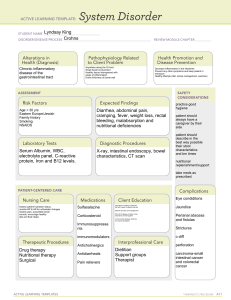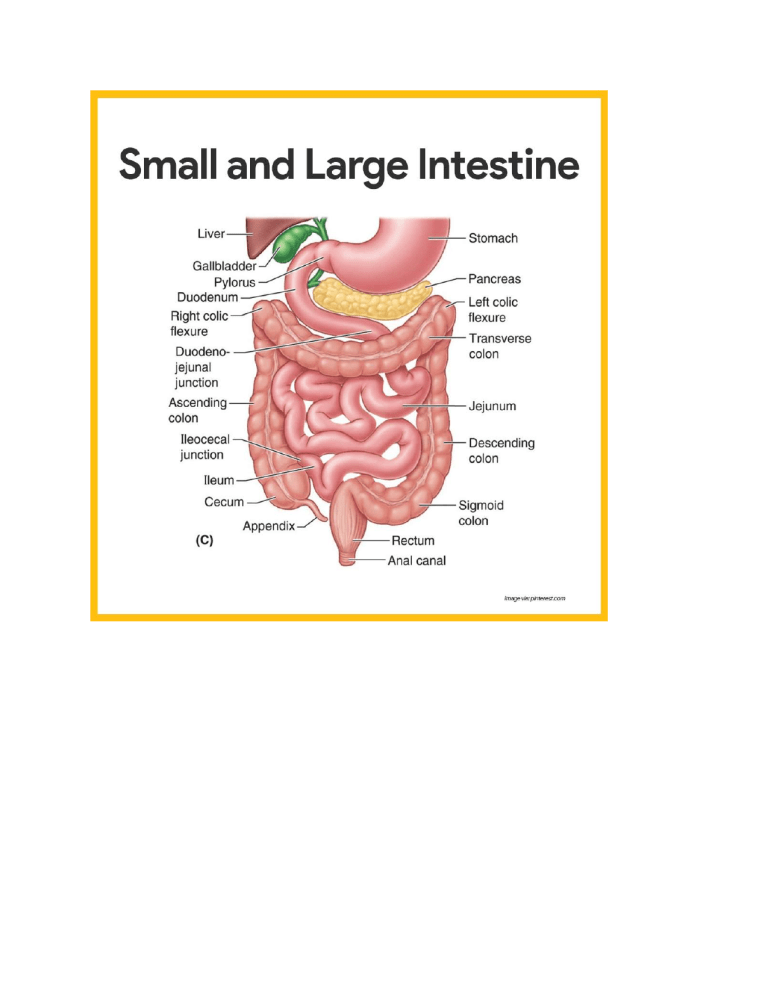
Read GI Pathoma before starting. Oral Cavity Cleft lip/Palate: Full thickness defect of lip/palate due to failure of facial prominences to fuse. Occur together and are multifactorial. Aphthous ulcer: painful, superficial ulcerations of oral mucosa. Arises due to stress and resolves randomly. Grayish base surrounded by erythema. Bechet syndrome: Recurrent man of aphtohous ulcer (Stress caused, disappear spontaneously), uveitis and genitcal ulcers. Due to Immune complex vasculitis. Oral herpes: HSV-1 causes vesicles involving oral mucosa, rupturing results in shallow, painful red ulcers. Occurs in childhood but remains dormant in ganglia of trigeminal nerve. Squamous cell carcinoma: Malignant neoplasm of Oral mucosa. Tobacco/alcohol are major risk factors. Floor of mouth most common location. Oral leukoplakia and erythroplakia are precursor lesions. 1. Leuokoplakia : white plaque which is NON scrapable and presents as squamous cell dysplasia 2. Leukoplakia is distinct from oral candiasis (thrush) and hairy leukoplakia. 1. Oral candiasis is white thrush on tongue and SCRAPPABLE. 2. Hairy leukoplakia is white, rough (“HAIRY”) on LATERAL TONGUE, Immunocompromised individuals. (AIDS) 3. Erythroplakia (red plaque) represents VASCULORIZED LEUKOPLAKIAsquamous cell dysplasia. 4. Erythroplkia and leukoplakia should be biopsied to rule out carcinoma. Mumps: viral infection causing bilateral inflamed parotid glands. Presentation: Orchitis, pancreatitis, aseptic meningitis. Risk of sterility in teenagers Lab: serum amylase increased due to salivary/pancreatic gland involvement Sialadenitis: Inflammation of salivary gland. Most common cause is (sialolthiasis) leading to S, Aureus infection, usually unilateral Plemorphic adenoma: benign tumor of stromal (cartilage) and epithelial tissue, most common tumor of salivary gland Presentation: occurs in parotid, mobile, painless mass at angle of jaw. High rate of reoccurrence. May transform into carcinoma, which presents with signs of facial nerve damage (facial nerve runs through parotid gland) Warthin tumor: Benign cystic tumor with GERMINAL CENTERS (lymph node like stroma) and abundant lymphocytes. Always occurs in parotid Muceoepidermoid carcinoma: Malignant tumor of mucinious and squamous cells, most common malignant tumor of salivary gland. Arises in parotid gland and involves facial nerve. 1. False mucosal teeth: a false diverticulum is an outpouching of mucosa and submucosa only (compare to true diverticulum which is out pouching of mucosa, submucosa and muscularis propria and adventitia) 2. Zanky Zenkers hoodie: Zenker diverticulm is a false diverticulum, in the posterior upper esophagus 3. Kids go for enjoyment: Zenker diverticulum is due to weakness of the cricopharyngeus muscle in the killian triangle(area in the hypopharynx) 4. Eating burning pizza: zenkers diverticulum may present with odynophagia (painful swallowing) 5. Stinky cheese: zenkers diverticulum may present with halitosis (Bad breath) 6. Regurigitating food: zenker’s diverticulum may present with regurigation 7. Protruding “hit A mouse” game: in a Hiatial hernia, the stomach herniates into the thorax through the esophageal hiatus 8. Sliding mouse-spring junction: in a sliding hernia, the gastroesophageal junction herniates through the esophageal hiatus (a type of hiatal hernia) 9. 2 protruding mice: in a paraesophageal hernia, gastic cardia herniates through the esophageal hiatues (sneaks up besides a normally placed esophagus) (a type of hiatal hernia) 10. Refleuxing acid: refluxing acid: hiatal hernias present with gastroesophageal influx (GERD) 11. Marshmallow pit: Mallory -weiss tears (mucosal tears in proximal stomach and distal esophagus) 12. Linear scratches on distal slide: Mallory-Weiss tears consists of linear longitudinal lacerations in the mucosa of the distal esophagus and proximal stomach 13. Drinking at marshmallow pit: Mallory-weiss tears are often due to alcohol abuse (increases intra gastric pressure from committing) 14. Wrenching at marshallow pit: Mallory-weiss tears and Boerhaave syndrome are caused by increased intragastric pressure during retching and vomiting 15. Coughing up red drink: Mallory-weiss tears present with mild to moderate hematemesis 16. Spilling red drink: Mallory-Weis tears can present with moderate hematemesis 17. Kick to stomach: Mallory-Weiss tears can cause epigastric pain 18. Ruptured bounce house: Boerhaave syndrome, there is transmural rupture of esophagus 19. Wrenching at marshallow pit: Mallory-weiss tears and Boerhaave syndrome are caused by increased intragastric pressure during retching and vomiting 20. PeriSCOPE: Boerhaave syndrome can be caused by esophageal endoscopy 21. Weakened bounce house: Conditions that weaken esophageal (infection, inflammation, structural defects) are risk factor for Boerhaave syndrome 22. Spilling red juice: Boerhaave syndrome causes severe hematemesis 23. Air puffed induced chest injury: Boerhaave syndrome causes severe sharp chest pain 24. Crunchy chip: Boerhaave syndrome can cause subcutaneous emphysema (pulpation of chest causes crunchy sound) 25. Wet pleural shirt: Boerhaave syndrome can cause pleural effusions (due to gastric contetns in pleural space) 26. Septic manhole cover and flame banada: Boeerhaave syndrome can cause fever, sepsis, and septic shock 27. Gargling: GERD is an imbalance between LES tone and intragastric pressure which causes reflux of gastric acid into esophagus 28. Loose drawstring: LES tone can cause GERD 29. Smoker: smoking can cause GERD (decrased LES tone) 30. Alcoholic: alcohol can cause GERD (decreases LES tone) 31. Coffee: caffeine can cause GERD (decreases LES tone) 32. Pregnant woman: pregnancy can cause GERD (decreased LES tone and increased intragastric pressure) 33. Obese guy: Obesity can cause GERD (increased intragastric pressure) 34. Punching chest: Gerd can present with non cardiac chest pain like heartburn 35. Coughing in bed: GERD can present with nocturnal cough 36. Inhaler: Gerd can present with nocturnal asthma 37. Choking throat: GERD can present with dysphagia (difficulty swallong) 38. Burning hole: GERD can progress to erosive esophagitis or esophageal ulcers 39. Clutching throat: erosive esophagitis due to GERD can present with odyophagia 40. Mucosal cake with pink and blue sprinkles: GERD causes esophagitis (histology shows eosinophils and lymphocytes infiltrating the mucosa) 41. Tall lower cake layer with thick frosting: servere GERD causes elongation of papillae of the lamina propria and hypertrophy of the basal cells of the mucosa 42. Barretts bear: GERD can lead to barretts esophagus (intesntinal metaplasia of the distral esophagus) 43. Squamous tiles: esophageal is normally lined with stratified squamous epithelium 44. Columnar stage: intestinal metaplasia of Baretts esophagus consist of columnar epitheilium 45. Scatted mucus cups: Intestinal metaplasia of barretts esophagus contains goblet cell hyperplasia 46. Metal intestines: intestinal metaplasia (baretts esophagus) 47. Ascending red velvety curtains: Baretts esophagus columnar epithelium extend upward from the gastroesophageal junction 48. Dirty dysplastic floor: dysplasia is a precancerous condition (compared to metaplasia), which is benign transformation of one cell type into another) 49. Cancer crab: Barrett’s esophagus (Metaplasia) can progress to Dysplasia and eventually cancer (esophageal adenocarcinoma) 50. Parasol: Gerd is treated with proton pump inhibitors (PPIS, suffix is “prasol” or H2 blockers (both reduce acid production in stomach) 51. Eosinophilic bilobed sling shot: eosinophilic esophagitis presents similar to GERD (dysphagia, chest/upper abdominal pain) after eating 52. Slingshot kid: eosinophilic esophagitis often occurs in childhood (unlike GERD, which occurs in adults) 53. Pink eosinophilic granules: Eosinophilic esophagitis involves epithelial infiltration of eosinophils through out the esophagus 54. Itchy nose and hives: eosinophilic esophagitis may present along with other atopic symptoms (eczema, allergic rhinitis, asthma, peripheral eosinophilia) 55. Breaking through parasol: Eosinophilic esophagitis may be resistant to PPIS Esophageal varices: Dilation of submucosal veins in lower esophagus caused by secondary portal hypertension. Rupture can present with painless hematemesis. From diagram, you can see as blood is backed up in the liver, it looks for other ways to escape. Esophagus veins 1. Hooked at throat: Esophageal cancer and motility disorders all present with Dysphagia (difficulty swallowing 2. Cancers crab in bear den: esophageal adenocacrcinoma (most common esophageal malignancy in the us) 3. Glandular fluff : Esophageal adenocarcinoma has gland-like features on histology similar to other adenocarcinomas 4. Barretts bears: barretts esophagus can cause esophageal adenocarcinoma (via progregression to dysplasia and then cancer) 5. Metal instestines: Barretts esophagus from normal statfied squamous epithelium to intestinal columnar epithelium 6. Smoker: smoking increases risk of esophageal adenocarcinoma (especially if pre-existing barretts esophagus) 7. Distal velvety curtains: esophageal adenocarcinoma primarily affects the distal third of the esophagus (including GE junction which is same area as GERD and barretts esophagus) 8. Stuck Solid guy with liquid passing by: esophageal adenocarcinoma presents with dysphagia (initiallty for solids, then also liquids) 9. Thin bear: esophageal adenocarcinoma presents with weight loss 10. Swalloing burning hot pizza: esophageal adenocarcinoma presents with odynophagia (painful swallowing) 11. Cancer crab on squamous table cloth : Esophageal squamous cell carcinoma is most common type of esophageal cancer world wide 12. Cured foods: foods with N-nitroso compounds (pickled egetables, meats) are all risk factor 13. Hot tea: hot beverages are a risk factor for esophageal sqyamous cell carcinoma 14. Chewable nut: betel nuts are a risk factor for esophageal squamous cell carcinoma 15. Alcoholic : alcohol is a risk factor 16. Smoker: tobacco smoke is a risk factor 17. Mid-body tutu: esophageal cell carcinoma occurs in middle third of the esophagus 18. Stuck solid guy with liquid passing by: Esophageal cell carcinoma presents with dysphagia (initallity for solids then progresses to liquids) 19. CLuthing throat: esophageal squamous cell carcinoma causes odynophagia (painful swallowing) 20. Thin actress: esophageal squamous cell carcinoma causes weight loss 21. Raised flat area: esophageal squamous cell carcinoma appears as raied plaques with ulceration 22. Pearl necklace: histology will show kertain pearls and intracellular briding (similar to all forms of squamous cell carcinoma) 23. Plumber-vinson: Plummer-vinson syndrome is atriad of dysphagia, iron deficenecy anemia and esophageal webs 24. Falling iron tools: plummer vinson syndrome is caused by chronic iron deficiency 25. Cobwebs: plummer-vinsion syndrome cause esophageal webs 26. Mucosal protursions: esophageal webs in plummer vinson syndrome are thin protursions of esophageal mucosa in the upper third of the esophagus->dysphagia for solids only 27. Stuck solid guy: Plummer vinsion syndrome presents with dysphagia for solids 28. Pale plubmbers overalls: plummer vinsion syndrome presents with iron defeicny anemia 29. Irritated qumpous tiles: plummer-vinson syndrome increases the risk of esophageal squamous cell carcinoma (due to irritant effect) 30. Squeezing lower esophageal harness: Achalasia is esophageal dysmotility caused by impaired relaxation of the LES->functional esophageal obstruction 31. Loss of safety plexus: achalasia is caused by impaired relaxation of the LES due to loss of the myenteric (Auerbach) plexus 32. Rusty nitric oxide exhaust and falling VIP pass: in achalasia, loss of myenteric (Auerbach) plexus causes decreased NO production and VIP which causes impaired relaxation of the LES smooth muscle 33. Idiot: Achalasia is usually idiopathic 34. Che’sGas: acquired achalasia is caused by Chagas disease (trypanosoma cruzi destroys myentric plexus) 35. Bird beak: in achalasia , increased LES tone leads to constriction of the LES and dilation of the esophagus more proximally (appears as bird beak on barium swallow) 36. Regurgitation food: achalasia presents with regurgitation of undigested food 37. Clutching chest: Achalasia presents with chest pain 38. Difficulty funneling liquid: achalasia presents with dysphagia for liquids (in aiddtion to solids) 39. Uncoordinated spasming ropeo: Diffuse esophageal spasm is a dysmotility disorder (in which impaired inhibitory neurotransmission) within the myenterix plexus which results in uncoordinated contractions 40. Corkscrew rope: Diffuse esophageal spasm appears as a corckscrew on barium swallow 41. Regurgitating: Diffuse esophageal spasm causes regurgitation 42. Diffuse esophageal spasm causes dysphagia for liquids (in addition to slids) 43. Sand bag crushing chest: diffuse esophageal spasm