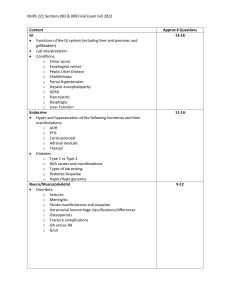
Contents
I. Pulmonology............................................................................................................... 6
1) Acute bronchitis, tracheobronchitis, bronchiolitis .......................................................................... 6
2) Chronic bronchitis, pulmonary emphysema, COPD ...................................................................... 7
3) Respiratory failure – pathophysiology and clinical features ........................................................ 11
4) Bacterial Community-acquired pneumonia (CAP)....................................................................... 13
5) Non-Bacterial Community-acquired pneumonia (CAP) ............................................................... 13
6) Hospital-acquired pneumonia (HAP) ........................................................................................... 13
7) Treatment of pneumonia ............................................................................................................. 16
8) Purulent diseases – bronchiectasis, pulmonary abscess ............................................................ 19
9) Pleural effusions .......................................................................................................................... 22
10) Pulmonary tuberculosis ............................................................................................................. 23
11) Pulmonary embolism (PE)......................................................................................................... 28
12) Diffuse parenchymal pulmonary diseases (DPLD) (AKA interstitial lung disease – ILD) .......... 30
II. Cardiology ............................................................................................................... 32
13) Diseases of mitral valve: Mitral stenosis ................................................................................... 32
14) Diseases of mitral valve: Mitral regurgitation (AKA mitral insufficiency).................................... 33
15) Diseases of aortic valve: Aortic stenosis ................................................................................... 36
16) Diseases of aortic valve: Aortic regurgitation (AR) .................................................................... 37
17) Endocarditis .............................................................................................................................. 38
18) Pericardial diseases- classification. Pericarditis. Cardiac tamponade. ..................................... 41
19) Myocardial diseases: Myocarditis.............................................................................................. 45
20) Myocardial diseases: Cardiomyopathies ................................................................................... 47
21) Acute heart failure (HF) ............................................................................................................. 50
22) Treatment of acute HF .............................................................................................................. 52
23) Chronic congestive heart failure ................................................................................................ 54
24) Parameters of cardiac function in CHF. Treatment of Chronic heart failure.............................. 57
25) Ischemic heart diseases: classification. Stable angina pectoris – clinical features, treatment .. 61
26) Acute coronary artery syndromes: acute myocardial infarction w/ST segment elevation ......... 64
27) Acute coronary artery syndromes w/out ST segment elevation: unstable angina pectoris,
myocardial infarction w/out ST segment elevation .......................................................................... 66
28) Conductive disturbances. Treatment of conductive disturbances. ............................................ 68
29) Rhythm abnormalities: Supraventricular arrhythmias – classification, hemodynamics, clinical
features ........................................................................................................................................... 73
30) Treatment of supraventricular arrythmias.................................................................................. 79
31) Rhythm abnormalities: Ventricular arrhythmias......................................................................... 82
32) Treatment of ventricular arrythmias........................................................................................... 85
33) Anti-arrhythmic drugs: classification, dosage ............................................................................ 87
34) Hypertension (HT) ..................................................................................................................... 89
35) Arterial hypertension – treatment .............................................................................................. 91
36) Acute rheumatic fever. Rheumocarditis .................................................................................... 93
37) Chronic cor pulmonale (AKA pulmonary heart disease) ........................................................... 95
38) Aortic diseases: aortic dissection, aortic aneurysm, Takayasu disease.................................... 96
III. Rheumatic diseases ............................................................................................. 101
39) Rheumatoid arthritis (RA) ........................................................................................................ 101
40) Ankylosing spondylitis (spondyloarthritis, Bechterev’s disease) ............................................. 103
41) Reactive arthritis (formerly known as Reiter syndrome), Rheumatic fever, Reiter’s syndrome,
Lyme disease ................................................................................................................................ 105
42) Rheumatic fever ...................................................................................................................... 106
43) Psoriatic arthritis ...................................................................................................................... 108
44) Systemic lupus erythematosus (SLE) AKA lupus.................................................................... 109
45) Systemic sclerosis (SSc) (AKA systemic scleroderma) .......................................................... 111
46) Polymyositis, dermatomyositis ................................................................................................ 113
47) Vasculitis/vasculitides – clinical features and classification .................................................... 115
48) Henoch-Schönlein purpura (AKA IgA vasculitis) ..................................................................... 117
49) PAN/Polyarteritis nodosa ........................................................................................................ 118
50) ANCA associated vasculitis..................................................................................................... 119
51) Large vessel vasculitis – Horton disease, Takayasu’s arteritis, Buerger disease ................... 120
52) Anti-phospholipid syndrome (APS) ......................................................................................... 123
53) Polymyalgia rheumatica and fibromyalgia ............................................................................... 124
54) Gout (podagra) ........................................................................................................................ 126
55) Osteoporosis ........................................................................................................................... 127
56) Osteoarthritis (OA) .................................................................................................................. 129
57) Treatment of rheumatic diseases w/biological and biosimilar drugs ....................................... 131
58) Humoral immunity changes in rheumatic diseases ................................................................. 133
IV. Hematologic diseases .......................................................................................... 135
59) Iron deficiency anaemia (IDA) ................................................................................................. 135
60) Macrocytic and megaloblastic anaemias................................................................................. 137
61) Hemolytic anaemias. Hemolysis ............................................................................................. 139
62) Aplastic anaemia. Agranulocytosis.......................................................................................... 142
63) Hodgkin’s lymphoma (HL) ....................................................................................................... 144
64) Non-Hodgkin’s lymphomas (NHL) ........................................................................................... 146
65) Chronic lymphocytic leukaemia (CLL) ..................................................................................... 149
66) Myeloma multiplex/multiple myeloma (MM) (AKA plasmacytoma, plasma cell myeloma,
myelomatosis, Kahler’s disease) ................................................................................................... 150
67) Chronic myelogenous/myeloid leukaemia (CML) .................................................................... 152
68) Polycythaemia vera (PV/PCV) (AKA primary polycythaemia) ................................................. 153
69) Acute myeloid leukaemia (AML).............................................................................................. 154
70) Acute lymphocytic leukaemia in adults (ALL) .......................................................................... 156
71) Haemorrhagic diathesis – features and classification. Thrombocytopenia – classification.
Autoimmune thrombocytopenia ..................................................................................................... 158
72) Haemorrhagic diathesis – classification. Haemophilia ............................................................ 161
V. Endocrine and metabolic diseases ....................................................................... 163
73) Diabetes mellitus – pathogenesis, clinical features ................................................................. 163
74) Diabetes mellitus – treatment w/insulin and oral medications ................................................. 164
75) Treatment of diabetic complications ........................................................................................ 167
76) Obesity and metabolic syndrome ............................................................................................ 169
77) Dyslipidemia ............................................................................................................................ 171
78) Hypothyroidism ....................................................................................................................... 172
79) Thyrotoxicosis. Hyperthyroidism ............................................................................................. 174
80) Nodular goiter. Endemic and sporadic goiter .......................................................................... 177
81) Hyperprolactinemia. Prolactinoma .......................................................................................... 180
82) Hypercalcaemic states ............................................................................................................ 182
83) 9 – Hypocalcaemic states ....................................................................................................... 183
84) 10 – Acromegaly and diabetes insipidus ................................................................................. 185
85) 11 – Hypercorticism (AKA Cushing’s syndrome and disease, hypercortisolism) .................... 187
86) 12 – Hypocorticism (AKA adrenal insufficiency, Addison’s disease)....................................... 189
87) Hypogonadism. Clinical features ............................................................................................. 193
88) Autoimmune disorders of the thyroid gland ............................................................................. 194
89) Polycystic ovary syndrome ...................................................................................................... 197
VI. Gastroenterology ................................................................................................. 201
90) Gastroesophageal reflux disease (GERD) .............................................................................. 201
91) H. pylori infection ..................................................................................................................... 202
92) Peptic ulcer ............................................................................................................................. 203
93) Malabsorption .......................................................................................................................... 205
94) Ulcerative colitis and Crohn’s disease – inflammatory bowel diseases (IBD) ......................... 206
95) Tumours of the colon (colorectal cancer – CRC) .................................................................... 210
96) Chronic viral hepatitis .............................................................................................................. 213
97) Fatty liver. Alcoholic and non-alcoholic steatohepatitis ........................................................... 218
98) Primary biliary cirrhosis (PBC). Primary sclerosing cholangitis ............................................... 219
99) Autoimmune hepatitis .............................................................................................................. 221
100) Liver cirrhosis – etiology, pathogenesis, clinical features...................................................... 222
101) Liver cirrhosis – complications: oesophageal varices, ascites, spontaneous bacterial peritonitis
(SBP), hepatorenal syndrome, portal encephalopathy .................................................................. 225
102) Ascites – diagnosis, differential diagnosis, treatment............................................................ 229
103) Cholelithiasis – etiology, pathogenesis, clinical features....................................................... 231
104) Cholelithiasis – complications: cholecystitis, cholangitis ....................................................... 233
105) Acute and chronic pancreatitis .............................................................................................. 236
106) Cholestasis/jaundice ............................................................................................................. 239
VII. Nephrology (Renal diseases) ............................................................................. 242
109) Membranous glomerulonephritis ........................................................................................... 246
110) IgA glomerulonephritis .......................................................................................................... 247
111) Membranoproliferative glomerulonephritis (MPGN) .............................................................. 247
112) Lupus nephritis ...................................................................................................................... 248
114) Renal Amyloidosis ................................................................................................................. 251
115) Acute urinary tract infections (UTIs) ...................................................................................... 253
116) Chronic pyelonephritis ........................................................................................................... 255
117) Renal tuberculosis ................................................................................................................. 256
118) Nephrolithiasis ....................................................................................................................... 257
119) Adult polycystic renal disease ............................................................................................... 258
120) Acute renal failure – renal parenchyma and treatment ......................................................... 260
121) Chronic renal failure – stages and clinical course ................................................................. 264
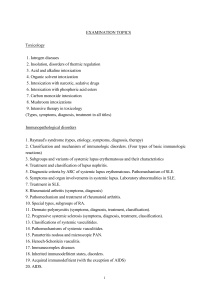
VIII. Toxicology and Allergology ................................................................................ 268
122) Toxicodynamics and toxicokinetics of exogenous poisons ................................................... 268
123) Treatment of acute exogenous poisoning ............................................................................. 269
124) Acute exogenous poisoning w/medicines used to treat cardiovascular diseases,
benzodiazepines, antipsychotics, antidiabetic, antipyretic, analgesics, and antiemetic agents .... 271
125) Acute exogenous poisoning w/alcohols: ethanol, methanol, ethylene glycol ........................ 274
126) Acute exogenous poisoning w/psychoactive substances...................................................... 276
127) Acute exogenous poisoning w/organophosphate compounds .............................................. 278
128) Acute exogenous poisoning w/carbon monoxide .................................................................. 279
129) Snake venom poisoning ........................................................................................................ 280
130) Acute exogenous poisoning w/mushrooms ........................................................................... 281
131) Hereditary angioedema (HAE) .............................................................................................. 283
132) Asthma: epedimiology, pathogenesis, clinical features, diagnosis and differential diagnosis 284
133) Insect allergy ......................................................................................................................... 289
134) Food allergy .......................................................................................................................... 290
135) Drug allergy: type I, II, III ....................................................................................................... 291
136) Drug allergy: type IV a, b, c, d ............................................................................................... 295
137) Anaphylaxis ........................................................................................................................... 297
138) Hypersensitivity pneumonitis (AKA extrinsic allergic alveolitis) ............................................. 298
IX. Oncologic Diseases ............................................................................................. 300
139) Renal tumors ......................................................................................................................... 300
141) Esophageal cancer ............................................................................................................... 306
142) Gastric cancer ....................................................................................................................... 307
143) Tumors of the colon .............................................................................................................. 309
144) Liver tumors .......................................................................................................................... 312
145) Pancreatic cancer ................................................................................................................. 315
146) Carcinoma of the biliary duct ................................................................................................. 317
147) Tumor of the thyroid gland .................................................................................................... 318
X. Principles of Treatment ......................................................................................... 323
148) Treatment of peptic diseases of the gastrointestinal tract ..................................................... 323
149) Treatment of Helicobacter pylori infection ............................................................................. 324
150) Principles in treatment of chronic liver disease ..................................................................... 326
151) Treatment of chronic viral hepatitis ....................................................................................... 328
152) Treatment of the liver cirrhosis complications: esophageal varices, ascites, spontaneous
bacterial peritonitis, hepato-renal syndrome, encephalopathy ...................................................... 330
153) Treatment of chronic cholestasis........................................................................................... 334
154) Antibacterial treatment of the biliary tract infection................................................................ 335
155) Treatment principles in poisoning.......................................................................................... 336
156) Treatment of urinary tract infection........................................................................................ 338
157) Treatment in glomerulonephritis ............................................................................................ 340
158) Diabetes mellitus - treatment with insulin and oral medications ............................................ 344
159) Treatment of diabetic complications. ..................................................................................... 350
160) Treatment with NSAIDs ......................................................................................................... 352
161) Treatment in predialysis period of chronic renal failure and indications for dialysis .............. 354
162) Clinical and pharmacological approach in NSAIDs therapy. ................................................. 357
163) Treatment of bacterial infection ............................................................................................. 357
164) Treatment with diuretics ........................................................................................................ 362
165) Treatment with steroids ......................................................................................................... 367
166) Treatment with immunomodulators ....................................................................................... 370
167) Treatment with cytostatics ..................................................................................................... 373
168) Treatment of the thromboembolism ...................................................................................... 376
169) Treatment of pneumonia ....................................................................................................... 379
170) Treatment of asthma. ............................................................................................................ 381
I.Pulmonology
1) Acute bronchitis, tracheobronchitis, bronchiolitis
Acute bronchitis (AKA chest cold)
Definition = short-term (acute) inflammation of the bronchi
Etiology = virus (most common – >90% - influenza A and B, parainfluenza, adenovirus, RSV,
rhinovirus, coronavirus) or bacterial infection, air pollution.
Pathophysiology
•
Damage caused by irritation of the airways → inflammation → neutrophils infiltrate the lung
tissue
•
Mucosal hypersecretion is promoted by a substance released by neutrophils
•
Further obstruction to the airways is caused by > goblet cells in the small airways (chronic
bronchitis)
Symptoms
•
Cough: dry in the beginning later w/sputum (expectorating cough). Self-limiting 2/3wks
•
Chest pain (retrosternal) during cough as a sign of tracheitis
•
Runny nose, sore throat, headache (symptoms of the preceding/ simultaneous URTI)
•
SOB (in bronchiolitis), wheezing
•
Fever, fatigue, weakness (malaise), loss of appetite, myalgias
Physical examination
•
Acute bronchitis is a clinical diagnosis
•
Coarse or ↓ vesicular breathing
•
Auscultation = wheezing, rhonchi, coarse crackles.
Lab tests
•
Blood = ↑ WBC, sedimentation rate, and CRP
•
Microbiology = sputum culture for bacterial infection, serological test for viral infection
Instrumental tests
•
Chest X-ray = ↑ lung markings. Chest X-ray used to exclude pneumonia
•
Spirometry = Restrictive type respiratory failure in bronchiolitis (↓ FVC and FEV1, FEV1/FVC
≥ 70%)
•
Blood gases = hypoxemia often w/hypercapnia in bronchiolitis
Complications = pneumonia and chronic bronchitis
Treatment = most cases are self-limiting and resolve themselves w/in a few weeks. Pain meds
(NSAIDs) help with symptoms; rest and hydration recommended. Anti-B not recommended
Tracheobronchitis
Definition = inflammation of the trachea and bronchi. It is characterised by a cough, fever, and
purulent sputum ∴ suggestive of pneumonia.
Etiology
•
Ventilator-associated = nosocomial infection usually contracted in an ICU when a mechanical
ventilator is used. The insertion a tracheal tube can cause an infection in the trachea which
then colonises and spreads to the bronchi
•
Fungal
•
Herpetic = caused by the HSV and causes small ulcers covered in exudate (containing
necrotic cells from the mucosal epithelium) to form on the mucous membranes
Bronchiolitis
Definition = blockage of the bronchioles in the lungs due to a viral infection. It usually only occurs in
children <2 years
Etiology = most commonly caused by RSV or human rhinovirus
Risk factors = preterm infant, younger age at onset of illness (<3 months), congenital heart disease,
immunodeficiency, chronic lung disease, neurological disorders, tobacco smoke exposure
Clinical findings = initially fever, rhinorrhoea, cough; respiratory distress as a result of bronchiole
obstruction presents w/tachypnoea, prolonged expiration, nasal flaring, cyanosis
Diagnosis
•
Clinical examination – auscultation = wheezing, crackles
•
CXR sometimes useful to exclude pneumonia, but not indicated in routine cases
DDx = asthma, bacterial pneumonia, congenital heart disease, whooping cough, CF, allergic rxn, FB
aspiration
Treatment
•
Infection will run its course and complications are typically from symptoms themselves.
•
Maintaining hydration and diet is important in management
•
Children w/severe symptoms may be considered for hospital admission – indications include =
toxic appearance, poor feeding, pO2 <92%, pre-existing heart/lung/neurological conditions,
immunodeficiency
2) Chronic bronchitis, pulmonary emphysema, COPD
Chronic bronchitis
Definition = productive cough that lasts for at least 3 months/> per year for 2 consecutive years.
When this occurs together w/↓ airflow it is known as COPD.
Pathophysiology
•
Smoking → exposure to irritants and chemicals → hypertrophy and hyperplasia of bronchial
mucinous glands (main bronchi) and goblet cells (bronchioles) → ↑ mucous production →
airway obstruction
•
Smoking = cilia are < mobile = hard to move mucous
•
Mucous hypersecretion + poor cilia function = productive cough
Excess mucus can narrow the airways, thereby limiting airflow and accelerating the decline in lung
function, and result in COPD. Excess mucus shows itself as a chronic productive cough and its
severity and volume of sputum can fluctuate in periods of acute exacerbations.
Predisposition factors = frequent respiratory infections, smoking, polluted environment
Symptoms = occasionally, slight morning cough; during exacerbation same as acute bronchitis
Physical examination, lab tests, and instrumental tests in cases w/exacerbation same as in acute
bronchitis
Complications
•
Bronchiectasis
•
Pulmonary emphysema (COPD)
•
Pneumofibrosis
•
Possible predisposition factor for neoplasm
Pulmonary emphysema
Definition = permanent dilation of pulmonary air spaces distal to the terminal bronchioles, caused by
destruction of the alveolar walls and pulmonary capillaries required for gas exchange.
Etiology
•
Smoking (incites lung injury)
•
Inherited (congenital) α1-antitrypsin (enz. protecting the lung from protease enz. such as
neutrophil elastase) deficiency
•
Pulmonary emphysema is a complication of chronic bronchitis, bronchiectasis, and bronchial
asthma
Pathophysiology
•
Emphysema is due to breakdown of elastin and other
alveolar wall components by proteases. Normally antiprotease enz. (e.g. α1-antitrypsin) protect the lung. In
emphysema:
•
Cigarette smoke/other irritants → attraction of
inflammatory cells → release of elastase (usually
inhibited by α1-antitrypsin) – in smokers anti-protease
production and release may be inadequate to
neutralise the excess protease production →
destruction of elastic fibers in lung → emphysema
Classification
•
Centrilobular emphysema (centroacinar emphysema) = most common type; classically seen
in smokers; characterised by destruction of the respiratory bronchiole (central portion of the
acinus); spares distal alveoli; affects upper lobes
•
Panlobular emphysema (panacinar emphysema) = rare; associated w/ α1-antitrypsin
deficiency; characterised by destruction of the entire acinus (respiratory bronchiole and
alveoli); affects lower lobes
•
Cicatricial emphysema = caused by exposure to quartz dust; characterised by chronic
inflammation and nodular scar formation
•
Giant bullous emphysema = characterised by large bullae that extrude into surrounding tissue;
bullae may rupture → pneumothorax
•
Senile emphysema = loss of pulmonary elasticity w/age; non-pathological – normal
consequence of aging
Symptoms
•
SOB, initially during exercise, later at rest, but it is not relieved significantly in sitting position
•
Cough w/sputum
•
Easy tiredness, fatigue
Physical examination
•
In patient w/respiratory failure = general cyanosis and polycythaemia
•
Short neck, sometimes high neck vv.
•
Barrel chest = occurs because the lungs are chronically overinflated w/air, so the rib cage
stays partially expanded all the time
•
↓ vocal fremitus, box-like percussion sound, lower position of lung bases, ↓respiratory
mobility, ↓ vesicular breathing w/prolonged exhale, often whistling and snoring wheezes.
Lab tests
•
Blood = ↑ Hb, RBC, HTC; ↓ sedimentation rate in patients w/respiratory failure and
polycythemia
•
Tests for infection are often required
Instrumental tests
•
Chest X-ray = > air in the lungs, dilated intercostal spaces, often ↑ lung markings for
concomitant chronic bronchitis and bronchiectasis
•
Spirometry = obstructive type respiratory failure (FEV1/FVC < 70%)
•
Blood gases = hypoxemia and hypercapnia, ↓ O2 saturation
Complications = R side HF, pneumothorax (very rare)
Chronic obstructive pulmonary disorder (COPD)
Definition = a type of obstructive lung disease characterised by chronic breathing problems and poor
airflow.
The term COPD encompasses 2 types of obstructive airway disease: emphysema, w/enlargement of
airspaces and destruction of lung tissue, and chronic (obstructive) bronchitis, w/↑ mucous production,
obstruction of small airways, and a chronic productive cough. People w/COPD often have
overlapping features of both disorders
Etiology = tobacco smoking, air pollution, occupational exposure, genetics
Classification (Global initiative for chronic obstructive lung disease – GOLD)
•
GOLD classifies COPD according to the severity of airflow limitation (GOLD 1-4) and the
ABCD assessment tool, which takes into account the modified British medical Research
Council dyspnoea scale, COPD assessment tool (CAT), and risk of exacerbation
•
COPD was previously classified into chronic bronchitis and emphysema. This is now
considered outdated as most COPD patient have a combo of both
Category
Symptoms
Exacerbations per year
FEV1% predicted
GOLD 1 (Class I)
Mild
≤ 1 (w/no hospital admission)
≥ 80%
GOLD 2 (Class II)
Moderate
≤ 1 (w/no hospital admission)
50% ≤ FEV1 < 80%
GOLD 3 (Class III)
Severe
GOLD 4 (Class IV)
•
≥2
•
≥ 1 leading to hospital
admission
30% ≤ FEV1 < 50%
Very severe
< 30%
Clinical findings
•
Symptoms are minimal or non-specific until the disease reaches an advanced stage
•
Presenting findings = chronic productive cough, SOB, tachypnoea, pursed lip breathing (>
common in emphysema), prolonged exhalation (> work needed to exhale), wheezing, crackles
cyanosis due to hypoxemia, tachycardia
•
Barrel chest is characteristic sign of COPD (> common in emphysema)
•
Advanced COPD = pulmonary HT → R sided heart failure (cor pulmonale) – symptoms
include peripheral oedema and bulging neck vv. (sign of ↑ jugular venous pressure)
•
Asynchronous movement of the chest and abdomen during respiration
•
Use of accessory respiratory muscles due to diaphragmatic dysfunction
•
Hyperresonant lungs; ↓ diaphragmatic excursion, and relative cardiac dullness on percussion;
↓ breath sounds on auscultation (“silent lung”)
•
Nail clubbing in the case of certain comorbidities (e.g. bronchiectasis, pulmonary fibrosis, lung
cancer)
•
“Pink puffer” – for people w/predominant emphysema = lack of cyanosis, the use of accessory
muscles, and pursed-lip (“puffer”) breathing
•
“Blue bloaters” – for people w/predominant chronic bronchitis = cyanosis (due to hypercapnia)
and fluid retention associated w/R sided heart failure
Pink puffer
Main pathomechanism
Clinical features
Emphysema
Blue bloater
Chronic bronchitis
•
Non-cyanotic
•
Productive cough
•
Cachectic (physical wasting)
•
Overweight
•
Pursed lip breathing
•
Peripheral oedema
•
Mild cough
PaO2
Slightly ↓
Markedly ↓
PaCO2
Normal (possibly in late hypercapnia)
↑ (early hypercapnia)
Diagnosis
•
Considered in anyone >35-40 who has SOB, chronic cough, sputum production, or frequent
winter colds and a history of exposure to risk factors for the disease
•
Pulmonary function test (spirometry – gold standard, confirms the diagnosis) = FEV1/FVC <
70%; ↓ FEV1 (<80%) (MNEMONIC = COP w/low FEVer)
•
ABG = many patients w/severe COPD have chronic hypercapnia due to CO2 trapping from
hyperinflation and progressive loss of pulmonary elasticity
•
CBC = ↑ serum hematocrit (chronic hypoxemia → ↑ release of EPO → ↑ erythropoiesis → ↑
secondary polycythemia (↑ in total RBC mass))
•
CXR = hyperinflated lungs (barrel chest), flattened diaphragm, ↑ retrosternal space, and
bullae
•
High-resolution CT of the chest may show the distribution of emphysema throughout the lungs
DDx
•
Other causes for SOB = congestive HF, PE, pneumonia, pneumothorax
•
Asthma = distinction is made on the basis of the symptoms, smoking history, and whether
airflow limitation is reversible w/bronchodilators at spirometry (post-bronchodilator test –
spirometry to establish baseline, inhalation of salbutamol, repeat spirometry again after 10-15
mins)
Delta FEV1 <12% (irreversible bronchoconstriction) = COPD is > likely
Delta FEV1 >12% (reversible bronchoconstriction) = asthma is > likely
Management
•
Stopping smoking, pulmonary rehabilitation (program of exercise, disease management, and
counselling, coordinated to benefit the individual), non-invasive ventilation, O2 therapy (PO2
<50-55 mmHg or O2 saturation <88%)
•
Vaccinations = pneumococcal (↓ incidence community-acquired pneumonia and invasive
pneumococcal disease), influenza (↓ incidence of lower RT infections and death)
1st line treatment of COPD consists of bronchodilators, inhaled corticosteroids (ICS), and
phosphodiesterase (PDE) type 4 inhibitors:
•
Bronchodilators:
Short-acting beta agonists (SABAs) = e.g. salbutamol,
fenoterol
Long-acting beta agonists (LABAs) = e.g. salmeterol,
formoterol
Short-acting muscarinic antagonists (SAMAs) = e.g.
Ipratropium bromide
Long-acting muscarinic antagonists (LAMAs) = e.g. Tiotropium bromide
•
ICS = e.g. Budesonide, fluticasone, Beclomethasone
•
PDE type 4 inhibitors = e.g. roflumilast
•
Theophylline can be used for severe and refractory COPD; long-term O2 therapy can be used
in case of PaO2 ≤ 55 mmHg or SaO2 ≤ 88% at rest
3) Respiratory failure – pathophysiology and clinical features
Definition = failure of the respiratory system to maintain gas exchange → hypoxia or hypercapnia
Classification and Etiology
Type 1 (hypoxemic)
•
Defined as hypoxemia (PaO2 < 60 mmHg) w/normo- or hypocapnia (PaCO2 ≤ 50 mmHg)
•
It is due to failure of the gas exchange function of the lung – failure of the lungs and heart to
provide adequate O2 to meet metabolic needs
This type of respiratory failure is caused by conditions that affect oxygenation such as:
•
Low ambient O2 (e.g. at high altitudes)
•
Ventilation-perfusion (V/Q) mismatch – most common = ↓ ventilation to normally perfused
regions or ↓ perfusion to normally ventilated regions (e.g. pulmonary embolism)
•
Alveolar hypoventilation = ↓ minute volume due to ↓ respiratory muscle activity (e.g. in acute
neuromuscular disease); this form can also cause type 2 respiratory failure if severe
•
Diffusion impairment = impaired gas exchange due to ↑ in distance for diffusion or a ↓ in the
permeability/SA of the respiratory membranes. Most commonly occurs in parenchymal
diseases such as pneumonia, pulmonary oedema, and ARDS
•
Shunt = pathologic condition in which alveoli are perfused but not ventilated – oxygenated
blood mixes w/non-oxygenated blood from the venous system (e.g. R→L shunt)
Type 2 (hypercapnic)
•
Defined as hypoxemia (PaO2 < 60 mmHg) w/hypercapnia (PaCO2 > 50 mmHg)
•
It is due to ventilatory failure – people are unable to maintain a level of alveolar ventilation
sufficient to eliminate CO2 and keep arterial O2 levels w/in normal range. Underlying
mechanism is hypoventilation
The underlying causes include:
•
↑ airway resistance (e.g. COPD, asthma, suffocation)
•
↓ breathing effort (e.g. drug effects, brain stem lesion, extreme obesity)
•
↓ in the area of the lung available for gas exchange (e.g. chronic bronchitis)
•
Neuromuscular problems (e.g. Guillain-Barre syndrome, motor neuron disease)
•
Deformed (kyphoscoliosis), rigid (ankylosing spondylitis), or flail chest
Type 3 (peri-operative)
•
Generally a subset of type 1 failure but is sometimes considered separately because it is so
common
•
Residual anaesthesia effects, post-operative pain, and abnormal abdominal mechanics
contribute to ↓ FRC and progressive collapse of dependant lung units
•
Causes of post-operative atelectasis include = ↓ FRC, supine/obese/ascites, anaesthesia,
upper abdominal incision, airway secretions
Type 4 (shock)
•
Describes patients who are intubated and ventilated in the process of resuscitation for shock
•
Cardiogenic, hypovolemic, septic
Clinical manifestations
Signs and symptoms of type I RF
(hypoxemia)
Signs and symptoms of type II RF
(hypercapnia)
Dyspnoea, irritability
Headache
Confusion, somnolence, fits
Behavioural change
Tachycardia, arrhythmia
Coma
Tachypnoea
Papilloedema
Cyanosis
Warm extremities
There are signs that suggest a possible underlying cause of RF including:
•
Hypotension usually w/signs of poor perfusion suggest severe sepsis or pulmonary embolism
•
HT usually w/signs of poor perfusion suggests cardiogenic pulmonary oedema
•
Wheeze and stridor suggest airway obstruction
•
Tachycardia and arrhythmias may be the cause of cardiogenic pulmonary oedema
•
Elevated jugular venous pressure suggests R ventricular dysfunction
•
Respiratory rate < 12 beats/min in spontaneously breathing patient w/hypoxia suggest
nervous system dysfunction
•
Paradoxical respiratory motion suggest muscular dysfunction
Diagnosis
•
ABGs; renal and liver function tests (may indicate etiology); CBC
•
Pulmonary function test = identifies obstruction, restriction, and gas diffusion abnormalities.
Normal FEV1 and FVC suggest disturbance in respiratory control; ↓ FEV1/FVC indicates
airflow obstruction; ↓ FEV1 and FVC and maintenance of FEV1/FVC suggests restrictive lung
disease
•
Capnography = provides a continuous reading of respiratory function and end tidal CO2
•
Pulse oximetry = gives a continuous measure of blood oxygen saturation
•
ECG = to monitor cardiac function
Treatment
•
Treatment of the underlying cause, if possible. This may involve medication such as
bronchodilators, anti-B, glucocorticoids, diuretics, amongst others. Respiratory
therapy/physiotherapy may be beneficial in some causes of RF
•
Type 1= O2 therapy to achieve adequate O2 saturations. Lack of response to O2 may be an
indication for other modalities such as heated humidified high-flow therapy, continuous
positive airway pressure (CPAP) or (if severe) endotracheal intubation and mechanical
ventilation
•
Type 2 = non-invasive ventilation, unless medical therapy can improve the situation
4) Bacterial Community-acquired pneumonia (CAP)
5) Non-Bacterial Community-acquired pneumonia (CAP)
6) Hospital-acquired pneumonia (HAP)
Definition = respiratory infection characterised by inflammation of the alveolar space and/or the
interstitial tissue of the lungs.
Etiology
Type of pneumonia
CAP
Common pathogens
Typical pneumonia:
•
Streptococcus pneumoniae (most common)
•
H. influenzae
•
M. catarrhalis
•
K. pneumoniae
•
S. aureus
Atypical pneumonia:
•
Bacteria = M. pneumoniae (most common); Chlamydia pneumoniae;
L. pneumophila → legionellosis; C. burnetti → Q fever
•
Viruses = RSV, influenza, CMV, adenovirus, SARS-CoV-2
•
HAP
G(-) pathogens = P. aeruginosa; enterobacteriaceae, Acinetobacter
species
•
S. aureus
•
S. pneumoniae
Lobar pneumonia
S. pneumoniae is most common cause
Bronchopneumonia
S. pneumoniae, S. aureus, H. influenzae
Interstitial pneumonia
M. pneumoniae, C. pneumonia, Legionella, viruses (RSV, CMV, influenza)
Pneumonia in
immunocompromised patients
Bacteria
•
Encapsulated bacteria (S.Pneumoniae, H.influenzae)
•
S. aureus
• G -ve bacteria
Fungal
•
Pneumocystis jirovecii
•
Aspergillus fumigatus
•
Histoplasma capsulatum
•
Candida species
•
Coccidioides immitis
Viral
•
CMV
Risk factors
•
Old age and immobility of any cause
•
Chronic diseases = pre-existing cardiopulmonary conditions (asthma, COPD, HF),
acquired/congenital abnormalities of the airways
•
Immunosuppression = HIV, DM, alcoholism, malnutrition
•
Impaired airway protection = altered consciousness (stroke, seizure, anaesthesia,
drugs/alcohol), dysphagia, smoking,
•
Environmental factors = crowded living conditions, toxins
Classification
Etiology
•
Primary pneumonia = no apparent pre-existing conditions that may predispose to pneumonia
•
Secondary pneumonia = pre-existing conditions that predispose to pneumonia – asthma,
COPD, HF, CF, viral URT infections, anatomical abnormalities, bronchial tumours
Location acquired
•
Community-acquired pneumonia (CAP) = pneumonia acquired outside of a healthcare
establishment
•
Hospital-acquired pneumonia (HAP) = nosocomial pneumonia, w/onset >48 hours after
admission. Ventilator-associated pneumonia is a subtype
•
Healthcare-associated pneumonia = pneumonia that is acquired in healthcare facilities
Clinical features
•
Typical pneumonia = pneumonia featuring classic symptoms (typical findings on auscultation
and percussion); manifests as lobar or bronchopneumonia
•
Atypical pneumonia = pneumonia w/< distinct classical symptoms and often unremarkable
findings on auscultation and percussion; manifests as interstitial pneumonia
Area of the lung affected
•
Lobar pneumonia = pneumonia affecting one lobe of a lung. Multilobar pneumonia refers to
involvement of multiple lobes; panlobar pneumonia involves all the lobes of a single lung
•
Bronchopneumonia = pneumonia affecting the tissue around the bronchi and/or bronchioles
•
Interstitial pneumonia = pneumonia affecting the tissue between the alveoli
•
Cryptogenic organising pneumonia = non-infectious pneumonia of unknown etiology
characterised by involvement of the bronchioles, alveoli, and surrounding tissue
Pathophysiology
Most commonly spread by microaspiration (droplet infection) of airborne pathogens or oropharyngeal
secretions
1) Failure of protective pulmonary mechanisms – e.g. cough reflex, mucociliary clearance,
alveolar macs
2) Infiltration of pulmonary parenchyma by the pathogen → interstitial and alveolar inflammation
3) Impaired alveolar ventilation → V/Q mismatch w/intrapulmonary shunting
4) Hypoxia due to ↑ alveolar-arterial O2 gradient
Pattern of involvement
Lobar pneumonia
•
Classic (typical) pneumonia of an entire lobe; primarily caused by pneumococci
•
Characterised by inflammatory intra-alveolar exudate, resulting in consolidation
•
Can involve the entire lobe or the whole lung
•
Stages = congestion (day 1-2), red hepatisation (day 3-4), grey hepatisation (day 5-7), and
resolution (day 8 to week 4). In stage 1 and 2 the alveolar lumen are only partially filled,
whereas in stage 2 and 3 they are filled w/exudate rich in RBC and WBC respectively
Bronchopneumonia
•
Most commonly a descending infection that is characterised by acute inflammatory infiltrates
that fill the bronchioles and adjacent alveoli (patchy distribution)
•
Usually involves the lower lobes or R middle lobe and affects ≥1 lobe
•
Manifests as typical pneumonia
Interstitial pneumonia
•
Characterised by a diffuse patchy inflammation that mainly involves the alveolar interstitial
cells
•
Bilateral multifocal opacities are classically found on CXR
•
Manifests as atypical pneumonia
•
Often has an indolent course (walking pneumonia)
Clinical manifestations
Typical pneumonia
Characterised by sudden onset of symptoms caused by lobar infiltration
•
Severe malaise
•
High fever and chills
•
Productive cough w/purulent sputum (yellow-green)
•
Tachypnoea and dyspnoea (nasal flaring, thoracic retractions)
•
Pleuritic chest pain when breathing, often
accompanying pleural effusion
•
Pain that radiates to the abdomen and epigastric
region (particularly in children
•
On examination = crackles and bronchial breathing on
auscultation; enhanced bronchophony, egophony, and
tactile fremitus; dullness on percussion (indicated
consolidation in cases of localised pneumonia)
Atypical pneumonia
Typically has an indolent course (slow onset) and commonly
manifests w/extrapulmonary symptoms
•
Dry cough
•
Dyspnoea
•
Auscultation often unremarkable
•
Common extrapulmonary features = fatigue, headaches, sore throat, myalgias, malaise
Diagnosis
•
Labs = CBC and inflammatory markers (↑ CRP and ESR, leukocytosis); ↑ serum procalcitonin
(an acute phase reactant that can help diagnose bacterial LRT infections); ABG = ↓ PaO2,
BMP, LFT’s
•
Microbiological blood + sputum culture, Ag test (pneumococcal urinary), PCR
(chlamydophilia), NAAT (Influenza, RSV)
•
CXR = opacity of ≥1 lobes (lobar); air bronchograms (appearance of translucent bronchi
inside opaque areas of alveolar consolidation); poorly defined patchy infiltrates scattered
throughout the lungs (bronchopneumonia); diffuse reticular opacity and absence of
consolidation (interstitial)
•
CT w/out contrast = localised areas of consolidation, air bronchograms, ground-glass
opacities, pleural effusion/empyema, nodules
•
Bronchoscopy = indicated in inconclusive CT and need for pathohistological diagnosis
•
Diagnostic thoracentesis
7) Treatment of pneumonia
Criteria for hospitalisation
Every patient should be assessed individually and clinical judgement is the most important factor. The
pneumonia severity index (PSI) and the CURB-65 score are tools that can help to determine whether
to admit a patient.
CURB-65 score
•
Confusion (disorientation, impaired consciousness)
•
Serum Urea > 7 mmol/L
•
Respiratory rate ≥30/min
•
BP = systolic ≤90 mmHg or diastolic ≤60 mmHg
•
Age ≥ 65 years
•
Each finding is assigned 1 point
•
Score 0 or 1 = patient may be treated as outpatient
•
Score ≥2 = hospitalisation is indicated
•
Score ≥ 3 = consider ICU level of care
•
If serum urea level is not known or unavailable, a score of ≥1 requires hospitalisation
Supportive therapy
•
Sufficient rest (not absolute bed rest) and physical therapy
•
Hydration with PO fluids or IV fluids (see IV fluids)
•
Treat hypoxemia.
•
Supplemental oxygen as needed for hypoxia, mechanical ventilation
•
Incentive spirometer
•
Antipyretics, analgesics as needed (e.g., acetaminophen)
•
Expectorants and mucolytics (N-acetyl cysteine)
•
Antitussives (e.g., codeine)
Empiric anti-B therapy for CAP in an outpatient setting
Patient profile
Recommended empiric anti-B regimen
Previously healthy
patient w/out
comorbidities or risk
factors for resistant
pathogens
Monotherapy w/one of the following:
Patients w/comorbidities
or risk factors for
resistant pathogens
Combo therapy
•
Amoxicillin (500 mg 3X/day)
•
Doxycycline (200 mg on 1st day, then 100 mg 1X/day orally)
•
Macrolide – azithromycin or clarithromycin (500 mg 2X/day)
•
In pregnancy = erythromycin (500 mg 4X/day)
•
An anti-pneumococcal β-lactam (amoxicillin-clavulanate, cefuroxime,
cefpodoxime) PLUS azithro-/clarithromycin or doxycycline
Monotherapy w/a respiratory fluoroquinolone:
•
Gemifloxacin (320 mg 1X/day)
•
Moxifloxacin (400 mg 1X/day)
•
Levofloxacin (500 mg 2X/day)
•
5 days of therapy is usually sufficient for CAP that is treated in the outpatient setting
•
Any patient being treated in a primary care setting should be re-examined after 48-72 hours to
evaluate the efficacy of the prescribed anti-B
Empiric anti-B therapy for CAP in an inpatient setting
Patient profile
Non-severe CAP/non-ICU
treatment
Recommended empiric anti-B regimen
Combo therapy
•
An anti-pneumococcal β-lactam (amoxicillin-sulbactam,
ceftriaxone, cefotaxime) PLUS azithro-/clarithromycin or
doxycycline
Monotherapy w/a respiratory fluoroquinolone:
•
Gemifloxacin (320 mg IV 1X/day)
•
Moxifloxacin (400 mg IV 1X/day)
•
Levofloxacin (500 mg IV 2X/day)
Severe CAP/ICU treatment
Combo therapy
•
An anti-pneumococcal β-lactam (amoxicillin-sulbactam,
ceftriaxone, cefotaxime) PLUS azithro-/clarithromycin or
doxycycline or a respiratory fluoroquinolone
Alternatives for patients w/a penicillin allergy:
Risk factors for MRSA
•
Aztreonam
•
PLUS a respiratory fluoroquinolone (moxi-/levofloxacin)
Add vancomycin (15-20 mg/kg IV every 8-12 hours) or linezolid (600
mg IV/oral every 12 hours, 10-14 days)
•
5-7 days is usually sufficient
•
Consider longer courses in: patients not responding to treatment; suspected or concern for
MRSA or P. aeruginosa infection; concurrent meningitis; unusual pathogens
•
If aztreonam is used instead of β-lactam anti-B (e.g. for penicillin allergy), the addition of
MSSA (methicillin susceptible S. aureus) (e.g. a fluoroquinolone) is necessary
•
Anaerobic coverage is not routinely recommended for suspected aspiration pneumonia
(unless lung abscess or empyema is suspected)
•
Corticosteroids are not routinely recommended as adjunct therapy
Empiric anti-B therapy for hospital-acquired pneumonia
Patient profile
Patients not at high risk for
mortality and w/out risk
factors for MRSA infection
Recommended empiric anti-B regimen
Monotherapy:
•
meropenem, cefepime, piperacillin-tazobactam
•
Patients not at high risk for
mortality but w/risk factors for
MRSA infection
An anti-pneumococcal, anti-pseudomonal β-lactam = imipenem,
OR levofloxacin
Combo therapy:
•
One of the following anti-B w/MRSA activity = Vancomycin or
Linezolid
PLUS one of the following:
•
Anti-pneumococcal, anti-pseudomonal β-lactam = Piperacillintazobactam, cefepime, ceftazidime, meropenem, imipenem
Patients at high risk for
mortality and patients
w/structural lung diseases
•
A fluoroquinolone = levo-/ciprofloxacin
•
Aztreonam
Combo therapy:
•
One of the following anti-B w/MRSA activity = Vancomycin or
Linezolid
PLUS any two of the following (avoid combining 2 β-lactams):
•
Anti-pneumococcal, anti-pseudomonal β-lactam = Piperacillintazobactam, cefepime, ceftazidime, meropenem, imipenem
•
A fluoroquinolone = levo-/ciprofloxacin
•
An aminoglycoside = Amikacin, Gentamicin, tobramycin
•
Aztreonam
•
Empiric anti-B therapy should be narrowed and/or de-escalated as soon as feasible
•
7 days of therapy are usually sufficient
•
Resistance patterns can vary widely; local antibiograms should be considered when starting
empiric treatment
8) Purulent diseases – bronchiectasis, pulmonary abscess
Bronchiectasis
Definition = an irreversible and abnormal dilation in the bronchial tree, leading to build-up of mucous
that can make the lungs > vulnerable to infection
Etiology
•
Pulmonary infections (i.e. bacterial, viral, fungal)
•
Disorders of secretion clearance or mucous plugging = CF, primary ciliary dyskinesia,
smoking
•
Bronchial narrowing or other forms of obstruction = COPD, aspiration, tumours, other
congenital and acquired conditions (congenital bronchiectasis, tracheomalacia)
•
Immunodeficiency
•
Chronic autoimmune inflammatory diseases = RA, Sjogren’s syndrome
Pathophysiology
•
Development requires 2 factors: an infectious insult and impaired drainage, obstruction, or a
defect in host defence
•
This triggers a host immune response from neutrophils (elastases), ROS, and inflammatory
cytokines that result in progressive destruction of normal lung tissue
•
“Vicious cycle” theory = predisposed individual develops an excessive inflammatory response
to pulmonary infection or tissue injury. The inflammation that results is partially responsible for
the structural damage to the airways. Structural abnormalities then allow for the stasis of
mucous, which favour continued chronic infection and the persistence of the vicious cycle.
Symptoms
•
Chronic productive cough (lasting months to years), w/copious mucopurulent sputum. The
sputum is in 3 levels – upper foam-like, middle (mucous) and lower (purulent).
•
Dyspnoea
•
Occasionally haemoptysis (blood in sputum)
•
Bad breath (halitosis, oral malodour)
•
Rhinosinusitis
•
Non-specific symptoms = fatigue, weight loss, pallor due to anaemia
•
During exacerbation the same as in acute bronchitis, but more severe, similar to pneumonia
Physical examination
Mainly in auscultation – crackles and rhonchi; wheezing (due to obstruction from secretions, airway
collapsibility, or a concomitant condition); bronchophony; occasionally clubbing of the fingers
Lab tests
•
Blood = ↑ WBC, neutrophils, sedimentation rate, and CRP in cases w/inflammation. May show
anaemia of chronic disease
•
Microbiology = sputum culture
Instrumental tests
• CXR (best initial test) = inflammation and fibrosis of bronchial walls → “tram track” lines; thinwalled cysts, possible w/air-fluid levels; late stage disease = honeycombing
• High-resolution CT (confirmatory test) = dilated bronchi w/thickened walls; possible signet-ring
appearance and tram track lines; cysts and honeycombing
• Sputum culture and smear = to determine infectious etiology
• Spirometry = findings consistent w/obstructive pulmonary disease (↓ FEV1/FVC)
• Bronchoscopy = to visualise tumours, FBs, or other lesions
• Blood gases = hypoxemia, sometimes w/hypercapnia
Management
• Acute exacerbation
o
o
o
Mucolytics
Outpatient anti-B: Fluoroquinolones (Lexofloxacin)
Inpatient anti-B: MRSA (vancomycin, linezolid)
• Supportive measures
o Education, lifestyle changes, chest physiotherapy (airway clearance techniques)
o Vaccinations (influenza, pneumococcal)
o Long-term o2 therapy for chronic respiratory failure
o
Follow up every 6-12 months, spirometry every 12 months
• Treatment
o Mucoactive agents: Inhaled (hypertonic saline/ mannitol)/ Oral (N-acetly cysteine)
w/airway clearance techniques, such as high-frequency chest wall oscillation
o Bronchodilators (SABA, LABA, LAMA) in severe dyspnoea
o Corticosteroids – inhaled (asthma, CODD), systemic (ABPA)
o Long term anti-B therapy (≥ 3 exacerbations in 1 year)
w/out P. aeruginosa: Azithromycin
w/ P. aeruginosa: Tobramycin/ Aztreonam. Eradication (Oral Ciprofloxacin)
Non-tuberculous mycobacteria: Macrolide + Rifampin + Ethambutol
MRSA: eradication therapy
• Anti-inflammatories = macrolides and corticosteroids
• Invasive
o Surgical resection of bronchiectatic lung/ lobectomy: indicated in p. hemorrhage
o Pulmonary artery emobolization
o Lung transplantation
Complications
•
Local = pneumofibrosis, pulmonary emphysema
•
General = amyloidosis, respiratory failure
Pulmonary abscess
Definition = a localised collection of pus and necrotic tissue w/in lung parenchyma primarily caused
by aspiration, and secondarily by tumors, microbial infection, immunocompromised, septic emboli etc.
Risk factors =
•
Risk factors for aspiration, such as:
o
o
Impaired consciousness
Impaired swallow in neurological disorders and vocal cord paralysis
•
Increased oropharyngeal bacterial growth (e.g., periodontal disease, dental abscesses,
tonsillitis)
•
Bronchial obstruction (e.g., lung cancer, foreign body aspiration, bronchial stenosis)
•
Immunocompromised state
•
Pneumonia, bronchiectasis
•
Impaired respiratory mucus clearance (e.g., cystic fibrosis)
Causative pathogens
•
Most commonly = mixed infections caused by anaerobic bacteria that colonise the oral cavity
(e.g. Peptostreptococcus spp., Prevotella spp., Bacteroides spp., Fusobacterium spp.)
•
Less commonly = monomicrobial lung abscess caused by S. aureus, K. pneumoniae, or S.
pyogenes
•
Others
o
o
Parasitic (Entamoeba histolyitca)
Fungal (Aspergillus spp, Histoplasma spp)
Clinical manifestations = indolent presentation w/symptoms that evolve over weeks to months
(>6wks) or may be acute (< 4-6wks)
•
Fever
•
Cough w/production of foul-smelling purulent sputum
•
Anorexia, weight loss, fatigue
•
Night sweats
•
Hemoptysis
•
Pleuritic chest pain
Physical Exam
o Digital clubbing
o Dullness to percussion
o Amphoric breath sounds over abscess (harsh, hollow, high-pitched breath sounds)
Diagnosis
•
CXR/CT w/ IV contrast = irregular rounded cavity w/an air-fluid level that is dependent on
body position
o Location of abscess
Due to aspiration: typically unilateral
•
Right M lobe (typically caused by aspiration in the prone or upright
position)
•
Posterior segments of the U lobes or the superior segments of the L
lobes (typically caused by aspiration in the recumbent position).
Due to hematogenous dissemination: typically bilateral and multiple
•
CBC: ↑ WBC, maybe anemia of chronic disease
•
Gram stain, culture, and sensitivity of expectorated sputum/ pleural fluid (takes time, which is
why empirical treatment is usually initiated 1st)
•
Additional testing: HIV screening, bronchoscopy for FB, tumor, echocardiography for septic
endocarditis, clinical swallow assessment for dysphagia
Treatment
•
Admit and start immediate empiric ant-B therapy after cultures for 3-6wks
•
Anti-B treatment: Broad spectrum which covers anaerobes (e.g. ampicillin-sulbactam,
carbapenems, or clindamycin). Anti-B against Gram +ve cocci in IV drug use
o No risk of MRSA: Ampicillin-sulbactam (3g/day), Ceftriaxone+Metronidazole, Clindamy
o
•
Risk of MRSA: Vancomycin, Linezolid (600mg IV x2/day)
Interventional therapy for large abscess, significant hemoptysis, or if meds fail
o Bronchoscopic drainage/ percutaneous catheter drainage
o Surgical resection (segmentectomy or lobectomy) may be considered
Complications
•
Extension or rupture into the pleural cavity, causing:
o Pleural empyema
o Pleural effusion
o Bronchopulmonary fistula
o Pneumothorax
•
Recurrence of abscess
9) Pleural effusions
Definition = an excessive amount of fluid between the pleural layers that impairs the expansion of the
lungs OR an accumulation of fluid in the pleural cavity between the visceral and parietal pleurae
Etiology, pathophysiology, and classification
Pleural effusions can be classified by:
•
The origin of the fluid = serous fluid (hydrothorax), blood (hemothorax), chyle (Chylothorax),
pus (pyothorax/empyema)
•
By pathophysiology = transudative or exudative pleural effusion
Transudative pleural effusion
Definition
Transudate = extravascular fluid w/low
protein content and low specific
gravity.
Pathophysiology
Causes
•
↑ capillary hydrostatic pressure
•
↓ capillary oncotic pressure
(AKA colloid osmotic pressure)
•
Congestive HF
•
Hepatic cirrhosis
•
Nephrotic syndrome
•
Protein-losing enteropathy
•
Chronic kidney disease (Na+
retention)
Exudative pleural effusion
Exudate = any fluid that filters from the
circulatory system into lesions or areas of
inflammation. It has high protein content and
high specific gravity.
•
↑ capillary permeability (e.g. due to
inflammation)
•
Infection = pneumonia, TB, pleural
empyema, parasitic illness
•
Malignancies = lung cancer, metastatic
breast cancer, lymphoma,
mesothelioma
•
PE
•
Autoimmune disease = vasculitis,
lupus, RA, sarcoidosis
•
Trauma
•
Pancreatitis
Clinical manifestations
•
Patients w/small pleural effusion (<300 ml) are often asymptomatic
•
Characteristic symptoms = dyspnoea; pleuritic chest pain (sharp retrosternal pain) (can also
have abdominal pain which is confused w/acute appendicitis); dry cough; fever; symptoms of
the underlying disease
•
Inspection and palpation = asymmetric expansion and unilateral lagging on the affected side;
↓ tactile fremitus due to fluid in pleural space
•
Auscultation = faint/absent breath sounds over area of effusion, pleural friction rub
•
Percussion = dullness over the area of effusion
Diagnosis
•
CXR = standard initial imaging for detecting effusion; lat. decubitus view – allows for detection
of fluid collections as small as 5 ml
•
US = quick bedside assessment and for thoracentesis planning
•
CT = gold standard but use is limited due to radiation and contrast exposure
•
Diagnostic thoracentesis = to definitively establish the underlying etiology
Treatment
•
Stabilise patients w/respiratory distress = provide supplemental oxygen; consider urgent
therapeutic thoracentesis for certain patients (signs of ↑ work of breathing, RF, or
hemodynamic compromise secondary to the effusion)
•
Identify and treat the underlying condition
•
Therapeutic thoracentesis = removal of fluid. Indicated for large effusion w/SOB and/or
cardiac decompensation and complicated parapneumonic effusions
•
Indwelling pleural catheter can be used for patients w/rapidly accumulating pleural effusions. It
allows recurrent fluid removal w/out repeated puncture
10) Pulmonary tuberculosis
Definition = an infectious disease caused by M.TB characterised by growth of nodules (tubercles) in
the tissues, especially the lungs
M. tuberculosis
•
Obligate aerobes that thrive in an O2 rich environment – explains their tendency to cause
disease in the upper lobe/upper parts of the lower lobe of the lung, where the ventilation and
O2 content are greatest
•
Intracellular pathogens, usually infecting the macs, which explains the T-cell type of immunity
and the ↑ n.o of lymphocytes in the infected patients.
•
Acid-fast bacteria, which is used for diagnosis w/Ziehl-Neelsen acid-fast staining procedure
•
It is an airborne infection spread by droplet nuclei that are harboured in the respiratory
secretions of people w/active TB. Coughing, sneezing, and talking all create respiratory
droplets.
Predisposition factors
•
Immunosuppression (TB is considered to be the most common cause of mortality in patients
w/HIV globally)
•
Contact w/sick person
•
Malnutrition and overcrowding
•
Alcoholism, smoking, drug abuse
•
Diabetes mellitus
•
Pre-existing damage to the lungs (e.g. silicosis, COPD)
•
Treatment w/TNF-α inhibitors
Pathogenesis
The pathogenesis of TB in a previously unexposed immunocompetent person is centred on the
development of a cell-mediated immune response that confers resistance to the organism and
development of tissue HS to the tubercular antigens. The destructive features of the disease such as
caseating necrosis and cavitation, result from the HS immune response rather than the destructive
capabilities of the tubercle bacillus.
•
M.TB enters the lungs through respiratory droplets and reaches the alveoli
Surface adhesion of M.TB to alveolar macs → inhibition of mycobacterial growth
and/or killing → involvement of additional immune cells (T cells) and deployment of
local immune response
•
Failure of the host to deal w/the infection leads
the bacteria to multiply and destroy alveolar
macs
•
Macs produce cytokines and chemokines, and
thus involve more cells to help contain the
bacteria.
•
The cell-mediated immune response results in
the development of a grey-white,
circumscribed granulomatous lesion (Ghon
focus) that contains the tubercle bacilli, modified macs, and other immune cells (epitheloid
cells, T and B cells)
•
When the n.o of organisms is high, the HS rxn produces significant tissue necrosis, causing
the central portion of the Ghon focus to undergo soft, caseous (cheese-like) necrosis.
•
Tubercle bacilli drain along lymph channels to the tracheobronchial lymph nodes of the
affected lung, and there evoke the formation of caseous granulomas
•
The spread of the TB process from primary site can be done in several ways = neighbouring
spread, bronchogenic, lymphogenic, and haematogenous
•
The combo of primary lung lesion (Ghon focus) + lymph node granulomas (pulmonary
lymphadenopathy) = Ghon complex
•
The Ghon complex undergoes progressive fibrosis, often followed by radiologically detectable
calcification (Ranke complex), and despite seeding of other organs, no lesions develop.
•
The Ranke complex is an evolution of the Ghon complex – it results from further healing and
calcification of the lesion, making it visible on CXR
•
A Ghons complex retains viable bacteria, making them sources of long-term infection, which
may reactivate and trigger secondary TB later in life
•
The primary tuberculous complex has a classical triad = primary affect w/perifocal
inflammation, lymphangitis, and regional lymphadenitis
•
Phases of primary tuberculous complex = infiltration, destruction, and dissemination
•
When treatment has started, reversal phases occur = draw back, compaction, and
calcification
•
TB of intrathoracic lymph nodes (bronchadenitis) is a major clinical form and major source for
TB dissemination. Can have infiltrative and tumorous forms
Infiltrative = caseous necrosis in the lymph node is < pronounced while the perifocal
inflammation predominates (non-specific)
Tumorous = caseous necrosis is > pronounced and there is < expressed perifocal
inflammation. This form is a sign for a greater duration of the specific process in the
lymph nodes of the lungs
Classification
•
Primary TB (primary infection) is divided into latent TB and active primary TB
•
Latent TB = primary infection w/out any pathological findings or radiological imaging; however,
screening tests indicating previous infection w/M.TB are +ve
•
Active primary TB infection (only 1-5% of cases) = primary infection w/radiologicalpathological findings of TB
•
Secondary infection is a reactivation TB = following a latent primary TB infection; 80% begin in
the lungs; endogenous reactivation (immunodeficiency) is very common whereas exogenous
reinfection is rare
Clinical manifestations
Primary TB
•
A form of the disease that develops in previously unexposed and ∴ unsensitised people
•
It manifests in childhood and typical features are:
Marked perifocal inflammation
Involvement of the draining lymph nodes
Instability to immunity
Evident intoxication syndrome
Mainly lymph-hematogenous dissemination of TB
•
Around 95% of people w/primary TB go on to develop latent infection (no signs of active TB
and don’t feel ill) in which T cells and macs surround the organism in granulomas that limit
their spread. People w/latent TB don’t have the active disease and can’t transmit the organism
to others
•
In ~ 5% of newly infected people, the immune response is inadequate → develop progressive
primary TB w/continued destruction of lung tissue and spread to multiple sites w/in the lung
•
General symptoms = fever (subfebrile), chills,
fatigue, lack of appetite and weight loss, night
sweats, lymphadenopathy, significant nail
clubbing may occur. These symptoms
depend on the severity of the diseases and
its duration.
•
Pulmonary symptoms = dyspnoea,
productive cough (possibly hemoptysis)
lasting >3 weeks
•
Chest pain provoked by breathing and cough
in patients w/pleuritis
Miliary TB
•
A form of TB that is characterised by a wide dissemination into the body and by the tiny size
of the lesions (1-5 mm)
•
Its name comes from a distinctive pattern seen on a CXR of many tiny spots distributed
throughout the lung fields w/the appearance similar to millet seeds – thus the term “miliary” TB
•
It may also infect any n.o of organs including the lungs, liver, and spleen
•
You can get acute, subacute, or chronic miliary TB
Secondary TB
•
A form of TB occurring in adults and characterised by lesions near the apex of the upper lobe
of the lung that may cavitate or heal w/scarring.
•
It may result from reinfection w/the tubercle bacilli or from reactivation of a dormant old lesion
(endogenous infection)
•
The infiltrative-pneumonic form of primary TB dominates, w/little involvement of regional
lymph nodes. It mainly has bronchogenic pathway of dissemination
•
80% pulmonary TB; 20% extrapulmonary TB
•
The most common sites of extrapulmonary TB include the bones, pleura, lymphatic system,
and liver. TB may also affect the CNS, heart, urogenital and GI tracts and the skin.
Diagnosis
History
•
Intoxication syndrome
•
Cough for >3 weeks
•
Complaints from different organs
•
Contact w/TB patient; living conditions
•
BCG status
Physical examination
•
For pulmonary TB there is no characteristic finding
•
Observe intoxication syndrome, chronic low fever (subfebrile), cough, night sweats, ↓ appetite
and weight loss.
Lab tests
•
Blood = ↑ WBC w/lymphocytosis; slightly ↑ESR; often anemia w/iron deficiency.
•
Microbiology = smear of sputum/pleural fluid for acid fast staining procedure; culture of
sputum/pleural fluid. NAAT test. Mycobacterium culture
•
Immunology = Tuberculin skin test/Mantoux (TST/PPD) test = intradermal inoculation of 0.1
ml tuberculin on the frontal side of the forearm. Result after 72 h.
Diameter < 5 mm = -ve result = vaccinal strain has been eliminated and the patient
should be revaccinated
Diameter > 15 mm = +ve result. >10 mm is +ve result for immunocompromised and
children <4
•
One of the main disadvantages of Mantoux test is cross-sensitivity to BCG vaccine
•
An interferon gamma release assay (IGRA) blood test screens for exposure to TB by indirectly
measuring the body's immune response to Ag’s derived from these bacteria.
o The QuantiFERON-TB Gold test (QFT-TB Gold) is used to detect active and latent TB
by measuring IFNγ.
o T-spot TB test = measuring the T cells specific to M. tuberculosis Ag’s
Instrumental tests (radiology)
•
CXR = In active pulmonary TB, infiltrates or consolidations and/or cavities are often seen in
the upper lungs w/ or w/out mediastinal or hilar lymphadenopathy or pleural effusions
(tuberculous pleurisy). However, lesions may appear anywhere in the lungs.
•
TB of the tracheobronchial lymphatic nodes = enlarged mediastinum on both sides
•
Haematogenous disseminated TB (miliary TB) = multiple small round shadows spread in both
lungs. In later stages some of them can form caverns, others can heal w/calcification.
•
Tuberculoma = round shadow in the apex of the lung;
•
Cirrhosis = patchy and streaky shadows causing deformations in both lungs.
•
Often CT and bronchoscopy are required usually for differential diagnosis w/tumours.
•
CT can help in detection of active lesions, assess disease activity, differentiate between active
and latent disease, staging of disease, and monitoring response to treatment
HIV and TB coinfection
•
Fluorescent AFB smear microscopy, specialized culture mediums
•
Severe disease + CD4 count < 100 cells/mm3: lateral flow urine lipoarabinomannan assay
Treatment
First line drugs
•
Rifampicin, Isoniazid, Pyrazinamide, and Ethambutol –mnemonic RIPE
•
Mnemonic RHZE can also be used. Isoniazid is H and pyrazinamide is Z
•
The WHO also includes streptomycin in the first line drugs
Standard antituberculosis therapy
•
Intensive phase: 2 months of rifampin 10mg/kg/day PLUS isoniazid 5mg/kg/day, pyrazinamide
25mg/kg/day, and ethambutol 25mg/kg/day
•
Continuation phase: 4 months of rifampin PLUS isoniazid
•
Adjuvant treatment: Pyridoxine to prevent vitamin B6 deficiency resulting from isoniazid
(promotes pyridoxine excretion) for all individuals at risk of neuropathy
•
For latent TB, the standard treatment is 6-9 months of daily isoniazid alone or 3 months of
weekly (12 total doses) of isoniazid/rifapentine combo.
Second line drugs
They are used to treat disease that is resistant to 1st line therapy – i.e. for extensively drug resistant
TB (XDR-TB) or multidrug resistant TB (MDR-TB). A drug may be classed as 2nd instead of 1st
because = may be < effective than 1st line, may have toxic side effects, or it may be effective but
unavailable in many developing countries
•
ORAL: Fluoroquinolones (levofloxacin), linezolid, cycloserine
•
IV: Aminoglycosides (amikacin, kanamycin), carbapenem
•
Polypeptides – capreomycin, viomycin, enviomycin
•
Thioamides
•
Cycloserine and terizidone
Third line drugs
These are drugs that may be useful but have doubtful/unproven efficacy = rifabutin, macrolides,
linezolid, arginine, vitamin D.
Surgery: Elective partial lung surgery can be beneficial.
Prevention of TB involves administration of the BCG vaccine
11) Pulmonary embolism (PE)
Definition = obstruction of ≥ 1 pulmonary aa. by a thrombus; other possible causes for lung embolism
may be amniotic fluid, fat, or air.
Etiology
•
Deep vein thrombosis (DVT) = most common cause
•
Fat embolism
•
Air embolism
•
Amniotic fluid embolism
•
Others = bacterial embolism, pulmonary tumour embolism, pulmonary cement embolism
Pathophysiology
Mechanism = thrombus formation (Virchow’s triad – see below) → DVT in the legs or pelvis (most
commonly iliac v.) → embolisation to pulmonary aa. via IVC → partial or complete obstruction of
pulmonary aa.
The development of thrombosis is classically due to a group of causes named Virchow’s triad:
•
Alterations in blood flow = immobilisation (after surgery, long-haul flight), injury, pregnancy,
obesity, cancer (last 3 are also procoagulants)
•
Endothelial injury = catheterisations causing direct injury
•
Factors affecting the properties of the blood (procoagulant state) = oestrogen containing
hormonal contraception; genetic thrombophilia; acquired thrombophilia; cancer
Pathophysiologic response of the lung to arterial obstruction:
•
Infarction and inflammation of the lungs and pleura = causes pleuritic chest pain and
hemoptysis; leads to surfactant dysfunction → atelectasis → ↓ PaO2; triggers respiratory drive
→ hyperventilation and tachypnoea → respiratory alkalosis w/hypocapnia
•
Impaired gas exchange = mechanical vessel obstruction → V/Q mismatch → arterial
hypoxemia and ↑ alveolar-arterial (A-a) gradient
•
Cardiac compromise = ↑ pulmonary a. pressure due to blockage → R ventricular pressure
overload → forward failure w/↓ CO → hypotension and tachycardia
•
Pulmonary VC and bronchospasm
Clinical manifestations
•
Sudden onset of symptoms, often triggered by specific event (e.g. sudden physical
strain/exercise)
•
Dyspnoea and tachypnoea (>50% of cases); sudden pleuritic chest pain, worse w/inspiration
(~50% of cases); tachycardia (~25% of cases), hypotension
•
Cough and hemoptysis
•
Jugular venous distension and Kussmaul sign (in the event of a massive PE)
•
Low-grade fever
•
Possibly ↓ breath sounds, dullness on percussion, split 2nd heart sound audible in some cases
•
Features of DVT = unilaterally painful leg swelling
•
Features of massive PE = syncope and obstructive shock w/circulatory collapse
Diagnosis
•
Most important = ↑ level of D-dimer (fibrin monomer produced during the transformation of
fibrinogen into fibrin), which proves that there is active formation of fibrin thrombus
somewhere in the circulation but not obligatory in the lungs ∴ high sensitivity but low
specificity (+ve results in all forms of fibrinolysis)
•
Spirometry = restrictive type respiratory failure
•
ABG = hypoxemia w/hypocapnia (because of the tachypnoea)
•
CBC = mild leukocytosis may be present; troponin may be ↑; BNP may be ↑
•
ECG = tachycardia, deep Q in lead III and deep S in lead I, diffuse repolarisation changes (-ve
ST and T waves); possible overloading of the R ventricle, R axis deviation and RBBB
•
Chest X-ray = in the acute stage there might be seen ↓ or absent vascularisation in one or
both lungs in the area distally from the blockage; when some of the main branches are
affected the actual place of the blockage might be seen on the X-ray. Usually used to rule out
other causes
•
CT pulmonary angiography (high sensitivity and specificity), MRI, and V/Q scintigraphy (V/Q
scan) = shows zone/(s) w/↓ perfusion
•
Echocardiography = ↑ pressure in the pulmonary a.; often dilated R ventricle and relative
tricuspid insufficiency
•
Abdominal ultrasound = would detect dilated vena cava and hepatic vv. and often enlarged
liver
Treatment
Tumour type
Location
Characteristics
Histology
Non-small cell lung cancer (NSCLC) (85% of all cancers)
Lung adenocarcinoma
Peripheral
•
Most common type
•
Glandular tumour
•
> common in F and nonsmokers
•
Mucin-producing cells
•
Lepidic
•
Associated w/mutations in
adenocarcinoma =
growth along alveolar
walls (alveolar
thickening)
EGFR, ALK, and KRAS
genes
•
Common findings =
hypertrophic
osteoarthropathy (digital
clubbing)
•
Better prognosis than other
types
Lung squamous cell
carcinoma (SCC)
Central
•
Strong association
•
w/smoking
Solid, epithelial
tumour
•
Cavitary lesions arising
from a hilar bronchus
•
Intercellular bridges
(desmosomes)
•
Parathyroid hormone
•
Keratin pearls
protein → hypercalcemia
Large cell carcinoma
Peripheral
•
Strong association
w/smoking
•
Highly
undifferentiated
•
Poor response to chemo
•
Pleomorphic giant
•
Early metastases
•
Poor prognosis
cells
Lung neuroendocrine tumours
Small cell lung cancer
(SCLC)
Central
•
•
Strong association
w/smoking (extremely rare in
non-smokers)
•
Neuroendocrine
Kulchitsky cells
•
Rapid growth pattern
Associated w/several
•
Expressed tumour
markers =
chromographin A,
synaptophysin,
neuron-specific
enolase
paraneoplastic syndromes
•
Undifferentiated and very
aggressive w/early
metastases
•
Associated mutations = Lmyc oncogene
Large cell
neuroendocrine
carcinoma
Peripheral
Bronchial carcinoid
tumour
Central or
peripheral
•
Generally, high grade
tumours
•
Poor prognosis
•
Good prognosis w/an
indolent course
•
Metastases are rare
•
Possible carcinoid syndrome
(e.g. flushing, diarrhoea)
•
Mass effect of tumour (e.g.
wheezing)
•
Stabilise the patient and provide supportive care
•
Assess bleeding risk
•
Consider empiric parenteral anticoagulation while awaiting a definitive diagnosis
•
Risk stratify the patient based on prognostic models
•
Initiate therapy based on risk stratification and bleeding risk = thrombolytic therapy or
embolectomy for massive PE; anticoagulation (LMWH or DOACs) or IVC filter for sub-massive
and non-massive PE
12) Diffuse parenchymal pulmonary diseases (DPLD) (AKA interstitial
lung disease – ILD)
Definition = a heterogeneous group of disorders marked by inflammatory changes in the alveoli.
Etiology
•
Occupational, environmental, and iatrogenic causes = pneumoconioses (asbestosis, silicosis);
radiation pneumonitis
•
Drugs = chemotherapeutic agents (bleomycin, busulfan, MTX); other agents (amiodarone,
nitrofurantoin, phenytoin)
•
Secondary to underlying disease
Granulomatous ILD = sarcoidosis (non-caseating granulomas in multiple organs,
including the lung), granulomatosis w/polyangiitis, eosinophilic granulomatosis
w/polyangiitis
HS rxns = HS pneumonitis, eosinophilic pneumonia
CT disorders = RA, scleroderma, lupus, mixed CT disease
Infectious disease = TB, legionellosis
Alveolar filling diseases = Goodpasture syndrome, idiopathic pulmonary
hemosiderosis
Bronchoalveolar carcinoma
•
Idiopathic ILDs = idiopathic pulmonary fibrosis (IPF) (most common); acute interstitial
pneumonia, cryptogenic organising pneumonia.
Pathophysiology = repeated cycles of tissue injury in the lung parenchyma w/aberrant wound healing
→ collagenous fibrosis → remodelling of the pulmonary interstitium
Clinical manifestations
•
Main symptoms = exertional dyspnoea that progresses to dyspnoea at rest; persistent nonproductive cough; fatigue; bibasilar, inspiratory crackles/rales on auscultation
•
Later stages of the disease = digital clubbing due to hypoxia; loud inspiratory squeaks
Diagnosis
Due to the wide variety of subtypes and symptoms, there is no generally recommended diagnostic
algorithm. Physical exams, serology, pulmonary function tests, and imaging is performed almost
always, while lavage or biopsy depend on the individual case
•
Pulmonary function tests = restrictive lung disease (e.g. low lung volumes, high/normal
FEV1/FVC ratio); ↓ diffusing capacity for carbon monoxide (DLCO) (highly sensitive
parameter)
•
Labs = ABGs show ↑ alveolar-arterial PO2 gradient and ↓ PO2; screen for rheumatic and
autoimmune diseases
•
CXR = normal in ~10%; ↑ in reticular opacities (sign of fibrosis); ground-glass opacities
•
CT/high resolution CT = honeycombing (multiple cystic lesions w/in the lung parenchyma due
to fibrosis – indicates end-stage disease); traction bronchiectasis; irregular thickening of the
interlobular septa
•
Biopsy = indicated for atypical/rapidly progressive symptoms
•
Bronchoalveolar lavage = may be indicated for acute and rapidly progressive symptoms,
sarcoidosis, HS pneumonitis, or IPF.
Treatment
•
In secondary disease, the 1st step is to limit exposure to toxic substance, cease therapy
w/causative drug, or treat the underlying disease
•
Anti-B if bacterial interstitial pneumonia is suspected
•
Corticosteroids and immune modulators
•
Pirfenidone and nintedanib are commonly used for ILD
•
O2 for symptomatic or end-stage ILD
•
Lung transplantation in end-stage ILD
•
The majority of patients w/IPF (>70%) don’t respond to therapy and experience progressive
respiratory failure
II.Cardiology
13) Diseases of mitral valve: Mitral stenosis
Definition = narrowing of the opening of the mitral valve (normally 3-6 cm2). Clinically significant
stenosis when the opening is narrower than 1.5 cm2.
Etiology = Rheumatic fever (most common); Autoimmune diseases (RA, SLE); Congenital defects
Pathophysiology
•
Mitral valve stenosis is characterised by fibrous replacement of valvular tissue, along
w/stiffness and fusion of the valve apparatus
•
Mitral valve stenosis → obstruction of blood flow into the L ventricle (LV) → limited diastolic
filling of LV (↓ LV EDV) → ↓ stroke volume → ↓ CO (forward HF)
•
Mitral valve stenosis → ↑ in L atrial (LA) pressure (overtime there is dilation of LA) → backup
of blood into lungs → ↑ pulmonary capillary pressure → cardiogenic pulmonary oedema →
pulmonary HT → backward HF and R ventricular hypertrophy (as it becomes difficult for R
ventricle to pump blood to lungs)
•
Dilation of LA also causes muscle wall to stretch → pacemaker cells become > irritable →
atrial fibrillation (A-Fib) → stopping of blood flow → thrombus formation
•
I stage = hypertrophy, followed by dilatation of L atrium; peripheral hypoperfusion; and ↑
pressure in pulmonary vv. and lung congestion
•
II stage = ↑ pressure in pulmonary a., causing hypertrophy and dilatation of the R ventricle
w/relative tricuspid valve insufficiency, followed by dilatation of the R atrium and congestion in
the peripheral circulation
Clinical manifestations
•
Initially asymptomatic (onset ~10 years after acute rheumatic carditis)
•
Dyspnoea (incl. paroxysmal nocturnal dyspnoea) and orthopnoea, especially when supine
•
Haemoptysis
•
Hoarseness (compression of the recurrent laryngeal n. by the enlarged L atrium)
•
Dysphagia (compression of the oesophagus by the enlarged L atrium)
•
Mitral facies (mauve discolouration of the cheeks due to low CO and systemic VC)
•
A-Fib and embolic complications (e.g. focal neuro deficits, cyanotic extremities)
•
Later stages = signs and symptoms of R HF
Diagnosis
Auscultation
•
Diastolic murmur typically heard best at the 5th ICS at the mid-clavicular line (the apex of the
heart); heard loudest when patient is lying on their side
•
Loud S1 (1st heart sound)
•
ECG
•
Opening snap of the mitral valve high freq sound after S2 early to middiastolic sound
P mitrale = an ECG sign of L atrial enlargement; characterised by biphasic P wave and/or
prolongation of the P >0.1 s (wide P wave)
•
A-Fib – sinus tachy w/ irregular rhythm
•
Signs of R ventricular hypertrophy (Sokolow-Lyon index) – Right axis deviation
CXR
•
PA image = LA enlargement w/prominent L auricle (L atrial appendage) → straightening of the
L cardiac border; signs of pulmonary congestion
•
Lat. image = dorsal displacement of the oesophagus (visible in barium swallow test); signs of
R ventricular hypertrophy
Echocardiography (most important method for detecting and assessing valvular
abnormalities). TTE
•
Assess mitral valve structure, function, and stenosis severity = leaflet thickening and rigidity,
calcification, sub valvular thickening, and ↓ mitral valve area (≤1.5 cm2 is considered to be
severe)
• Assess for L atrial thrombus and concomitant mitral regurgitations
Coronary angiography = may be conducted prior to surgery to assess the risk of associated CAD
Lab tests = ↑BNP/ NT-proBNP, CBC- Leukocytosis, BMP – renal impairment, LFT’s – congestive
hepatopathy, ↑CRP – inflammation in RD
Additional tests = TEE, Stress testing, Cardiac catheterization
Treatment
•
Conservative =
o
o
o
o
•
Serial TTE exams for early monitoring and intervening at right time
Optimized medical therapy – Treat Cardiac RF’s – DB, HL, HT, treat A.fib
treatment of Acute HF (diuretics only!); BB/CCB to ↓ HR and CO (!!Careful of
HypoTN); endocarditis prophylaxis in high risk cases (e.g. prosthetic valve). Nitrates –
P.Conges, For Rheumatic HD – anti-B prophylaxis
Anticoagulation – warfarin (target INR 2.5) for A.fib, intracardiac thrombus, prosthetic
valves
Interventional (if MS severe and symptomatic) = 1st line is percutaneous mitral valve balloon
commissurotomy (PMBC) if there are no calcifications, no L atrial thrombus, and no/mild mitral
regurgitation
•
Surgery: open commissurotomy and surgical valve replacement (mechanical or biological
prosthetic valve)
Complications = A-Fib (thromboembolism), congestive HF, progressive congestion of the lungs (→
pulmonary oedema, pulmonary HT)
14) Diseases of mitral valve: Mitral regurgitation (AKA mitral
insufficiency)
Definition = leakage (regurgitation) of blood from the LV into the LA due to incomplete closure of the
mitral valve during systole.
