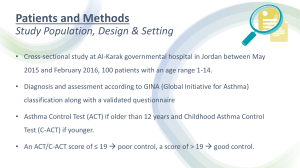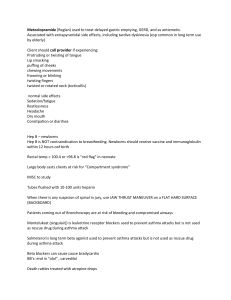
Information for Behavioral Health Providers in Primary Care Asthma What is Asthma? Asthma (AZ-ma) is a chronic (long-term) lung disease that inflames and narrows the airways. Asthma causes recurring periods of wheezing (a whistling sound when you breathe), chest tightness, shortness of breath, and coughing. The coughing often occurs at night or early in the morning. Asthma affects people of all ages, but it most often starts in childhood. In the United States, more than 22 million people are known to have asthma. Nearly 6 million of these people are children. Overview The airways are tubes that carry air into and out of the lungs. People who have asthma have inflamed airways. This makes the airways swollen and very sensitive. They tend to react strongly to certain substances that are breathed in. When the airways react, the muscles around them tighten. This causes the airways to narrow, and less air flows to the lungs. The swelling also can worsen, making the airways even narrower. Cells in the airways may make more mucus than normal. Mucus is a sticky, thick liquid that can further narrow the airways. This chain reaction can result in asthma symptoms. Symptoms can happen each time the airways are irritated. Sometimes symptoms are mild and go away on their own or after minimal treatment with an asthma medicine. At other times, symptoms continue to get worse. When symptoms get more intense and/or additional symptoms appear, this is an asthma attack. Asthma attacks also are called flare-ups or exacerbations. Asthma Information Sheet (continued) Figure A shows the location of the lungs and airways in the body. Figure B shows a cross-section of a normal airway. Figure C shows a cross-section of an airway during asthma symptoms. . It's important to treat symptoms when first noticed. This will help prevent the symptoms from worsening and causing a severe asthma attack. Severe asthma attacks may require emergency care, and they can cause death. Outlook Asthma can't be cured. Even when you feel fine, you still have the disease and it can flare up at any time. But with today's knowledge and treatments, most people who have asthma are able to manage the disease. They have few, if any, symptoms. They can live normal, active lives and sleep through the night without interruption from asthma. For successful, comprehensive, and ongoing treatment, take an active role in managing your disease. Build strong partnerships with your doctor and other clinicians on your health care team. What Causes Asthma? The exact cause of asthma isn't known. Researchers think a combination of factors (family genes and certain environmental exposures) interact to cause asthma to develop, most often early in life. These factors include: An inherited tendency to develop allergies, called atopy (AT-o-pe) Asthma Information Sheet Ver3.0 – July 2013 Page - 2 Asthma Information Sheet (continued) Parents who have asthma Certain respiratory infections during childhood Contact with some airborne allergens or exposure to some viral infections in infancy or in early childhood when the immune system is developing If asthma or atopy runs in your family, exposure to airborne allergens (for example, house dust mites, cockroaches, and possibly cat or dog dander) and irritants (for example, tobacco smoke) may make your airways more reactive to substances in the air you breathe. Different factors may be more likely to cause asthma in some people than in others. Researchers continue to explore what causes asthma. Who is at Risk for Asthma? Asthma affects people of all ages, but it most often starts in childhood. In the United States, more than 22 million people are known to have asthma. Nearly 6 million of these people are children. Young children, who have frequent episodes of wheezing with respiratory infections, as well as certain other risk factors, are at the highest risk of developing asthma that continues beyond 6 years of age. These risk factors include having allergies, eczema (an allergic skin condition), or parents who have asthma. Among children, more boys have asthma than girls. But among adults, more women have the disease than men. It's not clear whether or how sex and sex hormones play a role in causing asthma. Most, but not all, people who have asthma have allergies. Some people develop asthma because of exposure to certain chemical irritants or industrial dusts in the workplace. This is called occupational asthma. What are the Signs and Symptoms of Asthma? Common asthma symptoms include: Coughing. Coughing from asthma is often worse at night or early in the morning, making it hard to sleep. Wheezing. Wheezing is a whistling or squeaky sound that occurs when breathing. Chest tightness. This may feel like something is squeezing or sitting on your chest. Asthma Information Sheet Ver3.0 – July 2013 Page - 3 Asthma Information Sheet (continued) Shortness of breath. Some people who have asthma say they can't catch their breath or they feel out of breath. They may feel like they can't get air out of their lungs. Not all people who have asthma have these symptoms. Likewise, having