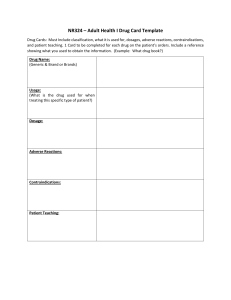
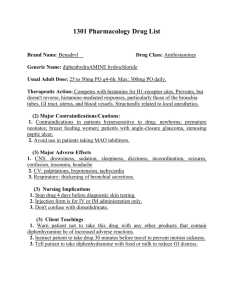
PATHO/PHARM 1 ● bethanechol (Urecholine) ● T: Nonobstructive urinary retention ● P: Muscarinic cholinergic receptor ● MOA: Direct-acting parasympathomimetic that interacts with muscarinic receptors to stimulate smooth muscle contractions in GI and urinary tracts. ● Adverse: Patients w/ disorders can aggravate their GI tract by increasing contractions ● Use: Treatment of nonobstructive urinary retention in ppl. w/ atony (decrease in muscle tone) of bladder ● Admin Alert: Normally oral, subcutaneous 3-4x/day @ 5mg ● Contraindications: Asthma, epilepsy, Parkinson’s, hypertrophy, bradycardia Bee makes you pee (urinate) ● physostigmine (Antilirium) ● T: Antidote for anticholinergic toxicity ● P: AchE inhibitor ● MOA: Indirect parasympathomimetic that inhibits the destruction of ACh by AChE. Effects occur at the neuromuscular junction ● Adverse: Bradycardia, asystole, restlessness, seizures, urinary frequency ● Use: reverses life threatening delirium caused by atropine ● Admin Alert: IM or IV; first-line for anticholinergic toxicity or Parkinson’s; administer slowly over 5 minutes. Monitor BP, HR, and respirations ● Contraindications: Asthma, epilepsy, diabetes, CV disease, or bradycardia ● Treatment of OD: atropine (AtroPen) psycho → mind → delirium from atropine OD ● atropine (AtroPen) ● T: Antidote for AChE poisoning ● P: Muscarinic cholinergic receptor (ACh) BLOCKER ● MOA: Blocks parasympathetic actions of ACh and induces symptoms of SNS. Has no effect on nicotinic receptors at therapeutic level. ● Adverse: Dry mouth, constipation, urinary retention, increased HR ● Use: Treat IBS, increased HR, and dilates pupils ● Admin Alert: Orally and subcutaneously ● Contraindications: Glaucoma, obstructed GI, BPH ● Treatment of OD: physostigmine (Antilirium) sounds like “airplane” → fight or flight ● phenylephrine (Neo-Synephrine) ● T: Nasal decongestant, mydriatic, antihypotensive ● P: Adrenergic drug ● MOA: Selective alpha-adrenergic agonist (alpha1) ● Adverse: Intranasal can cause burning of mucosa if used for long, ophthalmic can cause narrow glaucoma. High doses can lead to reflex bradycardia. Severe AE w/ IV infusion ● Use: Nasal Decongestant, Pupil Dilation, or Raise low BP ● Admin Alert: Parenteral can cause tissue injury with extravasation, phenylephrine ophthalmic drops may damage soft contact lenses ● Contraindications: Acute pancreatitis, heart disease, hepatitis ● Black Box: Severe reactions including death may occur via IV infusion. -phrine → nasal spray → decongestant ● prazosin (Minipress) ● T: Antihypertensive ● P: Adrenergic-Blocking Drug ● MOA: Selective Alpha1-Adrenergic Antagonist that competes with norepinephrine at its receptors on vascular smooth muscle in arterioles and veins ● Adverse: Orthostatic hypotension, unconsciousness, dizziness, drowsiness, lightheadedness ● Use: Decrease peripheral resistance to reduce blood pressure ● Admin Alert: low first dose to avoid orthostatic hypotension ● Contraindications: Safety during pregnancy and lactation is not yet established ● Treatment of OD: Fluid expanders or Vasopressors PrazOsin =lOw dose to lOwer BP ● atorvastatin (Lipitor) ● T: Antihyperlipidemic ● P: STATIN, HMG-CoA reductase inhibitor ● MOA: Inhibit HMG CoA reductase ● Adverse: GI complaints, hepatotoxicity, MOST SERIOUS: rhabdomyolysis ● Use: Treat Hyperlipidemia with a goal of reducing the risk of myocardial infarction (MI) and stroke. ● Admin Alert: Administer with food, May be taken at any time during the day ● Contraindications: Serious liver disease, unexplained persistent elevations of serum transaminase, and prior hypersensitivity to the drug “HMG! fat rhabbis don’t get pregnant” ● cholestyramine (Questran) ● T: Antihyperlipidemic ● P: Bile Acid Sequestrant ● MOA: Questran binds with Bile Acids (containing cholesterol) in an insoluble complex that is excreted in the feces ● Adverse: Constipation, bloating, gas, and nausea ● Use: To treat Hyperlipidemia ● Admin Alert: Mix POWDER thoroughly with 60 -180 mL of water, noncarbonated beverages, highly liquid soups, pulpy fruits (applesauce), Have the PT drink immediately to avoid irritation or obstruction in the GI tract. Also, give other drugs more than 2 hours before or 4 hours after the PT takes cholestyramine. ● Contraindications: Total biliary obstruction cholesterol is on a quest out of the body ● gemfibrozil (Lopid) ● T: Antihyperlipidemic ● P: Fibric Acid Drug (Fibrate) ● MOA: up to 50% reduction in VLDL with an increase in HDL. The MOA is unknown. Less effective than statins at lowering LDL. ● Adverse: Gallstones, Lopid can affect liver function, Most Common are GI Related: dyspepsia (indigestion), diarrhea, nausea, and abdominal pain. ● Use: Hypertrygliceridemia and Hypercholesterolemia ● Admin Alert: Administer with meals to decrease GI distress ● Contraindications: Hepatic impairment, severe chronic kidney disease (CKD), preexisting gallbladder disease in the name- fibr ● losartan (Cozaar) ● T: Drug for hypertension ● P: angiotensin II receptor blocker ● MOA: Blocks the release of Aldosterone by inhibiting angiotensin II ● Adverse: Hypoglycemia, dizziness, UTI, fatigue, and anemia ● Use: Treatment of HTN ● Admin Alert: May produce dizziness and fainting: PT should get up slowly from a sitting or lying position. DO NOT administer if PT is Pregnant ● Contraindications: Pregnancy or lactation, concurrent use with aliskiren ● Treatment of OD: Hypotension, Normal Saline blocks Aldosterone by Angiotensin II → cozAAr ● nifedipine (Adalat CC/ Procardia XL) ● T: Drug for HTN and angina ● P: Calcium channel blocker ● MOA: Selectively blocks calcium channels in myocardial and vascular smooth muscle, including those coronary arteries ● Adverse: r/t vasodilation such as: headache, dizziness, peripheral edema, heartburn, nausea, and flushing ● Use: Prescribed for HTN and variant or vasospastic angina ● Admin Alert: Discontinue gradually to prevent rebound hypotension ● Contraindications: Prior sensitivity to nifedipine or other CCB’s ● Treatment of OD: Vasopressors, Calcium infusions may be indicated CC → calcium channel blocker procaRdia → raynaud's syndrome ● doxazosin (Cardura) ● T: Drug for HTN and BPH (Benign Prostatic Hyperplasia) ● P: Alpha1-Adrenergic Blocker ● MOA: Selective Alpha1-Adrenergic blocker ● Adverse: dizziness, dyspnea, asthenia (lack of energy), headache, hypotension, orthostatic hypotension, and somnolence (sleepiness) ● Use: Dilate arteries and veins to lower