Etiology
•
Primary MR (organic) = MR caused by direct involvement of the valve leaflets or chordae
tendineae
Degenerative mitral valve disease (mitral valve prolapse, mitral annular calcification,
ruptured chordae tendineae)
Rheumatic fever
Infective endocarditis
Ischemic MR (e.g. papillary muscle rupture following acute MI)
•
Secondary MR (functional) = caused by changes of the LV that leads to valvular
incompetence – CAD/prior MI → papillary muscle involvement; Dilated cardiomyopathy and
LHF
•
Acute MR = acute dysfunction of the mitral valve leads to volume overload and symptoms of
acute HF
•
Chronic MR = to preserve CO, valve dysfunction is initially compensated for by cardiac
remodelling. Over time, remodelling affects LV ejection fraction (EF), leading to HF
Pathophysiology
•
Acute MR = ↑ LV EDV → rapid ↑ in L atrial and pulmonary pressure → pulmonary venous
congestion → pulmonary oedema
•
Chronic (compensated) MR = progressive dilation of the LV (via eccentric hypertrophy) → ↑
volume capacity of the LV(preload and afterload return to normal) → ↑ EDV → maintains ↑ SV
(normal EF)
•
Chronic (decompensated) MR = progressive LV enlargement and myocardial dysfunction → ↓
SV → ↑ ESV and EDV → ↑ LV and LA pressure → pulmonary congestion, possible acute
pulmonary oedema, pulmonary HT, and R heart strain
Clinical manifestations
Acute MR
•
Dyspnoea,
•
Symptoms of LHF (Dyspnoea, Orthopnoea, Pulmonary oedema, Paroxysmal nocturnal
dyspnoea, Cardiac asthma),
•
Signs and symptoms of pulmonary oedema - (e.g., bibasilar, fine, late inspiratory crackles),
•
Cardiogenic shock (poor peripheral perfusion, tachycardia, tachypnoea, and hypotension),
•
Palpitations.
•
Auscultation = soft, decrescendo murmur; no murmur in severe regurgitation w/LV systolic
dysfunction or hypotension; potentially S3 heart sound
Chronic MR
•
Individuals w/chronic compensated MR may be asymptomatic. Over time there may be
decompensation and patient can develop congestive HF
•
Symptoms = Dyspnoea (including exertional dyspnoea), Dry cough; Fatigue; Palpitations;
symptoms of LHF (and potentially RHF)
•
Auscultation =
o Lateral displacement of the apical impulse – LV dilatation,
o Quiet S1 – because of inability of mitral valve to shut;
o S3 may be heard in advanced stages (from diastolic ventricular volume overlaod) and
S4 may be heard in secondary MR;
o Holosystolic murmur (high-pitched, blowing) – radiates to the L axilla and heard best
over the apex
Diagnosis
AHA staging for MR
Stage
Extent of MR
A
At risk of MR (minimal regurgitation)
B
Progressive MR (moderate regurgitation)
C1
Asymptomatic severe MR (LVEF > 60%)
C2
Asymptomatic severe MR (LVEF ≤ 60%)
D
Severe symptomatic MR
Labs =
•
Troponin (may be ↑ and indicates myocardial ischemia);
•
BNP (normal in acute, normal or ↑ in chronic);
•
Blood culture in suspected infective endocarditis
Echocardiography (TTE)
•
Indications = to assess valve apparatus, size, and function of the LV and LA, and grade the
severity
•
Transthoracic echocardiography is modality of choice for initial assessment of all patients
w/suspected valve abnormality
•
Transoesophageal echocardiography is indicated prior to surgery
ECG
•
Acute = findings are non-specific – Sinus rhythm; A-Fib; Sinus tachycardia w/non-specific ST
and T wave abnormalities (due to volume overload); Signs of acute ischemia in ischemic MR
•
Chronic = ECG changes usually reflect cardiac remodelling – LV hypertrophy (50% of
patients); P-Mitrale; A-Fib; signs of R heart strain w/ P-pulmonale in later stages
CXR
•
Indications = assess for pulmonary oedema and rule out other causes of SOB
•
Decompensated MR and acute MR = signs of pulmonary congestion
•
Acute MR = normal-sized cardiac silhouette
•
Chronic MR = changes related to cardiac remodelling and associated HF may be visible – LV
enlargement (laterally displaced L cardiac border), LA enlargement (straightening of the L
cardiac border and double density sign)
Additional tests
•
Cardiac MRI (CMR): if both TTE and TEE findings are inconclusive, and for suspected
cardiomyopathy or ischemic MR
•
Stress echo: in ischemic MR and to help assess the need for surgery
•
CT angiography: in suspected ischemic cardiomyopathy
•
Coronary angiography: in suspected ischemic MR, prior to surgical intervention
Treatment
•
Acute MR = all patients w/acute primary MR should undergo urgent surgical repair
(preferable) or valve replacement (in severe destruction of MV). If secondary MR is
suspected, identify and treat the underlying cause (e.g. revascularisation therapy for ischemic
MR). while awaiting surgery.
o HF symptoms should be managed w/drugs (diuretics (furosemide), vasodilators
o
o
o
(nitroprusside, nitrates), anti-HT drugs (BB, ACE-I, ARB’s),
Inotropes -Dobutamine (Hypotension)
A-fib – consider cardiac resynchronisation therapy
Bridging therapy for those who are unstable or symptoms continue to deteriorate –
Intra-aortic balloon pump, then consider LVAD, ECMO.
•
Chronic MR = Management is guided by the symptoms and extent of HF and the cause of
MR. medical therapy should be initiated in all patients to optimise cardiac function, but surgery
is the definitive treatment option
o
Surgery – Transcatheter mitral repair
Indications – LVEF 30-60%, (<30% LVEF surgery not recommended)
Complications = HF, pulmonary oedema, cardiogenic shock, A-Fib, endocarditis
15) Diseases of aortic valve: Aortic stenosis
Definition = narrowing of the opening of the aortic valve → ↑ resistance to ejection of blood from LV
into the aorta. Normal = 3 cm2, clinically significant < 1.5 cm2
Etiology
•
Aortic valve sclerosis = calcification and fibrosis of aortic valve leaflets (AKA age-related
progressive calcification). Mean age = 65-70 years
•
Bicuspid aortic valve = fusion of 2 of the 3 aortic-valve leaflets in utero (congenital defect) –
results in a 2 leaflet valve (instead of the normal 3 leaflets). It is the most common heart valve
malformation and predisposes it to dystrophic calcification and degeneration
•
Rheumatic fever
Pathophysiology
•
Narrowed opening of the aortic valve during systole → obstruction of blood flow from LV → ↑
LV pressure → LV concentric hypertrophy – walls of LV are equally thickened; sarcomeres
are added in parallel to existing ones. This leads to ↑ LV O2 demand, impaired ventricular
filling during diastole → LHF, and ↓ coronary flow reserve
•
Initially, CO can be maintained
•
Later, the ↓ distensibility of the LV reduces CO and may then cause backflow into the
pulmonary vv. and capillaries → higher afterload (pulmonic pressure) on the R heart → RHF
•
If the valve doesn’t open properly, as the LV contracts → high pressure created until valve
eventually snaps open = ‘ejection click’
•
I stage = L ventricle hypertrophy, peripheral hypoperfusion
•
II stage = dilatation of the L ventricle, followed by relative mitral insufficiency and lung
congestion
•
III stage = HT in pulmonary a., followed by hypertrophy and dilatation of the R ventricle
w/relative tricuspid insufficiency
Clinical manifestations
•
May remain asymptomatic for years, particularly w/mild/moderate stenosis.
•
Major symptoms = syncope (and dizziness), angina pectoris, and dyspnoea (typically
exertional) – MNEMONIC for main symptoms = SAD
•
Physical examination = small bp amplitude, ↓ pulse pressure, weak and delayed distal pulse
(pulsus parvus et tardus), palpable systolic thrill over the bifurcation of the carotids and
aorta
•
Auscultation = harsh crescendo-decrescendo murmur best heard at 2nd right ic space, late
systolic ejection murmur that radiates bilaterally to the carotids; soft S2 (softer closing of the
aortic valve due to reduced mobility); S4 best heard at the apex; early systolic ejection click
from the abrupt stop of the valve leaflets upon opening
Diagnosis
Echocardiography (gold standard) = calcification and narrowing of aortic valve; ↑ mean aortic
pressure gradient and transvalvular velocity; signs of cardiac remodelling (concentric hypertrophy)
ECG = signs of LV hypertrophy – Skolow-Lyon index (RV5 or RV6 + SV1 or SV2≥ 3.5 mV) + LV strain
pattern – ST depression and T wave inversion in V5/V6 leads; Non-specific ST segment and T wave
abnormalities
CXR = visible calcifications w/in aortic valve may indicate more severe disease; narrowing of the
retrocardiac space; signs of cardiac remodelling (enhanced cardiac silhouette) and associated HF (Xray signs of LV hypertrophy, pulmonary congestion, post-stenotic dilatation of the aorta)
Diagnostic hemodynamic cardiac catheterisation
•
Definitive diagnostic test to evaluate aortic valve area, CO, and mean aortic pressure gradient
•
Consider in patients w/inconclusive non-invasive testing or discrepancy between symptoms
and testing
•
In most cases, coronary angiography is also required
Treatment
•
Definitive management requires valve repair/replacement.
o Symptomatic and severe stenosis = Valve replacement
o Asymptomatic and mild/moderate stenosis = echocardiography monitoring + treating
co-morbidities
•
Types of valve replacement – Surgical AVR, Transcatheter AVR (TAVR), Percutaneous
Balloon Valvuloplasty in children
•
Medical management of comorbidities = all patients should be screened and treated for other
cardiac risk factors.
o Prophylaxis for those undergoing dental procedures and those who have rheumatic
heart disease.
16) Diseases of aortic valve: Aortic regurgitation (AR)
Definition = incomplete closure of the aortic valve during diastole that leads to reflux (regurgitation) of
blood from the aorta into the LV (backflow of blood)
Etiology
•
Acute AR = infective endocarditis, aortic dissection, chest trauma
•
Chronic AR:
Congenital bicuspid valve = most common cause in young adults and in developed
countries
Rheumatic heart disease = most common cause in developing countries
Distortion or dilation of the ascending aorta and aortic root = CT disorders (e.g. Marfan
syndrome, EDS), tertiary syphilis (syphilitic aortitis)
Pathophysiology
•
General = regurgitation of blood from aorta into LV → ↑ systolic and ↓ diastolic BP → ↑ pulse
pressure (difference between them) → water-hammer pulse (blood slams like a hammer
against walls of a. in each heart beat)
•
Acute AR = because LV cant sufficiently dilate in response to regurgitant blood, LV enddiastolic pressure ↑ rapidly → pressure transmits backwards into pulmonary circulation →
pulmonary oedema and SOB. If severe = ↓ CO → cardiogenic shock and myocardial ischemia
•
Chronic AR = initially, a compensatory ↑ in SV can maintain adequate CO despite
regurgitation (compensated HF). Over time, ↑ LV EDV → LV enlargement and eccentric
hypertrophy (sarcomeres added in series to existing ones) → LV dysfunction →
decompensated HF
Clinical manifestations
•
Acute AR = sudden, severe dyspnoea; pulmonary oedema; cardiac decompensation
secondary to HF; symptoms related to underlying disease (e.g. fever due to endocarditis,
chest pain due to aortic dissection)
•
Chronic AR = may be asymptomatic for up to decades; palpitations; symptoms of LHF
(exertional dyspnoea, angina, orthopnoea, fatigue, syncope); symptoms of ↑ pulse pressure
(e.g. head pounding, rhythmic nodding/bobbing of the head in synchrony w/heartbeats – de
Musset sign)
•
High pulse pressure (water-hammer pulse) = pulsing of carotid aa. w/rapid upstroke and
downstroke; visible capillary pulse (Quincke sign); nodding of the head w/each pulse
•
Displacement of the apex beat to 6th/7th ICS to the L of the midclavicular line, enlargement of
the area of relative dullness
•
Auscultation = S3 heart sound; high-pitched, blowing, decrescendo early diastolic murmur –
best heard at Erb point (AR due to valvular disease) or along the R sternal border (AR due to
aortic root disease), w/transversal propagation, best heard in sitting position
Diagnosis
Echocardiography (gold standard) = abnormal valve leaflets; regurgitant AR jet on Doppler flow
tracing; ↑ LV size and volume; dilated aorta; fluttering of ant. mitral valve leaflet
Optional screening tests include ECG (signs of LV hypertrophy) and CXR (prominent aortic root/arch,
enlarged cardiac silhouette)
Treatment
•
Conservative treatment (treatment of HF) for asymptomatic patients and those incompatible
w/surgery
•
Surgery = aortic valve replacement and long-term anti-coagulation therapy for mechanical
valve
17) Endocarditis
Definition = inflammation of the endocardium (inner layer of the heart), which affects mainly the
valves but also the interventricular septum, chordae tendinae, and the mural endocardium. Most often
valves in the L side of the heart are affected
Classification = Infective and Non-infective (Libman-Sacks endocarditis is a form of non-infective
associated w/SLE)
Etiology
•
Infective endocarditis (IE) = Acute - most commonly caused by staphylococci (S. aureus) and
Sub-acute - viridans streptococci (S. sanguinis, S. mitis, S. mutans). Less than 10 of cases
are caused by enterococci. Candida and A. fumigatus can be causes in immunocompromised
patients
•
Non-infective endocarditis = usually occurs during a Hypercoagulable state such as systemwide bacterial infection, or pregnancy; and can occur in Cancer patients, underlying Trauma,
Autoimmune conditions – SLE, RA, Anti-Phospholipid syndrome, Chronic infections – TB,
Pneumonia, Osteomyelitis
Risk factors for Infective endocarditis
•
Demographic - M sex; age >60 years
•
Cardiac conditions = previous IE; acquired valular disease – RHD, Aortic stenosis/prosthetic
valves; congenital heart defects (VSD, Bicuspid AV);
•
Non-cardiac (Bacteraemia) = Poot dental status/dental procedures; infected peripheral venous
catheters, surgery, non-sterile venous injections (IV drug users); bacterial infections of various
organs (UTIs), immunocompromised (HIV, Diabetes), Chronic haemodialysis
Pathophysiology
•
Damage to the endothelial lining of the valves – underlying sub endothelium collagen and
tissue exposed → platelets and fibrin adhere → sterile vegetation → localised
infection/contamination → bacteremia → bacterial colonisation of damaged valve areas →
formation of fibrin clots encasing the vegetation → valve destruction w/loss of function
•
Frequency of valve involvement = mitral > aortic > tricuspid > pulmonary
•
Consequences = bacterial thromboemboli from bacterial vegetation → vessel occlusion
w/infarctions; metastatic infections of other organs; formation of immune complexes and AB
against tissue Ag’s → glomerulonephritis; Osler nodes
Clinical manifestations
Non-specific/constitutional symptoms = fever and chills (90%); tachycardia; malaise, weakness,
night sweats, weight loss; dyspnoea; cough, pleuritic chest pain; arthralgias, myalgias
Cardiac manifestations
•
New heart murmur development or change to a pre-existing one
MR = holosystolic murmur, loudest at apex, radiates to L axilla
AR = early diastolic murmur, loudest at L sternal border
Tricuspid regurgitation = holosystolic murmur, loudest at L sternal border; seen in IV
drug users, concomitant HIV infection, immunocompromised, and patients w/central
venous catheter
•
Signs of progressive HF due to valve insufficiency (left sided IE)= dyspnoea,oedema
•
Signs of acute cardiac decompensation (pulmonary oedema)
•
Arrhythmias – sign of perivalvular abscess
Extracardiac manifestations
•
> common in L sided endocarditis (w/the exception of pulmonary emboli)
•
Mainly caused by bacterial microemboli and/or the precipitation of immune complexes
•
Petechiae; especially splinter haemorrhages (haemorrhages underneath fingernails)
•
Janeway lesions = small, nontender, erythematous macules on palms and soles
•
Osler nodes = painful nodules on pads of fingers and toes; caused by immune complex
deposition
•
Roth spots = round retinal haemorrhages w/pale centers
•
Signs of acute renal injury, including haematuria, anuria (due to renal a. occlusion or GN),
•
Splenomegaly and possible L upper quadrant pain (splenic a. occlusion)
•
Neurological manifestations (seizures, paresis) due to septic embolic stroke, hemorrhages,
meningitis, encephalitis or abscess
•
Arthritis
•
Pulmonary embolism (sign – dyspnoea) – caused by septic emboli from tricuspid valve
Classification
Diagnosis
Duke criteria for definitive vs possible diagnosis
Criteria
Findings
Major
Typical organisms from 2 separate blood cultures
Characteristic echocardiographic findings of IE
New valvular regurgitation
Minor
Predisposing condition (e.g., underlying heart abnormality, IV drug use)
Fever > 38°C (100.4F)
Vascular abnormalities (Arterial emboli, septic infarctions, Janeway lesions)
Immunologic phenomena (GN, Osler nodes, Roth spots, RF +ve)
Microbiology: positive blood cultures not fulfilling major criteria
Diagnostic category
Definite IE if any of the following are present:
≥ 2 major criteria
≥ 1 major criterion PLUS ≥ 3 minor criteria
≥ 5 minor criteria
≥ 1 pathological criterion
Possible IE if any of the following are present:
≥ 1 major criterion PLUS ≥ 1 minor criterion
≥ 3 minor criteria
Lab = CBC: Leukocytosis (left shift); ↑ CRP and ESR; ↓ RBC, Hb, and HCT (anaemia); +ve bacterial
cultures
Echocardiography (TTE/TEE) = Valvular vegetations; Abscess; New valvular regurgitation – w/
valve proplapse, perforation or destruction; Prosthetic valve dehiscence. Other high-risk findings
include valve aneurysm, fistula or pseudoaneurysm, and HF
Tissue sampling (post surgery) = histopathology of resected valves (gold standard); gram stain and
culture; molecular testing
ECG = tachycardia or tachyarrhythmia, often extrasystoles, and repolarisation changes
Abdominal US = if splenic abscess or infarction is suspected
Treatment =
•
Medical therapy anti-B
o Empirical
Consider in hemodynamically unstable or acute symptoms
o
o
•
Native valve: vancomycin + ceftriaxone/cefepime
Prosthetic valve endocarditis: Add gentamicin PLUS rifampin
Targeted
Duration: 2-6 wks
MSSA- beta-lactams (e.g., Nafcillin, Oxacillin)
MRSA: Vancomycin
Prosthetic valve endocarditis (≤ 1 year after placement): add gentamicin PLUS
rifampin to regimen.
Viridans group streptococci: Penicillin G, Ampicillin
Prophylaxis (1h before procedure)
No penicillin allergy: Amoxicillin OR Ampicillin
Penicillin allergy: a macrolide: Azithromycin/ Clindamycin
Surgical therapy: valve repair/replacement
o
Indications - Prosthetic valve endocarditis, Valve dysfunction, HF, New heart block
Noninfective endocarditis (nonbacterial thrombotic endocarditis) - Libman-Sacks endocarditis
•
Definition: Rare, noninfective form of endocarditis due to sterile platelet thrombus formation on
the heart valves (usually mitral and aortic valves).: a type of noninfective endocarditis with
verrucous vegetations in individuals with systemic lupus erythematosus or antiphospholipid
syndrome
•
Clinical features: Valves and cardiac function are rarely impaired, Compared to IE,
vegetations are easily dislodged and embolization is common, leading to hemorrhages under
the nails, skin, and retina, Most affected individuals are asymptomatic until embolization
occurs.
•
Diagnostics: Negative blood cultures, Echocardiography: valve vegetations, Biopsy (definitive
diagnosis),
•
Treatment: Anticoagulation with heparin, and underlying condition
Prosthetic valve thrombosis
•
Definition: Usually affects mechanic valves, Rare if anticoagulation is adequate
•
Etiology: insufficient anticoagulatory therapy after valve replacement
•
Clinical features: Signs of acute Left heart failure: dyspnea and cough, Right heart failure:
edema and jugular venous distention, Deterioration of general condition, cardiac arrhythmias,
cerebral emboli (stroke)
•
Diagnostics: transesophageal echocardiography
•
Treatment: Anticoagulation and fibrinolysis, Surgical valve replacement
18) Pericardial diseases- classification. Pericarditis. Cardiac
tamponade.
Pericardial effusion
Definition = an accumulation of fluid in the pericardial cavity between the parietal and visceral
pericardium (can be acute/chronic)
Etiology
Any process that leads to injury or inflammation of the pericardium and/or inhibits appropriate
lymphatic drainage of the fluid from the pericardial cavity leads to fluid accumulation.
•
Hemopericardium = cardiac wall rupture; chest trauma; aortic dissection; cardiac surgery
•
Serous or serosanguinous pericardial effusion = idiopathic; acute pericarditis; malignancy;
post-pericardiotomy surgery; uremia; autoimmune disorders (SLE, RA, sarcoidosis);
hypothyroidism
Clinical manifestations
Initially asymptomatic in most cases – small effusions may produce no symptoms or abnormal clinical
findings. Even a large effusion that develops slowly may cause few or no symptoms. However, a
sudden accumulation of even 200 ml may ↑ Intracardiac pressure to level that seriously limit the
venous return to the heart. Symptoms of cardiac compression also may occur w/relatively small
accumulations of fluid if the pericardium has become thickened by scar tissue or neoplastic
infiltrations.
•
SOB, especially when lying down (orthopnoea)
•
Retrosternal chest pain
•
Can cause compressive symptoms = hoarseness, nausea, dysphagia, hiccups
•
Apical impulse is difficult to locate or non-palpable
•
Ewart sign = dullness to percussion at the base of the L lung w/↑ vocal fremitus and bronchial
breathing due to compression of lung parenchyma by the pericardial effusion
Diagnosis
Echocardiography = Anechoic space between the pericardium and epicardium (volume can be
assessed by measuring the distance between the pericardial layers):
•
<10 mm = small effusion (~300 ml)
•
10-20 mm = moderate effusion (~500 ml)
•
>20 mm = large effusion (>700 ml)
Hemorrhagic or purulent effusions may be echogenic
ECG = normal in smaller effusions; low voltage, complexes and electrical alternans (alternation of the
QRS appearance between beats) in larger effusions
CXR = performed to exclude other causes of dyspnoea
•
PA view = normal in small effusions; enlarged cardiac silhouette and clear lungs may be seen
in moderate effusions; water bottle sign in large pericardial effusions
•
Lat. view = post. inf. bulge sign; pericardiac fat pad sign
Cardiac CT and MRI = can help localise and quantify the effusion, especially in a loculated effusion
Pericardiocentesis = fluid aspiration from the pericardial cavity. Used to analyse the pericardial fluid
but more importantly can also provide symptomatic relief in patients w/hemodynamic compromise.
•
Transudative effusion (clear) = due to non-inflammatory causes – HF, renal failure, nephrotic
syndrome, post-radiotherapy
•
Exudative effusion (cloudy, chylous) = inflammatory or malignant causes – viral infection,
inflammation, malignancy, autoimmune disease
•
Haemorrhagic effusion (bloody) = post-cardiac surgery, cardiac rupture, aortic dissection, TB,
malignancy
•
Purulent effusion (thick, yellowish-white, cloudy) = TB, bacterial infection
Treatment
•
Small effusions may resolve w/treatment of the underlying cause
•
In uncertain diagnosis or w/larger effusions that are causing symptoms = pericardial fluid
drainage (pericardiocentesis, pericardial window, pericardiotomy)
Pericarditis
Definition = inflammation of the pericardium (the fibrous sac that surrounds the heart)
Classification
•
Acute pericarditis = pericarditis that either occurs as an isolated process or w/concurrent
myocarditis (myopericarditis). Perimyocarditis is a condition that predominantly affects the
myocardium w/pericardial involvement
•
Transient constrictive pericarditis = constrictive pericarditis that lasts <3 months
•
Chronic pericarditis = pericarditis that lasts >3 months
Constrictive pericarditis is characterised by compromised cardiac function caused by a
thickened, rigid, and fibrous pericardium secondary to acute pericarditis.
Effusive-constrictive pericarditis = pericardial effusion occurs in addition to a thickened
pericardium, which can lead to tamponade
•
Pericarditis can also be classified as = serous, purulent, fibrinous, caseous, and haemorrhagic
Etiology
•
Idiopathic
•
Infectious = most commonly viral (e.g. coxsackie B virus); bacterial (staphylococci,
streptococci, M. TB); fungal; toxoplasmosis
•
MI = post-infarction fibrinous pericarditis – w/in 1-3 days as an immediate rxn; Dressler
syndrome = weeks to months following an acute MI
•
Post-operative (post-pericardiotomy syndrome) = blunt or sharp trauma to the pericardium
•
Uremia (e.g. due to acute or chronic renal failure)
•
Radiation
•
Neoplasm (e.g. Hodgkin lymphoma)
•
Autoimmune CT disorders (SLE, RA)
Pathophysiology
•
Local VD, ↑ capillary permeability, accumulation of WBC
•
Capillaries that supply the serous pericardium become permeable → plasma proteins
(including fibrinogen) exit the capillaries and enter the pericardial space → fibrosis – over
time, it becomes harder for heart to relax/expand → ↓ stroke volume and ↑ HR
Clinical manifestations
Acute pericarditis
•
Sharp, pleuritic, retro-sternal or L precordial chest pain – typically aggravated by coughing,
swallowing, or deep inspiration; improved on sitting and leaning forward; can radiate to the
neck and shoulders (most commonly to the L side)
•
Pericardial friction rub (high-pitched scratching on auscultation) = indicates friction between
the visceral and parietal pericardial tissue. Best heard over the L sternal border during
expiration while the patient is sitting up and leaning over
•
Pericardial effusion = faint heart sounds, Ewart sign
•
Low-grade intermittent fever, tachypnoea, dyspnoea, dry cough
Chronic pericarditis – constrictive pericarditis
•
Signs of fluid overload (i.e. backward failure) = jugular v. distension (↑ jugular venous
pressure); Kussmaul sign; hepatic v. congestion (hepatomegaly, painful liver capsule
distension, hepatojugular reflux); peripheral oedema
•
Symptoms of ↓ CO (i.e. forward failure) = fatigue, dyspnoea or exertion; tachycardia;
pericardial knock; pulsus paradoxus
Chronic pericarditis – effusive-constrictive pericarditis
•
Characterised by symptoms of chronic constrictive pericarditis, pericardial effusion, or a
mixture of both
•
Smaller or slow-growing effusions = patients may be asymptomatic
•
Large effusions or rapidly-growing effusions = symptoms of cardiac tamponade (Beck triad,
dullness at the L base of the lung)
Diagnosis
ECG
•
Stage 1 = Diffuse, non-specific (“saddle-shaped”) ST elevations in all leads except aVR and
V1 (ST depression; PR segment depression
•
Stage 2 = ST segment normalises in ~1 week
•
Stage 3 = inverted T waves
•
Stage 4 = ECG returns to normal baseline after weeks to months
Echocardiography
•
Pericardial effusion
•
↑ pericardial thickness (constrictive type)
•
Abnormal ventricular filling w/sudden halt during early diastole
CT and cardiac MRI
•
Pericardial thickening (>2 mm); calcifications; normal cardiac silhouette
•
May show pericardial effusion
CXR (PA and lat. views)
•
Acute = usually normal; may show enlarged cardiac silhouette
•
Chronic constrictive = normal/slightly ↑ size; pericardial calcifications; clear lung fields
•
Chronic effusive-constrictive = PA may show globular-shaped heart and sharp cardiophrenic
angles; lat. may show the “fat pad” sign
Pericardiocentesis w/pericardial fluid analysis = Indicated for large effusion, tamponade,
suspected malignant or purulent pericarditis
Cardiac catheterisation (for chronic pericarditis)
•
Similar pressures in the L and R atria and RV at the end of diastole (e.g. “equalisation of
pressures”)
•
Normal pulmonary a. systolic pressure <40 mmHg
•
Mean RA pressure >15 mmHg
•
Square root sign (AKA dip-and-plateau waveform) = sudden dip in the R and L ventricular
pressure in early diastole followed by a plateau during the last stage of diastole
•
In effusive-constrictive type, RA pressure remains persistently elevated after
pericardiocentesis
Labs = ↑ inflammatory markers may support diagnosis of pericarditis but aren’t part of diagnostic
criteria – leukocytosis; ↑ troponin, ESR, CRP, and CK
Treatment
•
Treatment of the underlying cause (if known)
•
Acute pericarditis is often self-limited; but NSAIDs (aspirin, ibuprofen) can alleviate symptoms
and prevent a recurrence. Consider anti-inflammatory therapy also for chronic pericarditis
(transient constrictive may respond)
•
Surgery = pericardiocentesis; pericardiectomy (complete removal of the pericardium) –
indicated for chronic pericarditis w/persistent symptoms of HF
Pericardial tamponade (AKA cardiac tamponade)
Definition = a pathophysiological process whereby ↑ intrapericardial pressure from a pericardial
effusion causes compression of the heart (especially the RV) (compression of the heart due to the
accumulation of fluid/pus/blood in the pericardial sac)
Etiology = pericardial effusion
Pathophysiology
Pericardial fluid collection (e.g. bloody or serous) → ↑ pressure in the pericardial cavity →
compression of the heart (especially of the RV due to its thinner wall) → interventricular septum shift
toward the LV chamber → ↓ ventricular diastolic filling → ↓ SV (and venous congestion) → ↓ CO and
equal end-diastolic pressures in all 4 chambers
Clinical manifestations
•
Beck triad = hypotension, muffled heart sounds, distended neck vv.
•
Tachycardia, pulsus paradoxus (pathologic ↓ of >10 mmHg in systolic BP during inspiration)
•
Pallor, cold sweats
•
LV failure
•
Symptoms of RHF
•
Obstructive shock, cardiac arrest (presenting as pulseless electrical activity)
Diagnosis
Echocardiography
•
Chamber collapse = early signs are RA collapse during systole and RV collapse during
diastole; later = LA collapse
•
Swinging motion of the heart due to fluid in the pericardial cavity = inspiration (↓ in LV filling)
and exhalation (↑ in LV filling and ↓ in RV filling)
•
Blood flow changes during inspiration = aortic and mitral valve ↓; pulmonary and tricuspid
valve ↑
ECG = sinus tachycardia; low voltage QRS complexes; electrical alternans; pulseless electrical
activity in cardiac arrest
Treatment = urgent decompression of the heart = urgent pericardiocentesis
19) Myocardial diseases: Myocarditis
Definition = infectious or immune inflammation of the myocardium (heart muscle)
Etiology
•
Infectious = viral – most common (coxsackie virus, EBV, HCV); bacterial infection (acute
rheumatic fever, C. diphtheriae, brucella, borrelia, M.TB, H. influenzae); fungal (candida,
aspergillus); or parasitic (T. cruzi → Chagas disease)
•
Non-infectious = CT disorders (SLE, sarcoidosis); vasculitis syndromes (e.g. Kawasaki
disease)
•
Toxic myocarditis = toxins (CO poisoning); meds (sulphonamides); chemo; alcohol; cocaine;
radiotherapy
Pathophysiology
•
Most forms of myocarditis involve the infiltration of heart tissues by one or two types of proinflammatory blood cells, lymphocytes and macs
•
Myocardial inflammation causes swelling → damage to cardiac myocytes ability to contract →
↓ contractility → ↓ CO. Tachycardia also occurs in order to ↑ the contractility of the heart
•
Severe myocarditis → fibrosis of myocardium → long-term problems w/heart contraction →
HF
Clinical manifestations
•
Often asymptomatic – may range from acute, fulminant cases to chronically active/persistent
myocarditis
•
Preceding (1-2 weeks) flulike symptoms (fever, arthralgia, myalgia, URT infections) = indicate
possible viral cause
•
Fatigue, weakness, dyspnoea; N/V
•
Cardiac arrhythmias = sinus tachycardia; ventricular extrasystoles w/palpitations or syncope,
heart block w/bradyarrhythmia
•
Chest pain (often described as “stabbing”) = indicates pericardial involvement
(perimyocarditis)
•
Acute decompensated congestive HF w/dilated cardiomyopathy → dyspnoea, oedema,
nocturia and liver congestion
•
Cardiogenic shock in fulminant cases
•
Auscultation = brief systolic murmurs; S3 and S4 gallops in HF; pericardial friction rub if
pericarditis is present
Diagnosis
Labs = ↑ cardiac enzymes (CK, CK-MB, troponin T), ↑BNP, ↑ESR, ↑CRP; Leukocytosis; virus
serology
ECG/24-hour Holter monitoring = although findings are very non-specific, myocarditis should be
suspected if the following findings are observed:
•
Sinus tachycardia
•
Arrhythmias: atrial/ ventricular ectopic beats, complex ventricular arrhythmia, atrial
tachycardia
•
Repolarisation abnormalities = non-specific T wave and ST segment changes; possible ST
segment elevations may mimic MI (rule out MI w/ loss of R wave w/Q)
•
Heart block = RBBB, complete heart block, AV block
•
Rule out MI = loss of R wave and pathological Q wave specific to MI
CXR and CT = cardiac enlargement, pulmonary congestion, pleural effusions
Echocardiography = findings often unremarkable – Ventricles dilated w/diffuse hypokinesia; ↓ EF
and impaired contractility; pericardial effusion
Myocardial biopsy = via cardiac catheterisation of the L heart and MRI-supported biopsy – possible
detection of viral DNA/RNA
Treatment
•
Supportive = rest, analgesics, cardiac monitoring, O2, management of fluid status
•
Causative treatment = anti-B for bacterial cause; antimycotics (fluconazole, amphotericin B)
for fungal infections
•
Treatment of complications = treatment of HF (diuretics, ACEIs, BB); treatment of cardiac
arrhythmias (amiodarone); heart transplantation
Complications = Dilated cardiomyopathy, HF/ sudden cardiac death, Arrythmias, AV block,
Intracardiac thrombus, Cardiac tamponade
Prognosis = is especially poor for infants and small children.
20) Myocardial diseases: Cardiomyopathies
Definition = chronic disease of the myocardium, which deteriorates its function and causes total HF
Classification
•
Dilated/congestive/primary (DCM) = condition in which the heart becomes enlarged and
can’t pump blood effectively. Most common type
•
Hypertrophic (HCM) = a genetic condition characterised by LV hypertrophy w/out an obvious
cause (no cardiac or causative systemic diseases) → heart is < able to pump blood
effectively. 2nd most common
•
Restrictive (RCM) = a form of cardiomyopathy in which the walls of the heart are rigid (but
not thickened). Thus, the heart is restricted from stretching and filling w/blood properly. Least
common
Etiology
DCM
•
Mostly idiopathic
•
Genetic predisposition (TTN gene
HCM
•
mutation)
•
IHD
•
Arterial HTN
•
Infectious: Coxsackie B; Chagas
disease; HIV, RHD
•
Systemic disorders: Sarcoidosis,
hemochromatosis, beri beri
(thiamine deficiency)
•
Toxins = cocaine, alcohol, meds
(doxorubicin)
•
Peripartum cardiomyopathy
•
Inherited (AD) mutation
of = myosin binding
protein C, β-Myosin
heavy chain
RCM
•
Mostly idiopathic
•
Systemic disorders =
amyloidosis, sarcoidosis,
hemochromatosis,
systemic sclerosis
Other conditions
associated w/LV
hypertrophy = chronic
HT, aortic stenosis,
amyloidosis, Fabry
disease, Friedreich’s
ataxia
•
Heart disease = Loffler
endocarditis, endocardial
fibroelastosis
•
Post-radiation fibrosis
•
Post-surgery (open heart)
HCM can be obstructive type (HOCM) (70% of cases) w/LV outflow tract obstruction that is dynamic;
or non-obstructive type (30%)
Pathophysiology
DCM
•
Causative factors ↓ contractility of the myocardium → compensatory mechanisms (FrankStarling law) are activated to maintain CO → ↑ EDV (preload) → myocardial remodelling →
eccentric hypertrophy and dilation of the ventricle → ↓ myocardial contractility → systolic
dysfunction and ↓ EF → HF
•
↓ LV contractility due to dilation leads to LHF and eventually RHF
HCM
•
Characterised by concentric hypertrophy of the LV; incl. interventricular septum → diastolic
dysfunction → ↓diastolic filling → ↓ systolic output volume → ↓ peripheral and myocardial
perfusion → cardiac arrhythmia and/or HF and ↑ risk of sudden cardiac death
RCM
•
Proliferation of CT → ↓ elasticity of myocardium → ↓ ventricular compliance (LV wall stiffness
↓ its ability to expand in volume in response to pressure) → ↓ diastolic filling → atrial
congestion → atrial enlargement and severe diastolic dysfunction → systemic venous
congestion
Clinical manifestations
DCM
•
General = gradual development of Congestive HF symptoms – exertional dyspnoea, ankle
oedema, ascites, angina pectoris
•
Physical examination = relative mitral/tricuspid valve regurgitation (systolic murmur); S3
gallop; LV impulse displacement; jugular venous distension; rales (both lung fields);
palpitations; diffuse abdominal and peripheral oedema
HCM
•
Symptoms worsen w/exercise, dehydration, and use of certain drugs (e.g. diuretics,
ACEIs/ARBs, digoxin)
•
Frequently asymptomatic (especially non-obstructive type)
•
Exertional dyspnoea
•
Angina pectoris – hypertrophic cardiac tissue has an ↑ O2 demand while LV outflow tract
obstruction limits blood flow to the coronary vessels
•
Dizziness, light-headedness, syncope
•
Palpitations, cardiac arrhythmias
•
Sudden cardiac death (particularly during/after intense physical activity)
•
Physical examination = systolic ejection murmur (crescendo-decrescendo); possible
holosystolic murmur from mitral regurgitation; sustained apex beat; S4 gallop; paradoxical
split of S2; pulsus bisferiens (LV outflow obstruction causes a sudden quick ↑ of the pulse
followed by a slower longer ↑ – biphasic pulse)
RCM
•
Most common = dyspnoea
•
Symptoms of RHF = jugular venous distension, peripheral oedema, ascites, hepatomegaly,
Kussmaul sign (JV distension upon inspiration)
•
Less common = possible S4
Diagnosis
DCM
•
Approach = investigate underlying cause, assess cardiac function, assess structural
remodelling
•
Labs = ↑ BNP in concomitant HF; troponin and CK-MB to rule out MI
•
Echocardiography = assess cardiac remodelling and function = atrial and/or ventricular
dilation, ↓ LVEF, wall movement abnormalities (e.g. inferolateral hypokinesis in muscular
dystrophy and acute myocarditis), systolic dysfunction
•
CXR = cardiomegaly (L-sided hypertrophy w/a balloon appearance), pulmonary oedema
(signs of LHF decompensation)
•
ECG (non-specific for DCM) = conduction disorders (AV block/LBBB), A-Fib, arrhythmias, ↓
QRS voltage (due to ↓amount contractile tissue), change cardiac axis
HCM
•
Following criteria needed for diagnosis = LV non-dilated hypertrophy AND absence of other
cardiac/systemic diseases that could explain hypertrophy
•
Echocardiography w/Doppler =
o
o
asymmetrically thickened LV wall (≥15 mm/ N=8mm), typically involving the septum;
outflow tract abnormalities; LA enlargement; diastolic dysfunction.
Specific to HOCM = asymmetrical septal thickening, dynamic LVOT obstruction by
mitral valve during systole, and LVOT pressure gradient ≥30 mmHg (N=12)
•
ECG = signs of LVH, deep Q waves, giant inverted T waves in precordial leads, LBBB, nonspecific ST and T changes
•
CXR = heart normal/enlarged; LA enlargement common in mitral regurgitation; possibly signs
of pulmonary congestion
•
Provocation tests (exercise testing) = obligatory if no obstruction is discernible at rest
•
Cardiac MRI = evaluation of ventricular morphology
RCM
•
Echocardiography = diastolic dysfunction, normal/↑ EF, atrial enlargement and dilation, wall
thickening is possible
•
ECG = low voltage, LBBB and other conduction disorders, non-specific abnormalities in S and
T waves
•
CXR = signs of pulmonary congestion
•
Cardiac catheterisation = high atrial pressure, abnormal ventricular pressure
•
Endo/myocardial biopsy = histology shows fibrosis
Treatment
DCM
•
Treat underlying disease = avoid cardiotoxic drugs/alcohol; treat infections (benznidazole for
Chagas disease) /endocrine disorders (BB for hyperthyroidism)
•
Treatment of HF = sodium restriction; ACEIs/ARBs, BB, diuretics, digoxin, Spironolactone
•
Anticoagulation = in the case of mechanical valves, intraventricular thrombus and/or A-Fib
•
Surgery = automated implantable cardioverter defibrillator (AICD) (if LVEF <35%); heart
transplantation (failure of medical therapy)
HCM
•
General = lifestyle changes (healthy body weight, avoid dehydration/excess alcohol/strenuous
exercise). Asymptomatic patients don’t require pharmacological or invasive treatment – only
regular checkups
•
Consider AICD for primary/secondary prevention of sudden cardiac death in high-risk patients
– known history of ventricular fibrillation, sustained ventricular tachycardia, or cardiac arrest
•
Meds = 1st line BB (propranolol, atenolol, or nadolol); 2nd line non-dihydropyridine CCBs
•
Surgery = septal reduction therapy, dual chamber pacemaker, heart transplant
RCM
•
Treatment is generally limited and often palliative – treat underlying disease and symptomatic
treatment
•
Symptomatic = maintain sinus rhythm (BB), ↑ ventricular filling time and ↓ sympathetic activity
(cardioselective CCBs), ↓ preload (ACEIs), diuretics for fluid overload
•
Anticoagulation to prevent embolism in patients w/history of A-Fib
•
Heart transplant (in patients w/refractory symptoms)
21) Acute heart failure (HF)
Definitions
•
Acute HF = rapid onset of new or worsening signs and symptoms of HF
•
Acute decompensated HF (ADHF) = acute HF due to decompensation of pre-existing
disease/cardiomyopathy (most common)
•
De novo HF = acute HF occurring for the 1st time in a patient w/out known cardiomyopathy
Etiology
Type of acute
HF
De novo HF
Underlying etiology
•
Acute myocardial dysfunction = cardiac ischemia, myocarditis, drug-induced
cardiomyopathy, peripartum cardiomyopathy, thyroid storm
•
Acquired valvular pathology = acute mitral regurgitation after acute coronary syndrome,
bacterial endocarditis, non-bacterial thrombotic endocarditis
ADHF
•
Extracardiac pathologies that affect LV output = pulmonary embolus, pericardial effusion
causing tamponade, aortic dissection
•
Uncontrolled/refractory HT
•
New/worsening cardiac ischemia
•
Arrhythmias (A-Fib, complete heart block)
•
Serious infections/sepsis
•
Drugs = Non-adherence to HF drugs, NSAID use, drugs w/-ve inotropic properties
(Verapamil), starting/uptitrating BB, recreational drugs(cocaine, alcohol), pioglitazone
•
Anemia
•
Renal failure
•
Volume overload
•
40-50% of cases = no trigger is found
Clinical manifestations
Clinical features of acute HF are commonly classified according to perfusion and the presence of
congestion at rest
•
Congestion (most common) = clinical features of L HF (acute dyspnoea and orthopnoea,
flash pulmonary oedema [HT, PC, and minimal peripheral edema])
o signs of ↑ work of breathing: accessory muscle use (e.g., sternocleidomastoid and
o
o
o
o
•
scalene muscles), tripod positioning, nasal flaring, retractions (intercostal, subcostal,
and suprasternal), grunting, pursed lips, and paradoxical breathing.
Coarse crackles/rales, cough (can be with frothy, bloody sputum),
S3 gallop sound on auscultation
Severe cases – central cyanosis (complication of pulmonary edema)
Clinical features of R HF: peripheral oedema, JVD, Hepatojugular reflux, Ascites
Hypoperfusion = weakness, fatigue, altered mental status; signs of poor peripheral perfusion
(cold, clammy skin; peripheral cyanosis; skin mottling)
Adequate perfusion
Hypoperfusion
No evidence of congestion (~5%
of patients)
Evidence of congestion (~95%
of patients)
Warm and dry
Warm and wet
Cold and dry
Cold and wet
•
Adequate perfusion = strong peripheral pulse, warm skin, and capillary refill time <2 seconds.
•
No congestion = lungs are clear on auscultation, no signs of ↑ WOB, and minimal oedema
•
Congestion = orthopnoea, ↑ jugular venous pressure, S3 heart sound, oedema, and
pulmonary rales
Diagnosis
•
Labs = ↑ BNP [>500pg/ml] (or NT-proBNP). To evaluate for underlying cause or severity,
check troponin [mildly elevated], BMP [↑Cr, ↓Na, {↓K, Metabolic alkalosis - diuretics}] and
electrolytes, CBC [Anemia], LFT’s, Thyroid function tests
•
ECG = indicated to exclude acute coronary syndrome. Findings may include = A-Fib, LV
hypertrophy, bundle branch block, non-specific ST changes, low voltage QRS (in pericardial
effusion, pulmonary edema); ECG may also be normal
•
CXR = pulmonary congestion – ABCDE – alveolar oedema (bat wings), Kerley B lines
(interstitial oedema), cardiomegaly, dilated prominent pulmonary vessels, and effusions
•
Echocardiography = ↓/normal LVEF, diastolic dysfunction, pericardial effusion, LA dilation,
valvular disorders – Mitral regurgitation,
•
Cardiac MRI = may show evidence of fibrosis, cardiomyopathy, or perfusion defects
•
Cardiac CT = assessment of coronary aa. and structural defects
DDx = acute coronary syndrome, pneumonia, COPD, ARDS, PE
Cardiogenic shock
Shock = a life-threatening disorder of the circulatory system that results in inadequate organ
perfusion and tissue hypoxia, which in turn, causes metabolic disturbances and, ultimately,
irreversible organ damage.
Cardiogenic shock = persistent hypotension and tissue hypoperfusion due to cardiac dysfunction in
the presence of adequate intravascular volume and LV filling pressure.
Etiology = MI (most common), arrhythmias, HF, cardiomyopathy, myocarditis, ventricular septal
defect, severe aortic/mitral regurgitation, certain drugs (BB/CCB), blunt cardiac trauma
Pathophysiology
Underlying event causes dysfunction of the heart → HF → ↓ CO and BP → ↑ catecholamines → VC
and ↑ myocardial O2 demand → ↑ RAAS → further ↑ VC and retention of sodium and water →
shunting of blood to brain and vital organs → insufficient perfusion of peripheral organs
Clinical manifestations
•
Weak pulse, tachycardia
•
Hypotension
•
Dyspnoea
•
Mental status change
•
Other clinical features related to the underlying disease = chest pain in MI; palpitations and
syncope in arrhythmias
•
Physical examination might show = cold, clammy extremities, poor capillary refill; abnormal
auscultatory findings (S3, S4); pulmonary oedema, diffuse lung crackles; ↑ JVP and distended
neck vv.
Diagnosis = mostly clinical
•
Identify the cause = ECG (MI, arrhythmias); cardiac markers (to identify acute coronary
syndrome); echocardiography (valvular lesions)
•
Pulmonary a. catheterisation = to monitor hemodynamic parameters as a guide to therapy (↑
Pulmonary Wedge Capillary P, ↓ CO, ↑ Systemic Vascular Resistance)
Treatment = based on underlying etiology
•
Cardiopulmonary resuscitation if necessary
•
Fluid bolus only in cases of ↓ BP and/or PCWP <15 mmHg
•
Inotropic therapy (to maintain perfusion) = dopamine in patients’ w/hypotension; dobutamine
in patients w/normal BP
•
Vasopressors (noradrenaline)
•
Intra-aortic balloon pump if medical therapy fails
•
Diuresis
Complications = pulmonary oedema, acute renal failure
22) Treatment of acute HF
Hemodynamically unstable patients (i.e. cardiogenic shock)
Treatment
Dry and
cold
1) Consider an initial small fluid bolus (250-500 ml)
•
Assess fluid responsiveness; consider additional bolus if fluid responsive (ability of
fluid therapy to measurably ↑ CO (e.g. by 10-15%) for a given patient)
• Reassess for volume overload (e.g. tachypnoea, signs of ↑ WOB)
2) If shock persists, start a vasopressor, ideally, noradrenaline
3) Administer inotropic support (dobutamine/NA) if hypoperfusion persists despite fluids and
vasopressors
Wet and
cold
1)
2)
3)
4)
Prioritize respiratory support
Administer inotropic support
If shock persists, start a vasopressor, ideally, noradrenaline
One systolic BP is >90 mmHg, start diuretics
Hemodynamically stable patients
For dry and warm = optimise oral therapy
For wet and warm and wet and cold (if SBP >90) = start
diuretics for volume overload, consider a vasodilator.
Respiratory support in acute HF
•
Ensure the patient is sitting upright
•
Supplemental O2 = indicated for patients w/SpO2
<90% or PaO2 < 60 mmHg
•
High-flow nasal cannula = consider in patients
w/SpO2 <90% non-responsive to basic O2 delivery
system
•
Invasive mechanical ventilation = indicated for hypoxemic respiratory failure unresponsive to
non-invasive positive-pressure ventilation; refractory hypoxaemia (PaO2 <60 mmHg);
hypercapnia (PaCO2 >50 mmHg); acidosis (pH < 7.35)
Meds
•
Initial therapy of acute decompensated HF usually includes some combo of a vasodilator
(nitroglycerin), a loop diuretic (furosemide), and non-invasive positive-pressure ventilation.
•
Common types of meds prescribed for HF = ACEI, vasodilators, BB, aspirin, and cholesterol
lowering meds (statins)
•
Vasodilators (nitro-glycerine/ Sodium nitroprusside) = often used as part of initial therapy.
Indicated for acute HF caused by hypertensive emergency, flash pulmonary oedema, and
adjuvant to diuretics for symptomatic relief of dyspnoea.
o !! Avoid in patients w/ Acute HF and Hypotension
•
Diuretics = initial treatment w/diuretics and IV nitroglycerin to relieve volume overload and
congestive symptoms. !!Monitor electrolytes and replenish.
o First line: I.V Furosemide plus Nitroglycerin, if persistent HF - then combination
therapy w/ Thiazide diuretic
•
ACEI/ARBs = should be continued unless there is significant decline in renal function (Monitor
serum Cr)
•
BB (metoprolol, Carvedilol, bisoprolol) = for patients not previously on them, BB should be
started cautiously at low dose after stabilisation and slowly uptitrated.
Surgery
•
Acute HF due to acute aortic regurgitation is a surgical emergency associated w/high mortality
•
HF may occur after rupture of a ventricular aneurysm
•
Cardiac tamponade may require surgery
•
Surgery is sometimes recommended to treat the underlying pathology (e.g. coronary a.
bypass surgery, heart valve repair/replacement, heart transplant)
•
During these procedures, devices such as pacemakers or defibrillators may be implanted
23) Chronic congestive heart failure
Definitions
•
Congestive HF (CHF) = a progressive clinical syndrome in which the heart is unable to pump
enough blood to meet the metabolic needs of the body. Characterised by ventricular
dysfunction that results in blood congestion and low CO
•
Systolic dysfunction = CHF w/↓ SV, ↑ EDV, and ↓ EF
•
Diastolic dysfunction = CHF w/↓ SV, normal/↓ EDV, and preserved EF. Characterised by
low myocardial compliance (due to compensatory hypertrophy)
•
Right HF (RHF) = CHF due to RV dysfunction
•
Left HF (LHF) = CHF due to LV dysfunction. Long-standing LHF is the most common cause
of RHF
•
Biventricular (global CHF = CHF in which both the LV and RV are affected (1-sided CHF
commonly progresses to biventricular CHF) → results in development of both RHF and LHF
symptoms
•
Chronic compensated CHF = clinically compensated type of CHF in which the patient has
signs of CHF on echocardiography but is asymptomatic or symptomatic and stable
•
Acute decompensated CHF = sudden deterioration of CHF or new onset of severe CHF due
to an acute cardiac condition (e.g. MI)
Classification
Classification according to:
•
The degree of involvement of the pump function of the L ventricle – HF w/preserved ejection
fraction [HFpEF – ≥50%]; HF w/mid-range EF [HFmrEF – 40-49%]; HF w/↓ EF [HFrEF –
<40%]
•
The time course – asymptomatic LV systolic dysfunction; chronic HF (stable/decompensated);
acute HF; congestive HF
•
The side of the heart affected – LHF; RHF; biventricular HF
•
The severity of symptoms and exercise intolerance (according to The New York Heart
Association (NYHA) functional classification)
Class I = no limitations of physical activity; no symptoms of CHF
Class II = slight limitations of moderate/prolonged activity (climbing 2 flights of
stairs/ heavy lifting); comfortable at rest
Class III = marked limitations of physical activity (short walk, dressing); comfortable
only at rest
Class IV = confined to bed, discomfort during any form of physical activity; symptoms
at rest
Etiology
Systolic dysfunction (↓ EF)
General causes
Specific causes
Further risk factors
Diastolic dysfunction (preserved
EF)
•
CAD, MI
•
HT
•
Valvular heart disease
•
DM (diabetic cardiomyopathy)
•
Renal disease
•
Infiltrative diseases (hemochromatosis, amyloidosis)
•
Dilated cardiomyopathy
•
Restrictive cardiomyopathy
•
Cardiac arrhythmias
•
Hypertrophic cardiomyopathy
•
Myocarditis
•
Pericardial tamponade
•
Constrictive pericarditis
Obesity, smoking, COPD, heavy drug use, alcohol abuse
Pathophysiology
CHF is characterised by ↓ CO (CO = SV X HR – determined by preload, afterload, and ventricular
contractility) that results in venous congestion and poor systemic perfusion.
Underlying mechanism of ↓ CO
Systolic ventricular dysfunction (most common) due to:
•
↓ contractility = damage and loss of myocytes (post-MI, CAD, DCM)
•
↑ afterload = ↑ in mean aortic pressure, outflow obstruction (HT, aortic stenosis)
•
↑ preload = ventricular volume overload
• Cardiac arrhythmias
Diastolic ventricular dysfunction due to:
•
↓ ventricular compliance = ↑ stiffness or impaired relation of the ventricle → ↓ ventricular filling
and ↑ diastolic pressure → ↓ CO
•
↑ afterload = ↑ in pulmonary a. pressure
• ↑ preload = ventricular volume overload
HFrEF
•
↓ contractility → Systolic V dysfunction → ↓ LVEF = ↓ CO → poor organ perfusion → organ
dysfunction (e.g. hypotension, renal dysfunction)
HFpEF
•
Diastolic dysfunction:
↑ LV volume and pressure → backup of blood into the lungs → ↑ pulmonary capillary
pressure → cardiogenic pulmonary oedema → orthopnoea
↓ CO → systemic venous congestion → oedema and progressive congestion of
internal organs
Nutmeg liver = macroscopic appearance of the liver which resembles a nutmeg seed
due to ischemia and fatty degeneration from hepatic venous congestion
Compensation mechanisms to maintain CO when SV is ↓
•
↑ adrenergic activity = ↑ in HR, BP, and ventricular contractility
•
↑ of RAAS = activated following ↓ in renal perfusion secondary to ↓ of SV and CO – ↑
angiotensin II (peripheral VC → ↑ systemic BP → ↑ afterload; VC of efferent arterioles → ↓ net
renal blood flow and ↑ intraglomerular pressure → maintained GFR) and ↑ aldosterone
secretion (↑ renal Na+ and H2O resorption → ↑ preload)
•
Secretion of brain natriuretic peptide (BNP) = a hormone release in response to ↑ ventricular
filling and stretching.
Clinical manifestations
General features of HF
•
Nocturia – in the supine position, CO ↑ and renal VC ↓
→ ↑ in filtered urine and Nocturia
•
Fatigue
•
Tachycardia, various arrhythmias
•
S3/S4 gallop on auscultation – S3 gallop indicates
rapid ventricular filling; S4 gallop indicates ventricular
hypertrophy (↓ compliance)
•
Pulsus alternans – alternating strong and weak pulses (w/regular pulse rhythm) caused by
alterations in CO
•
Cachexia
Clinical features of LHF
Symptoms of pulmonary congestion (blood backs up into the lungs)
•
Dyspnoea, orthopnoea
•
Pulmonary oedema
Paroxysmal nocturnal dyspnoea = nocturnal bouts of coughing and acute SOB.
Caused by reabsorption of peripheral oedema at night → ↑ venous return
•
Cardiac asthma = ↑ pressure in the bronchial aa. → airway compression and bronchospasm.
Symptoms mimic asthma, w/SOB, wheezing, and coughing
•
Fatigue – due to ↓ CO
•
Cyanosis and hypoxia (severe) – due to impaired gas exchange
•
Physical examination = bilateral rales; laterally displaced apical heart beat (precordial
palpation beyond the midclavicular line); coolness and pallor of lower extremities
Clinical features of RHF
Symptoms of fluid retention and ↑ central venous pressure (BP in the RA or SVC)
•
Peripheral pitting oedema – as a result of fluid transudation due to ↑ venous pressure
•
Hepatic venous congestion symptoms = abdominal pain, jaundice
•
Other symptoms of organ congestion = nausea, loss of appetite, congestive enteropathy
•
Blood backs up to the body in R HF → systemic v. congestion → jugular venous distension
•
When blood backs up to the liver and spleen → fluid moves into interstitial spaces w/in those
organs = hepatosplenomegaly
•
If the liver is congested for a long period of time = cardiac cirrhosis and liver failure
•
Excess interstitial fluid near surface of liver and spleen can move to peritoneal spaces →
ascites (build up of fluid in peritoneal space)
•
Physical examination = jugular venous distension; Kussmaul sign; hepatosplenomegaly;
hepatojugular reflux
Diagnosis
Labs = ↑ BNP and ANP; CBC may show anaemia; electrolytes (hyponatremia = poor prognosis);
RFT = ↑ creatinine, ↓ Na; urine analysis; fasting glucose
ECG = abnormalities are common but non-specific and non-diagnostic
•
Signs of LV hypertrophy = ↑ QRS voltage and duration; L axis deviation; ST-T abnormalities;
P wave abnormalities
•
Assessment of prior or concurrent heart conditions = previous or acute MI, arrhythmias
•
Signs of pericardial effusion and pericardial tamponade = low voltage ECG
CXR = differentiate CHF from pulmonary disease
•
Signs of cardiomegaly = cardiothoracic width ratio >0.5; boot-shaped heart on PA view
•
Pulmonary congestion
Echocardiography (gold standard) Assess ventricular function and hemodynamics
•
Atrial and ventricular size
•
Interventricular septum thickness = >11 mm indicates cardiac hypertrophy
•
Systolic function = LVEF (normal 50-70%, borderline 41-49%, ↓ ≤40%)
•
Diastolic function = diastolic filling, ventricle dilation
•
Investigate etiology = valvular heart disease, wall motion abnormalities
Others:
•
Cardiac stress test = assess functional impairment due to CHF or other conditions
•
Radionuclide ventriculography = assess LV volume and LVEF
•
Cardiac MRI = assess cardiac morphology and function
•
Coronary angiography = detect/confirm CHD and possible percutaneous coronary
intervention
24) Parameters of cardiac function in CHF. Treatment of Chronic heart
failure
Parameters of cardiac function in CHF.
•
Heart rate - number of heart contractions per minute (bpm), 60-100 normal
•
Stroke Volume - Volume of blood pumped by L/R ventricle in a single heart beat
o SV = EDV - ESV
•
Ejection fraction - the proportion of EDV ejected from the ventricle.
o
o
•
•
Cardiac Output- the volume of blood the heart pumps per minute.
o CO = SV * HR ~ 5 L/min at rest
o
CO = O₂ Consumption/ (arterial O₂ content - venous O₂ content) – Fick’s law
o
MAP = 1/3 SBP + 2/3 DBP
Myocardial O₂ demand - amount of O₂ required for optimal heart function
o
•
Depends on: HR, contractility, wall tension, afterload
Cardiac blood pressure.
o
o
o
o
•
EF= (SV) EDV-ESV/ EDV. normal 50-70%.
Index lor myocardial contractility.
RA: < 5 mmHg
RV: 25/5 mmHg
LA (pulmonary capillary wedge pressure): <12 mmHg
LV: 130/10 mmHg
Factors affecting Cardiac Output: preload, afterload, contractility.
o
o
o
•
Preload- the extent to which heart muscle fibres are stretched before the onset of
systole. Depends on EDV.
Venous constriction - ↑ venous tone ↑ venous blood return ↑EDV ↑
preload
Circulating blood ↑ volume of blood ↑ venous return to the heart ↑EDV
↑ preload
Afterload- the force against which the ventricle contracts to eject blood during systole.
Determined by MAP in the aorta which is influenced by total peripheral
resistance
↑ afterload ↑ LVP ↑ LV wall stress.
Contractility- the inherent ability of the heart muscle to contract
↑ by sympathetic innervation, catecholamines, exercise, thyroid hormones,
digitalis
Cardiac index – volume of blood ejected from the heart (cardiac output, L/min) in relation to
body surface area; Normal range - 2.8-4.2 L/min/m². Easier to measure vs CO
General measures
•
Salt restriction (2-3g/day) in symptomatic patients
•
Fluid restriction in patient’s w/oedema and/or hyponatremia
•
Weight loss and exercise
•
Cessation of smoking and alcohol consumption
•
Immunisation = pneumococcal vaccine and seasonal
influenza vaccine
•
Patient education = Self-monitoring and symptom
recognition; monitoring of potential medication side
effects
•
Treatment of underlying conditions and contributing
comorbidities (HT, atrial fibrillation, IHD, DM2)
•
Offer a personalised exercise-based cardiac
rehabilitation programme unless condition is unstable
Drugs
•
1st line drugs = ACEIs/ARBs, diuretics, BB
•
2nd line drugs = ivabradine, hydralazine + nitrate, digoxin, Valsartan/sacubitril
•
Invasive = implantable cardiac defibrillator, biventricular pacemaker (cardiac
resynchronisation therapy), coronary revascularisation, valvular surgery, heart transplant
Drug
Diuretics
ACEIs
NYHA stages
All stages
All stages
Indications
•
Begin treatment w/loop
diuretics (furosemide) to treat
volume overload
•
Thiazides may be added for
a synergistic effect
•
Initiate treatment w/ACEIs to
↓ preload, afterload, and
improve CO
•
If patient doesn’t tolerate the
drug, substitute w/ARB
Side effects
•
Monitor for
hypokalemia and
hyponatremia, weight
gain, and volume
status
•
Monitor for
hyperkalemia,
hypotension, ↑
creatinine (renal
impairment)
Beta
blockers
•
All stages
Add a β-blocker once the
•
patient is stable on ACEIs
Aldosterone
antagonists
Stages 2-4
•
Particularly beneficial for
patients w/HT and post-MI
•
May be beneficial in select
patients
•
Patients w/EF <35% and
Contraindicated in
acute decompensated
HF
•
Monitor for
hyperkalemia
after MI
•
Drug
Ivabradine
Spironolactone; eplerenone
as an alternative
NYHA
stages
Stages 2-4
Indications
•
If the highest tolerable dose
of beta blocker is reached
and the patient is still
symptomatic or if they have
contraindications to beta
Side effects
•
blockers
Hydralazine + nitrate
Stages 3-4
•
Patients w/EF <35% and a
sinus rhythm w/a resting HR
>70/min
•
Patients w/EF <40%
•
Particularly beneficial for
African-American patients
•
Alternative if ACEIs and
Contraindicated
in severe
bradycardia,
acute
decompensated
HF, and severe
hepatic
dysfunction
•
Monitor for
volume depletion
and hypotension
ARBs are not tolerated
Digoxin (0.25 mg
1X/day)
Stages 2-4
•
In HFrEF
•
If symptoms persist despite
treatment w/1st line drugs
•
May be given to control
ventricular rate in atrial
•
Contraindicated
in severe AV
block
fibrillation (if beta blockers
are contraindicated)
Angiotensin receptorneprilysin inhibitor
(Valsartan/Sacubitril)
All stages
•
Persistent or worsening
symptoms despite adequate
treatment regimen w/1st line
•
w/ACEIs
drugs in patients w/HFrEF
•
•
Administered as Valsartansacubitril combo
Impaired breakdown of
angiotensin II, substance P,
and natriuretic peptides → ↑
natriuresis, diuresis, and VD
→ ↓ ECF
↑ risk of
angioedema if
used in combo
•
Cough
•
Dizziness,
hypotension
•
Hyperkalemia
•
Progression of
CKD (↑
creatinine)
Treatment summary
•
1st = ACEI + BB. Add on a mineralcorticoid receptor antagonist (spironolactone) if symptoms
continue
•
Consider ARB if patient is intolerant of ACEI
•
Consider hydralazine + nitrate if intolerant of both ACEI and ARB
•
2nd = if symptoms persist despite 1st line treatment, seek specialist advice and consider ≥1 of
the following
Replace ACEI/ARB w/Sacubitril/Valsartan if EF <35%
Add ivabradine for sinus rhythm w/HR >75 and EF <35%
Add hydralazine and nitrate (especially if of Afro-Caribbean descent)
Add digoxin for HF w/sinus rhythm to improve symptoms
•
Treat all other comorbidities
Add anti-coagulants = warfarin (5 mg 1X/day, max 10 mg), dabigatran (150 mg
2X/day), rivaroxaban (15 mg 1X/day, max 20 mg)
Add an anti-arrhythmic = amiodarone (200 mg 1X/day)
Contraindicated drugs
•
NSAIDs = worsen renal perfusion; ↓ effect of diuretics; may trigger acute cardiac
decompensation
•
Inhalation anaesthetics = induce myocardial depression and peripheral VD; ↓ sympathetic
activity
•
CCBs (verapamil and diltiazem) = -ve inotropic effect; worsen symptoms and prognosis
•
Pioglitazone = promote the progression of CHF (↑ fluid retention and oedema); ↑
hospitalisation rate
•
Moxonidine = ↑ mortality in HFrEF
•
Antidepressants (citalopram) = causes a dose-dependent QT prolongation
Device therapy and surgery
•
Cardiac resynchronisation therapy (CRT) = the insertion of electrodes in the LV and RV, as
well as on occasional the RA, to treat HF by coordinating the function of the LV and RV via a
pacemaker
•
Implantable cardiac defibrillator/automated implantable cardioverter defibrillator = a device
implantable inside the body, able to perform cardioversion (arrhythmia is converted to a
normal rhythm), defibrillation, and pacing of the heart (generates electrical impulses)
•
L ventricular assist device (LVAD) = an electromechanical device for assisting cardiac
circulation, which is used to completely replace the function of a failing heart.
•
Cardiac transplantation = option for especially young patients w/refractory end-stage disease
25) Ischemic heart diseases: classification. Stable angina pectoris –
clinical features, treatment
Definitions
•
Ischemic heart disease (IHD) = ↓ blood flow to the heart muscle due to build-up of plaque in
coronary aa.
•
Coronary artery disease (CAD) = IHD due to narrowing or blockage of coronary aa., most
commonly due to atherosclerosis, resulting in a mismatch between myocardial O2 supply and
demand
•
Angina = chest pain caused by myocardial ischemia (necrosis of myoctes has not yet
occurred) due to narrowing or spasm of the coronary a.
•
Stable angina = a type of angina that occurs upon exertion, mental stress, and/or exposure to
cold and usually subsides w/in 20 mins of rest or after administration of nitroglycerin
•
Vasospastic (AKA variant/Prinzmetal) angina = angina caused by transient coronary
spasms (usually due to spasms occurring close to areas of coronary stenosis
Etiology and risk factors
Atherosclerosis is the most common cause – build-up of plaque w/in tunica intima of the arterial
wall, which can restrict blood flow. Risk factors include:
•
HT
•
Smoking; excessive alcohol
•
Diabetes; obesity; poor diet; high blood cholesterol; lack of exercise
•
Depression, stress
•
Family history – CV event <55yrs
Pathophysiology
Plaque formation and coronary a. stenosis
•
Plaque formation
•
Stable atherosclerotic plaque → vascular stenosis → ↑ resistance to blood flow in the
coronary aa. → ↓ myocardial blood flow → O2 supply-demand mismatch → myocardial
ischemia
•
The extent of coronary stenosis determines the severity of the O2 supply-demand mismatch
and, thus, the severity of myocardial ischemia. Severe ischemia results in MI
Myocardial O2 supply-demand mismatch
•
Definition = mismatch between the amount of O2 the myocardium receives and the amount it
requires
•
Factors ↓ supply = coronary atherosclerosis and sequelae, including = rupture of an unstable
plaque (most common), thrombosis, and stenosis; vasospasms (↑ HR, anemia)
•
Factors ↑ demand = ↑ HR, ↑ afterload, anemia
Clinical manifestations
Angina
Angina is the cardinal symptom of CAD. Patients usually become symptomatic when the degree of
coronary stenosis reaches ≥70%
•
The small opening that blood flows through is enough to supply the heart during rest = no pain
•
Exercise/stress = ↑ O2 demand = heart needs to work harder and thus needs > blood and O2
→ chest pain – blood flow can’t meet metabolic demands of myocardium
Symptoms include:
•
Typically, retrosternal chest pain/pressure. Pain may radiate to the L arm, neck, jaw,
epigastric region, or back. It is not affected by body position or respiration; no chest wall
tenderness; may gradually ↑ in intensity; may present as GI discomfort (indigestion); may be
absent in geriatric and diabetic patients
•
Dyspnoea
•
Dizziness, palpitations
•
Restlessness, anxiety
•
Autonomic symptoms (e.g., diaphoresis, N/V, syncope)
Stable angina
•
Symptoms are reproducible/predictable
•
Symptoms often subside w/in minutes w/rest or after administration of nitroglycerin
•
Provoking factors = physical exercise, stress, HT, tachycardia or extreme bradycardia,
hypoglycaemia, cold weather (↑ need of O2 by the myocardium)
Vasospastic angina
•
Patients are generally younger (~50yrs), females (commonly Japanese) and have risk factors
such as stress, cold exposure, other vasospastic disorder (Raynaud), use of stimulants ~
cocaine and smoking, which is a common and very significant factor for both types of anginas
•
Symptoms occur during rest or w/minimal exercise and frequently occurs nocturnally
(midnight-8 AM)
•
Not affected by exertion
Diagnosis
Patient history = Patients age (M>40y, W>60y), sex and history of chest pain. Assess RF’s
•
Retrosternal chest pain of characteristic nature and duration (e.g., transient retrosternal
pressure)
•
Provoked by exertion or emotional stress
•
Relieved by rest and/or nitroglycerin
•
Typical angina = all 3, Atypical = 2, Non-anginal chest pain = 0/1
Physical Exam = findings of
•
Atherosclerosis – absent foot pulses, carotid bruit
•
Congestive HF
•
Valvular heart disease
Resting ECG = best initial test for all types of chest pain; usually normal in stable angina.
•
Findings indicating previous MI/ unstable angina
o ST depression/ T wave inversion/flattening indicated
Labs = often ↑ levels of cholesterol (high LDL, low HDL) and triglycerides (high VLDL), blood sugar,
uric acid (metabolic syndrome)
Cardiac stress test, echocardiography (detect wall motion abnormalities)
Cardiac catheterisation = gold standard of CAD diagnosis since it provides:
•
Information of several parameters = coronary blood flow, pressure w/in heart chambers, CO,
O2 saturation
•
Direct visualisation of coronary aa. (coronary angiography)
•
Opportunity for direct therapeutic intervention using percutaneous coronary intervention
Coronary CT angiography: Determine no of vessels involved 1,2 etc/ involvement of LMCA
•
≥ 50% narrowing of the LMCA
•
≥ 70% narrowing of other coronary arteries, e.g., RCA, LCA, LAD
Holter monitoring = can detect silent ischemia and arrhythmias; can be used to evaluate HR
variability and pacemaker/ICD function
Radionuclide myocardial perfusion imagine (PET/SPECT) = to visualise perfusion
Coronary MRI
Treatment
•
All patients require risk factor reduction and anti-platelet, anti-anginal drugs
•
Mild CAD = pharmacologic therapy to reduce myocardial O2 demand (MVO2)
o 1st line BB (since they provide both symptomatic relief and secondary prevention) –
!!except in vasospastic angina, and nitrates.
Carvedilol – 6.25-25 mg every 12hrs
Nitrates
•
Nitroglycerin 0.3-0.6mg sublingually every 5mins for 15mins for duration
of angina attack
o
o
•
• Long acting (w/ BB) – Isosorbide dinitrate 5-40mg, 2-3times a day
line CCBs, ranolazine; combo therapy)
Amlodipine (DHP) – 5-10mg once daily
3rd line Ranolazine (if rest are ineffective or not well tolerated) – 500mg/ 12hrs.
2nd
Secondary prevention
o
o
o
o
o
Antiplatelet – Aspirin (75-150mg once daily)
ACEi/ ARB’s – Lisinopril/ Losartan – w. HT, DM, CKD, LVEF <40%
Atorvastatin – 40mg once daily. Lipid lowering therapy
Smoking cessation, increased physical activity
Treat comorbidities
•
Moderate CAD = (Complex CAD, 2/1 vessel disease, LMCA, LAD stenosis)
o Offer Revascularisation therapy: Percutaneous Transluminal Coronary Angioplasty
(PTCA)/ Percutaneous Coronary Intervention (PCI).
•
Severe CAD = (>50% stenosis of LMCA, LV dysfunction)
o Coronary A. Bypass Grafting (CABG)
o PCI
26) Acute coronary artery syndromes: acute myocardial infarction w/ST
segment elevation
Definitions
Acute coronary syndrome (ACS) = the suspicion or confirmed presence of acute myocardial
ischemia. ACS may be further classified into the following categories:
•
NSTE-ACS = ACS manifesting w/out ST-elevations on ECG – NSTEMI (+ve myocardial
injury biomarkers) and unstable angina (absence of detectable biomarkers)
•
STE-ACS = ACS manifesting w/ST-elevations on ECG (STEMI)
Myocardial infarction (MI) = death (irreversible ischemic necrosis) of the myocardium due to lack of
blood flow and complete blockage of the coronary aa. It is classified into 5 subtypes:
•
Type 1 = MI caused by atherosclerotic plaque disruption or acute coronary thrombosis (due to
erosion, ulceration, fissuring, dissection, or rupture of an atherosclerotic plaque). ↓ myocardial
blood flow → sudden death of myocardial cells
•
Type 2 = MI secondary to an O2 supply-demand mismatch
•
Type 3 = MI resulting in death when biomarker values are unavailable
•
Type 4 = MI related to percutaneous coronary intervention
•
Type 5 = MI related to coronary a. bypass grafting
STEMI = ST-elevation MI; NSTEMI/non-STEMI = no ST-elevation MI
Etiology
Any condition that causes occlusion of the coronary aa, ↓ myocardial O2 supply, or ↑ O2 demand can
potentially lead to myocardial ischemia and MI
•
CAD (most common cause)
•
Coronary a. vasospasm (e.g. vasospastic angina, cocaine use)
•
Coronary a. dissection
•
Coronary a. embolism
•
Myocarditis
•
Thrombophilia
•
Vasculitis
•
Myocardial O2 supply-demand mismatch – e.g. due to hypotension, severe anemia, HCM, and
severe aortic stenosis
Pathophysiology
Atherosclerotic plaque disruption
•
Stable atherosclerotic plaque = manifests as stable angina
•
Unstable plaques are lipid rich and covered by thin fibrous caps = high risk of rupture and
ACS
•
Inflammatory cells in plaque secrete enzymes to breakdown the ECM → weakening of the
fibrous cap → minor stress → rupture of fibrous cap → exposure of highly thrombogenic lipid
core → thrombus formation → coronary a. occlusion
Coronary a. occlusion
•
Partial occlusion = ↓ myocardial blood flow → supply-demand mismatch → myocardial
ischemia. Usually affects the inner layer of the myocardium (subendocardial infarction);
typically manifests clinically as unstable angina and/or NSTEMI
•
Complete occlusion = impaired myocardial blood flow → sudden death of myocardial cells.
usually affects the full thickness of the myocardium (transmural infarction); typically manifests
clinically as STEMI
•
The most commonly occluded coronary aa. (in descending order) = L ant. descending (LAD),
R coronary a., circumflex a.
Clinical manifestations
Classic presentation
•
Acute retrosternal chest pain = typically dull, squeezing pressure and/or tightness; commonly
radiates to L chest, arm, shoulder, neck, jaw, and/or epigastrium; precipitated by
exertion/stress
•
Dyspnoea (especially w/exertion)
•
Pallor; N/V
•
Diaphoresis (excess sweating); anxiety
• Dizziness, light-headedness, syncope
Other findings
•
Tachycardia EXCEPT for septal infarction (location of AVN → AV block → bradycardia)
•
Symptoms of CHF (orthopnoea, pulmonary oedema) or cardiogenic shock (hypotension,
tachycardia, cold extremities)
• New heart murmur on auscultation (e.g. new S4)
Atypical presentations = > likely in elderly, Diabetic, and F
•
Stabbing, sharp chest pain
•
No/minimal chest pain = “silent MI” w/out chest pain is > common in patients w/DM, as a
result of polyneuropathy
•
Autonomic symptoms = N/V, diaphoresis
More common in inferior wall infarction = epigastric pain, bradycardia
Diagnosis
ECG (12-lead)
•
Significant ST elevation in 2 contiguous leads
•
Other findings include pathological Q waves, ST-segment shifts, and T wave inversions
•
Classical timeline of ECG changes = acute stage (myocardial damage ongoing), intermediate
stage (myocardial necrosis present), and chronic stage (permanent scarring)
•
The sequence of ECG changes over several hours to days = hyperacute T waves → ST
elevation → pathological Q wave → T wave inversion → ST normalisation → T wave
normalisation
Cardiac biomarkers
•
Cardiac troponin (cTn) is the most important biological marker of myocardial necrosis. In
acute myocardial injury changes occur in sequential measurements; in myocardial injury there
is cTn elevation above the 99th percentile of the upper reference limit
Biomarker
Troponin T/I
Rise
Regular assays =
6-8 hours
High-sensitive
assays = 1-3
hours
Max.
12-24
hours
Normalisation
7-10 days
Characteristics
•
Cardiac-specific marker w/highsensitivity for myocardial
necrosis
•
The degree of elevation
correlates w/the size of infarct
and risk of mortality
CK-MB
~4-9 hours
12-24
hours
2-3 days
•
No longer commonly used;
replaced by cTn
•
CK-MB is > specific to cardiac
tissue than total CK
•
Myoglobin
~1 hour
4-12
hours
24 hours
Can be helpful for evaluating
reinfarction because of its short
HL
Non-specific marker; no longer
commonly used
Additional labs = ↑ WBC and CRP; BNP may be ↑; LDH and AST may be ↑ due to cell necrosis
Coronary angiography = best test for definitive diagnosis of coronary occlusion to identify site and
degree of vessel occlusion; can be used for concurrent intervention
Imaging = transthoracic echocardiography (assess LV function and identify wall abnormalities) and
cardiac CT w/IV contrast
Histopathology
Treatment
•
Immediate revascularisation = emergency PCI
•
Monitoring = serial 12-lead ECG, continuous cardiac monitoring, serum troponin
measurement
•
Dual anti-platelet therapy (aspirin + clopidogrel) and anticoagulants (unfractionated heparin or
LMWH)
•
Adjunctive therapy = sublingual/IV nitroglycerin, morphine IV (severe chest pain), BB, statins,
O2 (only in case of cyanosis or dyspnoea)
27) Acute coronary artery syndromes w/out ST segment elevation:
unstable angina pectoris, myocardial infarction w/out ST segment
elevation
Definition
Unstable angina (AKA crescendo angina) = angina pectoris that is irregular – a pattern of angina
that occurs randomly/unpredictably and is unrelated to any obvious trigger such as exercise/stress.