these symptoms doesn't always mean that someone has asthma. A lung function test, done along with a medical history (including type and frequency of symptoms) and physical exam, is the best way to diagnose asthma for certain. The types of asthma symptoms, how often they occur, and how severe they are may vary over time. Sometimes symptoms may just be annoying. Other times they may be troublesome enough to limit activities of daily living. Severe symptoms can threaten one’s life. It's vital to treat symptoms when they are first noticed them so they don't become severe. With proper treatment, most people who have asthma can expect to have few, if any, symptoms either during the day or at night. What Causes Asthma Symptoms to Occur? A number of things can bring about or worsen asthma symptoms. Your doctor will help you find out which things (sometimes called triggers) may cause your asthma to flare up if you come in contact with them. Triggers may include: Allergens found in dust, animal fur, cockroaches, mold, and pollens from trees, grasses, and flowers Irritants such as cigarette smoke, air pollution, chemicals or dust in the workplace, compounds in home décor products, and sprays (such as hairspray) Certain medicines such as aspirin or other nonsteroidal anti-inflammatory drugs and nonselective beta-blockers Sulfites in foods and drinks Viral upper respiratory infections such as colds Exercise (physical activity) Other health conditions—such as runny nose, sinus infections, reflux disease, psychological stress, and sleep apnea—can make asthma more difficult to manage. These conditions need treatment as part of an overall asthma care plan. Asthma Information Sheet Ver3.0 – July 2013 Page - 4 Asthma Information Sheet (continued) Asthma is different for each person. Some of the factors listed may not affect you. Other factors that do affect you may not be on the list. Talk to your doctor about the things that seem to make your asthma worse. How is Asthma Diagnosed? Primary care doctors will diagnose asthma based on medical history, a physical exam, and results from tests. He or she also will determine the level of asthma severity—that is, whether it's intermittent, mild, moderate, or severe. Severity level will determine what treatment is started. A Veteran may need to see an asthma specialist if: Special tests are needed to be sure you have asthma. If a life-threatening asthma attack has occurred. If the Veteran needs more than one kind of medicine or higher doses of medicine to control your asthma, or if you have overall difficulty getting your asthma well controlled. If the Veteran is thinking about getting allergy treatments Medical History The doctor may ask about family history of asthma and allergies. He or she also may ask about the presence of asthma symptoms, and when and how often they occur. The doctor will also want to know if the symptoms seem to happen only during certain times of the year or in certain places, or if they get worse at night. The doctor also may want to know what factors seem to set off symptoms or worsen them. The doctor may ask about related health conditions that can interfere with asthma management. These conditions include a runny nose, sinus infections, reflux disease, psychological stress, and sleep apnea. Physical Exam The doctor will listen to the Veteran’s breathing and look for signs of asthma or allergies. These signs include wheezing, a runny nose or swollen nasal passages, and allergic skin conditions such as eczema. Keep in mind that someone can still have asthma even if these signs aren’t present on the day of the examination. Diagnostic Tests Lung Function Test: The doctor will use a test called spirometry to check how the lungs are working. This test measures how much air a patient can breathe in and out. It also measures how fast the patient can blow air out. The doctor also may Asthma Information Sheet Ver3.0 – July 2013 Page - 5 Asthma Information Sheet (continued) give the patient medicines and then test again to see whether the results have improved. If the starting results are lower than normal and improve with the medicine, and if your medical history shows a pattern of asthma symptoms, your diagnosis will likely be asthma. Other Tests: Your doctor may order other tests if he or she needs more information to make a diagnosis. Other tests may include: Allergy testing to find out which allergens may be involved, if any. A test to measure how sensitive the airways are. This is called a bronchoprovocation test. Using spirometry, this test repeatedly measures lung function during physical activity or after receiving increasing doses of cold air or a special chemical to breathe in. A test to show whether another disease with the same symptoms as asthma, such as reflux disease, vocal cord dysfunction, or sleep apnea may be present. A chest x-ray or an EKG (electrocardiogram). These tests will help find out whether a foreign object or other disease may be causing asthma symptoms. How Is Asthma Treated and Controlled? Asthma is a long-term disease that can't be cured. The goal of asthma treatment is to control the disease. Good asthma control will: Prevent chronic and troublesome