causes retrosternal chest pain 44. Anginal anvil: in diffuse esophageal spasm, chest pain is similar to angina (and also relieved by nitrates) 45. Dragon talon crest: Crest syndrome (calcinosis, Raynaud syndrome, Esophageal dysmotility, Sclerodactyly, Telangiectasias) is a variant of systemic sclerosis (autoimmune disease targeting vascular endothelium, cause tissue fibrous) 46. Fibrous vines in lower stage: Crest syndrome, esophageal dysmotility is due to fibrous replacement of the muscularis in lower esophagus 47. Dripping water: CREST syndrome presents with dysphagia for liquids and solids 48. Refluxed acid: Crest syndrome, decreased esophageal tone can lead to GERD (increasing risk of barrettes esophagus) Squamous cell carcinoma spread 1. Upper 1/3-cervical nodes 2. Middle 1/3-mediastinal tracheobronchial nodes 3. Lower 1/3-celiac and gastric nodes 1. Damaged peptic concrete: acute gastropathy (damaged gastric mucosa due to deficient mucus lining or direct toxic effect) 2. Fire extinguisher: NSAIDS can cause acute gastropathy (direct toxic effect; and inhibition of COX1 which decreases prostaglandin synthesis and decreases mucus production) 3. Smoking and drinking: both alcohol and tobacco have direct toxic effects on the gastric epithelium, which can lead to acute gastropathy 4. Flaming peptic concrete: acute gastropathy can lead to acute gastritis (vascular congestion, edema, and neutrophilic infiltration on histology) 5. Leaking shallow hole: severe damage may lead to an erosion which extends through the gastric epithelium into the lamina propria (may cause acute hemorrhagic erosive gastropathy) 6. Leaking deep hole through rebar layer: gastric ulcers are erosions that have extended through the muscalris mucosa into the submucosa (risk for bleeding). Acid damage results in superficial inflammation (damage to epithelium), Erosion (loss of epithelium), ulcer (Loss of mucosal layer) 7. Curling ulcers can develop with severe burns 8. Dumping bucket on burn: curling ulcers develop due to hypovolemia and creased gastric mucosal perfusion (decreased blood flow) 9. Burning curly drill bit: Cushing ulcers develop with high intracranial pressure 10. Vegas sign: increased intracranial pressure causes massive vagal output->(ach will bind to parietal cells) increases gastric acid producing causing Cushing ulcers 11. Stomach on fire: acute gastritis can cause vague epigastric pain (dyspepsia) 12. Nauseated: acute gastritis can cause nausea, vomiting, anorexia 13. Chronic grandfather clock: chronic gastritis (H.Pylori, infection, Autoimmune gastritis) 14. Helicopter: h.pylori infection is most common cause of chronic gastritis (T CELL, TYPE IV HSV) 15. Helicopter sinking through mucus: H.pylori invades the stomach mucus layer to reside on the gastric epithelium 16. Pink commas: H.pylori is a comma-shaped gram-bacilli 17. Helicopter adjacent to distal stomach: h.pylori usually infects the antrum first 18. Fire under helicopter: initial infection wth H.pylori can cause acute gastritis 19. Spotlight pointing across the stomach: H.pylori infection spreads from antrum to the body of the stomach 20. Chronic shack roof on fire: chronic h.pylori infection causes inflammation of gastric mucosa. 21. First responders: chronic inflammation due to H.purlo infection displays a prominent neutrophil infiltrate 22. Thinning fabric: chronic inflammation from H.Pylori leads to chronic atrophic gastritis (mucosal atrophy and loss of acid and hormone secreting glands which causes decreased gastrin and acid secretion 23. White mucus knots in columnar fence: chronic inflammation from H.pyrloi leads to intestinal metaplasia ( normal gastric columnar epithelium develops goblet cell hyplerplasia) 24. Intestinal metal pipes: Chronic inflammation from H.Pylori leads to intestinal metaplasia 25. Cancer crab: intestinal metaplasia (due to chronic inflammation from H.pylori) can progress to dysplasia and cancer 26. Pile of lymphoid tissues: chronic H.pylori infection can lead to Mucosa-Association Lymphoid (MALT). Chronic antigenic prescence of H.pylori causes accumulation of lymphocytes, which organie into lymphoid tissue with germinal centers 27. Blue tissues: histology will show MALT appear blue due to presence of lymphocytes 28. Crab on helicopter: MALT (caued by H.pylori) can transform into gastric lymphoma 29. Biopsy grabber: H.pylori infection can be diagnosed with gastric biopsy (antrum and body) 30. Ammonia spray bottle: Urease testing of gastric biopsy specimen increases sensitivity of testing for H.Pylori 31. Gas from ammonia bottle: H.pylori can be diagnosed with a urea breath test (drinks radiolabeled urea and urease in H.pylori metabolizes it into radiolabeled CO2 which is detected on breath). 32. Antibody forklift: autoimmune metaplastic atrophic gastritis, auto antibodies cause destruction of parietal cells and intrinsic factor 33. Targeting parietal protests: parietal cells location in body of stomach/fundus, are targeted in autoimmune metaplastic atrophic gastritis 34. Dropping lemons: autoimmune metaplastic atrophic gastritis, destruction of parietal cells causes decreased secretion of gastric acid. Achloryhdria (no acid), which will cause G cells to undergo hyperplasia 35. Obserized “GAS” can: AMAG, gastin levels are increased (destruction of parietal cells, decreased HCL secretion, hyplerplasia of gastin producing G cells in antrum causes hypergastinemia) 36. “NO intrinsic right”: in autoimmune metaplastic atrophic gastritis, Intrinsic factor is decreased (normally binds to vitamin B12 to facilitate its absorption). B12+Intrinsic factor complex is absorbed in terminal ielum 37. Mushroom cloud “blast”: AMAG, decreased B12 absorption causes pernicious anemia (megalablastic anemia which has a large fragile erythrocytes). Non-infectious causes of chronic gastritis (Chronic granulomatosis, sarcoidosis, Celiac, Radiation induced gastritis) 38. Jackhammer eroding through rebar layer: Peptic ulcer disease penetrate through the muscularis into the submucosa 39. PUD helicopter: PUD develops over time with chronic gastritis (example H.pylori) 40. Lesser curvate hole: Gastric ulcer most commonly occur in lesser curvature of stomach 41. Distal duodenal ulcer: Duodenal ulcer (more common than gastric ulcer), NOT malignant 42. Knocked-Over STOP sign: H.pylori-mediated chronic gastritis leads to destruction of antra delta cells which causes decreased somatostain release. Triple therapy treatment will resolve (Gastriti, ulcer and metaplasia) 43. GAS tanks: in chronic gastritis, (H.pylori), loss of somatostatin leads to uninhibited gastrin production, hypertrophy of brunners gland 44. Activaated protester throwing lemons at gas guy: increased gastrin causes acid secretion by parietal cells 45. Lemon juice in duodenal hole: in chronic gastritis , increased acid delivery to the dueodenum leads to dueondeal erosion and ulcers 46. Fire extinguisher: NSAID use is a risk factor for peptic ulcer disease in the stomach (works with H.pylori) 47. Smoker: smoking is a risk factor for peptic ulcer disease (gastric and duodenal) 48. Eating lunch with active jacke hammer: Gastric peptic ulcer disease, epigastric pain is worse with meals (due to increased gastrin mediated acid secretion) 49. Eating lunch with inactive jackhammer: duodenal peptic ulcer disease, epigastric pain is improved with meals due to decreased passage of acid into duodenum after food intake, and release of bicarbonate from pancreas. BLEEDING FROM GASTRODUODENAL ARTERY 50. Hole leaking blood: peptic ulcer disease can cause upper GI bleeding (melena or hematemesis if severe) 51. Black tar: peptic ulcer disease can cause melena (“black tarry stools” due to oxidation of iron from hemoglobin breakdown) a complication of upper GI bleeds (proximal to suspensory ligament of the duodenum) 52. Big gastric blood pipe: gastric ulcers may bleed heavily due to erosion into left gastric artery 53. “Path obstructe0p d” Gastric outlet obstruction is a complication of peptic ulcer disease (due to inflammation causing swelling of pylorus), presents with nonbilious emesis 54. Big duodenal air pipe: duodenal ulcers can lead to perforation (most common in anterior duodenum) 55. Small gastric air pipe: gastric ulcers can lead to perforation (less common than in duodenal ulcers) 56. Suspender strap popping: ulcer perforation causes shoulder pain (acute peritonitis->irritation of diaphragm and phrenic nerve->pain in C3-C5 dermatomes) 57. Black belt: Ulcer perforations causes radiolucency, between right hemididaphragm and liver on upright abdominal X-ray (due to free air in abdominal cavity) 58. Grabbing crab: Peptic ulcers and surrounding areas are biopsied to rule out malignancy How do you know if ulcer is benign or malignant? ->benign ulcer : SMALL, PUNCHED OUT ->malignant ulcer : LARGE, IREEGURAL, Heaped up margins 1. Broken gastric rickshaw: gastroparesis (delayed gastric emptying WITHOUT mechanical obstruction) 2. Nauseated: gastroparesis presents with nausea and vomiting 3. Holding abdomen: gastroparesis presents with abdominal pain 4. Broken VEGAS sign: gastroparesis is caued by dysfunction of the vagus nerve (PNS) which impairs peristalsis of food through stomach 5. Severed wire: iatrogenic effects (example, surgical injury to vagus nerve) 6. “idiot”: idiopathic cause 7. Elevated candy: diabetes can cause gastroparesis 8. Mortar/Pestle: CCBs and TCA can cause it 9. “raMEN Try it”: Menetriers disease (hypertrophy of stomach rugal folds due to hyperplasia of mucus-secreting cells) 10. Thick ramen noodles: Menetries disease, hypertrophy of rugal folds inhibits peristalsis of food through the stomach 11. Excessive mucus: in menetriers disease, hyperplasia of mucus-secreting cells results in decreased number of acid-secreting gastric glands which caused decreased protein digestion 12. Nauseated: Menetriers disease presents with nausea and vomiting 13. Holding abdomen Menetriers disease presents with abdominal pain and early satiety 14. Tarry black borth: Menetriers disease can cause melena and hematemesis (symptoms of upper GI bleeding) 15. Losing meat chunks: menetriers disease is a “protein-losing enteropathy” due to increased permeability of stomach mucosal cells 16. Thin girl: Menetriers disease presents with weight loss, muscle wasting, hypoalbuminemia, peripheral edema 17. Cancer crab: Menetriers disease is a risk factor for gastric adenocarcinoma 18. Giant cancer crab: Gastric adenocarcinoma (most common malignancy of stomach, more common in East Asian countries) 19. Hanging intestines: intestinal type gastric adenocarcinoma (large irregular, ulcer with heaped up margins) 20. Grandfather clock: Chronic atrophic metaplastic gastritis the biggest risk factor for intestinal type gastric adenocarcinoma 21. Helicopter fan: H.Pylori mediated chronic gastritis is a risk factor for ITGA 22. Antibody on gastric pot: autoimmune gastritis is a risk factor for ITGA. Blood type A Risk factor as well. 23. Hanging meats: consumption of salt , salt preserved foods and nitrosamine preserved foods are risk factor for gastric adenocarcinoma 24. Smoking and drinking: smoking and drinking also causes gastric adenocarcinoma 25. Epstein’s bar : EBV is a risk factor for gastric adenocarcinoma 26. Cauliflower: intestinal type-gastric adenocarcinoma (forms a bulky exophytic mass) occurs in lesser curvature of the antrum and pylorus 27. Oozing red sauce: intestinal type gastric adenocarcinoma may cause bleeding and ulcerations 28. Mucinous rice: histology, intestinal type gastric adenocarcinoma shows glandular structures filled with mucin 29. “claw adhering”: rubber band E cadherin (an intracellular adhesion molecule) 30. Losing claw adhering band: in diffuse-type gastric adenocarcinoma, loss of normal E-cadherin proteins results in decreased intracellular connections causing disorganized cell growth 31. Crabs infiltrating along wall: diffuse type gastric adenocarcinoma, disorganized cells growth leads to diffuse invasion through out stomach (“infiltrative growth pattern”) 32. Leather stomach purse: diffuse type gastric adenocarcinoma causes a fibrosing desmoplastic reaction->linits plastica (“leathre bottle” stomach) 33. Ring jewlerry: hitology shows “signet rings” (mucin taining vacuoles displace nucleus to cell membrane 34. Rings on liver purse, lapels and pockets: gastric adenocarcinoma (intestinal and diffuse types), most commonly go to liver, lungs and ovaries 35. Chess board with white T knights and B antibody archers: Primary gastric lymphomas (B or T type) 36. Helicopter-like fan: H pylori mediated chronic gastritis is a risk factor for gastic lymphoma 37. Grandfather clock: chronic atrophic metaplastic gastritis is a risk factor for gastric lymphoma 38. Pile of blue lymphoid tissue: H.Pylori mediated chronic gastritis induces MALT (mucosa associated lymphoid tissue), which can progress to gastric lymphoma 39. Epstein stake Bar: EBV infection can cause gastric lymphoma 40. Marginalized B archers and large B archers: gastric lymphomas are most commonly marginal zone B cell or diffuse B cell lymphoma. Chronic inflammation. 