blood pressure or to relieve dysuria in PT’s with BPH ● Admin Alert: Monitor PT closely for profound hypotension and possible syncope 2-6 hours following the first few doses due to the first-dose phenomenon (sudden and severe fall in blood pressure). ● Contraindications: Prior sensitivity to Alpha1-blockers ● Treatment of OD: Vasopressor or IV Fluids dox drops bp(h) ● Hydralazine ● T: Drug for HTN and HF ● P: Direct-acting vasodilator ● MOA: direct vasodilation of arterial smooth muscles; it has no effects on veins ● Adverse: Headache, reflex tachycardia, palpitations, flushing, nausea, and diarrhea. Sodium & Fluid Retention ● Use: lower BP, decrease risk for HF ● Admin Alert: abrupt withdrawal of the drug may cause rebound HTN and anxiety ● Contraindications: PT’s with angina, rheumatic mitral valve heart disease, or lupus ● Treatment of OD: Hypotension, Vasopressor or an IV infusion of fluids hydra- H diseases with excess fluid ● diphenhydramine (Benadryl) ● T: Drug to treat allergies ● P: H1-receptor antagonist; antihistamine ● MOA: H1-receptor (Histamine Receptor) antagonist ● Adverse: significant drowsiness, dry mouth, tachycardia, mild hypotension, may cause PHOTOSENSITIVITY ● Use: Treat minor symptoms of allergy and the common cold, such as sneezing, runny nose, and tearing of the eyes ● Admin Alert: Risk for anaphylactic shock when administered parenterally, IM inject deep into large muscle to decrease tissue irritation ● Contraindications: BPH, narrow angle glaucoma, and GI obstruction, asthma or hyperthyroidism diphenhydrAMINE is a antihistAMINE ● fluticasone (Flonase) ● T: Treats allergic rhinitis, asthma, and skin inflammation ● P: Corticosteroid ● MOA: decreases local inflammation in the nasal passages ● Adverse: Nose bleed (Epistaxis) ● Use: Reduce nasal stuffiness ● Admin Alert: Follow directions from manufacturer closely ● Contraindications: Because corticosteroids can mask signs of infection, PT’s with known bacterial , viral, fungal, or parasitic infections (especially of the respiratory tract) should not receive intranasal corticosteroids. floNASE → nasal spray ● oxymetazoline (Afrin) ● T: Nasal Decongestant ● P: Sympathomimetic ● MOA: Activates alpha-adrenergic receptor in the SNS, causes the arterioles in the nasal passages to constrict, thus drying the mucous membranes ● Adverse: Rebound congestion if used for longer than 3-5 days, minor stinging and drying in the nasal mucosa ● Use: Relief from nasal congestion within minutes and lasts for 10+ hours ● Admin Alert: wash hands to prevent aniscoria (blurred vision and inequality of pupils) ● Contraindications: Thyroid disorders, HTN, diabetes, or heart disease Afrin activates alpha adrenergic to cause arteriole constriction ● dextromethorphan (Delsym) ● T: cough suppressant ● P: centrally acting antitussive ● MOA: acts in the medulla to raise the cough threshold, non opioid ● Adverse: drowsiness, headache, upset GI (CNS depression, paradoxical excitation, respiratory depression, slurred speech, coma, seizures - in abuse situations or severe rxns) ● Use: mild cough ● Admin Alert: ● Contraindications: chronic cough (r/t asthma, smoking, emphysema), children under 6 y/o, grapefruit juice, alcohol, MAOIs ● Treatment of OD: orphans always be coughing ● albuterol (ProAir) ● T: Bronchodilator ● P: Beta2 - adrenergic agonist ● MOA: Short Acting Beta Agonist (SABA), Selectively stimulates beta2adrenergic receptors - This action activates the SNS, which relaxes smooth muscles thus resulting in bronchodilation. ● Adverse: Palpitations, headaches, throat irritation, temor, nervousness, restlessness, and tachycardia; less common: insomnia and dry mouth ● Use: relieve bronchospasm, facilitate mucus drainage, inhibit release of inflammatory mast cells ● Admin Alert: proper use of inhaler is essential for effective delivery of the drug, Nurse should observe and instruct PT in proper use ● Contraindications: Hx of cardiac disease, CAD, or HTN alBuTerol = beta two ● ipratropium (Atrovent) ● T: bronchodilator ● P: anticholinergic ● MOA: muscarinic cholinergic receptor blocker, blocks the parasympathetic nervous system leading to bronchodilation ● Adverse: cough, drying of nasal mucosa, hoarseness, bitter taste, intranasal admin causes epistaxis ● Use: inhalation and intranasal to relieve and prevent bronchospasm in COPD, *often combined w/ albuterol to tx emphysema & bronchitis* ● Admin Alert: nasal spray relieves runny nose, Metered Dose Inhaler (MDI) wait 3 min b/w doses, Avoid contact with eyes, Cat B ● Contraindications: soybean or peanut allergy b/c soya lecithin is used as a propellant in the inhaler; atropine has additive anticholinergic side effects ● Treatment of OD: Lina remembers by opium makes you vibe, ipratropium will mellow you out/breathe easy ● beclomethasone (Qvar) ● T: anti-inflammatory ● P: inhaled corticosteroid ● MOA: dampens the activation of inflammatory cells and inc the production of anti-inflammatory mediators, dec inflammation ● Adverse: hoarseness, dry mouth, changes in taste, cataracts in adults, growth inhibition in children, masks infections ● Use: first line drug for tx of persistent asthma ● Admin Alert: need 3-4 weeks of therapy, intranasal tx of allergic rhinitis, do NOT interchange PO & nasal, Cat C ● Contraindications: EXTREME caution in pediatric patients ● Treatment of OD: “cue”var- corticosteroid bec has asthma ● montelukast (Singulair) ● T: Anti Inflammatory drug for asthma prophylaxis ● P: leukotriene modifier ● MOA: Leukotrienes are immune system mediators that promote inflammation, edema, and bronchoconstriction when released in the airways. montelukast (Singulair) blocks leukotriene receptors to prevent airway edema and inflammation ● Adverse: Headache, nausea, diarrhea ● Use: Preventative drug for persistent, chronic asthma, exercise-induced bronchospasm, allergic rhinitis ● Admin Alert: Only drug in this class approved for pediatric use, not to be used to terminate an acute asthma attack, take drug 2 hours before exercise if used to prevent exercise-induced bronchospasms ● Contraindications: Pre-existing liver impairment should take with caution “luk” in both name and P class ● dextran 40 (Gentran 40) ● T: Plasma Volume Expander ● P: Colloid ● MOA: Raises osmotic pressure of the blood, causing fluid to move from the interstitial spaces to the blood. Expands the plasma volume which then increases BP, cardiac output, and improves venous return to the heart. ● Adverse: HTN-tachycardia, peripheral edema, distended neck veins, dyspnea, cough ● Use: Fluid replacement for hypovolemic shock, ● Admin Alert: Emergency administration IV 1.2–2.4 g/min, Non–emergent administration infusion rate <240 mg/min ● Contraindications: PT with acute kidney injuries, severe dehydration, severe heart failure, or hypervolemic disorders. ● Treatment of OD: If normal kidney function, discontinue infusions. If CKD, administer osmotic diuretic dexTRAN transports fluid out of cells ● sodium chloride (NaCl) ● T: Drug for Hyponatremia ● P: Electrolyte, Sodium Supplement ● MOA: NaCl keeps proper fluid balance and keeps our tissues hydrated ● Adverse: Hypernatremia (FRIED SALT, thirst, fatigue, muscle twitching, convulsions, altered mental status, and decreased level of consciousness) ● Use: To treat hyponatremia, corneal edema, OTC nasal spray is used to relieve inflamed nasal membranes ● Contraindications: PT’s with hypernatremia, heart failure, or impaired kidney function. ● Treatment of OD: Diuretics may be used to reduce pulmonary or peripheral edema ● potassium chloride (KCl) ● T: Drug for Hypokalemia ● P: Electrolyte, potassium supplement ● MOA: Supplemental KCL is administered to restore normal potassium levels ● Adverse: Hyperkalemia (Dysrhythmias, Heart block, muscle twitching, fatigue, paresthesia, dyspnea, cramping, & diarrhea; MURDER) ● Use: Preferred drug for Hypokalemia, Treats mild alkalosis. ● Admin Alerts: Administer upright to prevent esophagitis, don’t crush or chew tablets, dilute liquid forms before giving PO or through a nasogastric tube. ● Contraindications: hyperkalemia, CKD, chronic kidney disease, systemic acidosis, severe dehydration, extensive tissue breakdown (severe burns), adrenal insufficiency, administration of K-sparing diuretic ● Treatment of OD: K-sparing diuretic held, K-supplements/dietary restricted, treat w/ IV of 10% dextrose solution containing 10-20 units of insulin. potass-idic (treats alkalosis) ● sodium bicarbonate ● T: Drug for acidosis or Bicarbonate deficiency ● P: Electrolyte, sodium and bicarbonate supplement ● MOA: Bicarbonate Ion directly raises the pH of Body Fluids ● Adverse: Metabolic Alkalosis (confusion, irritability, slow RR, & vomiting) ● Use: Treat Acidosis ● Admin Alerts: 2-3 hours before or after meals/medications, do not add oral preparation to calcium containing solutions ● Contraindications: Metabolic Alkalosis, HTN, Peptic Ulcers, Diarrhea, or Vomiting ● Treatment of OD: Administration of Acidic Agents bi carb is basic ● furosemide (Lasix) ● T: Drug for HF and HTN ● P: Loop Diuretic ● MOA: Prevents absorption of Sodium and Chloride in the nephron loop ● Adverse: Hypokalemia, Hypotension and Dehydration, Hypovolemia may cause Orthostatic Hypotension ● Use: diminished cardiac output and renal flow, treats acute heart failure because of its ability to remove excess fluid from a PT in a short period ● Admin Alert: Check for low K levels, infants and neonates have a prolonged half-life of this drug (use with caution) ● Contraindications: Hypersensitivity to sulfonamides (anuria, hepatic coma, severe fluid or electrolyte) furosemide sounds like formaldehyde- both liquids → diuretic lasix for liquids in the loop ● hydrochlorothiazide (Microzide) ● T: Drug for HTN and edema ● P: Thiazide Diuretic ● MOA: Thiazide acts on the tubule to decrease the reabsorption of Na+ ● Adverse: Hypokalemia, Hyponatremia ● Use: most widely prescribed diuretic for HTN ● Admin Alert: early in the day to avoid nocturia, K+ supplements may be indicated ● Contraindications: Anuria, prior hypersensitivity to thiazides or sulfonamides thiazide in the name Thiazide acts on the Tubule ● spironolactone (Aldactone) ● T: Anti-hypertensive drug, drug for reducing edema ● P: Potassium-sparing diuretic, aldosterone antagonist ● MOA: inhibits aldosterone - increases Na+ and water excretion and potassium retention ● Adverse: Hyperkalemia, Male: gynecomastia, Female: irregular cycles ● Use: treats mild HTN ● Admin Alert: give with food, do not give with ACE inhibitor, do not give with K+ supplements ● Contraindications: anuria, hyperkalemia, serious CKD ● Black Box: tumors in animals has been found, should only be used in specific indications Spironolactone K+ sparing + inhibits aldosterone ● human regular insulin (Humulin R) ● T: parenteral drug for diabetes, pancreatic hormone ● P: short-acting hypoglycemic drug ● MOA: promotes utilization of glucose for energy needs and inhibits gluconeogenesis ● Adverse: Hypoglycemia, tachycardia, diaphoresis, drowsiness ● Use: used to help maintain blood glucose levels within normal limits ● Promote cellular uptake of glucose, amino acids, and potassium ● - promote protein synthesis ● - glycogen formation and storage ● - fatty acid storage as triglycerides ● - conserve energy stores by promoting the utilization of glucose for energy needs ● - inhibits gluconeogenesis ● Admin Alert: ensure PT has had sufficient food and is not hypoglycemic, ONLY IV drug, rotate injection sites, administer 30 minutes before meals ● Contraindications: CKD, hypoglycemia, hypokalemia should be monitored closely Regular goes Right into the vein ● metformin (Glucophage) ● T: Antidiabetic drug ● P: Biguanide ● MOA: reduces fasting and postprandial glucose levels by decreasing the hepatic production of glucose (gluconeogenesis) and reducing insulin resistance ● Adverse: GI related including nausea, vomiting, abdominal discomfort, metallic taste, diarrhea, and anorexia ● Use: Preferred oral drug to treat type 2 DM ● Admin Alert: Extended release tablet, must be swallowed whole so do not crush or chew; fasting blood glucose checked every 3 months, discontinue immediately upon signs of acidosis ● Contraindications: ● Black Box: May cause lactic acidosis, Characteristics of LA is fruity breath, confusion, jaundice, muscle cramps, weakness ● Treatment of OD: Hemodialysis, treatment for lactic acidosis. Filtering of acid out of blood through the form of dialysis. “I met a big diabetic that wants to lose weight” ● Heparin ● T: anticoagulant (Parenteral) ● P: Indirect thrombin inhibitor ● MOA: Prevents the enlargement of existing clots and the formation of new ones by binding to antithrombin II which inactivates several clotting factors and inhibits thrombin activity ● Adverse: abnormal bleeding, HIT (Heparin induced thrombocytopenia) PT might experience an increase in adverse thromboembolic events. ● Use: Prolong coagulation time , thereby preventing excessive clotting within blood vessels ● Admin Alert: Dose is based on weight, do not massage site after injection ● Contraindications: Active internal bleeding, bleeding disorders, severe HTN, recent trauma, intracranial hemorrhage, or bacterial endocarditis. ● Treatment of OD: Protamine sulfate (5 min onset) is administered in cases of serious hemorrhage to neutralize heparin’s anticoagulant activity. Heparin works Hella fast and is gone Hella fast ● warfarin (Coumadin) ● T: Anticoagulant (Oral) ● P: Vitamin K antagonist ● MOA: Slow onset due to warfarin binding to the plasma proteins and is thus unavailable to produce its effect. (Blocks Vitamin K from assisting with clotting, inhibits clotting factors II, VII, IX, X) ● Adverse: Abnormal bleeding ● Use: Prevent stroke, MI, DVT, and pulmonary embolism in PT’s undergoing hip or knee surgery pr in those with long-term indwelling central venous catheters or prosthetic heart valves. ● Admin Alert: If life threatening bleeding occurs, anticoagulant effects of warfarin can be reduces by IM Vitamin K administration ● Contraindications: PT’s with recent trauma, active internal bleeding, bleeding disorders, intracranial hemorrhage, severe HTN, bacterial endocarditis, or severe liver/kidney disease ● Black Box: Warfarin can cause major fatal bleeding and regular monitoring of INR, International Normalized Ratio, is required (Normal value is 2-3) ● Treatment of OD: Vitamin K Warfarin has a Weaker effect and takes a Week to work ● clopidogrel (Plavix) ● T: antiplatelet drug ● P: ADP Receptor Blocker ● MOA: Prolongs bleeding time by inhibiting platelet aggregation, directly inhibiting ADP binding to its receptor ● Adverse: Flu Like symptoms such as: headache, dizziness, bruising, and rash/pruritus, abnormal bleeding ● Use: Prevent thrombi formation in PT’s who recently experienced a thromboembolic event such as stroke or MI. ● Admin Alert: Discontinue drug 5 days prior to surgery ● Contraindications: Active bleeding ● Black Box: poor metabolizers will exhibit less therapeutic effect and more adverse cardiovascular effects ● Treatment of OD: Platelet transfusions Cleopatra is a clot blocker ● alteplase (Activase) ● T: drug for dissolving clots ● P: Thrombolytic ● MOA: Identical to human TPA (Tissue Plasminogen Activator), To convert Plasminogen to Plasmin which then dissolves fibrin clots ● Adverse: Abnormal Bleeding, spontaneous ecchymoses, hematomas, or epistaxis should be reported immediately to the HCP ● Use: Preferred drug of treatment of stroke due to thrombus and is used off-label to restore the patency of IV catheters. ● Admin Alert: must be given w/in 12 hours of onset of symptoms of MI and w/in 3 hours of a thrombotic stroke for maximum effectiveness. Avoid parenteral injections to prevent unnecessary bleeding. ● Contraindications: Active internal bleeding, history of stroke, or head injury within the past 3 months, recent trauma or surgery, severe uncontrolled HTN, intracranial neoplasm, or arteriovenous malformation (artery/vein entanglement) AlTePlase → TPA ● aminocaproic acid (Amicar) ● T: Clot stabilizer ● P: Hemostatic/antifibrinolytic ● MOA: Inactivates plasminogen, the precursor of the enzyme plasmin that digests the fibrin clot. ● Adverse: Cautiously used in PT with a Hx of Thromboembolic disease. ● Use: Situations in which there is excessive bleeding because clots are being dissolved prematurely by plasminogen. ● Admin Alert: Rapid IV infusion may cause hypotension or bradycardia, monitor for dysrhythmias ● Contraindications: Disseminated Intravascular Clotting (abnormal blood clots forming inside vessels) Makes the blood stay still ● epoetin alfa (Epogen, Procrit) ● T: Erythropoiesis-stimulating drug ● P: Erythropoietin ● MOA: functionally identical to human erythropoietin, stimulates erythropoiesis (RBC formation) ● Adverse: HTN, headache, fever, nausea, and edema, tumor growth in cancer patients ● Use: Stimulate RBC formation ● Admin Alert: Do not shake the vial (deactivates the drug), SQ is preferred over IV because lower doses are needed and absorption is slower. ● Contraindications: uncontrolled HTN, hypersensitivity to mammalian cell products, myeloid malignancies ● Black Box: risk of serious cardiovascular and thromboembolic events. TIAs (Transient ischemic attacks), MIs, and strokes have been seen in PT with CKD who are on dialysis; give with anticoagulants ● Treatment of OD: OD is too many erythrocytes, which can be corrected by phlebotomy in the name- poetin ● filgrastim (Granix, Neupogen) ● T: drug for increasing neutrophil production ● P: colony-stimulating factor ● MOA: increase neutrophil production in the bone marrow and to enhance the phagocytic and cytotoxic functions of existing neutrophils ● Adverse: fatigue, rash, epistaxis, decreased platelet counts, neutropenic fever, nausea, and vomiting ● Use: Shorten the length of time of neutropenia (low WBC, high risk for infection) ● Admin Alert: do not administer w/in 24 hours before or after chemotherapy with cytotoxic drugs because this will decrease filgrastim’s effectiveness ● Contraindications: Hypersensitivity to E. coli filgrastim stimulates neutrophils ● cyanocobalamin (Nascobal) ● T: Drug for anemia ● P: Vitamin Supplement ● MOA: Supplemental Vitamin B12, PO is only effective if PT has sufficient amounts of intrinsic factor (glycoprotein secreted by stomach to enable Vitamin B12 absorption) ● Adverse: Hypokalemia, arthralgia (joint pain), dizziness, or headache ● Use: Indicated in PT’s with Vitamin B12 deficiency anemia ● Admin Alert: administer quickly if PO preparations are mixed with fruit juices (ascorbic acid (Vitamin C)) ● Contraindications: sensitivity to cobalt, folic acid deficiency anemia, severe pulmonary disease, heart disease (monitor for Na retention) Nas(al)cob(12)al cyanocobalAMIN is a vitAMIN ● ferrous sulfate (Feosol) ● T: Antianemic drug ● P: Iron supplement ● MOA: Supplemental Iron Vitamin ● Adverse: GI Upset (take with food will diminish symptoms but all diminish Fe effects by 50-70%, ideally 1-2 hours after meal), dark stools, constipation (increase dietary fiber) ● Use: reverse symptoms of iron deficiency anemia ● Admin Alert: Monitor HbG and Hct levels because excess iron is toxic, IV prevent infiltration (leaking to surrounding tissues), Z-track method when administering deep IM injection, DO Not crush or empty capsule contents, do not give capsules within 1 hour of bedtime ● Contraindications: ● Black Box: non intentional OD of iron-containing products are the leading cause of fatal poisoning in children ● Treatment of OD: antidote for acute iron intoxication is deferoxamine (Desferal), this