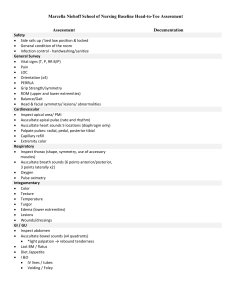
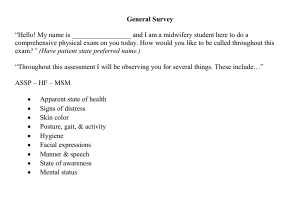
Head to Toe Assessment script Introduction Hi my name is Jocelyn Gonzales and I'm a first year nursing student with Durham college and today I'm going be conducting a head to toe assessment is that OK The first thing I'm going to do is an environmental scan I'm going to make sure the O2 is working with the nasal prongs in the packaging I'm going to make sure the suction's working and also the yanker and I'm going to make sure the beds in the lowest position with the bed rails up and the brakes I'm going to also make sure that the call bell is within reach and there's no clutter surrounding the bed Next I'm going to do a general scan of my patient and I can see that my patient skin colour is good for their ethnicity is alert and awake in a lying down position they also seem to have no signs of distress or pain on their face Pain Questions Next I'm going to ask you a couple of questions. So what brings you in today? Is there anything makes it better or anything that makes it worse? What does it feel like? Does the pain radiate or move anywhere throughout your body? on a scale of zero to 10 zero being no pain and 10 being the worst pain you've ever felt can you tell me what number you would rate it? When did this pain start? Do you know what's causing this pain? Pre-assessments So I already have taken my patients vital signs For my patients temperature I got 36.5°C which is in the normal range of 36°C to 38°C I got my patients blood pressure which was 124 / 84 which is in the normal range of 90 / 60 to 140 / 90 My patients radial pulse was 84 beats per minutes which is in the normal range of 60 to 100 beats per minute My patients respirations were 18 which is in the normal range of 12 to 20 and my patients 02 saturation was at a 97 which is in the normal range of 95 to 100 Neuro Next I'm going to assess my patience level consciousness using a person place and time Can you please tell me your name first and last, the date month and year and place. Next I'm going to be a assessing my patient pupils. Can you stare at my finger while I shine a light, so I can see that my patients pupils are equal round reactive to light and they also accommodate. Upper extremities next I'm going to inspect my patients upper extremities. I could see the skin colour is good for their ethnicity there's no signs of cyanosis or pallor or edema and their skin looks intact. Next I'm going to palpate my patients upper extremities. Their skin is warm to touch, their radial pulse is strong and equal bilaterally, their regular pulse is also strong and equal bilaterally. Next I'm going to ask you to squeeze my fingers. It is noted that they are strong bilaterally. Next I am going to check cap refill it is good less than three seconds. Anterior chest next I am going to inspect the anterior chest and i could see that the skin colours good for their ethnicity the elliptical is good their ribs are sloping downwards and there's no signs of them using any accessory muscles and the transverse ratio is 1:2 Next I am going to palpate the anterior chest for any tenderness or masses and it is noted that there are no tenderness or masses present next I'm going to auscultate the anterior chest using the five point sequence. Their airway seems to be good equal strong bilaterally and there's no signs of advantageous breathing. This is when I would assess any dressings like tracheostomy tubes of chest tubes or check the O2 instruction again Heart Next I would inspect the pericardium the skin colour looks good for ethnicity. Next I would auscultate I'm using the ATM sequence. Starting with the aortic valve which is in the second right intercostal space an this is where S2 is louder than S1. Then I would auscultate the pulmonic valve which is in the second left intercostal space and this is where S2 is louder than S1. Next I would move to the third intercostal space which is erbs point an this is where S2 an S1 are equal. I would go to the tricuspid valve next and it is located at the 4th intercostal space and this is where S1 is louder than S2. Then I would go to the 5th intercostal space which is the mitral valve and this is where S1 is larger than S2. This is also where the apical rate is heard on the left lateral side and you would use the bell to assess. Abdomen Has there been any change in your appetite do you have any Constipation diarrhea nausea or vomiting next I am going to inspect the abdomen. I could see that the skin colour is good for their ethnicity and their abdomen is a bit rounded and there are no strike striation marks or scars and it looks symmetrical next I'm going to auscultate the abdomen starting in the right lower quadrant going clockwise an I'm going to listen for 5 seconds and if there are no bowel sounds present I would listen for 5 minutes in each quadrant next I would palpate the abdomen starting in the right lower quadrant I would palpate the tender areas last Anne not palpate any masses I would assess any dressings like colostomy and ileostomy I would also assess the urine output an any catheters like Foley I would also assess for any bruits Lower extremities next I'm going to inspect the lower extremities and I could see the skin colour is good for their ethnicity there's no signs of cyanosis pallor or edema the skin is intact and the hair distribution is even next I'm going to palpate. The skin is warm to touch the Doris pedias is equal strong bilaterally. Can you please push up against my hand. Their muscle strength is strong bilaterally. Now I'm going to check cap refill it is good less than three seconds now I'm going to assess any dressings next I am going to set my patient up in high fowlers posterior chest next I am going to inspect the posterior test I could see that it's symmetrical the skin colour is good for their ethnicity and there's no signs of using any accessory muscles and the spine seems to be in the midline next I'm going to palpate the chest to look for any tenderness or masses there are no tenderness or masses present. Next I am going to auscultate the chest using the nine point sequence and a 2.3 lateral for the side. It's noted that they have a clear good airway bilaterally and there is no adventitious breath sounds present and this is when I would assess any dressings the patient has lastly I would discuss my findings with your health care provider and and come up with a goal plan and provide a discharge plan if that is appropriate.