41. GIST arcade hall: GI stromal tumor (GIST-mesenchymal tumor derived from interstital cells of CAJAL) 42. Rhythm game: GIST is derived from the interstial cells of Cajal (GI “pace maker” cells , responsible for Peristalsis 43. Tool kit: GIST is caused by gain of mutation functions in C-KIT oncogene 44. Tire swing game: C-kit is a tyrosine kinase 45. Under mucosal door: GISTs form well-circumscribed fleshy, submucosal masses 46. Mushroom family: familial adenomatous polyposis (FAP) causes colon polys, but NOT gastric polys, and is a risk factor for adenocarcinoma Metastatis via node/liver. Virchow node (involves left supraclavicular node-), Krukenberg tumor (bilateral metastases to ovaries with signet ringsDIFFUSE TYPE), Sister Mary Joseph nodule (subcutaneous periumbilical metastasisINTESTINAL TYPE). 1. Small bowel obstruction 2. Latching on to shirt: adhesions are most common cause of small bowel obstruction (due to mechanical constriction of bowel) 3. Scalpel graffiti: prior abdominal cause of abdominal adhesions (well-demarcated zones) 4. Cancer crab skateboard: small bowel tumors can cause obstruction 5. Green face: small bowel obstruction presents with nausea/vomiting 6. Collie” small bowel obstruction presents with colicky abdominal pain 7. Plunger: small bowel obstruction presents with constipation (inability to pass flatus or stool) 8. Large belly: small bowel obstruction presents with distended abdomen (due to back up of gas in intestines) 9. Drun: small bowl obstruction presents with tympanic abdomen (due to backup of gas in intestines) 10. “tink, tink”: small bowel obstruction presents with high-pitched “tinkling” bowel sounds on abdominal auscultation (due to abnormal peristalsis) 11. Black cloud graffiti: X-ray shows small bowel obstruction displays bowel distension (dilated loops of bowel) and air fluid levels (horizontal contrast line) 12. Wide to narrow half-pipe: Xray of small bowel obstruction shows a “transition” point location of obstruction, point where dilated proximal bowel meets normal distal bowel) 13. Broken skateboard: Ileus is caused by hypomotility (similar to symptoms of small bowel) 14. Dilated colon pants: Ileus, bowel is uniformly dilated (including colon and rectum) 15. Broken boombox: Ileus presents with diminished or absent bowel sounds (due to decreased peristalsis) 16. Scalpel graffti: Surgery can cause ileus 17. Drug bottles: drugs can cause ileus 18. SEPTIC cover: sepsis can cause ileus 19. Elevated candy jar: Diabetes can cause ileus (due to dysfunctional parasympathic nervous system) 20. Arterial rail: Superior mesenteric artery 21. Red ramp: Aorta 22. Crushed kid: Superior mesenteric artery syndrome, the third position of duodenum is compressed between the aorta and SMA (can cause small bowel obstruction) 23. Losing padding: SMA is caused by severe rapid weight loss (shrinking mesenteric fat paddecreased cushioning around duodenumduodenal compression) 24. Painful burrito: SMA presents with recurrent post prandial abdominal pain 25. Telescoping camera lengs: Intussusception (occurs when segment of proximal bowel telescopes beneath more distal bowel) 26. Skull shirt: Intussception can cause bowel ischemia and necrosis (due to impaired venous return) 27. Pile of lymphoid tissues: Hyperplastic lymphoid tissue (post viral infection, ROTA VIRUS) can serve as a lead point to initiate intussception (usually in toddlers) 28. Mecklers hecklers: Meckels diverticulum can serve as a lead point to initiate intussusception 29. Mushroom hats: polys and tumors serve as a lead point to initiate intussception 30. Small ramp meets large landing zone: Ileocecal junction is most common site for intussception 31. Gooey red jelly: Intussusception presents with “currant jelly” stools (blood and mucus) 32. Handle bat at RLQ: intussception presents with RLQ mass (location at illoceal junction) 33. Target cushion: abdominal ultrasound, intusscepation has a target appearance due to telescoped bowel 34. “berry-yum”: barium enema can diagnose and treat intussception (moves telescoped bowel) 35. Weakness in chain link fence: hernias can occur as a result of weakning of biromuscular tissue >intrabdominal contents protrude through defect 36. Running: strenuous exercise is a risk factor for hernias 37. Tight abdominal belt: chronic elevated intra-abdominal pressure (heavy lifting, chronic cought, constipation, pregnancy) are all risk factors for hernia 38. Older male: hernias are more common in older age (decreased tissue strength) and in men 39. Hand cuffs: Incarcerated hernia (abdominal contetns[omentum, small bowel, colon] unable to escape hernia 40. Consticted blue and red strings: incarcerated hernias can cause constriction of veins within bowel->decreased venous and lymphatic drainage->swelling->compromised arterial blood flow 41. Skull tattoos: bowel strangulation can lead to necrosis 42. Torn pants: bowel strangulation can lead to perforation 43. Septic cover: bowel strangulation can lead to sepsis 44. Hesselbachs construction: Hesselbachs triangle (bound by inguinal ligmanet, rectus abdominus, inferior epigastric vessels) 45. Tube: inguinal canal 46. Tarp under skater tunnel: inguinal ligament (base of inguinal canal) forms inferior border of hasselbachs triangle) 47. Striated wooden wall: rectus abdominus muscle (medial border of hesselbachs triangle) 48. Arterial and venous tubes: inferior epigastric vessels (lateral border of hesselbachs triangle) 49. Directly pressing on fence: Direct inguinal hernias pass through hesselbachs triangle (medial to inferior epigastric vessels) 50. Sneaking though tube: Indirect inguinal hernias pass though canal (lateral to inferior epigastric vessels) 51. Sneaking from undertrap: Femoral hernias: pass through femoral canal (located inferior -postior to inguinal ligament 52. Shirt and hoodie: Indirect inguinal hernias are covered by all 3 layers of spermatic fascia (external, oblique aponeurosis, cremastric fascia, transversalis fascia) 53. Direct inguinal hernias are covered by external spermatic fasica 54. Weakened fence: Direct inguinal hernias are a result of weakness in the floor of the inguinal canal 55. Virginia Co Patent: Indirect inguinal hernias are a result of persistent Patent processes vaginalis 56. Woman with skull tattoo: femoral hernias occur mostly in females 1. Ooze canister: carcinoid tumor (most common primary small bowel malignancy) 2. Neural transformer: carcinoid tumors derived from neuroendocrine cells 3. Ooze in distal intestinal pipes: ileum is most common site for carcinoid tumors 4. Slime in gastric tunnel :Carcinoid tumors can occur in stomach 5. Slime in haustra tunnel: carcinoid tumors can occur in the colon 6. Ooze in appendiceal pipe: carcinoid tumors are the most common primary malignancy of appendix 7. Chest zone: carcinoid tumors can occur in the lungs 8. Child in the ooze: Bronchial carcinoid tumors are most common primary lung cancer in children 9. Coughing blood: bronchial carcinoids presents with coughing and hemoptysis 10. Yellow ooze: carcinoid tumors appear yellow on gross pathology 11. Purple spots on pink: histology shows islands of small round purple cells within pink connective tissue (CHROMOGRANIN +) 12. Granular granite: electron microscopy shows tumor cells display cytoplasmic granules (contain secretory products and hormones) 13. Path obstructed: small bowel carcinoid tumors may cause intestinal obstruction 14. Inflamed appendiceal pipe: carcinoid tumors of the appendix may cause appendicitis (due to obstruction of the appendiceal lumen) 15. Climbing into liver base: GI carcinoid tumors may metastasizes to the liver 16. Liver armor: because of first pass metabolism in liver, substances secreted by carcinoid tumors in the GI tract do not cause systemic symptoms 17. Consuming histamine bee: carcinoid tumors secrete histamine, which is metabolized by the liver 18. Consuming smiley serotonin pizza: carcinoid tumors secrete serotonin, which is metabolized by liver 19. Bunch of pizza and bees: vasoactive substances (serotonin, histamine) cause symptoms (“carcinoid syndrome”), if tumor metastasizes to the liver or beyond GI tract (by passes the first pass metabolism) 20. Red face: carcinoid syndrome causes episodic flushing (face, neck, chest) due to excessive histamine secretion 21. Red face mask: carcinoid syndrome causes vascular teleangictasias on nose and cheeks (due to vasodilation from vasoactive factors) 22. Brown waterfall: carcinoid syndrome cause secretary diarrhea (too much serotonin cause increased intestinal motility) 23. Wheezy party blower: carcinoid syndrome may cause episodic bronchospasm and wheezing 24. Carcinoid syndrome can cause valvular disease (plaque like vegetations) in the right heart (for example tricuspid and pulmonic valves) 25. Smiley graffiti: carcinoid valvular disease is due to too much serotonin which causes increased fibroblast growth 26. Leaking wheel: carcinoid valvular disease can cause regurgitation (may later progress to stenosis) 27. Consuming serotonin smiley pizza: lung metabolize serotonin 28. Catching histamine bee: lungs metabolize histamine 29. Lung chest armour: lungs metabolize vasoactive substances secreted by carcinoid tumors (including serotonin, there fore no serotonin reaches left heart, NO LEFT HEART VALVULAR DISEASE) 30. “HI-AA”: carcinoid syndrome is diagnosed with urine 5-HIAA (5-hydoxyindoeleactic acid) a breakdown of serotonin 31. Stop sign: somatostatin analogues are used to treat carcinoid syndrome (bind to somatostatin receptors and inhibit release of serotonin) 32. 8 sides sign: OCTreodite is a somatstain analogue 33. Super pincher crab: small bowel adenocarcinoma 34. Glandy bubbles: histology shows glandular structures 35. Proximal duodenal pipe: duodenum is the most common site for small bowel adenocarcniomas 36. Mutated shroom family: Familial adenomatous polyposis (FAP), causes polys in duodenum and colon and is a risk factor 37. Lynch worm: Lynch syndrome is a risk factor for small bowel adenocarcinoma 38. Peutz pop: Peutz-jeghers syndrome 39. Hammers: Peutz-jeghers syndrome causes multiple non-neoplastic hamartomatous polys through out GI system (mostly small bowel) 40. Domino: Autosomal dominant 41. Creeping crab: Peutz jegurs syndrome is a risk factor for small bowel adenocarcniomas (as well as colorectal and non GI cancers) 42. Peutz-jeghers syndrome causes mucocutaneous hyperpigmentation (mouth, lips, palms, genitalia) 43. Skipping cobble stones: Crohns disease is a risk factor for small bowel adenocarcinoma 44. Distal pipe: Crohn disease (and resulting small bowel adenocarcinoma) commonly affects the ileum 1. Day of the dead: intestinal ischemia and necrosis occurs because of low perfusion to bowel 2. Tall tombstone projections with vascular ivy: villi of small and large bowel (contain small capillaries and venulues) 3. Crypt: crypts of small and large bowel contains secretory and stem cells 4. Small vascular ivy near surface: arteries become smaller and more susceptible to ischemia as they move toward luminal surface of villi 5. Cracking dead vascular ivy: bowel ischemia and necrosis start at the luminal surface of villi>leads to sloughing of villi 6. Proliferating crypt flowers: in the bowel, crypts are initially spared from ischemia and become hyperplastic (although later affected as ischemia progresses) 7. First responders: ischemia leads to a neutrophilic infiltrate 8. Patches of red marigolds: bowel ischemia leads to patchy areas of mucosal hemorrhage 9. High pressure water: ischemia and inflammation lead to bowel wall edema->increased pressure obstructs venous drainage->further decrease in perfusion 10. Top arterial bowsprit: super mesenteric artery (SMA) supplied small intestines and proximal large bowel 11. Low arterial bowspirit: Inferior mesenteric artery supplies distal large bowel 12. Black intestinal design: acute intestinal occlusion (most likely to occur in the SMA leads to acute mesenteric ischemia) 13. Poop emboli from thrombotic nest: occlusion of the SMA by an embolus causes acute mesenteric ischemia 14. Irregulary ireegular TV signal: acute mesenteric ischemia via embolus formation 15. Thrombotic straw dress: thrombus formation in the SMA (due to rupture of atherosclerotic plaques) causes acute mesenteric ischemia 16. Abdominal pain perplexing doctor: acute mesenteric ischemia causes severe abdominal pain (out of proportion to physical exam) 17. Green face: acute mesenteric ischemia (causes nausea/vomiting) 18. Broken speaker: acute mesenteric ischemia causes loss of bowel sounds (due to ileus) 19. Dressed in all black with ripped sleeve: acute mesenteric ischemia can lead to bowel infarction and perforation 20. Septic: acute mesenteric ischemia can lead to sepsis 21. Open door: non occlusive acute intestinal ischemia 22. Hypotensive fainting: non occlusive acute intestinal ischemia is caused by hypoperfusion of intestinal vessels 23. Water shed: the colon has watershed areas (areas most susceptible to hypoperfusion) 24. Arterial trees barley reaching each other: arteries in the colon connect with each other via small shared vessels (anastomoses) 25. Losing water: hypovolemia can cause acute colonic ischemia (because of poor perfusion) 26. Septic: septic shock can cause acute colonic ischemia (because of poor perfusion) 27. Heart shirt: cardiogenic shock can cause acute colonic ischemia 28. Acute colonic ischemia: most commonly occurs in the elderly 29. Corner tree attachment: watershed area between SMA and IMA (located at the splenic flexure), where the transverse colon meets the descending colon 30. Distal tree attachment: watershed area between IMA and rectal arteries (located at the distal end of sigmoid colon) 31. Catching left abdomen: acute colonic ischemia causes crampy left abdominal pain and tenderness (Watershed areas are on the left side) 32. Red blood puddle: acute colonic ischemia can cause bloody stools (due to necrosis and hemorrhage) 33. Broken speaker: acute colonic ischemia can cause loos of bowel sounds (due to ileus) 34. Septic: acute colonic ischemia can cause sepsis 35. Anvil: Chronic mesenteric ischemia causes intestinal angina 36. Grandfather clock: chronic 37. Greasy pipe: chronic mesenteric ischemia occurs secondary to atherosclerosis of mesenteric vessels 38. Obese grandma: chronic mesenteric ischemia is most common in obese older females 39. Greasy spatula: other atherosclerosclerotic disease (coronary heart disease, cerebrovascular disease, peripheral vascular disease) is a risk factor for chronic mesenteric ischemia 40. Clutching belly: chronic mesenteric ischemia presents with postprandial abdominal pain (due to increased oxygen demand during digestion) 41. Aversion to burrito: Chronic mesenteric ischemia presents with aversion to eating (due to post prandial abdominal pain() 42. Thin skeleton: chronic mesenteric ischemia presents with weight loss 43. Tangled red strings: Angiodysplasia of GI tracts (caused by malformed blood vessels which are thin-walled, dilated, torturous, composed only of endothelium 44. Colonic dress: angiodysplasia most often occurs in colon , especially cecum 45. Pool of blood: angiodysplasia presents with recurrent, painless hematochezia 46. Stenotic arched hat: bleeding of angiodysplasia is associated with aortic arch stenosis Hereditary Hemorrhagic Telangiectasia: AD disorder, resulting in thin-walled vessels in GI and nasopharync which rupture and bleed. 1. Pinched stomach bottle: pyloric stenosis 2. #1 bay boy: pyloric stenosis is far more common in males (especially in first-born males) 3. Vomiting white milk: pyloric stenosis presents with non-bilious (because proximal to duodenum) projectile vomiting immediately after feeding 4. One month calendar: pyloric stenosis presents around 1 month 5. Muscular baby sitter: pyloric stenosis is caused by hypertrophy of the pyloric sphincter (takes ~1 month to develop) 6. Round bottle nipple: pyloric stenosis may present with a palpable “olive-shaped” mass at the pylorus (periumbilical region) 7. Schisis string next to umbilicus : gastroschisis (paraumbilical herniated of the abdominal contents through the ventral abdominal wall) 8. Uncovered string: in gastrochisis, herniated organs are NOT COVERED by peritoneum 9. Elephant seal: omphalocele (failure of GI contents to return to the abdominal cavity during embryologic development) 10. Elephant seal collar: omphalocele is a true umbilical hernia (through umbilical ring) 11. Hand covered by puppet: in omphalocele, herniated abdominal organs are COVERED by peritoneum 12. Trisomy triplets with chromosome waistbands: omphaloceles are associated with trisomies (trisomy 18/13) and other defects like cardiac and neural tube 13. Intestines springing out of box: congenital diaphragmatic hernia (CDH), abnormal organs herniate through the left hemidiaphragm and into the thorax 14. Scrunched up lung shirt: congenital diaphragmatic hernia can cause pulmonary hypoplasia and pulmonary hypertension (due to compression of lungs by abdominal organs) 15. Skull and X bones: chest X ray can be used to diagnose congenital diaphragmatic hernia (bowel gas and abdominal organs above the diaphragm) 16. Broken tracheal and esophageal slide: Tracheosphageal fistula 17. September: the fistulas are a result of failure of SEPTAION of the trachoesophageal tube 18. 4th and 5th: tracheesophageal septation normally occurs at 4-5 weeks 19. Tube-slide connection: TE fistula (trachea and esophagus and connected by a bridge) 20. Stuck in tube: esophageal atresia (normal trachea) 21. Distal tube connection: type C-TE fistula (most common ), proximal esophagus ends as blind pouch, distal esophagus connects to trachea) 22. Vomiting while stuck on esophageal ring: type-C TE fitisula causes non bilious emesis (proximal esophagus ends in blind pouchfood never reaches intestines) 23. Distended belly stuck in tube: Type C-TE fistula causes abdominal diestenion (due to flow of air from trachea into stomach) 24. Refluxing onto lung shirt: type-CTE fistula causes recurrent pneumonitis and aspiration pneumonia (due to reflex of acidic stomach contents into lungs) 25. Wet baby doll: type C-TE fistula causes polyhydramnios in utero (due to fetus unable to swallow amniotic fluid) 26. Abnormal doll: TE fistula can be associated with other congenital anomalies (including vacteral association*vertebral defects, anal atresia, cardiac defects, tracheo-esophageal fistula, renal anomalies, and limb abnormalities) 27. C curved tube: duodenum 28. Duodenal atresia occurs when second portion of duodenum fails to recanalize 29. Green vomit: Duodenal atresia presents with BILIOUS emesis (due to obstruction distal to ampulla of vater). ASSOCIATED WITH DOWN SYNDROME 30. Two fun domes with skull and X bones: X ray shows double bubble sign (one bubble of air in stomach and one in proximal duodenum) 31. Obstructing end of tube: distal intestinal atresia (jejunum or ileum) 32. Compressing red vascular hair: distal interstinal atresia is caused by in utero vascular accident (decreased blood flow to intestine->decreased delivery of oxygen+nutrients->impaired intestinal growth 33. Green vomit: distal intestinal atresia presents with bilious vomiting (due to obstruction distal to ampulla) 34. Distal intestinal atresia presents with abdominal distension (due to accumulation of air proximal to obstruction) 35. Violinist: Vitellineduct (omphalomesentric duct, connects ileum to yolk sac during fetal life or vitelline duct connects V(M)idgut to V(y)olk sac 36. Meckler hecklers: Meckle divertcilulum (true diverticulum in the ileum), forms if vitelline duct fails to obliterate 37. Gastric violin : Meckel diverticula can contain gastric mucosa (most common)and other ectopic issue, (pancreatic, endometrial etc) 38. Tarry black paint: Meckel diverticula can present with painless melena (functional ectopicgastric tissueulceration and bleeding 39. 2 signs: Meckel diverticulum occurs in 2% of population, exists 2 feet proximal to ileocecal valve, 2 inches in length, presents ~2 years of age, 2male:1female ratio 40. Technique book: Mecker diverticulum can be diagnosed with a technetium-99m pertechenate scan (gastric mucosa takes up technetium-99m) 41. Horse-spring ride: Hirschsprungs disease RECTAL SUCTION BIOPSY+Removal of non ganglion cells area 42. Migrating crest border: Hirschsprung develops due to failed neural crest cell migration (normally migrate from embryonic ectoderm into organs) 43. Disconnected plug: In Hirschsprung’s disease, the impaired migration of neural crest cells leads to absent innervation (absent neural ganglia) of distal colon (most likely includes rectum). 44. Tightly wound rectum spring: in absence of innervation, the rectal muscles remain contracted 45. Dilating “s” slinky: colon proximal to the constriction (sigmoid colon), fills with stool and dilated forming a MEGAcolon 46. Blackened stool stuck in spring: hirschsprungs disease presents with failure to pass meconium within 48 hrs of birth 47. Yo-yo not rotating: Intestinal malrotation (failure to undergo normal 270 degree counter clockwise rotation during fetal development 48. Yo-yo in RUQ pocket: intestinal malrotation, cecum is located in RUQ 49. String compressed belly: can cause duodenal obstruction (due to fibrouds bands called LADDS BANDS). Which connected abnormally located cecum to retroperitoneum 50. Distended belly and green face: intestinal malrotation, duodenal obstruction can leadto abdominal distension and vomiting 51. Knot in waist sweater: intestinal malrotation, twisting around Ladds bands can cause midgut volvulus (surgical emergency due to risk of bowel necrosis) 52. Death metal baby: Necrotizing enterocolitis 53. Small emancipated baby: necrotizing enterocolitis develops in premature and underweight infants 54. Baby bottle: necrotizing enterocolitis begins when some infant starts feeding (bacteria introducts into gut overpowers the immature gastrointestinal immune system) 55. Inner layer of bacterial wallpaper: necrotizing enterocolitis, bacteria invade the bowel wall 56. Necrotizing enterocolitis: presents with abdominal distension and bloody stools 57. Black outlines: Entercolitis causes pneumatosis intestinalis (pockets of gas in intestinal wall, causes black outlines of bowel lumen on X-ray) 58. Necrotizing enterocolitis can cause extensive bowel necrosis and death 1. Saddle bags: Diverticulosis 2. False mcusy teeth: colonic diverticula are false diverticular (herniated of mucosa and submucosa only) vs (herniation of mucosa, submucosa and muscularis in true diverticula) 3. Border: most colonic diverticula form on the mesenteric border 4. S snake: diverticula are most commonly found in the sigmoid colon 5. Red vines penetrating fence: vasa recta arteries penetrate the muscularis at the mesenteric border (creates weakening that facilitates diverticulum formation) 6. Plunger: chronic constipation is a risk factor for divertulosis (straining generates high pressure within the colon) 7. Dumping red: divertuclosis causes painless, hematochezia (vasa recta injury causes rupture) 8. Fire next to saddle bag: diverticulitis is a complication of divertuclosis 9. Leaking saddle bag: Diverticulitis is caused by perforation of a diverticulum (increased intraluminar pressure or congealed food particles->erosion of diverticular wall->perforation) 10. Flame bandan: divertulitis presents with fever 11. Diverticulitis presents with nausea/vomiting 12. Left lower abdominal fire: divertuclitis presents with LLQ pain (location of sigmoid colon) 13. Red inflamed pouch: divericulitis can cause abscess formation (can cause partial colonic obstruction) 14. Leaking poopy water: diverticulitis can cause fistulas (most commonly colovesical fistula>pneumatruai->pyuria, fecaluria) 15. Murkey pool: appendicitis 16. Obstructing rock: adults, appendicitis is most commonly due to obstruction from an inspissated fecalith (also fibrosis, malignancy or carcinoid tumor) 17. Soggy tissues: children, appendicitis is most commonly due to obstruction from lymphoid tissue, hyperplasia (follows infection) 18. Applying pressure: appendicitis leads to increased intraluminal pressure (obstruction>accumulation of mucus->distension->pressure on appendiceal wall) 19. Squeezing vascular sleeve: appendicitis, vessels and lymphatics in the wall of the appendix are compressed (due to increased intraluminal pressure) 20. Appendicitis can cause ischemia and necrosis (due to compression of vessels in appendiceal wall) 21. Fire next to murky pool: appendicitis causes inflammation 22. First responders: appendicitis, histology shows neutrophil infiltration 23. Appendicitis, bacterial overgrowth leads to bacterial invasion into the wall 24. Inflamed red pouch: appendicitis can lead to abscess formation 25. Perforating pouch: appendices can lead to perforation 26. Clutching mid abdomen: appendicitis initially presents with vague periumbilical pain (inflammation of visceral peritoneum is innervated by autonomic nervous system afferent fibers (T10 spinal root T10 dermatome) 27. Right -sides appendicitis presents with sharp localized RLQ pain (due to inflammation of parietal peritoneum (somatic afferent fibers) 28. Mcburnies lookout point: late appendices presents with localized RLQ pain at mcburnys point (1/3 between umbilicus and right anterior superior iliac spine) 29. Green face: appendicitis presents with nausea/vomiting 30. Flame bandana: appendicitis presents with fever (usually later ) 31. Relieving defecation: Irritable bowel syndrome (IBS), presents with vague abdominal pain relieved bydefecation 32. Water and clumpy dirt: IBS may present with diarrhea and/or constipation (varying consistency) 33. Radio frequency: IBS presents with varying bowel movement frequency 34. Twisted leash: large bowel volvulus (twisting of a portion of bowel around its mesentry) 35. Cactus roots: in volvulus, bowel twists at its mesenteric rotos 36. Dead cactus: volvulus can cause strangulation (leads to ischemia and necrosis) 