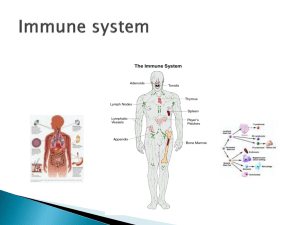
Immune organs and tissues Shijie Sun (Associate Prof.) Department of Immunology, DMU KEY POINTS: • To master: – The components of human immune organs and tissues, and their functions • To be familiar with: – The function of MALT • To understand: – Lymphocyte homing; lymphocyte recirculation Basic Components of the Immune System Immune organs Immune cells Immune molecules Basic Components of the Immune System Immune organs Central lymphoid organ Peripheral lymphoid organ bone marrow spleen thymus lymphoid nodes MALT Immune cells Immune molecules Membranous Stem cell Lymphocyte Monocyte macrophage Dendritic cells mononuclear Other cell Granulocytes Mast cell Platelets Erythrocyte TCR BCR CD Molecule MHC Adhesion molecule secretory Ig Complement cytokine Central (primary) lymphoid organs bone marrow, thymus To provide a microenvironment necessary for lymphocytes maturation. Peripheral (secondary) lymphoid organs To trap antigen and provide sites for mature lymphocytes to interact with that antigen. Spleen,lymph nodes,MALT 1. Central (primary) lymphoid organs (1) Bone Marrow Function : microenvironment for i the developing of blood cells and immune cells ii B cell and NK cell maturation iii humoral immune response Self-renewing stem cell Lymphoid progenitor Myeloid progenitor Pluripotent stem cell Natural killer (NK) cell B lymphocyte T lymphocyte Erythroid CFU Megakaryocyte Basophil CFU Eosinophil CFU Granulocyte-monocyte CFU Erythrocytes Platelets Basophils Eosinophils Neutrophils monocyte Hematopoietic inductive microenvironment, HIM 1. Stromal cells, such as macrophage, fibroblasts, reticular cell, endothelial cells. 2. Hematopoietic growth IL3,4,6,7,SCF, GM-CSF,etc. factors, including 3. Extracellular matrix: Function: To provide environment for hematopoiesis and regulate cell survival, proliferation, differentiation and trafficking. Case 1. SCID Q1: Why could the bone marrow transplantation treat SCID? Q2: How to find the suitable donor? Q3: Would you like to be a volunteer to donate your BM or stem cells? (2) Thymus Cortex: outer compartment, is densely packed with immature T cells, called thymocytes. Medulla: inner compartment, is sparsely populated with thymocytes. Function: To secrete various hormones; promote the differentiation of thymocytes. DN cell Cortex cortical epithelial cell DP cell macrophage Dendritic cell Medulla cell SP cell cell medullary epithelial cell Enter peripheral lymphoid tissues and organs T cells differentiate in thymus Athymic nude mice (Foxn1nu) a nature animal model for T cell selective deficiency Athymic nude mice are kept behind a barrier with HEPA filtered air, autoclaved fee, bedding, water and cages. A research assistant uses aseptic procedures to protect these mice from organisms in the environment. DiGeorge Syndrome This disorder typically results from various deletions in a region on chromosome 22q11.2 containing up to 50 genes, with the T-box transcription factor (TBX1) thought to be most influential. Q: could the Digeorge syndrome be treated with bone marrow transplantation? 2 Peripheral (Secondary) lymphoid organ Lymph nodes Spleen Mucosa-associated lymphoid tissue (MALT) Generative lymphoid organs Peripheral lymphoid organs Recirculation blood B Bone marrow stem cell lymphocytes lineage Bone marrow Lymph node Spleen Mucosal and cutaneous lymphoid tissues Mature B lymphocytes T lymphocytes lineage Blood, lymph Thymus Mature T lymphocytes Recirculation Maturation of lymphocytes (1) Lymph nodes Structure of lymph nodes Cortex cortex: B cell riched zone paracortex: T cell riched zone、 HEV Medulla Function of lymph nodes 1. Home for mature T/B lymphocytes T: 75%, B: 25% 2. Main site for adaptive immune response DC, FDC 3. Lymphocyte recirculation 4. Physical and biologic filters: Mφ (2) Spleen Structure of spleen T cell zone HE (IHC) B cell zone (IHC) Function of spleen: 1. Home for T/B lymphocytes B: 60% , T: 40% 2. Main site for adaptive immune response 3. Synthesize some complement components 4. Physical and biologic filter (3) Mucosa-associated lymphoid tissue (MALT) or mucosal immune system (MIS) The organized and diffuse lymphoid tissues found in submucosal regions of the body, such as alimentary, genitourinary and respiratory tracts. For example: tonsils, Peyer’s patches, vermiform appendix ,etc. A solitary lymphoid nodule in the large intestine. This nodule is localized in the mucosa and submucosa of the intestinal wall. 1.Appendix of a 10 year old 2.Appendix from a 36-year old man Secrete antibodies across the mucosal surface Local (mucosal) immunity Immune response in intestinal lymph system sIgA Mucosal epithelium M cell Macrophage IgA Th B Plasma cell 3 Recirculation of lymphocytes Homing : primary →→→secondary Recirculation : secondary →→→secondary secondary →→→tissue Native T cell Lymph node without antigen Blood vessel Activated T cell High endothelial venule Peripheral tissue site of infection/inflammation microbes Efferent lymphatic vessel Lymph node with antigen Afferent lymphatic vessel Lymphatic vessel Peripheral blood vessel Efferent lymphatic vessel Thoracic duct Pathways of T lymphocyte recirculation Summary Quiz: Q: All blood cells in an adult human can trace their ancestry to which compartment within the body? A.Thymus B.Bone marrow C.Lymph node D.Peyer's patch E.None of the above Quiz: Q: All blood cells in an adult human can trace their ancestry to which compartment within the body? A.Thymus B.Bone marrow C.Lymph node D.Peyer's patch E.None of the above A: B Quiz: Q: Which of the following is NOT considered as primary lymphoid tissue? A.Draining lymph node B.Thymus C.Peyer's patch D.Choices A and C are not primary lymphoid tissue. E.None of the above is primary lymphoid tissue. Quiz: Q: Which of the following is NOT considered as primary lymphoid tissue? A.Draining lymph node B.Thymus C.Peyer's patch D.Choices A and C are not primary lymphoid tissue. E.None of the above is primary lymphoid tissue. A: D Case 1. SCID Q1: Why could the bone marrow transplantation treat SCID? Q2: How to find the suitable donor? Q3: Would you like to be a volunteer to donate your BM or stem cells? Case 2. Elizabeth Bennet was born with a low body weight of 2.1 kg, and dysmorphic facial features were noted, including low-set ears as well as a relatively small mouth with an undersized lower jaw (micrognathia) . At 2 days of life, Elizabeth developed feeding difficulties, rapid breathing, increased fatigue, and a bluish discoloration of the skin. At 4 days of age, Elizabeth developed seizures. She was found to have very low blood levels of calcium (6.2 mg dl–1, normal 8.5–10.2 mg dl–1) and was treated with calcium and vitamin D. With the help of fluorescence in situ hybridization (FISH), she was found to have a deletion of the chromosomal region 22q11.2 on one of her two copies of chromosome 22, consistent with a diagnosis of DiGeorge syndrome. Questions: • Would bone marrow transplantation work in patients with DiGeorge syndrome? • What could be the reason that patients with DiGeorge syndrome are at higher risk of autoimmune manifestations? thank you for your attention