It is acute myocardial ischemia that is not severe enough to cause detectable quantities of myocardial
injury biomarkers or ST-elevations on ECG.
It has at least 1 of the 3 features:
1. It occurs at rest (or w/minimal exertion), usually lasting > 10 mins (15-30 min)
2. It is severe and of new onset
3. It occurs w/a crescendo pattern (i.e. distinctly > severe, prolonged, or frequent than before)
MI w/out ST elevation (NSTEMI) = acute myocardial ischemia that is severe enough to cause
detectable quantities of myocardial injury biomarkers but w/out ST-elevations on ECG
Pathophysiology
Due to partial occlusion of the coronary a. → ↓ blood supply → myocardial ischemia. It usually affects
the inner layer of the myocardium (subendocardial infarction). The pathophysiology of UA/NSTEMI
can be divided into 5 stages:
1) The development of the unstable plaque that ruptures or plaque erosion w/superimposed nonocclusive thrombosis
2) An obstruction such as spasm, constriction, dysfunction, or adrenergic stimuli
3) Severe narrowing of the coronary lumen
4) Inflammation
5) Any physiological state causing ischemia related to ↓ O2 supply such as fever or hypotension
Clinical manifestations = similar to STEMI; see conditions for UA above
Diagnosis
ECG
•
No ST elevation present
•
Non-specific signs of ischemia may be present = ST depression, transient ST deviations ≥ 0.5
mm in symptomatic patients at rest, T wave inversions of ≥ 2 mm in V1-V6
Cardiac troponin (troponin T/I)
•
Measure levels at arrival and after 1-6 hours; repeat if symptoms or ECG changes occur;
consider repeat after 72 hours as a marker of infarct size
•
Findings = elevation above the 99th percentile in NSTEMI; usually normal in UA
Transthoracic echocardiography = generally not necessary and should not delay reperfusion
therapy. May be helpful in patients w/atypical symptoms or if diagnosis is unclear
Treatment
•
Invasive management depends on risk stratification (e.g. TIMI score) – very high-intermediate
risk patients require coronary angiography w/in 2-72 hours; low risk patients need further
testing to evaluate the need for angiography
•
Patients w/NSTEMI that have unstable hemodynamics, intractable angina, suspected post.
infarction, and/or L main-vessel occlusion require urgent PCI, even if no ST elevations are
present
•
Anticoagulants, antiplatelet therapy (e.g. aspirin, ADP receptor inhibitors)
•
Adjunctive therapy = statins, anti-HT agents, pain management (opioids, nitrates)
28) Conductive disturbances. Treatment of conductive disturbances.
Bradyarrhythmias
•
Bradyarrhythmias = HR < 60 beats/min; include sinus node dysfunction and atrioventricular
(AV) block
•
Sinus bradycardia = sinus node dysfunction resulting in ↓ HR <60 bpm
•
Results from a failure of either impulse initiation (SAN) or impulse conduction (AVN)
•
The 2 mechanisms by which bradycardia occurs = ↓ automaticity (SAN) and conduction block
(AVN)
Etiology
•
↑ Vagal tone (parasympathetic NS; ↑ vagus n. stimulation → causes ↓ automaticity of the
heart) = physiologic (athletes, sleeping) or pathologic (obstructive sleep apnoea,
neurocardiogenic – i.e., vasovagal response, pain, carotid sinus HS)
•
Ischaemia = MI (inf. wall MI due to R coronary a. occlusion), unstable/variant angina,
ischaemic cardiomyopathy
•
Inflammatory/infiltrative = myo-/endocarditis, amyloidosis/fibrosis, sarcoidosis, acute
rheumatic fever, hemochromatosis, systemic sclerosis, lupus, RA, lymphoma
•
Infections = lyme disease, Chagas disease, diphtheria, Legionella, malaria, toxoplasmosis,
infective endocarditis
•
Metabolic/endocrine = hyperkalemia, poisoning overdose (CO, cyanide, mercury),
hypothyroidism, adrenal hormone imbalance (pheochromocytoma, hypoaldosteronism)
•
Congenital = neuromuscular disease (LGMD, myotonic dystrophy), congenital AV block,
congenital heart disease, genetic mutations, hereditary motor sensory neuropathies
•
Degeneration of the conducting system = senile amyloidosis, familial progressive cardiac
conduction defect, aortic/mitral stenosis, idiopathic degenerative fibrosis
•
Iatrogenic = valve surgery, catheter ablation, complications of heart transplant
•
Meds = anti-arrhythmic drugs (adenosine, amiodarone, quinidine), anti-HT drugs (BB, nondihydropyridine CCB, clonidine, methyldopa), psychoactive drugs (lithium, opioids, phenytoin,
SSRIs), intoxication w/other agents (digoxin, propofol, muscle relaxants, ivabradine, cannabis)
•
Other = hypothermia, anorexia nervosa, ↑ intracranial pressure (Cushing’s triad of ↓ HR, HT,
and irregular RR), HT, hypertensive cardiomyopathy, ↑ RV pressure (RBBB), valvular
disease.
Symptoms = usually asymptomatic until the rate drops < 50 bpm; when symptomatic, it may cause
fatigue, weakness, dizziness, sweating, and at very low rates, fainting. Signs of unstable bradycardia
include signs of hypoperfusion, respiratory distress, chest pain, pulmonary oedema, shock, and
altered mental status
Management
ABCDE survey
•
No pulse = start CPR; pulse present = continue through ABCDE survey
•
Identify and treat hypoxemia = supplemental O2 to goal SpO2 >94%
•
Obtain a 12-lead ECG (only if immediately available)
•
Monitoring and supportive care = continuous cardiac monitoring and pulse oximetry, crash
cart at bedside, frequent BP assessment, IV access
Determine if patient is hemodynamically stable/unstable (Signs of AHF, shock, HoTN)
Signs of unstable present = administer atropine (0.5mg i.v every 3-5min). If atropine is ineffective,
alternatives: epinephrine: 2-10mcg/min, Dopamine: 2-20/mcg/kg/min OR prepare for emergency
transvenous pacing and follow algorithm for unstable bradycardia
Determine if patient is symptomatic or not
•
Symptomatic, stable bradycardia = most patients can be observed and won’t require
intervention. Patients w/severe symptoms should receive atropine. Patients w/2nd/3rd degree
AV block should be considered for transcutaneous/transvenous pacing
•
Asymptomatic bradycardia = usually no treatment is required
Overview of bradycardia based on ECG findings
Rhythm
Narrow QRS complex
Regular
Wide QRS complex
•
Sinus bradycardia
•
3rd degree AV block
•
1st degree AV block
•
•
2nd degree AV block, Mobitz II, w/fixed
2nd degree AV block, Mobitz II,
w/fixed conduction ratio
conduction ratio
Irregular
•
A-Fib
•
2nd degree AV block, Mobitz II
•
Atrial flutter w/variable AV block
•
Combo of A-Fib and any degree of
•
2nd
degree AV block – Mobitz I or II
AV block
Sick sinus syndrome (SSS) (AKA sinus node dysfunction, SAN disease)
Definition = dysfunction of the SAN that is responsible for several types of arrhythmias. It comprises
bradyarrhythmias (e.g. sinus bradycardia, sinoatrial pauses, blocks, and arrest), and may alternate
w/supraventricular arrhythmias, in which case it is referred to as tachycardia-bradycardia syndrome
(periods in which atrial tachyarrhythmias and bradycardia alternate)
Etiology
•
Degeneration and fibrosis of the SAN and surrounding myocardium (most common cause) –
SSS most commonly occurs in elderly individuals
•
Meds (BB, CCB – verapamil, diltiazem)
Symptoms
Symptoms vary or may be entirely absent depending on the extent of bradycardia/tachycardia
•
Symptoms of bradycardia = dizziness, syncope, lack of ↑ HR during physical activity, AdamsStokes attacks (a sudden loss of consciousness, usually w/out warning and lasting for a few
seconds, due to an abnormal heart rhythm)
•
Tachycardia-bradycardia syndrome = palpitations, dyspnoea, angina pectoris
Diagnosis
•
ECG = non-respiratory sinus arrhythmia, bradycardia, sinus arrest, sinoatrial pauses, or SA
block; in cases of tachycardia-bradycardia syndrome: atrial tachycardia, atrial flutter, or A-Fib
•
Holter monitoring (continuous, ambulatory, battery operated ECG worn by patients for 24-48
hrs) = detects bradycardic episodes and sinus pauses
•
Exercise stress testing = shows an inadequate ↑ HR during physical activity (chronotropic
incompetence)
•
Atropine challenge test = shows an inadequate ↑ HR after admin of atropine
•
Electrophysiology studies = may show prolonged sinus node recovery time
Treatment
•
All patients = address reversible causes (e.g. meds); asymptomatic patients = no pacemaker
placement needed
•
Symptomatic patients =
o Initial therapy for Hemodynamically unstable: 1. atropine, 2. temporary cardiac pacing.
o Long-term therapy: Pacemaker for isolated symptoms of bradycardia.
Tachycardia-bradycardia syndrome requires pacemaker and meds –
cardioselective BB: metoprolol)
•
For A-fib, a-flutter: check need for anti-coag (CHAD-VASC)
Atrioventricular (AV) block
Definition = AV block is characterised by an interrupted or delayed conduction between the atria and
ventricles. There are 3 degrees of AV block, categorised according to the extent of the
delay/interruption.
Etiology = see causes of bradycardia above (AV block is very common in the period immediately
following an MI)
Pathophysiology
•
AV block results from the interruption of the electrical impulse anywhere w/in the AV
conduction system including the AVN, bundle of His, and L and R bundle branches
•
Blocks at the level of the AVN = impulse passes thorugh the AVN → normal propagation
through conduction system → narrow QRS complex
•
Infranodal block = can be at the level of/ below the bundle of His; ventricular depolarisation is
impeded → wide QRS complex
•
More distal AV blocks = typically result from > extensive damage to the conducting system →
↑ risk of progression to complete heart block.
Clinical manifestations
•
Asymptomatic (common) = especially w/1st degree and Mobitz type I
•
Clinical features of end-organ hypoperfusion (due to bradycardia) may be present = fatigue,
exercise intolerance, dyspnoea, dizziness, syncope
•
Irregular rhythms (e.g. Mobitz I) = palpitations
•
Loss of AV synchrony (e.g. extreme 1st/3rd degree block) (causes the atria to contract against
closed AV valves) = feeling of pulsations in the neck/chest, cannon A waves (retrograde
pressure throughout the venous system that may appear as pulsations in the jugular v.),
symptoms of HF (CO may ↓ if synchrony ↓ ventricular filling → fatigue, dyspnoea, exercise
intolerance)
•
Significant pauses of asystole = Stokes-Adams attacks (caused by ventricular asystole, most
commonly due to 3rd degree AV block), cardiac arrest
1st degree AV block
•
A delayed (but undisrupted) AV conduction resulting in prolonged PR interval (> 0.2 s)
•
No interruption in atrial to ventricular conduction
•
Rate of SAN = HR
•
Usually asymptomatic; often discovered incidentally on ECG
•
Risk of progression to complete heart block = low, as the block results from slowed
conduction through the AVN
•
Treatment is not usually required as it is a benign condition
2nd degree AV block
Mobitz type I (Wenckebach)
•
Characterised by a progressive, yet reversible block of the AVN.
•
On ECG, this is defined by a progressive prolongation of the PR interval, w/a resulting
dropped beat (the PR interval gets longer and longer until a beat is finally dropped, or
skipped)
•
A dropped beat means a regular atrial impulse does not reach the ventricles (a normal P
wave is not followed by a QRS complex)
•
Mostly regular rhythms separated by short pauses, which may lead to bradycardia (regularly
irregular rhythm)
•
Rate of SAN > HR
•
Risk of progression to complete heart block = typically low, as the block is most often at the
level of the AVN (blocks at the level of the bundle of His/the His-Purkinje system are rare)
•
May be seen in healthy individuals (e.g. athletes w/↑ vagal tone); patients are often
asymptomatic
Mobitz type II
•
A sudden, unexpected failure of the His-Purkinje cells to conduct the electrical impulse
•
On ECG, the PR interval is unchanged from beat to beat, but there is a sudden failure to
conduct the signals to the ventricles, and a resulting random skipped beat
•
The conduction of atrial impulses to the ventricles typically follows a regular pattern e.g:
3:2 block = regular AV block w/3 atrial depolarisations but only 2 atrial impulses that
reach the ventricles (HR = 2/3 SAN rate)
4:3 block = regular AV block w/4 atrial depolarisations but only 3 atrial impulses that
reach the ventricles (HR = ¾ SAN rate)
•
While 2:1 block follows a regular pattern, it cannot be classified as Mobitz I/II and is classified
separately
•
Risk of progression to complete heart block = high (>50%), as it is typically due to infranodal
block (usually in the His-Purkinje system) (all patients should be admitted for continuous
cardiac monitoring and treatment w/ pacemaker)
2:1 AV block
•
Inhibited conduction of every 2nd atrial depolarisation (P wave) to the ventricles (HR = ½ SAN
rate)
•
Cannot be classified as Mobitz I/II as only 1 PR interval is observed before the subsequent
dropped complex
•
Risk of progression to complete heart block = depends on the level of the block – block at the
level of the AVN (> common) – low; infranodal block (< common) – high
3rd degree AV block (complete heart block)
•
A complete disruption of AV conduction resulting in loss of communication between the atria
and ventricles (no conduction), causing them to beat independently of one another
•
P waves and QRS complexes have their own regular rhythm but bear no relationship to each
other (AV dissociation)
•
Risk of progression to cardiogenic shock/cardiac arrest = high; sudden onset 3rd degree AV
block can result in ventricular asystole, which lasts until an escape rhythm takes over
•
Escape rhythms = a myocardial electrical rhythm generated by ectopic pacemaker cells. They
can be generated by sites that are usually located near the AVN or the bundle of His
Ventricular escape rhythm = generated at the level of the bundle of His; HR 20-40
bpm; wide QRS complexes
Junctional escape rhythm = generated at the level of the AVN; HR 40-60 bpm; narrow
QRS complexes
•
Symptoms = dizziness, fatigue, breathlessness, Stokes-Addams attacks, Cannon A waves,
palpitations
Treatment
•
For unstable patients = interventional include atropine, transvenous/transcutaneous pacing,
inotropic meds (e.g. IV adrenaline); continuous investigations and definitive management
once the patient is stabilised
•
Stabilised patients = identify and treat the underlying cause; typically, no specific treatment if
asymptomatic and no infranodal block – outpatient screening and monitoring of progression
w/ periodic ECG’s.
o
For high-risk patients (Mobitz-II, 2:1, high-grade, 3rd grade AV block)= continuous
cardiac monitoring, admission for temporary pacing, permanent pacemaker w/ Holter
for all patients w/irreversible blocks
Bundle branch block
Definition = a defect of the bundle branches or fascicles in the electrical conduction system of the
heart. Results in QRS complex ≥0.12 s
•
RBBB = dysfunction of the R bundle of His → delayed R ventricle contraction
•
LBBB = cardiac conduction alteration in which there is a delay or obstruction of impulses sent
through the LBB pathway, leading to delayed L ventricle contraction.
Pathophysiology = BBB → transmission of impulse via remaining functional branch or fascicle →
slower ventricular depolarisation → long QRS complex
RBBB
•
An rsr’, rsR’ or rSR’ complex (lowercase letter = lower amplitude than normal) (forming a
characteristic “rabbit ears” or M shape) in leads V1, V2
•
Tall secondary R wave in V1
•
Wide, slurred S waves in leads I, V5, V6
•
Associated feature = ST depression and T wave inversion in V1, V2, and sometimes V3
•
Acronym = MarroW – because V1 can look like a “M”, and V6 makes a “W” – Marrow has
“RR” in the middle for R
LBBB
•
No R wave in lead V1
•
Deep S waves (forming a characteristic W shape)
•
Wide, notched R waves in leads I, aVL, V5, V6 (forming a characteristic M shape)
•
Loss of Q waves in the lat. leads
•
Acronym = WilliaM – because V1 can look like a “W”, and V6 makes a “M” – William has “LL”
in the middle for L
Bifascicular block
A RBBB w/either of the following:
•
L ant. fascicular block (common form) = L axis deviation, qR pattern in lead aVL
•
L post. fascicular block (rare) = R axis deviation, rS pattern in leads I and aVL, qR pattern in
leads III and aVF
Clinical manifestations = patients tend to be asymptomatic
Treatment = specific treatment is not usually required, although treatment for underlying disorder is
indicated
29) Rhythm abnormalities: Supraventricular arrhythmias –
classification, hemodynamics, clinical features
•
Cardiac arrhythmias = accelerated, slowed, or irregular HR caused by abnormalities in the
electrical impulses of the myocardium (OR an abnormality w/in either rate, rhythm, sequence
of conduction, or origin of conduction of electrical impulses of the myocardium)
•
Tachyarrhythmias = HR > 100 beats/min)
•
Supraventricular tachycardias (SVTs) = a group of tachyarrhythmias arising from
abnormalities in pacemaker activity and/or conduction involving myocytes of the atria and/or
AVN. The tachycardia is generated in either the SAN, AVN, atrial myocardium, or the bundle
of His above the bifurcation.
•
They are generally due to one of two mechanisms = re-entry or ↑ automaticity
↑ SNS tone = due to hypovolemia, hypoxia (anaemia, lung disease, PE),
sympathomimetic drugs (cocaine, amphetamines)
Metabolic activity = fever, hyperthyroidism
•
Physiologic sinus tachycardia = normal sinus mechanism precipitated by physical exertion,
stress, acute illness w/fever/infection/pain, hyperthyroidism, or pulmonary insufficiency
Definitions
•
Paroxysmal tachycardia = an arrhythmia w/an abrupt onset and termination that can last from
seconds to days (e.g. AV nodal re-entrant tachycardia)
•
Re-entry = a mechanism that causes an impulse in the heart (which would normally die out) to
return via conduction circuit to reexcite the tissue, leading to an extra beat (or, if it continues,
an ongoing tachyarrhythmia) – e.g. AVNRT and AVRT
•
Aberrant conduction = abnormal conduction of a myocardial impulse (due to e.g. BBB,
conduction delay, or an accessory pathway). It results in a wide QRS complex, as the
depolarisation of the ventricle happens > slowly (from myocyte to myocyte) rather than
through rapidly conducting Purkinje fibers
•
Ventricular preexcitation = premature activation of the ventricles by an accessory pathway
•
Pre-excitation syndrome = combo of ventricular preexcitation + associated arrhythmias; WPW
is the most common e.g.
Atrial flutter
Definition = a SV tachyarrhythmia that is usually caused by a macro re-entrant rhythm w/in the atria. It
is characterised by a regular, rapid atrial rate
Etiology = similar to A-Fib; may additionally result from the treatment of A-Fib (flecainide,
propafenone, amiodarone)
Pathophysiology
Type I (common; typical/isthmus-dependent flutter) = caused by a counter clockwise (> common) or
clockwise (< common) macro-reentrant activation of cardiac muscle fibers in the RA that travels along
the tricuspid annulus and passes through the cavotricuspid isthmus (between the IVC and the
tricuspid annulus)
Type II (rare; atypical atrial flutter) = various re-entrant rhythms that don’t involve the cavotricuspid
isthmus, are not well defined, and/or occur in the LA
Clinical manifestations
•
Most patients are asymptomatic
•
Less commonly = symptoms of arrhythmias, such as palpitations, dizziness, syncope, fatigue,
or dyspnoea
•
Tachycardia w/a regular pulse
•
Symptoms of the underlying disease (e.g. murmurs of mitral stenosis)
Diagnosis
ECG findings:
•
Rate = 75-150 bpm (depending on conduction)
•
Atrial rate ≥ ventricular rate
•
Regular, narrow QRS complexes
•
Rhythm may be regularly irregular (if flutter occurs w/a variable AV block occurring in a fixed
pattern – 2:1 or 4:1) or irregularly irregular (w/a variable block occurring in a non-fixed pattern)
•
Sawtooth appearance of P waves = identical flutter waves (F waves) that occur in sequence
at a rate of ~300/min (best seen in leads II, III, and aVF)
•
Predominantly negative deflections in leads II, III, and aVF
•
Flat deflections in I and aVL
Treatment = similar to A-Fib; rate control is > difficult to achieve than in A-Fib
Atrial fibrillation (A-Fib/AF)
Definition = the most common type of SV tachyarrhythmia characterised by uncoordinated atrial
activation that results in an irregular ventricular response.
Etiology
The exact causes are unknown, but several risk factors have been identified:
•
Cardiovascular risk factors = advanced age, HT, DM2, smoking, obesity, sleep apnoea
•
Intrinsic cardiac disorders = CAD, valvular heart disease (especially mitral valve disease),
CHF, WPW syndrome, sick sinus syndrome, cardiomyopathies, pericarditis
•
Non-cardiac disorders = pulmonary disease (COPD, PE, pneumonia), hyperthyroidism,
catecholamine release and/or ↑ sympathetic activity (sepsis, pheochromocytoma, cocaine,
amphetamines), electrolyte imbalances (hypomagnesemia, hypokalemia), drugs (adenosine,
digoxin), excess alcohol consumption, chronic kidney disease
MNEMONIC = PARASITE to remember the major risk factors for A-Fib = Pulmonary disease,
Anaemia, Rheumatic heart disease, Atrial myxoma, Sepsis, Ischaemia, Thyroid disease, Ethanol
Classification
A-Fib can be classified according to:
•
Haemodynamic stability
Unstable A-Fib = A-Fib manifesting w/signs of hemodynamic instability (e.g. chest
pain, altered mental status, acute pulmonary oedema, hypotension, or cardiogenic
shock)
Stable A-Fib = A-Fib w/out signs of hemodynamic instability
•
Ventricular rate
A-Fib w/rapid ventricular response = rate > 100-110 bpm (tachycardic A-Fib)
A-Fib w/slow ventricular response = rate < 60 bpm (bradycardic/slow A-Fib)
•
Onset and duration
New-onset A-Fib = new presentation or diagnosis of A-Fib, regardless of duration
Paroxysmal A-Fib = A-Fib that resolves w/in 7 days of onset either following treatment
or spontaneously; the frequency of recurring episodes may vary
Persistent A-Fib = continuous A-Fib for >7 days
Long-standing persistent A-Fib = continuous A-Fib for >1 year
Permanent A-Fib = persistent A-Fib in which therapeutic attempts are no longer made
to convert to or maintain sinus rhythm unless the patient and the treating physician
agree to do so
•
Method of detection
Clinical A-Fib = an episode of A-Fib lasting ≥30 sec that is documented on a surface
ECG; may be symptomatic or asymptomatic
Subclinical A-Fib = asymptomatic A-Fib not previously detected on a surface ECG that
is discovered on implanted cardiac devices and confirmed on Intracardiac
electrograms
•
Mitral valve involvement
Valvular A-Fib = A-Fib in patients w/moderate-severe mitral valve stenosis or an
artificial (mechanical) heart valve
Non-valvular A-Fib = A-Fib in patients w/out moderate-severe mitral valve stenosis or
an artificial (mechanical) heart valve
Pathophysiology
The exact mechanisms are not well understood. Suggested mechanisms include:
•
Volume overload, hemodynamic stress → atrial hypertrophy and/or dilatation
•
Atrial ischaemia
•
Inflammation of the atrial myocardium
•
Altered ion conduction by the atrial myocardium
The new onset of A-Fib triggers a vicious circle that can ultimately lead to long-standing A-Fib w/atrial
remodelling:
•
A-Fib is triggered by 1/both of the following:
Bursts of electrical activity from automatic foci near the pulmonary vv. or in diseased,
fibrotic atrial tissue
Pre-excitation of the atria as a result of aberrant pathways (e.g. WPW)
•
A-Fib is sustained by re-entry rhythms and/or rapid focal ectopic firing. Re-entry rhythms are >
likely to occur w/enlarged atria, diseases heart tissue, and/or aberrant pathways
•
Atrial remodelling = electrophysiological changes in the atria occur w/in a few hours of A-Fib
onset (electrical modelling); if A-Fib persists, atrial fibrosis and dilatation (structural
remodelling) occur w/in a few months. Electrical and structural remodelling ↑ susceptibility to
A-Fib, resulting in a vicious cycle
Effects of A-Fib = the atria contract rapidly but ineffectively and in an uncoordinated fashion → stasis
of blood w/in the atria → risk of thromboembolism and stroke. Irregular activation of the ventricles by
conduction through the AVN → tachycardia
Clinical manifestations
•
Most patients are asymptomatic
•
Less commonly = symptoms of arrhythmias, such as palpitations, dizziness, syncope, fatigue,
or dyspnoea
•
Symptoms of the underlying disease (e.g. murmurs of mitral stenosis)
•
Tachycardia w/an irregularly irregular pulse
•
Apex-pulse deficit = difference between the rate of apex heart beat and that of the peripheral
pulse. Manifests when only some cardiac contractions are strong enough to transmit a pulse
wave to the periphery; n.o of cardiac contractions (perceived w/stethoscope/palpated on the
chest) is higher than peripheral pulse rate (e.g. radial a.)
•
Complications of long-standing A-Fib = acute L HF → pulmonary oedema; thromboembolic
events (stroke/transient ischaemic attack, renal/splenic infarct, intestinal/acute limb
ischaemia); life-threatening ventricular tachycardia
Diagnosis
ECG findings
•
Rhythm = irregularly irregular RR intervals
•
Rate = variable; tachycardia is common; atrial rate > ventricular rate
•
P waves = P waves are indiscernible; fibrillatory waves (f waves) are seen instead at 300600/min (prominent, coarse f waves w/higher amplitudes in leads V1, II, III, and aVF in recentonset A-Fib; low amplitude in long-standing A-Fib); PR intervals are not distinguishable
•
QRS complex = typically narrows QRS complex (< 0.12 sec); broad complexes may be seen
in aberrant conduction or in complete AV block
Others
•
Lab studies = assess CBC, electrolytes, BUN, TSH and FT4, LFT, troponin levels, BNP,
toxicology
•
Transthoracic echocardiogram = indicated for all patients w/new-onset A-Fib to assess
cardiac function and rule our underlying structural cardiac disease (e.g. mitral stenosis)
•
CXR = to evaluate for pulmonary disease or HF
•
Cardiac stress test = if underlying IHD is suspected
•
Electrophysiological study
•
Sleep study = if sleep apnoea is suspected
Treatment
•
Unstable patients = emergent electrical cardioversion
•
For stable patients, the goal is to control HR and/or rhythm
Rate control
•
Pharmacological options = BB (metoprolol, atenolol) or non-dihydropyridine CCB (diltiazem,
verapamil) are 1st line; digoxin is 2nd line; amiodarone is 3rd line
•
Surgical options = AV nodal ablation and implantation of a permanent ventricular pacemaker –
eliminates need for meds but leads to lifelong dependence on a pacemaker
Rhythm control (i.e. cardioversion)
•
Goal = termination of A-Fib (or flutter) and restoration of sinus rhythm in order to prevent atrial
remodelling and improve symptoms
•
Contraindications = long-standing A-Fib, reversible causes, high risk of thromboembolic
events
•
Initiate anticoagulation before cardioversion to ↓ the risk of stroke
•
Following cardioversion, consider daily anti-arrhythmic drugs to maintain sinus rhythm
•
Electrical cardioversion = gradually ↑ strengths of direct current shock (synchronised w/the R
wave) are administered under procedural sedation until sinus rhythm is restored. Can be
performed in an emergency in unstable patients or selectively in stable patients
•
Pharmacological cardioversion = guidelines suggest flecainide, propafenone, and sotalol as
1st line therapy in patients w/out heart disease patients w/CHF can be started on amiodarone
or dofetilide
•
Interventional cardioversion = creation of scar tissue that prevents the spread of ectopic
impulses
Anticoagulation (before cardioversion)= for A-Fib <48 hrs and unstable A-Fib give heparin or DOAC;
for stable A-Fib of unknown duration or ≥48 hrs give DOACs or warfarin (w/a goal INR of 2-3)
AV-nodal re-entrant tachycardia (AVNRT) (most common type of PSVT)
Definition = a tachyarrhythmia caused by a dysfunctional AVN that contains 2 electrical pathways,
which form a re-entry circuit
Pathophysiology
•
The AVN contains 2 electrical pathways, 1 fast and 1 slow → the electrical impulse circles
around the AVN w/in both pathways → a continuous circuit conducts impulses to the
ventricles → tachycardia
•
~90% of cases (typical AVNRT) are due to anterograde conduction across the slowconducting pathways and retrograde conduction in the fast pathway (although the reverse is
possible – atypical AVNRT)
Clinical manifestations = sudden development of rapid regular palpitations, dizziness
Diagnosis (ECG findings)
ECG may be normal between episodes of tachycardia. Findings may be indistinguishable from those
of orthodromic AVRT and include:
•
HR typically 150-220 bpm
•
Typically narrows QRS complex (wide QRS may be seen if there is aberrant conduction)
•
Regular rhythm
•
P wave is typically absent (it falls or is “buried” in the QRS complex)
Treatment
Acute management
•
Hemodynamically unstable = electrical cardioversion
•
Hemodynamically stable w/narrow QRS complex = vagal manoeuvres (1st step); IV meds if
SVT persists (adenosine is 1st line; alternatively non-dihydropyridine CCB or BB)
•
Hemodynamically stable w/wide QRS complex = AV nodal blocking agents are safe if there is
an established diagnosis of AVNRT
Long-term management
•
Infrequent and mild episodes may be managed w/self-guided vagal manoeuvres
•
1st line = percutaneous catheter ablation of the slow pathway (ablation of fast pathway is
associated w/higher incidence of AV block)
•
2nd line = drugs – BB, verapamil, or diltiazem; flecainide or propafenone
AV re-entrant tachycardia (AVRT) (AKA AV reciprocating tachycardia)
Definition = a tachyarrhythmia caused by an accessory pathway that creates a re-entrant circuit w/the
AVN. WPW is a common cause of AVRT but they are not synonymous.
Pathophysiology
Accessory pathways may be manifest or concealed:
•
Manifest pathways = can conduct in both anterograde (atrium → ventricle) and retrograde
(ventricle → atrium) directions. Anterograde conduction is > common and leads to
preexcitation seen on the ECG in sinus rhythm
•
Concealed pathways = can conduct only in a retrograde direction; not visible on ECG in sinus
rhythm
There are 2 types of AVRT; the direction of the impulses helps distinguish between them:
•
Orthodromic AVRT (most common – 90-95%) = anterograde conduction through AVN (narrow
QRS); retrograde conduction through accessory pathways. It can occur w/a
concealed/manifest pathway
•
Antidromic AVRT (rare – 5-10%) = anterograde conduction through accessory pathways;
retrograde conduction through AVN. Wide QRS complex, as ventricular depolarisation
happens slowly from myocyte to myocyte rather than through the rapid His-Purkinje system.
only occurs w/a manifest pathway
Diagnosis (ECG findings)
•
HR = 150-250 bpm
•
Regular rhythm
•
QRS complex = narrow in orthodromic; wide in antidromic
•
P wave = P wave typically follows QRS in orthodromic; short PR interval in antidromic
•
Orthodromic AVRT = Because the AP is conducting in a retrograde direction, there is no
visible delta wave during the tachyarrhythmia; can be indistinguishable for AVNRT
•
Antidromic AVRT = the morphology of the QRS complex means that the delta wave is
frequently not visible
Treatment = same as AVNRT
Wolff-Parkinson-White syndrome (WPW)
Definition = a congenital condition characterised by intermittent tachycardias and signs of ventricular
pre-excitation on ECG, both of which arise from an accessory pathway known as the bundle of Kent
Pathophysiology
•
A congenital accessory pathway, the bundle of Kent, connects the atria and ventricles,
bypassing the AVN and leading to ventricular pre-excitation
•
Accessory pathway = an abnormal electrical connection outside the AVN that allows for
propagation of impulses between the atrial myocardium and the ventricle)
•
May be associated w/structural abnormalities of the heart, in particular Ebstein anomaly
•
~10% of patients have multiple accessory pathways (> common w/coexisting structural heart
disease)
•
May be asymptomatic (WPW pattern) or associated w/arrhythmias (WPW syndrome)
including AV reciprocating tachycardia (most common; 80%), A-Fib (15-35%), atrial flutter
(5%)
Clinical manifestations = SOB, peripheral oedema, nocturia, pronounced neck vv., palpitations,
tachycardia, fatigue, weakness, fainting
Diagnosis (ECG findings)
•
While in sinus rhythm, a pre-excitation pattern may be present = short PR interval, ECG delta
wave (a slurred upstroke at the start of the QRS complex, secondary to pre-excitation),
widened QRS
•
Can show any of the arrhythmias associated w/WPW
Treatment
Electrophysiological studies are used for risk stratification and to establish presence and location of
an accessory pathway; catheter ablation of the accessory pathway is the 1st line treatment. Meds
would include non-dihydropyridine CCBs or BB, or class III anti-arrhythmic drug (amiodarone or
sotalol); if there is no associated heart disease = flecainide or propafenone
30) Treatment of supraventricular arrythmias
General principles:
•
Pulseless patients require CPR
•
Patients with unstable tachycardia with pulse require - electrical cardioversion.
•
Stable patients:
o Vagal manoeuvres: Valsalva manoeuvre, Carotid massage
o
o
Medical therapy.
Catheter ablation.
Treatment of AVNRT- and AVRT
•
Acute management
o
o
o
•
if Pulseless CPR
Hemodynamically unstable cardioversion
Hemodynamically stable
narrow complex Vagal maneuver, medical (adenosine, verapamil, diltiazem,
metoprolol)
wide QRS complex
Long term management
•
infrequent and mild episodes may be managed with self-guided vagal maneuvers.
o 1st line – percutaneous catheter ablation of the slower pathway
o AVNRT= 2nd line - Pharmacological therapy-
o
o
BB - propranolol 10-40mg x3
Verapamil 40-160mg x3
Diltiazem 300120mg x3 /extended release 120-360 once
AVRT- if preexcitation pattern exist.
Known heart disease - Sotalol 40-160mg every 12h
No heart disease – Propafenone 150-300mg x3, Felcainide 50-150mg every
12h
AVRT- if preexcitation patterns not visible verapamil, diltiazem, metoprolol. Alternative
amiodarone
Treatment of WPW
•
AV nodal blocking agents and vagal maneuvers are contraindicated
•
Acute Cardioversion/ iv procainamide
•
Long term ablation of extra pathway
Treatment of focal atrial tachycardia
•
Acute same as for AVNRT
•
Long term Catheter ablation
•
Medications- Metoprolol, verapamil, diltiazem
•
Pacemaker implantation
Treatment of multifocal atrial tachycardia
•
Management of underlying causes
o
Manage exacerbations of chronic diseases
Correct reversible conditions, e.g., hypoxemia, acidosis, electrolyte
abnormalities.
Discontinue potential offending medications.
IV magnesium may be helpful even in patients with normal magnesium levels.
•
Rate control
o Beta blockers-Metoprolol
o Calcium channel blockers-Verapamil
•
AV node radiofrequency ablation: Consider in refractory MAT.
Treatment of Atrial fibrillation and flutter
•
Unstable patients Cardioversion
•
Stable patients control heart rate or rhythm
o Onset > 48h – rate control
o Onset< 48h – consider rate or rhythm control
Use CHA2DS2VASC to assess the risk of thromboembolism
If intermediate or high risk – start anticoagulants- Heparin (80 units), LMWH, or direct oral
anticoagulants (dabigatran, rivaroxaban)
Rate control
•
The goal is to normalize the ventricular heart rate to reduce symptoms.
•
Target resting heart rate
o
o
•
< 110/minute: for patients who remain asymptomatic or have normal LV systolic
function
< 80/minute: for patients who continue to be symptomatic with a lenient rate
First-line
o Beta blockers (e.g., metoprolol 2.5-5mg iv, atenolol , propranolol 1mg iv repeated
every 2 mins)
Preferred when Afib is due to hyperthyroidism and in pregnant patients
Avoid in patients with COPD.
o Nondihydropyridine calcium channel blockers(e.g., diltiazem 0.25mg\kg iv,
verapamil 0.075-0.15mg\kg iv)
Avoid in patients with decompensated heart failure (LV systolic dysfunction/low
ejection fraction).
Can be safely used in heart failure with preserved normal LV systolic function.
•
Second line: digoxin
•
Third line: amiodarone
•
AV nodal ablation and implantation of a permanent ventricular pacemaker
Rhythm control
•
Electrical cardioversion
o Gradually increasing strengths of direct current shock (synchronized with the R wave)
are administered under procedural sedation until sinus rhythm is restored.
•
Pharmacological cardioversion
o
Inpatient regimens using intravenous or oral antiarrhythmics:
Dofetilide 125-500mcg PO every 12h
Ibutilide 1mg iv
Flecainide 200-300mg PO
Propafenone 450-800mg PO or 150mg iv
Amiodarone 600-800mg PO
•
Interventional cardioversion
o Description: Creation of scar tissue that prevents the spread of ectopic impulses.
o Catheter radiofrequency ablation of atrial tissue
31) Rhythm abnormalities: Ventricular arrhythmias
Premature ventricular contractions (PVCs) (AKA PV beats)
Definition = extra, abnormal heartbeats caused by ectopic foci w/in the ventricles
Etiology = idiopathic; cardiovascular disease (CAD, myocarditis); electrolyte imbalances
(hypokalemia, hypomagnesemia); certain drugs (digoxin, psychiatric meds); caffeine; alcohol
Classification
•
Monomorphic PVC = each PVC has the same configuration → identical origin
•
Polymorphic PVC = PVCs have different configuration → multiple foci
Clinical manifestations
•
Most patients are asymptomatic
•
Skipped beats (due to a compensatory pause after a PVC)
•
If frequent PVCs, possible → light-headedness, dizziness, palpitations, irregular heartbeat
Diagnosis
ECG
•
Common = QRS >0.12 sec w/a block-line QRS morphology; PVCs are often followed by a
compensatory pause
•
May be random/adhere to a specific pattern, including = single PVC, couplet, triplet (3 in a
row), bigeminy (1 extrasystole after every single sinus beat), trigeminy (1 extrasystole after
every 2 sinus beats)
Additional procedures (indicated in case of frequent, symptomatic PVCs) = 24-hr Holter monitoring,
exercise stress test, echocardiography
Treatment = most patients don’t require any treatment; treat any underlying disease; only treat
frequent and significantly symptomatic PVCs w/antiarrhythmic agents or w/catheter ablation if meds
fail
Ventricular tachycardia (VT)
Definition = a potentially life-threatening arrhythmia originating in the cardiac ventricles
Classification
Ventricular tachycardia = ≥3 consecutive ventricular complexes (wide QRS complex) at a frequency
of ≥100 bpm. it can be classified by duration or morphology
•
Non-sustained ventricular tachycardia (NSVT) = VT lasting <30 sec w/spontaneous
termination
•
Sustained VT = VT lasting ≥30 sec or VT causing hemodynamic instability w/in 30 sec
•
Monomorphic VT = QRS morphology similar in all beats, indicating a single arrhythmogenic
focus
•
Polymorphic VT = QRS morphology varies in each beat, indicating multiple arrhythmogenic
foci
Premature ventricular complex = <3 consecutive ventricular complexes often followed by a
complete compensatory pause
Electrical storm = ≥3 episodes of sustained tachycardia/defibrillations w/in 24 hrs
Etiology
Cardiac causes
•
Cardiac scars = secondary to MI or cardiac surgery
•
Myocardial ischemia = secondary to angina
•
Inflammatory causes = myo-/endocarditis, rheumatic heart disease
•
Idiopathic
•
Conduction disorders = inherited cardiomyopathies or inherited arrhythmia syndromes
(channelopathies)
Extracardiac causes
•
Acquired long QT syndrome = drug-induced QT prolongation (class I and III antiarrhythmics,
macrolides, fluoroquinolones); electrolyte imbalances (hypokalemia, hypomagnesemia,
hypocalcaemia)
•
Certain drugs = digoxin toxicity, antiarrhythmics, recreational drugs (cocaine)
Pathophysiology
VT can result from an alteration in myocardial automaticity, electrical conduction, or ventricular
repolarisation secondary to several factors
•
Monomorphic VT = ↑ automaticity, re-entry circuit
•
Polymorphic VT = abnormal ventricular repolarisation (e.g. due to long QT syndrome, drug
toxicity, electrolyte imbalances)
Effect = asynchronous atrial and ventricular beats and rapid ventricular rhythm → ↓ blood flow into
the ventricle during diastole → ↓ CO. consequent hemodynamic compromise → symptoms of
syncope, MI, angina
Clinical manifestations
•
Often asymptomatic, especially in NSVT
•
Cardiovascular features = palpitations, tachycardia, chest pain/pressure,
dyspnoea/orthopnoea, symptoms of ↓ CO (dizziness, hypotension, syncope, cardiogenic
shock and loss of consciousness), cardiac arrest
•
Symptoms may be unprovoked or exacerbated by physical and/or emotional triggers
Diagnosis
ECG findings
•
Rate = ≥100 bpm
•
Rhythm = typically regular
•
QRS complexes = >0.12 s (3 small squares); mono/polymorphic VT
•
Signs of AV dissociation = dissociated P waves (no relationship between P waves and QRS),
fusion complexes (mixed QRS morphology containing components of a ventricular complex
and a normal sinus QRS morphology), capture beats (seen occasionally)
Lab studies = electrolytes, serum magnesium levels, toxicology screen, drug levels, troponin, BNP
Imaging (to evaluate for structural cardiac defects) = echocardiography (1st line), MRI (to assess for
myocardial scarring and infiltrative diseases), cardiac CT (can assess coronary aa.)
Additional tests include exercise stress test, Holter monitoring, and coronary angiography.
Treatment
•
Treat underlying diseases and correct any reversible causes (electrolyte imbalances, drug
toxicity)
•
Long-term management = BB (↓ risk of sudden cardiac death) are 1st line; other drugs
(amiodarone, sotalol, flecainide, non-dihydropyridine CCB) may be combined w/BB if
symptoms persist.
•
Implantable cardioverter-defibrillator (ICD) = used to terminate episodes of VT in order to
prevent sudden cardiac death; typically combined w/pharmacological therapy; may be used
for primary/secondary VT prevention
•
Ablation (radiofrequency catheter ablation or surgical ablation) = potential curative treatment
for VT; following an electrophysiological (EP) study, the arrhythmogenic focus is ablated
Torsades de pointes tachycardia
Definition = a type of polymorphic VT occurring in patients w/a prolonged QT interval
Etiology = congenital long QT syndrome (LQTS), acquired LQTS
Clinical manifestations = similar to VT
Diagnosis
•
Lab and imaging = same as VT
•
ECG findings = polymorphic VT w/QRS complexes that typically appear to twist around the
isoelectric line, usually in self-limiting bursts; often preceded by bigeminy (every normal
complex is followed by a premature complex) and followed by several premature ventricular
contractions; R-on-T phenomenon may also be seen
Treatment
•
Hemodynamically unstable patients = defibrillation + CRP; stable patients = IV magnesium
sulphate
•
Identify and treat the underlying etiology of QT prolongation = restrict the use of drugs that
cause QT prolongation, avoid electrolyte imbalances
•
Long-term management = consider BB to ↓ risk of sudden cardiac death; consider ICD
implantation or L cardiac sympathetic denervation if BB aren’t effective
Ventricular fibrillation (V-Fib)
Definition = a life-threatening cardiac arrhythmia characterised by disorganised, high-frequency
ventricular contractions that result in diminished CO and hemodynamic collapse
Etiology
•
Underlying cardiovascular disease = CAD (most common); previous MI, myocarditis,
cardiomyopathy, severe CHF, heart valve disease
•
Congenital heart defects (e.g. pulmonary atresia)
•
Electrolyte imbalances (e.g. hypokalemia, hyperkalemia)
•
Electrophysiologic disorders = WPW syndrome, LQTS → torsade de pointes
Pathophysiology
•
Normal electrical conduction can be disrupted by re-entry → chaotic, circulating excitation of
the myocardium (= V-Fib) → simultaneous contractions at multiple foci → insufficient CO →
hemodynamic collapse → loss of consciousness and possible death (sudden cardiac death)
•
Re-entry excites areas of the myocardium that have previously been activated (w/in the sake
conduction cycle) and are out of the refractory period (and ∴ excitable again)
•
Re-entry can be caused by = changes to the conduction pathways (e.g. unexcitable scar due
to past MI), abnormal patters of excitation (e.g. LQTS, premature ventricular complex)
Clinical manifestations = possible early signs (non-specific) include chest pain, palpitations, fatigue,
dyspnoea, dizziness; ultimately loss of consciousness and death
Diagnosis
ECG
•
Commonly preceded by VT
•
General appearance = arrhythmic, fibrillatory baseline, usually >300 bpm; erratic undulations
w/indiscernible QRS complexes; no atrial P waves
•
Ventricular flutter = ventricular rates of ~240-300 bpm; frequently transitions to V-Fib
Evaluation of underlying conditions (during or directly after initial management):
•
ECG
•
Labs = cardiac enz., electrolytes, TSG, drug levels and toxicology screen, ABGs
•
Imaging = coronary angiography, echocardiography, nuclear imaging
Treatment
•
Resuscitation for V-Fib = advanced cardiac life support; if V-Fib doesn’t respond to the
standard protocol (refractory V-Fib), consider admin of lidocaine, procainamide, or
magnesium
•
Post-resuscitation care = intensive care monitoring, maintain application of anti-arrhythmic
that were used during successful resuscitation (usually Iv amiodarone/lidocaine), consider
admin of BB, treat underlying causes; ICD
32) Treatment of ventricular arrythmias
Ventricular tachycardia
Sustained:
•
Assess for hemodynamic stability and signs of unstable tachycardia
•
Attach defibrillator pads to unstable patients and use cardioverter-defibrillator or bedside
monitor to obtain a rhythm strip for rapid assessment.
•
Hemodynamically unstable patients
o Pulseless VT CPR and defibrillation as soon as possible
o Polymorphic VT defibrillate
o Monomorphic VT → electrical cardioversion.
•
Hemodynamically stable patients
o
o
1st line- pharmacological conversion with antiarrhythmics
Prolonged QT – Amiodarone 150mg IV
No QT prolongation - Procainamide 20-50mg/min or Satolol
Refractory VT- electrical conversion
Non sustained:
•
Treat reversible causes if identified
o correct electrolyte imbalance, stop drugs that prolong QT
Long term management for sustained and non-sustained VT
•
Pharmacological therapy –
o B-blockers
o Class lc of Class VI antiarrhythmics
may be combined with B-blockers.
•
Automated implantable cardioverter defibrillator (AICD)
o
•
used for recurrent VT
Ablation (For recurrent VT, antiarrhythmics, not tolerated)
o Radiofrequent ablation or
o Surgical
Treatment of premature ventricular contractions.
•
Most patients do not require any treatment
•
Treat any underlying disease (CAD. myocarditis)
•
Only frequent and symptomatic PVCs are treated
o Anti-arrhythmic therapy
o
Catheter ablation
Treatment of Torsades de pointes
•
Hemodynamically unstable defibrillation + CPR
•
Hemodynamically stable magnesium sulphate 1-2g iv
o
•
identify and treat the underlying etiology of QT prolongation
restrict or withdraw QT prolonging drugs
Maintain electrolyte balance
Treat hypoxia with O2
Check and treat Hypothyroidism
Long term management o consider B-blockers to minimize the risk of sudden cardiac death
o consider AICD or left cardiac sympathetic denervation if QT prolongation presists.
o In case congenital QT prolongation
Avoid activities that stress the heart
Avoid cold temp (swimming, skiing)
o
o
1st line: Beta blockers: propranolol
AICD and left cardiac sympathetic denervation
Treatment of Ventricular Fibrillation
•
Resuscitation
o Advanced Cardiac Life Support
CPR, Rhythm and pulse check
Defibrillation Resume CPR
If 2nd cycle of defibrillation is unsuccessful IV access
After 2nd cycle
•
Epinephrine 1mg iv
After 3rd unsuccessful cycle
•
Amiodarone 300mg iv OR
o
•
• Lidocaine 1-1.5 mg/kg iv
if V-Fib does not respond to standard ACLS
lidocaine, procainamide, magnesium
Post resuscitation care →
o intensive care monitoring
Management of vital signs and removal of acute metabolic imbalance
Mild therapeutic hypothermia
Maintain application of antiarrhythmics that were used during the resuscitation
•
usually, iv amiodarone or iv lidocaine
consider Beta blockers
ICD if high risk for recurrence.
33) Anti-arrhythmic drugs: classification, dosage
Anti-arrhythmic drugs are classified according to their effects on the AP of cardiac cells and their
presumed mechanism of action.
Class I – Na+ channel blockers
Na+ channel blockers have a membrane stabilising or anaesthetic effect on the cells of the
myocardium. They slow the rate and amplitude of phase 0 depolarisation; reduces cell excitability;
and reduces conduction velocity. Class I agents are divided into 3 groups based on their effect on the
length of the AP:
•
IA = lengthens the AP (R shift) – e.g. quinidine, disopyramide (IR 300-800 mg daily; MR 250375 mg every 12 hours)
Used in ventricular arrhythmias and prevention of recurrent paroxysmal atrial fibrillation
Rapidly and completely absorbed after oral administration; extensive 1st pass
metabolism
Side effects = blurred vision, headaches, tinnitus, disorientation, and psychosis
(symptoms of cinchonism)
•
IB= shortens the AP (L shift) – e.g. lidocaine (1-4 mg/min or 50-150 mg IV LD), phenytoin
Used for treatment of ventricular tachycardia and fibrillation during and immediately
after MI
i.v. administration to avoid 1st pass metabolism
Side effects = nystagmus, drowsiness, slurred speech, paresthesia, confusion.
•
IC = don’t significantly affect the AP (no shift) - e.g. flecainide (initially 50 mg 2X/day, ↑ up to
300 mg if necessary. For ventricular arrhythmias = 100 mg 2X/day 3-5 days) and propafenone
(150 mg 3X/day; 300 mg 2X/day – max 300 mg 3X/day)
Used to prevent paroxysmal atrial fibrillation and recurrent tachyarrhythmias. Reserved
for patients who don’t have significant CAD/LV dysfunction
Flecainide is absorbed orally and metabolised by the liver. Useful for supraventricular
and ventricular arrhythmias. Propafenone also has hepatic metabolism, and the
metabolites are excreted in the urine and faeces.
Side effects = blurred vision, dizziness, nausea. Propafenone may also cause
bronchospasm – should be avoided in asthma patients
Class II – β blockers
•
Useful in treating tachyarrhythmias caused by ↑ sympathetic activity. Also useful for atrial
flutter and fibrillation. They prevent ventricular arrhythmias following a MI
•
Predominant action on the SAN
•
Metoprolol (50 mg 2-3X/day) is the most widely used in treatment of cardiac arrhythmias.
•
Propranolol (10-40 mg 3-4X/day) has membrane stabilising effect however it is non-selective
= ↑ risk of bronchospasm (metoprolol is selective therefore has ↓ risk)
•
Extensively metabolised in the liver
•
Esmolol (50-200 μg/kg/min) is very short acting and is used for IV administration in acute
arrhythmias that occur during surgery/emergency situations. It has a fast onset of action and a
short HL = ideal for acute situation and also limits is adverse effect profile.
•
Side effects = photosensitivity, skin pigmentation, thyroid disturbances, liver disease
Class III – K+ channel blockers (e.g. Amiodarone – main, sotalol, dronedarone)
•
Mechanism of action = prolongation of the AP duration and the refractory period by blocking
K+ channels.
•
Therapeutic uses = treatment of severe refractory supraventricular and ventricular
tachyarrhythmias
Amiodarone = by mouth 200 mg 3X/daily for 1 week, then 200 mg 2X/day for 1 week,
followed by a maintenance dose, usually 200 mg daily or the minimum dose to control
arrhythmia. For IV = 5 mg/kg over 20-120 mins w/ECG monitoring, max 1.2 g/day
Sotalol = 80 mg daily in 1-2 divided doses, then ↑ to 160-320 mg daily in 2 divided
doses
•
Pharmacokinetics = incompletely absorbed after oral administration; long HL (several
weeks); distributes extensively in adipose tissue
•
Side effects = pulmonary fibrosis, hepatotoxicity, corneal deposits, blue-gray skin
discolouration, and hypo- or hyperthyroidism (amiodarone contains iodine and is structurally
related to thyroxine)
•
Use of low doses and close monitoring reduce toxicity, while retaining clinical efficacy
Class IV – Ca2+ channel blockers
•
Class IV drugs are the non-dihydropyridine Ca2+ channel blockers verapamil (40-120 mg
3X/day or IV 5-10 mg over 2 mins, 3 for elderly) and diltiazem.
•
They decrease conduction through the AVN, and shorten phase 2 (plateau) of the AP. They
thus reduce contractility, so may
be inappropriate in heart failure
•
Use = for supraventricular
arrhythmias
•
Both drugs are metabolised in the
liver and side effects = headache,
ankle oedema, constipation.
Class V – other agents
•
Digoxin = inhibits Na/K ATPase - ↑
myocardial contractility
•
Adenosine = slows conduction
time through the AVN and
interrupts re-entry pathways
through the AVN, and restores
normal sinus rhythm in patients w/supraventricular tachycardias
34) Hypertension (HT)
Definition = long-term medical condition in which the BP in the aa. is persistently elevated (>140/90
mmHg). Can lead to CAD, stroke, heart failure, peripheral vascular disease, vision loss. Classified
into primary and secondary HT
Category
Systolic pressure
(mmHg)
Diastolic pressure
(mmHg)
Hypotension
<90
and/or
<60
Optimal
<120
and
<80
Normal
120-129
and/or
80-84
High normal/pre-HT
130-139
and/or
85-89
Stage I
140-159
and/or
90-99
Stage II
160-179
and/or
100-109
Stage III
≥180
and/or
≥110
Isolated systolic HT
≥140
and
< 90-110
Classification and Etiology
Primary (essential) HT
Definition = form of HT that has no identifiable cause. It is the most common type, affecting 95% of
hypertensive patients; it tends to be familial and is likely to be the consequence of an interaction
between environmental and genetic factors
Risk factors include:
•
Non-modifiable = +ve family history, ethnicity, advanced age
•
Modifiable = obesity, DM, smoking, excessive alcohol, diet high in Na+/low in K+, physical
inactivity, psychological stress
Secondary HT
Definition = HT caused by an identifiable underlying primary cause; accounts for 5-10% of cases of
HT in adults
•
Renal = renal a. stenosis, glomerulonephritis
•
Endocrine = Cushing syndrome, hyperthyroidism, Conn syndrome
•
Coarctation of the aorta
•
Estrogen = oral contraceptives
•
Neurologic = ↑ ICP, psychostimulant use
•
Treatment = glucocorticoids, NSAIDs
•
MNEMONIC = RECENT
Subtypes include white coat HT (HT detected only in clinical settings or during BP measurement at
the GP) which is due to anxiety experienced by the patient; isolated systolic HT which can occur in
the elderly or secondary to ↑ CO; and masked HT (normal office BP, high ambulatory/home BO).
Pathophysiology
•
CO and peripheral resistance are the 2 determinants of arterial pressure
•
CO is ↑ early in the disease course,
w/total peripheral resistance (TPR)
normal; over time CO drops to normal
levels but TPR is ↑. 3 theories have
been proposed to explain this:
Overactive RAAS leads to VC
and retention of Na and H2O.
The ↑ in blood volume leads
to HT
An overactive SNS, leading to ↑ stress responses
Polygenic cause
Clinical manifestations
HT is usually asymptomatic until:
•
Complications of end-organ damage arise
•
Or an acute ↑ in bp occurs (hypertensive crisis)
Secondary HT usually manifests w/symptoms of the underlying disease (e.g. abdominal bruit in
renovascular disease, oedema in CKD, daytime sleepiness in obstructive sleep apnoea). Nonspecific symptoms are:
•
Headaches (especially early morning) – pain/tightness at the back of the head
•
Fatigue, sleep disturbances, drowsiness
•
Vertigo, nausea, blurred vision
•
Epistaxis (nose bleeds)
•
Chest discomfort, palpitations
•
Strong, bounding pulse on palpitation
•
Nervousness
Diagnosis
BP monitoring = repeated measurements on both arms – HT is diagnosed if the av. BP on at least 2
readings obtained on at least 2 separate visits is elevated. Also, can do long-term measurement of
BP (24 hours)
Treatment
35) Arterial hypertension – treatment
Treatment Algorithm:
Office Blood pressure target values:
•
18-65yrs: SBP (120-130mmHg) NOT <120, DBP (70-79)
•
≥ 65yrs: SBP (130-139mmHg), DBP (70-79)
Lifestyle interventions:
Interventions
Target
Weight loss
Ideal body weight
Diet
DASH diet (Diet approach to stop HT)
Diet rich in fruits, vegetables and whole
Low in saturated and trans fats
< Dietary sodium
<5g/day
Increase dietary potassium (except w/ CKD)
Restrict alcohol consumption
Regular aerobic exercise
Smoking cessation
Pharmacological treatment:
<14U/wk – Men
<8U/wk - Women
At least 30min of moderate activity for 5-7days/wk
Special populations:
•
HT + CAD: ACEi/ARB + BB/CCB OR CCB + (t)diuretic/BB OR BB + diuretic
•
HT + CKD: ACEi/ARB + CCB OR ACEi/ARB + (t)diuretic (or loop diuretic)
•
HT + HFrEF: ACEi/ARB + (t)diuretic (or loop diuretic) + BB (+ spironolactone in step 2)
o
Avoid n-DHP CCBs
•
HT + Afib: ACEi/ARB + BB/n-dhp CCB OR BB + CCB
Step 2: ACEi/ARB + BB + DHP-CCB/(t)diuretic OR BB + DHP CCB + (t)diuretic
•
HT + Diabetes: ACEi/ ARB
•
HT + Asthma: ARBs, CCB, OR thiazide diuretics (avoid BB)
•
HT + Osteoporosis: Thiazide diuretics
•
HT + Gout: ARBs (losartan)/ ACEi/ CCB (avoid thiazide diuretics)
•
HT + Pregnancy: labetalol, hydralazine, nifedipine, or methyldopa
Additional treatments: Thiazides/ Clonidine
Drug class
ACEIs
Dosages
• Lisinopril- 10mg/day
• Enalapril- 5mg/day
ARBs
Thiazide diuretics
CCBs
•
Losartan- 50mg/day
•
Valsartan- 80mg/day
•
Chlorthalidone- 12.5mg/day
• DHPs: Amlodipine- 2.5mg/day
N-DHP’s less commonly used
•
BB
Verapamil: 100mg/day
Alpha+Beta blockers:
• Carvedilol: 6.35mg/x2/day
• Labetalol: 100mg/x2/day
Non-cardioselective
• Propranolol- 80mg/day
Cardioselective
• Bisoprolol- 2.5mg/day
Loop diuretics
Furosemide- 10mg/x2/day
K+ sparing diuretics
Alpha blockers
• Spironolactone
Alpha-1
• Doxazosin
Alpha-2
• Clonidine: 0.05mg/x2/day
• Methyl-dopa: 125mg/x2/day
Direct renin inhibitors
• Aliskiren: 150mg/day
Direct arterial vasodilators
• Hydralazine: 100mg/day in 2/3doses
36) Acute rheumatic fever. Rheumocarditis
Definition = delayed inflammatory complication of group A β-hemolytic streptococcal pharyngitis
(involving the heart, joints, skin, and CNS) that usually occurs w/in 2-4 weeks of acute infection. Peak
incidence 5-15 years
Etiology
•
Previous infection w/group A β-hemolytic streptococcus (GAS), also referred to as S.
pyogenes.
•
Usually acute tonsillitis or pharyngitis (“strep throat”)
•
GAS infections of the skin (e.g. impetigo, cellulitis) tend to be complicated by poststreptococcal GN rather than rheumatic fever
Pathophysiology
Exact pathogenesis is not yet entirely understood
Most commonly accepted mechanism = acute tonsillitis/pharyngitis caused by GAS w/out anti-B
treatment → development of AB against streptococcal M protein → cross-rxn of AB w/n. and
myocardial proteins (most commonly myosins) due to molecular mimicry → type 2 HS rxn → acute
inflammatory sequelae
Clinical manifestations
•
General = fever, fatigue, malaise,
•
Joints = migratory polyarthritis (non-destructive, mainly involving large joints)
•
Heart:
Pancarditis (AKA perimyoendocarditis) (endocarditis, myocarditis, and pericarditis)
Valvular lesions (most commonly on high pressure valves) = mitral valve (65%), aortic
valve (25%), tricuspid valve (10%)
DCM
•
CNS = Sydenham chorea (involuntary, irregular, non-repetitive movements of the limbs, neck,
head, and/or face)
•
Skin = subcutaneous nodules; erythema marginatum (centrifugally expanding pink/light-red
rash w/a well-defined outer border and central clearing; located on trunk and limbs w/the face
being spared)
MNEMONIC = JONES criteria (replace O w/♥ symbol) – J = Joints, ♥ = Pancarditis, N = Nodules, E =
Erythema marginatum, S = Sydenham chorea
Diagnosis
Diagnosis is based on the Jones criteria, which mainly describe the clinical findings of the condition.
Evidence of a preceding GAS infection is also preferred. Lab tests and imaging may be necessary to
assess any outstanding Jones criteria
For the Jones criteria, 2 major or 1 major + 2 minor or 3 minor criteria are required for diagnosis
Low risk population
Major criteria
Minor criteria
High risk population
•
Arthritis (migratory polyarthritis)
•
•
Carditis (pancarditis, including
valvulitis)
•
Polyarthralgia
•
Sydenham chorea
•
Carditis (pancarditis, including
•
Subcutaneous nodules
•
Erythema marginatum
•
+ everything else in low risk
•
Polyarthralgia
•
Monoarthralgia
•
↑ body temp (≥38.5°C)
•
↑ body temp (≥38°C)
•
↑ ESR (≥60)/CRP (≥3)
•
↑ ESR (≥30)/CRP (≥3)
•
Prolonged PR interval
•
Prolonged PR interval
Arthritis (monoarthritis or
migratory polyarthritis)
valvulitis)
•
Labs – normochromic, normocytic anaemia of chronic inflammation; leukocytosis
•
AB/Ag test = measures AB against metabolites of GAS = ↑ ASO and anti-streptococcal
DNAse B titer (ADB)
•
Echocardiography = may show mitral/aortic regurgitation
Treatment
•
General = bedrest (especially important in patients w/carditis)
•
Anti-B to eradicate GAS = oral penicillin V is drug of choice; alternatives include amoxicillin,
benzathine IM, cephalosporins, and macrolides
•
Anti-inflammatory therapy = NSAIDs (aspirin is preferred; alternatively ibuprofen or naproxen);
glucocorticoids if NSAIDs fail
•
Treatment of complications
Rheumocarditis
Definition = a clinical manifestation of rheumatic fever, which allows to determine the severity of the
underlying disease and the tactics of the patient. RA may be the only isolated sign of rheumatism or
be part of a clinical symptom complex, along w/other manifestations of the underlying pathology
Pathophysiology
The main trigger in the development of the classic form of rheumatic heart disease, as a
manifestation of rheumatism, is an acute streptococcal infection localized in the mucous membrane
of the upper RT, as evidenced by the findings of numerous randomized studies. Thus, in 80% of the
examined patients w/rheumatic heart disease, high titres of anti-streptococcal AB of different
serotypes are detected
Clinical manifestations
The development of the clinical symptom complex and the intensity of certain manifestations of
rheumatic heart disease depend on the localization of the inflammatory process and its
prevalence. The greatest activity of symptoms is acute rheumatic heart disease, in which there is a
primary lesion of the endocardium and the rapid dynamics of the growth of clinical manifestations,
which may be specific and somatic in nature.
•
Main carditis manifestation is myocardium and endocardium i.e. Endomyocarditis
•
HR changes
•
Heart birders dilation (predominantly to the L)
•
Apex beat decreasing
•
Gallop rhythm
•
Systolic murmur in 5 point apex (test valvulitis)
Treatment
All cases of primary rheumatic heart disease are subject to inpatient treatment in the
cardiorheumatology department, after which the patient is recommended to undergo a course of
rehabilitation therapy in a sanatorium of cardiological profile and undergo a routine examination by a
cardiologist in an outpatient setting.
37) Chronic cor pulmonale (AKA pulmonary heart disease)
Definition = altered structure (hypertrophy, dilation) or impaired function of the RV caused by
pulmonary HT or pulmonary stenosis resulting from a primary disorder of the respiratory or pulmonary
a. system.
Chronic cor pulmonale is the most common form and is slowly progressive; acute form is due to a
sudden overload of the RV, is usually caused by acute PE, and is a life-threatening condition.
Etiology
•
Acute form = almost always due to acute massive PE
•
Chronic form = caused by diseases of the airway, pulmonary vasculature, and chest wall –
COPD, chronic sleep apnoea, bronchiectasis, idiopathic pulmonary arterial HT, kyphoscoliosis
Pathophysiology
↑ Pressure in pulmonary circuit → ↑ RV afterload → dilatation and/or hypertrophy of the R heart →
RHF (cor pulmonale) and arrhythmias → death
Chronic cor pulmonale usually results in RV hypertrophy, whereas acute cor pulmonale usually
results in dilation. Hypertrophy is an adaptive response to a long-term ↑ in pressure. Individual
muscle cells grow larger (in thickness) and change to drive the ↑ contractile force required to move
the blood against greater resistance
Clinical manifestations
•
Common = dyspnoea and/or syncope on exertion; chest pain; fatigue; cyanosis; clinical
features of underlying etiology (e.g. COPD, sleep apnoea)
•
Less common = hoarseness, cough, hemoptysis
•
Physical examination = loud and palpable S2 (often split); jugular v. distension; symptoms of
RHF (palpitations, peripheral oedema, ascites, hepatomegaly, jaundice); nail clubbing;
parasternal heave
Diagnosis
Doppler echocardiography (best initial test)
•
Hypertrophy and/or dilation of the RV
•
Dilation of the coronary sinus
R heart catheterisation (confirmatory test)
•
Incomplete or complete RBBB
•
In some cases, P pulmonale
•
S1Q3T3 pattern in acute cor pulmonale
CXR
•
RV hypertrophy = prominent R heart border, loss of retrosternal space due to RV enlargement
in lat. view
•
Vascular changes = pronounced central pulmonary aa.
•
Signs of underlying cause (e.g. nodular opacities in interstitial lung disease, barrel chest in
COPD
Treatment
•
Initial therapy should be directed at the underlying cause (e.g. bronchodilators and ICS for
COPD, CPAP for patients w/obstructive sleep apnoea)
•
Patients who don’t respond to initial treatment = evaluation for pulmonary vasodilator therapy
in a specialised center
•
Additional measures = physical exercise, O2 therapy, diuretics for fluid retention
38) Aortic diseases: aortic dissection, aortic aneurysm, Takayasu
disease
Aortic dissection
Definition = a tear in the inner layer (tunica intima) of the aorta that leads to a progressively growing
hematoma in the intima-media space.
Localisation
•
Ascending aorta = 65% of cases
•
Descending aorta, distal to the L subclavian a. = 20% of cases
•
Aortic arch = 10% of cases
•
Abdominal aorta = 5% of cases
Etiology
Acquired
•
HT (most common risk factor) = ~70% of patients have HT, which can lead to propagation of
the dissection and ↑ the risk of rupture
•
Trauma = e.g. deceleration injury in a RTA, or iatrogenic injury during valve replacements or
graft surgery
•
Vasculitis w/aortic involvement (e.g. syphilis)
•
Use of amphetamines and cocaine
•
3rd trimester pregnancy (or early postpartum period)
•
Atherosclerosis
Congenital
•
CT disorders = Marfan syndrome, EDS
•
Bicuspid aortic valve
•
Coarctation of the aorta
Classification (mainly Stanford classification)
Stanford A aortic dissection = any dissection involving the ascending aorta (defined as prox. to the
brachiocephalic a.), regardless of its origin
•
Can extend proximally to the aortic arch and distally to the descending aorta
•
Generally requires surgery
•
Complications = aortic regurgitation and cardiac tamponade
•
They are > dangerous since they are > likely to cause the aorta to rupture
Stanford B aortic dissection = any dissection not involving the ascending aorta
•
Descending aorta = originating distal to the subclavian a.
•
Most cases can be managed w/medical therapy (e.g. BB, vasodilators)
MNEMONIC = Stanford A = affects the ascending aorta; Stanford B = begins beyond
brachiocephalic vessels
Pathophysiology
Common anatomic sites of origin (aorta is prone to rupture because of its high intrinsic wall pressure)
= above (2.2 cm) the aortic root, aortic arch, distal to the L subclavian a.
Transverse tear in the aortic intima (“entry”) → blood enters the media of the aorta and forms a false
lumen in the intima-media space (this creates a double-barrelled aorta consisting of the true aortic
lumen and the newly formed false lumen) → hematoma forms and propagates longitudinally
downwards
•
Rising pressure w/in the aortic wall → rupture
•
Occlusion of every single branching vessel (coronary aa., aa. supplying the brain, renal aa.,
aa. supplying the lower limbs) → ischemia in the affected areas
•
A 2nd intimal tear may result in a “re-entry” into the primary aortic lumen
Clinical manifestations
•
Sudden and severe tearing/ripping pain = located in the ant. chest (ascending) or back
(descending), interscapular or retrosternal pain (> common in thoracic dissection), neck and
jaw (aortic arch affected), abdomen or periumbilical, colicky pain (> common in abdominal
dissection)
•
HT (due to underlying HT and/or severe pain) or hypotension (e.g. due to shock from blood
loss, cardiac tamponade)
•
Asymmetrical BP and pulse readings between limbs
•
Syncope, diaphoresis, confusion or agitation
•
A heart murmur (an aortic regurgitation in a prox. dissection)
Diagnosis
Assess the risk of acute aortic dissection using the aortic dissection detection risk score (ADD-RS)
•
Score 0-1 (low-moderate risk) = diagnostic workup (e.g. ECG, labs, CXR) as clinically
indicated
•
Score 2-3 (high risk) = expedite definitive imaging (CT and magnetic resonance angiography
of chest, abdomen and pelvis; transoesophageal echocardiography). Definitive imaging is
used to determine the type of lumen, location, and extent of the dissection membrane. The
identification of a false lumen is highly suggestive of aortic dissection
ECG = ordered for all patients. Findings are variable and include:
•
Normal findings
•
Signs of LV hypertrophy
•
Non-specific changes (ST depression, T wave changes)
•
ST elevation due to coronary a. occlusion
Labs = ↑ D-dimer; evaluate for signs of end-organ damage (troponin, BMP, lactate); pre-op labs
(CBC, group and save, BMP, coagulation panel)
CXR = initial imaging in low-moderate risk patients; AP view
•
Characteristic = may be normal; widened mediastinum (>8 cm) at level of the aortic knuckle;
alteration of the mediastinal contour; mediastinal mass; calcium sign (displacement of the
intimal calcification of >6 mm)
•
Additional findings = double aortic contour; pleural cap; pleural effusion; blurring of aortic
knuckle; tracheal shift; widening of the paratracheal stripe
CT and magnetic resonance angiography of the chest, abdomen, and pelvis
•
Intimal dissection flap
•
Double lumen
•
Aortic dilatation
•
Regions of malperfusion
•
Aortic hematoma
•
Contrast leak (indicates rupture)
Transoesophageal echocardiography
•
Dissection flap (w/Doppler flow)
•
Double lumen in the ascending aorta
•
Thrombosis in false lumen
•
Pericardial effusion
Others = catheter angiography, US
Treatment
•
Urgent cardiothoracic surgical consult for all patients w/suspected or confirmed dissection,
regardless of location (replacement of the dissection w/polyester graft implant or stent
implantation only for type B) = type A requires immediate surgery (due to high risk of rupture)
and type B should be treated conservatively unless complications occur
•
BP control is essential in all patients to prevent progression of the dissection
•
Supportive care = analgesia (morphine)
•
Admission to ICU w/close monitoring and surveillance imaging
Complications = aortic rupture and acute blood loss; MI, aortic regurgitation, tamponade, pericarditis,
stroke (type A); acute abdomen, acute renal failure (both)
Aortic aneurysm
Definitions
•
True aneurysm = enlargement (dilatation) of an artery due to a weakened vessel wall.
•
False aneurysm = external hematomas w/a persistent communication to a leaking a.
•
Aortic aneurysm = dilatation of the aorta (all 3 layers) to >1.5X the normal size
Classification
•
Aortic root aneurysm, or aneurysm of the sinus of Valsalva
•
Thoracic aortic aneurysms – these are further classified as ascending (most common), aortic
arch, or descending aneurysms
•
Abdominal aortic aneurysms (“AAA, triple A”) – most common. Further classified as infrarenal
(most common; 1/3 will extend into the iliac aa.) and suprarenal; saccular (spherical) and
fusiform (spindle shaped)
•
Thoracoabdominal aortic aneurysms – components of both thoracic and abdominal aortic
aneurysms
Etiology
•
Atherosclerosis = most common
•
Trauma
•
CT disorders (e.g. Marfan syndrome, EDS)
•
Aortitis (aortic wall inflammation) = due to autoimmune disease (e.g. vasculitis, RA) or
infection (e.g. cardiovascular syphilis)
•
Risk factors = smoking, advanced age, HT, +ve family history
Pathophysiology
Thoracic aortic aneurysms
•
Ascending thoracic aortic aneurysm = most often due to cystic medial necrosis
•
Descending thoracic aortic aneurysm = typically as a result of atherosclerosis
Both
•
Inflammation and proteolytic degradation of CT proteins; and/or SMCs in high-risk patients →
loss of structural integrity of the aortic wall → widening of the vessel wall → may cause
disruption of the laminar blood flow and turbulent
•
Possible formation of thrombi in aneurysm → peripheral thromboembolism
Clinical manifestations
Aortic aneurysms are usually asymptomatic or non-specific symptoms. They are often discovered
incidentally on imaging
Thoracic aortic aneurysms
•
Chest pressure (mass effect of aneurysm on adjacent structures)
•
Thoracic back pain
•
Features of mediastinal compression/compression = dysphagia (oesophagus); upper venous
congestion (SVC syndrome); hoarseness (recurrent laryngeal n.); cough, wheeze, stridor
(trachea); Horner syndrome (sympathetic trunk)
Abdominal aortic aneurysms
•
Lower back pain
•
Pulsatile abdominal mass at or above the level of the umbilicus
•
Bruit on auscultation (due to disrupted laminar blood flow and turbulence in the aorta)
•
Peripheral thrombosis and distal atheroembolic phenomena (e.g. blue toe syndrome and
livedo reticularis)
•
↓ ankle brachial index
Diagnosis
Thoracic aortic aneurysms
•
CXR = abnormal aortic contour, widened mediastinum, tracheal deviation
•
CT angiography of the chest (best confirmatory test) = dilatation of the aorta, possible mural
thrombus, possible dissection/perforation/rupture
•
MR angiography of the chest w/ and w/out contrast
•
Transthoracic and transoesophageal echocardiography
•
Catheter angiography
Abdominal aortic aneurysms
•
Abdominal US is the best initial and confirmatory test = dilatation of the aorta ≥3 cm, thrombus
may be present. Disadvantages = low sensitivity for aneurysmal leaks, branch a. involvement,
and suprarenal involvement, and its findings are insufficient for procedural planning
•
CT angiography of the abdomen and pelvis w/IV contrast
•
MR angiography of the abdomen and pelvis w/out IV contrast
•
Arteriography (aortagraphy abdomen)
Treatment
•
Unstable patients (rupture) = emergency repair (open surgical repair or endovascular
aneurysm repair)
•
Symptomatic patients = urgent TAA repair
•
Asymptomatic patients = aneurysm surveillance; elective TAA repair when size or growth
thresholds are passed
•
All patients = conservative management w/reduction of CV risk factors
Complications = rupture, embolism, aortic dissection, post-op complications
III.Rheumatic diseases
39) Rheumatoid arthritis (RA)
Definition = an inflammatory autoimmune disorder characterised by joint pain, swelling, and synovial
destruction. It mainly affects middle aged women
Etiology
It is a chronic, inflammatory autoimmune disorder of unknown etiology – hypotheses suggest the
etiology is multifactorial, w/the following factors playing a role:
•
Genetic predisposition = family history of RA ↑ risk around 3-5 times. RA is strongly
associated w/specific HLA types (HLA-DR4, HLA-DR1)
•
Environmental = smoking, silica exposure, infections
•
Obesity
•
F sex
Pathophysiology
•
Initially, non-specific inflammation affects the synovial tissue, which is later amplified by
activation of T cells (autoimmune response).
•
With time, it may lead to inflammatory joint effusion and synovial hypertrophy, as well as
progressive destruction and deterioration of cartilage and bone.