37. Right gun pouch: children, volvulus occur in cecum 38. S snake: adults, volvulus occurs in sigmoid 39. Plunger: Chronic constipation most common risk factor for large bowel volvulus 40. Obstructed canyon: large bowel obstruction 41. Cancer crabs: malignancy is most common cause of large bowel obstruction 42. Large painful belly: large bowel obstruction presents with abdominal pain and distension 43. Green face dripping brown water: large bowel obstruction presents with nausea/vomiting including feculent vomiting 44. Collie: large bowel obstruction presents with colicky abdominal pain 45. Tink: large bowel obstruction presents with high pitched tinkling bowel sounds 46. Drumming: large bowel obstruction causes hyperresonance to percussion (due to gas filled bowel) 47. Dark clouds with horizontal base: X-ray, large bowel obstruction displays dilated loops of bowel (appears as dark pockets of gas) and air fluid levels (appear as horizontal contrast lines) 1. Fiery intestines: Inflammatory bowel disease (Ulcerative colitis and Crohn disease) 2. Young white guy: IBD is common in Caucasian and jewish people 3. Fiey hat: IBD presents with fever 4. IBD presents with weight loss: IBD 5. Clutching abdomen: IBD presents with abdominal pain 6. Brown puddle: IBD presents with diarrhea 7. Union canon: Ulcerative colitis (mucosal and submucosal) Ulcer means damage to mucosa and submucosa 8. Rusty rectal stool: Ulcerative colitis ALWAYS affects rectum 9. Rust travelling proximally: ulcerative colitis spreads proximally from rectum in a continuous pattern 10. Smooth end of canon: ulcerative colitis, colon has a “lead pipe” appearance on contrast enema (due to loss of normal haustral projections) 11. First respodners with perinuclear battle plan: pANCA (perinuclear anti neutrophil cytoplasmic antibibodies) are elevated in ulcerative colitis 12. Eroding through 2 layers: Ulcerative colitis, inflammation affects only the mucosa and submucosa 13. Dirt islands in hole: Ulcerative colitis, colon contains “Pseudopolys” (islands of normal mucosa within ulcerate tissue), loss of haustra 14. Inflamed cannonball within wall: histology shows abscesses with colonic crypts 15. Shrapnel striking left side: ulcerative colitis presents with left sided abdominal pain (due to location in rectum and distal colon) 16. Bloody puddle: Ulcerative colitis presents with blood diarrhea (frequent and small volume due to rectal inflammation) 17. Mega cannon: UC causes toxic mega colon (inflammation extends to colonic smooth muscle>smooth muscle paralysis->severe colonic dilation) 18. Exploding canon: UC, toxic mega colon can lead to perforation 19. Cancer crab belt: UC, increases risk of colon cancer (more then Crohn disease),Extent of disease spread and time length determine outcome to cancer. SMOKING IS PROTECTIVE AGAINST ULCERATICE COLITIS. 20. Scaly snake in billary tree: UC, increases primary sclerosing cholangitis (PSC) (autoimmune disorder of intra and extrahepatic bile ducts) 21. Cobble stones patches: Crohn disease (full thickness damage)occurs as multiple separate areas of disease (“skip lesions”) 22. Cobblestone path from mouth to anus arch: Crohn disease can affect any portion of the GI tract from mouth to anus 23. Antibody sac: Anti-saccharomyces cerevisiae are present 24. Hit on right waist: crohn disease presents with RLQ abdominal pain (due to location in ileum and cecum) 25. Debris-littered brown puddle: crohn disease presents with malabsorption of fats and fat-soluble vitamins (inflammation of distal ileum->poor reabsorption of bile acids->impaired absorption of fat) 26. MacroCages: crohn disease causes formation of non caseating granulomas (containing aggregations of macrophages) 27. Broken through all wall layers: Crohn disease causes transmural bowel inflammation 28. Tight abdominal gauze: Crohn disease can cause fibrotic strictures (transmural inflammation>bowel wall thickening->narrowed lumen) 29. Pulling strings: Crohn disease, X-ray shows “string sign” due to strictures 30. Obstructing rocks: Crohn disease, strictures can cause bowel obstruction 31. Fistulizing trench: Crohn disease can lead to fistulas (transmural inflammation leads to epithelization across bowel wall->connections between bowel and bladder, skin vagina or other bowel segments) 32. Pale erosions on mouth arch: Crohn disease causes aphthous ulcers in mouth and esophagus 33. Inflammatory bowel disease can cause arthritis (migratory polyarthritis, sacroiliitis, ankylosing spondylitis) (HLA-B27) 34. Red spots on shin columns: inflammatory bowel disease can cause erythema nodosum (painful erythematous nodular rash on shins) due to inflammation of fat cells 35. Skin wounds: inflammatory bowel disease can cause pyoderma gangrenosum (skin ulcers due to neutrophil dysfunction) not infectious or gangrenous 36. Shrapnel on kidney tray: inflammatory bowel disease can cause renal calculi (due to increased absorption of oxalate…calcium oxlate nephrolithiasis) 37. Red-rimmed goggles:inflammatory bowel disease can cause eye disease (anterior uveitis, iritis, episcleritits), (presents with eye pain and redness) 38. 5 pointed star: inflammatory bowel disease is treated with 5-ASA (sulfasalazine, mesalamine) 1. Mushroom caps: polys are outgrowths of mucosa most commonly found in colon (pedunculated or sessile or neoplastic vs non-neoplastic) 2. Hamartomatous hammer: hamartomatous polys (non neoplastic) 3. Hamartomatous polys are disorganized growths of mature cells 4. Happy old guy: hamartomatous polys are mature and benign 5. Peutz-pop: Pretuz-jeghers syndrome presents with hamartomatous polys in GI (commonly in duodenum) 6. Domino: Peutz-jeghers and juvenile polyposis syndromes (familial cause of hamartomatous) polys ) are autosomal dominant 7. Peutz-jeghers syndrome: presents with pigmented macules around mouth, lips, palms, gentalia 8. Infant with hammer: Juvenille polyposis syndrome common in children <5 and presents with hamartomatous polyps 9. Mushroom emerging from the behind: Juvenille polys are most common in rectum and may prolapse through anal sphincter 10. Bleeding mushroom: juvenile polyps present with lower GI bleeding (hematochezia) 11. Little mushroom spots: Juvenile polys display small cytic glands (filled with mucin and debris) 12. Creeping carb beetle: Juvenile polyposis syndrome is associated with increased risk of colon cancer (despite polys being benign) 13. Big hyperplastic mushroom: hyperplastic poly (non-neoplastic epithelial proliferation) 14. Happy lilpolyps: Hyperplastic polys are benign 15. Mucous-y goblet shrooms: Hyperplastic polys are epithelial proliferations that contain abundant goblet cells 16. Sawing near the surface: hyperplastic polys have serrated architecture only at the surface (crypts remain smooth shape) 17. Sawing on stalk-less mushroom Sessile serrated polyp ( premalignant flat lesion of the colon) 18. Sawing all the way through: Sessile serrated polyps have serrated architecture throughout (cryps included) 19. Creeping crab beetle: serrated polyps and adenomas have the potential to transform 20. Adding shingles to mushroom house: adenomatous polys (adenomas) are the most common type of poly 21. Creeping crab beetle: Serrated polyps and adenomas have potential to transform into cancer 22. Oversized mushroom next to crab beetle: larger adenomas are more likely to transform into cancer 23. 1 horn: adenomas >1cm are more likely to transform into cancer 24. increasingly disorganized purple weeds next to crab beetle: Adenomas with a greater degree of dysplasia (more hyperchromatic, elongated and stratified epithelium) are more likely to transform into cancer 25. Tubular horn: Tubular adenomas (small pedunculated polys composed of dysplastic mucosal cell that form tube-shaped glands) 26. Tubular perforations: tubular adenomas display round tubular gland across sections on histology 27. Finger-like stalk-less fungus: Villous adenomas (sessile, larger than tubular adenomas, long glands with villi-like projections). Progress to carcinoma if >2m, VILLOUS, SESSILE GROWTH 28. Villus fungus next to crab beetle: Villous adenomas are more likely to transform into cancer as compared to tubular adenomas 29. Polyp family: Family adenomatous poplyposis (FAP), inherited syndrome that causes thousand of adenomatous polyps early in life 30. Domino: FAP is AD 31. A pulled carrot: germline mutation in the APC gene causes FAP 32. Cancer fighting ribbon: APC is a tumor suppressor gene 33. A single pulled carrot stalk: in FAP, only one APC allele has a germline mutation (second mutation occurs during persons life time, referred to as a second hit 34. Abundant mushrooms: FAP presents with thousands of poyls 35. family crab beetle: FAP progresses to colon cancer in nearly 100% of cases (treated is prophylactic colectomy) 36. gardner with mushroom field: Gardner syndrome (FAP variant), presents with adenomatous polys and SOFT TISSUE TUMORS 37. Bone garden fence: Gardner syndrome presents with osetomas (benign bone tumor) 38. Ski nrash: Gardner syndrome presents with cutanoues lesions 39. Overgrowth sunglasses on gardner: gardner syndrome presents with hypertrophy of retinal pigment epithelium 40. Tooth gardening stool: Gardner syndrome presents with dental abnormalities (impacted and supernumary teeth) 41. Elder lillipolyp wearing tuban: Turcot syndrome (FAP variant), presents with colon adenomas and brain tumors (medulloblastomas) 42. Crab beetle attacking lilipolp: Colorectal cancer (most common adenocarcinoma-3rd most common cancer and 2nd most common cause of cancer death). S.Bovis will cause COLORECTAL CANCER. Second pathway is microsatellite sequences (unstable) 43. Old man lilipoly riding crab: peak incidence of colorectal cancer is 60-70 years of age, with men affected slightly more than women 44. Family photo: family history of colorectal cancer is risk factor 45. Smoker: smoking is a risk factor for colorectal caner 46. Alcohol bottle: alcohol use is a risk factor for colorectal cancer 47. Round lilipoly: obesity is a risk factor 48. Fiery intestines: inflammatory bowel disease is a risk factor 49. A pulled carrot: Mutations in APC gene can lead to adenomas or adenomatous polyps 50. Carrots: APC gene product controls concentration of beta-catenin and interacts with E-cadherin 51. Cancer-fighting ribbon: APC is a tumor suppressor gene 52. Cancerous rat: mutations in the L-RAS protooncogene leads to unstoppable cell divions. KRAS codes for a protein that regulates the cell cycle. 53. Mushrooms increase in size: adenomas increase in size as a result of mutations in K-RAS 54. Broken city wall: basement membrane invasion marks malignant transformation of an adenoma into an adenocarcinoma 55. Broken checkpoint: mutations in p53 gene contribute to malignant transformation ( a tumor suppressor) normally prevents G1 to S phase transition. 56. Broken “Don’t CCross”: deletetions in DCC (deleted colon cancer) contribute to malignancy which normally activates apoptosis pathway 57. Cauliflower on the right: Right sides colon cancer (proximal ascending colon) presents as an EXOPHYTIC mass (usually non-obstructive despite extension into the lumen) 58. Occult watchman dropping iron tools: Right sided colon cancer often presents with iron deficeny anemia (from occult GI bleeding) 59. “Path obstructed” on left: Left sided colon cancer (descending colon) may present with colonic bstruction (due to luminal narrowing from infiltrative ulcerative lesions), leading to change in bowel habits 60. Apple core on left: Left sided colon cancer can present with an “apple core” lesion on imaging due to luminal narrowing 61. Sitting in red puddle: Left sided colon cancer presentswith hematochezia 62. Periscope: Colonscopy is the gold standard for screening and diagnosis of colon cancer 63. Fibrous hat: a higher fiber diet decreases the risk of colon cancer 64. Aspirin umpire guard: regular aspirin use decrease the risk of colon cancer 65. “CEA”: carcinoembryonic antigen can be used to monitor progression or recurrence of colon cancer 66. Lynch worm: Lynch syndrome (hereditary non-polyposis colorectal cancer) most common familiar cause of colocrectal cancer (NO ADENOMATOUS POYLPS) 67. Dominos: Lynch syndrome is autosomal dominant 68. Mismatched colors; Lynch syndrome is caused by germline mutations in mismatch repair genes (MSH2 and MLH1) 69. Cancer fighting ribbon: mismatch repair genes (MSH2 MLH1) are tumor suppressor genes 70. One falling antennae: Lynch syndrome is caused by inheritance of one germline mutation (second mutation is acquired during persons lifetime) 71. Crab belt buckle: Lynch syndrome is also associated with increased risk of other (endometrial, ovarian, colorectal) *p53 with COX (ASPIRIN PROTECTS AGAINST COX PRODUCTION) APC (CHROMSOME 5) creates risk for development of polyp. Tumor suppressor gene (both copies must be knocked out) T: Depth of invasion N: Spread to regional lymph nodes M-Meteastatis : distance spread, most common site is liver Lactulose intolerance: Decreased function of the