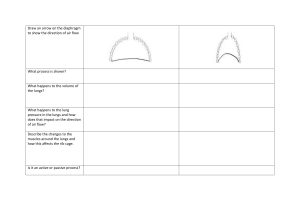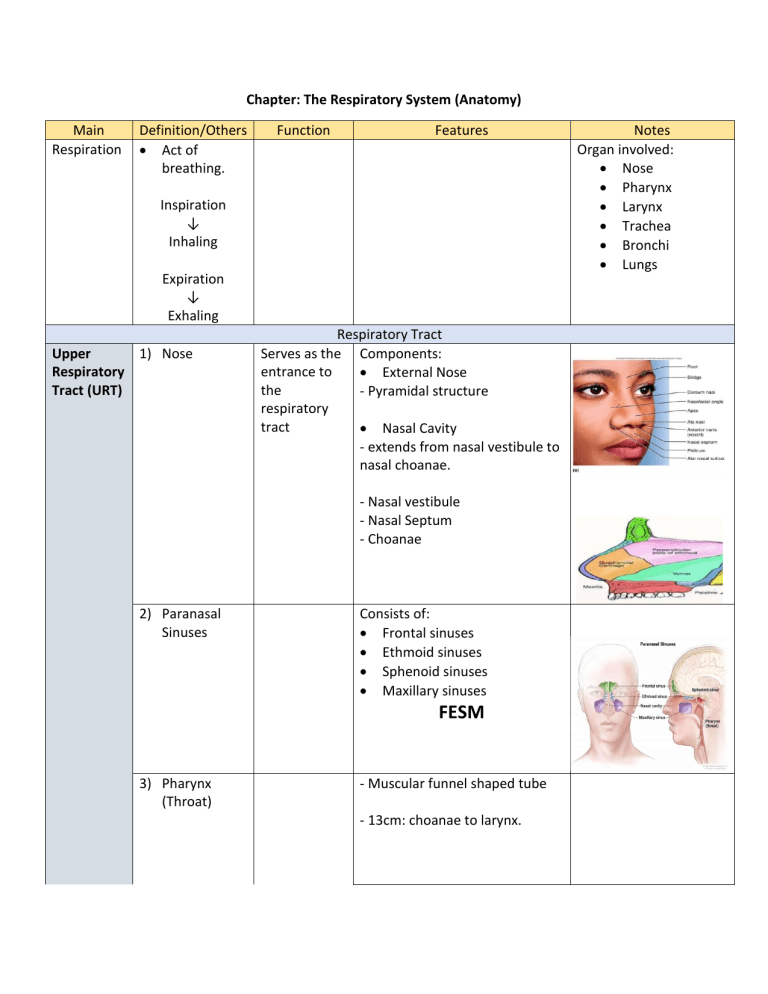
Chapter: The Respiratory System (Anatomy) Main Respiration Definition/Others • Act of breathing. Function Features Inspiration ↓ Inhaling Expiration ↓ Exhaling Upper 1) Nose Respiratory Tract (URT) Respiratory Tract Serves as the Components: entrance to • External Nose the - Pyramidal structure respiratory tract • Nasal Cavity - extends from nasal vestibule to nasal choanae. - Nasal vestibule - Nasal Septum - Choanae 2) Paranasal Sinuses Consists of: • Frontal sinuses • Ethmoid sinuses • Sphenoid sinuses • Maxillary sinuses FESM 3) Pharynx (Throat) - Muscular funnel shaped tube - 13cm: choanae to larynx. Notes Organ involved: • Nose • Pharynx • Larynx • Trachea • Bronchi • Lungs Regions: • Nasopharynx - Passes only air Lined by Epithelium: 1) Respiratory epithelium 2) Squamous epithelium • • Oropharynx Laryngopharynx - Pass air, food, & drink Lined by Epithelium: 1) Stratified squamous epithelium 4) Larynx (voice box) 1) Provides a patent airway. 2) Routes air & food into proper channels. 3) Voice production. Lower 1) Trachea Respiratory (windpipe) Tract (LRT) • Level = C4 to C6. Anterior to esophagus. • Composed 9 pieces cartilages: SINGLE: • Epiglottis • Thyroid • Cricoid PAIRS: • Arytenoid • Cuneiform • Corniculate • • • 2) Bronchial Tree • • • Level = C6 to T5 Anterior to esophagus. Superior border T5: Divided to L & R principal bronchi. Carina: ridge between openings of principal bronchi. Principal Bronchus Right Left Wider • Narrow Shorter • Longer (5cm) (2.5cm) • Oblique More vertical than L. 3) Lungs • • Shape: Pyraminal (conical) Weight: R: 625g L: 575g • Apex: • Blunt in shape (convex upward) • Grooved by subclavian artery. Base of lung • Semilunar & concave • Broad inferior • R: lobe of liver • L: lobe of liver, spleen, & fundus of stomach. • Descend: inhalation • Ascend: exhalation • Bronchopulmonary Segments • 10 per lungs. • R: 3 lobes • L: 2 lobes Lung Lobule • Contains: 1) Lymphatic vessels 2) Arteriole 3) Venule 4) Branch of terminal bronchiole. Terminal bronchiole ↓subdivides Respiratory bronchioles ↓subdivides Alveolar duct (2-11) **around circumference: numerous alveoli & alveolar sacs. *Alveoli: terminal pockets of the lungs where gas exchange occurs (within alveolar sacs) ** Alveolar ducts: connects alveoli to the bronchioles. Lungs - Alveoli Site of gas exchange. - Cup-shaped / grapelike outpouching. - Surrounded by network capillaries. Alveolar Epithelium: • Type I Pneumocytes • Type II Pneumocytes / Septal Cells • Alveolar Macrophages 4) Pleura Serous membrane or sac that investing lungs. • Parietal Pleura (outer) - line thoracic wall • Visceral Pleura (inner) - cover outer surface of lungs. - Separated by pleural cavity/space. • Pleural cavity: - contain pleural fluid. ** Pleural fluid permits two layers to move on each other with minimum friction. 