symptoms such as coughing and shortness of breath Reduce the need for quick-relief medicines (see below) Help maintain good lung function Let the patient maintain normal activity levels and sleep through the night Prevent asthma attacks that could result in emergency room visits or hospital admissions. To reach this goal, patients should actively partner with their doctor to manage asthma. Taking an active role to control asthma involves working with the doctor and other clinicians on the health care team to create and follow an asthma action plan. It also means avoiding factors that can make asthma flare up and treating other conditions that can interfere with asthma management. An asthma action plan gives guidance on taking your medicines properly, avoiding factors that worsen you asthma, tracking your level of asthma control, responding to worsening asthma, and seeking emergency care when needed. Asthma Information Sheet Ver3.0 – July 2013 Page - 6 Asthma Information Sheet (continued) Asthma is treated with two types of medicines: long-term control and quick-relief medicines. Long-term control medicines help reduce airway inflammation and prevent asthma symptoms. Quick-relief, or "rescue," medicines relieve asthma symptoms that may flare up. Initial asthma treatment will depend on how severe the disease is. Follow-up asthma treatment will depend on how well the patient’s asthma action plan is working to control symptoms and prevent asthma attacks. The level of asthma control can vary over time and with changes in home, school, or work environments that alter how often exposures to asthma-worsening factors occur. The doctor may need to increase medications if the asthma doesn't stay under control. On the other hand, if the asthma is well controlled for several months, the doctor may be able to decrease the medication. These adjustments either up or down will help to maintain the best control possible with the least amount medication. Following an Asthma Action Plan Patients can work with their doctor to create a personal written asthma action plan. The asthma action plan shows the daily treatment, such as what kind of medicines to take and when to take them. The plan explains when to call the doctor or go to the emergency room. The Behavioral Health Provider can encourage the patient to follow through with the plan and provide encouragement and/or corrective actions. See the National Heart, Lung, and Blood Institute's (NHLBI's) Asthma Action Plan for a sample plan. Avoid Things That Can Worsen Your Asthma A number of common things (sometimes called asthma triggers) can set off or worsen asthma symptoms. Once these factors are known, a patient can take steps to control many of them. (For more information on asthma triggers, see "What Are the Signs and Symptoms of Asthma?") For example, if exposure to pollens or air pollution makes asthma worse, patients may try to limit time outdoors when the levels of these substances are high in the outdoor air. If animal fur sets off asthma symptoms, pets with fur should be kept out of the home or bedroom. The NHLBI offers many useful tips for controlling things that make your asthma worse. (See page 2 of NHLBI's Asthma Action Plan.) If asthma symptoms are clearly linked to allergies, and exposure to those allergens can’t be avoided, then the doctor may advise the patient to get allergy shots for the specific allergens that bother the asthma. Patients may need to see a specialist if they're thinking about getting allergy shots. These shots may lessen or prevent asthma symptoms, but they can't cure asthma. Asthma Information Sheet Ver3.0 – July 2013 Page - 7 Asthma Information Sheet (continued) Several health conditions can make asthma more difficult to manage. These conditions include runny nose, sinus infections, reflux disease, psychological stress, and sleep apnea. These conditions will likely be treated as well. Medicines Doctors will consider many things when deciding which asthma medicines are best for the patient. Doctors usually use a stepwise approach to prescribing medicines. Asthma medicines can be taken in pill form, but most are taken using a device called an inhaler. An inhaler allows the medicine to go right to the lungs. Not all inhalers are used the same way. Ask the doctor and other clinicians on the health care team can show the patient the right way to use an inhaler. Long-Term Control Medicines Most people who have asthma need to take long-term control medicines daily to help prevent symptoms. The most effective long-term medicines reduce airway inflammation. These medicines are taken over the long term to prevent symptoms from starting. They don't give you quick relief from symptoms. Inhaled Corticosteroids. Inhaled corticosteroids are the preferred medicines for long-term control of asthma. These medicines are the most effective longterm control medicine to relieve airway inflammation and swelling that makes the airways sensitive to certain substances that are breathed in. Reducing inflammation helps prevent the chain reaction that causes asthma symptoms. Most people who take these medicines daily find they greatly reduce how severe symptoms are and how