lactase enzyme found in the brush border of enterocytes. Lactase normally breaks down lactose into glucose and galactose. Presentation: abdominal distension and diarrhea upon consumption of milk products; undigested lactose is osmotically active. Cause: Deficiency may be congenital (rare autosomal recessive disorder) or acquired (often develops in late childhood); temporary deficiency is seen after small bowel infection (lactase is highly susceptible to injury). Celiac disease: Auto-immune-mediated damage of small bowel villi due to gluten exposure; associated with HLA-DQ2 and DQS. Presenttation: Diarrhea, bloating, abdominal pain. Dermatitis herpetiformis (herpes-like vesicles on skin). IgA deposits on Tip of dermal papillae. Pathophysiology: Gluten in in wheat and grains; contains GLIADIN. Once absorbed, gliadin is deamidated by tissue transglutaminase (tTG).Deamidated gliadin is presented by antigen presenting cells via MHC class II. 3. Helper T cells mediate tissue damage Labs: IgA antibodies against endomysium, tTG, or gliadin; IgG antibodies are also present and are useful for diagnosis in individuals with IgA deficiency (increased incidence of lgA deficiency is seen in celiac disease). Duodenal biopsy reveals flattening of villi, hyperplasia of crypts, and increased intra-epitheliallymphocytes . Damage is most prominent in the duodenum; jejunum and ileum are less involved. Solution: gluten-free diet. Late complications: Small bowel carcinoma and T-cell lymphoma. Tropical Sprue: Damage to small bowel villi due to an unknown organism resulting in malabsorption. Presentation: Similar to celiac disease except, Ocurs in tropical regions (e.g., Caribbean) and occurs after infectious diarrhea and responds to antibiotics . Complications: Damage is most prominent in jejunum and ileum (secondary vitamin B12 or folate deficiency may ensue); duodenum is less commonly involved. Whipple disease: Systemic tissue damage characterized by macrophages loaded with Tropheryma whippelii organisms; partially destroyed organisms are present in macrophage lysosomes (+Pas). Foamy Whipped Cream in a CAN. foamy macrophages, Cardiac symptoms, Arthralgias, Neurologic symptons Location: small bowel lamina propria Pathophysiology: Macrophages compress lacteals and chylomicrons cannot be transferred from enterocytes to lymphatics. Results in fat malabsorption and steatorrhea Abetalipoproteinemia: Autosomal recessive deficiency of apolipoprotein B-48 and B-100 B. Presentation: Malabsorption-due to defective chylomicron formation (requires B-48) Labs: Absent plasma VLDL and LDL (require B-100) Hereditary hemorrhagic telangiectasia: Autosomal dominant disorder resulting in thin-walled blood vessels, especially in the mouth and GI tract, rupture and might bleed. Pancreatic insufficiency: Chronic pancreatitis, Cystic fibrosis, or obstructive cancer. Causes malabsorption of fat soluble vitamin ADEK and B12. 1. Canal entrance: rectum 2. Cannal exit: anus 3. Tooth bridge: rectum and anus converge at denate pectinate line 4. Columnar bricks: Superior to the dentate line, tissue derived from the dnoderm (mucosa is COLUMNAR) 5. Squamous title: Inferior to the dentate line, tissue derived from ectoderm (mucosa is SQUAMOUS) 6. Rope plexus under stomach tower: Superior to dentate line, innervation is via the inferior hypogastric plexus 7. Automatic sensor: Superior to the dentate line, innervation is by autonomic nerves (inferior hypogastric plexus) which detects STRECH only, NOT Pain. 8. Pedaling: Inferior to the dentate line, innervation via the inferior rectal nerve 9. Pedaler in pain: Any pathology below the dentate line can cause PAIN (innvervation via somatic ncerves) 10. Schooners PORThole: Above dentate line, venous blood drains into PORTAL circulation 11. “Intentional Marine Vessel”: Superior to dentate line, venous blood travels via the superior rectal vein->inferior mesenteric vein->portal vein 12. Pudendal paddle boat: Below the dentate line, venous blood drains into Systemic circulation (infefrior rectal vein->internal pudendal vein->internal iliac vein) 13. Dilated arterio venous pipes: hemorrhoids are dilated vascular structures in the submucosa of the anal canal 14. Dilated upper pipes: Internal hemorrhoids occur above the dentate line 15. Bleeding dilated pipes: Internal hemorrhoids cause bleeding (blood coating stool or dripping after pooping) 16. Happy canal worker: Internal hemorrhoids are painless (due to autonomic innvervation) 17. Dilated lower pipes: External hemorrohids occur inferior to the dentate line 18. Thrombotic driftwood: thrombosis of external hemorrhoids can cause acute pain 19. Older man using plunger: hemorrhoids are associated with older adults and chronic constipation (opiods, straining and pooping) 20. Pregnant woman: hemorrhoids occur in pregnancy (increased intra-abdominal pressure and IVC compression->venous pooling and engorgement) 21. Connected pipes: Upper anus/lower rectum is a portcaval junction (portal venous system communicates with the systemic venous system) 22. Steaming PORThole: high pressure in portal venous system (portal hypertension) can cause hemorrhoids (pressure transmitted to systemic venous system) 23. Barge pushing through anal gate: rectal prolapse, rectum pushed through a weak pelvic floor>prolapse through the anus 24. Telescoping; rectal prolapse, the layers of mucosa fold on each other 25. Plungers: Chronic constipating can cause rectal prolapse 26. Old woman holding baby: Rectal prolapse occurs in elderly women with a weak pelvic floor (history of multiple pregnancies) 27. Kid coughing: whooping cough can cause rectal prolapse (coughing -> increased intraabdominal pressure) 28. Thick tree sap: cystic fibrosis can cause rectal prolapse (coughing and strained defecation) 29. Top of tree cleft: Pilonidal (between but cheeks) abscesses form at the natal cleft (located at top of gluteal cleft) 30. Hairy tree bulge: breakdown of hair follicles in natal clef->pit collecting debris and flora->infection->pilonidal abscess 31. Machete draining pus: a pilonidal abscess is a painful pustulent sacroccygeal mass 32. Inner tube dragged over puddle with sharp rocks: anal fissures are initiated by trauma to the anal sphincter (hard stool, severe diahrea, vaginal delivery) 33. Shaky lines: in anal fissures, stretching and tearing of anal sphincter->spastic response>worsening stretching and tearing 34. Posterior inner tube rider: majority of anal fissures are posterior near the midline 35. Hat flaps: many fissures have an anal tag 36. Anterior cobble stones with skip lesions: anterior anal fissures are associated with Crohns disease, infection 37. Pipe draining to ocean: ano-rectal fistulas run from anus or rectum to skin surface 38. Epithelial pipe: fistuals are tunnels that eventually become epithelialized 39. Radiation sign: pelvic radiation can cause anorectal fistuals 40. Skipped cobble stones: crohn disease can cause anorectal fistuals (transmural inflammation of bowel->sinus tracts->fistulas) 41. Hermit crab shell: squamous crab shell: squamous cell carcinoma is the most common anal cancer and displays keratinization (cross bridges, kertain pealrs) 42. Un-shelled crab: basaloid carcinoma (non keratinized squamouscell) of the anus arises near the dentate line 43. Crab with glandular sponde: rectal adenocarcinoma arises above the dentate line and behaves like colon adenocarcinoma 44. Pill-bugs: infection with high risk HPV (16, 18) is a risk factor for squamous cell carcinoma of the anus 45. White wizard hat: HIV infection is a risk factor for squamous cell carcinoma of anus 46. Crutches: immunocompromised states are a risk factor for squamous cell carcinoma of the anus 47. Smoker: smoking risk factor for squamous cell carcinoma of the anus 48. Kissing men: men who have sex with men have higher risk for squamous cell carcinoma of the anus 49. Pooling blood: anorectal cancer often presents with bleeding Pancreas/Gall bladder/ Liver Annular pancreas: congenital malformation due to pancreas forming a ring around duodenum. Acute pancreatitis: inflammation and hemorrhage of pancreas due to autodigestion of pancreatic parenchyma by pancreatic enzymes. Pancreas release enzymes which are inactivated to prevent autodigestion. If activated enzymes are released (trypsin) then it will cause auto immune damage. Liquefactive necrosis, fat necrosis (sponififcation,pancreas is surrounded by fat). Cause: Alcohol (contracts sphincter of Audi, back flow of enzymes), gall stones (clogs ampulla and will clog the pancreatic duct). I GET SMASHED (Idiopathic, Ethanol, Trauma, Steroids, Mumps, Autoimmune disease, Scorpion sting, Hypercalcemia (Ca2+ activates enzymes) /Hypertryglyceridemia. Clinical: Epigastric abdominal pain which radiates to back, Nausea, vomiting Lab: Serum lipase (more specific) and amylase (both secreted from pancreas), Hypocalcaemia (saponification will use up ca2+) Complications: Shock (loss of blood), Pancreatic Pseudocyst (fibrous tissue will surround the liquefactive necrosis). Pancreatic abscess (infected E.coli), DIC and ARDS (amylase can go into blood and eat coagulation factors and activate them, enzymes chewing on alveolar surfaces can cause acute respiratory distress syndrome) Chronic Pancreatitis: recurrent acute pancreatitis which cause fibrosis of pancreatic parenchyma Cause: alcohol, cystic fibrosis Clinical: Epigastric abdominal pain radiating to back, Pancreatic insufficiency (not producing any enzymes and cause fat soluble vitamin deficiency’s (ADEK) and seborrhea. Dystrophic calcification of pancreas (heavily calcified), present with secondary diabetes mellitus (due to damage of islets of Langerhans). Complications: Increased risk of pancreatic adenocarcinoma. Pancreatic Carcinoma: adenocarcinoma of pancreatic ducts in elderly. Risk factors: Smoking and chronic pancreatitis Clinical pain: epigastric abdominal pain and weight loss, Obstructive jaundice with pale stools and palpable gall bladder (if at head of pancreas), secondary diabetes mellitus (body or tail). (head of pancreas cancer, palpable gall bladder, blockage causes back up pressure into gall bladder and makes it palpable) (head of pancreas cancer, bile flow is obstructed and will leak into the blood instead, conjugated bilirubin, will leak into blood causing jaundice. Since bile does not leak into duodenum, you will not get mixing of bile and stool will be pale (stool color is caused by bilirubin) **Thin, elderly patient, think of pancreatic cancer, especially if presenting with DIABETES Clinical features: Pancreatitis, Migratory thrombophlebitis (swelling and tenderness in extremities), Serum tumor marker is CA 19-9 Surgery: Whipple procedure, remove head/neck of pancreas. VERY POOR SURIVAL (<1 year) Gall bladder/Billary Artesia Billary Atresia: Failure to form or destruction of extrahepatic biliary tree. One or more of the hepatic ducts exiting the liver are not formed. Presentation: jaundice (conjugated bilirubin as it leaks into blood and does not mix with pancreas) and progression to cirrhosis (back up of pressure destroys the liver). Cholelithiasis (gall bladder): cholesterol stones or bilirubin stones in the bile. Caused by supersaturation (cholesterol/ca2+), decreased phospholipids or bile acids, Stasis. Cholestyramine decreases bile acids and will cause gall stones. FFFF (female, fertile, Fat, fourty) CholestrUl stones: most common in west and radioULscent. . Risk factors: Age Estrogen (increase HM-Coreductase which makes more cholesterol, and increase Lipo protein receptors to on hepatocytes to increase cholesterol uptake. Clofibrate (increases HMG-CoA reductase and decreases bile acids), Native American Crohn Disease (terminal ileum damage decreases reuptake bile acids/salts), cirrhosis (decreased production of bile salts) BillirubOn stones: radiOpaque Risk factors: Extravascular hemolysis by Biliary tract infection (E.Coli, Ascaris lumbricoides and Clonorchis sinesis). (reticulo-endothelial system)Splenic macrophages break down hemoglobin into heme (iron +protoporhyn), protporhyn converted into UCB. Liver conjugates it (CB) and throws it into bile, increasing risk of bilirubin gallstones. Gallstones Complications Bilary Colic: Gallstones lodged in cystic duct. As it contracts, causes PAIN (waxing and weaning), symptoms relieved if it passes down the common bile duct but may obstruct common bile duct (increase the risk of acute pancreatitis or obstructive jaundice. Acute cholecystitis: Gallstone blocks the cystic duct, causes back up of pressure in gallbladder which causes decreased perfusion and leading to inflammation. Presentation: RUQ pain and RADIATES TO RIGHT SCAPULA, fever, HIGH WBC, Nausea and vomiting, Increased ALP (epithelium contains ALP, which is released when the wall dies), rupture risk Chronic Cholecystitis: Chronic inflammation of gallbladder due to chemical irritation, histology shows ROTIKANSKY-ASCHOFF sinus formation Presentation: RUQ pain AFTER EATING, Porcelain gallbladder (dystrophic calcification) is late complication