Synovial lining hyperplasia
Pannus (destructive vascular granulation tissue) formation along the synovial tissue →
produce proteinases → destroy cartilage ECM
•
70-80% of patients have rheumatoid factor (RF) (an autologous AB – Ig RF) that reacts w/a
fragment of IgG to form immune complexes
•
Patients w/+ve RF are > likely to develop extra-articular manifestations of RA
The 3 phases of progression of RA are:
•
Initiation phase – due to non-specific inflammation
•
Amplification phase – due to T cell activation
•
Chronic inflammatory phase w/tissue injury resulting from the cytokines IL-1, IL-6, and TNF
Clinical manifestations
Articular (joint) manifestations
•
Polyarthralgia = symmetrical pain and swelling of affected joints (swollen, tender, warm joints);
most commonly affects the MCP, PIP, wrist and knee joints. The DIP joints, 1st CMC joint, and
the axial skeleton (except the cervical spine) aren’t typically affected
•
Morning stiffness (>60 mins) that usually improves w/activity
•
Joint deformities = “rheumatoid hand” is characteristic; hammer toe; atlanto-axial subluxation
(a loss of ligamentous stability between C1 and C2, which can result in compression of the
spinal cord, medulla, and/or vertebral aa. by the odontoid process, especially upon neck
flexion)
Extra-articular manifestations
•
General symptoms = fatigue, fever, loss of appetite and weight loss, sweating
•
Rheumatoid nodule in the skin (most common) = non-tender, firm, SC swellings (2 mm – 5
cm) which commonly occur in areas exposed to higher pressure; diffuse alopecia areata
occurs > commonly in RA
•
Other musculoskeletal = local osteoporosis around inflamed joints; CTS and tarsal tunnel
syndrome; tenosynovitis; bursitis
•
Eye = keratoconjunctivitis sicca; scleritis; and episcleritis
•
Lungs = fibrosis, pneumoconiosis (Caplan syndrome); rheumatoid pulmonary nodules;
pleuritis, pleural effusions
•
Endocrine = secondary Sjogren syndrome
•
Heart = pericarditis and myocarditis; higher risk of MI, stroke, and CHF
•
Vascular = peripheral vasculitis; Raynaud phenomenon; purpura; peripheral neuropathy
•
Teeth = periodontitis and tooth loss
•
Haematological = anaemia; neutropenia; splenomegaly (Felty syndrome)
Diagnosis
The diagnosis is based on diagnostic criteria including lab tests. Imaging may support the diagnosis,
but radiological joints findings are no longer included in the criteria, as they often become evident
only in late stages of the disease
Classification
ACR criteria for RA – RA = score of ≥ 6 points + confirmed presence of synovitis in at least typical
joint w/out an alternative, > probable diagnosis
Points
Joint involvement (pain/swelling)
Serology
Acute phase
reactants
-ve RF and ACPA
Normal CRP and
ESR
< 6 weeks
↑ CRP or ESR
≥ 6 weeks
0
≤1 large joints
1
2-10 large joints
2
1-3 small joints
Low +ve RF or
ACPA
3
4-10 small joints
High +ve RF or
Duration of
symptoms
ACPA
5
>10 joints (at least 1 small joint)
In clinical practice, the following criteria apply:
•
2/> swollen joints
•
Morning stiffness lasting >1 h for at least 6 weeks
•
Detection of RF or auto-ABs against ACPA such as auto-ABs to mutated citrulline vimentin
can confirm suspicion of RA. A –ve auto-AB result doesn’t exclude diagnosis of diagnosis of
RA
Lab tests
•
Non-specific = ↑ inflammatory markers (CRP, ESR), anaemia
•
Rheumatoid factor (RF) = IgM AB against Fc region of IgG; ↑ in about 80% of people w/RA
but can also be present in people w/other diseases and in a small % of healthy people; when
+ve in someone w/symptoms of RA, this test can be useful to confirm diagnosis
•
Anti-citrullinated protein ABs (ACPA) = may be used to help diagnose RA, especially early in
the disease – potentially before symptoms even appear – and in people who are RF -ve;
found in 60-70% of people w/RA; when used w/the RF test, ACPA results can help confirm a
diagnosis of RA.
•
Antinuclear AB (ANA) = this tests is used to screen for certain autoimmune disorders,
sometimes including RA, but is most often used to diagnose lupus
•
Synovial fluid analysis = cloudy yellow; sterile specimen w/leukocytosis; ↑ neutrophils,
granulocytes, and proteins; ↓ viscosity
Imaging
•
X-ray = early signs shows soft tissue swelling and demineralisation (juxta-articular); late signs
show joint space narrowing, erosions of cartilage and bone, demineralisation (generalised)
•
MRI (w/ or w/out contrast); US (joint effusion, pannus formation)
DDx = OA, psoriatic arthritis, gout, lyme arthritis, reactive arthritis, autoimmune-related arthritis
Treatment
•
General measures = cryotherapy for acute episodes of inflammation; physical and
occupational therapy; physical activity
•
Acute anti-inflammatory therapy = glucocorticoids – systemic (also need osteoporosis
prophylaxis) or intra-articular injections as needed; NSAIDs and COX-2 inhibitors
(prophylactic PPIs to prevent ulcers)
•
Long-term anti-inflammatory therapy w/disease-modifying anti-rheumatic drugs (DMARDs) =
methotrexate, hydroxychloroquine, sulfasalazine (for use in pregnancy), leflunomide, TNF-α
inhibitors (cetrolizumab, infliximab, adalimumab, etanercept), rituximab
•
Biologic therapy = for moderate-severe disease activity remaining after 3 months of DMARD
therapy – TNF-α inhibitors (rituximab, infliximab)
•
Surgery = synovectomy may be needed to prevent pain or tendon rupture when drug
treatment has failed – especially for affected fingers, hands, and wrists. Severely affected
joints may require joint replacement surgery (knee replacement)
40) Ankylosing spondylitis (spondyloarthritis, Bechterev’s disease)
Definition = chronic inflammatory disease of the axial skeleton that leads to partial or even complete
fusion and rigidity of the spine. M > F. Age 15-40yrs.
Etiology
•
Unknown cause – combo of genetic and environmental factors
•
The underlying mechanism is believed to be autoimmune or autoinflammatory
•
Genetic predisposition = 90-95% of patients are HLA-B27 positive (however, only 1-2% of
people w/HLA-B27 develop AS)
Clinical manifestations
Articular (joint) manifestations
•
Chronic dull pain that progresses slowly in the lower back or gluteal region and neck for
>3months, combined w/morning stiffness that improves w/activity. Pain is independent of
positioning, also appearing at night
•
Tenderness over the sacroiliac joints
•
Limited mobility of the spine (especially ↓ forward lumbar flexion)
•
Inflammatory enthesitis (e.g. of the achilles tendon, iliac crests, tibial tuberosities), painful on
palpation
•
Dactylitis; arthritis outside the spine (hip, shoulder, knee)
•
As the disease progresses, loss of spinal mobility and chest expansion, w/a limitation of ant.
flexion, lat. flexion, and extension of the lumbar spine, are seen
Extra-articular manifestations
•
General symptoms are common = fever, fatigue, weight loss
•
Most common = acute, unilateral ant. uveitis (~25% of cases)
•
Lungs = restrictive pulmonary disease due to ↓ mobility of the spine and thorax
•
GI = associated w/chronic IBDs
•
Prostatitis
•
Rare = aortic root inflammation and subsequent aortic valve insufficiency, atrioventricular
blocks, IgA nephropathy
Physical examination
•
Chest expansion measurement = to monitor disease severity – measure chest circumference
in full expiration and inspiration. Pathological difference < 2 cm and physiological difference >
5 cm
•
Reduced spinal mobility tests
o
o
o
o
•
Schober test (to assess lumbar forward flexion) = mark two points, L5/S1 and another
point 10 cm above → patient touches toes (w/out bending the knees) → distance
between the two points ↑ by ≥ 4 cm → physiological test result; a ↑ of < 4cm in
distance between these two points is pathological
Lateral lumbar flexion test – Patient stands against the wall and flexes to one side.
Distance between the tip of middle finger to floor is measured. Larger distance
indicates limited spinal mobility.
Chest circumference measurement after max expiration and inhalation to assess
thoracic spine mobility - <2.5cm increase is pathological
Occiput to wall distance measurement (Cervical) – to assess for Kyphosis – Occiput is
unable to touch the wall
Positive Sacroiliac Joint pain provocation tests –
o
o
Mennel sign = tenderness to percussion and pain on displacement of the sacroiliac
joints → indicates inflammation and/or degenerative changes
FABER test = FABER (flexion, abduction, and external rotation) provokes pain in the
ipsilateral hip, Pathological if there is pain/limited range of motion.
Diagnosis
•
Lab = ↑ CRP and ESR; auto-AB (RF, ANA) are –ve; HLA-B27 +ve in 90-95% of cases. CBC
may show anemia
•
X-ray = helps confirm diagnosis and evaluate disease severity; changes > evident in later
disease and usually occur symmetrically
Pelvis (best initial test) = to examine the sacroiliac joints – signs of sacroiliitis, including
ankylosis (fusion of the articular surfaces)
Spine = loss of lordosis w/↑ abnormal straightening of the spine; sclerosis of the
vertebral ligamentous apparatus – ‘dagger sign’; ossification of annulus fibrosis and
syndesmophytes resulting in a so-called ‘bamboo spine’ in AP view in the later
stages; signs of spondyloarthritis, including ankylosis of intervertebral joints
Thorax = ankylosis of costosternal and costovertebral joints
•
MRI = best method for early detection; > sensitive than CT for detecting sacroiliitis
DDx = mechanical low back pain, fibromyalgia, reactive/psoriatic arthritis, diffuse idiopathic skeletal
hyperostosis, osteophytes of the spine
Treatment
•
Physical therapy, Smoking cessation, Screen and treat Osteoporosis
•
Medical therapy = NSAIDs; TNF-α inhibitors (adalimumab); DMARDs (sulfasalazine, intraarticular glucocorticoids, Tofacitinib) in case of peripheral arthritis; temporary, intra-articular
glucocorticoids in severe cases
•
Surgery in severe cases to improve quality of life = Hip arthroplasty – severe hip arthritis,
Spinal osteotomy – severe kyphosis, joint replacement, spinal fusion.
Complications
•
Complete fusion of spine
•
Increased risk of Osteoporosis
•
Chalk stalk fractures
•
Restricted chest expansion and spine mobility – difficulty breathing
•
Pulmonary fibrosis
41) Reactive arthritis (formerly known as Reiter syndrome), Rheumatic
fever, Reiter’s syndrome, Lyme disease
Definition = an autoimmune condition that occurs after a bacterial infection of the GI or UT.
It belongs to a group of reactive arthropathies = sterile inflammatory joint disorders that are distant in
time and place from the initial inciting infective process. It is categorised as a seronegative
spondyloarthritis due to its association w/HLA-B27.
Etiology
Post-infectious autoimmune disorder (a type of molecular mimicry is assumed to be at work since
there is no evidence of pathogens in the synovial fluid)
•
Post-urethritis = after infection w/chlamydia (common) or U. urealyticum
•
Post-enteritis = after infection w/shigella, Yersinia, salmonella, or campylobacter
•
MNEMONIC = She Cherishes Cooking Yummy Salmon – Shigella, Chlamydia,
Campylobacter, Yersinia, Salmonella
Clinical manifestations
•
Latency period 1-4 weeks
•
Classical triad = conjunctivitis, urethritis, and arthritis (1/3) – can’t see, can’t pee, can’t climb a
tree (MNEMONIC)
•
Musculoskeletal symptoms = Oligoarthritis (acute, often asymmetrical w/migratory character,
mainly in lower extremities); Sacroiliitis; Enthesitis; Dactylitis
•
Extra-articular symptoms = Eyes - Conjunctivitis, Iritis, Episcleritis or Keratitis; Dermatologic
manifestations (Balanitis Circinata – skin lesions of glans penis resembling psoriasis,
Keratoderma blenorrhagicum – hyperkeratinisation of palms and soles); Oral ulcers, Cardiac
manifestations – Aortic regurgitation, AV blocks, Pericarditis
•
Symptoms from preceding infection = Diarrhoea, UT symptoms (Dysuria, Pelvic pain,
Urethritis, Prostatitis)
Diagnosis
Primarily a clinical diagnosis that may be supported by diagnostic steps, but there is no confirmatory
test
•
Labs = ↑ ESR and CRP; CBC - ↑ WBC and Platelets; test for potentially +ve HLA-B27; test for
-ve RF/anti-CCP anti-b; additional tests to confirm preceding infection (microscopy and culture
of synovial fluid, imaging, urine/stool culture, urethral swab – test for STI’s and HIV)
•
Arthrocentesis = to rule out DDx; findings include ↑ WBC w/mostly polymorphonuclear
leukocytes, -ve gram stain and cultures
•
Imaging – X-ray, MRI, Ultrasound of affected region - synovial hypertrophy,
hypervascularization of soft tissue, tendon thickening
•
Additional testing – ECG, Echocardiogram for cardiac manifestations. Slit lamp exam –
keratitis, anterior uveitis
DDx = Septic arthritis, Lyme disease, Syphilitic arthritis, RA, Seronegative spondyloarthritis, SLE,
Gout
Treatment
•
No curative treatment: goal of treatment is to control symptoms and treat underlying infection
as the disease usually resolves spontaneously within a year.
•
First line - NSAIDs for those with symptoms; Local treatment w/cryotherapy and
physiotherapy; Glucocorticoids (intraarticular or oral) as alternative to NSAIDs; DMARDs sulfasalazine or MTX in chronic cases (≥6 months)
•
For ongoing infection = anti-B
Prognosis
•
Resolves spontaneously within a year.
•
High rate of recurrence
42) Rheumatic fever
Definition = delayed inflammatory complication of group A β-hemolytic streptococcal pharyngitis
(involving the heart, joints, skin, and CNS) that usually occurs w/in 2-4 weeks of acute infection. Peak
incidence 5-15 years
Etiology
•
Previous infection w/group A β-hemolytic streptococcus (GAS), also referred to as S.
pyogenes.
•
Usually acute tonsillitis or pharyngitis (“strep throat”)
•
GAS infections of the skin (e.g. impetigo, cellulitis) tend to be complicated by poststreptococcal GN rather than rheumatic fever
Pathophysiology
Exact pathogenesis is not yet entirely understood
Most commonly accepted mechanism = acute tonsillitis/pharyngitis caused by GAS w/out anti-B
treatment → development of AB against streptococcal M protein → cross-rxn of AB w/n. and
myocardial proteins (most commonly myosins) due to molecular mimicry → type 2 HS rxn → acute
inflammatory sequelae
Clinical manifestations
•
General = fever, fatigue, malaise,
•
Joints = migratory polyarthritis (non-destructive, mainly involving large joints)
•
Heart:
Pancarditis (endocarditis, myocarditis, and pericarditis)
Valvular lesions (most commonly on high pressure valves) = mitral valve (65%), aortic
valve (25%), tricuspid valve (10%)
DCM
•
CNS = Sydenham chorea (involuntary, irregular, non-repetitive movements of the limbs, neck,
head, and/or face)
•
Skin = subcutaneous nodules; erythema marginatum (centrifugally expanding pink/light-red
rash w/a well-defined outer border and central clearing; located on trunk and limbs w/the face
being spared)
MNEMONIC = JONES criteria (replace O w/♥ symbol) – J = Joints, ♥ = Pancarditis, N = Nodules, E =
Erythema marginatum, S = Sydenham chorea
Diagnosis
Diagnosis is based on the Jones criteria, which mainly describe the clinical findings of the condition.
Evidence of a preceding GAS infection is also preferred. Lab tests and imaging may be necessary to
assess any outstanding Jones criteria
For the Jones criteria, 2 major or 1 major + 2 minor or 3 minor criteria are required for diagnosis
Low risk population
Major criteria
Minor criteria
•
High risk population
•
Arthritis (migratory polyarthritis)
•
•
Carditis (pancarditis, including
valvulitis)
•
Polyarthralgia
•
Sydenham chorea
•
•
Subcutaneous nodules
Carditis (pancarditis, including
valvulitis)
•
Erythema marginatum
•
+ everything else in low risk
•
Polyarthralgia
•
Monoarthralgia
•
↑ body temp (≥38.5°C)
•
↑ body temp (≥38°C)
•
↑ ESR (≥60)/CRP (≥3)
•
↑ ESR (≥30)/CRP (≥3)
•
Prolonged PR interval
•
Prolonged PR interval
Arthritis (monoarthritis or
migratory polyarthritis)
Labs – normochromic, normocytic anaemia of chronic inflammation; leukocytosis
•
AB/Ag test = measures AB against metabolites of GAS = ↑ ASO and anti-streptococcal
DNAse B titer (ADB)
•
Echocardiography = may show mitral/aortic regurgitation
Treatment
•
General = bedrest (especially important in patients w/carditis)
•
Anti-B to eradicate GAS = oral penicillin V is drug of choice; alternatives include amoxicillin,
benzathine IM, cephalosporins, and macrolides
•
Anti-inflammatory therapy = NSAIDs (aspirin is preferred; alternatively ibuprofen or naproxen);
glucocorticoids if NSAIDs fail
•
Treatment of complications
43) Psoriatic arthritis
Definition = arthritis (primarily on hands, feet, spine) that may occur w/psoriasis. 5-30% of psoriasis
patients are affected
Etiology = psoriasis (autoimmune genetic disease that is triggered by environmental factors –
infections, mechanical irritation, drugs such as BB, lithium, chloroquine)
Clinical manifestations
Psoriasis and psoriatic arthritis may occur independently or together. There are several types of
psoriatic arthritis:
•
Oligoarthritis (most common, 70%) = typically w/asymmetric involvement of both the DIP and
PIP (in contrast to RA, the MCP is usually not involved)
•
Spinal involvement (up to 40% of cases)
Other rheumatological features:
•
Enthesitis = inflammation of the enthesis (CT where tendons and ligaments insert into the
bone) – usually in and around the feet and ankles, especially the achilles tendon
•
Tenosynovitis
•
Dactylitis = inflammation and swelling of fingers and/or toes (“sausage digit”)
•
Arthritis mutilans = destruction of the IP joints and resorption of the phalanges w/further
collapse of the soft tissue of the fingers (“telescoping fingers” or “opera glass hand”)
Features of psoriasis include = scaly skin lesions (mainly on scalp, back, elbows, knees); itching; nail
involvement (nail pitting, brittle nails, oncholysis, oil drop sign)
Diagnosis
•
No specific test for diagnosis
•
Imaging studies = joint destruction (pencil-in-cup deformity of DIP joints on X-ray), ankylosis
(syndesmophytes, and in particular asymmetric paravertebral ossification)
Classification criteria for psoriatic arthritis (CASPAR) are helpful for diagnosing psoriatic arthritis; ≥3
points in the following 5 categories are required:
•
Evidence of psoriasis (2 points) – current disease manifestations, personal or family history
•
Personal or family history of the disease (1 point)
•
Psoriatic nail dystrophy (1 point)
•
Negative RF (1 point)
•
Dactylitis (1 point)
•
Radiologic signs (1 point)
Treatment = NSAIDs for mild; DMARDs for moderate-severe; physical therapy
44) Systemic lupus erythematosus (SLE) AKA lupus
Definition = a chronic systemic autoimmune disease in which the body’s immune system mistakenly
attacks healthy tissue in many parts of the body. it predominantly affects F of childbearing age (15-44
years)
Classification
•
Systemic lupus erythematosus (SLE)
•
Discoid (cutaneous) lupus erythematosus (DLE) is limited to skin symptoms and is diagnosed
by biopsy of rash on the face, neck, scalp, or arms. It is the most common type of chronic
cutaneous lupus (CCLE)
•
Subacute cutaneous lupus = associated w/skin lesions on parts of the body that are exposed
to sunlight
•
Drug induced lupus is a (generally) reversible condition occurring in people being treated for a
long-term illness. Symptoms generally disappear once the meds that triggered the episode
are stopped. Most common = quinidine, phenytoin, and hydralazine.
•
Neonatal lupus = rare, characterised by skin rash, liver problems, and low blood counts at
birth; usually resolves over several months
Etiology
Exact etiology is unknown; is presumably caused by a genetic susceptibility coupled w/an
environmental trigger which results in defects in the immune system. One of the factors associated
with SLE is vit D deficiency
•
Genetic predisposition = HLA-DR2 and HLA-DR3 are commonly present in individuals w/SLE.
Also, a genetic deficiency of classical pathway complement proteins (C1q, C2, C4) in ~10% of
cases.
•
Hormonal factors = hyperestrogenic states (e.g. due to oral contraceptive use,
postmenopausal hormonal therapy) are associated w/an ↑ risk of SLE
•
Environmental factors = UV light, stimulation of immune cells thorugh infection w/bacteria and
viruses (particularly EBV), medications (procainamide, hydralazine, phenytoin, sulpha drugs –
for drug induced lupus)
•
Risk factors = smoking, direct sunlight (SLE is aggravated by sunlight), F sex, black and Asian
ethnicity
Pathophysiology
Hormonal + environmental factors + genetic predisposition → loss of tolerance → production of AB
against perceived nuclear and cellular Ag’s → tissue damage via type 3 HS rxn and, to a lesser
extent, type 2 HS rxn
Mechanisms for development of auto-AB
Deficiency of classical complement proteins → failure of macs to phagocytose immune complexes
and apoptotic cell material (i.e. plasma and nuclear Ag’s) → dysregulated, intolerant lymphocytes
begin targeting normally protected intracellular Ag’s → auto-AB production (e.g. ANA, anti-dsDNA)
Mechanism of tissue damage
•
Type 3 HS → AB-Ag complex formation in microvasculature → complement activation and
inflammation → damage to skin, kidneys, joints, small vessels
•
Type 2 HS → IgG and IgM AB’s directed against Ag’s on cells (e.g. RBCs) → cytopenia
Clinical manifestations
SLE
•
Skin (85% of cases) = malar (butterfly) rash w/sparing of the nasolabial folds; photosensitivity;
discoid rash; oral ulcers; alopecia (non-scarring)
•
Joints = arthritis and arthralgia (90%); distal symmetrical polyarthritis
•
General = fever, fatigue, weight loss
•
Musculoskeletal = myalgia and lymphadenopathy
•
Serositis = pleuritis and pericarditis → effusions
•
Lungs = pneumonitis, interstitial lung disease, pulmonary HT
•
Heart = involvement of myocardium, pericardium, valves, and coronary aa.; Libman-Sacks
endocarditis (LSE)
•
GI = oesophagitis, hepatitis, pancreatitis
•
Kidneys = nephritis w/proteinuria (lupus nephritis)
•
Vascular = Raynaud phenomenon, vasculitis, thromboembolism
•
Neurologic = seizures, psychosis, personality changes, polyneuropathy
•
Hematologic = hemolytic anaemia, thrombocytopenia, leukopenia
DLE
•
Typically affects face, neck, and head (triggered by exposure to UV light
•
Begins as a discoid rash – erythematous raised patch w/adherent keratotic scaling and
follicular plugging
•
Heals and leaves scar tissue w/central atrophy
Subacute cutaneous
•
Usually affects the neck, shoulders, and forearms, but spares the face
•
Small erythematous lesions that develop into annular or psoriasiform lesions (scars, changes
in pigmentation, and atrophy are not typically seen)
Drug induced
•
Fever, polyarthritis, serositis, myalgia, rash
•
Symptoms may manifests months or even years after drug intake
Diagnosis
SLE
•
Suspect SLE in patients w/symptoms in >2 of the organ systems listed in the American
College of Rheumatology (ACR) criteria for SLE
•
Screening test = anti-nuclear AB (ANA) titer (SLE is unlikely if the test is negative
•
ANA testing has the highest sensitivity (95%) but low specificity for SLE. Anti-dsDNA AB and
anti-Smith AB testing are the most specific for SLE ∴, confirm diagnosis w/these highly
specific tests
•
Anti-dsDNA AB is +ve in 70% of patients; anti-Sm AB is +ve in 30%
The acronym for the ACR diagnostic criteria for SLE = SOAP BRAIN MD:
•
SOAP = Serositis, Oral ulcers, Arthritis, Photosensitivity
•
BRAIN = Blood disorders, Renal involvement, ANA, Immunologic phenomenon, Neurologic
disorder
•
MD = Malar rash, Discoid rash
Other test findings include: ↑ ESR w/normal CRP; ↓ C3 and C4 complement levels; urinalysis and
urine microscopy shows proteinuria and/or casts; CBC may reveal anaemia and ↓ WBC and platelets
DLE = lupus band test (Ig deposits found only in macroscopically affected skin); often ANA and antiRo –ve
Drug induced
•
Anti-histone AB = characteristic for drug induced lupus and manifest in ~95% of cases. They
may also be present in SLE but are significantly < common
•
↑ ANA; no anti-dsDNA AB
Treatment
General management include avoiding sunlight exposure, stop smoking, and immunise patients
before initiating immunosuppressants.
Complications = lupus nephritis
Mild symptoms, no vital
organs affected
Severe symptoms, no vital
organs affected
Basic therapy
Hydroxychloroquine (or chloroquine)
Addition of MTX or azathioprine is there is no response
Induction
therapy
Low-dose, short-term, oral
glucocorticoids
Medium-dose, short-term, oral
glucocorticoids
Organ damage
High-dose IV glucocorticoids
Immunosuppressive agents (e.g. azathioprine, mycophenolate,
cyclophosphamide)
Biological agents (e.g. belimumab)
45) Systemic sclerosis (SSc) (AKA systemic scleroderma)
Definition = chronic disease caused by abnormal growth of CT (fibrosis), which leads to diffuse
thickening and hardening of the skin and often the inner organs. (Alternative definition = cutaneous
sclerosis in association w/a vasculopathy of small aa., producing multi-organ systemic disease)
Etiology and pathophysiology
•
Unknown cause
•
Autoimmune component
•
Inflammatory synthesis of ECM = fibroblast proliferation and ↑ synthesis of normal collagen
•
Non-inflammatory vasculopathy = underlying mechanism of many of the > severe disease
features such as CAD, pulmonary a. HT, and renal crisis
Clinical manifestations
Common symptoms:
•
Cutaneous findings
Thickening and hardening of the skin; skin is smooth and shiny
Sclerodactyly = fibrotic thickening and tightening of the skin of the fingers and hands
→ limited range of motion and possibly flexure contractures and necrotic spots
Multiple, painful ischemic digital ulcers w/atrophy and necrotic spots
Digital pitting = hyperkeratotic scarring, most commonly affecting fingertips
Lesions on the prox. nail fold
Depigmentation of the skin w/sparing of perifollicular pigmentation (salt-and-pepper
appearance)
Face = mask-like facies, no wrinkles, shortened frenulum, microstomia accompanied
w/characteristic perioral wrinkles
•
Vascular disease = Raynaud phenomenon; thromboembolism
•
Other = fatigue, weakness; joint stiffness/pain
Limited cutaneous SSc:
•
Skin manifestations usually restricted to hands, fingers, and face
•
Disease progression is slow
•
90% of cases, Raynaud phenomenon precedes the onset of other symptoms
•
Extracutaneous organ involvement may occur
•
Often manifests as CREST syndrome
C → Calcinosis cutis = small white Ca2+ deposits on the pressure points of the
extremities such as the elbows, knees, and fingertips
R → Raynaud phenomenon
E → Esophageal hypomotility = smooth muscle atrophy and fibrosis → oesophageal
dysmotility and ↓ LES pressure → dysphagia, GE reflux, heartburn → may lead to
aspiration, Barrett oesophagus, strictures
S → Sclerodactyly
T → Telangiectasia/AKA “spider vv.” (dilated/broken small blood vessels located near
the surface of the skin which cause threadlike red lines/patterns on the skin)
Diffuse cutaneous SSc:
•
Skin manifestations are widespread; typically spread proximally from the trunk to the elbow
•
Disease progression is rapid; extracutaneous organ manifestations are common
•
Musculoskeletal = arthralgia and myalgia → can result in contractures
•
GI = oesophageal dysmotility → dysphagia and reflux; small bowel dysmotility → bloating,
gas, constipation, and cramping
•
Lungs = pulmonary HT and interstitial lung disease, ↑ risk of lung cancer
•
Heart = myocardial fibrosis, myocarditis, pericarditis
•
Kidney = abnormal collagen deposition → thickening of renal arteriolar walls → ↓ renal blood
flow, renal HT, proteinuria.
•
Scleroderma renal crisis is a life-threatening complication characterised by oliguric renal
failure, malignant HT, microangiopathic hemolytic anaemia, and encephalopathy. It is treated
w/ACE inhibitors.
Diagnosis
•
Auto-AB = ANA present in about 90% of cases
Limited SSc = anti-centromere AB (ACA) (main parameter in CREST syndrome)
Diffuse SSc = anti-Scl-70 (anti-topoisomerase I AB) (poorer prognosis, in 40% of
cases); anti-RNA polymerase III (associated w/renal involvement)
•
Serum protein electrophoresis = ↑ γ-globulins
•
CBC and differential (DDx = mixed CT disease – MTCD, Sharp’s syndrome)
•
CXR = detects possible pulmonary involvement; other tests may be indicated on organspecific symptoms
DDx = mixed CT disease (MCTD, Sharp syndrome)
Treatment
•
Treatment focuses on organ-specific, symptomatic therapy.
•
General = physical therapy and massage; prevent dry skin w/warm oils and paraffin baths and
avoiding soap; phototherapy
•
Immunosuppressive therapy (methotrexate/MTX) – for diffuse SSc or severe organ
involvement
•
Organ specific therapy = e.g. PPIs in cases of GERD
46) Polymyositis, dermatomyositis
Definitions
Polymyositis = inflammatory myopathy affecting the proximal skeletal muscles
Dermatomyositis = inflammatory myopathy that presents similarly to Polymyositis, w/the addition of
skin involvement
Etiology
Polymyositis = cell-mediated toxicity; against unidentified skeletal muscle Ag’s, chiefly affecting the
endomysium
Dermatomyositis = idiopathic or paraneoplastic AB-mediated vasculopathy, associated
w/malignancies (non-HL; lung, stomach, colon, or ovarian cancer)
Clinical manifestations
General features of both polymyositis and dermatomyositis
•
Proximal muscle weakness affecting both sides of the body (progresses w/in weeks to
months)
The pelvic and shoulder girdle muscles are most commonly affected
Other muscles, e.g. the neck flexors, may also be affected
Leads to difficulties combing hair, standing up, and climbing stairs
Dysphagia (30%) because of oesophageal muscle involvement
•
Muscle tenderness in ~33% of cases
Polymyositis
•
Foot drop in 1/both feet can be a symptom of advanced polymyositis
•
Systemic involvement includes interstitial lung disease and heart disease, such as HF and
conduction abnormalities
Dermatomyositis
•
Gottron papules = prominent erythematous papules, symmetrically distributed on the extensor
surfaces of the hands. Most commonly affects the MCP and IP joints
•
Mechanic’s hands = thickening and hyperpigmentation of the skin of the tips and sides of the
fingers, resulting in irregular, dirty-appearing hands
•
Heliotrope rash = erythematous rash on the upper eyelids, sometimes accompanied by
oedema
•
Midfacial erythema
•
Photosensitive poikiloderma = Shawls sign (erythema of upper back, post. beck, and
shoulders), V sign (erythema of the upper chest and neck), Holster sign (erythema of the lat.
thighs)
Diagnosis
•
Diagnosis is based on clinical presentation, labs, and pathology findings.
•
Polymyositis is diagnosed if the following criteria is fulfilled = proximal muscle involvement,
+ve lab findings, EMG suggestive of inflammatory myopathy, and typical biopsy findings
•
Dermatomyositis is diagnosed if additional cutaneous manifestations are present
•
If ≥2 criteria are fulfilled, poly/dermatomyositis is considered a possible diagnosis
Labs
•
↑ Muscle enz. = ↑ CK and ↑ Aldolase; additional ↑ enz. include myoglobin, LDH, AST, ALT
•
Inflammatory markers = ↑ ESR/CRP, leukocytosis, γ-globulin in protein electrophoresis
•
AB
ANA = not specific as it is +ve in only 1/3 of cases
Myositis-specific AB (MSAs) = anti-Jo-1 AB (histidyl-tRNA synthetase) and anti-Mi-2
AB (helicase)
Anti-Jo-1 AB = 5% dermatomyositis, 30% polymyositis
Anti-Mi-2 AB = ~10% of cases; > favourable prognosis; typically in patients
w/dermatomyositis
Anti-signal recognition particle AB (anti-SRP) = associated w/severe treatmentresistant necrotising myopathy; typically in patients w/polymyositis
Other procedures
•
EMG = abnormal in 90% of cases
•
Imaging = MRI may be helpful in identifying inflammation and a potential biopsy site, although
it is not always recommended
•
Muscle biopsy = muscle fiber necrosis, degeneration, and regeneration
Polymyositis = cell-mediated inflammatory infiltrates that predominantly involve
cytotoxic CD8+ T cells in the infrafascicular and endomysial region
Dermatomyositis = AB-mediated inflammatory infiltrates that predominantly involve
CD4+ T cells, plasmacytoid dendritic cells, and B cells in the perifascicular and
perimyseal region that lead to perifascicular atrophy
•
Skin biopsy = for suspected dermatomyositis
Treatment
•
Physical therapy
•
UV light protection for patient w/dermatomyositis
•
Drug of choice = corticosteroids (e.g. prednisolone)
•
Alternative treatment = immunosuppressant (MTX and azathioprine), IV Ig, plasmapharesis
47) Vasculitis/vasculitides – clinical features and classification
Definition = a heterogeneous group of autoimmune diseases, all characterised by inflammation of
blood vessels (vasculitis) and subsequent ischaemia and damage to the organs supplied by these
vessels
Etiology = primary (idiopathic) or secondary (response to hep B/C infection, myeloma, autoimmune
diseases)
Classification
The vasculitides are commonly classified based on etiology, pathological findings, and prognosis.
One classification system divides the conditions into 3 groups: small, medium-sized, and large vessel
vasculitides.
Small vessel vasculitis (microscopic polyangiitis, granulomatosis w/polyangiitis, Behcet’s
syndrome, Henoch-Schonlein purpura)
•
Involved in a n.o of different diseases, most of which are mediated by type 3 HS rxn
•
Commonly involve the skin and are often a complication of an underlying disease (i.e.
vasculitis associated w/neoplasms or CT disease) and exposure to environmental agents (i.e.
serum sickness and urticarial vasculitis)
•
Can be split into ANCA-associated (Churg-Strauss syndrome, granulomatosis w/polyangiitis,
microscopic polyangiitis) or non-ANCA associated (Behcet’s disease, Henoch-Schonlein
purpura) vasculitis of small vessels
Medium-sized vessel vasculitis (e.g. PAN, Kawasaki disease, thrombangiitis obliterans)
Large vessel vasculitis (e.g. Giant cell/temporal arteritis, Takayasu arteritis)
Takayasu arteritis (aortic arch syndrome)
•
Definition = granulomatous inflammation of the aorta and its major branches, resulting in
stenosis of involved blood vessels and subsequent vascular symptoms
•
Symptoms = long history of non-specific symptoms; ↓ bilateral brachial and radial pulses
(“pulseless disease); bilateral carotid bruits; syncope and angina pectoris; impaired vision;
Raynaud phenomenon; HT; movement-induced myalgia in ≥1 limbs; skin manifestations
(erythema nodosum, urticaria)
•
MNEMONIC = I can’t TAKA YA pulse (pulseless disease)
•
Diagnosis = ↑ ESR; angiography (gold standard) detects vascular stenosis; biopsy of affected
vessel (granulomatous thickening of aortic arch; plasma cells and lymphocytes in media and
adventitia; vascular fibrosis)
•
Treatment = corticosteroids, anti-HT drugs, surgery if critical stenosis occurs
Diagnosis requires ≥3 of the following diagnostic criteria to be filled:
•
Age of onset ≤40 years
•
Claudication of upper/lower extremities while in use
•
Audible bruit over the subclavian a. or abdominal aorta
•
↓ brachial a. pulse
•
BP difference >10 mmHg between arms
•
Abdominal arteriography of the aorta or large blood vessels in the extremities that is not due
to arteriosclerosis or fibromuscular dysplasia
Kawasaki disease (mucocutaneous lymph node syndrome)
•
Definition = an acute, necrotising vasculitis of unknown etiology
•
Symptoms = fever for at least 5 days; erythema and oedema of hands and feet; polymorphous
rash originating on the trunk; painless bilateral “injected£ conjunctivitis w/out exudate;
oropharyngeal mucositis (strawberry tongue, cracked and red lips); cervical lymphadenopathy
•
MNEMONIC = CRASH and BURN – Conjunctivitis, Rash, Adenopathy, Strawberry tongue,
Hands and feet; BURN = fever ≥ 5 days
•
Diagnosis = clinical diagnosis; echocardiography for evaluating coronary a. aneurysms; lab =
↑ ESR and CRP, leukocytosis, thrombocytosis
•
Treatment = IV Ig’s, high dose oral aspirin, IV glucocorticoids
Granulomatosis w/polyangiitis
The “C” disease = Curvy nose (saddle nose deformity), Chronic sinusitis, Cough, Conjunctivitis and
Corneal ulceration, Cardiac arrhythmias, non-Caseating granulomas on biopsy, cANCA,
Corticosteroids and Cyclophosphamide as treatment
Churg-Strauss syndrome (eosinophilic granulomatosis w/polyangiitis)
•
Definition = a multisystem disease characterised by necrotising granulomatous vasculitis
w/eosinophilia
•
Etiology = unknown
•
Symptoms = severe allergic asthma attacks (chief complaint); allergic rhinitis/sinusitis; skin
nodules, palpable purpura; Pauci-immune GN (GN w/out immune complexes or AB deposition
on histopathology); impaired mental status; pericarditis; GI involvement (bleeding, ischemia,
perforation); mononeuritis multiplex (loss of motor and sensory function, w/wrist/foot drop),
symmetric/asymmetric polyneuropathy
•
Diagnosis = peripheral blood eosinophilia; ↑ IgE; circulating MPO-ANCA/pANCA (~40%);
biopsy as confirmatory test (tissue eosinophilia, necrotising vasculitis, and necrotising
granuloma)
•
Treatment = immunosuppression w/glucocorticoids; possible in combo w/cyclophosphamide
Behcet’s disease
•
Definition = a systemic vasculitis that can affect aa. and vv. of all sizes
•
Etiology = autoimmune and infectious triggers; strong HLA-B51 association
•
Clinical features = recurrent painful aphthous ulcers; recurrent genital ulcerations; uveitis
and/or retinal vasculitis; skin lesions; arthritis of knee, ankles, hands, and/or wrists; ileocaecal
ulceration; vasculopathy (arterial thrombosis, aneurysms, thrombosis of large vv., super.
thrombophlebitis)
•
Diagnosis = +ve pathergy skin test – erythematous papule/pustule 24-48 hours after a needle
prick
•
Treatment = topical corticosteroids for ulcers, topical lidocaine for pain relief
•
MNEMONIC = PATHERGY – Positive pathergy test, Aphthous mouth ulcers, Thrombosis,
Hemoptysis (pulmonary a. aneurysm), Eye lesions, Genital ulcers, Young at presentation (3rd
decade)
48) Henoch-Schönlein purpura (AKA IgA vasculitis)
Definition = an acute immune complex-mediated small vessel vasculitis that most commonly occurs
in children (90% of cases <10 years)
Etiology
Exact pathogenesis is unknown and assumed to be multifactorial. Factors that likely play a role
include:
•
Preceding infection = up to 90% of cases preceded by viral/bacterial infection 1-3 weeks prior;
most commonly an upper RT infection caused by group A streptococcus; GI infections also
possible
•
IgA nephropathy
•
Genetic predisposition
•
Drugs (e.g. some anti-B and anti-arrhythmics) and vaccines (e.g. yellow fever, cholera)
Pathophysiology
Hypothesised mechanism = exposure to allergen/Ag (e.g. infection/drugs) → stimulation of Ig A
production → deposition of IgA immune complexes in vascular walls (e.g. in the skin, joints, GI,
kidneys) → activation of complement → vascular inflammation and damage
Clinical manifestations
HSP is characterised by a tetras of clinical features = palpable purpura, arthritis/arthralgia, GI
symptoms, and renal disease. HSP is one of the most important DDx to consider in cases of
paediatric limp.
•
Skin (~100%) = symmetrically distributed, raised, erythematous macules or urticarial lesions
that coalesce into palpable purpura (non-blanching skin lesions). Most common sites include
the lower extremities, buttocks, and other areas of pressure or constraint (e.g. from socks or
clothing)
•
Joints (~75%) = arthritis/arthralgia, most common in ankles and knees
•
GI tract (~60%) = colicky abdominal pain; can cause intussusception (invagination of proximal
part of bowel into a distal part → mechanical obstruction and bowel ischemia); bloody
stools/melena; N/V
•
Kidneys (~50%) = HSP nephritis w/signs and symptoms of nephritic syndrome
•
Other = scrotal swelling/pain/tenderness; CNS problems (headaches, seizures, ataxia,
central and peripheral neuropathy); RT (pulmonary hemorrhage, mild interstitial changes);
keratitis and uveitis in rare cases
Diagnosis
Labs (useful in patients w/incomplete/unusual clinical presentation)
•
CBC = ↑ platelets and WBC; ↓ Hb
•
Coagulation profile = usually normal
•
Serum AB and complement = ↑ IgA in serum; evidence of circulating IgA immune complexes;
↓ complement; ASO titers in case of preceding streptococcal infection
•
Serum chemistry = ↑ creatinine and/or BUN, electrolyte imbalance
•
Urinalysis to assess possible renal disease = hematuria, often w/RBC casts; possibly
proteinuria
•
Inflammatory markers = ↑ ESR/CRP
Imaging = abdominal US/CT – in patients w/marked abdominal symptoms or suspected
complications
Biopsy
•
For patients w/unusual skin presentations or severe renal involvement
•
Skin = leukocytoclastic vasculitis w/IgA and C3 immune complex deposition (hallmark) in
small vessels of the super. dermis
•
Kidney = mesangial IgA deposition, C3 complement and fibrin; crescent formation in > severe
cases
Treatment
Mild disease
•
Outpatient treatment; usually no treatment necessary (usually self-limiting)
•
NSAIDs for pain management, rest, and adequate hydration
•
Discontinuation of suspected precipitating drug, if applicable
Severe disease
•
Inpatient treatment
•
Systemic glucocorticoids for severe abdominal pain not relieved by NSAIDs
•
IV fluids to maintain hydration
•
In case of severe renal disease = IV Methylprednisolone pulse therapy; renal transplant in
end-stage disease; acute dialysis in AKI; consider anti-HT drugs if HT present; reduce salt
intake
49) PAN/Polyarteritis nodosa
Definition = systemic vasculitis of the small and medium-sized vessels, which leads to tissue
ischemia. Most commonly involves the skin, peripheral nn., muscles, joints, GIT, and kidneys
Etiology = often associated w/hep B/C infection
Clinical manifestations
•
Non-specific = fever, abdominal pain, muscle and joint pain
•
Kidney involvement (~60%) = HT, renal impairment
•
Coronary a. involvement (~35%) = ↑ risk of MI
•
Skin involvement (~40%) = rash, ulcerations, nodules
•
Neurological involvement = polyneuropathy
•
GI involvement = abdominal pain, melena, N/V
•
Usually spares the lungs
Diagnosis
Labs
•
Blood tests = serology for hep B/C; ↑ ESR; anaemia, leukocytosis
•
ANCA –ve (+ve pANCA in 15-30% of cases)
•
Urine analysis = proteinuria, hematuria
Muscle biopsy = transmural inflammation of the arterial wall w/leukocytic infiltration and fibrinoid
necrosis. The inflammatory lesions are usually in various stages of development and regeneration
Angiography = numerous small aneurysms and stenosis of small and medium-sized vessels of the
involved organs; most commonly seen in renal aa.
Treatment = immunosuppression (corticosteroids, cyclophosphamide); antiviral therapy against HBV
and HCV
50) ANCA associated vasculitis
Anti-neutrophil cytoplasmic AB (ANCA) associated vasculitis is a group of diseases characterised by
destruction
Granulomatosis w/polyangiitis (previously known as Wegener granulomatosis)
Epidemiology = peak incidence 40-60 years, M > F
Etiology = idiopathic
Pathophysiology
The following processes play a key role in the pathophysiology:
•
Aberrant epigenetic expression of proteinase-3 on the cell membrane of neutrophils
•
Formation of AB against proteinase-3 (PR3-ANCA) → binding of PR3-ANCA to PR3 activates
neutrophils → release of neutrophilic inflammatory mediators, formation of neutrophil
extracellular traps, complement activation → damage to endothelial cells of small blood
vessels
Clinical manifestations
•
Non-specific symptoms
•
ENT involvement (often the 1st clinical manifestation) = chronic rhinitis/sinusitis
(nasopharyngeal ulcerations → nasal septum perforation → saddle nose deformity); chronic
otitis and/or mastoiditis; oral ulcers; gingival hyperplasia
•
Lower RT = treatment-resistant pneumonia-like symptoms w/cough, dyspnoea, hemoptysis,
wheezing, hoarseness
•
Renal involvement = pauci-immune GN (indicates that there is little evidence of immune
complex/AB deposits) → RPGN; causes hematuria and RBC casts
•
Skin lesions = papules, vesicles, ulcers; purpura of the lower extremities; may lead to
necrotising vasculitis of small vessels → dry gangrene of digits
•
Ocular involvement = conjunctivitis, episcleritis, retinal vasculitis; corneal ulcers
•
Cardiac involvement = pericarditis, myocarditis; vasculitis of the coronary aa. → may lead to
MI and death
•
GPA triad = necrotising vasculitis of small aa., upper/lower RT manifestations, and GN
Diagnosis
•
Labs = ↑ creatinine, BUN, ESR, and CRP; normocytic normochromic anaemia; evidence of
PR3-ANCA/c-ANCA (highly sensitive and +ve in 90%); urinalysis shows microscopic
hematuria and proteinuria; RBC casts
•
Imaging = CXR/CT show multiple bilateral cavitating nodular lesions
•
Biopsy (confirmatory) = necrotic, partially granulomatous vasculitis of small and medium-sized
vessels; non-caseating, necrotising granulomas in the lung and upper airways; necrotising GN
Treatment
•
Mild disease = glucocorticoids + methotrexate (MTX)
•
Moderate-severe disease = glucocorticoids + cyclophosphamide or rituximab
•
Glucocorticoids should be tapered gradually
•
In the case of concurrent Goodpasture syndrome = plasmapharesis
•
Remission maintenance = immunosuppressive drugs (azathioprine, rituximab, MTX)
The “C” disease = Curvy nose (saddle nose deformity), Chronic sinusitis, Cough, Conjunctivitis and
Corneal ulceration, Cardiac arrhythmias, non-Caseating granulomas on biopsy, cANCA,
Corticosteroids and Cyclophosphamide as treatment
Churg-Strauss syndrome (eosinophilic granulomatosis w/polyangiitis)
•
Definition = a multisystem disease characterised by necrotising granulomatous vasculitis
w/eosinophilia
•
Etiology = unknown
•
Symptoms = severe allergic asthma attacks (chief complaint); allergic rhinitis/sinusitis; skin
nodules, palpable purpura; Pauci-immune GN (GN w/out immune complexes or AB deposition
on histopathology); impaired mental status; pericarditis; GI involvement (bleeding, ischemia,
perforation); mononeuritis multiplex (loss of motor and sensory function, w/wrist/foot drop),
symmetric/asymmetric polyneuropathy
•
Diagnosis = peripheral blood eosinophilia; ↑ IgE; circulating MPO-ANCA/pANCA (~40%);
biopsy as confirmatory test (tissue eosinophilia, necrotising vasculitis, and necrotising
granuloma)
•
Treatment = immunosuppression w/glucocorticoids; possible in combo w/cyclophosphamide
Microscopic polyangiitis
•
Definition = necrotising vasculitis of small vessels, typically w/pulmonary, renal, and skin
involvement
•
Manifestations are similar to granulomatosis w/polyangiitis; nasopharynx is usually not
affected
•
Clinical = renal (~90% – pauci-immune GN; HT); lungs (~50% – pulmonary vasculitis
w/hemoptysis); skin (~40% – palpable purpura, nodules, necrosis)
•
Diagnosis = biopsy of involved organ (fibrinoid necrosis w/infiltration of neutrophils; no
granulomas); MPO-ANCA/pANCA in ~70% of cases
•
Treatment = immunosuppression w/corticosteroids and cyclophosphamide
51) Large vessel vasculitis – Horton disease, Takayasu’s arteritis,
Buerger disease
Horton disease (AKA giant cell arteritis – GCA/temporal arteritis)
Definition = a type of autoimmune vasculitis that causes chronic inflammation of large and mediumsized aa., in particular the carotid aa., its major branches, and the aorta.
Epidemiology = peak incidence 70-79 years; F > M
Etiology = unknown – possible contributing factors include genetic predisposition (HLA-DR4) and
viral infections (parvovirus B19); association w/Polymyalgia rheumatica (up to 50% of patients also
have PMR)
Clinical manifestations
•
Non-specific symptoms = fever, weight loss, night sweats; symptoms of anaemia; myalgia and
arthralgia (mainly of shoulder and hip joints)
•
Cranial GCA = involves the extracranial branches of the common carotid, ICA, and ECA (the
temporal a. is the most commonly affected vessel) – new-onset uni/bilateral headache
(typically located over the temples; throbbing/dull); hardened and tender temporal a.; jaw
claudication (jaw pain when chewing); vision loss (due to inflammation and occlusion of the
ophthalmic a. and its branches); diplopia
•
Large-vessel GCA (< common; involves the aorta and its primary branches) = angina pectoris,
acute coronary syndrome; abdominal pain; limb claudication; asymmetrical pulses,
asymmetrical BP; vascular bruits
•
Symptoms of Polymyalgia rheumatica (if both diseases are present)
Diagnosis
•
Labs = ↑ ESR and CRP; additionally leukocytosis or normochromic anaemia
•
Temporal a. biopsy (gold standard; confirmatory test) = panarteritis of the large and mediumsized aa.; proliferation of the intima and subsequent stenosis of the a.; necrosis of the media;
fragmentation of the internal elastic lamina; predominantly mononuclear infiltration of the
vessels wall w/formation of giant cells
•
Duplex US = oedema and thickening of the vessel wall (halo sign); non-compressible a.;
stenosis and occlusion
Treatment
Initial high-dose glucocorticoid therapy (induction therapy; mainstay of treatment) for 2-4 weeks = oral
therapy (prednisolone) for uncomplicated disease; consider initial pulse therapy w/IV glucocorticoids
(methylprednisolone) before oral therapy for ischemic organ damage (impaired vision)
Maintenance therapy after acute symptoms have resolved; slowly taper glucocorticoids to the lowest
dose needed to control symptoms; length of treatment is generally ≥2 years.
Takayasu arteritis (aortic arch syndrome)
Definition = granulomatous inflammation of the aorta and its major branches, resulting in thickening
and stenosis of involved blood vessels and subsequent vascular symptoms
Epidemiology = peak incidence 15-45 years, Asian heritage, F > M
Clinical manifestations = non-specific symptoms; ↓ bilateral brachial and radial pulses (“pulseless
disease); syncope and angina pectoris; bilateral carotid bruits; impaired vision; Raynaud
phenomenon; HT; movement-induced muscular pain; skin manifestations (erythema nodosum,
urticaria)
MNEMONIC = I can’t TAKA YA pulse (pulseless disease)
Diagnosis = ↑ ESR; angiography (gold standard) detects vascular stenosis; biopsy of affected vessel
(granulomatous thickening of aortic arch; plasma cells and lymphocytes in media and adventitia;
vascular fibrosis)
Treatment = corticosteroids, anti-HT drugs, surgery (e.g. bypass) if critical stenosis occurs
Buerger disease (thromboangiitis obliterans)
Definition = an inflammatory, non-atherosclerotic, vaso-occlusive disease of both small and mediumsized aa. as well as vv. in the upper and lower limbs
Epidemiology = age of onset before 45 years; M > F
Etiology = smoking is the single most important risk factor
Pathophysiology
•
Inflammation of the intima w/neutrophilic infiltration and microabscess formation (endarteritis)
→ inflammation may also spread to the media but the internal elastic lamina usually remains
intact → development of cell-rich, inflammatory thrombi in the lumen → occlusion of the
vessel
•
Mononuclear cells, fibroblasts, and giant cells replace neutrophils
•
Reorganisation of the thrombus and perivascular fibrosis
•
Contiguous extension of the inflammatory process to the adjacent v. and n., resulting in the
encasement of the a., v., and n. in a fibrous sheath
Clinical manifestations
•
Patients may present w/acute limb ischaemia and/or symptoms of chronic peripheral a.
disease
•
Early manifestations = super. thrombophlebitis (which is often migratory) w/tender nodules
along the course of the v.; intermittent claudication; Raynaud disease
•
Late manifestations = rest pain; cool peripheral extremities; trophic nail changes; ulceration
and/or gangrene of the fingertips and/or toes; normal brachial and popliteal pulses but
poor/absent radial, ulnar, ant./post. tibial and/or dorsalis pedis pulsations
Diagnosis
•
Labs = ESR and CRP are w/in normal limits; auto-AB are absent and a hypercoagulability
screen is normal
•
Ankle-brachial index = ↓
•
Imaging = Doppler US (initial imaging), arteriography (modality of choice – shows nonatherosclerotic, smooth, tapering, segmental lesions that occlude distal vessels of extremities
w/corkscrew-shaped collateral vessels around the site of occlusion)
•
Biopsy (confirmatory)
Treatment
•
General = stop smoking; protection of fingers and toes from cold to prevent Raynaud
phenomenon
•
Medical therapy (may be used to improve circulation and control pain) = iloprost, CCB
(nifedipine, amlodipine), hyperbaric O2 therapy (useful in those w/critical limb ischaemia – late
stage manifestations)
•
Surgical therapy = revascularisation procedures usually can’t be performed; patients w/ulcers
may require debridement and anti-B treatment; patients who develop gangrene in the
extremities will require amputation
52) Anti-phospholipid syndrome (APS)
Definition = an autoimmune disease that ↑ the risk of thrombosis as a result of procoagulotory ABs
Etiology
•
Primary = idiopathic; associated w/genetic marker HLA-DR7
•
Secondary = lupus (most common cause of secondary APS); RA; neoplasms; HIV, Hep
A/B/C; bacterial infections (e.g. syphilis, lyme disease, TB)
Pathophysiology
Formation of procoagulatory anti-phospholipid AB → AB form complexes w/anticoagulant proteins,
thereby inactivating them (e.g. protein C/S, antithrombin III) → AB activate platelets and vascular
endothelium (leads to ↑ binding of platelets) → induction of a hypercoagulable state → ↑ risk of
thrombosis and embolism
Clinical manifestations
APS usually manifests w/recurring thrombotic events that may affect any organ
•
Venous = DVT, PE, livedo reticularis (blood clots in capillaries lead to swelling of venules,
resulting in a purplish, net-like discolouration of the skin), ulceration
•
Arterial = stroke, transient ischaemic attacks; occlusion of organ aa. (e.g. MI); occlusion of
distal extremity aa. (ischaemia and gangrene)
•
Capillaries = splinter haemorrhages
•
Pregnancy-related = recurrent miscarriages and premature births (caused by thrombosis of
placental vessels and possible subsequent placental infarction)
Diagnosis
•
History = arterial/venous thrombosis; recurrent miscarriages (≥1)
•
Serology = for anti-phospholipid ABs
Lupus anticoagulant = leads to a prolonged aPTT
Anticardiolipin AB (IgG and IgM) = patients w/APS often test false +ve for syphilis, as
the Ag used in syphilis test is cardiolipin
Anti-β2-glycoprotein AB = a group of AB that inactivate anticoagulant proteins and
activate platelets and vascular endothelium, thereby resulting in a hypercoagulable
state)
•
Blood tests = thrombocytopenia, hemolysis, leukocytopenia
Treatment
The key element of APS treatment is systemic anticoagulation
•
Acute management = SC LMWH or IV unfractionated heparin; in severe cases – high dose
glucocorticoids, plasmapharesis, and/or Ig’s
•
Secondary prophylaxis = low-dose aspirin for low risk patients; long-term treatment w/oral
warfarin for high-risk patients who don’t wish to become pregnant; LMWH + aspirin
(prevention of miscarriage) for those who wish to have children
53) Polymyalgia rheumatica and fibromyalgia
Polymyalgia rheumatica (PMR)
Definition = an inflammatory condition of unknown origin characterised by aching and morning
stiffness in the shoulder and pelvic areas
Etiology
•
Unknown
•
Possible contributing factors are genetic predisposition (HLA-DR4) and association w/giant
cell arteritis (~10% of patients w/PMR also have giant cell arteritis)
Clinical manifestations
Systemic symptoms
•
General symptoms = fever, weight loss, night sweats, fatigue, malaise
•
Depressed mood
•
Symptoms of anaemia
Musculoskeletal system – primarily affects the shoulders, neck, and pelvic girdle
•
New onset, symmetric pain that is worse at night
•
Morning stiffness (>45 min)
•
Muscular atrophy and weakness = not directly caused by PMR but resulting from ↓ activity
due to pain and stiffness
Diagnosis
•
↑ ESR, specifically >50 mm/h; ↑ CRP
•
Leukocytosis
•
Normochromic anaemia
•
Normal CK; -ve RF; no auto-AB
•
Bursitis on US of affected joints
Treatment
Low-dose oral glucocorticoids (alternatively IM glucocorticoids) – usually rapid response w/in 2-4
weeks; if no improvement after 2 weeks/relapse = ↑ dose
Fibromyalgia
Definition = a neurosensory disorder characterised by chronic widespread musculocutaneous pain
and a heightened pain response to pressure (allodynia)
Etiology
The pathophysiology is not fully understood, but its etiology is likely multifactorial – genetic
predisposition + environmental triggers (physical or psychosocial stress) + dysregulation of the
neuroendocrine system and ANS
Clinical manifestations
Common symptoms
•
Chronic, widespread pain, primarily at points where muscles and tendons attach to bones
(tender points)
•
Morning stiffness
•
Headache, fatigue,
•
Sleep disorders
•
Cognitive dysfunction (fibro fog – poor memory, difficulty concentrating, lack of clarity of
thought)
•
Paraesthesia
•
Further symptoms of ANS dysfunction = digestive problems, weight fluctuation, palpitations,
sexual dysfunction, night sweats
Common associations
The following disorders can manifest w/symptoms that sometimes resemble those seen in
fibromyalgia, and they may occur alongside it
•
Functional somatic syndromes = e.g. chronic fatigue syndrome, IBS, tension or migraine
headaches, chronic pelvic and bladder syndromes
•
Psychiatric disorders = depression, generalised anxiety disorder
•
Sleep disorders = sleep movement disorders such as restless leg syndrome
•
Inflammatory rheumatic diseases = SLE, RA
Diagnosis
Clinical diagnosis – ACR take into account
•
Symptom duration of at least 3 months
•
Patient self-reporting using the fibromyalgia score – widespread pain/tenderness in up to 19
different regions of the body (widespread pain index); presence and severity of symptoms
such as fatigue, sleep disturbance, depression, headache, and cognitive impairment
(symptom severity scale)
Lab values and imaging are normal (helpful for excluding other causes)
Treatment
•
Lifestyle changes = dietary recommendation, regular physical activity
•
Meds = initially monotherapy – low-dose Tricyclic anti-depressants (amitriptyline), SNRIs
(duloxetine) or anticonvulsants (pregabalin, gabapentin)
•
Non-responders = combo drug therapy; physical therapy; psychological interventions (CBT)
•
Avoid narcotic meds (e.g. opioids)
54) Gout (podagra)
Definition = an inflammatory crystal arthropathy caused by the precipitation and deposition of uric
acid crystals in synovial fluid and tissues and is characterised by recurrent attacks of a red, tender,
hot, and swollen joint.
Etiology
•
The crystallisation of uric acid, often related to high levels in the blood (hyperuricemia), is the
underlying cause of gout. This can occur because of diet, genetic predisposition, or ↓
excretion of urate.
•
Diet = food rich in purines yield high amounts of uric acid – red meat, seafood; alcohol,
fructose-sweetened drinks
•
Phosphoribosyl pyrophosphate synthetase (PRPS) = enz. that converts ribose 5-phosphate
into phosphoribosyl pyrophosphate. In a mutation that leads to super activity of the enz., we
can produce excess purine and uric acid.
•
Medical conditions = gout frequently occurs in combo w/other medical problems = metabolic
syndrome (combo of abdominal obesity, HT, insulin resistance, and abnormal lipid levels),
kidney failure, haemolytic anaemia, lead poisoning, and myeloproliferative diseases such as
polycythemia
•
Medication = diuretics have been associated w/attacks of gout; immunosuppressive drugs
cyclosporine and tacrolimus; β blockers, aspirin, and niacin
•
Risk factors = BMI ≥ 35 ↑ M risk of gout threefold; chronic lead exposure ; alcohol; diet (food
rich in purines); recent surgery or trauma
Pathophysiology
•
Urate levels can be ↑ because of: ↓ excretion (most common), ↑ production, or ↑ purine intake
•
Gout is a disorder of purine metabolism, and occurs when its final metabolite, uric acid,
crystallizes in the form of monosodium urate, precipitating and forming deposits (tophi) in
joints, on tendons, and in the surrounding tissues.
•
Factors that trigger urate crystal deposition include = ↑ uric acid levels, acidosis, or low temp.
(cool peripheral joints)
•
Microscopic tophi are usually encased in a fibrous matrix, which blocks interaction of the
crystals w/cells and therefore avoids inflammation
•
Naked crystals may break off due to minor physical damage to the joint, medical or surgical
stress, or rapid changes in uric acid levels. When they break through the tophi, they trigger a
local immune-mediated inflammatory rxn in macs → causes inflammatory cascade
Clinical manifestations
•
Acute inflammatory arthritis = a red, tender, hot, swollen joint. The MTP joint at the base of the
big toe is the most common site. Other joints = heels, knees, wrists, and fingers. Pain usually
begins over 2-4 h and during the night.
•
Fever, fatigue, tachycardia, chills, and malaise may sometimes occur
•
Hyperuricemia may result in other symptoms, including hard, painless, deposits of uric acid
crystals (tophi).
•
Extensive tophi may lead to chronic arthritis due to bone erosion; crystals precipitating in
kidneys → stone formation and subsequent urate nephropathy
•
Limited range of motion
Diagnosis
Labs
•
Blood test = may be hyperuricemia – ½ the time gout occurs w/out hyperuricemia and most
people w/↑ uric acid levels never develop gout; ↑ WBCs and ESR/CRP; kidney function (GFR,
creatinine, and creatinine clearance)
•
CBC helps differentiate between septic arthritis and gout
•
RF or ANA may be ordered to rule out other causes of arthritis symptoms. A blood culture
may also be done if septic arthritis is suspected
Imaging
•
Indicated if synovial fluid analysis is unsuccessful or cannot be performed. It can be useful to
identify supportive findings but cannot rule out septic arthritis
•
US = signs of acute joint inflammation, bone erosions, signs of urate crystal deposition
(double contour sign)
•
Dual-energy CT = can detect crystals w/in deeper anatomical structures (spine) and extraarticular sites
•
Conventional CT and MRI = can identify erosions and tophi; used less frequently
•
X-ray = punched-out lytic bone lesions
Arthrocentesis w/synovial fluid analysis (gold standard) = identification of needle-shaped
monosodium urate crystals in synovial fluid or a tophus under polarised light microscopy
Treatment
•
General = lifestyle modifications that may help reduce the risk of flares (limit alcohol
consumption, purine intake, and high-fructose corn syrup; weight loss); management of
comorbidities
•
Acute flare = rest and ice the affected joint; meds include glucocorticoids, NSAIDs, or
colchicine (1st line); 2nd line include IL-1 inhibitors or ACTH
•
Chronic gout = urate lowering therapy – allopurinol (1st) (xanthine-oxidase inhibitor);
probenecid (2nd) (uricosurics); pegloticase (3rd) (recombinant uricase)
•
Administer anti-inflammatory prophylaxis before initiation urate lowering therapy, as otherwise
the drugs could trigger, prolong, or worsen an acute gout flare
55) Osteoporosis
Definition = a skeletal condition in which the loss of bone mineral density leads to ↓ bone strength and
an ↑ susceptibility to fractures OR a metabolic bone disease characterised by a loss of mineralised
bone mass causing ↑ porosity of the skeleton and susceptibility to fractures
Etiology
Primary osteoporosis (most common form)
•
Type I (postmenopausal osteoporosis) = postmenopausal women – oestrogen stimulates
osteoblasts and inhibits osteoclasts; the ↓ oestrogen levels following menopause lead to ↑
bone resorption
•
Type II (senile osteoporosis) = gradual loss of bone mass as patients age (especially > 70
years)
•
Idiopathic osteoporosis in kids (8-13) and young adults (<50 years)
Secondary osteoporosis
•
Drug-induced/iatrogenic = most commonly due to systemic long-term therapy
w/corticosteroids; other = long-term therapy w/anti-convulsants, anti-coagulants, PPIs
•
Endocrine/metabolic = hypercortisolism, hypogonadism, hyperthyroidism,
hyperparathyroidism, renal disease
•
Multiple myeloma
•
Excessive alcohol consumption
•
Immobilisation (bedridden, wheelchair, fractured limb in a cast)
Risk factors
•
Cigarette smoking
•
Malabsorption, malnutrition (e.g. vit D deficiency), anorexia
•
Low body weight
•
Family history of osteoporosis
•
Ethnicity = EU and Asian ancestry predisposes for osteoporosis
Pathophysiology
•
Underlying mechanism is an imbalance between bone resorption and bone formation
•
3 main mechanisms by which osteoporosis develops are = an inadequate peak bone mass
(the skeleton develops insufficient mass and strength during growth), excessive bone
resorption, and inadequate formation of new bone during remodelling
Clinical manifestations
•
Mostly asymptomatic
•
Fragility fractures = pathological fractures that are caused by everyday-activities (e.g. bending
over, sneezing) or minor trauma (falling from standing height)
Common locations = vertebral (most common) → femoral neck → distal radius (Colles
fracture) → other long bones (e.g. humerus) → hip
•
Vertebral compression fractures = commonly asymptomatic but may cause acute back pain
and possible point tenderness w/out neurological symptoms. multiple fractures can lead to ↓
height and thoracic kyphosis (dowager hump)
Diagnosis
Labs
•
Urine = ↑ cross-links (bonds between collagen molecules) (e.g. deoxypyridinoline), markers of
bone turnover
•
Blood = normal Ca+, phosphate, PTH and possibly ↑ AP in primary; abnormal results
depending on the underlying disease in secondary
Imaging
•
Dual-energy X-ray absorptiometry (DXA)
Non-invasive technique that calculate bone mineral density (BMD) by using 2 x-ray
beams; measurement sites = lumbar spine and femoral neck
Osteoporosis = T-score ≤ 2.5 SD (T-score is the different in SD between the patient’s
BMD and the BMD of a young adult F reference mean)
•
Plain radiography of the whole skeletal system if osteoporosis is diagnosed = ↑ radiolucency
is detectable in cortical bones once 30-50% of bone mineral has been lost; vertebral
compression fractures (diagnostic)
•
Quantitative CT = measurement of true bone volume density in g/cm3
DDx = osteomalacia (bone softening), hyperparathyroidism, metastases, multiple myeloma
Treatment
•
Drugs = bisphosphonates; alternatively teriparatide (PTH analog), raloxifene (SERM),
denosumab (monoclonal AB), calcitonin, hormonal therapy
•
Prophylaxis includes ensuring enough calcium and vitamin D in the diet, avoiding alcohol and
smoking, physical activity, and avoiding/minimising use of glucocorticoids
56) Osteoarthritis (OA)
Definition = a disabling joint disease characterised by non-inflammatory degeneration of the join
complex (articular cartilage, subchondral bone, and synovium) that occurs w/old age or from overuse
and mainly affects the weight-bearing and high-use joints (knee > hip > hand, lower back), OR
A chronic progressive arthropathy characterised by destruction of articular cartilage and its underlying
bone w/in a joint as well as bony overgrowth which results in bones rubbing together and creating
stiffness, pain, and impaired movement.
It is the most common type of arthritis; incidence ↑ w/age; F > M
Classification
OA can be classified according to the underlying cause:
•
Idiopathic OA = no identifiable underlying cause; can be localised or generalised; genetic
factors have been implicated, but not definitively proven
•
Primary OA = occur due to intrinsic defects in the articular cartilage that cause joint narrowing,
subchondral bone thickening, and ultimately a painful joint
•
Secondary OA = hemochromatosis, Wilson disease, EDS, DM, avascular necrosis, congenital
disorders of joints, Alkaptonuria, joint trauma
Etiology
•
Modifiable risk factors = obesity, excessive joint loading or overuse (mechanical stress)
•
Non-modifiable risk factors = age (>55), sex, family history, history of joint trauma or injury,
anatomic factors causing asymmetrical joint stress (varus/valgus knees), haemophilic
haemarthrosis and deposition diseases that stiffen cartilage
Pathophysiology
Chronic mechanical stress on the joints and age-related ↓ in proteoglycans → cartilage loses
elasticity and becomes friable → degeneration and inflammation of cartilage → joint space narrowing
and thickening and sclerosis (stiffening) of the subchondral bone
Clinical manifestations
Early clinical findings
•
Pain during or after exertion that is relieved w/rest
•
Pain in both complete flexion and extension
•
Crepitus on joint movement
•
Joint stiffness and restricted range of motion
•
Radiating or referred pain (e.g. coxarthrosis may lead to knee pain)
•
Possible varus formation if the knee is affected (loss of cartilage usually begins medially)
•
Joints are usually asymmetrically involved (as opposed to RA)
Late clinical findings = constant pain, morning joint stiffness usually lasting <30 min, more severely
restricted range of motion
Subtypes and variants
•
Heberden’s nodes = pain and nodular thickening on the dorsal sides of the DIP
•
Bouchard’s nodes = pain and nodular thickening on the dorsal sides of the PIP
•
Rhizarthrosis = OA of the 1st CMC joint (between trapezoid and 1st metacarpal)
•
Hallux rigidus = arthrosis of the 1st MTP, characterised by hypertrophy of the sesamoid bones
•
OA of the hip (coxarthrosis) and knee (gonarthrosis)
Diagnosis
OA is usually a clinical diagnosis. Radiographic evidence of joint degeneration supports the diagnosis
of OA.
4 key radiological signs of OA:
•
Irregular joint space narrowing (usually 6-7 mm)
•
Thickening of subchondral bone (subchondral sclerosis) = dense area of bone just below the
cartilage zone of a joint, formed due to a compressive load on the joint
•
Osteophytes (bone spurs) (secondary sign) = bony projections that develop on joint surfaces
as spurs or densifications. They develop on the edges of the joint and thereby ↑ the joint
surface
•
Subchondral (bone) cysts = fluid-filled cysts that develop at the surface of the joint due to local
bone necrosis induced by the joint stress of OA
Other tests include synovial fluid analysis (usually non-inflammatory) and arthroscopy (can show a
thickened capsule, synovial hypertrophy, and/or ulcerated cartilage)
Treatment
•
General = weight loss, regular low-impact exercise (swimming, riding a bike), shoe inserts (in
valgus deformity), targeted muscle growth, physiotherapy, topical and heat therapy
•
Meds = peripheral analgesics (paracetamol, NSAIDs) or opioid analgesics (tramadol). Meds
should be used as acute and symptomatic therapy only; long-term NSAID use should be
avoided due to its many side effects
•
Interventional therapy = intraarticular glucocorticoid injections (not long-term option)
•
Surgical = endoprosthesis (joint replacement); if that fails or in select subtypes – arthrodesis
(operative ankylosis)
57) Treatment of rheumatic diseases w/biological and biosimilar drugs
Biological agents
Definition = a group of recombinant proteins (often AB) that are engineered to interfere w/specific
immunological processes. They are most commonly used in the treatment of autoimmune diseases
and malignancies. The naming of AB follows a certain classification scheme:
•
The suffix “-mab”, indicates a monoclonal AB
•
Second to last syllable = describes the origin – e.g. “xi” = chimeric, “u” = human
•
Third to last syllable = denotes the target – e.g. li(m) = immune system
B cell inhibitors (e.g. rituximab)
•
Work by killing B lymphocytes that can cause inflammation.
•
Must be administered IV for 2 sessions every 6-12 months. Each session lasts 4-6 hrs
•
Patient is at risk of infections and transfusion rxns
IL-1 blockers (e.g. anakinra) = target IL-1 (inflammatory mediator); prescribed less often as they
must be self-injected once daily
IL-6 inhibitors (e.g. sarilumab) = prevent IL-6 from attaching to cells and causing inflammation.
T-cell inhibitors (e.g. abatacept) = attach to the surface of T-cells; administered by IV for 30 mins
every other week for 6 weeks; person transitions to getting infusions every 4 weeks after that
TNF inhibitors (e.g. infliximab, adalimumab) = inhibit TNF, which is responsible for the early
stages of inflammation; prescribed more frequently as they have the longest history as a treatment for
RA
Most biological treatments are taken either via IV infusion or by self-injection. These meds can’t be
taken as a pill because the molecules contained w/in are usually considered too small to pass into the
bloodstream. As a result, they must be delivered directly into or very close to the blood. Some
treatments work very quickly after they are administered whilst others may need significantly more
time to take effect.
TNFi:
•
Inhibits TNF, which is an inflammatory cytokine decrease inflammation.
•
All are monoclonal antibodies except Etanercept (Decoy receptor for TNF)
•
Indications:
•
o
o
o
o
RA,
IBD;
Psoriasis,
Ankylosing spondylitis
o
o
o
o
reactivation of infections: TB, VZV
Drug induced Lupus
worsening of CHF
↑ Risk of BCC, SCC
SE:
•
Contraindicated in
o CHF NYHA III
Non-TNFi:
•
Abatacept- selective T-cells Co stimulation inhibitor
o
o
o
•
Tocilizumab- IL-6 inhibitor
o
o
o
•
Indications:
RA
Giant Cell Arteritis
Juvenile Idiopathic Arthritis
SE:
Infections,
myelosuppression, nephrotoxicity, liver toxicity, hyperlipidaemia
Contraindicated in
Infection
before major surgery
Anakinra- IL-1 inhibitor (requires daily injection)
o
o
o
•
Indications:
RA
SE:
Infections,
COPD exacerbations
Contraindicated in
if patient has infection
before major surgery
Indications:
RA
SE:
Infections,
COPD exacerbations
Contraindicated (same as above)
Rituximab: inhibits CD20 B-Lymphocytes
o
o
Indications:
RA
CLL lymphoma
Immune thrombocytopenic purpura
MS
Autoimmune hemolytic anema
SE:
Toxic epidermal necrolysis
Tumor lysis syndrome
ARDS
Progressive multifocal leukoencephalopathy
58) Humoral immunity changes in rheumatic diseases
RA is an autoimmune-mediated chronic systemic inflammatory disease that primarily affects synovial
joints but often shows extra-articular manifestations. Auto-Ag’s targeted by auto-AB found in RA
display a wide spectrum of cellular components, suggesting that RA is characterized by accumulated
autoreactivities in both B and T cells. Among diverse auto-AB found in patients w/RA, rheumatoid
factor (RF) and anti-citrullinated protein antibody (ACPA) are the two most remarkable that provide
useful clinical and pathophysiological information
Pathogenic Roles of RFs
RFs, directed to the Fc portion of IgG, are normally induced by immune complexes (ICs) and
polyclonal B cell activators such as bacterial LPS and the EBV. The physiological roles of RFs are:
•
To enhance IC clearance by increasing its avidity and size,
•
To help B cells uptake IC, and thereby, efficiently present antigens to T cells
•
To facilitate complement fixation by binding to IgG-containing ICs
Changes in the humoral immune response for RHA
•
RFs are locally produced by B cells in lymphoid follicles and germinal center-like structures
from the inflamed synovium
•
RFs to enhance IC formation w/pre-existing auto-AB, including ACPAs, may potentiate the
arthritogenicities of these auto-AB and perpetuate inflammation.
•
ACPA-containing IC (ACPA-IC) induced proinflammatory responses from macs when formed
in the presence of IgM or IgA RFs
•
A cycle among ACPA generation, immune complex formation, RF production, and chronic
inflammation, eventually leads to tissue damage.
Fc Receptor Binding
•
IgG exerts an effect via multimeric interactions w/the FcR by forming ICs.
•
ICs containing citrullinated peptides may serve as danger-associated molecular patterns
(DAMPs) to stimulate innate immune cells.
•
IC formation w/citrullinated proteins and induction of cytokine secretion
•
FcR engagement by ACPAs are also able to polarize macs to the pro-inflammatory pathways
Complement Activation
•
The key functions of the complement system include clearance of MOs and circulating ICs
through opsonization. Three pathways exist by which the complement system is activated,
each utilizing different recognition molecules to initiate activation: classical, alternative, and
lectin pathways.
•
All of these pathways can be activated by ICs
•
Complement activation products, such as C3a, C5a, or the MAC play an important role in
collagen-induced arthritis.
•
Complement consumption is observed in the synovial fluid of RA patients
NET Formation
•
Neutrophil extracellular traps (NETs) are networks of extracellular fibers primarily composed
of highly condensed chromatins and antimicrobial peptides released from neutrophils, the key
function of which is to trap and kill pathogens.
•
NETosis is a form of programmed cell death characterized by release of NETs.
•
These trigger, including microbial and non-microbial (auto-AB, immune complex, cytokines, or
other stimuli) components can induce NET formation or NETosis via TLRs, FcRs, or
complement receptors on neutrophils (this is part of the innate that leads to humoral via
inflammatory markers)
•
Osteoclastogenesis
•
ACPAs can directly stimulate osteoclast and enhance osteoclastogenesis.
IV.Hematologic diseases
59) Iron deficiency anaemia (IDA)
Definition = lack/ inability of iron to be used in erythropoiesis causing ↓ synthesis of Hb. It is the most
common form of anemia worldwide
Anemia = a ↓ in the total n.o of circulating RBCs, represented by a ↓ in Hb conc., HCT, or RBC count.
It may be due either to inadequate RBC production, excessive RBC destruction, or blood loss
Etiology
•
Insufficient intake of iron (strict vegan diet, chronic undernutrition)
•
↓ absorption of iron =
o
o
o
o
coeliac disease/IBD (abnormal changes in the structure of the duodenum),
insufficient production of HCl (hypo-/achlorhydria) – due to atrophic gastritis,
abnormalities/gastrectomy – alters the acidic environment needed for iron to be
converted into its absorbable form. Also, bariatric surgery: Roux-en-Y bypass
chronic diarrhoea
•
↑ Demand = pregnancy, lactation, growth spurt, EPO therapy
•
↑ Loss
o
o
Blood loss/bleeding = GI bleeding: PUD, IBD, ↑NSAID use, GI/Colon cancer,
Hookworm infection – Helminthiasis
Menorrhagia, Hemophilia, vW disease
Meckel diverticulum, Dialysis-dependent renal failure, Frequent blood donation
Pathophysiology
Iron deficiency → ↓ binding of iron to protoporphyrin (last rxn in heme synthesis) → ↓ production of
Hb
Clinical manifestations
•
Signs and symptoms of anemia = fatigue, lethargy, pallor (seen in conjunctiva), cardiac
symptoms (tachycardia, angina, dyspnoea on exertion, pedal oedema, and cardiomyopathy in
severe cases)
•
Brittle nails, koilonychia (spoon-like nail deformity); hair loss
•
Pica (eating disorder characterised by appetite for and ingestion of non-nutritive substances
like hair, plant, cloth), dysphagia
•
Angular cheilitis = inflammation and fissuring of the corners of the mouth
•
Atrophic glossitis = erythematous, oedematous, painful tongue w/loss of tongue papillae
(smooth, bald appearance)
•
IDA can be associated w/Plummer-Vinson syndrome = triad of IDA, post-cricoid dysphagia,
and upper oesophageal webs. It is associated w/an ↑ risk of oesophageal squamous cell
carcinoma and glossitis
•
MNEMONIC = DICEd Plumm – Dysphagia, IDA, Carcinoma of the oesophagus, Esophageal
webs in Plummer-Vinson syndrome
Diagnosis
CBC
•
↓ Hb, ↓ HCT, ↓ RBC (initially normal, ↓ w/prolonged deficiency)
•
↓ MCV = microcytic (can also be normocytic); ↓ MCH = hypochromic
•
Normal/ ↓ reticulocyte count
•
↑ RDW (Red cell Distribution Width) = differentiates IDA from anaemia of chronic disease and
thalassemia traits (where RDW is usually normal)
•
↑ platelet count (reactive thrombocytosis)
Iron studies
•
↓ serum ferritin; ↓ serum iron↓ transferrin saturation (<20%); ↑ serum transferrin and ↑
TIBC (total iron binding capacity) and sTfR (Serum soluble transferrin receptor) – combo of
these 3 results is diagnostic of IDA (NB! ↑ ferritin doesn’t rule out IDA as it could be ↑ in
response to simultaneous inflammation)
•
↑ serum free erythrocyte protoporphyrin; normal or ↑ EPO
Change
Parameter
↓
Hb, HCT, RBC, MCV, MCH, serum ferritin, serum iron
↑
TIBC, transferrin, RDW, platelet count
Peripheral blood smear = Anisocytosis and hypochromasia (↑ zone of central pallor).
