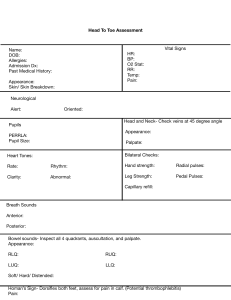
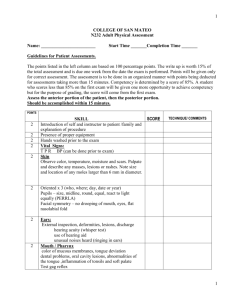
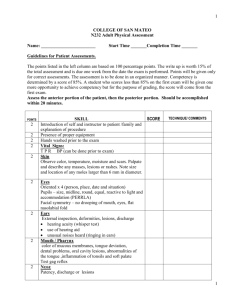
General Survey “Hello! My name is _________________ and I am a midwifery student here to do a comprehensive physical exam on you today. How would you like to be called throughout this exam?” (Have patient state preferred name.) “Throughout this assessment I will be observing you for several things. These include…” ASSP – HF – MSM Apparent state of health Signs of distress Skin color Posture, gait, & activity Hygiene Facial expressions Manner & speech State of awareness Mental status Motor System, Gait, & Spine “Next I am going to evaluate your gait and steppage.” Have patient walk to other side of room: 1) normal gait, 2) heel-to-toe, 3) on toes, and 4) on heels. “Next I will have you stand on one leg and do a deep knee bend, and repeat on the other leg. Please hop up and down on one foot a few times, and on the other foot up and down a few times.” Have patient stand with back to you. “Now I am going to examine your back for symmetry of shoulders, scapulae, and hips.” Palpate down the vertebrae right on top of the spinous processes, starting at cervical spine down to lumbosacral spine, assessing for tenderness. (Use thumbs/one hand) Palpate the paravertebral muscles; muscles alongside spine, assessing for tenderness. Palpate trapezius muscle and between scapulae. Next, have patient bend at waist. Stand behind them and examine for scoliosis and symmetry. Have patient touch toes. Motor System, Gait, & Spine, cont’d “Next, we are going to do some range of motion exercises…” have patient lean back stand up straight, lean to the left, lean to the right hold hips and have patient rotate torso to left side, and right side Rhomberg Test & Upper arm drift To do the Rhomberg test and assess for upper arm drift, have patient stand with eyes closed, arms out in front with palms up. “Normally I would have you stand here for 60 seconds, with me standing behind you for safety in case you start to sway, but you look really stable. Now I am going to tap your arms to check for upper arm drift.” Tap each arm twice. Upper and Lower Extremities Have patient sit on a comfortable surface facing examiner (seat, exam table, bench). Examine fingernails for capillary refill, dorsum of the hands, palms, touch skin on forearms, assessing for texture, temperature, and turgor (pinch arms). Check radial pulses bilaterally simultaneously. Palpate the epitrochlear nodes on the inside of the elbow bilaterally. Joint Palpation – Starting with one arm and assessing for tenderness, palpate the joints, starting with fingers, moving up to wrist, elbow, and shoulder, all the way around. Next do shoulder range of motion, with one hand on shoulder, hold arm at the wrist and move through a circle, feeling for crepitus, popping, clicking, or snapping. Repeat on other arm. “Next I am going to assess range of motion in your upper extremities.” ROM of elbows (flex and extend) ROM of wrists (up and down, side to side) ROM of hands (spirit fingers and ball fingers into fist and stretch out) Upper and Lower Extremities, cont’d Strength assessment – Have patient place hands on knees, palms up, and squeeze your fingers bilaterally. Have patient put arms up, bending at elbow. Apply resistance and have patient pull and push against forearms, pull and push lifting elbows out and in. Move to legs. Apply resistance to lower extremities and have patient pull legs towards table, away from table, in with knees, and out with knees. On feet, have patient pull up with feet, and push down against your hands with feet. Rapid alternating Movements – Have patient tap feet quickly against yours like pressing on a gas pedal. Next move up to hands, have patient flap hands face up and face down quickly on their lap. Next have patient rapidly alternate tapping fingers against thumbs, both at the same side with patient holding their hands up. “Now I’m going to have you extend your arms out to the side and bending at the elbows, alternate touching each pointer finger to your nose. Keep doing this while your eyes are closed. Now open your eyes, and I’m going to have you chase my finger, putting your hand back to your lap after every time I move my finger. Next, lift your arm up above your head, and bring it down and touch my pointer finger. Close your eyes and do it a few more times.” Upper and Lower Extremities, cont’d Sharp and Dull Using a cotton wisp, have