drug binds to iron and excretes it through the urine (reddish brown color) Fe → iron ● ibuprofen (Advil, Motrin) ● T: Analgesic, anti-inflammatory drug, antipyretic ● P: NSAID ● MOA: Inhibition of prostaglandin synthesis ● Adverse: nausea, heartburn, epigastric pain, dizziness ● Use: mild to moderate pain, fever reduction, musculoskeletal disorders such as rheumatoid arthritis and osteoarthritis ● Admin Alert: Give on an empty stomach as tolerated, possible hypersensitivity reactions if PT has asthma or allergies to aspirin ● Contraindications: Active peptic ulcers ● Black Box: increased risk of serious thrombotic events, MI’s, and stroke. increased risk of GI adverse effects including bleeding, ulceration, and perforation ● Treatment of OD: None specifically, administration of an alkaline drug will increase urinary excretion of ibuprofen. Side effects: NSAID NSwelling Allergy Impaired renal function Damage to stomach wall ● Prednisone ● T: Anti-inflammatory drug ● P: (synthetic) Corticosteroid ● MOA: its actions are the result of being metabolized to an active form, which is also available as a drug called prednisolone ● Adverse: Long term therapy may result in Cushing’s syndrome (hyperglycemia, fat redistribution to the shoulders and face, muscle weakness, bruising, and bones that easily fracture. ● Use: inflammation (limited to 4-10 days), Long-term therapy (alternative dosing is used to prevent Cushing’s syndrome) ● Admin Alert: IM (deep injections to prevent atrophy or abscesses), Do not use if signs of systemic infection are present, drug use must be slowly tapered if used for more than 10 days ● Contraindications: Active viral, bacterial, fungal or protozoan infections. the 5 S’s of steroids: Sick, Sad, Sex (lower libido), Salt (retains more= weight gain), Sugar (raises blood sugar) ● acetaminophen (Tylenol) ● T: Antipyretic analgesic ● P: Centrally acting COX inhibitor ● MOA: Reduces fever by direct action at the level of the hypothalamus and dilation of peripheral blood vessels, which enables sweating and dissipation of heat. ● Adverse: Risks of acute acetaminophen poisoning increases with duration of use, symptoms include: anorexia, nausea, vomiting, dizziness, lethargy, diaphoresis, chills, abdominal pain, and diarrhea. Excessive use is the #1 cause of acute liver failure in the United States. LIVER DAMAGE ● Use: No anti-inflammatory properties, used for treatment of fever in children and for relief of mild to moderate pain when aspirin is contraindicated. ● Admin Alert: never administer to PT who consume alcohol regularly (drug induced hepatotoxicity), advise that acetaminophen is contained in many OTC products and extreme care must be used to not duplicate doses. ● Contraindications: Alcoholism ● Treatment of OD: Acetadote is given IV to protect the liver from toxic metabolites. ACetaminophen is Centrally Acting (AC -CA) ● hepatitis B vaccine (Engerix-B) ● T: Vaccine ● P: Vaccine ● MOA: provides active immunity to Hepatitis B ● Adverse: pain at the injection site and mild to moderate fever or chills ● Use: Preventative measure to protect PT against HBV. ● Admin Alert: Adults - Deltoid muscle injection, Epinephrine should be available to treat a possible anaphylactic reaction. ● Contraindications: Hypersensitivity to yeast or HBV Vaccine, if PT displays hypersensitivity to the first dose (DO NOT administer following doses). Use with caution in PT’s with a fever, active infection or compromised cardiopulmonary status. Allergy to yeast Hep B is recomBinant vaccine ● interferon alfa-2b (Intron A) ● T: Immunostimulant ● P: interferon, biologic response modifier ● MOA: warn surrounding cells that an infection has occurred. ● Adverse: Flu Like symptoms: fever, chills, dizziness and fatigue. Headache, nausea, vomiting, diarrhea, and anorexia are common. LONG TERM therapy risk for immunosuppression, hepatotoxicity, and neurotoxicity. ● Use: Approved to treat cancers (hairy cell leukemia, malignant melanoma, nonHodgkin’s lymphoma, AIDS-related Kaposi’s sarcoma) as well as viral infections (HPV, chronic HBV and HCV) ● Admin Alert: Administer under careful guidance from HCP ● Contraindications: Autoimmune Hepatitis and hepatic decompensation. Neonates and infants shouldn’t receive this drug due to it containing benzyl alcohol interferes with the virus spreading ● cyclosporine (Gengraf, Neoral, Sandimmune) ● T: Immunosuppressant ● P: Calcineurin inhibitor ● MOA: inhibits helper T-cells (most important cell in adaptive immunity), suppresses immune system ● Adverse: Reduction of urine output, HTN and tremor, headache, gingival hyperplasia (overgrowth of gum tissues around teeth), and elevated hepatic enzymes ● Use: Prophylaxis of kidney, heart, and liver transplant rejection, psoriasis, and xerophthalmia (an eye condition of diminished tear production caused by ocular inflammation) ● Admin Alert: Neoral and Sandimmune are not bioequivalent and require HCP supervision upon administration. ● Black Box: May result in serious infection and possible skin malignancies cyclo (calcineurin)- sporin (suppresses) ● morphine (Astramorph) ● T: Opioid analgesic ● P: Opioid receptor antagonist ● MOA: Morphine Binds with both mu and kappa receptor sites to produce profound analgesia ● Adverse: dysphoria (restlessness, depression, and anxiety), hallucinations, nausea, constipation, dizziness, and an itching sensation. ● Use: Symptomatic relief of serious acute and chronic pain after nonnarcotic analgesics have failed ● Admin Alert: Morphine causes peripheral vasodilation which results in orthostatic hypotension, never open capsules or crush extended release tablets ● Contraindications: Severe or acute asthma, GI obstruction, and severe liver or kidney impairment ● Treatment of OD: IV administration of naloxone (Narcan) morphine to Mu & kappa ● naloxone (Narcan) ● T: Drug for treatment of acute opioid overdose and misuse ● P: opioid receptor antagonist ● MOA: blocks both the mu and kappa receptors ● Adverse: rapid loss of analgesia, increased blood pressure, tremors, hyperventilation, nausea and vomiting, and drowsiness ● Use: Used for complete or partial reversal of opioid effects in emergency situations ● Admin Alert: administer for a RR of <10 bpm, keep resuscitative equipment accessible ● Contraindications: Should not be used for Respiratory depression caused by non opioid medications ● Treatment of OD: O2, IV fluids, vasopressors, and other supportive measures nalox- blox opiods ● aspirin (acetylsalicylic acid) ● T: Non-opioid analgesic, NSAID, Antipyretic ● P: Salicylate; COX inhibitor ● MOA: inhibits Thromboxane-A2, inhibits COX-1 & COX-2 (inhibiting the synthesis of prostaglandins ● Adverse: May cause Salicylism: Tinnitus, dizziness, headache, excessive perspiration; Also GI discomfort and abnormal bleeding ● Use: Inhibits prostaglandins (influence inflammatory response), Mild to moderate relief of fever ● Admin Alert: Discontinue 1 week prior to surgery, aspirin is excreted in the urine and will alter urine lab values. ● Contraindications: Anticoagulant therapy such as heparin or warfarin ● Treatment of OD: Tx - activated charcoal, gastric lavage, laxative, or drug therapy for OD symptoms such as dizziness, drowsiness, abdominal pain, or seizures. A’s- Aspirin & Acetylsalicylic → analgesic, antipyretic, antiinflammatory ● sumatriptan (Imitrex) ● T: antimigraine drug ● P: triptan; 5-HT (serotonin) receptor drug; vasoconstrictor of intracranial arteries ● MOA: Triptans act by causing vasoconstriction of cranial arteries, doesn’t normally affect overall BP ● Adverse: dizziness, drowsiness, or a warming sensation ● Use: Acute migraine relief ● Admin Alert: Monitor changes in LOC and observe for seizures (r/t reduction in carotid arterial blood flow), HCP may want to administer first dose w/in the hospital setting (r/t risk for cardiac ischemia), HTN may result in dysry ● Contraindications: Recent MI, Hx w/ angina pectoris, HTN, or diabetes ● Treatment of OD: Drug therapy for weakness, lack of coordination, watery eyes and mouth, tremors, seizures, or breathing problems. in the name -triptan suma wrestlers are big- big headaches ● vitamin A (Aquasol A) ● T: Lipid-soluble vitamin ● P: Retinoid ● Adverse: Acute ingestion produces CNS toxicity, including headache, irritability, drowsiness, delirium, and possible coma. ● Use: night blindness and slow wound healing, general growth and development of bones, teeth, and epithelial membranes ● Admin Alert: Low dose - Preg A ● Contraindications: Above RDA dose - Preg X what A NIGHT - night vision increased vit A makes you HARD (Headache, Anorexia/ Alopecia, Really painful bones, Dry skin/ Drowsiness) ● folic acid (Folacin) ● T: Water-soluble vitamin ● Adverse: IV related: feeling flushed after injections, allergic hypersensitivity by the IV route ● Use: To reverse symptoms of deficiency (vitamin B12), fatigue, breathlessness, numbness, poor balance, and memory trouble. ● Contraindications: anemias that aren’t caused by folate deficiency folic acid for the fetus ● magnesium sulfate (MgSO4) ● T: Magnesium supplement ● P: Electrolyte ● Adverse: IV (requires careful observation to prevent toxicity), early signs of Mg OD ● Use: treat hypomagnesemia ● Admin Alert: IV: monitor decreased cardiac function, serum Mg levels, give required dose over 4 hours. ● Contraindications: Serious cardiac disease, PO administration: undiagnosed abdominal pain, intestinal obstruction, or fecal impaction. ● Treatment of OD: Signs: respiratory or cardiac suppression, Tx: calcium gluconate may be administered IV toxicity makes you BURP (BP decreases, Urine output decreases, Respirations decrease < 12, Patellar reflex absent) ● orlistat (Alli) ● T: Anti Obesity drug ● P: Lipase inhibitor ● MOA: modest increase in weight reduction ● Adverse: GI related: flatus (gas) with discharge, oily stool, fecal urgency, and abdominal pain. May decrease effectiveness of fat-soluble vitamins and warfarin. Rapid weight loss increases the risk for cholelithiasis. ● Use: Indicated in PT with a BMI above 30 or BMI above 27 w/ other risk factors such as HTN, hyperlipidemia, and diabetes ● Admin Alert: Administer w/ or 1 hour before a meal containing HIGH FATS ● Contraindications: Malabsorption syndromes, gallbladder disease, hypothyroidism, organic causes of obesity, anorexia nervosa, and bulimia nervosa ● Treatment of OD: Beta-Adrenergic Blockers may be administered to treat symptoms of HTN and tachycardia -statin = antilipidemic orliSTAT → antifat (obesity) ● penicillin G ● T: antibacterial ● P: cell wall inhibitor; natural penicillin ● MOA: to kill bacteria by disrupting their cell walls ● Adverse: Diarrhea, nausea, and vomiting. Anaphylaxis is the most serious side effect (can take several weeks to show signs of allergy) ● Use: Drug of choice against streptococci, pneumococci, and staphylococci. Also for gonorrhea and syphilis ● Admin Alert: Observe PT for 30 minutes following administration to monitor for allergic reactions, DO NOT mix with aminoglycosides (1-hour between medications) ● Contraindications: Use with caution in severe renal disease PENCILLINS PENETRATE gram POSITIVE bacteria cell walls Don’t mix the G’s → penicillin G and aminoGlycosides ● cefazolin (Ancef) ● T: antibacterial ● P: Cell wall inhibit; first generation cephalosporin ● MOA: inhibits cell wall biosynthesis by binding penicillin-binding proteins which stops peptidoglycan synthesis ● Adverse: Rash and Diarrhea ● Use: Treatment and Prophylaxis of Bacterial infections, gram-positive ● Admin Alert: IM injections deep into large muscle mass, not effective against MRSA ● Contraindications: Hypersensitivity to cephalosporins or penicillins, caution with CKD CEFazolin= CEPHalosporin, inhibit CEll wall synthesis ● tetracycline (Sumycin) ● T: antibacterial ● P: Protein synthesis inhibitor ● MOA: inhibits bacterial growth by inhibiting translation, inhibit protein synthesis ● Adverse: causes vaginal, oral and intestinal superinfections; GI irritation nausea, vomiting, epigastric burning, and diarrhea. Discoloration of teeth and PHOTOSENSITIVITY ● Use: Gram + and Gram - treatment, used for peptic ulcer disease, topical or PO for acne ● Admin Alert: Drink with full glass of water, antacids and tetracycline 1-3 hours apart ● Contraindications: second half of pregnancy, children 8 yrs and younger, severe renal or hepatic impairment cyclone in your stomach ● erythromycin (ERYC, Erythrocin) ● T: Antibacterial ● P: Macrolide; protein synthesis inhibitor ● MOA: Inhibit protein synthesis by binding to the bacterial ribosome; at low doses is bacteriostatic and at high doses bactericidal ● Adverse: Nausea, abdominal cramping, and vomiting (food reduces); high doses may be cardiotoxic w dysrhythmias; older adults/renal or hepatic impairment might experience hearing loss, vertigo, and dizziness (neurotoxic) ● Use: PT’s unable to tolerate penicillin, Bordetella pertussis (whooping cough), Legionella pneumophila (Legionnaire disease), Mycoplasma pneumonia, diptheria ● Admin Alert: Empty stomach w/ full glass of water, shake