Bone marrow biopsy (rarely indicated) = in patients w/suspected IDA and non-diagnostic iron
studies, low bone marrow iron is diagnostic of IDA
Evaluation of underlying cause =
•
GI cause - occult GI bleeding – Colonoscopy with EGD.
•
Stool analysis – for ova and parasites
•
Gynecologic cause – Menorrhagia workup
•
Renal – Urinalysis, Renal US
•
Pulmonary – Iron staining of sputum sample, chest imaging
Treatment
•
Diet modification = ↑ consumption of iron-rich diet (meats, iron-fortified food, fresh green leafy
veg)
•
Oral iron therapy = indicated in all patients w/IDA and initially administered for 3-6 months.
Adequate response if Hb >1g/dl in 1 month.
Adverse effects (are common leading to intolerance, nonadherence) include GI discomfort,
nausea, constipation, black stool.
Absorption may be enhanced by consumption of vitamin C; foods and drugs that ↓ intestinal
absorption should be avoided
o Ferrous sulfate 325mgx1
o Ferrous fumarate 325mgx1
o Ferrous gluconate 325mgx1
•
Parenteral iron therapy = for patient’s intolerant to oral therapy, for those w/intestinal
malabsorption and chronic bleeding despite oral therapy.
Adverse effects: Thrombophlebitis, Myalgia, arthralgia, and headaches within 1–2 days of
infusion. Rarely anaphylaxis
Available forms include
o Iron dextran: 1st dose- 25mg then 100mg i.v. daily
o
o
o
•
Iron sucrose 200mg i.v Once per week
Ferrous gluconate 125mg i.v Once per week
Ferumoxytol 510mg i.v Once per week
Blood transfusion = recommended for severe anaemia (Hb <7 g/dL).
o
•
Avoid in hemodynamically stable patients with mild to moderate IDA
Treat the underlying cause
o Hookworm infection: Antihelminthics
o
o
o
Malnutrition or malabsorption: Identify and treat with supplements
GI – H.pylori eradication therapy
Uterine bleeding – hormonal therapy
60) Macrocytic and megaloblastic anaemias
Definition =
•
Macrocytic anaemia = anaemia in which the RBCs are larger than their normal volume (↓
Hb, high MCV > 100 fL). It can be classified according to bone marrow appearance as
megaloblastic and non-megaloblastic macrocytic anaemia
•
Megaloblastic anaemia = impaired DNA formation during RBC production due to lack of B12/
folate in their active forms or use of anti-metabolite drugs. It is characterised by many large,
immature, and dysfunctional RBC (megaloblasts) in the bone marrow and by hyper
segmented neutrophils
•
Vitamin B12 and folate/folic acid deficiency anaemia = anaemia caused by lack of vit B12
(and folic acid) leading to impaired DNA replication and mitosis of hemopoietic cells
(erythroblasts, Myelocytes, megakaryocytes which are bigger than usual), epithelial and
neuroepithelial cells
Etiology
Vitamin B12 deficiency
•
Malabsorption = ↓ intrinsic factor (IF) – due to atrophic gastritis (autoimmune atrophic gastritis
– most common cause of B12 deficiency, or H. pylori infection) or gastrectomy
•
↓ uptake of IF-B12 complex in terminal ileum due to = alcohol use disorder, IBD, coeliac,
pancreatic insufficiency, surgical resection of the ileum
•
Malnutrition = anorexia nervosa, strict vegan diet
•
↑ demand = pregnancy, lactation, leukaemia, fish tapeworm infection
• ↓ absorption from meds = neomycin, metformin, PPI
Folate deficiency
•
Malabsorption = IBD, coeliac, surgical resection of the SI
•
Malnutrition = alcohol use disorder, unbalanced diet (“tea and toast” diet)
•
↑ demand = pregnancy, lactation, severe hemolytic anemia
•
Drug related = methotrexate, anti-epileptic drugs (phenytoin), trimethoprim
Pathophysiology
Vitamin B12 deficiency
•
Vitamin B12 is a water-soluble cofactor for enzymatic rxns of DNA synthesis (via methionine
synthase) and odd-chain FA metabolism (via methylmalonyl CoA mutase). A deficiency of
B12 leads to enz. dysfunction
•
Dysfunctional methionine synthase = ↓ tetrahydrofolate (THF – cofactor in AA and nucleic acid
synthesis) → ↓ DNA synthesis → large, nucleated hematopoietic cells including megaloblasts
→ megaloblastic precursors undergo apoptosis or are phagocytosed → pancytopenia. ↓
methionine → neuropathy; ↑ homocysteine → endothelial damage → predisposes to CV
disease
•
Dysfunctional methylmalonyl CoA mutase = accumulation of methylmalonyl CoA and its
precursor which replaces acetyl-CoA in neuronal membranes → demyelination →
neurological manifestations
•
Pernicious anemia = type of B12 deficiency caused by auto-AB against IF and/or gastric
parietal cells (type 2 HS rxn)
Folate deficiency
•
Similar to above - ↓ THF → ↓ DNA synthesis → megaloblastic erythropoiesis and
megaloblastic anaemia (+ ↓ in other cell lines)
•
↓ methionine + ↑ homocysteine → endothelial damage → ↑ risk of CV disease
•
During fetal development = nucleotide synthesis impairment → NT defects
Clinical manifestations
Vitamin B12 deficiency
•
Signs of anaemia = fatigue, pallor
•
Mild scleral icterus and/or jaundice; worsening vision
•
Autonomic dysfunction = impotence, incontinence
•
Glossitis
•
Neuropsychiatric disease = e.g. reversible dementia, depression, paranoia
•
Neurological disturbances are generally symmetrical = peripheral neuropathy (tingling,
paresthesia, coldness).
Subacute combined degeneration of the spinal cord with the following symptoms:
Paresthesia, impaired proprioception, loss of vibratory sensation, tactile sensation, and
position discrimination due to demyelination of the dorsal columns
Spastic paresis due to demyelination of the lat. corticospinal tracts
Gait abnormalities resulting from damage of spinocerebellar and dorsal columns
Folate deficiency = signs of anaemia; glossitis; no neurological symptoms
Diagnosis
Vitamin B12 deficiency
•
Signs of megaloblastic anemia = ↓ Hb, ↑ MCV (macrocytic), ↑ MCH (hyperchromic),
hypersegmented neutrophils, ↓ reticulocytes
•
Frequently thrombocytopenia and leukopenia (possibly pancytopenia)
•
If vitamin B12 levels are normal, then check for = homocysteine (↑); and methylmalonic acid
(MMA) (↑) to help rule out folate deficiency
•
If B12 levels are ↓, determine the underlying cause = test for auto-AB (anti-IF and anti-parietal
cell AB). If auto-AB are –ve, perform Schilling test (to determine cause of B12 deficiency),
gastroscopy, or D-xylose absorption test
Stages of Schilling
test
Stage 1
Stage 2
Description
Oral radiolabelled B12 + IM
dose of unlabeled B12
Oral radiolabelled B12 + IF
Radiolabelled B12 measures in urine
•
Normal excretion = malnutrition or ↑
demand is most likely cause
•
↓ excretion = perform stage 2
•
Normal excretion = malabsorption due to
lack of IF
•
↓ excretion = perform stage 4
Stage 3
Oral radiolabelled B12 + anti-B
Stage 4
Oral radiolabelled B12 +
pancreatic enz.
•
Normal excretion = bacterial overgrowth
•
↓ excretion = perform stage 4
•
Normal excretion = lack of pancreatic
enz. (e.g. chronic pancreatitis)
Folate deficiency
•
Signs of megaloblastic anaemia
•
↑ homocysteine; MMA is normal (unlike B12 deficiency, where MMA is ↑)
•
Hypersegmented neutrophils and pancytopenia may be present)
•
Folate serum levels are not reliable – some healthy patients exhibit folate levels below the
normal range
Treatment
Vitamin B 12 deficiency
•
IM supplementation of vitamin B12 (e.g. cyanocobalamin, hydroxycobalamin)
•
Prevent future deficiency by treating the underlying disease
Folate deficiency
•
Oral folate supplementation for 4 months or until hematologic recovery takes place
•
Nutritional counselling to ↑ folate uptake
•
Due to risk of NT defects, F trying to become pregnant should initiate folate supplementation
before conception
61) Hemolytic anaemias. Hemolysis
Definition = hemolytic anaemias a group of conditions characterised by an excessive breakdown of
RBC’s. They can be classified according to the cause of hemolysis (intrinsic or extrinsic) and by the
location of hemolysis (intravascular or extravascular)
Etiology
Type
Definition
Causes
By RBC pathology
Intrinsic
↑ destruction of RBCs due to a
defect w/in the RBC (often
inherited disorder)
•
RBC membrane defects = hereditary spherocytosis,
paroxysmal nocturnal haemoglobinuria (PNH)
•
Enz. defects = G6PD deficiency, pyruvate kinase deficiency
(PKD)
•
Haemoglobinopathies = SCA, thalassemia, haemoglobin C
disease
Extrinsic
Abnormal breakdown of
normal RBCs
•
Mechanical destruction in large vessels
•
Shearing of RBCs due to occlusion of small vessels by
microthrombi
•
Immune rxns due to infections (mycoplasma) or tumours
(CLL)
•
Infections causing ↑ destruction of RBCs (malaria, babesia)
•
Isoimmune rxns (ABO/Rh incompatibility)
•
↑ degradation by the spleen (Hypersplenism)
•
Toxins (snake bites) and oxidising agents (Cu poisoning)
•
G6PD deficiency
•
Immune-mediated anemia (PNH, transfusion ABO
By location of RBC breakdown
Intravasc
ular
↑ destruction of RBCs w/in the
blood vessels
incompatibility, hemolytic anemia of newborn)
Extravasc
ular
↑ destruction of RBCs by the
reticuloendothelial system
(mainly the spleen)
•
Macroangiopathic anemia (mechanical destruction by
prosthetic heart valves)
•
Microangiopathic anemia (DIC, SLE, HELLP syndrome)
•
RBC defects (SCA, spherocytosis, PKD)
•
Immune-mediated anaemia (warm and cold agglutinin
disease, PNH)
Clinical manifestations
•
Signs of anemia = fatigue, pallor, exertional
dyspnoea; in severe cases = tachycardia, angina,
leg ulcers
•
Signs of hemolysis = jaundice, pigmented
gallstones (due to accumulation of indirect bilirubin
in bile), splenomegaly (extravascular), back pain
and dark urine in severe hemolysis w/haemoglobinuria
•
Signs of ↑ hematopoiesis (mostly in severe chronic anaemias e.g. thalassemia)
Bone marrow expansion = widening of the diploic space of the skull, biconcave
deformity of the vertebral bodies
Cortical thinning and softening of the bone → ↑ risk of pathologic fractures
Extramedullary hematopoiesis = hepatosplenomegaly
Diagnosis
Approach
1. Perform initial laboratory studies to confirm anemia and hemolysis
2. Anemia workup: CBC w/ MCV, reticulocyte count + classify anemia by morphology
3. Hemolysis workup: Add LDH, haptoglobin, bilirubin, urinalysis, and peripheral blood
smear (PBS)
4. Obtain a direct Coombs test (i.e., DAT) to narrow the differential:
a. DAT positive: antibody-mediated hemolytic anemia
b. DAT negative: nonantibody-mediated hemolytic anemia
5. Consider further investigations of the underlying etiology based on clinical suspicion and DAT
results.
6. !! If the patient has severe symptoms of anemia or a life-threatening cause is suspected (i.e.,
TTP/HUS, DIC, HELLP syndrome, acute hemolytic transfusion reaction), proceed directly to
treatment in parallel with diagnostic evaluation.
CBC
• ↓ Hb, HCT, and RBC
• MCV = depends on underlying condition and acuity of hemolysis –
o normal in most hemolytic anaemias; (consider a. of chronic disease)
o ↑ in severe reticulocytosis; (consider macrocytic anemia)
o ↓ in thalassemia; (consider IDA)
• WBC count can be ↑ in inflammation/malignancy;
• ↓ platelets in microangiopathic hemolytic anemia + Evan syndrome (TTP+AIHA)
• Reticulocytes: use corrected RC count for patients w/ anemia
o ↑ reticulocytes (≥ 2%) – loss of RBC → reactive ↑ in erythropoiesis → ↑ in reticulocytes
in the peripheral blood
o Can be normal: due to delayed bone marrow response or concomitant bone marrow
suppression/ disease
Specific workup
BLOOD
• ↓ haptoglobin < 25–28 mg/dL (only free, unbound haptoglobin is measured) = in blood plasma,
haptoglobin binds free Hb released from broken down RBCs, resulting in ↓ free circulating
haptoglobin
• ↑ lactate dehydrogenase (LDH) = non-specific; indicates ↑ cellular breakdown
o
↑↑ (4-5 times) intra-vascular, ↑ extravascular
• ↑ indirect (unconjugated bilirubin) = Hb released from RBC → heme is catabolised to
unconjugated bilirubin, which accumulates → jaundice
o Marker for extravascular hemolysis
URINE
• ↑ Urobilinogen in urine usually in extravascular hemolysis
o
unconjugated bilirubin + albumin → this complex is transferred to the liver and
metabolised to conjugated bilirubin → conjugated bilirubin is excreted via bile and
turned into urobilinogen by colonic bacteria → urobilinogen is reabsorbed into
enterohepatic circulation and excreted in urine
• Hemosiderinuria usually in intravascular hemolysis
o
Hb taken up by PCT → haemic iron is trapped w/in epithelial cells of the tubule,
forming hemosiderin → cells containing hemosiderin are sloughed off and excreted
into the urine → brown colour
• Hemoglobinuria usually in intravascular hemolysis
o In hemolytic crisis = ↑ free Hb → Hb binds to transport proteins → if max capacity of
these proteins is reached, free Hb circulates in the bloodstream → haemoglobinuria →
brown-coloured urine
Coombs test
• The direct Coombs test detects AB attached directly to the RBC surface
• The indirect (or not direct) Coombs test detects serum AB not bound to RBCs
• The test uses Coombs serum, which contains anti-human globulins. A +ve result in a patient
w/hemolysis supports the diagnosis of AB-mediated, extracorpuscular anemia
Peripheral blood smear = used to detect pathologic RBC forms
• Intravascular hemolytic anemia = schistocytes, Heinz bodies and bite cells in G6PD deficiency,
intracellular organsisms (malaria, babesiosis [ixodes]) ↑ reticulocytes
• Extravascular hemolytic anemia = sickle cells in SCA, target cells in SCA and thalassemia (also
teardrop cells), Hb C (also Hb crystals w/in RBC), smudge cells in CLL, ↑ reticulocytes
Measure ADAMTS13 activity if there is no obvious secondary cause of MAHA
• ADAMTS13 activity ≥ 10%: TTP unlikely
• ADAMTS13 activity < 10%: TTP likely
Treatment
• Symptomatic treatment by blood transfusion, if there is marked anemia. (contraindicated w/+ve
Coombs test)
• MAHA (Microangiopathic HA): Medical EMERGENCY
o If TTP suspicion is high: Refer for urgent plasma exchange (plasmapheresis). consider
o
corticosteroid therapy (e.g., prednisone 1mg/kg).
Treat secondary cause: HELLP, Hypertensive emergency, DIC
• In severe immune-related hemolytic anemia = steroid therapy
• In steroid resistant cases = rituximab or addition of an immunosuppressant (azathioprine,
cyclophosphamide)
• Sometimes splenectomy can be helpful where extravascular hemolysis, or hereditary
spherocytosis, is predominant
• Pyruvate Kinase deficiency- Phototherapy and/or exchange transfusions
62) Aplastic anaemia. Agranulocytosis
Aplastic anaemia
Definition = a disorder of pluripotent bone marrow stem cells that results in a ↓ of all 3 hematopoietic
cell lines – RBCs, WBCs, and platelets (pancytopenia). (Pancytopenia caused by bone marrow
insufficiency)
Etiology
•
Idiopathic in >50% of cases – possible immune-mediated; may follow acute hepatitis
(hepatitis-associated aplastic anemia)
•
Medication side effects = carbamazepine, methimazole, propylthiouracil, NSAIDs,
chloramphenicol, sulfa drugs, cytostatic drugs (esp. alkylating agents/ antimetabolites)
•
Toxins = benzene, cleaning solvents, insecticides
•
Ionising radiation
•
Viruses = parvovirus B19, HBV, EBV, CMV, HIV
•
Fanconi anaemia = a hereditary AR disorder due to a DNA crosslink repair defect resulting in
bone marrow failure
Pathophysiology
Exact mechanisms are unknown. It is suggested that exposure to etiological agents generates a
cellular immune response resulting in production of cytokines by activated T cells → suppress normal
stem cell growth and development
Clinical manifestations
•
Onset may be insidious or may occur suddenly w/great severity; may occur at any age
•
Anemia (↓ RBC) = fatigue, pallor, malaise
•
↓ platelets = purpura, petechiae, ecchymosis, mucosal bleeding
•
↓ neutrophils/WBC = ↑ susceptibility to infection
Diagnosis
•
CBC = pancytopenia; normochromic normocytic/ macrocytic anaemia
•
↓ Reticulocytes <0.2%, since the marrow is not producing any RBC
•
↑ EPO
•
Bone marrow biopsy = hypocellular fat-filled marrow (dry bone marrow tap); RBCs normal
morphology
Treatment
•
Remove the causative agent
•
Supportive therapy = treatment of infections, blood and platelet transfusions
•
Bone marrow stimulants (e.g., GM-CSF, eltrombopag)
•
Immunosuppressive therapy (to prevent further autoimmune marrow destruction) =
cyclosporine, tacrolimus, alemtuzumab
•
Consider hematopoietic cell transplantation in young patients
Agranulocytosis
Definition = absence of granulocytes or severe neutropenia (usually defined as absolute neutrophil
count < 500/mm3)
Etiology
Drug-induced agranulocytosis (~70% of cases)
•
Immune-mediated mechanism (type 2 HS rxn) = drugs or drug-protein complexes stimulate
the development of AB against granulocytes
•
Drug toxicity mechanism = direct damage to myeloid precursors = e.g., anti-thyroid drugs,
anti-inflammatory (sulfasalazine, NSAIDs), anti-B (TMP/SMX), anti-psychotics (clozapine),
anti-convulsants (carbamazepine), chemotherapeutic agents, colchicine
Drug-independent agranulocytosis (~30% of cases)
•
Bone marrow disorders and malignancies = aplastic anaemia, leukaemia, myelodysplastic
syndromes, vitamin B12 deficiency, folate deficiency
•
Peripheral granulocyte destruction = hypersplenism, autoimmune diseases
Clinical manifestations
•
May be asymptomatic
•
Triad of = aphthous stomatitis, sore throat (agranulocytic angina), and fever
•
Infection of any organ may be rapidly progressive (e.g., pneumonia, UTIs)
Diagnosis
•
CBC = absolute neutrophil count < 500/mm3
•
Bone marrow biopsy = normocellular (normal amounts and types of cells) blood marrow
w/underdeveloped promyelocytes (if fully matured, would have been the missing
granulocytes)
Treatment
•
If drug-induced = stop causative agent
•
Consider G-CSF (filgrastim) for non-drug induced cases, or following chemo
•
Anti-B for infection
•
Close monitoring of WBC
63) Hodgkin’s lymphoma (HL)
Definition = a malignant lymphoma that is typically of B-cell origin. It has a bimodal age distribution,
w/peaks in the 3rd and 6th-8th decades of life.
Etiology
The exact causes are unknown, but several risk factors have been associated w/HL:
•
Strong association w/Epstein-Barr virus (EBV)
•
Immunodeficiency = organ/cell transplantation, immunosuppressants, HIV, chemo
•
Autoimmune diseases = e.g., RA, sarcoidosis
Clinical manifestations
•
Painless lymphadenopathy (painless enlargement of the lymph nodes)
Cervical lymph nodes (~60-70% of patients) > axillary lymph nodes (~25-35% of
patients) > inguinal lymph nodes (~8-15% of patients)
Involvement of a single group of lymph nodes
Contiguous pattern of lymph node spread
Mediastinal mass → chest pain, drug cough, and SOB
Splenomegaly and hepatomegaly may occur if the spleen or liver are involved
•
B symptoms = night sweats, weight loss >10% in the past 6 months, fever >38°C
•
Non-specific back pain: nephrotic syndrome (caused by minimal change disease)
•
Pel–Ebstein fever (cyclical fever) = intermittent fever w/periods of high temp for 1-2 weeks,
followed by afebrile periods for 1-2 weeks. Relatively rare but specific for HL
•
Alcohol-induced pain = pain in involved lymph nodes after ingestion of alcohol. Relatively rare
but highly specific for HL
•
Pruritus (focal or generalised)
Staging (Cotswold modified Ann Arbor system)
Stage
Description
I
Involvement of 1 lymph node (IN) or 1 extranodal focus (IE)
II
Confined to 1 side of the diaphragm = involvement of ≥2 (IIN) lymph node areas or extranodal
foci (IIE)
III
On both sides of the diaphragm = involvement of ≥2 (IIIN) lymph node areas or extranodal foci
(IIIE)
IV
Disseminated spread = into ≥1 extralymphatic organs independent of lymph node involvement
Each stage is classified: A (no symptoms), B (symptoms are present), E (extra-lymphatic involvement), or
S (splenic involvement)
Diagnosis
•
CBC = ↑/↓ WBC count; Anemia; Eosinophilia
•
Serum chemistry = ↑ LDH; hypercalcemia (due to paraneoplastic syndrome)
•
Histology of lymph node biopsy (obligatory) = Reed-Sternberg cells (RSCs)
(pathognomic/Hallmark of HL); Hodgkin cells (mononuclear, malignant B cells); inflammatory
background (lymphocytes, neutrophils, eosinophils, macs, plasma cells); granuloma formation
•
CXR/CT = detection and measurement of masses and enlarged lymph nodes in chest,
abdomen, and pelvis
•
Bone scintigraphy or PET-CT = performed before treatment to assess disease spread
Classification
Classification
Subtype
Classical HL (95%)
Nodular sclerosing
(NSHL)
Characteristics
•
Most common subtype
•
Localisation = mediastinal
and cervical
Mixed-cellularity
(MCHL)
•
Good prognosis
•
Commonly found in
immunocompromised
patients
•
Localisation = abdominal
Pathology
Nodules of RSCs w/in
lacunae, separated by
collagenous tissue
w/sclerosing appearance;
Lymphocyte rich
Nodules w/numerous RSCs,
and ↑ n.o of histiocytes,
eosinophils, and plasma cells
and splenic
Lymphocyte-rich
(LRHL)
Lymphocyte
depleted (LDHL)
•
Good prognosis (slightly
worse than NSHL)
•
Rare
•
Localisation = cervical and
axillary
•
Very good prognosis
•
Very rare
•
Commonly found in
Presence of RSCs, and
reactive lymphocytosis that
causes distortion of the lymph
node architecture
Numerous RSCs, and ↓ n.o of
lymphocytes
immunocompromised
patients
Nodular
predominant HL
(5%)
Nodular
lymphocyte
predominant HL
(NLPHL)
•
Localisation = below the
diaphragm
•
Poor prognosis
•
Rare
•
Very good prognosis (but
slightly worse than LRHL)
Popcorn cells.
Lymphocyte predominant
cells; tumour cells are –ve for
CD15 and CD30
Treatment
•
Early stage (I and II) = combo of chemo and radiotherapy – chemo approach is
o
•
ABVD (adriamycin, bleomycin, vinblastine, dacarbazine)
Advanced stage (III and IV) = combo of chemo and radiotherapy in select cases. 3 possible
treatment approaches are commonly considered:
ABVD
Stanford V = doxorubicin, vinblastine, mechlorethamine, vincristine, bleomycin,
etoposide, prednisone
BEACOPP = bleomycin, etoposide, adriamycin (doxorubicin), cyclophosphamide,
oncovin (vincristine), procarbazine, prednisone
•
Primary refractory or relapsed disease = trial of alternative chemo or consideration of highdose chemo and autologous stem cell transplantation
•
Unfavorable factors for Hodgkin lymphoma (relevant for treatment regimen dosages)
o High ESR
o High LDH
o Involvement of three or more lymph node areas
o Large mediastinal tumor
o Bulky disease (tumors measuring ≥ 10 cm across)
Prognosis
•
•
Good prognosis
o
5-year survival rate ∼ 80–90% (in children > 90%)
o
o
Best prognosis: LRHL and NLPHL
Prognosis is largely determined by disease stage (lower stage w/ better prognosis)
∼ 10–20% of patients will develop secondary malignancies (especially lung cancer; related to
radiation therapy and chemotherapy)
64) Non-Hodgkin’s lymphomas (NHL)
Definition = a group of blood cancers that includes all types of lymphomas except HL. They account
for 95% of lymphomas (they are the most common hematopoietic neoplasm, being ~10X > common
than HL). Incidence ↑ w/age, peak incidence >50yrs
Etiology = exact cause is unknown
•
Chromosomal translocation = most commonly t(14:18)
•
Infections = EBV, HIV, HTLV-1 (human T-cell lymphotropic virus), HCV, H. pylori (associated
w/gastric lymphomas: MALT, DLBCL)
•
Autoimmune disease = hashimoto thyroiditis, RA
•
Immunodeficiency = congenital immunodeficiency, AIDS, history of chemo and/or
immunosuppressive therapy
•
Environmental factors = aromatic hydrocarbons (benzene), radiation
Classification
B cell lymphomas (85% of all NHL) = follicular lymphoma (most common low-grade in adults), and
diffuse large B-cell lymphoma (most common NHL in adults). (Visit amboss)
Follicular lymphoma
Indolent
(low-grade)
Hairy cell leukemia
Marginal zone B-cell lymphoma
Waldenstrom macroglobulinemia
Small Lymphocytic lymphoma
Aggressive
(high-grade)
Diffuse large B-cell lymphoma
Mantle cell lymphoma
Burkitt lymphoma (most common in children)
Precursor B-cell Lymphoblastic lymphoma
T cell lymphomas (15% of all NHL) = mycosis fungoides is the low grade and high-grade forms
include Sezary syndrome, adult T-cell lymphoma, among others (visit amboss)
Indolent
(low-grade)
Mycosis fungoides
Sezary syndrome
Aggressive
(high-grade)
Adult T-cell lymphoma
Aggressive NK-cell leukemia
Angioimmunoblastic T-cell lymphoma
Precursor T-cell Lymphoblastic lymphoma
Clinical manifestations
•
Nodal:
o
o
o
•
Extranodal: symptoms depend on the affected tissue. B symptoms are common.
o
o
o
o
•
Painless lymphadenopathy w/ fatigue = involvement of multiple lymph nodes; noncontiguous pattern of spread
High grade
Rapidly growing mass/ nodes
B symptoms = weight loss, fever, night sweats
Low grade
Slow-growing lymphadenopathy (over months-years)
Splenomegaly, hepatomegaly
Signs of bone marrow involvement: anemia, bleeding, ↑ susceptibility to
infections
GI tract: e.g., early satiety, GI bleeding
Neurological: e.g., headache, focal neurologic symptoms
Primary cutaneous NHL/ secondary skin infiltration: rash, plaques, tumors, ulcers
Thyroid involvement (rare): e.g., nodules, goiter
Oncologic emergencies/paraneoplastic syndromes (seen in advanced stages)
o Tumor lysis syndrome,
o Hypercalcemia,
o Spinal cord compression,
o Superior vena cava syndrome,
o Cardiac tamponade,
o Lymphomatous meningitis, and a CNS mass.
Diagnosis
Labs
•
CBC = ↑/↓ WBC (commonly leukopenia, lymphocytosis), anemia, thrombocytopenia
•
Serum chemistry = ↑ LDH, hypercalcemia (secondary to paraneoplastic syndrome in
aggressive NHL), serum β2-microglobulin: may be ↑
•
Virus serology testing (e.g., HIV serology, HBV, HCV, EBV, HTLV-1)
Confirmatory tests
•
Nodal disease
o
o
•
Excisional lymph node biopsy = monomorphous lymphocytic proliferation
Alternatives: Core-needle, incisional lymph node biopsy
Extranodal disease
o
Excisional tissue biopsy w/ endoscopy/US
•
Bone marrow aspiration and biopsy = in all patients for staging
•
Immunohistochemistry = B cell lymphomas are CD20+; T cell lymphomas are CD3+
•
Imaging = X-ray and CT (for staging); MRI (patients w/neurologic symptoms); endoscopy (for
tumour localisation, staging, biopsy); possible PET-CT
•
Lumbar puncture w/CSF examination (cytology; detection of EBV DNA)
HL vs. NHL
Feature
Hodgkin’s lymphoma
Age distribution
Non-Hodgkin’s lymphoma
Bimodal (late adolescence and older
adulthood)
Etiology
•
Immunosuppression
•
Chromosomal translocation
•
EBV infection
•
Autoimmune diseases
•
Infections
•
Multiple lymph node groups
•
Can start in almost any part of the
•
Lymph node
involvement
↑ w/age (peak > 50 years)
Localised to a single group of
nodes above the diaphragm
•
Starts in a single node
•
Orderly, stepwise spread
(contiguous)
•
body
•
Non-orderly spread (non-contiguous)
•
Extranodal involvement common
Extranodal involvement rare
Histology
Reed Sternberg cells
Majority are neoplastic cells of B-cell lineage
Prognosis
Good
Worse
Staging = similar to the one used for HL. Classification:
•
Limited disease (stage I + II) = lymph node involvement confined to 1 side of the diaphragm
•
Advanced disease (stage III and IV) = lymph node and/or extranodal involvement on both
sides of the diaphragm
Treatment
The choice of treatment is mainly based on the tumour grade, rather than the disease stage. There
are a few exceptions such as primary CNS lymphoma (intrathecal MTX + chemo), hairy cell
leukaemia, Burkitt lymphoma, CLL, multiple myeloma.
Grade
Low grade NHL
High grade NHL
Stage
Therapeutic intention
Therapy
Limited stage
Curative
Radiation therapy
Advanced stage
Palliative
Watch and wait;
polychemotherapy
All stages
Curative
Polychemotherapy
Polychemotherapy:
•
Most NHL = CHOP regimen – Cyclophosphamide, Hydroxydaunorubicin (doxorubicin),
Oncovin (vincristine), Prednisolone
•
B-cell NHL = R-CHOP – combo of CHOP + CD20 AB (rituximab)
Additional measures
•
Supportive treatment: adequate hydration + nutrition, DVT prophylaxis, anti-emetics for chemo
induced n/v.
•
If patients benefit, then: splenectomy (B-cell lymphomas, hairy cell leukemias)/ hematopoietic
stem cell transplantation (HSCT): (DLBCL, Mantle cell, Mature T-cell)
Prognosis
•
Typically, the prognosis of NHL is worse than that of Hodgkin lymphoma.
o Low-grade lymphomas: median survival of 6–10 years
o High-grade lymphomas: survival typically several months (years in less aggressive
variants)
•
Indicators of poor prognosis: old age, number of involved nodal and extranodal sites, ↑ LDH, ↑
beta2 microglobulin
65) Chronic lymphocytic leukaemia (CLL)
Definition = low-grade B-cell lymphoma w/lymphocytic leukocytosis (↑ WBC) – a monoclonal disorder
characterised by a progressive accumulation (due to uncontrolled proliferation) of functionally
incompetent lymphocytes). It is the most common type of leukaemia in adults.
Etiology = unknown
Risk factors include = advanced age, environmental factors (organic solvents), M sex (2X > likely),
family history, possible persistent EBV infection or other factors causing chromosomal abnormalities
Pathophysiology
Acquired mutation in hematopoietic stem cells → ↑ proliferation of leukaemic B cells w/impaired
maturation and differentiation in the bone marrow, resulting in:
•
Suppression of the proliferation of normal blood cells = immunosuppression
(hypogammaglobulinemia, granulocytopenia), thrombocytopenia, anemia
•
Infiltration of the lymph nodes, liver, and spleen
Clinical manifestations
•
~50% of cases remain asymptomatic for a long period, resulting in late or incidental diagnosis
•
B symptoms = weight loss, fever, night sweats, fatigue
•
Painless lymphadenopathy; hepatomegaly and/or splenomegaly may occur
NB! Lymphadenopathy is a typical finding in lymphoid malignancies such as CLL and
helps to differentiate CLL from CML, a myeloid malignancy
•
Repeated infections = severe bacterial infections (necrotic erysipelas), mycosis (candidiasis),
viral infections (herpes zoster)
•
Symptoms of anaemia (fatigue, pallor) and thrombocytopenia (mucosal bleeding, bruising,
petechiae)
•
Dermatologic symptoms = leukaemia cutis, chronic pruritus, chronic urticaria
Diagnosis
•
CBC = persistent lymphocytosis w/high % of small mature lymphocytes; findings that indicate
suppression of normal myelopoiesis (granulocytopenia, low RBC and platelet counts)
•
Blood smear = smudge cells (Gumprecht shadows) – mature lymphocytes that rupture easily
and appear as artefacts on a blood smear
MNEMONIC = in CLL, the smudge cells on peripheral smear appear to be Crushed
Little Lymphocytes
•
Flow cytometry = detection of B-CLL immunophenotypes (CD5, CD19, CD20, CD23)
•
Serum AB electrophoresis = AB deficiency (↓ γ globulin fraction)
•
Bone marrow aspiration (may help during later stages of the disease) = high % (>30%) of
small, mature lymphocytes; ↓ n.o of myeloid progenitor cells
•
Genetics = FISH analysis to detect mutations associated w/CLL (e.g. del(17p13))
•
Others = US (spleno/hepatomegaly, liver histology, lymph node biopsy)
DDx = ALL, autoimmune hemolytic anemia, mantle cell or hairy cell lymphomas
Staging – uses the Rai staging system
Stage
Risk
0
Low risk
I
II
III
IV
Intermediate risk
High risk
Finding
Isolated lymphocytosis (>15,000/mm3)
+ Lymphadenopathy
+ Hepatomegaly and/or splenomegaly
+ Anaemia (Hb < 11 g/dL)
+ Thrombocytopenia (< 100,000/μL)
Treatment
CLL is a low-grade malignancy, noted for its slow rate of cell division and disease progression;
treatment is often not necessary or is unlikely to improve survival time. Medical therapy is palliative,
and the only curative treatment option is stem cell transplantation.
•
Asymptomatic CLL (Rai stage 0, slow disease progression) = observe and monitor disease
progression
•
Symptomatic CLL or advanced stage (Rai stage > 0, accelerated disease progression) =
chemotherapy; if CD20+ = rituximab; targeted therapy w/ibrutinib
•
Refractory CLL or early recurrence in fit, young patients = allogeneic stem cell transplantation
•
Treatment regimens: 65-70yrs= Chlorambucil+Rituximab, Ibrutinib; <65yrs (FCR=
Fludarabine, Cyclophosphamide, Rituximab); Del(17p13)+ve= Alemtuzumab
66) Myeloma multiplex/multiple myeloma (MM) (AKA plasmacytoma,
plasma cell myeloma, myelomatosis, Kahler’s disease)
Definitions
•
Plasma cell dyscrasia = a group of conditions characterised by the abnormal proliferation of
the same type (monoclonal) of a plasma cell that may also secrete a monoclonal Ig and/or Ig
fragment (e.g. light chain)
•
Plasmacytoma = an early-stage plasma cell dyscrasia characterised by a single lesion that
affects bones (solitary plasmacytoma of bone) or soft tissue (solitary extramedullary
plasmacytoma), or in rare cases multiple solitary lesions in soft tissue, bone, or both (multiple
solitary plasmacytoma)
•
Multiple myeloma = a malignant plasma cell dyscrasia characterised by uncontrolled
proliferation and the diffuse infiltration of monoclonal plasma cells (which produce monoclonal
paraprotein – M-protein) in the bone marrow
Classification = based on immunoglobulin type
•
IgG and IgA = typical MM; majority of patients
•
Bence Jones protein (free light chains excreted in urine) = 15-30% of MM
•
IgD, IgE, and IgM = very rare subtypes of MM
Etiology = unknown.
Risk factors include = chronic immune stimulation, autoimmune disorders, ionising radiation,
occupational exposure to pesticides/herbicides, infection (chronic infections, HSV, EBV etc.), possibly
genetic
Pathophysiology
Neoplastic proliferation of plasma cells:
•
Bone marrow infiltration by malignant plasma cells → suppression of hematopoiesis →
leukopenia, thrombocytopenia, anemia (pancytopenia)
•
Cell proliferation → osteolysis → hypercalcemia
Overproduction of monoclonal Ig and/or light chains (dysproteinemia):
•
Non-functioning AB → functional AB deficiency → ↑ susceptibility to infections
•
↑ serum viscosity → hyperviscosity syndrome
•
During elimination by the kidneys, they damage the tubules causing chronic tubulointerstitial
nephropathy w/arterial HT and chronic renal failure
Clinical manifestations
•
Often asymptomatic
•
CRAB criteria – encompasses the most common signs and indicates organ damage = Ca2+
↑; Renal failure/insufficiency; Anaemia; Bone lesions
•
B symptoms = mild fever, night sweats, weakness, weight loss
•
Bone pain, especially back pain (most common symptom)
•
Spontaneous fractures
•
↑ risk of infection; ↑ risk of petechial bleeding
•
Foamy urine (caused by Bence Jones proteinuria)
Diagnosis
•
CBC = anemia, thrombocytopenia, leukopenia, eventually pancytopenia; ↓ reticulocytes
•
Peripheral blood smear = Rouleaux formation
•
Biochemistry = ↑ total protein levels, hypercalcemia, ↑ creatinine, ↑ ESR, paraprotein gap, ↑
β2 microglobulin
•
Electrophoresis and immunofixation = serum protein electrophoresis – best initial test
(monoclonal gammopathy w/M protein (M spike)); urine protein electrophoresis (Bence Jones
protein)
•
Urinalysis = 24-hour urine collection (protein, creatinine clearance), urine dipstick –ve for
protein
•
Bone marrow biopsy (confirmatory test) = do FISH and cytology (clusters of plasma cells)
•
Imaging = 1st choice is low-dose whole body CT (WBLD-CT); alternatives include skeletal
survey (multiple lytic lesions), FDG/PET, MRI
Treatment
•
Asymptomatic patients = watch and wait, unless patients have ≥60% clonal cells, excessive
free light chains or ≥1 bone lesion
•
Symptomatic patients = if eligible (young patients) for hematopoietic stem cell transplantation
(HSCT) – induction therapy followed by autologous HSCT; if ineligible – chemo alone (e.g.
dexamethasone and lenalidomide). Chemo (melphalan)
•
Supportive therapy = bisphosphonates and radiation therapy for osteolysis and bone pain;
blood transfusions, G-CSF, and EPO for pancytopenia w/anaemia and ↑ risk of infection
Complications
•
Kidney: Myeloma cast nephropathy (myeloma kidney), Light chain deposition disease
(LCDD), hypercalciuria and nephrocalcinosis, Analgesic nephropathy (from long term NSAID
use for bone pain)
•
AL amyloidosis, Infections, Secondary plasma cell leukemia, hypercalcemic crisis
67) Chronic myelogenous/myeloid leukaemia (CML)
Definition = malignancy of the hematopoietic stem cells w/excessive uncontrolled proliferation of the
myeloid lineage (especially granulocytes) in the bone marrow and their accumulation in the blood –
they suppress the other cell lines.
Etiology
•
Idiopathic (most cases)
•
Ionizing radiation, toxicity (benzene)
•
M sex; advanced age
•
Genetic abnormality = Philadelphia chromosome
Pathophysiology
Reciprocal translocation between chromosome 9 and chromosome 22 → formation of Philadelphia
chromosome t(9;22) → fusion of the ABL1 gene (chromosome 9) and BCR gene (chromosome 22)
→ formation of BCR-ABL fusion gene → inhibits physiologic apoptosis and ↑ mitotic rate →
uncontrolled proliferation of functional granulocytes
Uncontrolled proliferation of granulocytes → infiltration of bone marrow → suppression of
hematopoiesis → 1st suppresses erythropoiesis and later thrombocytopoiesis
Clinical manifestations
Chronic phase
•
Can persist up to 10 years and is often subclinical
•
When symptomatic, features include B symptoms, splenomegaly (discomfort in LUQ);
lymphadenopathy is not typical
•
Unlike AML, CML is not characterised by recurrent infections during early stages, since the
granulocytes are still fully functional
Accelerated phase
•
Erythrocytopenia = anaemia
•
Neutropenia = infection and fever
•
Extreme pleocytosis (rapid proliferation of malignant cells) = infarctions (spleen, MI, retinal
vessel occlusion), leukaemic Priapism, myelofibrosis (terminal stage)
•
Extreme splenomegaly = palpable in LLQ or pelvic cavity
Blast crisis (terminal stage of CML)
•
Symptoms resemble those of acute leukaemia
•
Rapid progression of bone marrow failure → pancytopenia, bone pain
•
Severe malaise
•
Subtypes = myeloid blast crisis → AML (2/3); lymphoid blast crisis → ALL (1/3)
Diagnosis
CBC
•
Leukocytosis w/midstage progenitor cells (e.g. Myelocytes, metamyelocytes) and mature cells
(e.g. neutrophils, Myelocytes)
•
Basophilia and eosinophilia
•
Blasts can indicate transition to the accelerated phase
•
Thrombocytosis – in late stages, thrombocytopenia may occur due to bone marrow
suppression
•
NB! CML causes the most severe leukocytosis of all forms of leukaemia. Increasing
basophilia is a sign of acceleration
Cytochemistry = ↓ leukocyte alkaline phosphatase (LAP) versus a leukemoid rxn
Cytogenetics = confirmation of BCR-ABL (Philadelphia chromosome) fusion gene
Bone marrow = hyperplastic myelopoiesis (predominantly granulocytosis); ↑ granulocytic precursor
cells
WHO classification of CML phases according to blast count in peripheral blood and bone
marrow = chronic (<10%), accelerated (10-19%), and blast crisis (≥20%)
Treatment
•
Targeted therapy = 1st line for chronic and accelerated phase – tyrosine kinase inhibitors
(imatinib, dasatinib, nilotinib); lifelong therapy; side effects include PE, QT prolongation, N/V,
diarrhoea, pancytopenia
•
Allogeneic stem cell transplantation = if targeted therapy is not successful or in young patients
w/out major comorbidities (the only curative option)
•
Blast phase = acute leukaemia treatment chemo for AML/ ALL
•
Further treatment options for TKI resistant patients: Omacetaxine, Hydroxyurea/ IFN-a to
reduce leukocyte counts, Systemic chemo, Allogenic HSCT
68) Polycythaemia vera (PV/PCV) (AKA primary polycythaemia)
Definition = a neoplastic disease of the pluripotent cells of the bone marrow characterised by an
absolute ↑ in total RBC mass accompanied by ↑ WBC and platelet counts OR a chronic
myeloproliferative neoplasm that is characterised by an EPO-independent, irreversible ↑ in RBC,
granulocyte, and platelet counts
Pathophysiology
The JAK2 (Janus kinase 2) oncogene codes for a non-receptor tyrosine kinase in hematopoietic
progenitor cells. JAK2 is essential for the regulation of erythropoiesis, thrombopoiesis
(megakaryopoiesis), and granulopoiesis.
95% of primary PV patients have mutation in the JAK2 gene (gain or function) → ↑ tyrosine kinase
activity → EPO-independent proliferation of myeloid cell lines → ↑ blood cell mass (erythrocytosis,
thrombocytosis, and granulocytosis) → hyperviscosity + slow blood flow → ↑ risk of thrombosis and
poor oxygenation
Clinical manifestations
•
Often asymptomatic (incidental finding on routine blood tests)
•
B symptoms
•
Hyperviscosity syndrome = triad of mucosal bleeding, neurological symptoms, and visual
changes
•
Plethora = facial flushing (due to high RBC mass), cyanotic lips (↑ Hb levels associated w/PV
paradoxically result in ↓ O2 supply)
•
Pruritus = worsens when the skin comes into contact w/warm water (aquagenic pruritus)
•
Erythromelalgia = manifests w/intense, burning pain and erythema of the feet
•
Non-specific neurological symptoms = dizziness, headache, visual disturbances, tinnitus
•
Splenomegaly
•
Peptic ulcer disease
•
Symptoms of thrombotic and hemorrhagic complications
•
NB! Patients w/PV are at ↑ risk of thrombosis and bleeding
Diagnosis
•
↑ Hb/HCT, ↑ RBC, ↑ WBC, ↑ platelets; ↓ EPO
•
↑ uric acid, ↑ LDH, ↑ LAP, ↓ serum iron levels, ↓ ESR
•
SaO2 = normal
•
Diagnosis according to WHO = all 3 major criteria OR the 1st 2 major criteria + the minor
criteria
Major criteria = evidence of ↑ RBC (↑ Hb/HCT/red cell mass); bone marrow biopsy
showing hypercellularity w/trilineage growth; evidence of a genetic mutation in the
JAK2 gene
Minor criteria = ↓ EPO
Treatment
•
Phlebotomy = periodic removal of blood via venupuncture temporarily reduces counts and
hyperviscosity
•
Anti-platelet prophylaxis = aspirin
•
Cytoreductive therapy = determined on an individual basis; recommended if risk factors are
present – hydroxyurea, interferon alpha, JAK2 inhibitor
Complications = venous/arterial thrombosis, haemorrhagic complications, AML in late stages,
myelofibrosis (fibrotic transformation of the bone marrow)
69) Acute myeloid leukaemia (AML)
Definition = cancer of the myeloid line, characterised by rapid growth of abnormal cells that
accumulate in the bone marrow and blood and interfere w/hematopoiesis. Peak incidence is at 65
years; 80& of acute leukaemias during adulthood are myelogenous
Classification
The French-American-British (FAB) classification = distinguishes between 8 subtypes of AML
according to the histopathological appearance of the cells
•
M0 = acute myeloblastic leukaemia w/out maturation
•
M1 = acute myeloblastic leukaemia w/minimal granulocyte maturation
•
M2 = acute myeloblastic leukaemia w/granulocyte maturation
•
M3 = acute promyelocytic leukaemia (APL)
•
M4 = acute myelomonocytic leukaemia
•
M5 = acute monocytic leukaemia
•
M6 = acute erythroid leukaemia
•
M7 = acute megakaryoblastic leukaemia
Etiology
•
No identifiable cause or risk factors in most cases
•
Pre-existing hematopoietic disorder (most common identifiable cause) = myelodysplastic
syndromes, aplastic anaemia, myeloproliferative disorders
•
Environmental factors = alkylating chemo, ionising radiation, benzene, tobacco
•
Genetic/chromosomal factors = down syndrome (10-20X higher risk compared to general
population), Fanconi anaemia
Pathophysiology
Acquired somatic mutations (chromosomal translocations and other genetic abnormalities) in early
hematopoietic precursors → clonal proliferation of a lymphoid or myeloid stem cell line and arrest in
cell differentiation and maturation in early stages of hematopoiesis → rapid proliferation of abnormal
and dysfunctional blasts (w/impaired apoptosis pathways) → accumulation of leukaemic WBC in the
bone marrow → disrupted normal hematopoiesis → leukopenia (↑ risk of infections);
thrombocytopenia (↑ bleeding); and anaemia
Immature blasts enter the bloodstream → infiltration of other organs (particularly the CNS, testes,
liver, and skin)
Clinical manifestations
Clinical features are either related to bone marrow failure, infiltration of organs by leukaemic cells, or
a combo of both.
General features of acute leukaemia:
•
Sudden onset of symptoms and rapid progression (days to weeks)
•
Anaemia = fatigue, pallor, weakness
•
Thrombocytopenia = epistaxis, bleeding gums, petechiae, purpura
•
Immature leukocytes = frequent infections, fever
•
Hepatosplenomegaly (caused by leukaemic infiltration) (> common in ALL – 60% than AML –
10%)
Clinical features of AML
•
Leukaemia cutis (or myeloid sarcoma) = nodular skin lesions w/a purple or gray-blue colour
•
Gingival hyperplasia (AML subtype M4 and M5)
•
Signs of CNS involvement = e.g. headache, visual field changes (uncommon)
Diagnosis
CBC = leukaemic hiatus (a gap in the differentiation of WBC in which there is a high n.o of blast cells
and mature leukocytes but no intermediate forms), thrombocytopenia, anemia
Peripheral blood smear = presence of blasts = ↑ myeloblasts – some subtypes (especially M3)
exhibit Auer rods (pink-red, rod-shaped granular cytoplasmic inclusion bodies) which are
myeloperoxidase (+).
Bone marrow aspiration and biopsy (confirmatory tests) = >20% myeloblasts in the bone marrow
Morphology
Histochemistry
Cytogenetics
Immunophenotyping by flow
cytometry
•
Large blasts (2-4X the size of RBC) w/round/kidney-shaped
nuclei, > cytoplasm than in ALL
•
Prominent nucleoli
•
Fine granules
•
Auer rods (50% of cases)
•
Myeloperoxidase (+)
•
Terminal deoxynucleotidyl transferase (-)
•
PAS (-)
•
Translocation t(15:17) (particularly M3)
•
Philadelphia translocation in <2% of patients
•
Majority of subtypes are +ve for CD13, 33, 34, 117, and HLADR
Treatment
•
Aggressive chemo = induction (4-6 wks), re-induction (4-6 wks), consolidation (several
months), and maintenance therapy (up to 24 months – to maintain remission)
•
Standard regimen = cytarabine, anthracyclines; for APL – ATRA (all-trans retinoic acid) and
arsenic. Addition of BCR-ABL tyrosine kinase inhibitor for Philadelphia translocation
•
Intrathecal chemo = chemo administered directly into the subarachnoid space via spinal tap or
a device placed under the scalp (only indicated if there is confirmed CNS involvement)
•
Allogeneic stem cell transplantation = patients who don’t achieve remission through chemo;
poor prognostic factors (unfavourable cytogenetics)
•
Supportive therapy = preventing infection, managing side effects (anti-emetics, nutritional
support, transfusion for severe cytopenia), uric acid stone prophylaxis (hydration, allopurinol)
70) Acute lymphocytic leukaemia in adults (ALL)
Definition = cancer of the lymphoid line characterised by the development of large n.o’s of immature
lymphocytes (lymphoblasts). It is the most common malignant disease in children (peak incidence 2-5
years). ~80% of acute leukaemias during childhood are lymphoblastic
Classification
Current WHO classification = classifies ALL into subtypes of precursor lymphoblastic
leukaemia/lymphoma based on morphologic and genetic factors:
•
B lymphoblastic leukaemia w/recurrent genetic abnormalities
•
B lymphoblastic leukaemia, not otherwise specified
•
Precursor T lymphoblastic leukaemia/lymphoma
Immunophenotype classification = based on the origin (B/T cell) and maturity of the leukaemic
cells
•
B-cell ALL (~80-85%) = early (pro-B), common, precursor, and mature B-cell (AKA Burkitt
leukaemia) ALL
•
T-cell ALL (~15-20%) = early (pro-T), intermediate, and mature T-cell ALL
Etiology
•
No identifiable cause or risk factors in most cases
•
Prior bone marrow damage due to alkylating chemo or ionising radiation
•
Adult T-cell leukaemia/lymphoma is linked to infection w/HTLV
•
Genetic/chromosomal factors = down syndrome (10-20X higher risk compared to general
population), neurofibromatosis type 1, ataxia telangiectasia
Pathophysiology
Same as AML (see above – Q11)
Clinical manifestations
General features of acute leukaemia (same as AML – see above Q11)
Clinical features of ALL
•
B symptoms = fever, night sweats, unexplained weight loss
•
Painless lymphadenopathy
•
Bone pain = presenting as limping or refusal to bear weight in children
•
Airway obstruction (stridor, difficulty breathing) due to mediastinal or thymic infiltration
(primarily in T-cell ALL)
•
Features of SVC syndrome = feeling of fullness in the head, SOB, oedema of upper
extremities, distention of super. vv. of the chest, face, and upper extremities
•
Meningeal leukaemia (or leukaemic meningitis) = headache, neck stiffness, visual field
changes, or other CNS symptoms
•
Testicular enlargement (rare finding)
Diagnosis
CBC = thrombocytopenia, anaemia; WBC may be ↑/normal/↓
Peripheral blood smear = present of blasts = ↑ lymphoblasts
Bone marrow aspiration and biopsy (confirmatory tests) = >20% lymphoblasts in the bone
marrow
Morphology
•
Large blasts (1.5-3X the size of RBC) w/large, irregular nuclei (high
nuclear to cytoplasm ratio)
Histochemistry
•
Inconspicuous nucleoli
•
Coarse granules
•
No Auer rods
•
Myeloperoxidase (-)
•
Terminal deoxynucleotidyl transferase (+)
Cytogenetics
•
PAS (+)
•
Philadelphia translocation = ~20-30% in adults and only 2-3% in
children
•
Translocation t(12:21) = most common specific abnormality in childhood
B-ALL
Immunophenotyping by flow
cytometry
•
Hyperdiploidy is common in pre-B-ALL
•
B-ALL is usually +ve for = CD10 (marker for pre-B), CD19, and CD20
•
T-ALL is usually +ve for = CD2-CD8, especially CD3
Treatment
•
Aggressive chemo – standard regimen = vincristine, glucocorticoids, cyclophosphamide,
doxorubicin, L-asparaginase. Addition of BCR-ABL tyrosine kinase inhibitor for Philadelphia
translocation
•
Intrathecal chemo = indicated for all children to prevent meningeal leukaemia
•
See AML (see above – Q11) for additional measures
71) Haemorrhagic diathesis – features and classification.
Thrombocytopenia – classification. Autoimmune thrombocytopenia
Haemorrhagic diathesis
Definition = unusual susceptibility to bleed (haemorrhage) mostly due to hypocoagulability (a
condition of irregular and slow blood clotting), in turn caused by a coagulopathy. Therefore, this may
result in the ↓ of platelets being produced and leads to excessive bleeding.
Etiology
•
Acquired = anticoagulation w/warfarin, liver failure, vitamin K deficiency, disseminated
intravascular coagulation (DIC), hemotoxic venom from some snakes, viral hemorrhagic fever,
leukaemia
•
Autoimmune causes of acquired coagulation disorders
•
Impaired wound healing (scurvy); thinning of the skin (Cushing’s syndrome)
•
Genetic = lack of genes that produce the protein coagulation factors
Clinical manifestations = petechiae, purpura, ecchymoses, blood in stool, bleeding gums, prolonged
epistaxis
Complications = soft tissue bleeding, joint damage, retinal bleeding, transfusion transmitted infection,
adverse reactions to clotting factor treatment, anaemia, exsanguinations (bleeding to death), cerebral
hemorrhage
Diagnosis
•
History of presenting illness; past medical history (specifically ask about conditions that can
affect hemostasis – cirrhosis, CKD, cancer, autoimmune conditions); family history; meds
(anticoagulants, antiplatelets); nutrition (vitamin C/K deficiency)
•
CBC = can detect thrombocytopenia
•
Peripheral blood smear = may show irregular-shaped platelets in thrombocytopenia
•
Coagulation studies = PT, INR, aPTT
•
Bleeding time; liver and renal function tests
Thrombocytopenia
Definition = abnormally low levels of platelets (thrombocytes) OR platelet count below the normal
range (< 150,000/mm3)
Etiology
Impaired platelet production in bone marrow
Bone marrow conditions → ↓ megakaryocytes → ↓ thrombopoiesis
•
Bone marrow failure = aplastic anaemia, PNH
•
Bone marrow suppression = drugs, chemo, radiation
•
Congenital thrombocytopenia = Wiskott-Aldrich syndrome, Alport syndrome, Bernard-Soulier
syndrome, Fanconi anaemia, von Willebrand disease
•
Infection = CMV, EBV, HCV, HIV, parvovirus B19, VSV
•
Malignancy = leukaemia, lymphoma, bone marrow infiltration
•
Nutritional deficiency = vitamin B12 and/or folate deficiency
↑ Platelet turnover in periphery
•
Immune thrombocytopenia (ITP) and other autoimmune diseases
•
DIC and sepsis
•
Thrombotic thrombocytopenic purpura (TTP) and hemolytic uremic syndrome
•
Drug-induced immune thrombocytopenia
•
Pregnancy = pre-eclampsia; HELLP syndrome
•
Infection
•
Post-transfusion thrombocytopenia
•
Mechanical damage due to artificial heart valves or extracorporeal circulation (dialysis)
Redistribution, dilution, and other causes
•
Liver disease and chronic alcohol abuse (↓ production of EPO in liver)
•
Splenomegaly (sequestration of thrombocytes in an enlarged spleen)
•
Thrombocytopenia following transfusion or fluid resuscitation
Clinical manifestations
Platelet count
Mild
> 70-000 –
Moderate
20,000 – 70,000/mm3
Severe
<
149,999/mm3
20,000/mm3
Symptoms
Typically = no abnormal bleeding, i.e. asymptomatic
thrombocytopenia
•
Prolonged bleeding following surgery/trauma
•
Easy bruising
•
Occasionally = petechiae and purpura
•
Spontaneous bruising (ecchymoses), petechiae, and
purpura
•
Bleeding from the mucosa or after minimal trauma
•
↑ Risk of spontaneous, life-threatening bleeding
Diagnosis
•
CBC = ↓ platelet count (< 150,000/mm3); depending on etiology, anemia or pancytopenia may
be present
•
Coagulation studies = ↑ bleeding time
•
Peripheral blood smear = abnormal platelet morphologies and cells; platelet clumping may be
seen in pseudothrombocytopenia
•
Liver and renal function tests
•
Additional tests to check for the suspected etiology
Treatment
•
For all patients = treat any significant bleeding, treat underlying cause, consider empiric
treatment for immune thrombocytopenic purpura (ITP)
•
Asymptomatic or mildly symptomatic w/platelet count < 50,000/mm3 = consult haematology
•
Asymptomatic patients w/platelet count > 50,000/mm3 = repeat CBC in 1-4 weeks or if the
patient becomes symptomatic – if platelet count ↓, consult haematology; if platelet count ↑,
follow-up until platelet count has normalised
•
Emergency management includes haemostatic control to stop bleeding, platelet transfusion,
and IV Ig if there is an immune cause
Autoimmune thrombocytopenia (AKA immune/idiopathic thrombocytopenic purpura – ITP)
Definition
•
Thrombocytopenic purpura = purpura associated w/a ↓ in circulating platelets
•
ITP = isolated low platelet count (thrombocytopenia) w/normal bone marrow and the absence
of other causes of thrombocytopenia. It is an autoimmune disease w/AB detectable against
several platelet surface structures
Etiology
•
Primary ITP = idiopathic; may also be triggered by a previous viral/bacterial infection
•
Secondary ITP = associated w/lymphoma, leukaemia (particularly CLL), SLE, HIV, HCV, drug
rxns
Pathophysiology
IgG AB against GpIIb/IIIa on platelets → platelet-AB complex removed from circulation by spleen → ↓
platelet count → bone marrow megakaryocytes and platelet production ↑ in response
Clinical manifestations = commonly asymptomatic; symptoms depend on platelet counts. They
include:
•
Spontaneous formation of bruises (purpura), and petechiae (tiny bruises); bleeding;
hematuria; melena
•
A very low count may result in spontaneous formation of hematomas in the mouth or on other
mucous membranes
•
Acute ITP (typically in children) = following a viral infection
•
Chronic ITP (typically women of childbearing age) = insidious onset or an incidental finding
Diagnosis
•
CBC = ↓ platelet count; otherwise normal
•
Bleeding time = ↑
•
Peripheral blood smear = platelets are normal to large in size
•
HIV and HCV testing
•
Consider bone marrow biopsy in atypical cases = ↑ n.o of platelet-synthesising
megakaryocytes
Treatment
•
For children = no bleeding → observation; severe bleeding/↑ risk of bleeding →
glucocorticoids and/or IV Ig
•
For adults = 1st line is corticosteroids (alternatively IV Ig); 2nd line is splenectomy
72) Haemorrhagic diathesis – classification. Haemophilia
Haemophilias
Definition = disorders of blood clotting and consequently may lead to serious bleeding
Etiology
•
Caused by an X-linked recessive defect (inherited or spontaneous mutation) or AB production
against clotting factors
Haemophilia usually affects M, as it is primarily an XR disorder
•
Haemophilia A (80%) = factor VIII deficiency
•
Haemophilia B (20%) = factor IX deficiency
•
Haemophilia C (very rare) = factor XI deficiency – ↑ frequency in Ashkenazi Jews, caused by
an AR defect
Pathophysiology = deficiency of one of these factors impairs the formation of the fibrin clot, especially
the activation of thromboplastin
Clinical manifestations
•
Spontaneous or delayed onset bleeding (joints, muscular and soft tissue, mucosa) in
response to different degrees of trauma
Repeated haemarthrosis → joint destruction
Recurrent bruising or hematoma formation
Oral mucosa bleeding, epistaxis, excessive bleeding following small procedures
•
Further sites/symptoms of haemorrhage = CNS (headache, neck stiffness), GI (melena,
haematemesis), genitourinary (hematuria)
•
Female carrier may show mild symptoms
•
NB! Petechial bleeding is a common sign of platelet disorders, NOT coagulation disorders
such as haemophilia
Severity
Clinical signs
Factor VIII/IX activity
Physiologic condition
None
≥ 50%
Mild haemophilia
Hematomas following severe trauma
> 5% to < 50%
Moderate haemophilia
Hematomas following mild trauma
≥ 1% to 5%
Severe haemophilia
Spontaneous hematomas
< 1%
Diagnosis
•
Patient and family history
•
Genetic testing
•
Screening = normal PT and platelet count; ↑ aPTT
•
If aPTT is prolonged → mixing study. If mixing study is +ve → quantitative assessment of
factor activity levels
Treatment
•
Substitution of clotting factors = when needed (trauma/surgery) for mild-moderate
haemophilia; prophylactic for severe haemophilia
•
Desmopressin can be used in mild haemophilia A – synthetic analog of vasopressin, which
triggers release of factor VIII from endothelial cells
•
Anti-fibrinolytic therapy = used in addition to factor substitution; inhibits the breakdown of clots
to ↓ the risk of bleeding
V.Endocrine and metabolic diseases
73) Diabetes mellitus – pathogenesis, clinical features
Definition and Classification
Diabetes mellitus (DM) describes a group of diseases characterised by chronic hyperglycaemia
•
Type 1 DM (“insulin-dependent DM”, IDDM, or “juvenile diabetes”) = results from the
body’s failure to produce enough insulin due to an autoimmune response that triggers the
destruction of insulin-producing β-cells
•
Type 2 DM (“non-insulin-dependent DM”, NIDDM, or “adult onset diabetes”) = begins
w/insulin resistance, a condition in which cells fail to respond to insulin properly. As the
disease progresses a lack of insulin may also develop. The primary cause is excessive body
weight and not enough exercise
•
Gestational diabetes = occurs when pregnant women w/out a previous history of diabetes
develops a high blood glucose level
•
Maturity onset diabetes of the young (MODY) = different forms of AD inherited DM that
manifest before the age of 25 years and are not associated w/obesity or Autoantibodies.
Etiology
DM 1
•
Autoimmune β cell destruction in genetically susceptible individuals – patients who are HLADR3 and HLA-DR4 +ve are 4-6x more likely to develop DM1
•
Association w/other autoimmune conditions = hashimoto thyroiditis, type A gastritis, celiac
disease, primary adrenal insufficiency
DM 2
•
Hereditary and environmental factors
•
Association w/metabolic syndrome
•
Risk factors = obesity, high calorie diet, high waist-to-hip ratio (visceral fat accumulation),
physical inactivity, 1st degree relative w/DM2, ethnicity, HT, dyslipidemia
Pathophysiology
DM 1
Genetic susceptibility + environmental trigger (e.g. previous viral infection) → autoimmune response
w/production of auto-AB (e.g. anti-GAD) that target insulin-producing cells → progressive destruction
of insulin-producing β cells in the IOL by autoreactive T cells → destruction of 80-90% of β cells →
absolute insulin deficiency → ↑ blood glucose levels
DM 2
Peripheral insulin resistance:
•
Numerous genetic and environmental factors
Central obesity → ↑ plasma levels of free FAs → impaired insulin-dependent glucose
uptake into hepatocytes, myocytes, and adipocytes
↑ serine kinase activity in liver, fat, and skeletal muscle cells → phosphorylation of
insulin receptor substrate (IRS)-1 → ↓ affinity of IRS-1 for PI3K → ↓ expression of
GLUT4 channels → ↓ cellular glucose uptake
Pancreatic β cell dysfunction:
•
Accumulation of pro-amylin (islet amyloid polypeptide) in the pancreas; → ↓ endogenous
insulin production
•
Initially, insulin resistance is compensated by ↑ insulin and amylin secretion
•
Over the course of the disease, insulin resistance progresses, while insulin secretion capacity
declines
•
After a period of impaired glucose tolerance w/isolated postprandial hyperglycemia, DM
manifests w/fasting hyperglycemia
Clinical manifestations
DM 1
•
Onset
DM 2
Sudden; diabetic ketoacidosis
•
is often the 1st manifestation
•
Alternatively, children may
present w/acute illness and
classic symptoms
Gradual, majority of patients are
asymptomatic
•
Hyperosmolar hyperglycaemic state
(esp. in elderly)
•
Symptoms of complications may be the
1st clinical sign of the disease
Characteristic
features
•
Classic = polyuria, polydipsia, polyphagia
•
Non-specific = fatigue, visual disturbances (blurred vision), calf cramps, poor
wound healing, pruritus
Weight loss; a thin appearance is typical for DM1
Benign acanthosis nigricans
Diagnosis – values in mg/dL (mmol/L)
DM
Pre-diabetes
Healthy
Fasting plasma glucose
≥ 126 (≥ 7)
100-125 (5.6-6.9) = impaired
fasting glucose
< 100 (< 5.6)
2-hour glucose value
after OGTT
≥ 200 (≥ 11.1)
140-199 (7.8-11) = impaired
glucose tolerance
< 140 (< 7.8)
Glycated Hb (HbA1C)
≥ 6.5%
5.7-6.4%
< 5.7%
•
C-peptide = ↓ C-peptide indicate absolute insulin deficiency (DM1); ↑ levels may indicate
insulin resistance and hyperinsulinemia (DM2)
•
Urine analysis = microalbuminuria (early sign of diabetic nephropathy), glucosuria, ketone
bodies (usually accompanied by glucosuria – +ve in acute metabolic decompensation in DM)
74) Diabetes mellitus – treatment w/insulin and oral medications
Rational therapy for DM2 – treatment algorithm
•
HbA1C target for adults = <7% (53 mmol/mol) – individual assessment, depending on
patient’s age, duration of diabetes, presence of comorbidities, and/or complications, and life
expectancy
•
The guidelines for the treatment of DM recommend an individualised treatment strategy
•
If the target A1C is not reached w/in 3 months w/conservative treatment, the next step in the
therapeutic algorithm should be initiated
General measures
•
Weight reduction = patients w/BMI 27-35 benefit from a weight ↓ of 5%; in patients w/BMI >35,
weight ↓ of >10% is recommended
•
Physical exercise = all adults > 19 years should aim to be active daily. Over a week, this
should add up to at least 150 mins (2.5 hours) of moderate intensity physical activity (or can
do 75 mins of HIT spread across the week)
•
Blood pressure control of <140/90 mmHg
•
Improved blood lipid profile w/statin therapy
•
Low dose aspirin for M >50 and F >60 w/cardiovascular risk factors
•
Diet control = diet should consist of ~55% carbs (mainly complex carbs), 30% fat, and 15%
protein; have a high fiber diet – slows the absorption of carbs, stabilising blood glucose levels;
alcohol should (if possible) be consumed w/carbs to avoid hypoglycaemia
1st line therapy (monotherapy)
•
Metformin (standard-release) is the initial drug treatment for patients w/DM2.
•
Gradually ↑ the dose of standard-release metformin over several weeks to minimise the risk of
GI side effects (N/V, diarrhoea, pain, loss of appetite). If patient experiences GI side effects,
consider a trial of modified-release metformin.
500 mg w/breakfast for at least 1 week, then 500 mg w/breakfast and dinner for at
least 1 week, then 500 mg w/breakfast, lunch, and dinner thereafter; the usual max.
dose is 2 g daily (in divided doses)
For modified-release metformin = 500 mg 1X/day, ↑ every 10-15 days on the basis of
blood glucose measurements; max recommended dose is 2 g 1X/day w/dinner
Dose reduction of metformin may need to be adjusted based on renal function or
during concurrent treatment w/certain drugs
•
Metformin acts by ↓ gluconeogenesis and ↑ peripheral utilisation of glucose
•
Metformin is contraindicated in patients at risk of lactic acidosis (diabetic ketoacidosis, eGFR
<30 ml/min/1.73 m2, diseases which may cause tissue hypoxia, hepatic insufficiency); people
about to undergo elective surgery; prescribe w/caution to people w/mild-moderate CKD
•
If metformin is contraindicated, consider treatment w/a DPP-4 inhibitor OR pioglitazone OR a
sulfonylurea
•
Exercise particular caution w/pioglitazone as it is associated w/an ↑ risk of HF, bladder
cancer, and bone fracture.
2nd line therapy (dual therapy, 1st intensification of drug treatment)
If initial drug treatment w/metformin has not continued to control HbA1C to below the person’s
individually agreed threshold for intensification, consider dual therapy with:
Metformin + dipeptidyl peptidase-4 (DPP-4) inhibitor (alogliptin, sitagliptin, linagliptin)
•
DPP-4 rapidly degrades the glucose-dependent insulinotropic polypeptide (GIP) and
glucagon-like peptide 1 (GLP-1) which stimulate postprandial insulin secretion and suppress
glucagon secretion
•
Inhibitor of DPP-4 therefore results in ↑ circulating levels of GIP and GLP-1 following ingestion
of food, and to ↑ insulin and ↓ glucagon secretion
•
Side effects = GI effects, hypoglycaemia, headaches, dizziness, itching, rash, angioedema
Metformin + sodium-glucose cotransporter 2 (SGLT-2) inhibitors (canagliflozin, dapagliflozin)
•
SGLT-2 inhibitors reversibly inhibit SGLT-2 in the renal PCT to ↓ glucose reabsorption and ↑
urinary glucose excretion
•
Side effects = hypoglycaemia, itching, ↑ serum lipids, polyuria
Metformin + glucagon-like peptide 1 (GLP-1) agonist (exenatide, liraglutide)
•
GLP-1 mimetics bind to, and activate, the GLP-1 receptor to ↑ insulin secretion, suppress
glucagon secretion, and slow gastric emptying
•
GLP-1 agonists are self-administered by SC injection in the thigh, abdomen, or upper arm
•
Side effects = GI effects, hypoglycaemia, dehydration, skin reactions at injection site
Metformin + sulfonylurea (glibenclamide, gliclazide, glimepiride, glipizide, tolbutamide)
•
Sulfonylureas are insulin secretagogues. They act mainly by augmenting insulin secretion
•
Max doses =
Glibenclamide = 5 mg/day w/breakfast (15 mg max)
Gliclazide = 40-80 mg/day for standard release, adjusted according to response, and
max 160 mg. For modified release = 30 mg daily w/breakfast w/max dose 120 mg
Glimepiride = 1 mg daily before/w/1st main meal (4 mg max)
Glipizide = 2.5-5 mg daily (20 mg max)
Tolbutamide = 0.5-1.5 g daily in divided or single dose (2 g max)
•
Side effects = GI disturbances, HS rxns, weight gain, hypoglycaemia
•
Metformin + sulfonylurea may be associated w/↑ risk of cardiovascular mortality
If metformin is contraindicated, consider dual therapy with:
•
DPP-4 inhibitor + pioglitazone
•
DPP-4 inhibitor + sulfonylurea
•
Pioglitazone + sulfonylurea
Triple therapy OR second intensification of drug treatment
If dual therapy has not worked, consider either:
•
Triple therapy w/metformin + DPP-4 inhibitor + sulfonylurea or metformin + pioglitazone +
sulfonylurea
•
Starting insulin-based treatment
In adults w/DM2, only offer a GLP-1 agonist in combo w/insulin w/specialist care advice and ongoing
support from a consultant-led multidisciplinary team.
Insulin therapy
•
There are different types of regimens for people w/DM2 = 1, 2, or 3 insulin injections per day
regimen (injections of short-acting insulin or rapid-acting insulin analogue mixed
w/intermediate-acting insulin); OR multiple daily injection basal-bolus insulin regimen
(injections of short-acting insulin or rapid-acting analogue before meals, together w/≥1
separate daily injections of intermediate-acting insulin or long-acting analogue to cover the
basal requirement)
•
When starting insulin therapy (provided there are no contraindications or ARs), metformin
should continually be offered, and the need for other anti-diabetic drugs should be continually
reviewed
•
NICE recommends that neutral protamine hagedorn (NPH) insulin (1/2X/day according to
need) should be offered
•
NPH + a short-acting insulin (insulin lispro, insulin aspart) should be considered, particularly if
the HbA1C is ≥9%
•
Long-acting insulin (insulin detemir, insulin glargine) should be considered as an alternative to
NPH insulin if the patient needs assistant to inject insulin, if their lifestyle is restricted by
recurrent symptomatic hypoglycaemic episodes, or if they would otherwise need 2X/daily NPH
insulin injections in combo w/other anti-diabetic drugs
•
Pre-mixed insulin preparations that include short-acting insulin analogues should be
considered if the person prefers injecting immediately before a meal, hypoglycaemia is a
problem, or if blood glucose levels rise markedly after meals
•
Currently insulin + diet control is the only acceptable management for pre-gestational and
gestational diabetes as other drugs are contraindicated.
75) Treatment of diabetic complications
Diabetic nephropathy
Pathophysiology
•
Major cause of end stage renal disease (ESRD); seen in patients w/DM for >10 years
•
Chronic hyperglycemia → glycation of the BM → ↑ permeability and thickening of the BM and
stiffening of the efferent arteriole → hyperfiltration (↑ in GFR) → ↑ in intraglomerular pressure
→ progressive glomerular hypertrophy, ↑ in renal size, and glomerular scarring
(glomerulosclerosis) → worsening of filtration capacity
Clinical manifestations
•
Often asymptomatic; patients may complain of foamy urine
•
Progressive diabetic kidney disease w/signs of renal failure and risk of uremia
•
Arterial HT
Urine analysis = proteinuria – initially moderately ↑ albuminuria (microalbuminuria); eventually
significantly ↑ albuminuria (macroproteinuria) –
nephrotic syndrome may develop
Treatment and prevention
•
Strict glycemic control
•
Anti-HT treatment = 1st line ACEIs/ARBs;
2nd line agents to be added to 1st line –
diuretics, CCBs. Early anti-HT treatment
delays progressive of nephropathy
•
Dietary modification = daily salt intake < 56 g/day; phosphorus and K+ intake
restriction in advanced nephropathy;
protein restriction (proteinuria may be
improved as the GFR ↓ due to ↓ protein
availability, subsequently ↓ renal perfusion
and hyperfiltration)
Diabetic retinopathy
Ophthalmological findings and classification
•
Non-proliferative (mild, moderate, severe)
= accounts for most cases of retinopathy
Findings = intraretinal microvascular abnormalities (IRMA), including microaneurysms;
calibre changes in venous vessels; intraretinal haemorrhage; hard exudates; retinal
oedema, and cotton-wool spots
Visual loss, most commonly due to macular oedema
•
Proliferative retinopathy
Findings = pre-retinal neovascularisation (hallmark); fibrovascular proliferation;
vitreous haemorrhage; traction retinal detachment; rubeosis iridis → secondary
glaucoma
Visual loss may be due to vitreous haemorrhage, retinal detachment, or neovascular
glaucoma
•
Macular oedema = clinically significant retinal thickening and oedema involving the macula,
hard exudates, and macular ischaemia. May occur in all stages of non-proliferative and
proliferative diabetic retinopathy
Clinical manifestations = asymptomatic until very late stages; visual impairment; progression to
blindness
Treatment
•
Non-proliferative = laser treatment (focal photocoagulation); intravitreal anti-VEGF injection
•
Proliferative = laser treatment (panretinal photocoagulation over the course of numerous
appointments); vitrectomy in case of traction retinal detachment and vitreal haemorrhage
•
Macular oedema = VEGF inhibitors; focal photocoagulation
Diabetic neuropathy
Distal symmetric polyneuropathy
•
Pathophysiology = chronic hyperglycaemia causes glycation of axon proteins w/subsequent
development of progressive sensorimotor neuropathy; typically affects multiple peripheral nn.
•
Clinical manifestations
Early = progressive symmetric loss of sensation in the distal lower extremities –
“stocking-glove” sensory loss pattern w/prox. progression is common; dysesthesia
(burning feet) may occur; similar pattern may occur in the upper extremities
Late = pain at rest and at night, but also ↓ pain perception, motor weakness, and
areflexia
•
Screening = tuning fork (↓ vibration sense); monofilament test (↓ pressure sense); pinprick
(pain) or temperature assessment (↓ sensation)
•
Treatment = strict glycemic control; pain management – anticonvulsants (pregabalin;
gabapentin, sodium valproate); antidepressants (Tricyclic – amitriptyline; SNRI – duloxetine);
opioids – should be used w/caution due to tolerance and drug dependence (tramadol,
oxycodone, morphine sulphate, dextromethorphan)
Autonomic neuropathy
Urogenital = erectile dysfunction; bladder dysfunction – urinary retention, incomplete emptying,
bladder distention, overflow incontinence, poor urinary stream
CVS = silent MI; orthostatic hypotension; persistent sinus tachycardia; ventricular arrhythmia
GI = gastroparesis (→ delayed gastric emptying, risk of postprandial hyperglycaemia) – nausea,
abdominal bloating, loss of appetite, early satiety; diarrhoea, constipation, incontinence; treatment
involves prokinetic agents (metoclopramide 1st line; erythromycin, cisapride)
Other = sweat gland dysfunction associated w/heat intolerance; pupillary dysfunction; risk of
hypoglycaemia due to absence of hormonal counterregulation (secretion of cortisol, glucagon, and
catecholamines)
Diabetic foot
•
2 types = neuropathic (most common) and ischaemic diabetic foot
•
NDF = warm, dry skin, foot pulses are palpable; IDF = cool, pale foot w/no palpable pulses
•
Diagnostics = neurological examination (evaluation of peripheral neuropathy); foot ulcer risk
assessment
•
Complications of NDF = malum perforans (painless neuropathic ulcers); diabetic neuropathic
arthropathy/Charcot foot (deformation of joints and bones)
•
Prevention of IDF = glycemic control, regular foot examinations, self-monitoring and proper
foot care
•
Treatment of foot ulcers = surgical debridement; regular wound dressing mechanical
offloading (fitting of therapeutic footwear or total contact cast); anti-B if foot ulcers become
infected; interventional/surgical revascularisation (patients w/underlying peripheral a.
disease); amputation if all else fails or severe life-threatening complications arise
76) Obesity and metabolic syndrome
Definition
•
Obesity = excess body fat accumulation w/multiple organ-specific pathologic consequences.