patient close eyes and touch them on their arms/hands and legs/feet, having them say “NOW” when they feel it brush against their skin. Using a Q-tip, break in half so there is a sharp edge and the cotton tip will be the dull edge. Alternate touching patient and have them discriminate between sharp and dull touch. (After every dull touch, do sharp in the same area.) DO THIS ON UPPER AND LOWER EXTREMITIES. Discriminative Sensation – Have patient close eyes and hold arms on laps with palms up, and place an item in one hand and have them identify what it is. Repeat the same thing with the other hand. (Items you can use could be a coin, paper clip, pencil.) “This is called stereognosis.” Point Discrimination - With patient’s eyes still closed, have them distinguish between 1 or 2 points of a paper clip touching them (fingers, palms, forearms bilaterally, NOT lower extremities). Extinction – “With your eyes still closed, the last test of discriminative sensation I am going to do is called extinction. I am going to touch you and I want you to point to where I am touching. Good.” (Once on arms using both fingers, once on legs using both fingers) Upper and Lower Extremities, cont’d Reflexes Using your reflex hammer, elicit the following reflexes bilaterally. Have patient relax and grit their teeth. Triceps (arm up, above elbow) Biceps (inside of elbow) Brachioradialis (on forearm near wrist) Patellar (knee) Ankle (Achilles tendon) Plantar responses Toes – Having patient close their eyes, wiggle their big toe, and hold it in an up or down position, and ask patient to tell you if it is up or down. Do this several times on each big toe. Next, with your patient’s eyes still closed, firmly hit 256Hz tuning fork on a hard surface and apply to the bone of second toe. Ask the patient to tell you what they FEEL. Repeat on other second toe. Face & Head Inspection – looking at face for symmetry of face, eyebrows, and eye structures. Palpation - skull and hair distribution, frontal, and maxillary sinuses, temporal pulses, TMJ joint (open and close mouth), motor portion of CN 5 - Masseter muscle, clench teeth and wag jaw back and forth. Sensory portion of CN 5 – look up, brush cotton wisp against cornea – watch for blink. Trigeminal nerve (CN 5) Sensory portion – Have patient close eyes, and do the sharp/dull test on face using Q-tip. (Remember after doing dull, do sharp in the same spot.) Do light touch with cotton wisp on face, ask patient to say “NOW” when she feels the cotton wisp. CN 7 – look up, examining for even lifting of eyebrows and wrinkling of the forehead. Have patient look at you. Have them… Close eyes and not let you open Smile with teeth them Puff out cheeks Smile Pucker up Neck Palpate the following lymph nodes: Occipital Tonsillar Submandibular Submental Posterior cervical Anterior cervical Supraclavicular (shrug) Infraclavicular Palpate for trachea symmetry (fingers in a V-shape) ROM of neck – head down, head back, turn to left, turn to right, ear to shoulder, ear to shoulder. Apply resistance and have patient turn head to one side and push your hand, other side and repeat. Place hands on shoulders and have patient lift against your resistance. “This tests cranial nerve #11.” Thyroid Palpation – anchoring pinky on clavicle, palpate the thyroid. Have patient turn head to left and right. Have patient glance down at left knee and swallow. Have patient glance down at right knee and swallow. Eyes & Cranial Nerves Inspection of eyes – eye structure, symmetry CN 2 (Confrontation) – Testing confrontation/peripheral vision (face patient, have patient cover eye and look at your forehead, tester covers opposite eye/match them straight across. Wiggle fingers in from different angles. When you test confrontation from the side that the patient’s eye is covered at, mirror the eye covering.) Repeat covering other eye. CN 3, 4, 6 (Extraocular movements) Have patient follow finger with eyes only, do NOT turn head. Make an H shape. State that you are looking for lid lag and nystagmus. Bring finger closer and closer to patient’s nose – convergence and accommodation Have patient look at your finger, and then change focus to the far wall. Corneal Light Reflex – have patient look at the light, examine to see if the light reflects evenly in both corneas Oblique lighting – use a penlight (state you would do it in a darkened room) Look for scratches, opacities, foreign bodies, “I see you have contacts” Eyes & Cranial Nerves, cont’d