suspensions, DO NOT give with or immediately before/after fruit juices. ● Contraindications: Grapefruit Juice, hypersensitivity to macrolides, PT’s taking terfenadine, astemizole, or cisapride erythrocyte= macrocell / erythromycin = macrolide ● gentamicin (Garamycin) ● T: Antibacterial ● P: Aminoglycoside ● MOA: Inhibits bacterial protein synthesis ● Adverse: Rash, nausea, headache, and fatigue. ● Black Box: neurotoxicity: ototoxicity and produces loss of hearing or balance, tinnitus, vertigo, and headaches (higher in CKD) ● Neuromuscular blockade and respiratory paralysis ● Nephrotoxic: oliguria, proteinuria, elevated BUN and creatinine ● Use: Enterobacter, E. coli, Klebsiella, Citrobacter, Pseudomonas, Serratia and MRSA ● Admin Alert: Use only IM and IV solutions that are clear and colorless or slightly yellow (discard otherwise); withhold drug if peak serum level lies above normal range of 5-10 mcg/mL ● Contraindications: Hypersensitivity to drug; monitor pre-existing renal impairment and hearing loss ● Treatment of OD: None Gentamicin is an aminoGlycoside (don’t mix w penicillin G) ● ciprofloxacin (Cipro) ● T: Antibacterial ● P: Fluoroquinolone; bacterial DNA synthesis inhibitor ● MOA: By inhibiting DNA gyrase, it affects bacterial replication and DNA repair ● Adverse: Nausea, vomiting, and diarrhea (uncommon, give w food to diminish); phototoxicity, headache, and dizziness ● Do not give w antacids or mineral supplements ● Black Box: Tendinitis and tendon rupture (older than 60, organ transplant recipients, and concurrent corticosteroid); muscle weakness in myasthenia gravis ● Use: UTI, sinusitis, pneumonia, skin, bone, and joint infections, infectious diarrhea, and certain eye infections ● Admin Alert: At least four hours before antacids and ferrous sulfate ● Contraindications: Hypersensitivity; discontinue if experience pain or tendon inflammation ● Treatment of OD: ciproFLOXacin makes your muscles and tendons flop FLOX Flop to the FLUORoquinolone b/c you ruptured a tendon ● trimethoprim-sulfamethoxazole (Bactrim) ● T: Antibacterial ● P: Sulfonamide; folic acid inhibitor ● MOA: Suppress bacterial growth by inhibiting the synthesis of folic acid (essential for periods of rapid cell division and growth) ● Adverse: Nausea and vomiting; hypersensitivity such as skin rash, itching, and fever; caution w CKD bc of crystalluria, oliguria, and kidney failure. Photosensitivity (avoid sunlight during therapy) ● Use: UTIs, Pneumocystis carinii pneumonia, shigella infections of small bowel, and acute chronic bronchitis ● Admin Alert: Oral with full glass of water ● Contraindications: Those w anemia due to folate deficiency; decreases potassium excretion so caution w hyperkalemia; pregnant women shouldn’t use bc crossing placenta may cause kernicterus ● Treatment of OD: Acidification of urine; 5-15 mg of leucovorin daily Sulfonamides SUCK, i.e. vampires i.e. blood loss i.e. anemias as SAE ● isoniazid (INH) ● Therapeutic Class: Antituberculosis Drug ● Pharmacologic Class: Mycolic acid inhibitor ● Actions/Uses: Most Effective Single Drug for TB isoniAZID is a mycolic AZID inhibitor ● amphotericin B (Fungizone) ● MOA: Binds to ergosterol in fungal cell membranes ● Causes them to become permeable or leaky ● Use: wide spectrum activity, covers most pathogenic to humans ● Adverse Effects: Kidney Damage (Monitor fluid & electrolytes), Ototoxicity (Assess for hearing loss, vertigo, unsteady gait, tinnitus) ● Admin: Administer premedication such as acetaminophen, antihistamines, and corticosteroids to decrease hypersensitivity reactions; withhold the drug is the BUN exceeds 40 mg/dL or serum creatinine rises above 3 mg/dL FUNGizone is an antiFUNGal ● fluconazole (Diflucan) ● MOA: to act by interfering with synthesis of ergosterol ● Use: To treat fungal infections in CNS, bone, eyes, urinary tract, respiratory tract ● Not effective against non-albicans CANDIDA Species ● Adverse Effects: Nausea, Vomiting, Diarrhea reported at high doses ● hypoglycemia may result when administered w oral hypoglycemics including glyburide. Drug levels decreased when used w rifampin F U fungal ● nystatin (Nystop) ● MOA: binds to sterols in the fungal cell membrane, allowing leakage of intracellular contents ● Use: Candida infections of intestines, vagina, skin, mouth ● Adverse Effects: minor skin irritation, nausea, vomiting, diarrhea ● Admin: Do not swallow, swish for two minutes statin → antilipid → binds to sterols in fungal cell membrane ● Chloroquine (Aralen) ● T: Antimalarial Drug ● P: Heme complexing agent ● Use: Prophylaxis and Treatment of Malaria ● Inhibits formation of Hs from heme released by digestion of Hb-> leads to parasite death ● More information in Module 11 Lecture Notes “quine” sounds like heme → heme complexing agent ● metronidazole (Flagyl) ● T: Anti-infective, antiprotozoan ● P: Drug that disrupts nucleic acid synthesis ● ER tablet must be swallowed whole and taken on an empty stomach ● Use: Metronidazole is also a preferred drug for giardiasis and trichomoniasis ● Can cause dry mouth and metallic taste ● Interaction: DO NOT MIX W ALCOHOL metro runs on gas → gas/ pollution is a carcinogen also can’t take alcohol on the metro metronidazole= metallic taste ● mebendazole (Vermox) ● MOA: as broad spectrum antihelminthic drug ● Use: To treat wide range of helminth infections ● Adverse Effects: As worms die, abdominal pain, distention, and diarrhea may be experienced. ● Admin: Drug most effective when chewed and taken with a fatty meal drug for worms- worms are bendy- also verm = worm ● zidovudine (Retrovir) ● MOA: Virus mistakenly uses zidovudine as nucleoside and creates a defective DNA strand so that HIV cannot continue ● Limits the transmission of HIV from mother to fetus; reduces viral load ● Goal: reduce viral load of blood Vudine is for Viruses Retrovir is a retroviral ● efavirenz (Sustiva) ● MOA: to bind directly to reverse transcriptase, disrupting enzyme’s active site ● Use: in combination with other antivirals in treatment using HAART; approved for children 3 months and older ● Admin: High-fat meals increase absorption by as much as 50% and can cause toxicity fav sounds like rave → CNS is affected at raves (AE) ● dolutegravir (DTG) ● T: Antiretroviral ● P: Integrase strand transfer inhibitor ● Use: Blocks the strand transfer of retroviral DNA, interrupting replication Dolutegravir can cause neural Defects ● acyclovir (Zovirax) ● T: Antiviral for herpesviruses ● P: Nucleoside Analog ● Use: herpesvirus, most effective against HSV-1 & HSV-2, only