Clinically, it is defined as BMI ≥ 30 [BMI = weight (kg)/height2 (m)]
•
Metabolic syndrome = a clustering of at least 3 of the 5 following medical conditions: central
obesity, HT, hyperglycaemia, hypertriglyceridaemia, and low serum HDL.
Classification of obesity
2 types of obesity based on distribution of fat have been described:
•
Upper body obesity – AKA central, abdominal, visceral, or M (android) obesity
Individuals are often referred to as being “apple” shaped
Absolute waist circumference = >40 in (M) or >35 in (F)
Waist-hip ratio = >0.9 (M) or >0.85 (F)
•
Lower body obesity – AKA peripheral, gluteal-femoral, or F (gynoid) obesity
Individuals are often referred to as being “pear” shaped
Etiology
•
Combo of excessive food intake and a lack of physical activity is thought to explain most
cases of obesity
•
A limited n.o of cases are due mainly to genetics, medical reasons, or psychiatric illnesses
•
Environmental factors causing obesity = ↑ consumption of sugary, fatty foods; ↑ portion sizes;
lack of exercise (sedentary lifestyle); insufficient sleep; stress; ethnicity (Asian population);
geriatric pregnancy; genetics (family history)
•
Associated conditions that ↑ obesity risk include = hypothyroidism, Cushing’s disease, growth
hormone deficiency, and some eating disorders (binge eating disorder)
•
Certain meds that may cause weight gain = insulin, sulfonylureas, atypical antipsychotics,
antidepressants, steroids, certain anticonvulsants (phenytoin, valproate), and some forms of
hormonal contraception
Pathophysiology
•
Leptin is a hormone produced by adipose tissue that acts on leptin receptors on peripheral
tissue and brain (hypothalamus)
•
Leptin levels rise after food intake, stimulating sensation of satiety, and fall during fasting,
stimulating the sensation of appetite
•
A deficiency in leptin signalling, either via leptin deficiency or leptin resistance, leads to
overfeeding and may account for some genetic and acquired forms of obesity
Clinical manifestations
Obesity ↑ the risk of many physical and mental conditions. These comorbidities are most commonly
shown in metabolic syndrome, a combo of medical disorders which includes DM 2, HT,
hypercholesterolemia, and hypertriglyceridemia.
Medical field
Conditions
Medical field
Conditions
Cardiology
CAD (angina and MI); CHF;
HT; dyslipidemia; DVT and
PE
Dermatology
Stretch marks; acanthosis nigricans;
lymphedema; hirsutism
Endocrinology
DM; PCOS; menstrual
Gastroenterology
GERD; fatty liver disease;
disorders; infertility;
complications during
pregnancy; birth defects
gallstones
Neurology
Stroke; migraines; carpal
tunnel syndrome; dementia;
MS
Oncology
Oesophageal; colorectal;
pancreatic; gallbladder; endometrial;
kidney; leukaemia; hepatocellular
carcinoma
Psychiatry
Depression in F; social
stigmatisation
Pulmonology
COPD; asthma; sleep apnoea
Rheumatology
and
orthopaedics
Gout; poor mobility;
osteoarthritis; low back pain
Urology and
nephrology
Erectile dysfunction; urinary
incontinence; chronic renal failure;
hypogonadism
Diagnosis
To diagnose metabolic syndrome, a person must have at least 3 of the following:
•
Abdominal obesity = waist circumference >35” in F and >40” in M
•
Hypertriglyceridaemia = > 1.7 mmol/L (150 mg/dl)
•
↓ HDL = < 1.3 mmol/L (50 mg/dl) in F and < 1 mmol/L (40 mg/dl) in M
•
HT = ≥ 130/85 mmHg
•
Raised fasting plasma glucose = ≥ 5.6 mmol/L (100 mg/dl)
Treatment
•
Lifestyle modifications = dietary changes (calorie restricted diet, diet low in saturated fat and
cholesterol), physical activity
•
Medical therapy = orlistat (synthetic derivative of a naturally occurring lipase inhibitor,
lipostatin; GI side effects – steatorrhoea, fecal incontinence, and frequent/urgent bowel
movements); treat complications (HT, DM, dyslipidemia)
•
Bariatric surgery (BMI ≥40 or between 35-40 w/other significant diseases (DM, HT) that could
be improved if they lost weight) = most commonly a sleeve gastrectomy – large part of the
greater curvature is removed, so that the remaining stomach resembles a sleeve; Roux-en-Y
gastric bypass is the 2nd most common
77) Dyslipidemia
Definition = abnormal conc. of lipids in the blood (e.g. hyperlipidemia, hypertriglyceridemia,
hypercholesterolemia)
Etiology
•
Acquired (> common) = obesity, DM, physical inactivity, excess alcohol consumption,
hypothyroidism, nephrotic syndrome, cholestatic liver disease, Cushing disease, certain drugs
(anti-psychotics, BB, oral contraceptives)
•
Inherited (< common)
Classification (Frederickson classification of inherited hyperlipoproteinemias)
Hyperlipoproteinemia
Type I
Name
Defect
↑ Lipoprotein
Symptoms
Familial
hyperchylomicronemia
Deficiency of
lipoprotein lipase
(LPL) or Apo C-II
Chylomicrons
Acute pancreatitis, eruptive
xanthomas,
hepatosplenomegaly, lipemia
retinalis
A
Familial
hypercholesterolemia
LDL receptor
deficiency
LDL
B
Familial combined
hyperlipidemia
↓ LDL receptor
and ↑ ApoB
LDL and VLDL
Premature atherosclerosis,
tuberous/tendon xanthomas,
xanthelasma, arcus lipoides
corneae
Type III
Familial
dysbetalipoproteinemia
Defective Apo E
synthesis
IDL
Premature atherosclerosis,
palmar and tuberoeruptive
xanthomas
Type IV
Familial
hypertriglyceridemia
↑ VLDL
production and ↓
elimination
VLDL
Premature atherosclerosis,
tuberoeruptive xanthomas,
acute pancreatitis (if
triglycerides >900 mg/dl)
Type V
Familial
↑ VLDL
production and ↓
LPL
VLDL and
chylomicrons
Eruptive xanthomas, features
of hyperglycemia, abdominal
pain
Type II
Pathophysiology = ↑ LDL and ↓ HDL → promote atherosclerosis → ↑ risk of cardiovascular events
Clinical manifestations
Typically there are no specific signs/symptoms.
Skin manifestations
•
Xanthomas = nodular lipid deposits in the skin and tendons. Extremely high levels of
triglycerides and/or LDL results in extravasation of plasma lipoproteins and their deposition in
tissue. Different types = eruptive, tuberous, tendinous, palmar, and plane.
•
Xanthelasmas = typically bilateral, yellow, flat plaques on the upper eyelids (nasal sides).
They are idiopathic and are associated w/hypercholesterolemia, ↑ LDL levels
Eye manifestations
•
Lipemia retinalis = opaque, white appearance of the retinal vessels, visible on funduscopic
exam. It is associated w/hyperlipoproteinemia type I, III, and IV
•
Arcus lipoides corneae = a yellow/grey discolouration of the corneal margins caused by
deposits of fat and cholesterol or by hyalinosis of corneal stroma. It is not pathological in
advanced age
GI manifestations
•
Fatty liver (hepatic steatosis) = associated w/abetalipoproteinemia, metabolic syndrome,
excess alcohol
•
Pancreatitis in severe hypertriglyceridemia; associated w/hyperlipoproteinemia type I and IV,
hypertriglyceridemia
Premature atherosclerosis = associated w/hyperlipoproteinemia type II – IV; manifests w/secondary
diseases such as CHD, MI, stroke, peripheral a. disease, carotid a. stenosis
Diagnosis
Lab analysis
•
Fasting lipid profile (to avoid postprandial fluctuations; fast for 9-12 hours prior to the test) =
total cholesterol, HDL, and triglycerides are measured
•
LDL can be measured directly using assays or estimated using the Friedewald formula – LDL
= total cholesterol – HDL – (triglycerides/5)
•
Pathological values on 2 different occasions are required to confirm the diagnosis
•
Dyslipidemia is diagnosed if LDL >130 mg/dl and/or if HDL levels <40 mg/dl
•
Identify the underlying cause = fasting blood glucose/HbA1C, TSH level, LFTs, urine analysis
Optimal levels
•
Total cholesterol = < 5.17 mmol/L (200 mg/dl)
•
Triglycerides = < 3.9 mmol/L (150 mg/dl)
•
LDL = < 2.6 mmol/L (100 mg/dl)
•
HDL = ≥ 1.55 mmol/L (60 mg/dl)
•
LDL:HDL ratio = < 3.5 (M) and < 3 (F)
Treatment
•
Lifestyle modifications = dietary changes (↓ saturated fat, cholesterol, alcohol), maintaining a
healthy weight, physical activity
•
Meds = statins (inhibit cholesterol synthesis); 2nd line lipid-lowering agents (fibrates, bile acid
resins, niacin, cholesterol absorption inhibitors) if there is a poor response to statins
78) Hypothyroidism
Definition = ↓ synthesis and secretion of thyroid hormones (thyroid gland is underactive) causing
cretinism in children (mentally retarded dwarfs) and in adults ↓ metabolism, accelerated
atherosclerosis and myxedematous infiltration (accumulation of glycosaminoglycans in the tissues)
Etiology and classification
•
Congenital hypothyroidism = sporadic (85% – thyroid hypo-/dysplasia, thyroid
aplasia/athyroidism, iodine deficiency) or hereditary (15% – defects in thyroid hormone
synthesis, peripheral resistance to thyroid hormones)
•
Primary hypothyroidism = insufficient thyroid hormone production – caused by diseases
directly affecting the thyroid gland, most common cause is Hashimoto thyroiditis. Other
causes include postpartum/De Quervain thyroiditis, iatrogenic, nutritional etc.
•
Secondary = lack of thyroid hormone secretion due to inadequate stimulation by TSH from the
pituitary gland (pituitary disorders → TSH deficiency)
•
Tertiary = inadequate release of TRH (thyrotropin releasing hormone) from the hypothalamus
(hypothalamic disorders → TRH deficiency)
•
Other common causes are panhypopituitarism (Simonds-Sheehan syndrome); pituitary
adenoma; ↓ intake of iodine; partial/total resection of the gland; drugs such as amiodarone,
thalidomide, interferon alpha, and lithium
Pathophysiology
•
Primary hypothyroidism = peripheral (thyroid) disorders → T3/T4 are not produced (↓ levels)
→ compensatory ↑ TSH
•
Secondary hypothyroidism = pituitary disorders → ↓ TSH levels → ↓ T3/T4
•
Tertiary hypothyroidism = hypothalamic disorders → ↓ TRH → ↓ TSH → ↓ T3/T4
Effects of hypothyroidism
Generalised ↓ in basal metabolic rate → ↓ O2 and substrate consumption, leading to:
•
CNS = apathy, slowed cognition
•
Skin and appendages = skin dryness, alopecia
•
Lipid profile = ↑ LDL, ↑ triglycerides
•
Cold intolerance
↓ Sympathetic activity = ↓ sweating, cold skin (due to ↓ blood flow), constipation (due to ↓ GI
motility), bradycardia
Hyperprolactinemia = ↑ prolactin production is stimulated by TRH → suppression of LH, FSH,
GnRH, and testosterone and stimulation of breast tissue growth
Myxedema = due to accumulation of GAGs and hyaluronic acid w/in the reticular layer of the oedema
•
Complex protein mucopolysaccharides bind water → non-pitting oedema
•
Initially, oedema is pretibial, but as the condition progresses it can generalise, resulting in a
range of symptoms
Clinical manifestations
•
Symptoms related to ↓ metabolic rate = fatigue, ↓ physical activity, cold intolerance, ↓
sweating, hair loss, brittle nails, cold and dry skin, weight gain (despite poor appetite),
constipation, bradycardia, hypothyroid myopathy (myalgia, stiffness, cramps)
•
Symptoms related to generalised myxedema = doughy skin texture, puffy appearance;
myxoedematous heart disease (DCM, bradycardia); hoarse voice; pretibial and periorbital
oedema, myxedema coma
•
Symptoms of hyperprolactinemia = abnormal menstrual cycle (esp. secondary amenorrhea; or
Menorrhagia); galactorrhoea; ↓ libido, ED, delayed ejaculation, and infertility in M
•
Further symptoms = impaired cognition (conc., memory), depression; HT; Goiter (in
Hashimoto thyroiditis) or atrophic thyroid (in atrophic thyroiditis)
Diagnosis
•
TSH = ↑ in primary (compensatory elevation); ↓ in secondary and tertiary hypothyroidism. In
subclinical hypothyroidism = mildly ↑
•
Free T4 (FT4) and free T3 (FT3) = ↓ – FT3 levels aren’t a good indicator of hypothyroidism.
Because of the ↑ conversion of FT4 to FT3, FT3 levels may be normal even in the case of
hypothyroidism, ∴ FT4 levels are > accurate
•
AB testing = thyroglobulin (Tg AB) and thyroid peroxidase (TPO AB) are detectable in most
patients w/autoimmune hypothyroidism
•
Radioactive iodine uptake test = ↓ uptake indicates hypothyroidism
•
Thyroid US = to assess size, structure, or blood flow
Treatment
Lifelong drug treatment:
•
L-thyroxine (levothyroxine, a synthetic form of T4) = peripherally converted to T3 (biologically
active) and rT3 (biologically inactive)
•
Liothyronine = synthetic form of T3
•
Indications = myxedema, hypothyroidism
•
Side effects = sweating, heat intolerance, tachycardia, palpitations, tremors, weight loss,
•
Follow-ups w/lab controls of thyroid function (TSH) at regular intervals; adjustment of dosage
if necessary
79) Thyrotoxicosis. Hyperthyroidism
Definition
Thyrotoxicosis = a hypermetabolic condition caused by an inappropriately high level of circulating
thyroid hormones irrespective of the source. Hormones = T3 (triiodothyronine) and T4 (thyroxine).
Hyperthyroidism = condition characterised by overproduction of thyroid hormones by the thyroid
gland; can cause thyrotoxicosis
•
Overt hyperthyroidism = ↓ serum TSH w/↑ serum free T4 and/or T3 levels; patients typically
experience symptoms of thyrotoxicosis
•
Subclinical hyperthyroidism = ↓ serum TSH w/normal serum free T4 and T3 levels; patients are
normally asymptomatic or mildly symptomatic; may progress to overt hyperthyroidism
Etiology
•
Hyperfunctioning thyroid gland = Graves disease (60-80%; autoimmune condition in which
circulating TSH receptor auto-AB lead to overstimulation of the thyroid gland and excess
thyroid hormone production); toxic multinodular goiter (15-20%); toxic adenoma (3-5%); TSHproducing pituitary adenoma (thyrotropic adenoma)
•
Destruction of the thyroid gland = thyroiditis – subacute, drug-induced, Hashimoto thyroiditis
•
Exogenous thyrotoxicosis
•
Ectopic (extrathyroidal) hormone production – struma ovarii or metastatic follicular thyroid
carcinoma
Pathophysiology
The exact cause of Graves’ disease is unclear – combo of genetic and environmental factors.
•
It is an autoimmune disorder that results from the production of thyroid-stimulating
immunoglobulins (TSI) by stimulated B lymphocytes.
•
These immunoglobulins bind to the thyroid-stimulating hormone (TSH) receptor to mimic the
action of TSH and stimulate thyroid growth and thyroid hormone overproduction (phenomenon
= antigenic mimicry)
•
↑ In thyroid hormones will cause a –ve feedback to the hypothalamus, suppressing additional
release of TRH and TSH
•
Since auto-AB still exist (TSI), it will result in ↑ T3 and T4 and ↓ TSH
•
Predisposition factors = family predisposition, F sex, endemic region (> iodine in water)
•
Provoking factors = stress, infection (EBV is a potential trigger), meds (e.g. amiodarone), toxic
environment
Effects of thyrotoxicosis
Generalised hypermetabolism (↑ substrate consumption)
•
↑ N.o of Na/K ATPase → ↑ of basal metabolism → promoted thermogenesis
•
↑ Catecholamine secretion and upregulation of β-adrenergic receptors → hyperstimulation of
the SNS
Cardiac effects
•
↑ N.o of ATPase on cardiac myoctes and ↓ amount of phospholamban → transsarcolemmal
Ca2+ movement → enhanced myocardial contractility
•
Hyperadrenergic state → ↑ CO
•
↓ Peripheral vascular resistance
Clinical manifestations
•
General = heat intolerance; excessive sweating (↑
cutaneous blood flow); weight loss despite ↑
appetite; frequent bowel movements (due to
intestinal hypermotility); weakness, fatigue;
oncholysis; warm, moist skin
•
Graves’ triad = diffuse goiter, ophthalmopathy
(exophthalmos, ocular motility disturbances, lid
retraction and conjunctival conditions), and pretibial
myxedema
•
Cardiovascular = tachycardia; palpitations, irregular
pulse; HT w/widened pulse pressure (systolic
pressure ↑ due to ↑ HR and CO; diastolic pressure ↓
due to ↓ peripheral vascular resistance); abnormal
heart rhythms, including A-Fib; chest pain
•
Musculoskeletal = fine tremor of the outstretched hands; hyperthyroid myopathy (mainly prox.
muscles); osteopathy (osteoporosis due to the direct effect of T3 on osteoclastic bone
resorption; fractures)
•
Endocrinological = glucose intolerance (↓ insulin sensitivity of peripheral tissue, impaired
insulin secretion); oligo/amenorrhoea, anovulatory infertility, dysfunctional uterine bleeding
(F); gynecomastia, ↓ libido, infertility, erectile dysfunction (M)
•
Neuropsychiatric = anxiety, emotional instability, depression, restlessness, insomnia.
•
If thyroid gland becomes very large, it may cause pressure symptoms and signs, including
dysphagia (difficulty swallowing), tightness in neck, and hoarseness
Diagnosis
•
Specific = ↓ TSH and ↑ FT3 and FT4; ↑ TSI. Other = ↓ total cholesterol, LDL and HDL levels;
hyperglycaemia; ↑ ESR in subacute thyroiditis
•
If Graves disease is suspected = TSH receptor AB (TRAb) (+ve in Graves); ↑ anti-TPO and
anti-Tg AB (non-specific)
•
ECG findings = tachycardia; A-Fib
•
Imaging = thyroid US w/Doppler; thyroid scintigraphy (nuclear imaging technique that allows
the structure and function of thyroid tissue to be visualised based on its selective uptake of
radioactive iodine); MRI for pituitary (to check for secondary hyperthyroidism)
•
Further evaluation = US-guided FNAC; other thyroid AB (thyroid peroxidase AB, thyroglobulin)
•
Biopsy = most common for thyroiditis
Treatment
•
Anti-thyroid drugs = methimazole or propylthiouracil (for 1st trimester of pregnancy and in
thyroid storm) – usually lasting 12-18 months
•
Radioactive iodine ablation = destruction of thyroid tissue using radioactive iodine. Indicated
for toxic multinodular goiter and toxic adenoma; contraindications to anti-thyroid drugs; highsurgical risk; limited life-expectancy
•
Thyroid surgery = for very large goiters or thyroid malignancies
Calcium homeostasis and calcium physiology
Total and ionised Ca2+ concentrations
Total Ca2+ = the total amount of Ca2+ circulating in the serum, comprising protein-bound, anionbound, and ionised Ca2+
•
~ 40% of the total serum Ca2+ is bound to proteins (mostly albumin) and is physiologically
inactive
•
Hypoproteinemia → ↓ total Ca2+ level but ionised Ca2+ level is unaffected → factitious
hypocalcaemia
•
pH influences the binding of Ca2+ to serum proteins
↑ pH → ↓ H+ in serum binding to proteins → ↑ Ca2+ binding to proteins → ↓ ionised
Ca2+ conc., compensatory ↑ PTH
↓ pH → ↑ H+ in serum binding to proteins → ↓ Ca2+ binding to proteins → ↑ ionised
Ca2+ conc., compensatory ↓ PTH
Ionised Ca2+ = the Ca2+ fraction that is not bound to any proteins but is physiologically active.
~ 45% of the total serum Ca2+
•
Functions as the main regulator of PTH
secretion
•
PTH secretion is influenced by pH
variations but not by changes in albumin
levels
•
An excess causes true hypercalcemia
whereas a deficiency causes true
hypocalcaemia
The physiological role of Ca2+
•
Ionised Ca2+ is responsible for stabilising
the resting membrane potential of cells – ↓
Ca2+ = ↑ membrane excitability; ↑ Ca2+ = ↓
membrane excitability
•
Acts as 2nd messenger in signalling pathways
•
Cofactor for several enz. (e.g. phospholipase A, GGT)
•
Required for the promotion of coagulation pathways
•
PTH = ↑ serum Ca2+; ↓ phosphate
•
Calcitriol (vitamin D3) = ↑ serum Ca2+
•
Calcitonin = ↓ serum Ca2+
80) Nodular goiter. Endemic and sporadic goiter
Goiter
•
enlarged thyroid gland
•
F > M (4:1)
• Freq ↓ w/ age
Nodularis
•
Nodules disordered growth of thyroid cells ofter w/ gradual development of fibrosis
Etiology:
1. Iodine deficiency (most common cause)
a. ↓ efficacy of thyroid hormone synthesis ↑ TSH
2. Inflammation
a. Hashimoto's
b. Subacute granulomatous thyroiditis.
3. Graves disease
4. Thyroid Cysts
5. Thyroid Adenomas
6. Thyroid Carcinomas
7. Ingestion of Goitrogens (ex: lithium carbonate)
8. Elevated TSH production. (Pituitary adenoma, paraneoplastic syndromes)
9. Congenital Goiter
Thyroid gland:
•
Normal adult thyroid gland weighs 20-30g, w/ volume of 7-10mL located caudal to larynx
o medial borders: trachea & esophagus
o lateral borders: carotid sheath.
o
anterior side: sternocleidomastoid, sternohyoid, sterothyroid, & the superior belly of the
amohyoid muscle
Classification
•
Growth pattern.
o
o
•
Diffuse goiter
Graves dis, Inflamm - Hashimoto's, TSH secreting pituitary adenoma, Iodine
deficiency
Nodular goiter
Uninodular: cysts, adenomas, cancer
Multinodular - toxic or non toxic
Thyroid function
o
o
o
Nontoxic: normal TSH, fT3, fT4: Iodine deficiency
Toxic: ↑ Thyroid hormone production.
Hypothyroid: ↓ Thyroid hormone production
Diagnosis:
•
Palpation of the th gland.
•
LAB. Th function
•
Imaging: US (CT, MRI)
•
Fine needle biopsy for cytology if suspected pathology requires.
WHO Classification
•
Grade 0 - NO goiter palpable or visible.
•
Grade 1 - palpable goiter, not visible when neck is held in normal position.
•
Grade 2 - clearly swollen neck visible in normal position
Diffuse Nontoxic (Simple) Goiter OR Colloid Goiter → Absence of nodules & Hyperthyroidism
•
Most commonly caused by Iodine deficiency - ( termed "Endemic Goiter)
o
o
o
OR Unknown cause (OR Sporadic Goiter)
OR Goitrogen exposure → brussel sprouts, cabbage, cauliflower.
OR Inherited defects
•
F>M
•
In iodine deficiency
o
o
•
Thyroid enlargement reflects a compensatory effort to trap more iodine & produce
sufficient hormone under conditions that are insufficient
TSH: normal OR ↑
Clinical features:
o Mostly Asymptomatic, symmetrically enlarged, nontender, generally soft without
palpable nodules
o If markedly enlarged: can cause tracheal OR esophageal compression.
dyspnoea upon exertion
dysphagia
o Pamberton's sign
o
LAB
bilateral arm elevation above the head results in facial plethora (flushed purple
cyanotic face) due to an obstructed thoracic inlet that ↑ venous pressure
(w/ symptoms of faintness)
Thyroid function tests to exclude hyper/ hypothyroidism
•
o
(in lodine deficiency: ↓T4, norm. T3, TSH
• + low urine iodine levels <50 mcg/L
Thyroid scan ↑ uptake in iodine deficiency
US
Iodine replacement induces variable regression.
Surgery rarely indicated unless there's evidence of compression.
Tx:
II. Nontoxic Multinodular Gaiter: w/ Nodules & Euthyroid.
•
Etiology: Genetic, autoimmune, environmental factors. F>M, ↑ freq. w/age
•
Clinical features
o Asymptomatic (Euthyroid): if large enough compressive symptoms, Pemberton’s sign.
•
Diagnosis
o Thyroid architecture is distorted w/ multiple nodules & morphology varying sizes, not
o
o
•
all are able to palpated – because some are deeply embedded
Thyroid function is normal
US (CT &MRI) to identify which nodules need to be biopsied
Hypoechogenic, microcalcified w/ irregular margins OR >1cm are suspicious.
Treatment
o Conservatively mainly
o Radiolodine can decrease goiter & may selectively ablate regions of autonomy ≈ 3.7
MBq/g of tissue
o Surgery for compression.
III. Toxic Multinodular Goiter → Subclinical Hyperthyroidism. OR mild thyrotoxicosis.
•
F>MM, usually in elderly
•
Pathogenesis similar to nontoxic MNG.
•
Clinical features
o Painters Goiter w/ multiple palpable nodules
typically already present for many years.
o Symptoms of thyrotoxicosis
Palpitations,
Tachycardia
Atrial fibrillation
Nervousness, tremor, weight loss
•
Diagnosis
o LAB: ↓ TSH, fT4 N/ ↑, fT3 ↑
o Thyroid scan: Heterogenous uptake w/ multiple regions of ↑ (hot nodules) & ↓ (cold
nodules) uptake
o US: for the cold nodules assessmento FNA may be needed.
•
Treatment –
o Antithyroid drugs (& B-Blockers for symptom control) –
o
o
Radioiodine ablation treats areas of autonomy & ↓ mass of goiter
Surgery (definitive tx). (pts Rould be rendered euthyroid before surgery
IV. Toxic Adenoma →Mild Thyratoxicosis.
•
Etiology: Acquired somatic, activating mutation in TSH-R, F>M, 30-50yrs
•
Diagnosis:
o
o
o
o
o
o
•
Abnormal (↓) TSH) (& ↑fT3). Symptoms of thyrotoxicosis
Presence of thyroid nodule usually palpable & painless
Absence of clinical features of other causes of thyrotoxicosis
US:
signs of benign thyroid nodule
Thyroid scan: definitive diagnostic test demonstrates
↑ focal uptake in the hyperfunctioning nodule (hot nodule)
& ↓ uptake in the remainder of th. gland - as the activity of the normal thyroid is
suppressed
FNA for suspicions
Treatment
o
o
o
o
Radioiodine Ablation. tx of choice
131-I is concentrated in the hyperfunctioning nodule w/ minimal uptake &
damage to the normal tissue
370-1110 mBq.
Surgical Enucleation OR lobectomy.
Antithyroid & B-Blocker drugs can normalize thyroid function
BUT NOT optimal for long term tx
Ethanol Injections & percutaneous radiofreq. thermal ablation under US guidance is
done for some.
ALL Thyroid Nodules should be evaluated for malignancy.
1. TSH levels.
a. ↑ TSH higher risk of malignancy in thyroid nodules.
b. ↓ TSH indication for thyroid scintigraphyi. to identity hyperfunctioning nodules
ii. these are rarely malignant
2. US
a. High risk pattern:
i. Solid hypoechoic nodule / part irregular margins, taller than wide shape,
microcalcifications, rim calcifications w/ excluding tissue, extrathyroid extension
81) Hyperprolactinemia. Prolactinoma
ETIOLOGY:
• Hyperprolactinemia is the most common pituitary hormone hypersecretion syndrome in both
men and women.
• PRL-secreting pituitary adenomas (prolactinomas) are the most common cause of PRL levels
>200 μg/L.
•
A.
B.
C.
D.
E.
F.
Less pronounced PRL elevation can also be seen with microprolactinomas but is more
commonly caused by drugs, pituitary stalk compression, hypothyroidism, or renal failure.
Physiological hypersecretion• Pregnancy; Lactation;
• Chest wall stimulation;
• Sexual intercourse;
• Stress;
Pituitary tumor • prolactinomas,=> tumors arising from lactotrope cells
• mixed GH/Prl secreting tumor,
• macroadenoma compressing stalk
Hypothalamic–pituitary stalk damage
• Tumors; Emptysella; Lymphocytic hypophysitis; Adenoma with stalk compression;
Granulomas; Rathke's cyst;
• Irradiation;Trauma; Pituitary stalk section; Suprasellar surgery
Systemic disorders• Chronic renal failure;
• Hypothyroidism → decreased T3/T4 → Increased TRH → Increased prolactin
• PCOS
• Cirrhosis ;
• Epileptic seizures
No cause found – idiopathic hyperprolactinemia
Drug-induced hypersecretion• Dopamine receptor antagonist - metoclopramide, domperidone
• Neuroleptics- Atypical antipsychotics: risperidone;
• Phenothiazines: chlorpromazine, perphenazine;
• Butyrophenones: haloperidol; Thioxanthenes;
• Antidepressants – tricyclics , selective serotonin reuptake
• inhibitors(SSRIs), MAO inhibitors, sulpiride, amisulpiride, imipramine,
• clomipramine, amitriptiline
• Dopamine synthesis inhibitors- α-Methyldopa;
• Catecholamine depletors- Reserpine;
• Opiates;
• H2 antagonists- Cimetidine, ranitidine;
• Calcium channel blockers- Verapamil;
• Hormones- Estrogens; TRH
Pathophysiology:
• increased prolactin → suppression of GnRH → decreased LH &FSH → decreased
estrogen and testosterone → hypogonadotropic hypogonadism
PRESENTATION:
• In Women; Amenorrhea, galactorrhea, and infertility are the hallmarks of
hyperprolactinemia
o If hyperprolactinemia develops before menarche, primary amenorrhea results;
o More commonly, hyperprolactinemia develops later in life and leads to oligomenorrhea
and ultimately to amenorrhea.
May have decreased libido, weight gain, mild hirsutism
•
In Men with hyperprolactinemia, diminished
o libido, infertility, gynecomastia,and visual loss (from optic nerve
o compression) are the usual presenting symptoms.
Gonadotropin suppression leads to reduced testosterone, impotence, and
oligospermia. True galactorrhea is uncommon in men with hyperprolactinemia
<10%.
The diagnosis of idiopathic hyperprolactinemia is made by exclusion of known
causes of hyperprolactinemia in the setting of a normal pituitary MRI.
LAB
Basal, fasting morning PRL levels (normally <20 μg/L) should be measured to assess
hypersecretion;
o In patients with markedly elevated PRL levels (>1000 μg/L), reported results may be
falsely lowered because of assay artifacts;
o Sample dilution is required to measure these high values accurately;
o Falsely elevated values may be caused by aggregated forms of circulating PRL, which
are usually biologically inactive (macroprolactinemia);
o Hypothyroidism should be excluded by measuring TSH and T4 levels.
o Exclude pregnancy- pregnancy test
Tumor size generally correlates directly with
o PRL concentrations; values >250 μg/L usually
o are associated with macroadenomas;
Men tend to present with larger tumors than
women, possibly because the features of male
hypogonadism are less readily evident
THERAPY:
• No treatment may be needed if asymptomatic and fertility is not desired =>should be
monitored by regular Prl measurement, and MRI scans
Cabergoline- a long-acting dopamine agonist with high D2 receptor affinity. The drug
effectively suppresses PRL for >14 days after a single oral dose and induces prolactinoma
shrinkage in most patients.
o (0.5 to 1.0 mg twice weekly)
Bromocriptine- a dopamine receptor agonist that suppresses prolactin secretion.
o Because it is short-acting, the drug is preferred when pregnancy is desired.
o In microadenomas bromocriptine rapidly lowers serum prolactin levels to normal in up
to 70% of patients, decreases tumor size, and restores gonadal function.
o In patients with macroadenomas, prolactin levels are also normalized in 70% of
patients and tumor mass shrinkage (≥50%) is achieved in most patients.
o (0.625–1.25 mg) at bedtime with a snack, followed by gradually increasing the dose.
o Most patients are controlled with a daily dose of ≤7.5 mg (2.5 mg tid).
Surgery- Indications for surgical adenoma debulking include dopamine resistance or
intolerance and the presence of an invasive macroadenoma with compromised vision
that fails to improve after drug treatment.
Radiotherapy for prolactinomas is reserved for patients with aggressive tumors that do not
respond to maximally tolerated dopamine agonists and/or surgery
82) Hypercalcaemic states
Definition = ↑ serum Ca2+ (> 2.62 mmol/L)
Etiology
•
Hyperparathyroidism = primary (parathyroid gland adenoma), secondary (renal insufficiency,
CKD), or tertiary (chronic secondary hyperparathyroidism)
•
Malignancy = most common cause is paraneoplastic production of PTHrP (e.g. SCC of the
lung, head and neck; breast, ovarian, bladder, and renal cancer; lymphoma and leukaemia);
osteolytic metastasis (e.g. multiple myeloma, breast cancer, lymphoma and leukaemia, renal
and prostate cancer); paraneoplastic production of calcitriol (e.g. lymphoma, ovarian
dysgerminoma)
•
Meds = thiazide diuretics (↓ renal Ca2+ excretion), Ca2+ supplements, excess vitamin D (↑
intestinal Ca2+ absorption)
•
Hyperthyroidism = ↑ thyroid hormone → ↑ osteoclastic activity → ↑ bone resorption
•
Long periods of immobilisation = lack of weight-bearing activities → osteoclastic activation →
bone demineralisation → hypercalcemia
Clinical manifestations
There is a general MNEMONIC for remembering the effects of hypercalcaemia: “Stones, Bones,
Groans, Thrones and Psychiatric Overtones”
•
Stones = nephrolithiasis, nephrocalcinosis
•
Bones = arthralgias, myalgias, fractures
•
Groans = abdominal pain, N/V, anorexia, constipation
•
Thrones = polyuria and dehydration (due to acquired renal ADH resistance. Although ADH is
being secreted, the kidneys no longer respond to it adequately – nephrogenic diabetes
insipidus)
•
Psychiatric Overtones = anxiety, depression, fatigue, cognitive dysfunction, insomnia, coma
Hypercalcaemia can result in an ↑ in HR (+ve Chronotropic effect) and ↑ in contractility (+ve inotropic
effect) → cardiac arrhythmias
Diagnosis = confirm true hypercalcemia; determine etiology; further tests = ECG (QT interval
shortening)
Treatment
•
Treatment of underlying disorder
•
Mild/asymptomatic hypercalcemia = encourage adequate oral hydration, ↓ dietary intake of
Ca2+; avoid thiazide diuretics, lithium, high-Ca2+ diet
•
Severe/symptomatic hypercalcemia = immediate therapy (IV hydration w/isotonic saline,
calcitonin) or cause-based therapy (bisphosphonates for excessive bone resorption; loop
diuretics for renal insufficiency or HF; dialysis in severe cases)
83) 9 – Hypocalcaemic states
Definition = ↓ serum Ca2+ (< 2.1 mmol/L)
Etiology
•
Hypoparathyroidism (low PTH) = due to surgical removal, autoimmune destruction, or
congenital disorders (e.g. DiGeorge syndrome) of the parathyroid glands
•
High PTH (secondary hyperparathyroidism) = due to vitamin D deficiency, CKD,
pseudohypoparathyroidism, hyperphosphatemia, acute necrotizing pancreatitis
•
Meds = loop diuretics (↑ renal Ca2+ excretion), calcitonin, glucocorticoids, PPIs (↓ absorption),
bisphosphonates (inhibit bone resorption)
•
Multiple blood transfusions and hemolysis = citrate in blood products chelates serum Ca 2+
•
Hypomagnesemia = → ↓ PTH secretion or induces PTH resistance → hypocalcaemia
•
Hyperventilation = redistribution of Ca2+ (respiratory alkalosis → protein-bound H+ ions are
released to balance pH → ionised Ca2+ binds to the newly freed protein-binding sites →
hypocalcaemia)
•
Renal tubular disorders
Clinical manifestations
Neurological manifestations
•
Tetany (↑ neuromuscular excitability) = paresthesias; spasms (carpopedal,
broncho/laryngospasms) and cramps; stiffness, myalgia
•
Manoeuvres to elicit latent tetany on physical exam = Chvostek sign (twitching of the facial
muscles elicited by tapping the facial n. below and in front of the ear); Trousseau sign
(ipsilateral carpopedal spasm occurring several mins after inflation of a BP cuff to pressures
above the systolic BP)
•
Seizure = may be initial or only symptom (generalised tonic-clonic seizures can occur in
severe hypocalcaemia or after acute drops in serum Ca2+)
Cardiovascular manifestations
•
Effects on CO = -ve Chronotropic effect (↓ HR) and –ve inotropic effect (↓ contractility) →
cardiac arrhythmias (symptoms include palpitations, irregular pulse, syncope)
•
ECG changes = QT prolongation, or intermittent prolongation of QTc (corrected QT interval)
•
Congestive HF
•
Hypotension
Manifestations of chronic hypocalcaemia
•
Psychologic/psychiatric = emotional instability, anxiety, depression, confusion/delirium,
psychosis
•
Ophthalmological = papilloedema (severe cases), cataracts, calcifications of the cornea
•
Neurological = pseudotumour cerebri, paradoxical CNS calcifications
•
Dental changes = altered morphology, dental enamel hypoplasia
•
Growth plate abnormalities and osteomalacia
Diagnosis
•
Confirm true hypocalcaemia = order total and ionised Ca2+ and/or check serum albumin and
calculate corrected Ca2+
•
Serum intact PTH; urine studies (24 hour urinary excretion of Ca2+ and Mg)
•
Determine etiology
•
Further tests = ECG (prolonged QT interval)
Treatment
Ca2+ supplementation = oral (calcium citrate/carbonate) supplementation for mild and/or chronic
hypocalcaemia (asymptomatic or only mild neuromuscular irritability, serum levels 1.9 – 2.12
mmol/L); IV (calcium gluconate/chloride) supplementation for severe and/or symptomatic
hypocalcaemia (serum levels < 1.9 mmol/L)
Treatment of the underlying condition = Hypoparathyroidism (Ca2+ and vit D supplementation);
discontinue causative meds (loop diuretics)
84) 10 – Acromegaly and diabetes insipidus
Acromegaly
Definition = a disorder that results from excess growth hormone (GH) after the epiphyseal growth
plates have closed
Etiology
•
Benign GH-secreting pituitary adenoma (>95% of cases)
•
Very rare = neuroendocrine or hypothalamic tumours, paraneoplastic syndromes
Ectopic secretion of GH by neuroendocrine tumours (e.g. SCLC, pancreatic islet-cell
tumour – as found in MEN1)
↑ Secretion of GHRH from a hypothalamic tumour or in paraneoplastic syndromes
Pathophysiology
Physiology of GH and insulin-like growth factor-1 (IGF-1)
•
GH secretion induced by stress, sport, and hypoglycemia; inhibited by hyperglycemia or food
intake
•
Hypothalamus secretes GHRH → ↑ secretion of GH → GH induces IGF-1 synthesis → ↑
serum IGF-1 via liver synthesis. This leads to → binding of IGF-1 to IGF-1 and insulin
receptors which stimulates cell growth and proliferation, inhibiting programmed cell death; ↑
secretion of somatostatin from the hypothalamus which ↓ GH and IGF-1 (-ve feedback)
Effects of a pituitary adenoma
•
Overproduction of GH → abnormally high serum IGF-1 levels → overstimulation of cell growth
and proliferation → symptoms of acromegaly
•
Tumour mass compresses neighbouring structures (e.g. optic chiasm) → symptoms of mass
effect
•
Impaired secretion of other pituitary hormones, especially gonadotropins → ↓ LH and FSH →
↓ testosterone and oestrogen
NB! Excess GH secretion before epiphyseal plate closure leads to pituitary gigantism w/a possible
height of ≥2 cm. GH excess after epiphyseal plate closure causes acromegaly, but no change in
height!
Clinical manifestations
•
Tumour mass effects = headache, vision loss (bilateral hemianopsia), CN palsies;
oligomenorrhoea, secondary amenorrhoea, galactorrhoea, vaginal atrophy in F; ED, ↓ libido
and testicular volume in M
•
Soft tissue effects = doughy skin texture, hyperhidrosis; deepening of the voice, macroglossia
w/fissures, obstructive sleep apnoea
•
Skeletal effects = enlarged nose, forehead, and jaw (macrognathia) w/diastema (enlarged gap
between the top incisors); widening hands, fingers, and feet; painful arthropathy (ankles,
knees, hips, spine)
Diagnosis
Hormone analysis
•
Serum IGF-1 conc. (best single test) = ↑ IGF-1 – acromegaly suspected
•
Oral glucose tolerance test (OGTT) w/baseline GH and measure GH after 2 hrs (the most
specific test) = acromegaly is rule out if GH is suppressed; if GH is not suppressed it is
confirmed acromegaly
Pituitary MRI = usually shows a visible mass – confirmed GH-secreting pituitary adenoma. If results
are normal, screen for extrapituitary cause (CT of chest and abdomen, measure GHRH)
DDx = gigantism, Marfan syndrome, pseudoacromegaly (med induced), prolactinoma
Treatment
•
Surgery = transsphenoidal adenomectomy (preferred method); surgical debulking (patients
w/parasellar disease and inoperable tumours)
•
Meds = somatostatin analogs, dopamine agonists (↓ tumour size and GH secretion); GH
receptor antagonists
•
Radiotherapy = conventional fractionated radiotherapy; stereotactic radiosurgery (gamma
knife, proton beam)
•
Follow up = assess IGF-1 and random GH level 12 weeks post surgery and then annually;
annual hormone testing for hypopituitarism; MRI 12 weeks post surgery
Diabetes insipidus (DI)
Definition = a condition in which the kidneys are unable to concentrate the urine
Etiology
Central DI (most common form) = caused by insufficient or absent hypothalamic synthesis or
secretion of antidiuretic hormone (ADH) from the post. pituitary
•
Primary (1/3) = most cases are idiopathic; hereditary form is rare; autoimmune etiology has
been suggested
•
Secondary (2/3) = brain tumours and cerebral metastasis (lung cancer, leukaemia/lymphoma);
neurosurgery (usually after removal of large adenomas); traumatic brain injury (pituitary
bleeding, subarachnoid hemorrhage); pituitary ischemia; infection (meningitis)
Nephrogenic DI (rare) = caused by defective ADH receptors in the distal tubules and collecting ducts
•
Hereditary (mutation in ADH receptor; very rare)
•
Acquired = adverse effects of meds (lithium); hypokalemia, hypercalcemia; renal disease (AD
PKD, renal amyloidosis); pregnancy
Dipsogenic DI = results from the excessive intake of fluids as opposed to deficiency of ADH. It may
be due to a defect or damage to the thirst centre, located in the hypothalamus, or due to mental
illness.
Gestational DI = occurs only during pregnancy and the postpartum period. During pregnancy,
women produce vasopressinase in the placenta, which breaks down ADH. It is thought to occur
w/excessive production and/or impaired clearance of vasopressinase.
Pathophysiology
•
ADH is made in the hypothalamus and stored in the pituitary. It helps regulate the amount of
fluid in the body i.e. controls water retention
•
> ADH in the blood = retain fluid. < ADH in the blood = excrete fluid
•
During dehydration, pituitary will release ADH
•
ADH usually acts by ↑ water permeability in the collecting ducts and DCT.
•
It binds to receptors on the DCT which stimulate translocation of aquaporins into the apical
membrane → reabsorption of free water into the bloodstream, thus concentrating urine (↓
urine volume and ↑ urine conc.)
Either ↓ ADH (central DI) or defective renal ADH receptors (nephrogenic DI) → impaired ability of the
kidneys to concentrate urine (hypotonic collecting ducts) → dilute urine (low urine osmolarity) → urine
osmolality changes
•
Normal = 500-800 mOsmol/kg
•
Partial DI = 300-500 mOsmol/kg
•
Complete DI = <300 mOsmol/kg, often <100 mOsmol/kg
Clinical manifestations
•
Polyuria w/dilute urine
•
Nocturia → restless sleep, daytime sleepiness
•
Polydipsia (excessive thirst)
•
In cases of low water intake → severe dehydration (altered mental status, lethargy, seizures,
coma) and hypotension
Diagnosis
Lab findings
•
Sodium = mild hypernatremia
•
ADH levels = ↓ in central DI; normal/↑ in nephrogenic DI
•
Plasma osmolality = high normal or slightly ↑ (280-290 mOsmol/kg)
•
Urine osmolality = low; urine specific gravity <1.006
Water deprivation test (confirmatory test)
•
After obtaining baseline lab values, patient stops drinking water for 2-3 hours before 1st
measurement
•
After 2-3 hours w/out drinking water = test urine volume and osmolality every hour; test Na+
and plasma osmolality every 2 hours
•
Water deprivation continues until = urine osmolality rises and reaches normal value (DI ruled
out and primary polydipsia confirmed); no change in urine osmolality despite ↑ plasma
osmolality; plasma osmolality >295-300 mOsmol/kg or Na+ ≥145 meq/L
•
In the later 2 situations → administer desmopressin (synthetic ADH analog) = in central DI,
urine osmolality ↑ after desmopressin admin (intact renal ADH receptors); in nephrogenic ID,
urine osmolality remains low (defective renal ADH receptors)
Treatment
•
Treat the underlying condition, ensure sufficient fluid intake, and initiate low-Na+, low-protein
diet
•
Central DI = desmopressin (synthetic ADH w/out VC effects) – intranasal, SC, or oral; side
effect of hyponatremia; alternatives include chlorpropamide
•
Nephrogenic DI = discontinuation of causative agent in med induced DI; thiazide diuretics;
NSAIDs; amiloride (patients w/lithium-induced DI as it blocks lithium entry through the Na+
channel)
85) Hypercorticism (AKA Cushing’s syndrome and disease,
hypercortisolism)
Definition
•
Hypercortisolism = ↑ synthesis and secretion of cortisol
•
Cushing’s syndrome (primary hypercortisolism) = signs and symptoms due to prolonged
exposure to glucocorticoids such as cortisol
•
Cushing’s disease (secondary hypercortisolism) = due to excessive production of ACTH
by pituitary adenomas
Etiology
Exogenous (iatrogenic) Cushing syndrome (most common cause) = prolonged glucocorticoid
therapy → hypercortisolism → ↓ ACTH → bilateral adrenal atrophy
Endogenous Cushing syndrome
•
Primary hypercortisolism (ACTH-independent Cushing syndrome) = autonomous
overproduction of cortisol by adrenal gland → ACTH suppression → atrophy of the
contralateral adrenal gland – causes include adrenal adenomas, adrenal carcinoma,
macronodular adrenal hyperplasia; 5-10% of cases
•
Secondary hypercortisolism is divided into:
Cushing disease (pituitary ACTH production) = pituitary adenomas → ACTH secretion
→ bilateral adrenal gland hyperplasia; 75% of cases
Ectopic ACTH production = paraneoplastic syndrome leading to ↑ ACTH secretion;
carcinomas (SCLC, renal cell carcinoma, pheochromocytoma); 15% of cases
Clinical manifestations
Skin
•
Thin, easily bruisable skin w/ecchymosis;
•
Stretch marks (classically purple abdominal striae)
•
Hirsutism; acne; flushing of the face
•
Delayed wound healing
•
Secondary hypercortisolism = hyperpigmentation (due to ↑ ACTH)
Neuropsychological = lethargy, depression, sleep disturbances, psychosis
Musculoskeletal = osteopenia, osteoporosis, pathological fractures; avascular necrosis of the
femoral head; muscle atrophy/weakness
Endocrine and metabolic
•
Insulin resistance → hyperglycemia → mild polyuria in the case of severe hyperglycemia
•
Dyslipidemia
•
Weight gain characterised by central obesity, moon facies, and a buffalo hump
•
Growth delay in children
•
↓ libido; virilisation, and/or menstrual abnormalities in F
Other features = secondary HT, ↑ susceptibility to infections, peptic ulcer disease, cataracts
MNEMONIC = CUSHINGOID (acronym for side effects of corticosteroids) = Cataracts, Ulcers,
Striae/Skin thinning, HT/Hirsutism/Hyperglycemia, Infections, Necrosis (of femoral head), Glucose
elevation, Osteoporosis/Obesity, Immunosuppression, Depression/DM2
Diagnosis
General lab findings = hypernatremia, hypokalemia, metabolic alkalosis; hyperglycemia;
hyperlipidemia; leukocytosis
Screening tests for hypercortisolism = ↑ 24-hr urine cortisol (3X the normal); ↑ early morning
serum cortisol following a low-dose dexamethasone suppression test; ↑ midnight salivary cortisol; ↑
midnight serum cortisol
Hormone analysis
•
Serum ACTH levels = suspect primary if ↓, secondary if normal/↑
•
If secondary hypercortisolism is suspected, use one of the following to differentiate the 2
types:
High-dose dexamethasone suppression test = Cushing disease if there is adequate
suppression of cortisol levels to <50% of baseline; ectopic ACTH production if there is
no suppression
CRH stimulation test = Cushing disease if ACTH and cortisol levels ↑ further; ectopic
ACTH production if there is no ↑
Imaging
•
CT and/or MRI of the abdomen = for adrenal tumours (if primary is suspected)
•
CT and/or MRI of the skull = if Cushing disease if suspected
•
Other tests if ectopic ACTH production is suspected = CXR and/or CT, abdominal and/or
pelvic CT, thyroid US
Treatment
Exogenous Cushing syndrome = consider lowering the dose of glucocorticoids; consider to the use
of alternative (e.g. azathioprine)
Endogenous Cushing syndrome
•
Inoperable disease (inoperable adrenal carcinomas, advanced SCLC) = drugs to suppress
cortisol synthesis (e.g. metyrapone, mitotane, ketoconazole)
•
Operable disease = surgical therapy to remove the pituitary, adrenocortical, or ACTHsecreting ectopic tumours.
86) Hypocorticism (AKA adrenal insufficiency, Addison’s disease)
Definition
•
Adrenal insufficiency = ↓ production of adrenocortical hormones (glucocorticoids,
mineralcorticoids, and adrenal androgens) from the adrenal glands
•
Primary hypocorticism (Addison’s disease) = insufficient adrenocortical hormone
production – caused by diseases directly affecting the adrenal gland
•
Secondary hypocorticism =↓ ACTH production (impaired hypothalamic-pituitary-adrenal
axis)
•
Tertiary hypocorticism = ↓ CRH production (impaired hypothalamic-pituitary-adrenal axis)
Etiology
Primary hypocorticism
Addison’s disease can be caused by abrupt destruction of the adrenal gland (acute adrenal
insufficiency) or by its gradual progressive destruction or atrophy (chronic adrenal insufficiency)
•
Autoimmune adrenalitis = ~80-90% of cases of primary adrenal insufficiency; associated w/
polyglandular autoimmune disease I (PGAD I) and II (PGAD II)
•
Infectious adrenalitis = TB (most common cause worldwide), CMV disease in
immunosuppressed, histoplasmosis
•
Adrenal hemorrhage = sepsis (→ hemorrhagic necrosis), DIC, anti-coagulants
•
Infiltration of the adrenal glands = tumours, amyloidosis, hemochromatosis
•
Adrenalectomy
•
Impaired activity of enzymes that are responsible for cortisol synthesis = cortisol synthesis
inhibitors (phenytoin, rifampin, ketoconazole, fluconazole), 21β-hydroxylase deficiency
•
Vitamin B5 deficiency (vit B5 ↑ production of adrenal hormones)
Secondary hypocorticism
Caused by conditions that ↓ ACTH production:
•
Sudden discontinuation of chronic glucocorticoid therapy or stress (e.g. infection, trauma,
surgery) during prolonged glucocorticoid therapy – prolonged iatrogenic suppression of the
hypothalamic-pituitary-adrenal axis due to long term cortisol therapy → ↓ CRH/ACTH release
(-ve feedback) → ↓ endogenous cortisol
•
Hypopituitarism = ↓ ACTH → ↓ endogenous cortisol
•
Postpartum ischemic infarction of the pituitary gland (Simmond-Sheehan syndrome)
•
Tumours of the pituitary gland
Tertiary hypocorticism
Caused by conditions that ↓ CRH production:
•
Most common cause is sudden discontinuation of glucocorticoid therapy
•
Rarer causes include hypothalamic dysfunction (trauma, mass, hemorrhage) = ↓ CRH → ↓
ACTH → ↓ cortisol release
Pathophysiology
Primary hypocorticism
Damage to the adrenal gland leads to deficiency in all 3 hormones produced by the adrenal cortex:
androgen, cortisol, and aldosterone. Symptoms don’t usually appear before >90% of the adrenal
cortices have been destroyed.
•
Hypoandrogenism = affects > commonly in F because M usually produce sufficient androgen
in the testes
•
Hypocortisolism leads to:
↑ ACTH → ↑ production of pro-opiomelanocortin (POMC) (in order to ↑ ACTH
production) → ↑ melanocyte-stimulating hormone (MSH) → hyperpigmentation of the
skin (bronze skin)
↑ ADH level → retention of free water → dilutional hyponatremia
↓ Expression of enz. involved in gluconeogenesis → hypoglycemia
Lack of potentiation of catecholamines action → hypotension
•
Hypoaldosteronism → hypotension (hypotonic hyponatremia and volume contraction),
hypokalemia, metabolic acidosis
Secondary hypocorticism = ↓ ACTH → hypoandrogenism and hypocortisolism; aldosterone
synthesis is not affected – mineralcorticoid production is controlled by RAAS and angiotensin II, not
by ACTH
Tertiary hypocorticism = ↓ CRH → ↓ ACTH → hypoandrogenism and hypocortisolism; aldosterone
synthesis is not affected
Clinical manifestations
•
Hypoaldosteronism (aldosterone normally ↑ renal Na+ and H2O reabsorption as well as K+ and
H+ excretion) = hypotension, salt craving
•
Hypocortisolism = weight loss, anorexia; fatigue, lethargy, depression; muscle aches;
weakness; GI complaints (N/V, diarrhoea); sugar craving; orthostatic hypotension
•
Hypoandrogenism = loss of libido; loss of axillary and pubic hair; loss/irregular menstruation
(F); impaired spermatogenesis (M)
•
↑ ACTH = hyperpigmentation of the skin, including areas that are not normally exposed to
sunlight (e.g. palmar creases, mucous membrane of the oral cavity)
MNEMONIC = Primary Pigments the skin, Secondary Spares the skin, Tertiary is due to Treatment
(cortisol)
Diagnosis
General lab findings =
●
Hyponatremia,
●
Hyperkalemia (not typically seen in secondary and tertiary),
●
Mild hypercalcemia,
●
Metabolic acidosis,
●
Hypoglycemia,
●
↑ creatinine and BUN as a result of hypovolemia,
● Eosinophilia
Diagnosis of hypocortisolism
•
Morning serum cortisol levels (best initial test) (<3 μg/dL)
•
Morning serum ACTH levels (↑ in primary [>100pg/ml], norm/↓ in secondary and tertiary)
•
ACTH stimulation test/cosyntropin test (confirmatory test): GOLD standard for Primary HC
o Primary: Cortisol levels remain low (18-20 μg/dL) despite ACTH administration
o Secondary/ Tertiary: Cortisol levels rise (18-20 μg/dL)
•
OR metyrapone stimulation test
Diagnosis of hypoaldosteronism =
●
↑ plasma renin activity/ concentration
● ↓ urine aldosterone level
Diagnosis of adrenal hypoandrogenism =
● ↓ DHEA-S
Identifying the underlying cause of adrenal insufficiency
•
Serum ACTH levels = used to distinguish between primary and secondary/tertiary – ↑ in
primary, ↓ in secondary/tertiary
•
CRH stimulation test = used to distinguish between secondary and tertiary – ↓ ACTH in
secondary, ↑ ACTH in tertiary
•
If primary =
o screen for auto-AB against 21-hydroxylase.
o adrenal imaging (US, MRI, CT) to detect lesions, masses, infection, or haemorrhage.
o screen for TB/HIV if infectious etiology is suspected
•
If secondary =
o
o
o
•
rule out iatrogenic cause (long-term cortisol intake),
head MRI (detect pituitary destruction/compression),
test for other pituitary hormone deficiencies (TRH, GnRH, prolactin, GH)
If tertiary =
o rule out iatrogenic cause,
o head MRI (detect hypothalamic destruction/compression),
o screen for congenital syndromes (DNA methylation analysis for Prader-Willi syndrome)
Treatment
Primary hypocorticism
•
Glucocorticoid replacement = hydrocortisone 20mg/day (2-3 daily doses – to emulate the
natural diurnal rhythm); and steroid stress dosing (↑ the dose during stressful situations –
infection, surgery, trauma)
•
Mineralcorticoid replacement = fludrocortisone: 50-100mcg/day
o (Prevents hyperkalemia, sodium loss, and volume depletion)
•
Loss of libido can be treated w/DHEA: 25-50/day (dehydroepiandrosterone)
•
Treatment of underlying cause
Secondary/tertiary hypocorticism
•
Only glucocorticoid replacement is necessary = hydrocortisone
•
And Loss of libido treated w/DHEA; treat underlying cause
•
Mineralcorticoid production is not ACTH-dependent and ∴ unaltered
•
In hypopituitarism = substitution of other hormones (e.g., TSH)
Complications – Adrenal crisis (Addisonian crisis)
•
Definition = acute, severe glucocorticoid deficiency that requires immediate emergency
treatment
•
Etiology = stress in a patient w/underlying adrenal insufficiency; sudden discontinuation of
glucocorticoids after prolonged use; bilateral adrenal hemorrhage or infarction; pituitary
apoplexy
•
Clinical features =
o
o
o
o
o
hypotension,
shock,
impaired consciousness, coma,
Fever,
GI complaint: Vomiting, diarrhoea, severe abdominal pain (which resembled
peritonitis);
•
Diagnosis: Clinical suspicion,
o Lab tests for hyponatremia, hyperkalemia, hypoglycemia, and metabolic acidosis
o Endocrine test if uncertain
Random cortisol levels (<10mcg/dl) prior glucocorticoid administration
ACTH stimulation test
•
Treatment =
•
Empiric glucocorticoid therapy
o Give high doses of hydrocortisone (100mg IV once then 200mg IV over 24hrs);
o Prednisolone (4-48mg divided in 4 doses/24hrs)
o
alternatively, dexamethasone (4 mg IV every 12 hours);
•
Consider adding Fludrocortisone: 50mcg/day (mineralocorticoid) if
o Patients receiving glucocorticoids other than hydrocortisone
o Patients with septic shock
•
Fluid resuscitation for hypotension/hyponatremia: 1L isotonic saline (0.9%) in first hr
•
Hypoglycaemia: IV dextrose 50%: 25g IV once
•
Search and treat underlying causes (sepsis)
•
Intensive care monitoring
87) Hypogonadism. Clinical features
Definition =
•
Hypogonadism = clinical syndrome associated w/impaired functional activity of the gonads
•
Primary hypogonadism (hypergonadotropic hypogonadism) = caused by defects inherent
w/in the gonad – insufficient sex steroid production
•
Secondary/central hypogonadism (hypogonadotropic hypogonadism) = results from
hypothalamic or pituitary defects (defect lies outside the gonad) – insufficient gonadotropinreleasing hormone (GnRH)and/or gonadotropin release at the hypothalamic-pituitary axis
Etiology
Primary hypogonadism
•
Primary gonadal insufficiency = Turner syndrome (F), Klinefelter syndrome (M), anorchia
•
Secondary gonadal insufficiency (damage to Leydig cells or ovarian tissue) = chemo, pelvic
irradiation, trauma/surgery, autoimmune disease, infections
Secondary hypogonadism
•
Genetic disorders = Kallmann syndrome, idiopathic hypogonadotropic hypogonadism, PraderWilli syndrome, Gaucher disease
•
Hypothalamic and/or pituitary lesions = neoplasm (prolactinoma, astrocytoma),
trauma/surgery/irradiation, infection
•
Eating disorders (functional hypothalamic amenorrhoea)
•
Drugs (opioids)
Pathophysiology
Diminished functional activity of the gonads → ↓ biosynthesis of sex hormones → impaired
secondary sexual characteristics and infertility
Hypergonadotropic hypogonadism = gonadal insufficiency → insufficient sex steroid production (↓
testosterone and oestrogen) → ↑ gonadotropin secretion (↑ FSH and LH) from the ant. pituitary →
lack of –ve feedback from the impaired gonads → further ↑ FSH and LH levels
Hypogonadotropic hypogonadism:
•
In Kallmann syndrome = impaired migration of GnRH cells and defective olfactory bulb → ↓
GnRH in hypothalamus → ↓ FSH and LH → ↓ testosterone and oestrogen
•
In hypothalamic and/or pituitary lesions = ↓ pituitary gonadotropins → ↓ testosterone and
oestrogen
Clinical manifestations
•
Delayed puberty = testicular hypoplasia, impaired muscle and body hair growth, high-pitched
voice, smooth skin (no acne), gynecomastia (M); primary amenorrhoea (F)
•
Developmental abnormalities w/genitalia (undescended testes, Hypospadias)
•
Infertility (↓ sperm count), impotence, and/or ↓ libido
•
Secondary amenorrhoea
•
Signs and symptoms of central hypogonadism = headaches, impaired vision, double vision,
galactorrhoea.
•
Features of the genetic diseases if present = gynecomastia (Klinefelter); webbed neck w/short
stature (Turner); muscular hypotonia, short stature, facial dysmorphia (Prader-Willi);
hepato/splenomegaly, painful bone crisis (Gaucher)
Diagnosis
Routine tests
•
↓ Serum testosterone (M) and ↓ serum oestrogen (F) levels
•
Determine if the source is primary/secondary hypogonadism = primary has ↑ GnRH, FSH/LH;
secondary has ↓ GnRH, FSH/LH
•
Bone scan may support the diagnosis = shows ↓ bone density (osteoporosis)
Further tests (based on suspected etiology)
•
Genetic testing = for Klinefelter, Turner, Prader-Willi, Kallmann syndromes
•
Serum prolactin (↑ in prolactinemia)
•
Pelvic US (e.g. gonadal dysgenesis in Klinefelter)
•
Brain MRI = for CNS lesions or Kallmann syndrome
•
ACTH stimulation test = to exclude congenital adrenal hyperplasia
Treatment
•
•
•
Treat underlying cause = e.g. surgical excision of tumour, drugs for prolactinomas
•
To improve fertility in postpubertal individuals w/secondary hypogonadism and, if
prepubescent, an alternative to triggering onset of puberty and growth = Pulsatile LH releasing
hormone or HCG in M; Pulsatile LHRH or gonadotropins in F
Hormone replacement therapy
Trigger onset of puberty in prepubertal individuals at appropriate age = testosterone
replacement therapy in M; oestrogen in F
88) Autoimmune disorders of the thyroid gland
A. Hashimoto Thyroiditis
Hashimoto disease is the most common form of autoimmune thyroiditis
Epidemiology: Sex: ♀ > ♂ (7:1)
• occurs in all age groups, most prevalent in women aged 30–50 years
Pathophysiology
• Unknown etiology: Genetic and environmental factors likely play a role.
• Immunological mechanisms:
• Associations with HLA-DR3, and DR5
○ Cellular (especially T cells) and humoral immune responses are activated. → active B
lymphocytes produce antibodies towards thyroid peroxidase (TPO) and
thyroglobulin (Tg) → destruction of thyroid tissue
• Associations: increased risk for non-Hodgkin lymphoma and autoimmune diseases (e.g.,
type 1 diabetes, SLE, Graves disease, Addison disease)
Clinical features:
• Early-stage
Primarily asymptomatic
Goiter: nontender or painless, rubbery thyroid with symmetrical enlargement
Hashitoxicosis: transient hyperthyroidism due to follicular rupture of hormonecontaining thyroid tissue that manifests with, e.g., irritability, heat intolerance, diarrhea.
Late-stage
o Thyroid may be normal-sized or small if extensive fibrosis has occurred.
o Hypothyroidism (e.g., cold intolerance, constipation, fatigue)
o
o
o
•
Diagnosis:
Thyroid metabolism
o Early-stage: transient hyperthyroidism possible (↓ (TSH), ↑ (FT3), and ↑ (FT4))
o Progression: subclinical hypothyroidism (↑ TSH; FT3 and FT4 normal)
o Late-stage: overt hypothyroidism (↑ TSH; ↓ FT4 and ↓ FT3)
Antibody detection
o Anti-TPO antibody positive (↑ anti-microsomal antibodies)
o Anti-Tg antibody positive
o Anti-TPO antibodies are also elevated in 70% of patients with Graves disease.
Other laboratory tests
o ↑ LDL and ↓ HDL ↓ Hb
Ultrasound
o Indications: to assess thyroid size, echotexture, and to exclude thyroid nodules
Fine-needle aspiration:
o to exclude malignancy or lymphoma, especially in cases of rapid goiter growth
Radioactive iodine uptake test (RIUT)
Differential:
• Diffuse toxic goiter/Graves disease
• Nontoxic/multinodular goiter
• Riedel thyroiditis (Riedel struma
• Postpartum thyroiditis
• Subacute thyroiditis (de Quervain thyroiditis)
Treatment
Levothyroxine (T4) replacement therapy
o Life-long oral administration of L-thyroxine (T4)
Life-long monitoring
o Due to decline in T4 production with increasing age
o Life-long monitoring of thyroid parameters (primarily TSH) is necessary to adjust
treatment accordingly and avoid hyperthyroidism
B. Graves disease
Graves disease is the most common cause of hyperthyroidism and often affects women. It is an
autoimmune condition that is associated with circulating TSH receptor autoantibodies leading to
overstimulation of the thyroid gland with excess thyroid hormone production.
Epidemiology• Most common cause of hyperthyroidism
• Sex: ♀ > ♂ (8:1)
• Typical age range: 20–40 years
Etiology:
• Genetic predisposition
o 50% of patients with Graves disease have a family history of autoimmune disorders
(e.g., type 1 diabetes mellitus, Hashimoto disease, pernicious anemia, myasthenia
gravis)
•
o Associated with HLA-DR3 and HLA-B8 alleles
o Autoimmunity: B and T lymphocyte-mediated disorder
Triggers
o Infectious agents: Yersinia enterocolitica and Borrelia burgdorferi
o Stress ( Stress causes cortisol-mediated immune suppression, which is often followed
by rebound immunologic hyperactivity and can trigger Graves disease in genetically
susceptible individuals)
Physical: surgery, trauma
Psychological
o Pregnancy
o Environmental factors: smoke, irradiations, drugs, endocrine disruptors
Pathophysiology
• General mechanism: B and T cell-mediated autoimmunity → production of stimulating
immunoglobulin G (IgG) against TSH-receptor (TRAb; type II hypersensitivity reaction) → ↑
thyroid function and growth → hyperthyroidism and diffuse goiter
Clinical features:
• Symptoms of hyperthyroidism
• Triad of Graves disease :
o Diffuse goiter
o Ophthalmopathy-exophthalmos, ocular motility disturbances, lid retraction
o Dermopathy (pretibial myxedema): non-pitting edema and firm plaques on the
anterior/lateral aspects of both legs
Diagnosis:
• The diagnosis of Graves disease is often apparent on clinical examination and is confirmed
through detection of specific thyroid antibodies.
• Best initial test: ↓/undetectable TSH and ↑ T3/T4
•
•
•
Measure thyroid antibodies
↑ TRAbs (Anti thyroid receptor antibody) (specific)
↑ Anti-TPO antibodies and anti-Tg antibodies (nonspecific)
•
Thyroid scintigraphy
o Indicated if TRAbs are low to establish a diagnosis
o Shows a diffuse uptake of radioactive iodine
o Contraindicatd in pregnancy
Thyroid ultrasound (with color Doppler)
o Indicated in pregnant women if TRAbs are low
o Shows an enlarged, hypervascular thyroid
•
Treatment• β-blockers: Propanolol 10 mg once. Rapid control of hyperthyroidism symptoms
• Antithyroid drugs: thionamides (e.g., methimazole 5-40 mg every 12-24 hours with
maximum 40 mg daily, propylthiouracil 50-150 mg)
• Radioactive iodine ablation
• Surgery: near-total thyroidectomy is rarely done in Graves disease
C. Subacute Lymphocytic thyroiditis-Postpartum thyroiditis
Affects approx. 5% of women and usually manifests during the 1st year after delivery
Most prevalent in women with type 1 diabetes mellitus, a history of postpartum thyroiditis, or
increased titers of thyroid peroxidase antibodies
Associated with increased titers of thyroid peroxidase antibodies
Pathophysiology:
1. Thyrotoxic phase
2. Hypothyroid phase
3. Euthyroid phase
The disease is self-limiting in most cases but a few patients may experience relapses, and permanent
hypothyroidism occurs in ∼ 15% of cases!
Clinical features:
• Painless, diffuse, firm goiter (thyroid size may be normal)
• Features of hyperthyroidism followed by features of hypothyroidism
Diagnostics:
• Thyroid function tests
o Thyrotoxic phase: ↑ T3 and T4 , ↑ thyroglobulin, ↓ TSH
o Hypothyroid phase: ↓ T3 and T4, ↑ TSH
• Confirmatory test
o ↑ ESR
o Radioiodine uptake study : ↓ iodine uptake (< 5%)
• Ultrasound: thyroid with poorly defined hypoechoic regions and decreased vascularity, giving
rise to a cobblestone appearance
Treatment
● Thyrotoxic phase
○ Consider beta-blockers
○ NSAIDs: pain control in the case of acute granulomatous thyroiditis
○ Occasionally corticosteroids (i.e. prednisolone)
○ Antithyroid drugs (e.g., methimazole) should NOT be administered.
● Hypothyroid phase: levothyroxine
89) Polycystic ovary syndrome
Polycystic ovary syndrome (PCOS) is one of the most common endocrine disorders in women. It is
characterized by hyperandrogenism (which primarily manifests as hirsutism, acne, and,
occasionally, virilization), oligoovulation /anovulation, and/or the presence of polycystic
ovaries .
PATHOPHYSIOLOGY
The exact pathophysiology is unknown.
•
Strong association with obesity → ↑ in peripheral estrogen synthesis from adipose tissue
and ↓ in peripheral sensitivity to insulin
•
Reduced insulin sensitivity (peripheral insulin resistance) and the consequent
hyperinsulinemia result in:
o Epidermal hyperplasia and hyperpigmentation (acanthosis nigricans)
•
↑ Androgen production in ovarian theca interna cells
o
↑ LH secretion → impaired follicle maturation with cyst formation due to lack of follicle
rupture and anovulation/oligoovulation → infertility
CLINICAL FEATURES: Onset: typically during adolescence.
Menstrual irregularities
1. 1* Primary or secondary amenorrhea – absence of menses for more than 3
months in individuals with previously regular cycles, or 6 months in individuals with
previously irregular cycles
2. 2* Oligomenorrhea
3. 3* Menorrhagia
4. 4* Infertility or difficulties conceiving
Insulin resistance and associated conditions
1. Metabolic syndrome (especially obesity) → ↑ risk of sleep apnea
2. Nonalcoholic fatty liver disease
Skin conditions
1. Hirsutism
2. Androgenic alopecia
3. Acne vulgaris
4. Oily skin
5. Acanthosis nigricans
Psychiatric conditions-Depression
Voice change may occur in severe forms of PCOS. However, it typically suggests a different
underlying cause of hyperandrogenism
Clinical features of hyperandrogenism
Virilization: the appearance of male secondary sexual characteristics in a female individual
1. Hirsutism: excessive male pattern hair growth (e.g., chin, upper lip, mid-sternum,
abdomen, back, buttocks)
2. Male-pattern hair loss
3. Acne
4. Increased muscle mass
5. Voice deepening
6. Clitoromegaly
Rapid onset of virilization is suggestive of exogenous androgen intake or androgen-secreting
tumours
Diagnostics
Laboratory tests to identify hyperandrogenemia
↑ Serum total testosterone
↓ SHBG – sex hormone binding globulin
Free androgen index - The ratio of the total testosterone level to the SHBG
level
Investigate for the underlying cause.
Treatment –
Medication to suppress or block androgen and manage symptoms of virilization
i. Oral contraceptive pills
ii. Antiandrogen drugs (e.g., spironolactone, finasteride)
Treat the underlying cause (e.g., surgery for androgen-secreting tumors).
DIAGNOSTICS: PCOS is diagnosed in adults based on the presence of at least two of the following Rotterdam
criteria, after other endocrinological conditions,
OCPs can interfere with the diagnostic accuracy of these criteria..
1) Oligoovulation and/or anovulation
2) Hyperandrogenism (based on clinical features or laboratory studies): for signs of acne,
alopecia, and hirsutism; and lab
3) Enlarged and/or polycystic ovary on ultrasound
a. Ovarian volume ≥ 10 mL
b. AND/OR the presence of multiple cystic follicles measuring 2–9 mm (string-of-pearls
appearance) in one or both ovaries
The 2018 International Evidence-based Guideline for PCOS recommends a threshold of ≥ 20 cystic
follicles.
US – Transvaginal – best visualization or transabdominal -focuses on the ovarian volume
Evaluate for comormidities – there’s and increased risk of metabolic syndrome and
endometrial cancer
LAB;
o Confirm hyperandrogenism:
Increased Testosterone
Increased androstenedione and dehydroepiandrosterone sulfated (DHEA) –
to rule out other causes
o Rule out differential diagnoses: e.g., pregnancy, . congenital adrenal hyperplasia,
Cushing syndrome, hyperprolactinemia, adrenal/ovarian tumours, hypothyroidism,
acromegaly
A. All patient TSH – rules out thyroid dis. Prolactin – rules out hyperprolctinemia
17-hydroxyprogesterone - Elevated in nonclassic congenital adrenal
hyperplasia
B. Patients with amenorrhea Serum or urine hCG – rules out pregnancy Serum
LH, FSH Features of hypercortisolism: Consider measuring cortisol in 24-hour urine, late-night salivary
cortisol, or a dexamethasone suppression test
A clinical picture of hyperandrogenism fulfils a diagnostic criterion of PCOS, even if
serum androgen levels are normal.
An elevated LH (with LH:FSH ratio > 2:1) is a characteristic finding in most patients
with PCOS but not necessary for diagnosis.
THERAPY
Encourage exercise and healthy eating (e.g. caloric restriction), and consider behavioral
strategies and modifications (e.g., setting goals, eating more slowly).
Target BMI < 25 kg/m2 (can reduce estrone production in the adipose tissue)
Patients not planning to conceive
o goals are to control menstrual irregularities and hyperandrogenism, treat comorbidities,
and improve quality of life.
1) Combined oral contraceptives
Indication: first-line treatment for hyperandrogenism and/or menstrual cycle
abnormalities
2) Metformin: improves menstrual irregularities, metabolic outcomes, and weight
(especially when combined with lifestyle modifications)s
3) Antiandrogens: controversial role ---spironolactone, finasteride, flutamide
Indications: can be considered for treatment of hirsutism and androgen-related
alopecia in patients unable to take or tolerate COCs
4) Additional interventions: antiobesity medications or bariatric surgery, may be
considered
Patients planning to conceive - management of comorbidities (e.g., weight loss for
overweight or obese patients) and induction of ovulation.
1) Letrozole: first-line therapy for ovulation induction aromatase inhibition reduces
estrogen production, stimulating FSH secretion and inducing ovulation
2) Clomiphene: alternative to letrozole ↑ pulsatile secretion of GnRH → ↑ FSH and LH →
stimulation of ovulation
3) Exogenous gonadotropins: for ovulation induction.
Agents: exogenous FSH and human menopausal gonadotropin
4) Metformin
5) Additional fertility interventions
Laparoscopic ovarian drilling A laparoscopic procedure in which ovarian tissue is reduced
with a laser beam or surgical needle to decrease its volume and androgen production
1) This hormonal shift can induce FSH secretion and improve ovarian function in patients
with polycystic ovary syndrome.
In vitro fertilization
A. Hirsutism: Nonpharmacological therapy is first-line (e.g., electrolysis, light-based hair
removal via laser or photoepilation)
B. Acne: Consider topical therapies (e.g., benzoyl peroxide, topical antibiotics)
COMPLICATIONS
A. Cardiovascular disease
B. Type 2 diabetes mellitus
C. Increased cancer risk (before menopause
a. Endometrial cancer
b. Ovarian cancer
c. Pancreatic cancer
d. Kidney cancer
e. Endocrine cancers (except thyroid)
D. Increased miscarriage rate
VI.Gastroenterology
90) Gastroesophageal reflux disease (GERD)
Definition = long-term condition in which there is reflux of stomach contents into the oesophagus,
resulting in either symptoms or complications.
Etiology
Factors that can contribute GERD include:
•
Hiatal hernia – ↑ the likelihood of GERD due to mechanical and motility factors
•
Obesity, pregnancy, stress
•
Iatrogenic (e.g. post-gastrectomy); GI malformations and tumours
•
Zollinger-Ellison syndrome – can be present w/↑ gastric acidity due to gastrin production
•
Hypercalcaemia – can ↑ gastrin production → ↑ acidity
•
Visceroptosis or Génard syndrome – stomach has sunk in the abdomen upsetting the motility
and acid secretion of the stomach.
