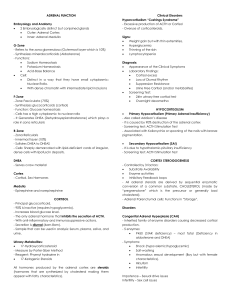
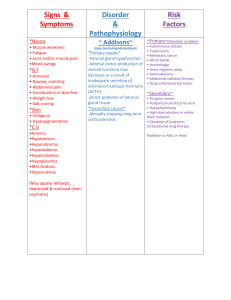
ADRENAL INSUFFICIENCY Dr Helena Vreede Chemical Pathology 2023 Learning Objectives • Understand the hypothalamic-pituitary-adrenal axis • Understand adrenal steroidogenesis, and the biochemistry and investigation of congenital adrenal hyperplasia (CAH) • Understand the biochemistry and investigation of adrenal insufficiency HYPOTHALAMIC-PITUITARY-ADRENAL AXIS Hypothalamus and Pituitary DA SS Hypothalamic and pituitary hormones Hypothalamic regulatory hormone Pituitary hormone Anterior Pituitary: GnRH Gonadotropin-releasing hormone FSH LH Follicle stimulating hormone Luteinizing hormone CRH Corticotropin releasing hormone ACTH Adrenocorticotropic hormone TRH Thyrotropin-releasing hormone TSH Thyroid stimulating hormone DA Dopamine (-) PRL Prolactin GHRH SS Growth hormone releasing hormone Somatostatin (-) GH Growth hormone Posterior Pituitary: ADH Antidiuretic hormone OT Oxytocin Regulation of pituitary function a) b) c) d) Stress can alter pituitary hormone secretion and be used to test for abnormality, e.g., insulin induces hypoglycaemia, and hypoglycaemic stress stimulates hypothalamic hormones such as CRH and GHRH, which in turn stimulate the production of pituitary hormones ACTH and GH Feed-back by products of end-organ endocrine glands (eg. steroids) or tissues (eg. IGF-l) act back, usually inhibiting, or in rare cases, enhancing, pituitary response to hypothalamic factors. Feed-back is thus negative or positive, and either long-loop (to hypothalamus) or short-loop (to pituitary). Cyclic fluctuations in pituitary hormone secretion (e.g. GH and ACTH) is mediated via CNS regulation of hypothalamic releasing factors; and may be altered in disease. Development. The endocrine system remains in equilibrium (constancy) via negative feed-back mechanisms. However, the degree of negative feedback is not constant. For example, sensitivity to negative feed-back by gonadal steroid on gonadotropin secretion diminishes during puberty, Thus the major changes of puberty only occur because these controlling mechanisms are no longer restraining. NB. Testing of pituitary dysfunction employs all of the above concepts. Hypothalamic – Pituitary – Adrenal axis Corticotropin releasing hormone (CRH) is a 41-amino acid peptide which stimulates adrenocorticotropic hormone (ACTH) secretion. Adrenocorticotropic hormone (ACTH) is a 39amino acid polypeptide that stimulates adrenal glucocorticoid (but not minerallocorticoid) secretion. ACTH secretion exhibits diurnal variation, highest at 08h00, lowest at midnight. Secretion is greatly increased by stress, and inhibited by cortisol in a classic negative feedback manner. Excessive secretion of ACTH occurs with some pituitary tumours (Cushing’s disease) and in primary adrenal failure (Addison's disease). It is also occasionally produced ectopically by nonpituitary tumours (eg. small cell lung CA). Decreased ACTH leading to secondary adrenal failure is usually part of generalised pituitary insufficiency, though it can occur in isolation. ADRENAL STEROIDOGENESIS Anatomy of the adrenal gland Hormones of the adrenal: overview Control: Adrenal gland: Renin-angiotensin-aldosterone system: Adrenal cortex: Zona glomerulosa Hormones: Aldosterone Hypothalamic-pituitary-adrenal axis: CRH → ACTH → Cortisol Adrenal cortex: Zona fasciculate Zona reticularis Cortisol Androgens Sympathetic nervous system Adrenal medulla Catecholamines Enzymes of adrenal steroidogenesis Short name Full name Adrenal cortex site P450scc Cholesterol side-chain cleavage enzyme and desmolase All zones 3βHSD 3-beta-hydroxysteroid dehydrogenase All zones 17OH 17-alpha-hydroxylase ZF + ZR 17,20-lyase 17,20-lyase ZR 21OH 21-hydroxylase ZF + ZG 11OH 11-beta-hydroxylase ZF + ZG 18OH + 18DH 18-hydroxlase + 18-dehydrogenase = = AS Aldosterone synthase ZG Summary pathway of steroid hormone production: Cholesterol Pregnenolone 17OH 1 17-OH-Pregnenolone 3βHSD 1 Progesterone 17OH Deoxycorticosterone 11OH 3 Corticosterone 2 17-OH-Progesterone DHEA 3βHSD 3βHSD 21OH 2 1 2 Androstenedione 21OH 3 11-Deoxycortisol 11OH 4 Cortisol 18OH 4 18-OH-Corticosterone 18DH 5 Aldosterone Mineralocorticoid pathway Glucocorticoid pathway Androgen pathway