effective at high doses against CMV and varicella zoster ● MOA: Prevents viral DNA synthesis, acyclovir decreases the duration and severity of acute herpes episodes. ● Hepato- and neurotoxic ● Lab tests: values for kidney function such as blood urea nitrogen (BUN) and serum creatinine may increase! ● Normal bun: 7 to 20 mg/dL ● Normal creatinine: 0.7 to 1.2 mg/dL Around the cyc(clock) lovir Mannitol - Fetty wap is not the Man At ALL and he had Glaucoma. - Treats glaucoma by decreasing intraocular pressure Rapid acting - LAG (bc no lagging in onset) Lispro Aspart Glulisine Exam 1 https://quizlet.com/598574973/drugs-exam-1-pathopharm-flash-cards/ Exam 2 https://quizlet.com/603101475/drug-cards-exam-2-flash-cards/ PATHO/PHARM 2 Ch: 19 - Drugs for Local and General Anesthesia ● Lidocaine (Xylocaine) ● T: Anesthetic (local/topical); antidysrhythmic (class IB) ● P: Sodium Channel Blocker; amide ● MOA: Acts by blocking neuronal pain impulses, blocks sodium channels located within the neuronal membranes ● Adverse: Side effects are uncommon with local anesthetics, early symptoms of toxicity is CNS excitement which leads to irritability and confusion; SERIOUS adverse effects include convulsions, respiratory depression, and cardiac arrest. ● Black Box: Use of 2% oral lidocaine, especially among infants, may lead to ingestion. Administering too much or accidental swallowing can lead to seizures, brain injury, cardiac abnormalities, and death. ● Use: Most frequently used injectable local anesthetic. Ex. spinal/epidural, postherpetic pain patch (Lidoderm), or dental procedures (DentiPatch). ● Admin Alert: Solutions containing preservatives or epinephrine are for local anesthesia only, DO NOT give to PT for dysrhythmias; Not for large areas or eyes; For Spinal/Epidural block use preparations labeled for IV use ● Contraindications: Sensitivity to amide-type local anesthetics, CI in PT w/ severe trauma or sepsis, blood dyscrasias, dysrhythmias, sinus bradycardia, and severe degrees of heart block. ● Propofol (Diprivan) ● T: General Anesthetic ● P: N-methyl-D-aspartate (NDMA) receptor agonist ● MOA: Almost immediate onset, NMDA receptor agonist ● Adverse: Pain @ injection site, apnea, respiratory depression, and hypotension; PIF (Propofol Infusion Syndrome) are metabolic abnormalities and organ system failures & is characterized by severe metabolic acidosis, hyperkalemia, lipidemia, rhabdomyolysis, hepatomegaly, and cardiac failure. ● Use: Most widely used IV anesthetic, induction and maintenance of general anesthesia, also has an antiemetic effect that can prevent nausea or vomiting. ● Admin Alert: Propofol may provide a faster onset and deeper sedation, only administered by those trained in anesthesia. ● Contraindications: Hypersensitive to the medication or its emulsion, which contains soybean and egg products. Use with caution in PT with cardiac or respiratory impairment. Not recommended for OB. ● Nitrous Oxide ● T: General Anesthesia ● P: Inhalation Gaseous drug ● MOA: Suppression of pain mechanism in the CNS, does not induce surgical anesthesia. Always combined with Oxygen (25-30%) and is administered through a semi closed tube or mask. ● Adverse: High doses - adverse signs of stage 2 anesthesia such as anxiety, excitement, and combativeness. Nausea and Vomiting are more common following the procedure than other inhaled anesthetics. May result in liver damage and has the potential to be abused (sometimes by medical personnel) ● Use: Short surgical or dental procedures because the PT stays conscious and can follow instructions while experiencing full analgesia. ● Admin Alert: Establish an IV before administering in case of emergent situations. ● Contraindications: Impaired LOC, head injury, inability to comply with instructions, decompression sickness, nitrogen narcosis, air embolism, undiagnosed abdominal pain or marked distention, bowel obstruction, hypotension, shock, COPD, cyanosis, chest trauma with pneumothorax, or someone being air transported. ● Isoflurane (Forane) ● T: Inhaled General Anesthetic ● P: GABA and glutamate receptor agonist ● MOA: Rapid onset of surgical anesthesia with smooth induction and a low degree of metabolism by the body. Cardiac output is well maintained compared to other inhaled general anesthetics. ● Adverse: Mild nausea, vomiting, and tremor. ● Use: Potent level of surgical anesthesia. Provides excellent muscle relaxation and may be used off-label as adjuvant therapy in the treatment of status asthmaticus. ● Admin Alert: Premedication should be selected according to the needs of the patient ● Contraindications: Known history of genetic predisposition to malignant hyperthermia should not use isoflurane. CI in PT’s with head trauma or brain neoplasms due to possible increase in intracranial pressure. Older PT’s are more susceptible to hypotension. ● Succinylcholine (Anectine, Quelicin) ● T: Skeletal muscle paralytic drug; neuromuscular blocker ● P: Depolarizing blocker; acetylcholine receptor blocking drug ● MOA: Acts on cholinergic receptor sites at neuromuscular junctions. At first, depolarization occurs, and skeletal muscles contract. The membrane is unable to repolarize as long as the drug stays attached to the receptor. ● Adverse: Can cause complete paralysis of the diaphragm and intercostal muscles; thus, mechanical ventilation is necessary during surgery. Bradycardia and respiratory depression are expected. If doses are high, the ganglia are affected, causing tachycardia, hypotension, and urinary retention. ● Black Box: Administered with trained personnel to monitor, assist, and control respiration. Cardiac arrest has been reported resulting from hyperkalemic rhabdomyolysis most frequently in infants or children with undiagnosed skeletal muscle myopathy or Duchenne’s muscular dystrophy. This drug is reserved for children in emergent situations. ● Use: IV skeletal muscle relaxant ● Contraindications: Used with extreme caution in patients with severe burns or trauma, neuromuscular diseases, or glaucoma. CI in PT’s with a family history of malignant hyperthermia or conditions of pulmonary, kidney, cardiovascular, metabolic, or liver dysfunction. ● ● ● ● ● ● ● ● T: P: MOA: Adverse: Use: Admin Alert: Contraindications: ● ● ● ● ● ● ● T: P: MOA: Adverse: Use: Admin Alert: Contraindications: ● ● ● ● ● ● ● T: P: MOA: Adverse: Use: Admin Alert: Contraindications: ● ● ● ● ● ● ● T: P: MOA: Adverse: Use: Admin Alert: Contraindications: ● ● ● ● ● ● ● T: P: MOA: Adverse: Use: Admin Alert: Contraindications: ● ● ● ●