•
Alcohol, heavy smoking, chocolate, caffeine, fatty foods
•
Certain medications such as prednisolone
Pathophysiology
•
GERD is thought to be associated w/temporary/brief relaxations of weak/incompetent LES
(i.e. LES isn’t closed properly). This allows reflux to occur and, in addition, ↓ clearance of the
refluxed acid from the oesophagus after it has occurred
•
Reflux occurs when the intragastric pressure is higher than that created by the LES
•
Delayed gastric emptying also may contribute to reflux by increasing gastric volume and
pressure w/greater chance for reflux
•
Oesophageal mucosal injury is related to the destructive nature of the refluxate and the
amount of time it is in contact w/mucosa
•
Impaired oesophageal acid clearance = normally, acid reflux is neutralised by saliva and
evacuated back to the stomach via oesophagus peristalsis. Clearance can be disrupted by ↓
saliva
Clinical findings
•
Typical symptoms = retrosternal burning pain (heartburn) – 30-60 mins after eating, relived by
sitting upright, often occurs at nigh); regurgitation; sour metallic taste in the mouth
•
Atypical = pressure sensation in the chest/non-cardiac chest pain; belching; bloating
dyspepsia; epigastric pain; nausea; halitosis
•
Extraoesophageal symptoms = chronic non-productive cough and night-time cough;
hoarseness (microaspiration of stomach contents leads to laryngeal and/or airway irritation);
dental erosions
•
Aggravating factors = lying down shortly after meals, certain foods/beverages
•
Physical examination = white surface of the tongue, possible odour
Diagnosis
•
No specific lab tests. In patients w/hiatal hernia may be found ↓ Hb. Ht, RBC, and Fe
•
Oesophagogastroduodenoscopy (EGD) = findings typically in the lower 1/3 of the oesophagus
– erythema, oedema, erosions, mucosal breaks, ulcerations, peptic ulcers, proximal migration
of the gastroesophageal junction (Barrett oesophagus/hiatal hernia)
•
Oesophageal pH monitoring (gold standard) = drops in oesophageal pH to ≤ 4
•
Manometry = identify problems w/the LES
DDx = other causes of chest pain (heart disease), extra-oesophageal reflux disease
Treatment
•
Lifestyle changes; proton pump inhibitors (omeprazole) or H2 receptor antagonists as
alternative or in addition to PPI
•
Surgery for severe GERD = Nissen fundoplication – upper part of the stomach is wrapped
around the LES to strengthen it and prevent acid reflux and to repair a hiatal hernia
Complications
•
Reflux oesophagitis = inflammation of oesophageal epithelium which can cause ulcers and
bleeding near the junction of the stomach and oesophagus
•
Oesophageal strictures = persistent narrowing of the oesophagus caused by reflux-induced
inflammation → dysphagia
•
Barrett’s oesophagus = intestinal metaplasia (changes of the epithelial cells from squamous
to intestinal columnar epithelium) of the distal oesophagus
•
Oesophageal adenocarcinoma
91) H. pylori infection
Definition = G(-), microaerophilic, spiral, flagellate, urease producing bacterium usually found in the
stomach. It causes gastritis, peptic ulcer, gastric adenocarcinoma, and low-grade gastric lymphoma
Epidemiology
The prevalence is high in developing countries (80-90%) and much lower (20-50%) in developed
countries. Infection rates are highest in lower income groups. Infection is usually acquired in
childhood; although the exact route is uncertain, it is most likely to be faecal-oral, or oral-oral. Once
acquired, the infection persists for life, unless treated.
Pathophysiology
Antral-predominant infection
Inflammation of the antrum → destruction of δ cells → ↓ somatostatin (normally reduces secretion of
GI hormones) → ↑ gastrin → ↑ production of gastric acids → prepyloric and duodenal ulcers
Body-predominant infection
Inflammation of the gastric body → local destruction of mucosa (via cytotoxins such as ammonia) →
↓ production of mucins and atrophy of the gastric glands → hypochlorhydria → hypergastrinemia and
epithelial dysplasia → epithelial metaplasia → ↑ risk of gastric cancers
Clinical manifestations
•
Up to 90% of people are asymptomatic; however, individuals have a 10-20% lifetime risk of
developing peptic ulcers
•
Acute infection = acute gastritis w/abdominal pain or nausea. If this develops into chronic
gastritis, symptoms are those of non-ulcer dyspepsia = abdominal pain, N/V, bloating,
belching
•
Bleeding in the stomach can occur → black stools; prolonged bleeding → anaemia
•
If bleeding is heavy → haematemesis, hematochezia, or melena may occur
•
Inflammation of the pyloric antrum is more likely to lead to duodenal ulcers, while inflammation
of the corpus (body) is more likely to lead to gastric ulcers
•
Chronic infection = ↑ risk of gastric cancer
Diagnosis
Non-invasive tests
•
Previously, serologic assays for AB to H. pylori were considered the test of choice (>85%
sensitivity and specificity). However, as the prevalence of infection has ↓, the % of false +ve
results has ↑ significantly, making these tests too unreliable
•
Urea breath tests = detection of a labelled carbon isotope in breath samples
•
Stool Ag assays = detects presence of H. pylori Ag in a stool sample; can be used for
diagnosis of current infection and proof of eradication after treatment
Invasive tests
•
EGD = used to obtain biopsy for histology staining and rapid urease test
•
Histology (gold standard) = staining and direct microscopic identification shows curved,
flagellate, G(-) rods
•
Rapid urease test = detection of ammonia production by the urease of H. pylori
Treatment
H. pylori eradication therapy (10-14 days) = triple therapy consisting of clarithromycin, amoxicillin or
metronidazole, and PPI (MNEMONIC – 3 days of C(AM)Ping)
92) Peptic ulcer
Definitions
•
Peptic ulcer = a defect in the gastric or duodenal mucosa w/a diameter of at least 0.5 cm and
a depth that reaches the muscularis mucosae
•
Gastric ulcer = a peptic ulcer of the gastric mucosa, typically located along the lesser
curvature in the transitional portion between the corpus and antrum
•
Duodenal ulcer = a peptic ulcer of the duodenal mucosa, usually located on the ant./post.
wall of the duodenal bulb
•
Erosive gastritis = acute mucosal inflammation of the stomach that does not extend beyond
the muscularis mucosae.
•
Duodenal ulcers are 3X > common than gastric ulcers and they occur ~10-20 years earlier
than gastric ulcers
Etiology
•
Chronic gastritis caused by H. pylori = up to 90% of duodenal ulcers and up to 80% of gastric
ulcers
•
Long term use of NSAIDs (mostly gastric ulcers)
•
Zollinger-Ellison syndrome/gastrinoma (duodenal ulcers) = a disease in which tumours
release abnormal amounts of gastrin which stimulates excess secretion of HCl from parietal
cells → damage to stomach mucosa → peptic ulcers
•
Alcohol, tobacco, spicy foods, and caffeine worsen peptic ulcers
•
Stress (shock, burns, operation)
•
Family predisposition
Pathophysiology
•
Gastric ulcers typically form in the lesser curvature of the antrum
•
Gastric ulcer is caused by inadequate natural defence of the stomach’s mucosa against
pepsin and HCl
•
H. pylori gastritis = ↑ acid secretion, ↓ protective factors/mucus production
•
Long-term use of NSAIDs = NSAIDs inhibit COX enz. which synthesise prostaglandins
(normally ↓ gastric acid secretion and ↑ bicarbonate and mucus secretion) → ↓
prostaglandins = gastric mucosa is susceptible to damage (erosions)
•
Duodenal ulcers typically occur right after the pyloric sphincter. Brunner gland (secrete
mucous rich in bicarbonate ions) hypertrophy occurs
•
Duodenal ulcer = pathologically excessive secretion of HCl
Clinical manifestations
Gastric ulcer
Common findings
•
Duodenal ulcer
Dyspepsia = postprandial heaviness, early satiety, and gnawing, aching, or
burning epigastric pain
•
Belching, bloating, and abdominal fullness
•
Pain relief w/antacids
•
Potential signs of internal bleeding (anaemia, haematemesis, melena)
•
~70% of patients are asymptomatic
•
Stool sample +ve for occult blood
Pain and eating
Pain in L epigastrium ↑
shortly after eating →
weight loss
Pain in R epigastrium; pain on an empty stomach that is
relieved w/food intake → weight gain.
Pain ↑ 2-5 hours after eating
Nocturnal pain
30-40% of patients
50-80% of patients
MNEMONIC = Gastric ulcer is associated w/pain after light (weight loss) Gorging. Duodenal ulcer is
associated w/relief after massive (weight gain) Desserts
Diagnosis
EGD (most accurate test to confirm the diagnosis)
•
Can do malignancy screening to differentiate peptic ulcers from gastric cancer
•
Invasive H. pylori testing
•
Simultaneous therapeutic measures = hemostasis treatment w/electrocautery for active
bleeding
•
Benign ulcer = smooth base, round edges, regular mucosa, typical location, chronic
inflammatory changes, and active granulation
•
Malignant ulcer = ulcerated mass protruding into the lumen, irregular edges, nodular/irregular
mucosa, atypical location, dysplasia and invasion of deeper layers
Biopsies
•
Gastric ulcers = multiple biopsies recommended – from edge and base of the ulcer (to rule out
malignancy); multiple biopsies from different areas of the stomach (to test for H. pylori)
•
Duodenal ulcers = obtain biopsies from ulcers w/endoscopic features that suggest malignancy
Treatment
•
Lifestyle changes: remove risk factors; avoid NSAIDs, restrict alcohol, smoking, stress
•
H. pylori eradication treatment if necessary
o
Triple therapy – Omeprazole (20-40mg/12hrs) + Clarithromycin (500mg/12hrs) +
Amoxicillin (1g/12hrs) for ~8weeks
•
Meds = antacids (CaCO3, MgOH, Al(OH)3) + acid suppression meds (PPI and H2 antagonists)
o Cytoprotective agents for GI mucosal protections – Sucralfate (1g/before meal) should
not be taken w/ PPI/H2 blocker, Misoprostol
•
Elective surgery =
o
o
For those with Medically refractory symptoms, Inability to tolerate or adhere to medical
treatment, massive bleeding, perforation, Confirmed UpGI malignancy
Types
Vagotomy (surgical division of ant. and post. vagal trunk of vagus n.)
Partial/total gastrectomy and reconstruction – Billroth, Roux-en-Y
Complications
•
Very deep ulcers can erode into underlying blood vessels → bleeding → haemorrhage into
GI tract can happen → rapid loss of blood → shock
•
Perforation = ulcer erodes all the way through the wall of the stomach or duodenum → GI
contents enter the peritoneal space
•
Penetration & fistula formation = penetration of the ulcer into adjacent organs, usually
pancreas, but also liver; the result is inflammation of the affected organs, most often
pancreatitis
•
Duodenal ulcer = perforation on ant. wall of duodenum → air collects under diaphragm →
irritating phrenic n. → referred pain up to the shoulder
•
Long standing duodenal ulcers near pyloric sphincter = much scarring or oedema → obstructs
normal passage of gastric contents → gastric outlet obstruction → nausea and vomiting
•
Malignancy Gastric ulcers have high malignant potential and should be biopsied, compared
to duodenal ulcers which are usually benign
93) Malabsorption
Definition
•
Malabsorption = the failure to transport dietary constituents (fats, carbs, proteins, vitamins,
minerals) from the lumen of the intestine into the ECF compartment for transport to various
parts of the body OR impaired absorption of digested food caused by alterations of the
intestinal mucosa
•
Global malabsorption = in diseases causing diffuse mucosal damage or a ↓ of the
absorptive surface (e.g. coeliac disease)
•
Partial malabsorption = caused by a localised absorption impairment, resulting in
deficiencies of specific nutrients (e.g. vit B12 deficiency in patients w/diseases affecting the
terminal ileum.
Etiology
•
IBD
•
Coeliac disease (gluten-sensitive enteropathy
•
Infections (e.g., tropical sprue, Giardiasis, traveller’s diarrhoea, Whipple’s disease
•
Lactose intolerance
•
SI resection (short bowel syndrome)
•
Chronic mesenteric ischaemia
•
Radiation colitis
•
Small intestinal bacterial overgrowth (SIBO)
Clinical manifestations
•
Global malabsorption = diarrhoea, steatorrhoea, abdominal distension, flatulence, weight loss,
fatigue, symptoms of specific deficiencies
•
Partial (isolated) malabsorption = only symptoms specific to individual nutritional deficiencies
(e.g., impaired cobalamin absorption w/megaloblastic anaemia)
•
Deficiency of fat-soluble vitamins = vitamin A (night blindness, xeroderma, xerophthlamia) and
vitamin D deficiency (Ricketts/osteomalacia, fatigue, bone pain, muscle
weakness/aches/cramps)
•
Deficiency of water-soluble vitamins
•
Zinc deficiency = immune dysfunction, impaired wound healing, hypogonadism, diarrhoea,
dermatitis, alopecia, abnormal taste and smell
•
Other deficiencies = protein (oedema, cachexia), IDA or microcytic anaemia, electrolytes
(hypokalemia or hypocalcaemia)
Diagnosis
•
Blood tests = macrocytic and/or microcytic anaemia; ↓ electrolytes, ↓ total protein, vitamin
deficiencies
•
Stool test = analysis of fecal fat over 72 hours; detection of pathogens
•
D-xylose absorption test = to assess the absorptive function of the upper SI – ↓ levels (urine
and blood) occur in malabsorptive disorders that involve damage to the intestinal mucosa
(coeliac, whipples disease) and in case of bacterial overgrowth. Normal (↑) levels suggest a
different cause
•
Hydrogen breath test = assess the intestinal absorption of individual carbs
•
Further testing for underlying diseases: e.g., celiac disease or lactose intolerance
Treatment
•
Symptomatic treatment = oral supplementation of fluid, nutrients, vitamins; calorie and proteinenriched diet; IV nutrition in severe cases (extensive intestinal resection)
•
Causal treatment of the underlying disease
94) Ulcerative colitis and Crohn’s disease – inflammatory bowel
diseases (IBD)
Etiology of inflammatory bowel diseases (ulcerative colitis and Crohn’s disease)
•
Exact cause is unknown, it arises as a result of the interaction of environmental and genetic
factors leading to immunological responses and inflammation in the intestine (immune
dysregulation and dysbiosis)
•
Ulcerative Colitis
o
Genetic predisposition = HLA-B27 association.
o
o
o
o
o
o
•
Ethnicity – White, Ashkenazi-jews
Family history of IBD
Protective factors – Smoking, Appendectomy
Diet = gluten sensitivity is common in IBD and associated w/having flare-ups. Diet high
in fat (esp. saturated and animal fats) are associated
Oral contraceptive intake
NSAID exacerbate UC
Crohn’s disease
o
o
HLA-B27 - NOD2 gene mutation in Crohn’s + Family history
Smoking = risk factor for Crohn’s; protective effect on UC
•
Microbiota = alterations in the microbiome may contribute to IBD
•
Breach of intestinal barrier = loss of integrity of the intestinal epithelium plays a key
pathogenic role in IBD
Ulcerative colitis (UC)
•
Definition = an IBD characterised by chronic mucosal inflammation and ulceration of the colon
and rectum
•
Mainly affects the mucosal and submucosal layer (unlike Crohn’s which involves all layers –
transmural)
•
May involve the rectum alone (ulcerative proctitis), rectum and sigmoid colon, or the entire
colon (pancolitis). Rectum is always involved.
•
Pattern: Continuous ascending inflammation beginning in the rectum and spreading
continuously proximally throughout the colon.
•
Lesions form in the crypts of Lieberkühn in the base of the mucosal layer
•
Inflammatory lesions can become necrotic and ulcerate
•
Mucosal layer develops tongue-like projections called pseudopolyps
Clinical manifestations
•
Intestinal symptoms = bloody diarrhoea w/mucus; fecal urgency; abdominal pain and
cramps; tenesmus
•
General = fatigue, fever, weakness
•
Skeletal (most common extraintestinal manifestation of UC) = osteoarthritis, ankylosing
spondylitis, sacroiliitis
•
Ocular = uveitis, episcleritis, iritis.
•
Biliary = primary sclerosing cholangitis – rare for patients w/UC to develop PSC, but up to
90% of all patients affected by PSC will also be affected by UC
•
Cutaneous = erythema nodosum, aphthous stomatitis, pyoderma gangrenosum
•
Types
o
o
o
•
Mild form → intermittent rectal bleeding, liquid stools
Moderate form → severe diarrhoea, frequent bleeding, abdominal pain
Severe form → continuous bloody stools resulting in severe anaemia (Hb <10g/dl), HR
>90/min, hypovolemia, impaired nutrition, fever >37.8
Course of the disease: Chronic intermittent, Chronic continuous, Acute fulminant
Diagnosis and treatment
Blood = ↑ ESR and CRP; leukocytosis; thrombocytosis, anaemia; ↑ perinuclear ANCA (medium
sensitivity but high specificity)
•
In case of concurrent PSC: ↑GGT
Colonoscopy + biopsy – GOLD standard for definitive diagnosis
•
Gross – early stages = inflamed, erythematous, oedematous mucosa; friable mucosa
w/bleeding on contact w/endoscope; fibrin-covered ulcers
•
Gross – chronic = loss of mucosal folds and haustra; strictures; deep ulcerations;
pseudopolyps (raised areas of normal mucosal tissue that result from repeated cycles of
ulceration and healing)
•
Pattern of disease involvement: Proctosigmoiditis, Left sided UC, Extensive UC
•
Histo – early stages = neutrophil infiltration limited to mucosa and submucosa; crypt
abscesses (neutrophil infiltration into the lumen of the intestinal crypts due to a breakdown of
the crypt epithelium)
•
Histo – chronic = lymphocyte infiltration; mucosal atrophy; altered crypt architecture; epithelial
dysplasia
•
NB! DON’T perform colonoscopy + biopsy in persons w/severe form/ acute flare → high risk of
perforation. Instead do a sigmoidoscopy as an alternative
Imaging useful for complications of UC: X-ray, Barium enema, CT, MRI, Ultrasound
Treatment
•
General = rehydration; supplementation of nutritional deficiencies; supplementation of
nutrition (severe cases may need feeding tube or parenteral nutrition)
•
Supportive meds = anti-diarrheal agents (loperamide), anti-cholinergics (propantheline,
dicyclomine) for abdominal cramping; NSAIDs, opioids, and anti-cholinergics should be
avoided in severe disease
•
Mild disease = 5-aminosalicylic acid derivatives (5-ASAs) – mesalamine, sulfasalazine,
olsalazine; if no improvement/not tolerated = topical corticosteroids (Budesonide) or oral
systemic corticosteroids
•
Moderate disease = oral and topical 5-ASAs, topical/systemic corticosteroids, anti-TNF
therapy (adalimumab), vedolizumab, tofacitinib
•
Severe disease = high dose oral and topical 5-ASAs, systemic corticosteroids, anti-TNF
therapy (adalimumab, infliximab), calcineurin antagonists (cyclosporin), vedolizumab,
tofacitinib, referral for surgery
•
Surgery = Proctocolectomy (curative)
o If medical therapy fails or complications arise – perforation, TMC, sepsis etc
o Proctocolectomy w/an ileal pouch-anal anastomosis (IPAA/J pouch) – resection of the
entire colon and rectal mucosa while sparing the anal sphincters
Complications = GI bleeding, toxic megacolon, fulminant colitis, colorectal cancer, colonic strictures,
amyloidosis
Crohn’s disease (CD)
Definition = a type of IBD that may affect any part of the GI tract from mouth to anus
Clinical manifestations
•
General = low-grade fever, weight loss, fatigue
•
CD most commonly affects the terminal ileum and colon, but involvement of any part of the GI
tract (from mouth to anus, except rectum) is possible
•
Transmural inflammation = involves the entire thickness of the bowel wall (all 3 mucosal
layers are affected) – submucosal layer is affected to the greatest extent
•
Intestinal symptoms = chronic diarrhoea, typically non-bloody; abdominal pain (RLQ);
malabsorption; palpable abdominal mass RLQ (adhesions); enterocutaneous/ perianal
fistulas often associated w/abscess formation (first signs);
•
Joints = enteropathic arthritis – e.g., sacroiliitis, AS, inflammation of peripheral joints
•
Eyes, and skin = same as UC
•
Oral lesions: Oral aphthae, Pyostomatitis vegetans
•
Liver/bile ducts = Cholelithiasis; urogenital system = urolithiasis (mostly calcium oxalate
stones)
Complications = intestinal fistulas and abscesses, intestinal obstruction, colorectal cancer, strictures,
intestinal perforation
Diagnosis and treatment
Blood = Anaemia (Pernicious, Iron deficiency, Chronic disease)
•
Monitor disease ↑ inflammatory markers (CRP, ESR, thrombocytes, leukocytes);
•
Rule out UC ↑ASCA, pANCA is most likely –ve
Stool = culture to rule out bacterial/parasitic infection;
•
Monitoring disease detection of fecal calprotectin and/or fecal lactoferrin; fecal occult
blood test
Endoscopy (Ileocolonoscopy) + biopsy
•
Skip lesions: Segmental/discontinuous pattern of involvement
•
Snail trails = linear longitudinal serpiginous ulcerations
•
Pinpoint lesions = small aphthous ulcerations
•
Cobblestone appearance of mucosa = inflamed sections followed by deep ulcerations that
resemble cobblestone
•
Erythema, transmural inflammation, fissures, fistulas, strictures
Can do EGD to evaluate involvement of the oesophagus, stomach, and duodenum.
Imaging for complications =
•
Cross-sectional enterography: MRE, CTE (oedematous intestinal wall thickening, strictures,
fistulas, abscesses)
•
Small bowel follow through (to detect fistulas “string sign”), US, abdominal X-ray, upper GI
series w/barium swallow.
Pathology
•
Skip lesions = a pattern of patchy, discontinuous inflammation in the bowel (affected areas
interspersed w/normal tissue)
•
Creeping fat; hypertrophic lymph nodes; transmural inflammation (non-caseating granulomas,
giant cells, distinct lymphoid aggregates of the LP)
Treatment
•
Lifestyle changes: Smoking cessation, avoid NSAID’s, manage stress, depression
•
Diet: treat nutritional deficiencies, malabsorption
•
Symptomatic treatment = anti-diarrheal agents (loperamide 4mg), topical corticosteroids, 5ASA, pain management
•
Induction phase: to manage acute flares; corticosteroids, biologics
•
Maintenance phase (for moderate-severe cases): to maintain remission; Anti-TNF (Infliximab)
+ thiopurines (Azathioprine); taper and discontinue steroids!!
•
Mild-moderate = topical corticosteroids: Prednisone, sulfonamides
o
If limited to right colon and ileum: Controlled ileal release Budesonide 9mg/day
•
Moderate-severe = oral s. corticosteroids: Prednisone (40mg) + Azathioprine /Infliximab,
Infliximab + Methotrexate, Mono: Vedolizumab
•
Severe to fulminant = IV systemic corticosteroids- Methylprednisolone (40mg) + Infliximab
•
Steroid refractory disease = TNF-α, if necessary, in combo w/thiopurine analogues
•
Surgery = non-curative, only used to treat severe complications or if medical therapy fails:
Balloon dilation = to treat intestinal stenosis
Percutaneous drainage of intraabdominal abscess = prevents retention of secretions
and abscessation; surgical drainage if this fails
Strictureplasty = to open the bowel stricture w/out having to resect the bowel
Limited resection (proctocolectomy) = in case of obstruction or strictures
Segmental colectomy: Laparoscopic/ open of diseased bowel segment
Comparison between Crohn’s and UC
Characteristic
Type of inflammation
Crohn’s disease
Granulomatous; transmural (deep)
UC
Ulcerative and exudative (nongranulomatous); super. (Limited to
mucosa)
Level of involvement
Transmural
Mucosal, submucosal
Areas of involvement
Any from mouth to colon, mainly ileum,
secondarily colon
Only colon, mainly rectum and L colon
Pain
Constant pain in RLQ (DDx acute
appendicitis)
Painful defecation, pain in LLQ
Diarrhoea
Common, typically non-bloody
Common, bloody w/mucus
Rectal bleeding
Rare
Common
Fistulas, strictures,
abscesses
Common
Rare
Skip areas
Yes
No
Pseudopolyps
No
Yes
Crypt abscesses
Uncommon
Common
Granulomas
Non-caseating granulomas
No granulomas
Cancer
SI, colon, non-Hodgkin
Cholangiocarcinoma, colorectal cancer
Antibodies
ASCA
p-ANCA
Surgery
Non-curative surgery for complications and
to alleviate symptoms
Curative surgery possible
(proctocolectomy)
95) Tumours of the colon (colorectal cancer – CRC)
Definition = development of cancer from the colon or rectum (LI)
Etiology (risk factors)
•
Advanced age: >40yrs
•
Hereditary syndromes = family history of CRC; familial adenomatous polyposis, (GS, TS, PJS,
JPS); hereditary nonpolyposis colorectal cancer
•
Associated conditions = colorectal adenomas and serrated polyps.
o IBD (chronic inflammation → hyperplasia → non-polypoid dysplasia → neoplasia).
(↑risk esp. w/ UC and PSC)
o DM-2
o Endocarditis from S.Gallolyticus
•
Lifestyle = smoking, alcohol
•
Diet = obesity, processed meat, high-fat and low-fiber
o Protective factors: long term use of NSAIDs, aspirin; physical activity, diet
Classification = proximal (caecum, ascending and transverse colon) and distal (descending and
sigmoid colon, rectum)
Most common type is adenocarcinoma w/4 types = polypoid, ulcerous, solitary, and infiltrative. Less
common types include = mucinous adenocarcinoma; signet ring cell, small cell, and Adenosquamous
carcinomas
Clinical manifestations
•
Often times asymptomatic, particularly during the early stages
•
Constitutional symptoms = weight loss, fever, night sweats, fatigue, abdominal discomfort
(symptoms similar to diverticulitis, especially in carcinoma of the rectosigmoid and descending
colon)
•
Symptoms of R side carcinomas (cecum, ascending, and transverse colon) = occult
bleeding/melena, IDA (due to chronic bleeding), diarrhoea, mostly exophytic mass
o
IDA in >50y men/post-menopausal women – think of CRC!
•
Symptoms of L side carcinomas (splenic flexure, descending and sigmoid colon, rectosigmoid
junction) = changes in bowel habits (size, consistency, frequency), blood-streaked stools
(visible/occult), colicky abdominal pain (due to obstruction), mostly infiltrating mass
o Bowel obstruction is the earliest sign due to smaller lumen and more solid fecal matter
on L side of colon
•
Symptoms of rectal carcinomas = hematochezia (passage of bright red, fresh blood in or
w/stools), ↓ stool calibre (pencil-shaped), rectal pain, tenesmus (urge to empty the
rectum/bladder), flatulence w/involuntary stool loss, fecal incontinence (involuntary).
o Consider CRC in any patient with Hematochezia!
•
Symptoms of advanced disease = palpable abdominal mass, intestinal obstruction or
perforation
•
Metastasis to liver (abdominal distension, hepatomegaly, RUQ pain, ascites, jaundice), or
lung (dyspnoea, cough, hemoptysis, pleural effusion). Less commonly to peritoneum w/ worse
prognosis (ascites, ab distension, diffuse ab pain, bowel obstruction). Rarely – Virchow node
(supraclavicular lymph node)
Diagnosis
Initial work-up
•
Digital rectal examination (with LGI symptoms) = distal rectal cancers are palpable
•
Complete colonoscopy (gold standard) + biopsies
o
o
Ulceroproliferative friable mass
Alternatives: CT colonography, capsule endoscopy
•
Flexible sigmoidoscopy +/- anoscopy: who are <40yrs, no RF’s/ red flags for CRC.
o Rule out hemorrhoids, fissures
•
Double-contrast barium enema (uncommon) = only if colonoscopy is incomplete. Shows
characteristic apple core lesion = a filling defect due to constriction of the colonic lumen by a
stenosing colon carcinoma
Staging and additional tests
•
Staging = endorectal US (depth of tumour), CT (abdomen, pelvis, and chest), MRI, PET-CT
•
Labs: CEA, CBC (IDA)), LFT’s (abnormal if metastasized)
•
Prognostic monitoring via carcinoembryonic antigen (CEA) = tumour marker – monitor levels
during course of treatment and the follow-up period to evaluate treatment response and
recurrence. Not useful in screening. Can also use CA19-9
AJCC staging for CRC
TNM
0
Tis, N0, M0
I
Up to T2, N0, M0
II
Up to T4, N0, M0
III
Any T, N1/N2, M0
IV
Any T, any N, M1
Description
Tumor in situ – no invasion
Tumor invasion
•
T1: submucosa
•
T2: muscularis propria
•
T3: subserosa
•
T4a: visceral peritoneum
•
T4b: adjacent tissue or organs
Regional LN involvement
•
N1: 1-3 LN
•
N2: 3-7 LN
Distant metastases
•
M1a: affecting only one organ or site
•
M1b: affecting more than one organ or site
•
M1c: peritoneal metastases (regardless of
metastasis to other organs)
Treatment
Treatment mainly depends on the location of the tumour and the TNM stage.
•
Curative approach = any primary tumour w/ or w/out regional spread; treatment involves
surgical resection and adjuvant chemo
•
Palliative approach = distant metastasis beyond the liver and/or lung; patient is not a surgical
candidate due to poor general health; treatment involves palliative chemo and palliative
surgery (to manage complications of the primary tumour such as obstruction)
Surgery options
•
Colon cancer
o
Types
R hemicolectomy = Resection of part of the distal ileum, the ileocecal valve,
cecum, ascending colon, hepatic flexure, and proximal third of the transverse
colon w/end-to-end/end-to-side ileocolonic anastomosis. T in cecum/ascending
colon
Extended RHC RHC + transverse colon w/end-to-end/end-to-side
ileocolonic anastomosis. T = in proximal/middle transverse colon
o
L hemicolectomy = distal 1/3 of the transverse colon, the splenic flexure,
descending colon, and sigmoid colon. Perform a colorectal anastomosis.
Sigmoid colectomy
Transverse colectomy
Total abdominal colectomy = indicated for hereditary and multifocal carcinomas
Stages
I Curative surgery
II, III Curative surgery + Adjuvant chemotherapy
IV Neoadjuvant chemo, if Resectable: CS +AC; Unresectable: palliative
chemo/surgery
•
Rectal cancer =
o Types
Transanal excision (early, localised disease- Stage I),
Low ant. resection (locally advanced disease; Stage II-III): Sphincter-preserving
resection of the rectum and sigmoid/ Total mesorectal excision
Abdominoperineal resection – Stage IV (if the distal margin to the rectum
cancer is < 2-5 cm to the anus – resection of rectum, sigmoid, and anus)
o Stages
I Curative surgery
II, III Neoadjuvant chemo and/or radiotherapy, Curative surgery, Adjuvant
•
chemotherapy, consider adjuvant radiotherapy
IV Neoadjuvant chemo, if Resectable: CS +AC/AR; Unresectable: palliative
chemo/surgery
The surgery option depends on the blood supply. Before resection, the arteries have to be
ligated. Also surrounding lymph nodes must be removed as they are near the blood supply.
•
Regional lymph node dissection
•
Resection of metastases in the liver and/or lung
•
Palliative surgery = intestinal bypass (ileocolonic anastomosis, colostomy), enteral stenting,
resection, colostomy
Systemic therapy
•
Chemotherapy –
o FOLFOX/FOLFIRI (FOLinic acid + 5-FU + OXaliplatin or IRInotecan);
o CAPOX (CAPecitabine + OXaplatin).
o Radiotherapy is not standard treatment choice in colon cancer due to adverse effects
on the SI, leading to enteritis and strictures.
•
Rectal cancer = neoadjuvant radio (locally advanced disease), adjuvant and palliative chemo
•
Biological treatment: anti-VEGF AB: Bevacizumab; EGFR AB: Cetuximab
96) Chronic viral hepatitis
Definition = chronic inflammatory rxn of the liver of >3-6 months duration.
Etiology
Of the hepatotropic viruses, only 3 are known to cause chronic hepatitis = HBV, HCV, and HDV.
•
HBV = 5-10% of chronic liver disease; < likely than HCV to progress to chronic infection
•
HCV = ~85% will develop chronic infection, accounts for most cases of chronic viral hepatitis
•
HDV = depends on concurrent infection w/HBV; only 5% of co-infected individuals develop
chronic disease, however >80% of superinfected people progress to chronic HDV-infection
HBV and HDV
•
Transmission = parenteral (contaminated needles or instruments that come into contact
w/the patient’s blood – IV drug users, healthcare personnel, blood transfusion patients,
tattooing/body piercing); sexual (M X M, multiple sexual partners/HBV +ve sex partners, sex
workers); mother-to-child (perinatal)
•
DNA virus of the hepadnaviridae family
•
Genome contains 4 genes encoding 5 proteins: S = surface Ag, C = core Ag and e Ag, P =
polymerase, X = X protein
•
Core Ag forms a protein shell around the viral DNA
•
The e (envelope) Ag is soluble and is released from infected cells into the blood → important
indicator of transmissibility
•
HDV expresses a protein Ag (HDAg) – marker for infection
•
Envelope contains surface Ag (HBsAg) – important for lab diagnosis and immunisation
•
Replication of HBV is distinguished by production of large amounts of defective particles w/out
viral DNA but w/HBsAg expressed on the surface
HCV
•
Transmission = parenteral, organ transplantation; sexual is rare; perinatal
•
High-risk groups = IV drug users, HBV/HIV +ve individuals, prison inmates
•
RNA virus of the flaviviridae family
•
There are 6 genotypes – the main ones in the US are genotype 1 and 2
•
Reinfection w/another HCV genotype is possible
•
The risk of chronic infection is multifactorial and depends on the host’s ability to clear the
pathogen through activation of multiple innate immunity pathways against the viral envelope.
Pathophysiology
HBV and HDV
Virus enters blood, infects hepatocytes, and viral Ag’s are displayed on the surface of the cells
Acute infection
•
In acute infection, the cellular immune response causes damage to hepatocytes
•
HBV-infected hepatocytes express viral peptides (HBcAg and HBeAg) on their surfaces →
detection of the HBV-derived peptides by lymphocytes and the subsequent activation of CD8+
T cells that attack the infected hepatocytes → hepatic inflammation w/destruction of
hepatocytes
Chronic infection = caused by viral persistence due to failing immune clearance, which promotes:
•
Persistent hepatic inflammation → necrosis, mitosis, and regeneration process → cirrhosis
and cellular dysplasia → HCC
•
Integration of HBV DNA into the host genome → altered expression of endogenous genes,
chromosomal instability → HCC
•
HBV proteins fulfil numerous immune-modulating functions that allow them to elude detection
by the immune system and avoid clearance
HCV
•
Infects mainly hepatocytes → death of hepatocytes is probably caused by immune attacks by
cytotoxic T cells
•
HCV infection strongly predisposes to hepatocellular carcinoma
•
Alcoholism greatly enhances rate of hepatocellular carcinoma in HCV-infected individuals
•
AB against HCV are made, but ~ 75% of patients are chronically infected and continue to
produce virus for at least 1 year = chronic carriers
•
Chronic active hepatitis and cirrhosis occur in approximately 10% of these patients
Clinical manifestations
HBV and HDV
•
Incubation period = 1-6 months. Chronic infection is defined as infection persisting for >6
months w/detection of HBsAg and, possibly, signs and symptoms of liver damage.
•
Most patients are inactive, non-contagious carriers
•
Potential reactivation of chronic inactive hepatitis can manifest variably = asymptomatic;
unspecific symptoms (fatigue, malaise, nausea, poor appetite, non-specific abdominal pain);
similar to acute hepatitis; hepatic failure
•
The younger when infected, the > likely a patient develops chronic HBV – only 5% of adults
compared to 90% of infants and ~50% of children 1-5 years
•
For acute infection = clinical course varies – serum sickness-like syndrome during prodromal
period (rash, arthralgia, myalgia, fever); subclinical hepatitis (~70%); symptomatic hepatitis
(~30% - serum sickness symptoms + nausea, anorexia, jaundice, RUQ pain). Symptoms
usually resolve after a few week weeks, but can last up to 6 months
HCV
Incubation period = 2 weeks – 6 months
Acute course = asymptomatic in 80% of cases. Symptomatic = malaise, fever, arthralgias, myalgias;
RUQ pain, tender hepatomegaly; N/V, diarrhoea; jaundice
Chronic course = seen especially in asymptomatic individuals (up to 85%), as the disease may go
undiagnosed, and treatment may be delayed or never initiated (carrier state).
•
Findings often mild, non-specific
•
Liver cirrhosis (up to 25%) w/in 20 years of infection
•
Extrahepatic features (common) = haematological (mixed cryoglobulinemia, lymphoma (B-cell
NHL), ITP, Autoimmune Hemolytic Anemia); renal (membranoproliferative GN, membranous
GN); rheumatological (polyarteritis nodosa, Sjogren syndrome); dermatological (Porphyria CT,
lichen planus); endocrine (DM, autoimmune thyroiditis), vascular (leukocytoclastic vasculitis),
Siladenitis
Diagnosis
HBV and HDV
•
Measure HBsAg and anti-HBc IgM – both appear in serum early on in disease
•
If HBsAg is +ve = measure HBeAg and HBV DNA to determine transmissibility
•
Lab tests for chronic hepatitis = mildly ↑ or unchanged AST/ALT, AST:ALT ratio ≥1, ↑GGT,
↑ALP, ↑ Ferritin, ↑ Bilirubin (mixed direct and indirect hyperbilirubinemia)
•
Lab tests for cirrhosis = ↓ albumin, ↑ INR/PT, ↑ bilirubin, ↓ CHE (serum cholinesterase)
•
US = ↓ echogenicity and no. of portal v. radical walls; ↑ liver echogenicity
•
Biopsy = indicated when diagnosis is uncertain and to exclude other causes of liver damage in
chronic disease
•
Test of common coinfections = HCV, HDV, HIV, syphilis
HCV
•
ELISA = detect anti-HCV AB
•
PCR for HCV RNA if AB are +ve –
o If positive PCR: active HCV infection (may be acute or chronic)
o If negative PCR: no active infection, but prior infection
o Determines HCV genotype and virus titer assists in treatment planning and monitoring
•
LFTs = ↑ transaminases w/AST:ALT ratio ≥1,
o
o
o
o
↓ total protein/albumin
↓ coagulation, (particularly ↑ prothrombin time),
↓ cholinesterase,
↑ cholestasis parameters (GGT, ALP, bilirubin)
•
Inflammatory markers = leukocytosis, ↑ ferritin
•
US = detection of cirrhosis and neoplasia (HCC)
•
Liver biopsy = if diagnosis is uncertain, fibrosis, response to therapy
•
Rule out coinfections = HIV, HAV, HBV
Pathology
HBV and HDV
In chronic phase:
•
Formation of lymphoid follicles and mononuclear infiltrates
•
Piecemeal necrosis = periportal liver cell necrosis w/lymphocytic infiltration; caused by a CD*+
T cell-induced hepatocyte apoptosis
•
Fibrous septa
•
Ground glass hepatocytes = hepatocytes w/swollen transparent cytoplasm due to hyperplasia
of the ER resulting in a ground glass appearance; pathognomonic for HBV
HCV
In chronic phase:
•
Lymphoid follicles in portal triad
•
Necroinflammation of periportal liver cells
•
Variable degree of fibrosis
•
Severe hepatocyte injury
•
Without treatment, the disease will ultimately progress to liver fibrosis, cirrhosis, and HCC
Treatment
HBV and HDV
•
General = weight loss, cessation of alcohol use, discontinuation of hepatotoxic meds
•
Nucleoside/nucleotide analogs = indicated in patients w/both decompensated and
compensated liver disease and for patients who don’t respond to interferon treatment.
o Tenofovir is preferred due to its high efficiency + low rates of drug resistance.
o Entecavir
o Lamivudine (not preferred due side effects, resistance)
•
Pegylated interferon alfa (PEG-IFN-α) = recombinant IFN-α conjugated w/polyethylene
glycol (PEG) w/antiviral and antineoplastic properties. It is contraindicated in decompensated
cirrhosis, leukopenia or thrombocytopenia, pregnancy, and autoimmune conditions
o
•
Contraindicated in : Decompensated Cirrhosis, Psychiatric conditions, Pregnancy,
Autoimmune conditions, Leukopenia, Thrombocytopenia
Liver transplant = indicated in end-stage liver disease due to HBV, and fulminant hepatic
failure
•
Prophylaxis w/hep B vaccination
•
Special populations
o Coinfection w/ HIV: Tenofovir, Emtricitabine, Lamivudine
o Coinfection w/ Hep C: Tenofovir, Entecavir, DAA’s for HCV
o
o
Coinfection w/ Hep D: PEG-IFN-a, Tenofovir, Entecavir
Hep B w/ Pregnancy: Tenofovir, (IFN is contraindicated)
HCV
•
Goal is to cure and SVR (sustained virological response): No HCV RNA w/in 6months
•
General measures = same as HBV
•
Chronic HCV infection is always treated w/a multidrug approach
•
Treatment chosen based on prior treatment, fibrosis, viral genotype and load
•
Combo of 2 direct-acting antivirals = antivirals target and inhibit HCV-encoded proteins that
are essential for the HCV replication cycle
Sofosbuvir + velpatasvir for 12 weeks (all 6 genotypes)
Glecaprevir PLUS pibrentasvir (all genotypes)
Ledipasvir + sofosbuvir for 8-12 weeks (genotypes 1, 4, 5, and 6)
•
Interferon + ribavirin = may be used in the treatment of all genotypes.
o still used as a last resort in cases of treatment failure due to severe adverse effects
such as arthralgia, thrombocytopenia, leukopenia) + teratogenic
o Interferon contraindicated in decompensated liver cirrhosis
o Ribavirin can be combined w/ other DAA’s.
•
Patient category
o
o
o
•
w/out Cirrhosis: Glecoprevir PLUS pibrentasvir for 8 weeks, Sofosbuvir PLUS
velpatasvir for 12 weeks
compensated Cirrhosis: Glecaprevir PLUS pibrentasvir for 8 weeks
Decomepensated Cirrhosis: Ledipasvir PLUS sofosbuvir PLUS ribavirin for 12 weeks
(1,4,5,6), Sofosbuvir PLUS velpatasvir PLUS ribavirin for 12 weeks (all)
Failed treatment
o w/ Glecaprevir + Pibrentesvir: then
o
add Sofusbuvir + Ribavarin for 16wks
or voxilaprevir for 12wks (plus ribavirin if compensated cirrhosis)
w/ Sofosbuvir + Velpatasvir + voxilaprevir then
G + pirentasvir + S + R for 16wks
S + Vel + Vox + R for 24 wks
•
In addition to any treatment regimen = vaccinations for hep A and B
•
No prophylactic hep C vaccination exists
•
Liver transplant = end-stage liver failure
Complications of CLF
Fulminant hepatitis, Cirrhosis, HCC, Secondary hemochromatosis
97) Fatty liver. Alcoholic and non-alcoholic steatohepatitis
Fatty liver – alcoholic liver disease
Definitions
•
Fatty liver (hepatic steatosis) = a condition where excess fat builds up in the liver
•
Alcoholic steatohepatitis = a chronic, progressive liver disease characterised by thickening
and scarring (fibrosis) of the liver as well as possible necrosis of liver tissue, brought on by
excessive, prolonged alcohol use
Etiology = alcoholism: significant alcohol consumption (>210 g/wk for M and >140 g/wk for F)
Pathophysiology
Hepatic degradation of ethanol results in NADH excess → ↑ NADH drives the formation of glycerol 3phosphate (G3P) from DHAP → ↑ in both G3P and FA causes ↑ triglyceride synthesis in the liver and
accompanying inflammation → steatohepatitis → chronic inflammation leads to hepatic fibrosis and
sclerosis → portal HT and eventually cirrhosis
Clinical manifestations
The stages of alcoholic liver disease may overlap and do not necessarily occur in sequence
Alcoholic fatty liver (reversible)
•
Mostly asymptomatic; some patients report feeling a sensation of pressure in the upper
abdominal area
•
Hepatomegaly
•
Regresses after cessation of alcohol consumption
Alcoholic hepatitis (reversible in mild cases)
•
Develops as a result of persistent, long-term alcohol use
•
Non-specific symptoms = nausea, loss of appetite, weight loss, low-grade fever w/tachycardia
•
Hepatomegaly w/hepatic tenderness; jaundice
•
Symptoms of w/drawal in alcohol-dependent individuals
•
If portal HT ensures, splenomegaly, ascites, and/or variceal bleeding may occur
Alcohol-related cirrhosis (irreversible) = final stage – clinical features of cirrhosis
Diagnosis
Lab tests
•
AST > ALT (both ↑) – ratio >2 in alcoholic hepatitis
•
↑ ALP (hepatitis), ↑ GGT
•
Impaired liver function (hepatitis) = ↑ bilirubin, ↑ PT, ↓ serum albumin, ↓ cholinesterase
•
↑ CDT (carb-deficient transferrin) = most specific biomarker of heavy alcohol use, regardless
of the presence of liver disease
•
Hepatitis = ↑ GLDH, ammonia
•
Macrocytic anaemia
Imaging
•
US – alcoholic fatty liver = mild hepatomegaly, blood vessels can’t be visualised, ↑ liver
echogenicity because of steatosis
•
US – hepatitis = resembles alcoholic fatty liver; however, disease is typically diffuse; additional
findings of periportal oedema
•
CT = ↓ liver attenuation
Pathology = fat in hepatocytes; infiltration of WBC (neutrophils in hepatitis and lymphocytes in
cirrhosis); Mallory bodies in hepatitis; fibrosis (hepatitis); fibrous septa and regenerative nodules
(cirrhosis)
Treatment = immediate cessation of alcohol use; in some cases, glucocorticoids (prednisolone in
severe disease)
Non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH)
Definitions
•
NAFLD = non-alcohol related accumulation of fat in the liver cells
•
NASH = NAFLD w/ chronic inflammation and damage of liver cells
Etiology = obesity and/or DM2 (metabolic syndrome); meds (amiodarone, glucocorticoids, oestrogen);
parenteral nutrition after SI resection/other GI interventions
Pathophysiology = ↑ insulin resistance → ↑ peripheral lipolysis, ↑ triglyceride synthesis, and ↑ hepatic
uptake of FAs
Clinical manifestations = often asymptomatic; hepatomegaly; may
progress to cirrhosis
Diagnosis (of exclusion)
•
↑ Transaminases (AST/ALT ratio < 1) – MNEMONIC = there
is > ALT than AST if the Liver is infiltrated w/Lipids
•
The reversal of the AST/ALT ratio to values > 1 may indicate
progression to cirrhosis
•
Rule out other causes of chronic hepatitis (e.g. heavy alcohol use, HBV/HCV, Wilson disease,
hemochromatosis, autoimmune hepatitis, α1-antitrypsin deficiency)
Treatment
•
Weight loss, optimisation of diabetic treatment
•
Discontinue responsible meds
•
Ursodeoxycholic acid may have anti-inflammatory and anti-apoptotic effects in liver
•
Vitamin E may ↓ oxidative stress + improve aminotransferase levels in NASH patients
Complications = cirrhosis, hepatocellular carcinoma
98) Primary biliary cirrhosis (PBC). Primary sclerosing cholangitis
Definition
•
Primary biliary cholangitis/cirrhosis (PBC) = chronic progressive liver disease of
autoimmune origin that is characterised by destruction of the intralobular bile ducts; middle
aged F > M
•
Primary sclerosing cholangitis (PSC) = progressive chronic inflammation of both the
intrahepatic and extrahepatic bile ducts; middle aged M > F
Etiology
PBC
•
Exact cause is unclear; however, it is considered as an autoimmune disease and is
associated w/other autoimmune conditions (RA, Hashimoto thyroiditis, Celiac disease,
CREST/ Sicca syndrome).
•
Inflammation and progressive destruction of the small and medium-sized intrahepatic bile
ducts (progressive ductopenia) → defective bile duct regeneration → chronic cholestasis →
secondary hepatocyte damage due to ↑ conc. of toxins that typically get excreted via bile →
gradual portal and periportal fibrotic changes → liver failure → liver cirrhosis and portal HT
(advanced stages)
PSC
•
Exact cause is unknown – has been associated w/chronic IBD (90% of patients have IBD,
87% of which have UC, 15%~ Crohn’s); presence of HLA-B8 and HLA-DR3
Clinical manifestations
PBC
•
Often initially asymptomatic. Signs and symptoms are mainly due to the resulting cholestasis,
liver cirrhosis, and portal HT
•
Signs of cholestasis: Fatigue (1st sign), Xanthomas and xanthelasma, jaundice, pruritus
(marked, generalized), pale stool, dark urine, hyperpigmentation
•
Signs of cirrhosis in later stages: Hepatomegaly, (dull lower margin, RUQ discomfort),
Splenomegaly
•
PSC
Maldigestion; xanthomas and xanthelasma
•
Often initially asymptomatic
•
Signs of cholestasis = jaundice, pruritus, pale stool/dark urine, fatigue; can leads to acute
cholangitis
•
Later stages = signs of cirrhosis (hepatosplenomegaly, portal HT, liver failure)
•
Symptoms of chronic IBD (UC/ Crohn’s)
Diagnosis
PBC
•
Labs = ↑ cholestasis parameters (↑ ALP, GGT, conj-bilirubin);
o transaminases normal to ↑ slightly,
o ↑ anti-mitochondrial AB (AMA) (>95%); ↑ ANA (up to 70%)
o ↑ IgM
•
Imaging = Abd-US (screen for mechanical bile obstruction);
o MRCP (to confirm intrahepatic bile duct occlusion)
•
Liver biopsy = in case of suspicion for an overlap syndrome or uncertain diagnosis; necessary
for staging
PSC
•
Labs = pANCA are present in up to 80% of cases (not specific);
o ↑ cholestasis parameters (↑ ALP, GGT, conj-bilirubin,)
o ↑ cholesterol
o Transaminases= normal or slightly ↑ (<300IU)
o ↑ IgM
•
MRCP/ERCP (ERCP > invasive but > accurate) or Percutaneous Transhepatic
Cholangiography (PTC)–
o
Findings: Multifocal strictures alternating w/dilation and beading of bile ducts
•
US = irregular diameter of the bile duct; diffuse thickening of the wall of the common hepatic
and bile ducts
•
Colonoscopy: for IBD
•
Liver biopsy: Onion skin scarring and fibrosis of bile ducts
Treatment
PBC
•
No cure: treatment consists of slowing disease progression and alleviating symptoms;
•
Liver transplant is the only definitive treatment
•
Symptomatic =
o 1st line= Ursodeoxycholic acid/ Ursodiol (slows disease progression + improves clinical
symptoms; delayed need for transplantation); treatment of pruritus
o
•
2nd line= Obeticholic acid (inhibits cholesterol synthesis)
Liver transplant necessary if liver cirrhosis is advanced
PSC
•
Symptomatic =Ursodeoxycholic acid + Tacrolimus (immunosuppressive (may ↓ cholestasis
parameters)
•
Treatment of pruritus (e.g., cholestyramine, rifampicin, naltrexone)
•
Supplementation of fat-soluble vitamins (ADEK);
•
In case of bile duct stenosis: ERCP w/duct dilation= potentially stent placement
•
Surgical = Liver transplantation is the only curative option; performed in case of advanced
liver cirrhosis
Complications
PBC= Malabsorption, Liver cirrhosis and portal hypertension, Osteoporosis
PSC= Steatorrhea, fat soluble vit deficiency, Cirrhosis
•
Malignancy: Cholangiocarcinoma, Gallbladder carcinoma, Colorectal carcinoma,
Hepatocellular Carcinoma, Pancreatic carcinoma
99) Autoimmune hepatitis
Definition = rare form of chronic hepatitis that predominantly affects F.
Classification
•
Type I (most common), occurs mainly in adults
o ↑ levels of ANA, ASMA, anti-SLA/LP, AMA
o susceptibility resides mainly w/the HLA-DRB1 gene
•
Type II = occurs mainly in children (2-14 years)
o
o
anti-LKM-1, ALC-1
often accompanied by other autoimmune disorders; genetic component is < well
defined
Etiology
•
Idiopathic; however, a genetic predisposition as well as an association w/viral infection (EBV,
measles) and certain drugs (e.g. methyldopa, nitrofurantoin)
•
It is commonly associated w/other autoimmune conditions
o
Type 1: Hashimoto’s thyroiditis, Graves, Celiac disease, UC, RA
o
Type 2: Hashimoto thyroiditis, Type 1 Diabetes mellitus, Vitiligo
Clinical manifestations
•
Insidious onset in most patients and its presentation varies widely, ranging from asymptomatic
disease to severe symptoms or even acute liver failure
•
Non-specific = fatigue, upper abdominal pain, weight loss
•
Signs of acute liver failure (~1/3 of patients) = jaundice, RUQ pain, fever, hepatomegaly,
splenomegaly, Ascites
Diagnosis
•
Lab tests = ↑↑ ALT, ↑AST; ↑GGT, ↑ALP
•
CBC: Normochromic anemia, thrombocytopenia, mild leukopenia, ↑ ESR
•
Serum protein electrophoresis: Hypergammaglobulinemia (↑ IgG),
•
Serum AB
o
o
•
Type 1 AIH: ANA, ASMA, anti-SLA/LP, AMA
Type 2 AIH: anti-LKM-1, ALC-1
Liver biopsy = should be performed to confirm the diagnosis following detection of auto-AB.
o Histological findings reveal an ongoing inflammatory process w/lymphocytic infiltration,
multiacinar necrosis and fibrotic changes. Bile duct changes
DDx = viral hepatitis, PSC, PBC
Treatment
•
Immunosuppressive meds =
o 1st line= Prednisone and Azathioprine,
o 2nd line= Mycophenolate, cyclosporine, tacrolimus
o
•
Maintenance therapy w/ low doses of azathioprine or prednisone
Liver transplant = indicated in cases of decompensated liver cirrhosis
100) Liver cirrhosis – etiology, pathogenesis, clinical features
Definition = a condition of impaired liver function caused by the formation of scar tissue (fibrosis) seen
at the terminal stages of chronic liver disease (chronic disease of the liver marked by degeneration of
cells, inflammation, and fibrous thickening of tissue)
Classification
•
Clinical = compensated and decompensated
•
Histological = macronodular (due to hepatitis), micronodular (alcoholic), mixed (Wilson’s
disease)
Etiology
•
Hepatotoxicity = long-standing alcohol use disorder, meds (paracetamol, amiodarone, MTX),
aflatoxin, chemicals: tetrachloromethane, pesticides
•
Chronic viral hepatitis = hep B, D, and C and the most common cause in the US
•
Primary biliary cirrhosis, Primary Sclerosing cholangitis = autoimmune disease of the liver.
•
Secondary biliary cirrhosis = develops due to cholestasis caused by chronic obstruction of the
bile ducts by stones, inflammations, tumours
•
Parasitic infections – malaria, leishmaniasis, schistosomiasis
•
Metabolic = NASH, Wilson’s disease, hemochromatosis, α1-antitrypsin deficiency
•
Hepatic v. congestion or vascular anomalies = Budd-Chiari syndrome (partial/complete
occlusion of hepatic v. by thrombus); cardiac cirrhosis (due to R HF)
•
Cryptogenic cirrhosis = uncertain etiology
Pathophysiology
Cirrhosis is characterised by irreversible diffuse fibrosis of the liver. It is a multifactorial pathogenesis
= cytokine-mediated activation of hepatic stellate cells has been identified as a central element for
developing fibrosis.
The following three mechanisms have been described in all types of cirrhosis:
Degeneration and necrosis of hepatocytes
•
Activated Kupffer cells destroy hepatocytes, activate hepatic stellate cells, and promote
inflammation
•
Inflammatory cytokines (e.g., TGF-β, PDGF) → hepatocyte apoptosis and hepatic stellate cell
activation (transform into myofibroblasts at injury sites) → excessive collagen production
Fibrotic tissue and regenerative nodules replace the liver parenchyma
•
Hepatocyte destruction triggers repair mechanism → excess formation of CT (fibrosis)
•
Excessive CT in periportal zone and centrilobular zone → regenerative nodules and fibrous
septa → compression of hepatic sinusoids and venules → ↑ portal v. hydrostatic pressure →
intrasinusoidal HT → ↓ functional sinusoids
Loss of liver function
•
Sinusoidal capillarisation → loss of fenestration and scar tissue formation → impaired
substrate exchange → loss of normal liver function
Clinical manifestations
•
Non-specific = initially asymptomatic; fatigue, malaise, anorexia, weight loss
•
Dermal features = pruritus, jaundice, spider naevi/angiomata (swollen blood vessels), caput
medusae (paraumbilical dilation of SC vv.), palmar and
plantar erythema, petechiae and purpura, nail
clubbing, lacquered lips w/smooth red tongue
•
Abdominal features = N/V, hepatomegaly (possibly
causing RUQ pain; advanced cirrhosis causes liver to
contract and shrink in size), splenomegaly, ascites
(abdominal fluid build-up due to hypoalbuminaemia)
•
Hormonal = hyperestrogenism (due to changes in
metabolism of sex hormones) – causes feminisation in
M (gynecomastia, hypogonadism (erectile dysfunction,
↓libido), ↓ body hair) and can cause amenorrhoea in F
•
Other = Asterixis (flapping tremor), fetor hepaticus
(bad breath w/sweet, pungent smell), peripheral
oedema (due to hypoalbuminaemia)
•
Specific clinical features: Hemochormatosis (bronze
diabetes), Wilson disease (parkinsonism/ personality
changes, indirect hyperbilirubinemia), Alpha-1
antitrypsin deficiency (lung emphysema)
•
Advanced = Hepatic encephalopathy = liver doesn’t clear ammonia and other nitrogenous
substances from the blood → carried to the brain, affecting cerebral function; haemorrhagic
diathesis (due to ↓ production of coagulation factors)
Diagnosis
•
CBC = anaemia (micro/macrocytic), thrombocytopenia
•
Parameters of hepatocyte damage = ↑ASAT, ALAT, GGT, ALP, GDH, ammonia; ↑ bilirubin
•
Parameters of impaired hepatic synthesis = ↑ PT (↑ INR) (due to ↓ production of coagulation
factors), ↓ total protein (↓ albumin), ↓ plasma cholinesterase
•
Other lab tests: hepatitis (anti-HBs, anti-HBc, HBsAg, anti-HCV); serum α1-antitrypsin levels;
hemochromatosis (serum iron, ferritin, and transferrin saturation), Wilson disease (serum and
urine Cu, serum ceruloplasmin), AIHA (IgG, AMA, ASMA, ALKM-1), PBC (AMA, ↑ALP,
↑bilirubin), PSC (↑pANCA, ↑GGT, ALP & bilirubin)
Imaging
•
Abdominal US = best initial imaging study – liver is w/diffuse fibrous changes often w/nodular
characteristic
Liver form and structure = nodular liver surface, atrophy of R lobe, loss of structural
homogeneity w/fibrous septa
Liver size = initially enlarged; atrophies and shrinks w/disease progression
Other = loss of intrahepatic portal and liver vv.; complications such as portal HT
Check diameter of portal v. (> 14 mm); and only in cardiac cirrhosis the hepatic vv. and
IVC are also enlarged
•
CT = hypertrophy of L and caudate lobes, regenerative nodules, irregular liver surface
•
Biopsy (gold standard) = only considered if clinical, lab, and US is unclear; helps identify
cause and DDx from carcinoma
Monitoring disease course
• Abdominal US every 6months
• HCC screening: abd US every 6m + AFP levels mesurement
• Gastroscopy: esophageal varices
Pathology
•
Fibrosis (fibrous septa)
•
Replacement of normal liver tissue w/collagenous regenerative nodules. Histological staging
is based on the size of the regenerative nodule – micronodular (1-3 mm), macronodular (>3
mm), or mixed
•
Abnormal cell activation w/infiltration of inflammatory cells
•
Loss of physiological vessel architecture (central v. disappearance)
Treatment
•
Treat underlying condition; prevent and treat complications; avoid hepatotoxic substances
(alcohol, drugs); vaccinations (hep A/B, pneumococcal, influenza, tetanus); balanced diet
•
Meds = non-selective BB (propranolol) to lower portal pressure and prevent variceal bleeding;
spironolactone and furosemide to manage ascites and oedema in patients
w/hypoalbuminaemia
•
Interventional procedures
o Paracentesis = to decompress abdomen due to ascites
o
•
Transjugular intrahepatic portosystemic shunt (TIPS) = used to lower portal pressure
and manage complications – used for refractory ascites, recurrent oesophageal
varices
Surgery = liver transplant is the only curative option in patients w/decompensated cirrhosis
Prognosis
Child-Pugh score: A prognostic grading scale to assess the severity of cirrhosis; based on:
Points assigned
Parameter
1
2
3
Ascites
Absent
Slight
Moderate
Albumin
>3.5 g/dL (35 g/L)
2.8 to 3.5 g/dL (28 to 35 g/L)
<2.8 g/dL (<28 g/L)
Bilirubin
<2 mg/dL
(<34.2 micromol/L)
2 to 3 mg/dL
(34.2 to 51.3 micromol/L)
>3 mg/dL
(>51.3 micromol/L)
INR
<1.7
1.7 to 2.3
>2.3
Encephalopathy
None
Grade 1 to 2
Grade 3 to 4
Class A
Class B
Class C
Total points
5-6
7-9
10-15
1-yr survival
100%
80%
45%
Scoring system
101) Liver cirrhosis – complications: oesophageal varices, ascites,
spontaneous bacterial peritonitis (SBP), hepatorenal syndrome,
portal encephalopathy
Major complications
•
Complications caused by portal hypertension
a. Ascites and subsequent spontaneous bacterial peritonitis
b. Esophageal variceal hemorrhage
•
Hematologic complications: coagulopathy
c. Prolonged aPTT, INR, and PT. (Fresh frozen plasma is used as treatment)
•
Metabolic complications or associated organ impairment
d.
e.
f.
g.
Jaundice
Hepatic encephalopathy
Hepatorenal syndrome
Hepatopulmonary syndrome
•
Tumors:
h. hepatocellular carcinoma (HCC)
•
Other complications
i.
Secondary hyperparathyroidism
j.
k.
l.
m.
Cirrhotic cardiomyopathy
Hepatic hydrothorax
Portal vein thrombosis
Diabetes mellitus secondary to liver disease
Decompensated cirrhosis: worsening of liver function in cirrhosis characterized by the presence of
jaundice, ascites, variceal hemorrhage, or hepatic encephalopathy
•
When patients develop major complications (e.g., spontaneous bacterial peritonitis,
hepatorenal syndrome), they are considered to have decompensated cirrhosis.
•
Precipitating factors: infection, alcohol use, medications, bleeding, or dehydration
1. Oesophageal varices
Definition = dilated sub-mucosal vv. (varices) of the distal (lower 1/3) oesophagus. Oesophageal
varices have a strong tendency to develop severe bleeding (oesophageal variceal haemorrhage)
which left untreated can be fatal. It is the most common form of upper GI bleeding in patients
presenting w/cirrhosis
Etiology = portal HT commonly due to liver cirrhosis
Pathophysiology
In portal HT, blood flowing through the hepatic portal system is redirected from the liver into areas
w/lower venous pressures. This means that collateral circulation develops in the lower oesophagus,
abdominal wall, stomach, and rectum. The small blood vessels in these areas become distended,
becoming more thin-walled, and appear as varicosities.
Clinical manifestations
•
Symptoms of upper GI bleeding = signs of circulatory insufficiency, haematemesis, melena,
and/or hematochezia
•
Non-specific GI symptoms (inconsistent) = nausea, meteorism (excessive accumulation of
gas in the GI tract → abdominal distention), ↑ belching, upper abdominal pain/retrosternal
discomfort, dysphagia
Diagnosis
Clinical diagnosis = sudden onset of severe upper GI bleeding in a patient w/signs of portal HT,
typically in combo w/liver failure. If bleeding occurs following retching/vomiting, consider a MalloryWeiss tear as a DDx
Treatment
•
Stabilisation = bring patient into shock position; maintain plasma volume; intubate patient w/↓
consciousness to prevent aspiration/airway obstruction; NG tube to remove the blood and
prevent hepatic encephalopathy
•
Meds = octreotide for 3-5 days (inhibits secretion of VD hormones → indirect splanchnic VC
→ ↓ splanchnic blood flow); vitamin K is indicated for patients w/coagulation disorders; anti-B
prophylaxis for 7 days to prevent infections (1st line IV ceftriaxone; alternatively oral
ciprofloxacin)
•
Endoscopic management = endoscopic band ligation (procedure of choice; used for primary
prophylaxis and prevention of recurring haemorrhage); alternatively injection sclerotherapy,
absolute alcohol, fibrin glue to stop variceal bleeding; Balloon tamponade using Blakemore
tube
2. Spontaneous bacterial peritonitis (SBP)
Definition = infection of the ascitic fluid in the absence of any focal intra-abdominal, surgically
treatable source of infection
Etiology = patients’ w/cirrhosis and ascites
Pathophysiology = bacterial translocation from the intestinal lumen to mesenteric lymph nodes →
spread to systemic and portal circulation → colonisation and subsequent infection of ascitic fluid.
Usually a monomicrobial infection – G(-) species (E. coli, Klebsiella) are most common
Clinical manifestations = subtle/absent symptoms and signs – diffuse abdominal pain/tenderness,
fever and chills, worsening ascites, new-onset of worsening encephalopathy, N/V,
constipation/diarrhoea
Diagnosis
•
SBP is diagnosed when the ascitic fluid neutrophil count is ≥ 250/mm3, w/ or w/out +ve
ascitic fluid bacterial cultures, and in the absence of another intra-abdominal source of
infection.
•
Labs = 2 blood cultures; inflammatory markers may be ↑; possible leukocytosis
•
Diagnostic paracentesis w/peritoneal fluid analysis
Treatment = empiric anti-B therapy usually w/IV cefotaxime (2g/8hrs i.v) (3rd gen cephalosporin) for
community-acquired infection. Supportive therapy includes electrolyte repletion, analgesics, antipyretics, and IV fluids
3. Hepatorenal syndrome
Definition = deterioration of kidney function in patients w/advanced liver disease
Etiology and Pathophysiology = exact pathomechanisms are not completely understood;
cirrhosis/portal HT → ↑ splanchnic vasodilators (NO) → ↓ arterial blood flow → activation of RAAS →
renal VC → ↓ GFR
Risk factors = generally attributed to loss of volume – drainage of large-volume ascites, GI bleeding,
forced diuresis, excess use of laxatives, post TIPS procedure, SBP
Clinical manifestations = ranges from oliguria to anuria w/progressive kidney failure; hypotension and
wide pulse pressure; features of decompensated cirrhosis
Diagnosis = clinical diagnosis based on ↓GFR in patients’ w/cirrhosis and no other causes for renal
failure or no detection of renal pathologies on US.
Diagnostic criteria include:
•
Cirrhosis
•
Serum creatinine ≥ 0.3 mg/dL w/in 48 hours or ≥ 50% from baseline
•
Lack of improvement in renal function after volume expansion w/albumin and at least 48
hours w/out diuretics
•
Urinary output ≤ 0.5 ml/kg
•
Decreased urine sodium levels (< 10 mmol/L)
•
No proteinuria > 500 mg/dL, no microhematuria, no acute pathological findings in the kidney
US
•
No exposure to nephrotoxic drugs
•
Absence of shock
Treatment
•
General = improvement of liver function if possible (e.g. stop alcohol use, avoid nephrotoxic
drugs)
•
Meds = combo of midodrine + octreotide + albumin non-critically ill; combo of noradrenaline
+ albumin critically ill patients
•
Surgical/interventional = renal replacement therapy (dialysis); placement of TIPS; liver
transplant is the only curative option
4. Portal/hepatic encephalopathy
Definition = fluctuations in mental status and cognitive function in the presence of severe liver disease
Etiology and Pathophysiology
Cirrhosis → ↓ hepatic metabolism and portosystemic shunt → accumulation of neurotoxic
metabolites, especially ammonia → excess glutamine and swelling produced by astrocytes →
cerebral oedema and ↑ intracranial pressure → neurological deterioration
Precipitating factors = ↑ absorption/production of ammonia (infections, GI bleeding, constipation) and
↓ metabolism of ammonia (renal failure, portal v. thrombosis, portosystemic shunts, hypovolemia and
electrolyte disturbances)
Clinical manifestations
Symptoms are usually reversible. There are no specific symptoms; diagnosis is made based on
neuropsychiatric changes in the presence of liver disease.
•
Fatigue, lethargy, apathy
•
Altered levels of consciousness, ranging from mild confusion to stupor/coma
•
Mood changes; personality changes
•
Disoriented, irritability
•
Memory loss; impaired sleeping patterns
•
Slurred speech
•
Asterixis = brief, low frequency, rhythmless tremor of the hand that occurs when the arm is
outstretched, and the wrist is extended
Diagnosis
•
Bases on medical history and clinical presentation
•
Assessment of mental status = no. connection test (patients are timed while connecting no.’s
in order which are randomly distributed on paper), psychometry-based diagnostic method
(e.g. mini-mental state examination)
•
Lab studies = ↑ serum ammonia levels (supports the diagnosis)
Treatment
•
General = avoid and correct precipitating factors (stop meds & alcohol, hypovolemia,
electrolytes); treat complications that may further aggravate the encephalopathy
•
Meds =
o
o
1st line lactulose (improves encephalopathy by ↓ absorption of ammonia in the bowel
and leads to increased ammonium excretion in the feces),
rifaximin is a broad-spectrum, non-absorbable oral anti-B that ↓ the n.o of ammoniaproducing intestinal bacteria and may be added to lactulose to prevent recurrent
episodes of encephalopathy
102) Ascites – diagnosis, differential diagnosis, treatment
Definition = abnormal accumulation of fluid in the peritoneal cavity (at least 500 ml of fluid
accumulates – technically it is >25 ml of fluid in peritoneal cavity)
Etiology
The etiology can be determined by using the serum-ascites albumin gradient (SAAG) based on
Starling’s law – SAAG = (albumin levels in serum) – (albumin levels in ascitic fluid)
High SAAG ascites ≥1.1g/dl (“transudate”) = portal HT
•
Pre-sinusoidal = splenic/portal v. thrombosis;
schistosomiasis
•
Sinusoidal = cirrhosis (most common);
alcohol-related liver disease; liver
metastases
•
Post-sinusoidal = RHF, constrictive
pericarditis; Budd-Chiari syndrome
All these causes result in ↑ pressure in portal v. → ↑
hydrostatic pressure in the hepatic vessels →
pushing of fluid out from the intravascular space to
the peritoneal cavity
Low SAAG ascites <1.1g/dl (“exudate”)
•
Hypoalbuminaemia = nephrotic syndrome (→ primary renal sodium retention), severe
malnutrition, protein-losing enteropathy
•
Malignancy (e.g. ovarian, breast, lung, stomach, colon, oesophagus, pancreatic, liver)
•
Infections (e.g. TB) → production of protein-rich fluid from the tubercles
• Pancreatitis → accumulation of pancreatic fluid in the peritoneal cavity
All results in ↓ intravascular osmotic gradient → secondary influx of water from the intravascular
space to the peritoneal cavity.
Pathophysiology
•
Portal HT → VD → ↓ systemic vascular resistance and ↓ mean arterial BP; activation of
endogenous vasoconstrictors, renal sodium and water retention, and renal VC →
hyperdynamic circulation
•
RHF = backflow of blood obstructing the venous outflow of the liver
•
Budd-Chiari syndrome = congestion of the portal/hepatic collateral vv. and hypertrophy of the
caudate lobe of the liver → compression of the sinusoids and intrahepatic IVC
•
Malignancy = various mechanisms – peritoneal carcinomatosis → blockage of lymphatic
channels and ↑ vascular permeability → ascites; lymph obstruction (by a lymphoma) →
chylous ascites
Clinical manifestations
•
Progressive abdominal distention: associated symptoms include
o early satiety,
o weight gain,
o dyspnoea,
o diarrhoea if chronic includes features of malnutrition
•
Fluid wave test = wave produced by tapping one side of the abdomen in a patient in supine
position; this wave will be transmitted to the other side via ascitic fluid
•
Shifting dullness = change of resonance from dull to tympanic when patient changes from
supine to lat. decubitus position
•
Abdominal pain may be present
•
Abdominal wall hernias (e.g. umbilical, inguinal, or incisional) – due to ↑ intra-abdominal
pressure pushing onto weak areas of the abdominal wall
•
Peripheral/generalised oedema
•
Signs of underlying disease = chronic liver disease (hepatosplenomegaly, spider angioma,
palmar erythema); HF (↑ jugular venous pressure); upper abdominal malignancy (Virchow’s
node; weight loss)
Diagnosis
•
Imaging = US (best initial test); CT
•
Clinical picture
•
Labs =
o
o
o
•
Liver chemistries: Serum albumin for SAAG calculation. Hypoalbuminaemia
BMP: hypervolemic hypotonic hyponatremia due to overhydration despite normal/↑
Na+ conc
CBC/ Coagulation panel to determine cause
US-guided diagnostic paracentesis for ascitic fluid analysis
Colour = clear in “transudate”; in “exudate”: cloudy (infection/ malignancy), bloody
(trauma/ malignancy), milky (chylous ascites), or dark brown (GB perforation)
Cell count = ↓ cell count in “transudate”; ↑ cell count w/neutrophils > 250/μL (indicates
SBP infection) in “exudate”
Ascitic fluid albumin for SAAG calculation
Ascitic total protein conc. = ↑ protein levels in RHF, malignancy (peritoneal
carcinomatosis), pancreatitis, and TB; ↓ protein levels in cirrhosis and nephrotic
syndrome
o Differentiate SBP (typically ≤ 1 g/dL) vs secondary peritonitis (>1g/dL)
Ascitic fluid culture, gram stain, Acid fast bacilli smear (TB)
Treatment
•
Treatment of the underlying disease (e.g. using anti-coagulation in case of a thrombosis or
anti-TB drugs in case of tubercular peritonitis)
•
Sodium restriction: 2g; regular weight control; water restriction/avoiding overhydration
•
Diuretic therapy for portal HT ascites = spironolactone (100mg/day)
o Sp (100mg/day) + fursosemide (40mg/day) for recurrent/ massive ascites;
o Ensure regular control of K+ and creatinine during diuretic therapy
•
Emperic anti-B therapy for patients w/ GI bleeding in cirrhosis, SBP
•
Therapeutic paracentesis (w/ human albumin in large volume paracentesis >5L)
o Tense ascites
o Refractory ascites
o Malignancy related
o Contrindications to diuretic therapy
•
Shunt
o
o
•
Transjugular intrahepatic portosystemic shunt (TIPS) (if due to portal HT) in refractory
ascites.
Peritoneovenous shunt
Surgery: Liver transplant, hernia surgery
Complications = spontaneous bacterial peritonitis , hernias, hepatorenal syndrome, hepatic
encephalopathy (in large-volume paracentesis)
103) Cholelithiasis – etiology, pathogenesis, clinical features
Definition = presence of gallstones in the gallbladder. F>M; incidence >40 years. In contrast,
choledocholithiasis is the presence of stones in the common bile duct.
Types of stones = cholesterol (95%), bilirubin/black (<10%), mixed/brown (<10%)
Etiology/Risk factors
Cholesterol stones (95%)
•
↑ Level of cholesterol – familial hypercholesterolaemia, diabetes, hyperthyroidism,
treatment w/hormonal contraceptive and other causes of ↑ estrogen levels; impaired
cholesterol metabolism in the liver due to hereditary enz. deficiency, or consequence of
hepatitis and cirrhosis
•
Obesity and F sex – ↑ risk of gallstones
•
Pregnancy = ↑ oestrogen → ↑ secretion of lithogenic bile (rich in cholesterol) → cholesterol
gallstones. ↑ Progesterone → SM relaxation, ↓ and impaired gallbladder contraction, and
subsequent bile stasis and formation of gallstones
•
Age >40 years, European, Native American, Hispanic
•
Indirect bilirubin in the bile – haemolytic anaemia, Gilbert’s disease
•
↑ Ca2+ levels – hyperparathyroidism
•
Rapid weight loss ↓ lipids imbalance in bile composition ↑ risk of gallstone formation
•
Obstructed drainage of the gallbladder or bile ducts – dyskinesia, atonia, stenosis
•
Malabsorption – e.g. Crohn’s disease, ileal resection, CF
•
Chronic cholecystitis
•
Rule of 6 F’s = F, fat, forty, fertile, familial predisposition, fair-skinned
Black pigment stones (<10%)
•
Chronic hemolytic anemias (e.g., sickle cell disease, hereditary spherocytosis)
•
(Alcoholic) cirrhosis
•
Crohn disease
•
Total parenteral nutrition
•
Advanced age
Mixed/brown pigment stones
•
bacterial infections and parasites (e.g., Clonorchis sinensis, Opisthorchis species) in the
biliary tract, sclerosing cholangitis
Pathophysiology
The change in the composition of the bile is the main factor responsible for the formation of the
stones; it is due to changed ratio of its usual ingredients (↑ level of cholesterol and ↓ level of
phospholipids and bile acids) or appearance of substances alien to the bile (indirect bilirubin or Ca2+)
Besides a high conc. of cholesterol, 2 other factors are important in causing gallstones:
•
1st = how often and how well the gallbladder contracts; incomplete and infrequent emptying of
the gallbladder may cause the bile to become overconcentrated and contribute to gallstone
formation
•
2nd = presence of proteins in the liver and bile that either promote or inhibit cholesterol
crystallization into gallstones.
•
In addition, ↑ estrogen levels (pregnancy or hormonal contraception) may ↑ cholesterol levels
in bile and also ↓ gallbladder movement, resulting in gallstone formation
•
Summary of above: 3 factors contributing to gallstone formation = abnormalities in
composition of bile, stasis of bile and inflammation of gallbladder
Cholesterol stones = abnormal hepatic cholesterol metabolism → ↑ cholesterol conc. in bile and ↓
bile salts and lecithin → hypersaturated bile → precipitation of cholesterol and CaCO3 →
cholesterol/mixed stones
Bilirubin stones = ↑ hemolysis → ↑ in circulating unconjugated bilirubin → ↑ uptake and conjugation
of bilirubin → precipitation of bilirubin polymers and stone formation
Clinical manifestations
•
Most gallstones are asymptomatic
•
Biliary colic = constant, dull RUQ pain lasting <6 hours (caused by impaction of a
gallstone in the neck of the gallbladder)
Especially postprandial: vagal stimulation (e.g., CCK release following a fatty meal)
→ gallbladder contraction → attempts to force the stone into the cystic duct
May radiate to the epigastrium, R shoulder, and back (referred pain)
•
N/V, early satiety, bitter taste in the mouth; bloating, dyspepsia
3 clinical forms of Cholelithiasis:
1) Latent form = no symptoms; the stone is discovered accidentally by abdominal ultrasound or
on X-ray
2) Dyspeptic form = main symptoms are N/V, bitter taste in the mouth, heaviness/dull pain in the
R hypogastrium, which is usually provoked by fatty and fried foods, eggs, chocolate, coffee,
alcohol
3) Biliary colic (gallstone attack – when the stone is obstructing the cystic duct or common bile
duct)
Diagnosis
Labs = usually normal in uncomplicated cholelithiasis but should be ordered to rule out other acute
biliary conditions and/or other causes of acute abdominal pain
Imaging
•
RUQ US/ Biliary POCUS (best initial test) = cholelithiasis (intraluminal highly echogenic foci;
strong post. acoustic shadowing) and biliary sludge
•
MRI abd w/MRCP = well-defined hypointense (on T2) filling defect(s) w/inn the gallbladder
lumen. For suspected choledocholithiasis.