PERRLA – Using ophthalmoscope, shine into eyes while having patient look straight ahead across the room, pupils equally round and reactive to light. Check for conceptual reaction – check if same thing happens in both eyes when light is shined into one. Ophthalmoscopic Exam Set the light to about 80% of its maximum brightness. Starting with right eye, use right hand, use right eye to examine (to avoid bumping noses). Turn off overhead lighting. Have patient look as far down across the room as she can and focus on a spot on the wall. State that you would turn off the lights for this exam. Take your left hand to steady the patients head, fingers on diopters, 15 degrees from nose, red reflex, follow that, visualize the optic disc, artery and vein. Now to examine the patient’s left eye, use your left eye, your left hand, catch red reflex, move in, adjust diopters, visualize optic disc, artery, vein. Ears and Cranial Nerve 8 Have patient put finger over one ear, walk to opposite side, cover side of mouth, and whisper 5 letters/numbers. This is cranial nerve 8 that tests hearing. Eyes & Cranial Nerves, cont’d Weber Test Firmly tap tuning fork (high frequency: specify that it is 512 Hz) on hard surface and place on top of forehead. Ask patient to tell you where they hear this – certain side or equally on both. Rhine Test Firmly tap tuning fork on hard surface and place on bone behind patient’s ear. Ask them to tell you when the sound disappears. When they say now, take tuning fork off bone and place it a few inches from ear, ask patient if they can hear something. ** Verbalize that air conduction is greater than bone conduction Examine Ears Palpate the preauricular nodes, post auricular nodes, auricle, pinna, tragus, tenderness Otoscopic Exam Pull up, out, and back on pinna, gently slide otoscope in on edge of outer ear, keep going until you come into focus ** Visualize what you are seeing = “pearly gray tympanic membrane, cone of light, landmarks” Eyes & Cranial Nerves, cont’d Nose and Cranial Nerve Inspect nose, looking for symmetry, occlude one nare and breathe in, and other side. Assesses patency. Now to assess the olfactory nerve, (CN 1) have the patient close their eyes and occlude one nostril. On the side of the patent nostril, waft a small container of a smell for patient to identify (essential oil, coffee grounds, cinnamon). Do the same on the other side with the opposite nostril. Have patient tip head back, using penlight, inspect patient’s nasal mucosa, the septum, inferior and middle turbinates on both sides. Eyes & Cranial Nerves, cont’d Mouth and Cranial Nerves 9, 10, 11 Look at the mouth using a penlight – lips, teeth, gums, buccal mucosa, parotid ducts, top of tongue, sides of tongue, under surface of tongue, salivary glands and salivary duct openings, anterior pillars, posterior pillars, and tonsils, posterior pharynx, hard and soft palate. Have patient say “ahhh,” look at even rise of uvula. Gag with tongue blade – testing CN 9 and 10. Have patient stick out tongue – look at symmetry, deviations, and fasciculation. “This tests cranial nerve 12; the hypoglossal nerve.” Neck, Posterior, Spine, Thorax, Lungs “Now with your back facing me, I am going to take a look at your back while you take a deep breath in and out.” Check for thoracic expansion – put hands around back of chest, have patient take a deep breath in and look for thumbs moving apart CVA tenderness – using fist, tap area where kidneys are. Should not elicit tenderness. Tactile fremitus – Have patient say 99 while you palpate their back bilaterally (NOT ON BONE) Percussion on back – use reflex hammer and tap on finger Start on shoulders, in between shoulder blades, under shoulder blades, sides of thorax Auscultation throughout lung fields – have patient take moderately deep breaths (in and out through an open mouth) while you start listening at the top Anterior Thorax & Lungs “Now with you facing me, the first thing I’m going to do is inspect across the precordium, the area of the chest in which the heart lies, looking for lifts and heaves.” (exposed chest) Have patient take a deep breath in and out Palpate down the costochondral junctions, where the ribs meet at the sternum, assessing for any tenderness (costal chondritis) Assess for fremitus on the anterior chest, have patient say “99” while you palpate with flat hands/fingertips Percuss across the chest Auscultate – have patient take moderately deep breaths while listening to anterior lung