often they occur. Inhaled corticosteroids are generally safe when taken as prescribed. They're very different from the illegal anabolic steroids taken by some athletes. Inhaled corticosteroids aren't habit-forming, even if taken every day for many years. But, like many other medicines, inhaled corticosteroids can have side effects. Most doctors agree that the benefits of taking inhaled corticosteroids and preventing asthma attacks far outweigh the risks of side effects. One common side effect from inhaled corticosteroids is a mouth infection called thrush. Often patients can use a spacer or holding chamber to avoid thrush. A spacer or holding chamber is attached to the inhaler when taking medicine to keep the medicine from landing in the mouth or on the back of the throat. Rinsing the mouth out with water after taking inhaled corticosteroids also can lower the risk of thrush. Asthma Information Sheet Ver3.0 – July 2013 Page - 8 Asthma Information Sheet (continued) With severe asthma, patients may have to take corticosteroid pills or liquid for short periods to get asthma under control. If taken for long periods, these medicines may increase the chance of cataracts and osteoporosis. Other Long-term Control Medicines. Other long-term control medicines include: Inhaled long-acting beta2-agonists. These medicines open the airways and may be added to low-dose inhaled corticosteroids to improve asthma control. An inhaled long-acting beta2-agonist shouldn't be used alone. Leukotriene modifiers. These medicines are taken by mouth. They help block the chain reaction that increases inflammation in the airways. Cromolyn and nedocromil. These inhaled medicines also help prevent inflammation and can be used to treat asthma of mild severity. Theophylline. This medicine is taken by mouth and helps open the airways. If the doctor prescribes a long-term control medicine, it should be taken every day to control asthma. Asthma symptoms will likely return or get worse if the medication is stopped. Quick-Relief Medicines All people who have asthma need a quick-relief medicine to help relieve asthma symptoms that may flare up. Inhaled short-acting beta2-agonists are the first choice for quick relief. These medicines act quickly to relax tight muscles around the airways during a flare-up. This allows the airways to open up so air can flow through them. Quick-relief medication is taken when asthma symptoms are first noticed. If patients are using this medicine more than 2 days a week, they should talk with their doctor about how well controlled the asthma really is. You shouldn't use quick-relief medicines in place of prescribed long-term control medicines. QuickEmergency Care Most people who have asthma can safely manage their symptoms by following the steps for worsening asthma provided in the asthma action plan. Patients should call their doctor for advice if: Medicines don't relieve an asthma attack. If peak flow is less than half of personal best peak flow number. Asthma Information Sheet Ver3.0 – July 2013 Page - 9 Asthma Information Sheet (continued) Call 9–1–1 for an ambulance to take you to the emergency room of your local hospital if: You have trouble walking and talking because you're out of breath. You have blue lips or fingernails. At the hospital, you will be closely watched and given oxygen and more medicines, as well as medicines at higher doses than you take at home. Such treatment can save your life. Asthma Treatment for Special Groups The treatments described in this section generally apply to all people who have asthma. However, some aspects of treatment differ for people in certain age groups and those who have special needs. Older Adults Doctors may need to adjust asthma treatment for older adults who take certain other medicines, such as beta blockers, aspirin and other pain relievers, and antiinflammatory medicines. These medicines can prevent asthma medicines from working properly and may worsen asthma symptoms. Older adults may develop weak bones from using inhaled corticosteroids, especially at high doses. Talk to your doctor about taking calcium and vitamin D pills and other ways to help keep your bones strong. People Having Surgery Asthma may add to the risk of having problems during and after surgery. For instance, intubation may cause an asthma attack. Patients should tell their surgeon about their asthma. The surgeon can take steps to lower your risks, such as giving you asthma medicines before or during surgery. References and Further Information National Heart Lung and Blood Institute Internet: http://www.nhlbi.nih.gov/health/dci/Diseases/Asthma/Asthma_WhoIsAtRisk.html These Information Sheets are designed to provide a brief overview of various medical conditions. Referring to the Information Sheets may help you communicate more effectively with other members of the Primary Care Team. The Information Sheets are by no means an exhaustive description of the disorders. If you need additional information, please engage in a more detailed search. Don’t forget to consult with other members of the Primary Care Team. They are an invaluable source of information! Asthma Information Sheet Ver3.0 – July 2013 Page - 10