Adrenal corticosteroids: types → effect Androgen precursors Mineralocorticoids Glucocorticoids CMO I = 18-Hydroxylase CMO II = 18-Dehydrogenase CMO I plus CMO II = Aldosterone Synthase ADRENAL HORMONES Adrenal hormone (1): Cortisol Cortisol is a 'glucocorticoid' (a cortical hormone that increases blood glucose levels): - In liver: increases gluconeogenesis and glycogen synthesis. - In muscle: decreases glucose uptake and consumption; increases glycogenolysis and protein catabolism; decreases protein synthesis. - In adipose tissue: increases lipolysis. Other: - Acts on the pancreas to decrease insulin and increase glucagon. (Cortisol and glucagon both “counter-regulatory hormones”) - Decreases peripheral tissue sensitivity to insulin - Increases appetite and food intake and may increase fat mass Other effects: • Cardiovascular: Sensitizes arterioles to effect of noradrenaline → maintains BP • Bone and calcium metabolism: Inhibits bone formation and increase bone resorption • Immunological: Inhibits prostaglandin, various interleukins, TNF. Is anti-inflammatory and immunosuppressive. • Effects on CNS: improves memory Adrenal hormone (2): Aldosterone CONGENITAL ADRENAL HYPERPLASIA Disorders of the Adrenal Gland • Hypoadrenalism: • Congenital adrenal hyperplasia • Primary adrenal insufficiency (Addison’s disease) • Hyperadrenalism: • Primary hyperaldosteronism (Conn’s) - semester 5 • Primary hypercortisolism (Cushing’s) - semester 5 • Disorders of the adrenal medulla: • Phaeochromocytoma - semester 5 Congenital Adrenal Hyperplasia 3βHSD deficiency: 21-OH deficiency: Rare >90% 11-OH deficiency: 17-OH deficiency: 5-10% <5% CAH: 21-Hydroxylase deficiency Commonest. >90% CAH. AR. Pathophysiology: Decreased GC: ↓ negative feedback ↑ ACTH → adrenal hyperplasia Decreased MC: Salt wasting Increased Androgens: Over-virilisation of newborn females (ambiguous genitalia) Diagnostic precursor: ↑ 17OH-Progesterone Female with 21-OH deficiency CAH: 21-Hydroxylase deficiency • Severe salt-losing form: • severe enzyme defect • potential adrenal crisis due to inadequate aldosterone • hypotension, shock, hyperkalaemia • boys at risk clinically • Simple virilising form: • mild enzyme defect • adequate cortisol and aldosterone production • accumulation of 17-OHP and excessive androgens • over-virilisation of newborn females (ambiguous genitalia) • virilised male (often un-noticed) • Non-classical form: • very mild enzyme defect (1:1000) • no neonatal masculinisation • young women present with menstrual irregularity, infertility, hirsutism • mimics PCOS • Treatment: • Cortisol and fludrocortisone • Monitor by measuring 17-OHP (keep slightly elevated but avoid over-treatment due to risk of iatrogenic Cushing’s) and androgens (testosterone, DHEAS) CAH: 3β hydroxysteroid dehydrogenase defn Rare. AR. Pathophysiology: Decreased GC: ↓ negative feedback ↑ ACTH → adrenal hyperplasia Decreased MC: Salt wasting Decreased Andostenedione → ↓Testosterone → Under-virilisation of newborn males Increased DHEA → Over-virilisation of newborn females Note: The only form of CAH that can present with ambiguous genitalia of both sexes Diagnosis: ↑ Pregnenolone, 17α-hydroxypregnenolone, DHEA, and renin CAH: 11-Hydroxylase deficiency AR. 5-10% CAH Pathophysiology: Decreased GC: ↓ negative feedback ↑ ACTH → adrenal hyperplasia Decreased Aldosterone, but increased Deoxycorticosterone = MC: Hypertension, HypoK Increased Androgens: Over-virilisation of newborn females (ambiguous genitalia) Diagnostic precursor: ↑ 11-Deoxycortisol (and ↑ 17OH-Progesterone) CAH: 17-Hydroxylase deficiency AR. <5% CAH Pathophysiology: Decreased GC: ↓ negative feedback ↑ ACTH → adrenal hyperplasia Decreased cortisol, but increased Corticosterone = weak GC: prevents adrenal crisis Increased MC precursors: Low renin hypertension in childhood with hypoK met alkalosis Decreased Androgens: Under-virilization of newborn males (ambiguous genitalia); Females delayed puberty CAH: Summary of features (1) 3βHSD deficiency: 21-OH deficiency: Rare >90% 11-OH deficiency: 17-OH deficiency: 5-10% <5% CAH: Summary of features (2) CAH MC defn Salt-wasting Hypertension Over-virilized Females Under-virilized Males 3β-HSD: sw Yes Yes - Yes + Yes + No - Yes + Yes + Yes - Yes +++ - No - Yes +++ - 3β-HSD: nsw 21-OH: sw Yes 21-OH: nsw 11-OH No - Yes +++ Yes +++ - 17-OH No - Yes +++ - Yes + ADRENAL INSUFFICIENCY Disorders of the Adrenal Gland • Hypoadrenalism: • Congenital adrenal hyperplasia • Primary adrenal insufficiency (Addison’s disease) • Hyperadrenalism: • Primary hyperaldosteronism (Conn’s) - semester 5 • Primary hypercortisolism (Cushing’s) - semester 5 • Disorders of the adrenal medulla: • Phaeochromocytoma - semester 5 Adrenal insufficiency • Primary adrenal hypofunction (Addison’s disease) (1:50 000) • Impaired capacity to secrete cortisol and aldosterone • Main causes: • Autoimmune (associated with Hashimoto’s thyroiditis, type I DM, • • • • • • other autoimmune diseases) Adrenal haemorrhage Meningococcal septicaemia (Friderichsen-Waterhouse syndrome) Infection: TB, fungal infection Neoplastic infiltration Haemochromatosis, amyloidosis Adrenoleukodystrophy • Secondary adrenal hypofunction • Iatrogenic due to rapid withdrawal of prolonged steroid therapy • Hypothalamic and pituitary disease • Lack of ACTH (no hyperpigmentation) • Cortisol deficiency • Intact aldosterone Addison’s disease • Clinical features: • orthostatic hypotension • dehydration • hypoglycaemia • pigmentation (excess ACTH) • fatigue • muscle weakness • weight loss • anorexia POMC: pro-opiomelanocortin; ACTH: adrenocorticotropic hormone; MSH: melanocyte-stimulating hormone; LPH: Lipotrophin; β-END: β-Endorphin • Addisonian crisis: hypotension, circulatory shock, abdominal pain (MEDICAL EMERGENCY) • Biochemical features: • Aldosterone deficiency • Na and water loss in urine • hyponatraemia • hyperkalaemia, metabolic acidosis • Cortisol deficiency • hypoglycaemia Investigation of adrenal insufficiency (1) Electrolytes (Na, K), blood gas Cortisol, ACTH, Aldosterone • Primary adrenal insufficiency: ↓ aldo ↓ cortisol ↑ ACTH • Secondary adrenal insufficiency:↓ ACTH ↓ cortisol Stimulation tests: evaluating the ability of the adrenal to respond to stimulation by ACTH. • Primary adrenal insufficiency: unable to respond • Secondary adrenal insufficiency: may be unable to respond immediately (adrenal was chronically understimulated), but may be able to respond after longer stimulation Investigation of adrenal insufficiency (2) 1. “Short” ACTH stimulation (synacthen / cosyntropin) test: • One dose of synacthen (low dose 1 ug or high dose 250 ug) • Measure cortisol before and 30 mins after Interpretation: • Normal: cortisol that increases to > 550 mmol/L • Subnormal response may be due to primary or secondary adrenal insufficiency 2. “Long” ACTH stimulation (synacthen / cosyntropin) test: • Synacthen stat plus depot injection x 3 days • Measure cortisol before, and at 1, 2, 4, 8 and 24 hrs after last dose Interpretation: • Normal: Rising cortisol with a peak at 4-8 hours • Primary adrenal insufficiency: no or poorly sustained response • Secondary adrenal insufficiency: slowly developing response with a peak at 24 hours Investigation of adrenal insufficiency (3) 3. Insulin tolerance test: • Insulin to induce hypoglycaemia with glu < 2.2 mmol/L ** Monitor • Hypoglycaemic stress stimulates ACTH Interpretation same as Synacthen test: • Normal: cortisol that increases to > 550 mmol/L • Subnormal response may be due to primary or secondary adrenal insufficiency 4. Metyrapone stimulation test: • Metyrapone inhibits the adrenal enzyme 11-β-hydroxylase which converts 11-deoxycortisol to cortisol. The reduced cortisol reduces negative feedback on the HPA, increases ACTH, and increases 11DOC ** Risk: reduced cortisol may precipitate Addisonian crisis Interpretation: • Normal HPA: ACTH and 11DOC increase • Subnormal response of 11DOC may be due to primary or secondary adrenal insufficiency Investigation of adrenal insufficiency (4) • Autoantibodies • Anti-adrenal (21-hydroxylase, 17-hydroxylase, cholesterol side- chain cleavage enzyme) • Anti-thyroid • Anti-Islet cell (type 1 DM) • Imaging • CT adrenal • CT or MRI of pituitary • CXR END For fun: From cholesterol to cortisol From cholesterol to cortisol: 1. Side chain cleavage and 20,22 Lyase -> Pregnenolone 2. 3β-hydroxysteroid dehydrogenase -> Progesterone 3. 17α-hydroxylase -> 17OH Progesterone 4. 21-hydroxylase -> 11deoxycortisol 5. 11-hydroxylase -> Cortisol