Ascending cholangitis: Bacterial infection of Bile ducts due to ascending infection of gram – bacteria. Presentation: sepsis, jaundice, abdominal pain. Increased incidence with choledocholithiasis (choledochlithiasis: obstruction makes it easy for bacteria to ascend and infecdt the bile duct as the stone blocks flow, REMEMBER, ANYTIME YOU HAVE BLOCKAGE, THERE IS INFECTION IN ANY SYSTEM) Gallstone Ileus: Gallstone enters and obstructs small bowel because of cholecystitis causing fistula between gallbladder and small bowel. Air in Biliary Tree (pneumobilia) 6 Gallbladder carcinoma: adenocarcinoma rising from glandular epithelstooium that lines the gallbladder wall and gall stones with porcelain gallbladder is a major risk factor. Presentation: cholecystitis in elderly woman and poor prognosis . VERY OLD WOMAN WITH NEW ONSET CHOLESCYSTITIS, THINK ABOUT GALLBLADDER CARCINOMA. Liver Jaundice: yellow discoloration of skin, (especially scleral icterus) due to increased serum bilirubin Bilirubin Metabolism: RBC break down hemoglobin into Heme + globin. Heme becomes iron and unconjugated bilirubin which conjugates it and stores in gall bladder. Released from gall bladder into duodenum and intestinal flora takes CB and convert it into Urobilinogen, which makes urine yellow. Disease Etiology Lab findings Extravascular hemolysis/Ineffective erythropoiesis High levels of UCB which ↑UCB overwhelm the livers ability to conjugate. Clinical features Dark urine due to ↑urine urobilinogen. Remember that UCB is NOT water soluble and absent in urine. Urine is yellow color because of CB. ↑Risk of bilirubin gallstones Physiologic jaundice of the newborn Newborn liver has low UGT activity (enzyme responsible for conjugation) ↑ UCB UCB is FAT SOLUBLE. Deposit in basal ganglia, neurologic symptoms and death (kerinictus). Treatment: Phototherapy makes UCB urine soluble. GilbARt syndrome Low activity of UGT and AR Gilbert-Najjar syndrome NO UGT ↑UCB Jaundice during stress (infections) otherwise healthy ↑UCB Kerinicterus, fatal DubAR-Johnson syndrome No bilirubin transport ↑CB protein so it cannot be transpoted into the calculi. As concentrations build up inside, CB leaks into blood instead Dark Liver, Biliary tract obstruction Dark urine Gall stones, pancreatic ↑CB, ↑Alkaline Rotor syndrome: Exactly same , except NO BLACK liver. Viral Hepatitis carcinoma, cholangiocarcinoma, parasites or liver fluke phosphatse, ↓UCB Inflammation disrupts hepatocytes and small bile ducts ↑ CB and ↑ UCB Dark urine because of when you destroy ↑Urine bilirubin. hepatocytes, increase UCB because they cannot be conjugated. When you destroy renal ducts, CB leaks into blood Whats in bile? CB, ALP, Cholestrol. Obstruction will cause leakage into blood (bilirubinuria) and pale stool, pyruritis (due to increased plasma bile acids), hypercholesteremia with xanthomas. Setorrhea with malabsorption of soluble vitamins. Viral hepatitis: inflammation of liver parenchyma due to EBV, CMV and hepatitis Acute hepatitis: Jaundice (Mixed CB and UCB) and <6 months Lab: ALT>AST Chronic hepatitis: 6> months. Virus Transmission Comments Hep A/E Fecal-Oral Hep A: travellers Hep E: undercooked food/water Acute hepatitis IgM=ACTIVE INFECTION IgG=Immunized or resolved infection *HEP E with pregnancy causes fulminant hepatitis (liver necrosis) Hep B Acute hepatitis (*Look at table below) Parenternal transmission (child birth, unprotected sex, IV drug use) Hep C Parnertal , IV Acute to chronic *Look FOR HCV-RNA to CONFIRM IFNECTION. Persistence of RNA indicates chronic disease Hep D Preexisting Hep B, then get Hep D, called superinfection (MORE DEADLY) Hep B + D at same time is coinfection). Stage HBsAG HBeAG HBcAB (surface antigen) (envelope) (core) Means that virus can be transferred to another person HBsAB (surface antibody) Acute + (first marker) + IgM (*Acute marker) - Window - - IgM - Resolved - (because IgM has - (resolved destroyed surface because IgM has antigen) destroyed envelope) IgG (Appearance IgG (protective) means that IgM was successful and acute infection has resolved). IgG is then activated to be protective. Chronic + ( >6 months then IgM failed, your in chronic hepatitis now) +/- IgG 1. Inflammation - - - IgG Cirrhosis: End stage liver damage via bands of fibrosis and regenerative nodules Pathophysiology: Fibrosis is mediated by TGF-B from Stellate cells Complications Portal HTN: Splenomegaly/ hypersplenism, portosystemic shunts (esophageal varices, Catpud medusa, hemorrhoids) , hepatorenal syndrome (renal failure) Decreased detoxification: Mental status changes, coma jaundice gynecomastia, spider angiomata, palmar erythema *Liver removes estrogen (gyno, spider angiomata, erythema), mental changes due to increased ammonia (cannot remove if liver crossed) Decreased protein synthesis: hypoalbuminemia (decrease oncotic pressure and cause edema), coagulopathy (cannot make coagulation factors or Vit K via epoxide reductase) Alcohol-Related liver disease (AST>ALT) Fatty liver accumulation of fat in hepatocytes and reversible. Alcoholic Hepatitis: binge drinking and damage mediated by acetaldehyde . swelling and ballooning with Mallory body (damaged intermediate filaments) (bottom right). Cirrhosis: Same as above cirrhosis NON-Alcohol-Related liver disease (ALT>AST) Hemochromatosis: Excess Iron deposits in organs, damaged caused by damage of free radicals (fenton reaction) Primary (defective HFE gene (C282Y) allows more Iron to enter blood, see image above) vs Secondary hemochromatosis (Blood transfusions, every bag of blood is bag of Iron) Presentation: Iron deposits in all organs ->Cirrhosis, secondary diabetes, bronze skin, cardiac arrythmia, gonadal dysfunction Lab: ↑Ferritin, ↓TIB , ↑Serum iron, ↑% saturation Biopsy: Brown pigment in hepatocytes. Brown pigment can be IRON or LIPOFUSCIN (wear and tear pigment). Differentiate between them, use Prussian blue stain, turns Iron BLUE Treatment: Phlebetomty (remove RBC), may cause hepatoceullular carcinoma WERlson disease: defects in (ATP7B gene), in ATP-mediated hepatocyte copper transport. Lack of transport of copper into bile and put into ceruplasmin (molecule which carried Cu2+ in blood) Pathogenesis: builds up in hepatocytes and leaks in serum, Cu+ mediated production of hydroxyl free radicals lead to tissue damage. Presents in child hood. Complications: Neurologic (present similar to other neuro degenerative diseases) , KAYSERFLEISHER RINGS in cornea, Labs: Increased Urinary copper, Decreased serum ceruplasmin, Increased copper in liver biopsy (copper cannot be put into bile) Treatment: D-penicillamine Primary Biliary Cirrhosis: (direct damage to bile ducts) granulomatous destruction of intrahepatic bile ducts, autoimmune (women) Etiology: ANTIBMITCONDRIAL ANTIBODY Clinical: Obstructive jaundice Primary Sclerosing Cholangitis: Inflammation and fibrosis of intrahepatic and extrahepatic bile ducts Histology: onion skin appearance or string of pearl appearance. Labs: P-ANCA + and Associated with ULCERATIVE COLITIS Clinical: Cirrhosis and cholangiocarcinoma Reye syndrome: Complete liver failure due t viral infection worsened with ASPIRIN USE IN KIDS. Pathogenesis: mitochondrial damage of hepatocytes Labs: hypoglycemia, elevated liver enzymes, death Liver tumors Hepatic Adenoma: benign tumor of hepatocytes associated with use of ORAL CONTRACEPTIVES Complications: Rupture and intraperitoneal hemorrhage, especially in pregnancy Liver tumor Risk factors: Chronic Hepatitis, Cirrhosis, ALFATOXINS (induce P53) DERIVED FROM ASPERGILLUS. Budd-Chiari syndrome: Central lobular congestion and fibrosis Another example of budd chiari would be constructive pericariditis which increases venonus pressure on liver. Hepatocellular carcinoma , poor prognosis. TUMOR MARKER IS AFP. Metastasis to liver: colon, lung, pancreas, breast. Multiple nodules in liver UWORLD Stress related mucosal disease: Shock trauma>hypovolemia/hypotension->local ischemia->Decreased mucosal protectonUlcer formation OR Intrascranial disase->vagal stimulation->Increased H+ secretion->Ulcer formation Comon tumor markers Maker Tumor Alpha-fetoprotein Germline/Hepatocellular carcinoma CA19-9 Pancreatic cancer Ca125 Ovarian (Endometrial) CEA Gastrointestinal (colorectal) HcG Choriocarcinoma/Germ cell Prostate specific Antigen prostate Hepatocellular Carcinoma by HEPTATITUS: virus generates local cytokines (pro inflammatory) and cause hepatocyte damage and fibrosis. Hepatic fibrosis will show malignancy cells (pleomorphic, prominent nucleoli, high nuclear to cytoplasmic ratio). Common hereditary Cancer syndromes Syndrome Gene Associated cancers AUTOSOMAL DOMINANT caused by inactivating tumor suppressor gene. Deletion of remaining allele (Second) causes loss of heterozygosity and malignant transformation potential. Lynch MHSC1 Colorectal cancer, syndrome MHSC 2 ovarian cancer, Endometrial cancer FAP APC Colorectal cancer, Desmoids and ostemoas , Brain tumors Von hippel VHL lindau sayndrome Hemangioblastomas, Clear cell renal carcinoma, Pheocytochroma Li-fraumeni TP53 syndrome Sarcomas, Breast cancer, brain tumors, Adrenocoritcol carcinoma , leukoemia, MEN 1 MEN1 Parathyorid adenomas, pituairty adenomas, pancreatic adenomas MEN 2 A RET Pheocytochroma MEN 2B Activating Medullary thyroid (gain of function) in carcinoma proto onco Pheochromycytoma, gene with Mucosal neurons + continuous cell RET and marfanoid division habitus (Tall thin long limbs) How would you differentiate between ZES and hypergastrienmia(acute gastritis?). Secretin test normally decreases gastrin but WILL NOT DECREASE gastrin in ZES. Rule this to rule out other tests. Also ulcers found beyond duodenal bulb will suggest ZES. Bile sludge: Bile sludge is caused by gastric hypomotility and is seen with more precipitates. Black or brown: Brown = infections. Black from hemolytic anemias or increased enterohepatic recycling of bilirubin (crohn disease) Cystinuria: AR condition and defect in amino acid transporter gene causing elevated urine cysteine levels. Cystine kidney stones present in childhood. Uric acid kidney stones: Turnor lysis syndrome (more uric acid producted) of thiazides ( causing less uric acid excretion) cause hyperuricemia and stones. Cystic fibrosis: thick, dehydrated and viscous mucus in organs with absence of vas deferens. Lungs (Thick secretions), GI (malabsorption, biliary disease), sweat glands (salty tasting). CFTR responsible for bringing in water and CL into cell. Cystic fibrosis clinical features (Chromosome 7) Respiratory Obstructive lung disease (bronchiectasis), recurrent pneumonia, chronic rhinosinusitis Gastrointestinal Obstruction->meconium ileus (NEWBORNS) or distal obstruction Pancreatic disease Billary Cirrhosis Reproductive Infertility (no vas deferens but normal sperm) Muscuoloskeletal Osteopenia->fractures Kypholiscyosis (SPINE deformity) Digital clubbing: Bronchopulmonary sequestration: Congenital malformation where lung is not connected to airway. Common variable immunodeficiency: Defect in B cell differentiation (low plasma and immunoglobins). High risk for auto immune, lung infections, Lymphoid). Save for IMMUNO. Bacterial peritonitis: dull appearing peritoneal surface with viscous white yellow-surface Familial hypercholestremia: AD, ldl receptor mutation in liver (cannot uptake cholesterol). IBD can cause Colorectal cancer. Ulcerative colitis>pancolitis->colorectal cancer. Clitis-associated colorectal cancer occurs in chronic inflammation and risk is proportionate to duration and severity of inflammation. Another way you can get colorectal cancer is sporadic (Radnomly) but effect elderly and present later on witih p53 gene mutation but early APC. colitis associated vs sporadic colorectal cancer Colitis-associated Sporadic Age Younger (40-55) Older >60 Origin of dysplasia Flat lesions (non Polypoid (lesions) polypoid) lesions Location Proximal >distal particulary with CD Distal>proximal Tumros Multifocal Singular Histology Mucionuss/signet Rarely mucinious ring cells Mutations: Early P53 mutation Early APC gene Late APC gene mutation mutation Late p53 mutation Anatomy of Colon blood supply: Question ID 413 Seborrheic dermatitis: scaly, greasy skin on scalp, face , ears, eyebrowns/eye lids in Parkison disease and HIV Causs of Cholestasis Intrahepatic Drug (erythromycin, contraceptives) Primary biliary cholangitis Cholestasis/Pregnancy Extrahepatic Choledoclithliasis Malignany (gall bladder, pancreatic cancer) Cyptococcus neoformans: yeast with a polysaccharide capsule that can be detected with india ink stain and can infect ANY organ. Pancreatic serous cystadenoma: benign tumor of pancreas, associated with VHL disease. Histology shows glycogen rich cuboidal epithelium. Intrapapillary mucinous neoplasm: atypical cells forming papillary projections and are benign tumors with malignancy potential. Pathogenesis of granulomas with Th1 and Th2 usmle ID 406 C.Difficle Risk factors Recent antibiotics, Hospitalization, PPI Pathogenesis Disruption of intestinal flora Exotoxins cause mucosal injury Pseudomembrane formation Clinical presentation Diarrhea, fulfilment colitis (common) Diagonisis EIA (enzyme immune essay) for bacterial toxin or glutamate dehydrogenase Treatment Oral vancomycin or fidaxomicin MICRO question->USMLE id 1396 Question ID 1143->Micro question again ID 431: Biochem last 2 options->go over, xanthine oxidase and also go over Glutamate dehydrogenase Fibroid necrosis : deposition of protenious material in blood vesels due to HTN Intragluteal pilonidal disease: acquired skin infection of natal cleft of buttocks. May present with draining sinus tracts, abd tenderness but NOT diarrhea. Entamoeba histolytica : amoebic dysentery which is hematochezia, abdominal pain, FLAST SHAPED ULCERS. PHARM (Vomitting) Pharmacology ok 1. 