5) Diaphragm • Primary muscle of respiration. • Dome-shaped septum dividing the thoracic from abdominal cavities Muscular fibers part: 1) a sternal part 2) a costal part 3) a lumbar part Inspiration : Descends Expiration : Ascends Mechanics of Ventilation Definition Process Thoracic volume/cavity Diaphragm Inspiration Breathing in of air. Active. Expanded/Bigger - Contract. - Dome moves downward into abdomen. Expiration Breathing out of air. Passive. Smaller - Relax. - Dome moves upward into abdomen. External intercostal muscles Ribcage Thoracic size Pressure Contract. Up and out. Increase Atmospheric pressure exceeds alveolar pressure. **Two main events cause expansion of thoracic volume: • • Relax. Down and in. Decrease Alveolar pressure exceeds atmospheric pressure. Contraction of diaphragm: activation of phrenic nerves. Contraction of the external intercostal muscles. Lung Volumes and Capacities. Lung Volumes 1. Tidal Volume (TV) 2. Inspiratory Reserve Volume (IRV) 3. Expiratory Reserve Volume (ERV) 4. Residual Volume • • • • • • • • • The amount of gas inspired or expired during a single breath under resting conditions. ~500ml Maximum amount of additional air that can be inspired from the end of a normal inspiration. ~3100ml. The maximum volume of additional air that can be expired from the end of a normal expiration. ~1200ml. The volume of air remaining in the lung after a maximal expiration. This is the only lung volume which cannot be measured with simple spirometer. ~1200ml. Lung Capacities 1. Total Lung Capacity (TLC) • • 2. Vital Capacity (VC) • • 3. Functional Residual Capacity (FRC) 4. Inspiratory Capacity (IC) TLC = TV + IRV + ERV + RV The volume of air contained in the lungs at the end of a maximal inspiration. VC = TV + IRV + ERV The maximum volume of air that can be forcefully expelled from the lungs following a maximal inspiration. ** VC% < 80% is abnormal. • FRC = ERV + RV • The volume of air remaining in the lung at the end of a normal expiration. • IC = TV + IRV • Maximum volume air that can be inspired from end expiratory position. This capacity is of less clinical significance than the other three. Dynamic Lung Volumes: Lung volumes that depend upon the air flow rates. 𝑭𝑬𝑽 1. Forced Vital • The volume that after full • 𝑭𝑽𝑪𝟏 is the ratio of FVE 1 to FVC Capacity (FVC) inspiration, then exhale with the most force and the most rate. • Hard & Long. • At least 6 seconds. 2. Time Forced • FVE 1 : Volume of air that can Expiratory be forcibly be blown out in Volume (FEV 𝑡 ) one second, after full inspiration. • FEV 1 , FEV 2, FEV 3 . 3. Peak Expiratory • Maximum flow rate in a single forced expiration. Flow Rate (PEFR) 4. Minute Ventilation (VE) 5. Alveolar Ventilation (VA) Lung Diseases, Ratio of FVE 𝟏 to FVC, & Spirometry Result. Condition 𝑭𝑽𝑬 𝟏 𝑭𝑽𝑪 Examples [%] Healthy Obstructive Diseases Normal respiration. Difficult to get air out of the lungs. > 80% < 80% ~ 45% Restrictive Diseases Difficult to get air in to the lungs. Normal @ Increased **but FVC & FVE 𝟏 lower than normal. • • • • • • • Emphysema Chronic bronchitis Asthma Interstitial fibrosis Sarcoidosis Muscular diseases Chest wall deformities