premium (xonemo@pelagius.net) lOMoARcPSD|35970034 puncture blood sample (poor circulation) COLD - not produce adequate blood flow - situation can be rectified by the phlebotomist, px’s hand needs to be warmed before puncture. The best way to warm is with a WARM WET WASHCLOTH (ideal temp 42 degree Celsius) for only 3-5 min. Warming of the puncture site can increase the blood flow sevenfold Finger-stick - most common, can be automatic or manual Lacer lancet - children >5 y.o, advanced type Heel-stick lancet - special depth to prevent injury, for newborn MICRO-COLLECTION CONTAINERS - the same action/additive with big tubes RING/GREAT FINGER - palmar surface of the distal phalanx, for children over 6 months and adults - side or tip should not be punctured because tissue is about half as thick as the tissue in the center of the finger *When you puncture the finger always CUT ACROSS the finger line. It delivers the best possible blood flow and facilities the formation of drops of blood. Any blood that does flow follows the lines of the fingerprint, resulting to no droplet formation. The blood from the capillary puncture is from the capillary area of the circulatory system. This blood in the capillary bed is predominantly arterial. The test result from the predominantly capillary blood is generally acceptable as a substitute for venous blood. Interstitial fluid - fluid in the tissue spaces between cells Intracellular fluid - fluid within cells from surrounding tissue Gas tubes - for arterial blood gas, without anticoagulant - must warm the site before collecting the specimen Slides - smear Ex. Malaria HEEL PUNCTURES - (plantar surface-medial or lateral)- are performed on infants less than 6 months of age, or on older premature infants who are the approximate size of a full-term 6 month old. EARLOBE - not recommended except for extreme cases such as severely burned patient, when no other location available. *The puncture site must be warm and not be swollen (edematous-build up of tissue fluid) Downloaded by Makyxazo Premium (xonemo@pelagius.net) lOMoARcPSD|35970034 *If all fingers are cold, warm the hand 3 min with a warm washcloth or heel warmer *Clean the finger with 70% Isopropyl alcohol. - then allow the area to air dry thoroughly before any puncture - the patient will feel a sting from the puncture if there is wet alcohol on the skin - if not dry---contaminate blood sample and the sample will become hemolyzed - even after the betadine ha been allowed to dry, it can cause elevated POTASSIUM, PHOSPHORUS or URIC ACID ● ● ● ● Rapid milking of the finger does not enhance the blood flow. Excess pressure may cause hemolysis or contamination of the sample with tissue fluid. Scraping of the blood from the surface of the skin does not allow the blood to flow into the microcollection device and HEMOLYZES the cells. The blood will spread the blood over the surface of the skin resulting to clot formation. Rotate the tube so the blood entering the tube contacts the anticoagulant coating the sides. Anticoagulant samples should be mixed by inverting 8-10 times once they are capped The phlebotomist must choose the correct device for the age of the patient and quantity of the sample needed. Puncture quick and deep enough to achieve the full depth of the blade and to obtain the sample needed. AREA OF CHOICE: Bones, arteries, and nerves are not near these areas SITES TO AVOID: possible damage to the posterior tibial artery First drop of blood- contains interstitial fluid that may interfere in the lab results. --0.5 mL of blood can be collected from a single puncture. *the puncture should not be done at a previous puncture site because of the possibility of infection. DO NOT PUNCTURE IN THE CENTRAL ARCH AREA OF THE FOOT - puncture in this area may result in damage to Downloaded by Makyxazo Premium (xonemo@pelagius.net) lOMoARcPSD|35970034 nerves, tendons, and cartilage. The same procedure with fingerstick capillary puncture. DOES NOT INJURE THE BONE OR NERVES OF THE HEEL The infants finger does not produce an adequate blood sample. ● Excessive crying - can result in elevated leukocyte count. The WBC count does not return to normal for up to 60 min. ● Hemolysis is the greatest concern with microcollection samples. Increase potassium ● Elevated Bilirubin- yellow color of serum may mask hemolysis ● Concentration-glucose, potassium, total protein and calcium have been reported to be different ● Sequential sample- when collecting sequential samples of glucose, potassium, total protein, or calcium, the phlebotomist should use the same collection method throughout the consecutive collections. LESSON 2: SPECIMEN HANDLING AND PROCESSING The goal of a phlebotomist is to provide acceptable samples for laboratory testing as required by the physician. Certain general criteria must be followed for a sample to be acceptable. If the criteria are not followed, the sample must be rejected and re-collected. LABEL OF THE TEST TO BE PERFORMED- especially for body fluids( CSF, PERITONEAL, PLEURAL) POTASSIUM- increased with presence of hemolysis or excess tissue fluid. Downloaded by Makyxazo Premium (xonemo@pelagius.net) lOMoARcPSD|35970034 - for unusual results of patient, further study EXPOSED TO LIGHT - bilirubin, Vitamin C,E, K. - wrap the tube with aluminum foil or use AMBER tubes. Never freeze whole blood STORAGE: maintain sample integrity, before disposal Room temperature is specified as between 15 and 30°C Refrigeration temperature is between 2 and 10°C CSF - if it is blood-stained in anyway this invalidates the test. We do not accept CSF sample with a RCC of greater than 150. PERITONEAL volume - If possible, > 500 mL or entire volume collected should be submitted. CONTAINER - different container per lab section plus extra container for additional tests. LABEL: patient’s name, type of specimen, test CENTRIFUGATION: except Bacteriology and Hematology tests CLOT- more than 30 mins, sample is not acceptable CENTRIFUGE - do not centrifuge the sample immediately, allow the sample to clot first - sample is not acceptable if na re-centrifuge SEPARATE - for Send-out/outside testing by other laboratory - if the test is not available in your lab STORAGE- store only plasma/serum, do not include rbcs FROZEN TEMPERATURE is at or below 20°C. Downloaded by Makyxazo Premium (xonemo@pelagius.net) lOMoARcPSD|35970034 VOLUME: more than half of the container CONTAINER: label must be on the body, not on the lid PROCESSING: accumulation of bacteria COLLECTION: refrain from having sex or masturbation for 2-5 days before sample collection. Delivering it to the laboratory within 60 minutes. PROCESSING: within 2 hours to observe the movement of parasite present. Stool specimen collected from the diaper is not allowed. Specimen should NOT contain urine, oil, tissue or other contaminants. COLLECTION: early morning collection, have the patiemt rinse the mouth with water and then expectorate deep cough sputum directly. VOLUME: 3 containers with 1 hour interval each - rinse your mouth out with water prior to collection and to avoid food for 1-2 hours before the sample is collected. The specimens are listed in order of priority; those listed are those most useful for testing for the greatest number of different pathogens with a single clinical specimen. Downloaded by Makyxazo Premium (xonemo@pelagius.net) lOMoARcPSD|35970034 Downloaded by Makyxazo Premium (xonemo@pelagius.net)