2. 3. 4. 5. Solitary track runner: the nucleus tractus solitaries (NTS, or vomiting center) located in the medulla, receives inputs from the GI tract, vestibular system, and area postremia Vomiting on track: the NTS projects neurons to other medullary nuclei to coordinate the vomiting response Stomach hammer throw area: The GI tract blood barrier (bb) communicates directly with the NTS (via CN X) Vegas sign at the stomach area: vagal afferents from the GI tract communicate with the NTS Smiley hammer at the stomach area: GI irritation (due to infection, chemotherapy, distension) causes mucosal serotonin release. 6. 17. (diphenhydramine, Meclizine) treat vestibular nausea (motion sickness) 18. 19. 9. 10. M1 motorcycle parking: the vestibular system contains M1 muscarinic receptors 20. Telescope: scopolamine (muscarinic agonist) treats vestibular nausea (motion sickness) 21. Seasick Sailor outfits: motion sickness (vestibular nausea) is treated with 1st generation H1 antagonists (diphenhydramine) and scopolamine 22. 7. 8. Bee swatters: 1st generation H1 receptor blockers “1-2-3” Hammer Throw!”: serotonin activates 5HT-3 receptors on the vagal afferents Semicircular canal: the vestibular system communicates directly with the NTS (via CN III) 23. Vests at the semicircular canal: the vestibulocochlear nerve (CN 24. III) from the vestibular system communicates with the NTS Seasick at the canal: the vestibular system is responsible or vertigo and 11. motion sickness (vestibular nausea) Tickler blocking the D-rings: metoclopramide antagonizes D2 receptors in the area postrema (treats chemotherapy induced vomiting) 25. 26. 27. Extreme postures on the pommelhorse next to the track: the area postrema 12. (chemoreceptor trigger zone) is located adjacent to the NTS (outside the BBB th 13. in the 4 ventricle) and responds to emetogenic substances (chemotherapeutic agents) 16. (treats chemo-induced or post-op vomiting) Hammer tightening gut: ondansetron can cause constipation Hammer hitting head: Ondansetron can cause headache and dizziness Twisted torsade’s streamer: ondansetron can prolong the QT interval and induce torsade’s Pile of smiley faces: Ondansetron can cause serotonin syndrome (symptoms include rigidity, tremor, hyperthermia, confusion) Allergy inducing, Q shaped dandelions: the vestibular system contains H1 histamine receptors (coupled to Gq) Contracted stomach: metoclopramide has upper GI prokinetic effects (increased esophageal peristalsis, decreased lower esophagus sphincter pressure, and enhanced gastric emptying) (useful for treatment of delayed gastric emptying due to postsurgical disorders and diabetic gastroparesis) 28. “Do not obstruct”: metoclopramide (D2 Antagonist) is 29. 14. Ribbon dancer blocking the hammer throw: Ondan”setron” antagonizes 5-HT3 receptor on vagal afferents in the GI tract (decreases vagal 15. stimulation) Extreme posture 2 D-Ring ropes: the area postrema contains D2 receptor 30. contraindicated in small bowel obstruction Adverse effects Mud puddle: metoclopramide can cause diarrhea (prokinetic effects) Sleeping judge: Metoclopramide can cause drowsiness, especially in the elderly Crying coach: metoclopramide can cause depression (central D2 blockade) EXTRA pyramidal newspaper hat: metoclopramide can cause extrapyramidal effects due to central D2 blockade (dystonia, akathisia, parkinsonian features) Sticking out tongue: metoclopramide can cause tardive dyskinesia with chronic use (central D2 blockade), especially in the elderly 1. Now More Spicy chicken: metoclopramide (D2 antagonist gonist) can cause neuroleptic malignant syndrome (symptoms include fever, rigidity, mental status changes, autonomic instability, rhabdomyolysis) 2. Elevated milk release: metoclopramide can cause elevated prolactin levels (central D2 blockade), leading to gynecomastia, amenorrhea, and decreased sexual drive 3. Twisted torsade’s streamer: metoclopramide can cause QT prolongation and induce torsade’s 4. plaNK1 pommel horse: the area postrema contains neurokinin 1 (NK1) receptors (activated by substance P) 5. Substance Pee check: substance P binds to the NK1 receptors in the area postrema 6. “participants”: aprepitant antagonizes the NK1 receptors in the area postrema (treats chemotherapy induced vomiting), the “a preppy aunt” is a better mnemonic 1. 2. 3. 4. 5. 6. “pour it all”: parietal cells in the gastric mucosa are responsible for acid secretion Battery powered puree pump: H+/K+ ATPase (proton pump) on the luminal membrane pumps H+ into the lumen Banana into the pump, lemons out: the H+/K+ ATPase exchanges one K+ for one H+ at the luminal membrane Sidewalk: lumen of the stomach Three P batters: ATPase driven process 7. 8. Bees swarming honey pot: histamine (released by the ECL cell) activates H2 receptors on the parietal cell Honey pot with 2 “S” handles: H2 histamine receptors 9. (coupled to Gs to increase cAMP) on the basolateral membrane Honey pot kid knocking over acid pitcher: 10. activation of H2 receptors upregulates the H+/K+ ATPase 11. increased acid secretion 12. 13. Enter CarefuLly: enterochromaffin –like (ECL) cells Bees released from ECL tree: the ECL cell releases histamine (activates the parietal cells) 14. Gas Powered blower releasing bees from ECL tree: gastrin 20. Tie dye t shirt: “-tidine” suffix of H2 receptor antagonists (ranitidine, cimetidine, famotidine, nizatidine) @ antagonists reduce the acid secretion that is mediated by histamine, this comes from the enterocrhomaffin like cell, this cell is initially by gastrin by the G cell, which is brought on by vagal stimulation. So H2 blockers work with Histamine, gastrin, and Vagal stimulation. But Vagal stimulation will also stimulate the parietal cell directly to secrete acid. H2 blockers are used at night to prevent nocturnal secretion of acid that is largely dependent on histamine, but only a modest effect on meal stimulation because vagus nerve will stimulate Parietal cells directly 21. Gargling: H2 blockers (ranitidine, cimetidine) treat GERD (PPI’s are first line) 22. 23. Ulcerated sidewalk: H2 blockers (ranitidine, cimetidine) treat duodenal ulcers (PPI’s are first line) Tie dye kid on the cement: cimetidine (H2 blocker with 24. antiandrogenic side effects) 25. Dented chrome bumper: Cimetidine inhibits cytochrome P-450 26. Pot lids on chest: cimetidine can cause gynecomastia when used 27. long term or in high doses 28. Droopy honey wand: cimetidine can cause impotence Milk shooting from nose: cimetidine can cause elevated serum prolactin levels 29. Girl scout blocking puree pump: Proton Pump Inhibitors (PPI’s) 15. (released by G cells) stimulates the ECL Cell to release histamine 30. irreversibly inhibit the H+/K+ ATPase (the final common Gas truck releasing gas tanks: G cells release gastrin (Which pathway for H+ secretion) stimulates ECL and parietal cells) 16. Gas powered acid pump: gastrin (released by G cells) stimulates 31. PRIZE: “-prazole” suffix of PPI’s (omeprazole, lansoprazole, the parietal cell to secrete H+ (minor effect) gastrin’s major 17. rabeprazole) effect is release of Histamine from ECL cells 32. 18. Motorcycle attached to stand in M3: M3 acetylcholine receptors are located on the parietal cell 19. Vegas sticker: vagal stimulation stimulates the parietal by the vagus nerve (M3 receptor) Vegas Sticker: vagal stimulation stimulates the G cell to release gastrin (VIA GRP) Gate release pull: gastrin releasing peptide (GRP) from the vagus nerve activates G Cells Gargling: H2 blockerrs (ranitidine, cimetidine) treat GERD but PPI’s are the first line Ulcerated sidewalk: PPI’s provide faster symptom relief for gastric and duodenal ulcers Jumbo gas tank on mower with crab logo: gastrinoma causing hypersecretion of gastric acid (Zollinger-Ellison syndrome – treat with PPI’s) 1. Swarm of bees over lawn mower: extra gastrin will stimulate parietal cell directly with increasing Histamine, PPI’s are the best medical treatment 2. Helicopter hat: PPI’s treat H.Pylori infection, with clarithromycin or amoxicillin/metronidazole 36. Adverse effects 1. Chocolate fondue fountain: PPI’s increase the risk for C.Diff infection 2. Dirty lung spots: PPI’s increase the risk for respiratory infections (pneumonia) 3. Medals bound to wagon: PPI’s decrease the absorption of Ca2+, Mg2+, and Fe2+ (requires acidic environment) 4. Fractured Axel: PPI’s increase the risk of osteoporotic hip fractures (due to decreased Ca2+ 2 bee swatters: H2 histamine receptor antagonists (rani”tidine”, cimetidine) inhibit acid secretion by parietal cells absorption) 10. 5. Porous wood: PPI’s may worsen osteoporosis (due to decreased Ca2+ absorption) 6. Falling magnets on girl scout: PPI’s can cause hypomagnesia 7. Stop sign: Somatostatin (octeoride ) inhibits release of histamine by ECL cells 8. Stop sign: Somatostatin (SST) inhibits the release of gastrin by G cells (and SST receptor positive gastrinomas) 9. Octagon shape of stop sign: octreotide (a long acting SST analog) inhibits ECL production Octagon: octreotide (a long acting SST analog) inhibits G cells (useful in the treatment of gastrinoma/Zollinger Ellison syndrome 1. Spa water: osmotic laxatives (magnesium compounds, lactulose, polyethylene glycol) are non-absorbable substances that draw water into the intestinal lumen and cause distension and peristalsis 2. 3. 4. 16. Magnets magnesium compounds (magnesium hydroxide (milk of magnesia), magnesium citrate) are osmotic laxatives PEG drain cover: polyethylene glycol (PEG) is an osmotic laxative (non absorbable sugar), commonly is iso electrolytic so not to draw electrolytes into the lumen (used for complete GI emptying before colonscopy) 5. 6. Relaxulose: lactulose is an osmotic laxative (non absorbable sugar) sever flatus and cramps may be AE’s Relaxulose into the liver and brain coral tank: lactulose is useful 7. 14. Stimulating suntan lotion: senna is a stimulant laxative a.k.a cathartic (stimulation of enteric nervous system and colonic secretions) 15. Brown gut: chronic use of senna causes melanosis coli (brown pigmentation of the colon) in the treatment of hepatic encephalopathy 17. Muddy slippers left outside: antidiarrheal agents (featured in massage room) Utopia: Opiate agonists (diphenoxylate, loperamide) treat 18. diarrhea MUssage: opioids treat diarrhea by activating u-opioid receptors 19. in the GI tract Lop-eared rabbit: Loperamide treats diarrhea (u-opioid agonist that does not cross the BBB (no analgesia or potential for 20. addiction) Loop eared rabbit hopping back and forth: opioid agonists (loperamide) increase colonic phasic segmenting activity which 21. increased colonic transit time 0 Dolphins: Diphenoxylate treats diarrhea (u-opioid agonist with some ability to cross the BBB (combines with atropine to prevent 22. abuse) Red stool and inflammatory candles outside door: antidiarrheal Cirrhotic liver and brain coral: hepatic encephalopathy (a 23. agents are contraindicated in patients with bloody diarrhea or neurologic complication of cirrhosis due to the buildup of 24. fever (treat the underlying cause) Clogged: opioids can cause constipation 9. ammonia ( NH3+) and other toxins) as ammonia gets shunted past the liver and ends up in the brain, leads to the rhythmic 25. VIP CUSTOMERS only crab: VIPoma and carcinoid tumor cause flapping of hands (asterixs) secretory diarrhea, pancreatic endocrine tumor secreting VIP Fish eating lactulose: intestinal bacteria metabolize lactulose 10. STOP sign: Octreotide treats the symptoms of VIPoma and into acidic metabolites carcinoid syndrome (secretory diarrhea) Acidic pH meter: acidic metabolites decrease the pH of the intestinal lumen 11. 12. Worker on the NH4+ release valve carrying the ammonia bottle: ammonia (NH3) is trapped as ammonium (NH4+) in the acidic lumen and excreted Fisherman removing fish: rifaximin (a poorly absorbed antibiotic) eradicates ammonia producing intestinal bacteria 13. (treats hepatic encephalopathy) 8. Spoiling mud bath: laxatives can cause diarrhea and dehydration Bulky seaweed outside of the shop: psyllium is a bulk forming laxative (indigestible hydrophilic colloid causes water absorption, distension and peristalsis. Water penetrating a canoe at the DOCK: docusate is a stool softener (surfactant agent that facilitates penetration pf stool by water and lipids)