fields Cardiac Exam – SITTING “Moving on to the heart, I am going to palpate across the precordium for thrills – aortic, pulmonic, Erb’s (right ventricular area), tricuspid, and mitral Palpate for the point of maximal impulse (PMI) – 5th intercostal space at the midclavicular line Auscultate across the heart with diaphragm – aortic, pulmonic, Erb’s, tricuspid, and mitral Auscultate across the heart with bell – aortic, pulmonic, Erb’s tricuspid, and mitral “Now I am going to have you lean forward, and going back to using my diaphragm, I’m going to place it right over the aortic area, breathe out all your air and hold your breath.” Repeat with pulmonic. This positioning helps to detect murmurs if they are present. Having the patient hold their breath ensures you won’t mistake a breath sound for a murmur. Neck Vessels Having patient lie supine, then elevate head up to 30 degrees. Using penlight, examine the veins on each side of the neck, looking at the internal venous pulsations and external jugular veins. Palpate carotid pulses, one side at a time, we do them separate to avoid a vagal response. Auscultate for bruits using the bell of the stethoscope, have patient hold breath while you listen. Cardiac Exam – SUPINE Keep patient in supine position at 30 degrees elevation. “To finish the heart exam, I am going to auscultate over aortic, pulmonic, Erb’s, tricuspid, and mitral areas to assess for any murmurs in this position.” Using the bell, listen over the aortic, pulmonic, Erb’s (right ventricular), tricuspid, and mitral. Auscultate for a mitral murmur using the bell, across midclavicular line at the 5 th intercostal space, have patient roll over to the left side after marking the landmark with stethoscope. Abdomen Keep patient in supine position at 30 degrees elevation. Inspect for contour, protuberance, if its concave, symmetry, any scars Auscultate for bowel sounds in RLQ Auscultate over aorta with diaphragm Auscultate for bruits with the bell – renal arteries (right and left upper quadrant) , iliac arteries (right and left lower quadrants), groin area for femoral bruits Percuss across entire abdomen – tympany will be the predominant sound. If any areas of dullness are heard, check again. Now place patient completely flat. Percuss for liver starting from the bottom right lower quadrant at the midclavicular line, until a change in sound is reached. Mark with a pen. Now percuss from top down (xylophone maneuver) until you reach a change in sound. Mark with a pen and measure distance. Normal liver range is 6-12 cm. Palpate for aorta make sure there is no aneurysm. Start around umbilicus, and slowly move upward, feel the pulsation. Palpate aorta again with both hands starting laterally and move in. Measure the distance, anything less than 3 cm is normal. Note that it is pulsating upwards and not laterally. (aneurysm) Abdomen, cont’d Light palpation throughout entire abdomen with one hand – assess for tenderness Deep palpation – have patient bend knees and put feet flat, helps the abdomen relax. Keep elbows close to body, use two hands, start with LLQ. Avoid epigastrium because it is normally tender. Patient can place knees down. Palpate liver. Mention it is not enlarged and contained under the costal margin. If it is under the costal margin, you will not feel it. Do a hooking maneuver, have patient take a deep breath in, hook during exhale, have her inhale again. Palpate spleen, place hand toward axilla, have patient turn to right side, palpate along costal margin. Palpate for kidneys, place one hand under back, palpate on top. Have patient inhale and exhale deeply. Most kidneys are nonpalpable. Have patient lift head, look at abdomen to see if there are any hernias. Palpate femoral pulses and inguinal nodes (NAVEL acronym – nerve, artery, vein, empty space, lymph nodes) Lower Extremities With patient in supine position, check the popliteal pulses bilaterally, pedal pulses bilaterally simultaneously, posteriorly Check for edema in feet and on shins. Press thumbs on tops of feet over medial malleolus and front of calves. Wiggle toes, wiggle ankles. Have patient bring knee to chest on left leg, knee to chest with right leg. Range of motion with hips – abduct, down, up, inward across midline, bend knee, do internal and external rotation, feeling knee for any crepitus. “Last thing you will do is I’m going to have you take one heel, place it on your opposite knee and run it down your shin. Repeat on the other side.”