•
CT w/IV contrast: well-defined hyperdense structure(s) w/in the gallbladder lumen, detects
only radiopaque stones: black pigment stones (cholesterol: radiolucent)
Treatment
Treatment of biliary colic
•
Bowel rest = NPO (nil per os)
•
Analgesics = NSAIDs: Ibuprofen 400mg/8hrs (preferred 1st line);
o Servere pain: opioids (morphine) +/- spasmolytics (dicyclomine)
• In patients w/protracted vomiting consider = IV fluid, anti-emetics, NG tube insertion w/suction
Surgical management = elective laparoscopic cholecystectomy
•
Indicated for symptomatic cholelithiasis or asymptomatic that has ↑ risk of gallbladder cancer,
↑ risk of developing complications/becoming symptomatic
• Contraindicated in suspected gallbladder cancer
Non-surgical alternatives
•
For those who are unable to undergo surgery or unwilling
•
lifestyle modifications (low fat diet), avoid estrogen/ fibrates therapy,
•
Oral bile acid dissolution therapy (for cholesterol stones): Ursodeoxycholic acid 250mg/12hr,
•
Extracorporeal shock wave lithotripsy: non-invasive method to fragment solitary stone
Complications:
•
Cholecystitis: Acute cholecystitis (most common), Chronic cholecystitis, Porcelain GB
•
Choledocholithiasis
•
Acute cholangitis
•
Acute biliary pancreatitis
•
Biliary-enteric fistula: Cholecystoenteric/choledochoenteric fistula (rare), which can cause
gallstone ileus (rare)
104) Cholelithiasis – complications: cholecystitis, cholangitis
Cholecystitis
Definition = inflammation of the gallbladder (acute/chronic). F>M; most common complication of
Cholelithiasis; incidence >50 years
Etiology and pathophysiology
Acute calculous cholecystitis (most common)
•
Cause = obstructing cholelithiasis
•
Pathophysiology = Cholelithiasis → passage of gallstones into the cystic duct → cystic duct
obstruction → distention and inflammation of the gallbladder
•
Secondary bacterial infection may also be present (E. coli, Klebsiella, Enterobacter) but is not
necessary for development of cholecystitis
Acalculous cholecystitis (5-10% of acute cholecystitis)
•
It is an acute life-threatening necroinflammatory disorder of the gallbladder, usually seen in
critically ill patients, that is not associated w/gallstones
•
Cause = conditions predisposing to bile stasis and ↓ perfusion of the gallbladder
•
Risk factors = multiorgan failure, severe trauma/burns, surgery, infection, sepsis,
immunodeficiency
Chronic cholecystitis
•
Chronic irritation of gallbladder mucosa by Cholelithiasis
•
Recurrent attacks of acute cholecystitis
Clinical manifestations
Acute cholecystitis
•
RUQ pain – typically more severe and prolonged (>6 hours) than in biliary colic; postprandial;
radiation to the R scapula (due to referred pain from phrenic n. irritation)
•
Positive Murphy sign = sudden pausing during inspiration upon deep palpation of the RUQ
(R hypogastrium) due to pain. It may be falsely negative in patients >60yrs
•
Guarding
• Fever, malaise, anorexia; N/V
Chronic cholecystitis = recurrent symptoms like acute cholecystitis but typically less severe and
often self-limiting.
Diagnosis
Diagnostic criteria for acute cholecystitis
Local signs of inflammation
Murphy sign; RUQ pain, tenderness, or mass
Systemic signs of inflammation
Fever, ↑ CRP, leukocytosis
Imaging findings
Any finding characteristic of acute cholecystitis
Interpretation
•
Suspected diagnosis = ≥1 local + ≥1 systemic signs of inflammation
•
Definite diagnosis = all the above + any characteristic imaging finding
Imaging
•
RUQ transabdominal US = gallbladder wall thickening (>3-5 mm); gallbladder distention;
gallbladder wall oedema; presence of gallstones and/or biliary sludge
•
Hepatoiminidiacetic acid scintigraphy (HIDA scan) (preferred confirmatory test) = high
sensitivity and specificity; can differentiate between acute and chronic. Involves IV injection of
99mTc-HIDA → selective uptake by hepatocytes → subsequent excretion into bile → bile
w/radiotracer enters gallbladder if the cystic duct is patent → visualisation of tracer w/in the
gallbladder via a gamma camera. Normally the gallbladder should be visualised w/in 4 hours;
w/acute cholecystitis this is not the case.
• Abdominal MRI/CT w/contrast
Severity grading of acute cholecystitis
•
Grade I (mild acute) = no evidence of organ dysfunction or severe gallbladder disease
•
Grade II (moderate acute) = no evidence of organ dysfunction; presence of at least 1 sign of
severe gallbladder disease (palpable tender RUQ mass, signs of significant local inflammation
on imaging, ↑ WBC)
• Grade III (severe acute) = dysfunction of at least 1 organ system
Diagnosis of chronic cholecystitis
•
Lab studies may be normal
•
Abdominal US/CT w/IV contrast = thickened gallbladder wall (gallbladder may appear
small/shrunken due to fibrosis); cholelithiasis is commonly present
•
All patients should be evaluated for choledocholithiasis before treatment
Treatment
Initial medical management = empiric anti-B, NPO, IV fluid resuscitation, electrolyte repletion,
analgesics (preferably NSAIDs), anti-emetics, NG tube insertion as needed
Early Laparoscopic cholecystectomy
•
Gold standard of treatment for acute calculous cholecystitis
•
Early laparoscopic cholecystectomy = performed w/in 10 days of symptom onset, preferably
w/in the initial 24-72 hours. Indicated in symptom duration ≤10 days in patients w/low surgical
and anaesthesia risks.
•
Delayed/interval laparoscopic cholecystectomy = performed 45 days after resolution of
symptoms. Indicated in high surgical/anaesthesia risk and symptom duration >10 days.
Gallbladder drainage
•
Minimally invasive measures in high surgical risk patients not responding to conservative
treatment. Contraindicated in uncontrolled bleeding diathesis
•
Options include percutaneous cholecystostomy or endoscopic gallbladder stenting
Complications = Gangrenous cholecystitis, GB perforation; cholecystoenteric fistula (abnormal
communication between gallbladder lumen and lumen of adjacent bowel); porcelain gallbladder
(calcification of the gallbladder due to chronic inflammation); gallbladder cancer
Cholangitis (acute/ascending cholangitis)
Definition = inflammation of the bile duct, usually caused by ascending bacterial infection.
Etiology & Pathophysiology
Biliary tract obstruction → bile stasis w/↑ intraductal pressure → bacterial translocation into the bile
ducts → bacterial infection ascends the biliary tract (even into the hepatic ducts and possibly into
systemic circulation → bacteremia → sepsis). Causes include:
•
Choledocholithiasis (most common)
•
Biliary strictures = congenital, infectious (HIV), inflammatory (PSC), or iatrogenic
•
Malignant obstruction
•
Extrinsic compression
•
Parasitic infection
Contamination of bile w/intestinal contents
•
Manipulation of the biliary tract (e.g. papillotomy, stent placement, ERCP, liver transplant)
•
Biliary-enteric fistula
Clinical manifestations
•
Charcot cholangitis triad (25-70% of patients present w/all 3) = abdominal pain (RUQ), high
fever, jaundice (least common)
•
Reynolds pentad = Charcot cholangitis triad + hypotension and mental status changes
•
Features of sepsis, septic shock, and multiorgan dysfunction may be present, depending on
the severity of the disease
Diagnosis
Systemic signs of inflammation
Fever and/or chills w/rigors; labs = ↑ WBC and CRP
Systemic signs of cholestasis
Jaundice; LFTs = ↑ bilirubin, GGT, ALP, ALT
Imaging findings
Biliary dilatation; thickened bile duct walls; evidence of underlying
etiology
Interpretation
•
Suspected diagnosis = ≥1 sign of inflammation + ≥1 sign of cholestasis OR characteristic imaging
finding
•
Definite diagnosis = all 3 are needed – sign of inflammation + sign of cholestasis + imaging finding
Imaging =
•
RUQ US (dilated common bile duct, dilated intra-hepatic bile duct, thick BD walls)
o Underlying cause: Choledocholithiasis, Biliary strictures Biliary tumor
•
CT w/contrast; MRI w/contrast w/MRCP
Treatment
•
Initial medical management = identify and treat sepsis; empiric anti-B; NPO; IV fluid
resuscitation; electrolyte repletion; analgesics, anti-emetics, NG tube insertion as needed
•
Procedures = ERCP-guided transpapillary biliary drainage (preferred), endoscopic US guided
biliary drainage, percutaneous transhepatic biliary drainage (if can’t do US-guided).
•
These procedures relieve the intraductal pressures w/in the biliary tree, which aids biliary
drainage from the hepatocytes into the gallbladder and from the gallbladder into
the duodenum. Biliary drainage and decompression of the biliary tree ↓ the risk of progression
of disease severity.
105) Acute and chronic pancreatitis
Definition
•
Acute pancreatitis = acute/sudden inflammation of the pancreas
•
Chronic pancreatitis = progressive inflammation and irreversible damage to the structure
and function of the pancreas.
Etiology
Acute pancreatitis
•
Most common causes = biliary pancreatitis (40%) (gallstones, constriction of ampulla of
Vater), alcohol-induced (30%), and idiopathic (15-25%)
•
Other causes = post ERCP, certain drugs (steroids, diuretics, sulphonamides), viral infections,
trauma, autoimmune and rheumatological disorders (e.g. Sjogren syndrome), hereditary
•
MNEMONIC for most common causes = I GET SMASHED = Idiopathic, Gallstones, Ethanol,
Trauma, Steroids/Sulphonamides, Mumps, Autoimmune, Scorpion poison,
Hypercalcemia/Hypertriglyceridemia, post-ERCP, Drugs
Chronic pancreatitis
•
Chronic heavy alcohol use (60-70% of cases, especially M)
•
Idiopathic pancreatitis (20-30%)
•
Pancreatic ductal obstruction (<10%) = strictures (due to trauma, stones)
•
Hereditary pancreatitis (~1%) = PRSS1 gene mutation, SPINK1 gene mutation
•
Autoimmune pancreatitis
•
Systemic disease = CF, severe hypertriglyceridemia, hypercalcemia
Pathophysiology
Acute pancreatitis
•
Abnormal activation of pancreatic enz. w/in the pancreas (usually activated in the duodenum)
(trypsin is activated 1st) due to direct injury to pancreatic acinar cells or secondary to
pancreatic ductal outflow obstruction (gallstones)
•
↑ Proteolytic and lipolytic enz. activity → destruction of pancreatic parenchyma
•
Attraction of inflammatory cells (neutrophils, macs) → release of inflammatory cytokines →
pancreatic inflammation
Sequelae of pancreatitis (depending on the severity of pancreatitis)
•
Capillary leakage = release of inflammatory cytokines and vascular injury by pancreatic enz.
→ VD and ↑ vascular permeability → shift of fluid from the intravascular space into the
interstitial space (third space loss) → hypotension, tachycardia → distributive shock
•
Pancreatic necrosis = uncorrected hypotension and third space loss → ↓ organ perfusion →
multiorgan dysfunction (mainly renal) and pancreatic necrosis
•
Hypocalcaemia = lipase breaks down peripancreatic and mesenteric fat → release of free FAs
that bind Ca2+ → hypocalcaemia (fatty saponification)
•
In mild type there is inflammation and oedema of the pancreas; in severe type there is
necrosis of the pancreas
Chronic pancreatitis
•
Autodigestion and inflammation = damage to pancreatic acinar cells; outflow obstruction of
pancreatic enz. or premature activation of trypsin → intrapancreatic activation of digestive
enz. → autodigestion of pancreatic tissue → inflammatory rxn
•
Fibrosis = exposure to toxins and/or inflammatory mediators → activation of pancreatic
stellate cells
Clinical manifestations
Acute pancreatitis
•
Constant, severe epigastric pain = radiates towards the back; worse after meals and when
supine; improves when leaning forwards; N/V
•
General examination = signs of shock (tachycardia, hypotension, oliguria/anuria; possibly
jaundice in patients w/biliary pancreatitis
•
Abdominal exam = abdominal tenderness, distention, guarding; ileus (inability of intestinal
contents to pass through intestinal tract) w/↓ bowel sounds; ascites
•
Skin changes (rare) = Cullen’s sign (periumbilical ecchymosis and bluish-red discolouration);
Grey Turner sign (flank ecchymosis w/discolouration); Fox’s sign (ecchymosis over the
inguinal ligament)
Chronic pancreatitis
•
Epigastric abdominal pain (main symptom; in later stages ,patients may not experience any
pain) = radiates to the back, relieved on bending forward, exacerbated after eating; initially
episodic pain and becomes persistent as disease progresses; N/V
•
Features of pancreatic insufficiency (late manifestation, after 90% of parenchyma is
destroyed) = steatorrhoea (exocrine enz. deficiency) – cramping abdominal pain, bloating,
diarrhoea (can lead to vit A/D/E/K deficiency); malabsorption and weight loss; pancreatic
diabetes (endocrine hormone deficiency)
Diagnosis
Acute pancreatitis
•
Diagnosis = if 2 of the 3 – typical abdominal pain migrating to the back, 3X normal ↑ of
amylase and lipase, typical image on CT/MRI
•
Tests to confirm clinical diagnosis = ↑ serum pancreatic enz. – lipase ≥3X the upper reference
range, amylase (non-specific)
•
Tests to assess severity = ↑ Hct indicates third space fluid loss and inadequate fluid
resuscitation; ↑ WBC; ↑ BUN; ↑ CRP and procalcitonin levels; ↑ ALT
•
Tests to determine etiology = AP and bilirubin levels (gallstones); serum calcium levels; serum
triglyceride levels (fasting)
•
US (most useful initial test) = to detect gallstones and/or dilatation of biliary tract – indistinct
pancreatic margins (oedematous swelling), peripancreatic fluid build-up; evidence of necrosis,
abscesses, pancreatic pseudocysts
•
CT = enlargement of pancreatic parenchyma w/oedema; indistinct margins w/surrounding fat
stranding; necrotising pancreatitis; pancreatic abscesses
•
MRCP and ERCP = for suspected biliary or pancreatic duct obstructions
•
X-ray = sentinel loop sign (dilatation of a loop of SI in the upper abdomen)
Chronic pancreatitis
Labs
•
Serum pancreatic enz. levels = lipase (specific) and amylase (non-specific) are often normal
•
Pancreatic function tests (direct) = fecal elastase-1 activity – confirms that steatorrhoea is due
to pancreatic lipase insufficiency
•
Pancreatic function tests (indirect) = cholecystokinin test, secretin test, CCK-secretin
pancreatic function test
Imaging
•
Abdominal CT (best imaging modality) = pancreatic ductal dilations and calcifications on plain
CT; “chain of lakes” appearance of the main pancreatic duct; pancreatic atrophy
•
ERCP = ductal stones (visible as filling defects); “chain of lakes” appearance; irregularity
and/or dilation of the main pancreatic duct
•
MRCP = ductal strictures and dilations, pancreatic calcifications
•
Abdominal US = indistinct margins and enlargement; calcifications, stones, dilations, strictures
•
Endoscopic US = ductal dilation and calcification, parenchymal lobularity
Treatment
Acute pancreatitis
•
General = hospital admin and assess severity; fluid resuscitation (aggressive hydration
w/crystalloids – lactated Ringer’s solution, normal saline); analgesia (IV opioids); bowel rest
(nil-per-mouth – NPO) and IV fluids until pain subsides; total parenteral nutrition in patients
who can’t tolerate enteral feeds
•
Drugs = analgesics (fentanyl or hydromorphone); anti-B (only in patients w/evidence of
infected necrosis); fenofibrates (in hyperlipidemia-induced acute pancreatitis)
Surgery = urgent ERCP and sphincterotomy (w/in 24 hrs) in patients w/evidence of
choledocholithiasis and/or cholangitis; followed by cholecystectomy (in all patients w/biliary
pancreatitis)
Chronic pancreatitis
•
General = avoid alcohol and smoking; pancreatic enz. replacement; small, regular meals (rich
in carbs, low in fat); parenteral admin of fat-soluble vitamins if necessary; insulin
administration for endocrine insufficiency
•
Pain management = NSAIDs, opioids for severe pain, low-dose tricyclic antidepressants
•
Surgery (if pancreatic cancer is suspected or in those w/intractable pain) =
pancreaticojejunostomy (if main pancreatic duct is dilated – >5 mm); resection of the affected
part of the pancreas (distal pancreatectomy, Whipple procedure); thoracoscopic bilateral
splanchnicectomy (destroys afferent nn. of the pancreas)
Complications
Acute pancreatitis = bacterial superinfection of necrotic tissue → fever; pancreatic pseudocysts;
pancreatic abscess; sepsis, DIC, ARDs
Chronic pancreatitis = pancreatic insufficiency; pancreatic pseudocysts; splenic v. thrombosis;
pancreatic ascites; pancreatic abscess; pancreatic cancer
106) Cholestasis/jaundice
Review on bilirubin formation
•
Bile is the substance that gives bile its colour. It is formed from ageing RBCs
•
Hb is phagocytosed by macs → heme + globin.
•
Globin is degraded into AA and plays no role in jaundice
•
Heme → biliverdin (green) – catalysed by heme oxygenase
•
Biliverdin → bilirubin (yellow) (unconjugated, free, or indirect bilirubin) – catalysed by biliverdin
reductase
•
Unconjugated bilirubin travels to the liver through the bloodstream, bound to serum albumin
(since it is not soluble)
•
In the liver it is conjugated w/glucuronic acid to become > water soluble → conjugated bilirubin
– catalysed by UDP-glucuronyl transferase
•
This conjugated bilirubin is excreted from the liver into the biliary and cystic ducts as part of
bile.
•
Intestinal bacteria convert the bilirubin into urobilinogen.
•
From here urobilinogen can take two pathways. It can either be further converted into
stercobilinogen, which is then oxidized to stercobilin and passed out in the faeces, or it can be
reabsorbed by the intestinal cells, transported in the blood to the kidneys, and passed out in
the urine as the oxidised product urobilin.
•
Stercobilin and urobilin are the products responsible for the coloration of feces and urine,
respectively.
Definitions
Jaundice = a yellowish discolouration of the skin, sclerae, and mucous membranes due to the
deposition of bilirubin
Cholestasis = ↓ in bile flow
•
Non-obstructive intrahepatic = impaired bile formation/secretion
•
Obstructive intrahepatic = biliary obstruction w/in the liver
•
Obstructive extrahepatic/post-hepatic = obstruction of the biliary ducts between the liver and
the duodenum
Classification
•
Pre-hepatic/hemolytic = caused by anything that causes an ↑ rate of hemolysis (G6PD
deficiency, SCA, thalassemia)
•
Hepatic/hepatocellular = caused due to parenchymal
cells of liver (hepatitis, hepatotoxicity, cirrhosis)
•
Post-hepatic/cholestatic/obstructive = caused due to
obstruction of biliary passage (most common is
choledocholithiasis and cancer in the head of the
pancreas)
Etiology
Unconjugated hyperbilirubinaemia
•
↑ Hb breakdown (hemolysis; G6PD deficiency, SCA, blood transfusions; thalassemia,
pernicious anaemia; internal haemorrhage)
•
Impaired hepatic uptake of bilirubin = drugs (sulphonamides, rifampicin), portosystemic shunt
•
Defective conjugation of bilirubin = inherited hyperbilirubinaemia, liver disease (hepatitis,
cirrhosis), thyroid disease
Conjugated hyperbilirubinaemia
•
↓ Excretion/impaired reuptake of bilirubin = biliary atresia
•
Intrahepatic cholestasis = liver disease, biliary tract disorders (PBC), infiltrative disorders (TB,
sarcoidosis, amyloidosis), others (drugs, pregnancy)
•
Extrahepatic cholestasis (biliary obstruction) = biliary tract disorders (choledocholithiasis,
cholangitis), tumours (pancreatic cancer, hepatic tumours, bile duct carcinoma), inflammation
(PSC, PBC), infectious diseases (liver flukes, yellow fever)
Clinical manifestations
In addition to jaundice, the following signs may also indicate cholestasis:
•
Pale, clay-coloured (acholic) stool (if bile containing bilirubin can’t reach the colon due to
cholestasis → discoloured stools)
•
Darkening of urine (direct bilirubin is water-soluble. Excess in serum = excreted in urine =
dark urine)
•
Pruritus
•
Fat malabsorption (steatorrhoea, weight loss)
•
Abdominal pain
Diagnosis
LFTs
•
Parameters of cholestasis = ↑ AP, GGT,
and bilirubin
•
↑ Transaminases; AST/ALT ratio
•
Hepatitis serology, auto-AB
•
Hemolysis markers = ↑ LDH, ↑ indirect
bilirubin, ↓ haptoglobin
•
Albumin and PT/INR
• Inflammatory markers
Imaging
US = high specificity and sensitivity for differentiating between different forms of cholestasis.
•
Obstructive cholestasis findings
Extrahepatic obstruction = dilated common bile duct w/possible double-duct sign
Intrahepatic obstruction = double-barrel shotgun sign
Cause of biliary obstruction, if present (stones, tumours, cysts)
•
Non-obstructive cholestasis findings = no signs of bile duct dilation; US may provide evidence
of underlying disease
Other tests (if necessary) = ERCP, MRCP, CT
Pre-hepatic
Intra-hepatic
Extrahepatic
Stool colour
Dark
Pale, clay-coloured
Pale, clay-coloured
Indirect bilirubin
↑↑
↑
Normal
Direct bilirubin
Normal
↑
↑↑
Urinary bilirubin
Normal
↑
↑↑
Urinary urobilinogen
↑↑
Normal or ↑
↓
Urine colour
Normal
Dark urine
Very dark urine
Cholestatic enz.
Normal
↑
↑↑
Transaminases
Normal
↑
Normal
US
Normal-appearing bile ducts
Hepatomegaly in conditions
involving hemolysis
Dilated intra-hepatic
Dilated extrahepatic
bile ducts
bile duct
Double-barrel shotgun Double-duct sign
sign
Treatment = manage underlying condition
VII.Nephrology (Renal diseases)
107) Acute Post-streptococcal glomerulonephritis (GN)
Definition = acute, diffuse immune inflammation of both kidneys affecting the glomerular basement
membrane (GBM), the mesangium and the capillary endothelium. Affects mainly children 3-13yrs and
patients >60yrs age.
Etiology and pathophysiology
•
10-30 days post infection w/β-haemolytic streptococci group A. The usual sources of infection
are mouth, pharynx, and the skin (impetigo, erysipelas)
•
Formation of immune complexes of streptococci Ag and ABs which are deposited or formed in
situ on the GBM (hunch-like sub-epithelial depositions) and in the mesangium causing local
inflammation w/stasis and proliferation of endothelial and mesangial cells (hyperplasia) and
infiltration w/polymorphonuclear leukocytes and monocytes
•
It is a type III HS rxn (immune complex mediated)
Symptoms
•
Usually appear 10-14 days after initial infection. 50% asymptomatic.
•
Signs =
o
o
o
Phases:
Nephritic syndrome: hematuria (cola coloured urine), HT, oedema (around eyes/
generalized), oliguria (diuresis < 500 ml/24 hr),
Fever, headache, malaise, anorexia, nausea,
Flank pain
•
Initial phase = when symptoms start to appear – after 10-14 days
•
Oligo-anuric phase (lasts for a week) – oliguria or anuria (diuresis < 100 ml/24 hours) due to ↓
GFR. The consequences are:
Hypervolemia = causes oedema (due to water and Na retention and ↑ capillary
permeability) and arterial HT which is usually mild/moderate. Complications include
possible L HF w/cardiac asthma and pulmonary or cerebral oedema
Impaired clearance function and regulation of electrolytes and acid-base balance =
retention of N substances, hyperkalaemia, and metabolic acidosis (fatigue, exhaustion,
confusion, drowsiness)
•
Polyuric phase (lasts 7-10 days) = characterized w/polyuria and gradual disappearance of all
symptoms of the oligo-anuric phase; however the excessive polyuria may cause dehydration
and hypokalaemia, the latter may provoke cardiac arrhythmias
•
Recovery phase (lasts 3-6 months) = during which the changes in the urine (proteinuria,
hematuria) disappear completely and the GFR is normalized
Diagnosis
Lab tests
•
Urine analysis (specific for the diagnosis) =
o Nephritic sediment: hematuria + RBC casts; mild proteinuria (usually between 1 to 2
g/l/24hrs); usually high specific gravity.
•
Slightly ↑ WBC, ↑ sedimentation rate and CRP, possible presence of cryoglobulins
•
Oliguric phase = ↑ BUN, creatinine, urea, uric acid, K+; decompensated metabolic acidosis
•
In polyuric phase = K+ may be ↓
•
Blood = ↑ anti-streptolysin O (ASO), ↑ ADB titre, ↓ C3 complement
•
CBC: Normocytic, normochromic anemia
Instrumental tests
•
Abdominal ultrasound = kidneys are slightly enlarged w/diffuse structural changes
•
ECG and CXR are usually required and possible echocardiography; ophthalmoscopy, CT and
consultation w/neurologist are required in patients w/suspected cerebral oedema
•
Renal biopsy is performed only in prolonged and atypical cases for DDx
DDx
•
Causes of acute GN = IgA nephropathy, lupus nephritis, bacterial endocarditis, type 1
membranoproliferative GN
•
Nephrotic syndrome
•
Causes of generalised oedema = malnutrition, malabsorption, renal/liver failure, R HF
Treatment = Self-limiting,
•
Treatment for
o Oedema: low-sodium and low-protein diet, loop diuretics
o BP control – ACEi/ ARB’s, CCB, low-sodium diet
o Persisting infection: anti-B therapy w/ penicillin G benzathine
o
Severe course: glucocorticoids and temporary dialysis
Complications = Acute Renal failure, Rapidly progressive GN, Pulmonary and cerebral oedema;
uremic coma, Nephrotic syndrome
108) Idiopathic nephrotic syndrome
Definition = characterized by massive proteinuria (>3.5 g/day), hypoalbuminemia, edema and
hyperlipidaemia. Other symptoms include weight gain, fatigue, and foamy urine.
Etiology
Primary NS = usually described by their histology:
•
Minimal change disease (MCD) = most common cause in children
o Idiopathic, tumours (Hodgkin lymphoma), drugs and toxicity (NSAID, antibiotics,
interferon, mercury, lithium), infections (mononucleosis, HIV), vaccination, allergy
(insects, etc)
•
Focal segmental glomerulosclerosis (FSGS) = most common in adults
o
Primary/idiopathic; secondary = due to drugs (heroin), HIV, morbid obesity, congenital
heart disease (CMT), Sickle Cell Disease
•
Membranous GN
o Primary: anti-PLA2R antibodies
o Secondary: Infections (HBV, HCV, malaria, syphilis), Autoimmune diseases (e.g.,
SLE), Tumors (e.g., lung cancer, prostate cancer), Medications (e.g., NSAIDs,
penicillamine, gold)
•
Membranoproliferative GN
o
SLE, hepatitis C, monoclonal gammopathy; complement-mediated MPGN –dense
deposit disease and C3 GN
•
Rapidly progressive GN (RPGN) (usually presents as a nephritic syndrome) = glomeruli are
present in a crescent moon shape. It is characterised by a rapid ↓ in GFR by at least 50%
over a short period.
Secondary NS = due to changes caused by systemic disease (usually described by their underlying
cause):
•
Diabetic nephropathy, amyloidosis (Multiple Myeloma, Rheumatoid Arthritis), lupus, syphilis,
HBV, Sjogren’s syndrome, cancer, HIV
Pathophysiology
•
Structural damage of glomerular filtration barrier massive renal loss of protein reactively
increased hepatic protein synthesis
o Loss of negative charge of GBM loss of selectivity of barrier
o Podocyte damage and fusion non-selective proteinuria
•
If protein loss exceeds hepatic synthesis (loss of protein > 3.5 g/day)
hypoproteinemia/hypoalbuminemia
o Decreased serum albumin decreased colloid osmotic pressure edema
o Elevated lipoproteins to compensate the loss of albumin (due to reactive hepatic
protein synthesis) decreased cholesterol and TGs lipiduria (fat casts)
o Decreased levels of antithrombin III and loss of fluid into the extravascular space
(thickening of the blood) hypercoagulability
o Loss of IGs increased risk of infection
o Loss of transport proteins vitamin D deficiency, thyroxine deficiency
Symptoms
•
Massive proteinuria (>3.5 g/1.73 m2 body surface area/day)
•
Hypoalbuminaemia (<2.5 g/dl) → hypervolemia → oedema:
Typically starts with periorbital oedema (puffiness around the eyes), characteristically
in the morning (common)
Peripheral Pitting oedema over the legs
Pleural effusion (fluid in pleural cavity) Dyspnoea
Pericardial effusion
Ascites (fluid in peritoneal cavity) Dyspnoea by compressing diaphragm
Anasarca (generalised oedema throughout the body)
•
Hypocalcemia symptoms: tetany, paresthesia, muscle spasms
•
Hyperlipidaemia → ↑ risk for atherosclerosis. It is caused by 2 factors:
Hypoproteinaemia stimulates protein synthesis in the liver, resulting in the
overproduction of lipoproteins
Lipid catabolism is ↓ due to lower levels of lipoprotein lipase
•
Thrombophilia/hypercoagulability = greater predisposition for formation of blood clots that
is caused by a ↓ in antithrombin III levels in the blood due to its loss in urine → risk for DVT,
pulmonary emboli, renal v. thrombosis
•
Lipiduria = frothy urine
•
Loss of Ig’s = ↑ risk of infections
•
Symptoms of underlying disease (e.eg lupus = malar rash)
Diagnosis
•
Urinalysis =
o
o
o
•
dipstick (usually shows ≥ 3+ protein).
24-hr urine collection (>3.5 g/24h) / spot urine P/Cr ratio (>3.5g/g)
urine sediment – nephrotic sediment = proteinuria, lipiduria (fatty casts), renal tubular
epithelial cell casts
RBC casts indicate concomitant GN
Additional laboratory studies
o
o
o
o
o
o
o
CBC: ↑ Hb/Hct may indicate hemoconcentration, anemia
BMP: ↑ Cr and/or ↑ BUN may be seen; ↓ Na is commonly seen.
Serum protein: ↓ total protein, ↓ albumin (< 3 g/dL)
Coagulation factors: ↓ ATIII, ↓ protein S, ↓ plasminogen; ↑ fibrinogen, ↑ D-dimer
Lipid profile: Hyperlipidemia (↑ LDL, ↑ triglycerides) may be present.
Vitamin D levels: ↓ 25-OH Vit-D
Inflammatory markers: ↑ ESR, ↑ CRP may suggest underlying infection, inflammatory
condition, or vasculitis.
Imaging
•
Abdominal ultrasound = no changes in the minimal change disease; diffuse structural changes
in the other two forms; in patients w/focal segmental sclerosis and hyalinosis the size of the
kidneys may be ↓; ascites may be found in some cases
•
CXR (for hydrothorax) and echocardiography (for hydropericardium) are required in some
cases
Renal biopsy to confirm diagnosis or guide management.
•
MCD = structural defect of the podocytes
•
Focal segmental GN = damage to the podocytes; IgM and C3 inside sclerotic
•
lesions; segmental sclerosis and loss of podocytes
•
Membranous nephropathy = deposition of antibodies between podocytes and the basal
membrane; thickening of glomerular capillary loops and basal membrane; subepithelial dense
deposits
•
Membranoproliferative GN = immune-mediated proliferation of the mesangium; IgG deposits
on BM
Treatment
•
General measures: low-sodium and low-protein diet, weight loss; ACEI or ARBs;
diuretics to reduce edema; treat hypercholesterolemia w/ statins, LMWH anti-coag.
o Minimal change disease = patients usually respond well to at least 12 weeks of
glucocorticoids (prednisone) - 60 mg/m2 for 4-8 wks, reduced to 40 for 4wks.
o
o
o
Focal segmental glomerulosclerosis = glucocorticoids; cyclosporine or tacrolimus in
steroid-resistant patients
Membranous nephropathy = glucocorticoids + cyclosporine/tacrolimus or
cyclophosphamide
Membranoproliferative GN = glucocorticoids, cytotoxic agents and calcineurin
inhibitors
•
Immunosuppressors (cyclophosphamide) = only indicated in recurring nephrotic syndrome in
corticosteroid dependent or intolerant people. Proteinuria must not be present if treatment is
to begin. Treatment is for 8 wks at a dose of 3 mg/kg/day. Patient can’t be suffering from
neutropenia or anaemia, which would cause further complications
•
Treat underlying disease
Complications: thrombotic complications (DVT, PE, renal vein thrombosis); atherosclerotic
complications (MI, stroke); CKD and end-stage renal disease (in FSGS and MN)
109) Membranous glomerulonephritis
It is the 2nd most common cause of nephrotic syndrome in adults. The inflammation of the BM causes
↑ leaking in the kidneys
Etiology
•
Primary/idiopathic = 85% are idiopathic
•
Secondary = remainder are due to autoimmune conditions (SLE), infections (syphilis, hep
B/C), drugs (captopril, NSAIDs), inorganic salts, or tumours
Pathogenesis
•
Caused by immune complex formation in the glomerulus
•
This triggers a response from the C5b-C9 complements which forms a MAC on the glomerular
epithelial cells
•
Stimulates release of proteases and oxidants damaging the capillary walls and causing them
to be “leaky”
Symptoms
Some people present as nephrotic syndrome w/proteinuria, oedema w/ or w/out kidney failure. Others
may be asymptomatic and may be picked up on screening or urinalysis. Definitive diagnosis requires
a kidney biopsy
Diagnosis
The presence of subepithelial deposits of anti-B between the podocytes and GBM
•
EM: subepithelial dense deposits (IgG and C3) with a spike and dome appearance
•
LM: diffuse thickening of glomerular capillary loops and basal membrane
•
IM: granular subepithelial deposits of immune complexes and complement
Treatment
•
For secondary membranous nephropathy treat underlying disease.
•
For treatment of idiopathic membranous nephropathy, the treatment options include
o RAAS inhibitors: ACEi, ARB, Direct renin inhibitors
o Severe/ refractory disease: Immunosuppressive drugs: cyclophosphamide AND
corticosteroid (prednisone)
Alternatives: cyclosporine, tacrolimus, rituximab
o Edema
Dietary sodium restriction <3g/day
Fluid restriction <1.5l/day
Diuretic: furosemide
o
o
Proteinuria: Antiproteinuric therapy (avoid in AKI, hyperkalemia, acute nephrotic s)
ACEi/ ARB
Avoid very high protein diet
Dyslipidaemia
o
Atorvastatin: 10mg/day
Hypercoagulability (Anticoagulants)
LMWH: Enoxaparin 40mg/day
110) IgA glomerulonephritis
Definition (AKA IgA nephropathy/Berger’s disease) = a primary GN characterised by the deposition of
IgA complexes in the glomerular mesangium
Etiology and pathogenesis
•
Exact cause is unknown. It is believed that it is an autoimmune condition
•
Galactose deficient IgA may act as auto-Ag’s that trigger production of glycan-specific autoAB and formation of circulating immune complexes that are deposited in the renal mesangium
•
These then induce glomerular injury through pro-inflammatory cytokine release, chemokine
secretion, and the resultant migration of macrophages into the kidney
Symptoms
•
40-50% of patients = episodic hematuria, which usually starts w/in a day/2 of a non-specific
URT infection. It may be accompanied by loin pain. The macroscopic hematuria may resolve
after a few days, though microscopic hematuria will persist.
•
30-40% of patients = asymptomatic w/RBC casts and proteinuria (< 2g/day) discovered on
urinalysis
•
Patients can also present w/acute or chronic (anaemia, HT) kidney failure
A variety of systemic diseases are associated w/aggressive IgA nephropathy such as liver failure,
cancer, coeliac disease, SLE, RA, HF, AS, and HIV
Diagnosis
•
Isolated hematuria = kidney ultrasound and cystoscopy to pinpoint source of bleeding (rule out
kidney stones and bladder cancer).
•
Renal biopsy is necessary to confirm diagnosis = proliferation of the mesangium w/IgA
deposits on immunofluorescence and EM
•
Urinalysis
Treatment
•
ACEIs to ↓ BP and proteinuria. ARBs for patients who can’t tolerate ACEIs
•
Prednisone for 4-6 months to patients who have IgA nephropathy w/preserved renal function,
nephrotic syndrome, and minimal change findings on light microscopy
111) Membranoproliferative glomerulonephritis (MPGN)
Definition = a type of GN caused by deposits in the glomerular mesangium and BM thickening,
activating complement and damaging the glomeruli
It shouldn’t be confused w/membranous GN in which the BM is thickened but the mesangium is not
Etiology and pathophysiology
It may be idiopathic or secondary in etiology (hep C is most common). Idiopathic types are subdivided
into 3 types based on ultrastructural appearance.
•
Type I = most common type, characterised by subendothelial and mesangial immune
deposits. It is believed to be associated w/the classical complement pathway
•
Type II = characterised by dense deposits in the BM. Most cases are associated
w/dysregulation of the alternative complement pathway
•
Type III = characterised by a mixture of subepithelial and subendothelial immune and/or
complement deposits
Membranoproliferative GN involves deposits at the intraglomerular mesangium which leads to
“splitting” of the GBM – Tram track appearance
Symptoms = proteinuria, hematuria, azotemia (high N levels in blood), oliguria, oedema, anaemia and
pallor
Diagnosis
•
Hypocomplementemia is a characteristic finding w/all types of MPGN. It results from ↑
breakdown and ↓ synthesis of C3. The ↓ C3 synthesis is likely caused by the -ve feedback by
C3 breakdown products
•
The GBM is rebuilt on top of the deposits, causing a “tram tracking” appearance under the
microscope. Mesangial cellularity is ↑
Treatment
•
Supportive
o Dietary sodium restriction <3.5g/day
o Fluid restriction <1.5l/day
•
Medical
o
o
o
o
•
RAAS inhibitors
Proteinuria and/or HT: ACEi/ ARB
Severe HT and/or Edema: Diueretics
Prednisone alone or in combination w/ Cyclosporine or Tacrolimus
Severe renal insufficiency/ kidney failure: Hemodialysis, Kidney transplant
112) Lupus nephritis
Definition = inflammation of the kidneys caused by SLE.
Etiology and pathophysiology
SLE is presumably caused by a genetic susceptibility coupled w/an environmental trigger which
results in defects in the immune system. Autoantibodies direct themselves against nuclear elements.
One of the factors associated with SLE is vit D deficiency
The characteristics of lupus nephritis are Ag specificity directed at nucleosome, high affinity auto-AB’s
form intravascular immune complexes, and auto-AB’s of certain isotypes activate complement.
Clinical findings
•
Clinical manifestations depend on the site of immune complex-mediated injury. Immune
complexes defined to the mesangium cause < inflammation than subendothelial immune
complexes, which have greater exposure to inflammatory cells and mediators in the blood
•
Symptoms include:
o hematuria
o hypertension
o edema
o Polyuria, dark foamy urine,
o Fever, joint and muscle pain
o Malar (butterfly) rash
Classification
•
Class I (minimal mesangial GN) = normal appearance under light microscope, but
mesangial deposits (of immune complexes) are visible under EM – very uncommon
•
Class II (mesangial proliferative GN) = mesangial hypercellularity (cell proliferation) and
matrix expansion. Microscopic hematuria w/ or w/out proteinuria may be seen
•
Class III (focal GN) = sclerotic lesions involving <50% of the glomeruli, which can be
segmental/global, and active/chronic, w/endocapillary or extracapillary proliferative lesions.
Subendothelial deposits can be seen on EM, and some mesangial changes may be present.
Hematuria + proteinuria , w/ or w/out nephrotic syndrome, HT, and ↑ creatinine
•
Class IV (diffuse proliferative nephritis) = most severe and most common subtype. >50%
of the glomeruli are involved w/same detail as above. Subendothelial immune complex
deposits may create a circumferential thickening of the capillary wall, forming “wire-loop”
structures on light microscopy. Hematuria + proteinuria, nephrotic syndrome, HT,
hypocomplementemia, ↑ anti-dsDNA titres and ↑ creatinine
•
Class V (membranous GN) = diffuse thickening of the glomerular capillary wall
(segmental/global) w/diffuse membrane thickening, and subendothelial deposits. Nephrotic
syndrome, microscopic hematuria, HT, and possible thrombotic complications
•
Class VI (advanced sclerosing lupus nephritis) = sclerosis of >90% of the glomeruli, and
represents end stage renal disease
Diagnosis
•
Urinalysis = nephritic picture – RBC casts, RBC, and proteinuria
•
Blood tests: BMP: ↑ creatinine
•
+ve staining for IgG, A, and M w/C1q, C3 and C4
•
Spot urine protein:creatinine ratio: proteinuria ≥ 0.5 g/g
•
X-rays, ultrasound
•
Kidney biopsy
Treatment
•
People w/class I/II usually require no treatment
•
Class III/IV: Induction and maintenance therapy
o Induction therapy
IV glucocorticoids (e.g., methylprednisolone)
PLUS, other immunosuppressants (e.g., mycophenolate or cyclophosphamide)
o Maintenance of remission
Oral prednisone
PLUS, mycophenolate OR azathioprine
o
Refractory or relapsing disease: Rituximab may be considered
113) Kidney and diabetes
Diabetic nephropathy (AKA diabetic kidney disease) – definition = the chronic loss of kidney function
occurring in those w/DM.
Pathophysiology
•
The kidney may be damaged by diabetes in 3 ways: glomerular damage, ischaemia resulting
from hypertrophy of afferent and efferent arterioles, and ascending infection
•
The earliest functional abnormality in the diabetic kidney is renal hypertrophy associated w/a ↑
GFR. This appears soon after diagnosis and is related to poor glycaemic control.
•
As the kidney becomes damaged by diabetes, the afferent arteriole becomes vasodilated to a
greater extent than the efferent glomerular arteriole → ↑ intraglomerular filtration pressure →
further damage to the glomerular capillaries.
•
This raised intraglomerular pressure also leads to ↑ local shearing forces, which are thought
to contribute to mesangial cell hypertrophy and ↑ secretion of extracellular mesangial matrix
material. This process eventually leads to glomerular sclerosis.
•
In nodular glomerulosclerosis (AKA Kimmelstiel-Wilson syndrome) there is nodular deposition
of hyaline in the mesangial portion of the glomerulus. As the sclerotic process progresses,
there is complete obliteration of the glomerulus, w/impairment of renal function
•
The initial structural lesion in the glomerulus is thickening of the BM. Associated changes
result in disruption of the protein cross-linkages that normally make the membrane an
effective filter. In consequence, there is a progressive leak of large molecules (particularly
protein) into the urine.
Risk factors
The incidence of diabetic nephropathy is higher in diabetic people w/1/> of the following conditions:
•
Poor control of blood glucose
•
Uncontrolled HT
•
DM 1, w/onset before age 20
•
Past or current cigarette use
•
Family history
Clinical manifestations
•
Microalbuminuria (1st sign) → oedema → nephrotic syndrome
•
Nocturia (frequent urination at night, foamy urine
•
Hypertension
•
Uremia (pruritus, N/V, pericarditis, pleuritis, paraesthesia’s, encephalopathy [seizures, coma])
•
Fatigue, headaches, malaise, N/V, lack of appetite, itching
Diagnosis
•
Microalbuminuria = urinary albumin excretion in the range of 30-300 mg/day
•
To stage the degree of damage in kidney disease, serum creatinine is determined and used to
calculate the estimated GFR (eGFR). Normal eGFR is ≥ 90 ml/min/1.73 m2
•
US – recommended for DDx if there is suspicion of UT obstruction, UTI, kidney stones, or
PKD
Treatment
•
BP control w/ACEIs/ARBs then add diuretics/CCBs– usually reduce proteinuria levels
•
Strict control of blood glucose
•
↓ dietary salt intake <5-6g/day, stop smoking
•
↓ protein restriction
•
↓ phosphorous and K+ intake in advanced nephropathy
Complications = end stage kidney disease (ESKD)
114) Renal Amyloidosis
Definition: Disease characterized by extracellular deposits of fibrillar amyloid protein leading to
Nephrotic syndrome. Commonly seen in elderly patients
Systemic amyloidosis – kidneys are most commonly affected, Liver – hepatomegaly, heart →
restrictive cardiomyopathy, conduction abnormalities, peripheral nerves, carpal tunnel, upper
pharynx, macroglossia
Etiology
•
1°/ Systemic Amyloidosis - Immunoglobulin light chains – AL Amyloid (80%)
o Plasma cell dyscrasia - Multiple myeloma (w/lytic bone lesions, plasma cell infiltration
of bone marrow), MGUS, Waldenstroms, macroglubulinemia
•
2° - Chronic inflammatory disease – AA Amyloid (serum Amyloid A prot. fragments, 3%)
o Chronic infectious diseases – TB, osteomyelitis, leprosy
o Chronic inflammatory diseases - Rheumatoid arthritis (40%), Ankylosing spondylitis,
psoriatic arthritis, SLE, Crohn’s, IBD
o Usually without renal involvement o Familial Mediterranean fever (FMF) ( Jews, Iraqi) → neuropathic,
o aging → cardiac; chronic dialysis → arthropathy
Pathogenesis
Extracellular amyloid deposits → pressure atrophy → organ dysfunction vessels, mesangium,
glomerular tuft, capillary walls, interstitium → sclerotic glomeruli.
Kidney large, pale with smooth even surface.
•
1° - Ig light chains (λ) are converted to amyloid fragments by macrophages
• 2° - deposition of β pleated serum amyloid protein
FMF - mutant transthyretin; aging - transthyretin; chronic dialysis - β2 microglobulin → Nephrotic
syndrome → Heavy proteinuria [40 – 60% end up on dialysis]
Sometimes associated with renal vein thrombosis
Clinical Presentation
•
Nephrotic syndrome = Proteinuria >3.5g/24hr, hypoalbuminemia, hyperlipidemia, lipiduria
•
Edema – periorbital, pleural, pericardial, generalized pitting edema => Anasarca
•
↓ immunity, Hypercoagulable state,
•
Renal insufficiency, HTN, Hemorrhagic diathesis
Diagnosis
•
Urine dipstick – protein 3+, 24 hr Urine > 3.5g/24hr
o
Immunoelectrophoresis: Serum – Ig light chains
o
•
urine – Bence Jones protein (light chains)
Biopsy – kidney or liver
o LM
Mesangial proliferation, H&E - Eosinophillic
o
o
Capillary wall thickening – wire loops
Apple green birefringence with Congo red stain under polarized light
Nodular glomerular sclerosis
IF - Ig deposits – subendothelial and subepithelial
EM – amyloid fibrils – small non branching randomly arranged, criss-cross patte
•
Biopsy - Abdominal fat pad aspirates (70% sensitivity), liver, bone marrow
•
Renal US - enlarged kidneys
•
SAP scan – nuclear imaging with I123 and Serum Amyloid P (SAP)
•
Serum Free light chain Nephelometry assay – early diagnosis and F/U
•
Labs findings of Nephrotic Syn, renal function test - ↑ S Cr, ↑ BUN etc.
DDx
•
(Differentials of Nephrotic syndrome and edema)
•
Congestive heart failure - ↑ JVP, pulm. Edema
•
Liver pathology – hypoalbuminemia
Treatment
No specific treatment, only delay progression of disease
Goals of treatment: Blood pressure control and symptomatic treatment of Nephrotic syndrome, treat
underlying condition
•
Edema
o Diet – salt and water restriction
o Diuretics – first line – Furosemide 40mg BDS, second line – thiazide diuretics
o +/- i.v. Albumin 20% 0.5g/Kg
•
Proteinuria
o
o
o
ACEi/ARB (avoid in pts with AKI, ↑K+ or abrupt onset of Nephrotic syn)
Thiazide diuretic 25 mg/day HCT, MRA – 25mg/day Spironolactone
Diet – adequate protein intake
•
Dyslipidemia Statins – Atorvastatin 10-80mg/day
•
Hypercoagulability
o
o
LMWH Enoxaparin 40mg/day
Warfarin – INR 2 – 3
• Vitamin D supplements, ABx for infections etc.
Specific
•
1° Amyloidosis – treat plasma cell dyscrasia
o
Melphalan (alkylating agent), Doxorubicin
Corticosteroids
Autologous hematopoietic Stem Cell transplant
•
2° Amyloidosis – control underlying condition
o Familial Med Fever – Colchicine (prevention of AA amyloid deposits and consequent
renal disease)
•
Dialysis - has poor outcome as difficult vascular access
•
Drugs disrupting formation of fibrils in R&D
Prognosis
40 – 60% of patients will end up on Dialysis. Systemic Amyloid - worse prognosis
Complications
•
CRF, Nephrotic syndrome – severe hypoproteinemia, Hypercoagulability and risk of
thromboembolic events, ↓ immunity, Vit D deficiency
•
Shy-Dregger Syndrome - severe hypotension if sympathetic ganglia are involved
•
Hemorrhagic diathesis
115) Acute urinary tract infections (UTIs)
Definition = UTI is the presence of bacteria/other MOs in the urine or genitourinary tissues, which are
normally sterile.
Classification
•
UTIs are usually referred to as simple (uncomplicated), recurrent, or complicated
•
Uncomplicated occur in patients w/out any physiological or anatomic abnormalities of the UT
and w/out obstruction of the UT
•
Recurrent UTIs are ≥3 infections in 1 year or ≥2 infections in 6 months
•
Complicated UTIs are caused by anatomic abnormalities or functional disorders of the UT (in
patients w/predisposing factors)
•
Lower UT infection = bladder infection (cystitis)
•
Upper UT infection = kidney infection (pyelonephritis) – considered > serious due to their
ability to cause renal damage
•
Super. infection = cystitis; deep tissue infection = prostatitis and pyelonephritis
Etiology
•
Most UTIs (community acquired) are caused by G- aerobic bacteria – 80-85% E. coli, 5-10%
caused by P. mirabilis and Klebsiella. S. saprophyticus (G+) contributes to 10-15% of cases.
Other species include Enterobacter, U. urealyticum, Serratia, P. aeruginosa, Citrobacter
•
Healthcare associated UTIs involve a broader range of pathogens including E. coli, Klebsiella,
Pseudomonas, C. albicans, Enterococcus, among others
Predisposition factors
•
Urinary flow obstruction which prevents bladder emptying and/or result in urinary stasis – e.g.
BPH, congenital malformations → vesicoureteral reflux, urinary bladder diverticulum,
neurogenic bladder, nephrolithiasis
•
Sex = F > likely to have UTI due to shorter urethra which is also in close proximity to the anal
and genital regions → bacteria spread from anal region which colonises the vagina →
ascending UTI. Also a higher risk in uncircumcised M
•
Pregnancy = hormonal changes → vesicoureteral reflux → ↑ risk of UTI
•
Postmenopause = ↓ estrogen → ↓ vaginal lactobacilli (protective vaginal flora) → ↑ vaginal pH
→ ↑ colonisation by E. coli
•
Prior conditions = previous UTIs, history of kidney surgery, immunosuppression, DM
•
Catheter-associated UTIs = caused by indwelling urinary catheters – most common cause of
nosocomial UTIs
•
Spermicide use ↑ risk. Diaphragm use is also associated.
Pathogenesis
•
Bacteria causing UTIs typically enter the bladder via the urethra. However, infection may also
occur via the blood (20%) or lymph
•
Infection is facilitated by host conditions that disrupt washout of the agent from the UT through
urine flow, change the protective properties of the mucin lining of the UT, disrupt the
protective function of the normal bacterial flora, or impair the function of the immune system
•
Virulence of the agent is derived from its ability to gain access to and thrive in the UT
environment, adhere to the tissues of the lower/upper UT, evade the destructive effects of the
host’s immune system, and develop resistance to antimicrobial agents
Clinical manifestations
Acute uncomplicated cystitis (lower UT)
•
Dysuria (burning w/urination; burning/painful voiding of small volumes of urine)
•
Having to urinate frequently (urge to urinate)
•
Hesitancy – sensation of not being able to urinate easily/completely
•
Suprapubic or lower abdominal pain
•
Cloudy, foul smelling, or bloody urine in 30% of patients
•
On examination, fever and costovertebral angle tenderness (CVAT) (succusio renalis) are
generally absent
Acute pyelonephritis (upper UT)
•
Fever, chills
•
Fatigue
•
Flank pain
•
Nausea + vomiting (N/V)
•
Symptoms of lower UTI may be present but are not obligatory
•
On examination, fever and CVAT (+ve succusio renalis) are present
Diagnosis
•
Urine specimen = clean-catch midstream sample – necessary to avoid contamination
w/vaginal or skin flora
•
Urine culture = +ve if it shows a bacterial colony count of ≥ 103 CFU/mL of a typical UT
organism.
•
Urinalysis = bacteruria, leukocyturia, erythrocyturia, nitrites (E. coli), proteinuria (usually <1-2
g/day). Hematuria may be present up to 30%
•
↑ CRP and ESR; leucocytosis w/ or w/out neutrophilia
•
US, CT – used to identify contributing factors, such as obstruction
Treatment
•
Uncomplicated UTIs = trimethoprim/sulfamethoxazole (TMP/SMX) (3 days), nitrofurantoin (5-7
days), or Fosfomycin (single dose) are typically 1st line. Cephalosporins, amoxicillin/clavulanic
acid, or a fluoroquinolone may also be used, though the latter is discouraged due to ↑
resistance and serious side effect
•
Pyelonephritis = longer course or oral anti-B or IV anti-B. Ciprofloxacin for 7 days in areas
where the resistance rate is 10%; IV ceftriaxone if it is >10%. TMP/SMX or
amoxicillin/clavulanate orally for 14 days is another reasonable option
116) Chronic pyelonephritis
Pyelonephritis = infection of the renal pelvis and parenchyma that is usually associated w/an
ascending bacterial infection of the bladder.
Risk factors include F sex, pregnancy, UT obstruction (FB’s or anatomic abnormalities),
immunosuppression, and acute kidney injury.
Chronic pyelonephritis – definition = a consequence of recurrent/persistent acute pyelonephritis. It is
a complex renal disorder characterised by chronic tubulointerstitial inflammation, tubular atrophy
(w/irreversible damage to the tubules), deep segmental cortical renal scarring and clubbing of the
pelvic calyces as the papillae retract into scars.
Predisposition factors = vesicoureteral reflex (VUR), UT obstruction (kidney stones, neurogenic
bladder)
Etiology and pathogenesis = reflux of infected urine into the renal pelvis
Clinical manifestations
•
Non-specific = mild fever, anorexia, malaise, weight loss
•
Persistent abdominal/flank pain
•
Lower UT symptoms = polyuria, ↑ urgency, hesitancy, nocturia, poor stream, incomplete
voiding
•
Hematuria
Diagnosis
•
Urinalysis = pyuria, proteinuria, WBC casts
•
Urine culture
•
Imaging = US, helical CT, IV Urogram. Hallmark finding is a large, deep, segmental, coarse
cortical scar usually extending to 1/> of the renal calyces. On US there is irregular contour of
the kidneys.
o Corticomedullary scarring of mainly the upper pole and clubbing of the renal calyces
Treatment
•
Treat the underlying cause
•
Long term anti-B – TMX, nitrofurantoin
•
Nephrectomy, kidney transplant
Complications = CKD, ESRD
Xanthogranulomatous pyelonephritis
•
An unusual form of chronic pyelonephritis characterised by granulomatous abscess formation,
severe kidney destruction, and a clinical picture that may resemble renal cell carcinoma and
other inflammatory kidney parenchymal diseases
•
Most present w/recurrent fevers, urosepsis, anaemia, painful kidney mass, kidney stones, and
loss of function of the affected kidney
•
Bacterial cultures are almost always +ve
•
Microscopically = granulomas and lipid-laden macs. It is found in roughly 20% of specimens
from surgically managed cases of pyelonephritis
117) Renal tuberculosis
Definition = a subset of genitourinary TB, accounts for 15-20% of extra-pulmonary TB and can result
in varied and striking radiographic appearances.
Etiology and pathogenesis
•
Caused by M. TB
•
Renal involvement in TB can be part of a
disseminated (hematogenous) infection or a
localised genitourinary disease
•
Renal infection results from haematogenous
spread at the time of primary infection,
w/multiple micro-abscesses developing at the
site of periglomerular capillary seeding.
Normal host immunity is usually able to
dampen the disease with the usual
development of a small inactive granuloma.
•
Usually there is a long latency between primary infection and presentation which in most case
occurs due to host immunity becoming compromised. These quiescent granulomas then can
reactivate, grow and eventually communicate with the calyces, leading to downstream
infection.
•
Ureters and bladder are infected when bacteria are excreted in urine
Clinical manifestations
•
Constitutional symptoms = weight loss, fever, chills, night sweats, fatigue, malaise
•
Flank pain
•
Hematuria
•
Storage symptoms = ↑ frequency of voiding, nocturia, urgency. Infection of the bladder wall
leads to granuloma formation and fibrosis, ↓ bladder capacity and, consequently, resulting in
these symptoms.
•
HT
•
Recurrent UTIs unresponsive to anti-B therapy
Diagnosis
•
Urine examination (due to low bacillary load, 5 early morning midstream urine samples should
be collected) = urinalysis (hematuria, sterile pyuria, proteinuria) and microbiology (acid-fast
staining, PCR, and culture)
•
Imaging (CT/IV urography) = renal scarring, hydroureteronephrosis, calcification involving the
entire UT, multiple ureteral structures, bladder wall thickening and fibrosis.
•
Cystoscopy = ulceration, granuloma, fibrosis
Treatment
•
Standard anti-B therapy for TB (see Pulmonology notes): RIPE
•
Ureteral stenting for strictures
•
Surgery = total/partial nephrectomy (indicated for recurrent secondary bacterial infections,
severe HT, and extensive disease w/non-functioning kidneys); bladder augmentation
118) Nephrolithiasis
Nephrolithiasis (AKA renal calculi/kidney stones) – definition = formation of stones in the kidney,
which may deposit along the entire urogenital tract from the renal pelvis to the urethra.
Classification of stones
Kidney
stone type
Calcium
oxalate
Incidence
80%
Circumstances
When urine is acidic
Colour
Black/dark
brown
Description
Some of the oxalate in the urine is
produced by the body. Ca and
oxalate in the diet play a role in stone
formation. Ca from bone may also
play a role in stone formation
Uric acid
5 – 10 %
When urine is
persistently acidic
Yellow/reddish
brown
Diets rich in animal proteins and
purines = organ meats, fish and
shellfish
Calcium
phosphate
5 – 10 %
When urine is
alkaline
Dirty white
Tends to grow in alkaline urine,
especially when proteus bacteria are
present
Struvite
10 – 15 %
Infections in the
kidney
Dirty white
Diet hasn’t been shown to affect
struvite stone formation
Cysteine
1–2%
Rare genetic
disorder
Pink/yellow
Cysteine leaks through the kidneys
and into the urine to form crystals
Extremely rare
Brick red
Xanthine
Predisposition factors
•
Dehydration = ↓ water intake, climate, professional environment
•
Obesity
•
High dietary intake of animal protein, sodium, sugars including honey, refined sugars, fructose
and high fructose corn syrup, oxalate, grapefruit juice and apple juice
•
Crohn’s disease = associated w/hyperoxaluria and malabsorption of Mg
•
Metabolic disorders = hyperuricemia and hyperuricosuria; hyperoxaluria; cysteinuria
•
Endocrine disorders = hyperparathyroidism
•
Infections of the kidney and the bladder
•
Obstruction of the urine flow
•
Family predisposition
•
Endemic predisposition = usually regions where water contains > CaCO3
Symptoms
•
Renal colic = sudden harsh pain usually in one of the lumbar regions, propagating towards the
bladder and the groin.
•
Hematuria
•
Nausea and vomiting, fatigue, sweating, restlessness
•
Urinary urgency
•
Pain and burning during urination are possible especially when the stone is in the bladder or
in the case of cystitis
•
In some cases, the colic may provoke hypertonic crisis w/its symptoms
•
Presence of fever indicates concomitant infection
Lab tests
•
Urine = RBCs and even RBC casts (during renal colic), mild proteinuria; WBC in case of
concomitant infections.
•
Blood count and sedimentation rate are normal unless there is infection
•
Creatinine and uric acid are usually normal
•
In cases w/severe bleeding or oncoming lithotripsy, coagulation status and blood group must
be checked
Instrumental tests
•
Abdominal ultrasound = would show the stones in the pyelon, calices, and the bladder or
hydronephrosis and dilation of the ureter in case of ureterolithiasis
•
Native X-ray of abdomen may show only roentgen +ve stones/radiopaque (oxalates,
phosphates, cysteine stones)
•
Roentgen –ve stones (uric acid stones) are visualized by venous urography when the contrast
is encircling the stone
•
Non-contrast spiral CT os imaging modality of choice in those w/acute renal colic
•
Chemical analysis of the stone must be performed when it is eliminated spontaneously or
instrumentally
•
Measurement of the pH of the urine is also important due to treatment and prophylaxis of
nephrolithiasis
Treatment
•
Small stones (<5mm) may pass spontaneously through urination w/in 4 weeks of onset of
symptoms
•
Hydration
•
Urine alkalisation for uric acid stones
•
Pain management = IV NSAIDs or opioids
•
Medical expulsive therapy to speed the spontaneous passage of stones in the ureter = αadrenergic blockers (tamsulosin) and Ca2+ channel blockers (nifedipine) may be effective
•
Lithotripsy = non-invasive technique for the removal of kidney stones which involves physical
destruction of the stones.
•
Uteroscopic surgery to remove large stones
Complications
•
Hydronephrosis in some cases followed by pyelonephrosis; in prolonged hydronephrosis (>1
month) the renal function may be irreversibly damaged and even the kidney may be totally
lost
•
Infections
•
In rare cases, when both ureters are obstructed → urinary retention and acute renal failure
119) Adult polycystic renal disease
Autosomal dominant polycystic kidney disease (ADPKD) (AKA adult PKD) – definition = a
multisystemic and progressive disorder characterised by the formation and enlargement of cysts in
the kidney and other organs (liver, pancreas, spleen). It is the most common form of inherited cystic
kidney diseases
Classification and pathophysiology
•
Type I = caused by mutations in the PKD1 gene and accounts for 85% of cases
•
Type II = caused by mutations in the PKD2 gene and accounts for 15% of cases
The products of these genes, polycystin-1 and
polycystin-2, are found in the primary cilia that line the
apical surface of the tubular epithelium. These primary
cilia are thought to act as sensors of urinary flow and as
signal transducers for tubular cell proliferation,
differentiation, and apoptosis.
The disease is characterized by a ‘second hit’
phenomenon, in which a mutated dominant allele is
inherited from a parent, with cyst formation occurring
only after the normal, wild-type gene sustains a
subsequent second genetic ‘hit’, resulting in renal
tubular cyst formation and disease progression
Epithelial cell proliferation and fluid secretion that lead to cystogenesis are two hallmark features in
ADPKD. During the early stages of cystogenesis, cysts are attached to their parental renal tubules
and a derivative of the glomerular filtrate enters the cysts. Once these cysts expand to ~2 mm in
diameter, the cyst closes off from its parental tubule and after that fluid can only enter the cysts
through transepithelial secretion.
Clinical manifestations
•
Pain – abdomen, flank, or back. Dull aching and an uncomfortable sensation of heaviness
may result from a large polycystic liver
•
Intermittent gross hematuria
•
Ballotable (palpable) kidneys
•
Complications of associated liver cysts, HT, UTIs (acute pyelonephritis, infected cysts,
perinephric abscess)
•
Subarachnoid haemorrhage associated w/berry aneurysm rupture
•
Uraemia and/or anaemia associated w/CKD
•
↑ RBC/EPO secretion from cysts
Diagnosis
•
US, CT, MRI
•
Genetic testing
•
Urine culture, CBC, serum chemistry profile (Ca, phosphorus)
DDx = acquired renal cystic disease, AR kidney disease, medullary cystic disease, tuberous
sclerosis, simple renal cysts
Treatment
•
Pain management, BP control (ACEIs/ARBs), treat UTIs, aquaretics (tolvaptan - ↓ speed in
gain of total kidney volume which can alleviate pain)
•
Renal cyst aspiration, laparoscopic cyst decortication (removal of cyst)
•
Nephrectomy, dialysis, kidney transplant
Complications
•
End-stage renal disease (ESRD)
•
Polycystic liver disease
•
Cerebral aneurysms
•
Kidney stones
120) Acute renal failure – renal parenchyma and treatment
Definition = sudden reversible impairment of the renal function causing retention of N-containing
substances, hypervolemia, electrolyte and acid-base misbalance. AKA acute kidney injury (AKI)
Classification = pre-renal, intrinsic, post-renal (retention of urine); oliguric and non-oliguric; w/slow or
rapid ↓ of GFR
Etiology and pathogenesis
Pre-renal causes
•
Pre-renal causes are those that ↓ effective renal blood flow and cause a ↓ in the GFR
(glomerular filtration rate). Both kidneys need to be affected as one kidney is still > than
adequate for normal kidney function
•
Notable causes = hypovolemia, hypotension, HF, liver cirrhosis, and local changes to the
blood vessels supplying the kidney (renal a. stenosis and renal v. thrombosis)
•
↓ blood flow → < blood to glomerulus → < blood is filtered → ↓ in GFR (how much blood the
kidneys filter through their glomeruli per minute)
•
As a result, < urea and creatinine are filtered out (i.e. > stays in the blood) → azotemia (high
levels of N-containing substances in the blood) and oliguria
•
Kidneys activate RAAS → aldosterone released from adrenal glands → reabsorption of Na+
back into the blood (water follows Na+)
Intrinsic/intra-renal
Due to disease processes which directly damage the kidney itself – parenchymal disorders
•
Tubules = acute tubular necrosis (epithelial cells that line the tubules die) due to ischaemia,
and nephrotoxins (aminoglycosides, lead) → the dead epithelial cells accumulate and block
the tubule → ↑ pressure in the tubules → ↓ GFR → oliguria, azotemia, hyperkalaemia,
metabolic acidosis
•
Glomerulus = glomerulonephritis – AB-Ag complexes deposit into glomerular tissue →
activation of complement → macs, Neu release lysosomal enz. → inflammation and damage
to podocytes → ↑ membrane permeability; proteins filtered into urine = proteinuria, hematuria
•
Interstitium = acute interstitial nephritis
Certain med classes such as calcineurin inhibitors (e.g. tacrolimus), aminoglycosides, amphotericin
B, and NSAIDs, can also directly damage the tubular cells of the kidney and result in a form of
intrinsic AKI
Post-renal
•
Caused by retention of urine due to obstruction of the urinary tract:
Kidney stones
Compression of ureter (intra-abdominal tumours)
Compression of urethra (benign prostatic hyperplasia)
•
Unilateral obstruction (1 ureter affected) = renal function preserved
•
Bilateral obstruction (both affected) → acute renal failure → build-up of urine and pressure
that backs up into kidney (hydronephrosis) → ↓ GFR → azotemia, oliguria. High pressure in
the tubules forces Na+ and water to be reabsorbed back into the blood
Phases
Phase
Features
Onset phase
•
Common triggering events = significant blood loss, burns,
fluid loss, diabetes insipidus
•
Symptoms of the underlying illness causing acute renal
Duration
Hours – days
failure may be present
Oliguric (anuric)
phase
•
Urine output <400 mL/day (oliguria), possibly as low as
< 2 weeks
100 mL/day (anuria)
•
Azotemia = ↑ retention of urea and creatinine → ↑ in blood
urea nitrogen (BUN)
•
Complications = fluid retention (pulmonary oedema),
hyperkalaemia, metabolic acidosis, uraemia.
Diuretic/polyuric
phase
•
Occurs when cause is removed
•
GFR returns to normal → ↑ urine production (polyuria),
7-14 days
tubular reabsorption remains disturbed
•
Recovery phase
Complications = loss of electrolytes (hyponatremia,
hypokalemia), dehydration
Kidney function and urine production normalise
Up to 2 years
Clinical manifestations
•
Main symptom is oliguria or anuria (diuresis < 400 and 100 ml respectively)
•
The clinical picture is often dominated by the underlying cause – symptoms of the disease
that caused the AKI
•
Azotemia leads to = fatigue, loss of appetite, headache, N/V
•
Hyperkalaemia = arrhythmias
•
Hypervolemia = SOB, pulmonary oedema
•
In severe cases = anxiety, confusion, drowsiness, coma
•
Consequences of AKI (MAD HUNGER) = Metabolic Acidosis, Dyslipidemia, High potassium,
Uraemia, Na+/H2O retention, Growth retardation, EPO failure (anaemia), Renal
osteodystrophy
Diagnosis
AKI can be diagnosed if any of the following is present (KDIGO classification):
•
↑ in serum creatinine by ≥0.3 mg/dl (≥26.5 μmol/l) w/in 48 hours; or
•
↑ in serum creatinine to ≥1.5 times baseline, which has occurred w/in the prior 7days: or
• Urine volume < 0.5 ml/kg/h for 6 hours
Other findings:
•
Urine:
Proteinuria and erythrocyturia; according to the etiology haemoglobinuria,
myoglobinuria, fibrin degradation products may also be present.
The specific gravity depends on the cause (high in acute glomerulonephritis, low in
acute tubulointerstitial nephritis).
Leukocyturia in cases w/infection; however, bacteriuria is seldom present because
acute renal failure in infections w/common bacteria is rare.
The osmolality of the urine gives a clue to the form of renal failure – osmolality of the
urine over 500 mOsm/l suggest prerenal cause; when under 300 mOsm/Kg – renal
and post-renal causes, usually acute tubular necrosis
•
↑, urea (BUN – blood urea nitrogen) and uric acid
•
↑ K+
•
Decompensated metabolic acidosis
•
Blood count usually mild anemia due to retention of water, the other changes are due to the
primary disease causing the renal failure as are some of the other biochemical tests (as liver
enzymes, bilirubin, etc)
•
Total protein and albumin are often ↓ as α-amylase is ↑ both in acute and chronic renal failure
(from the saliva glands, not the pancreatic gland)
Instrumental tests
•
Imaging of the kidneys and urinary tract is not necessary to establish a diagnosis of AKI
but may be needed to determine the etiology.
•
Ultrasound
o To exclude obstruction
o Check for Hydronephrosis if UTO suspected
o Renal dysfunction – CKD, Renal artery stenosis
•
Non contrast CT
o Find cause of obstruction
o UTO
•
ECG for hyperkalemia
o Tall, tented T waves, Inc PR interval, Absent p waves, Widened QRS. Sine wave
pattern
Treatment
•
Initiate treatment for the underlying cause of AKI based on the presumed
mechanism.
o
Prerenal: Correct adverse hemodynamic factors and replace the depleted
volume as needed.
o
Postrenal: Relieve the urinary tract obstruction.
o
Intrinsic: Consider a trial of IV fluids; identify and treat underlying causes that
require specific interventions.
•
Consider indications for acute dialysis and early nephrology consultation.
•
Provide supportive care to all patients.
o
o
o
o
o
o
Hold potentially nephrotoxic substances, ACE-Is, ARBs, NSAIDs, and
nonessential medications.
Consider additional supportive care measures (e.g., nutritional support, VTE
prophylaxis).
Ensure mean arterial blood pressure of 70 mmHg, adequate infusion
therapy
Diuretics – in case of hyperhidratation
Vasodilatation – renal doses of Dopamine
Treatment for elevated K+ (Infusion of glucose solutions + fast acting
insulin; Calcium gluconate;)
o
o
Treatment for metabolic acidosis - (NaHCO3)
Emergency dialysis treatment
•
Renal replacement therapy (RRT) – Dialysis
o Hemodialysis and hemofiltration, Peritoneal Dialysis
•
The main indications for blood purification and/or fluid removal are:
o
o
o
o
o
•
Symptomatic uraemia (including pericarditis or tamponade)
Electrolyte disturbances - hyperkalaemia not controlled by conservative
measures
Refractory fluid overload - Pulmonary Oedema unresponsive to diuresis
Acid base disturbances - severe acidosis
for removal of drugs causing the AKI, e.g. gentamicin, lithium, severe aspirin
overdose
Pre renal AKI
o Hypovolemia
IV fluid resuscitation with isotonic crystalloids to restore fluid losses
o
Shock
Immediate hemodynamic support
Identification of the cause of shock
o
Reduced effective arterial volume Cardiorenal syndrome: diuretic
therapy in acute heart failure
Hepatorenal syndrome management strategies include:
IV albumin, midodrine, and/or octreotide
o
•
Drugs that affect glomerular perfusion
Discontinuation of offending medications (e.g., ACE-Is, ARBs, NSAIDs)
Ensure adequate hydration.
Intrinsic AKI
o ATN
Discontinuation of potential nephrotoxins
Supportive care of AKI (mainstay of treatment) including IV fluid therapy with
isotonic crystalloids
o
AIN
•
TIPS for refractory HRS
•
Oliguric phase: strict fluid balance monitoring to avoid fluid overload
•
Polyuric phase: matching of fluid and electrolyte losses to prevent a
secondary kidney insult from hypovolemia
Discontinuation of potential nephrotoxins
Treatment of the underlying etiology
Glucocorticoid therapy may be considered.
Post-renal
o Bladder outlet obstruction
o
Urgent relief of urinary tract obstruction
•
Urethral catheterization
•
Consider suprapubic catheterization if a urethral catheter cannot
be passed.
Ureteral or renal pelvic obstruction
Urgent urology consult to relieve urinary tract obstruction
Management strategies include:
•
o
o
o
o
Ureteral stenting
• Percutaneous nephrostomy
Depending on underlying cause
Most need fluid resuscitation - crystalloids / ringers lactate
If there is uncertainty on volume status - fluid challenge of 250mL crystalloid is done
to prove hypotension is fluid responsive
Colloid is contraindicated
• Fluid balance
o
o
Hypovolemia
500mL crystalloid over 15mins
Reasses fluid state
Further bolus 250-500mL crystalloid
Stop when euvolemic
Hypervolemia
Oxygen supplementation
Fluid restriction
Diuretics - symptomatic
Renal replacement therapy
Complications = uremic coma, pulmonary and cerebral oedema, arrhythmias
121) Chronic renal failure – stages and clinical course
Definition = progressive irreversible impairment of the renal function causing progressive ↓ clearance
of nitrogen and other products including hormones, leading to general intoxication, misbalance in the
electrolyte and acid-base homeostasis, etc; (AKA chronic kidney disease – CKD) (kidney damage or
a GFR < 60 mL/min/1.73 m2 for 3/> months)
OR progressive decline in renal function (over a period of months/years) due to the permanent loss of
nephrons
Etiology
•
Most common = DM, HT, glomerulonephritis
Diabetes = excess glucose in the blood sticks to proteins (non-enzymatic glycation)
which affects the efferent arteriole (becomes stiff and narrow) → difficult for blood to
leave the glomerulus → ↑ pressure in glomerulus → hyperfiltration
HT = renal a. wall thickens → narrow lumen → < blood and O2 to the kidney →
ischemic injury
Primary glomerular disease =
FSGS, IgA nephropathy;
secondary = diabetic
nephropathy, lupus nephritis.
•
Idiopathic
•
Systemic diseases = lupus, rheumatoid
arthritis
•
Infections = HIV
•
Medications = NSAIDs
•
Smoking
Clinical manifestations
•
HT = due to fluid overload and production of vasoactive hormones created by the kidney via
the RAAS → ↑ risk of suffering from congestive HF
•
Uremia = symptoms include pericarditis, impaired immune function, skin disorders (itching,
gout), GI manifestations (nausea/vomiting), neurologic manifestations (encephalopathy) and
sexual dysfunction
Uremic frost = crystallised urea deposits that can be found on the skin of those
affected by CKD.
In CKD, the high level of urea in the bloodstream leads to high levels of urea secreted
by eccrine sweat glands as a component of sweat. As water evaporates off of the skin,
it results in a crystallisation of the remaining urea
Is > common in severe, untreated uremia and is associated w/serum BUN levels >200.
•
Hyperkalemia = malaise, arrhythmias. Usually it doesn’t develop until GFR falls to < 20-25
ml/min/1.73 m2, at which point the kidneys have ↓ ability to excrete K. Hyperkalemia in CKD
can be exacerbated by acidosis (which leads to extracellular shift of K) and from lack of
insulin
•
↓ EPO synthesis = anaemia
•
Fluid balance overload = symptoms range from mild oedema to pulmonary oedema
•
Hyperphosphatemia = ↑ CV risk, neuropathy, gastroenteropathy, susceptibility to infection,
coagulopathies. It also ↓ plasma Ca2+ → demineralisation
•
Hypocalcaemia = due to calcitriol deficiency and resistance to calcemic action of parathyroid
hormone. Later, this progresses to secondary hyperparathyroidism, renal osteodystrophy,
and vascular calcification that further impairs cardiac function. Bone pain
•
Metabolic acidosis (due to accumulation of sulphates, phosphates, uric acid) may cause
altered enz. activity by excess acid acting on enz.; and also ↑ excitability of cardiac and
neuronal membranes by the promotion of hyperkalaemia due to excess acid (acidosis)
Staging
CKD stage
GFR level (ml/min/1.73 m2)
Stage 1 (normal)
≥ 90
Stage 2
60 – 89
Stage 3
30 – 59
Stage 4
15 – 29
Stage 5
< 15
Diagnosis
•
↑ creatinine, urea, and uric acid
•
Hypocalcaemia and hyperphosphatemia; K+ is ↑ only in the oligoanuric stage or in cases
w/wrong treatment w/diuretics or other drugs which ↑ K+
•
Decompensated metabolic acidosis
•
Normochromic and normocytic anaemia (due to lack of EPO)
•
Urine = variable levels of proteinuria, erythrocyturia and leukocyturia depending on the
etiology; urine culture is always required; first the conc. function of the tubules is ↓ and then
the dilution; at the last stages there is isostenuria – specific gravity of the urine 1.010 – 1.011
•
Abdominal US usually w/signs of nephrosclerosis – ↓ size of the kidneys (< 9 cm) and
narrowed parenchymal zone (< 14-15 mm)
•
Renal biopsy is performed only in the early stages; in patients w/demonstrative
nephrosclerosis it is irrelevant
•
ECG, echocardiography and X ray of the chest are usually required
•
Consultation w/neurologist and ophthalmologist may be useful in some cases
Treatment
•
BP control (ACEIs/ARBs); diet control (low salt and protein diet); treatment of high lipid levels
(statins); treat anaemia (EPO or parenteral Fe); vit D supplements
•
Referral to a nephrologist
•
Renal replacement therapy in the form of either dialysis or kidney transplant (stage 5 CKD)
Nephrotic vs. nephritic syndrome
•
Nephrotic and nephritic syndrome are both common clinical manifestations of glomerular
disease
•
Both are composed of characteristic clinical and lab findings, which result from damage to the
glomeruli
•
Glomerular diseases are usually categorised by the syndrome they cause, which is either
nephritic or nephrotic
•
Some diseases that manifest w/nephritic syndrome can simultaneously cause nephrotic-range
proteinuria (>3.5 g/day), the main feature of nephrotic syndrome. When the criteria of both
syndromes are fulfilled, the findings are referred to as mixed nephritic-nephrotic syndrome
(most common causes are MPGN, and diffuse proliferative GN)
•
Nephrotic syndrome = a collection of signs and symptoms indicating damage to the
glomerular filtration barrier – nephrotic-range proteinuria (>3.5 g/day) + hypoalbuminaemia
and oedema
•
Nephritic syndrome = an inflammatory process (indicates glomerular inflammation) that is
defined as the presence of ≥1 of the following: hematuria w/acanthocytes, RBC casts in urine,
proteinuria (<3.5 g/day), HT, mild-moderate oedema, sterile pyuria, oliguria, and azotemia.
Nephrotic syndrome
Presentation
Nephritic syndrome
•
Heavy proteinuria (>3.5 g/day)
•
Proteinuria (<3.5 g/day)
•
Hypoalbuminaemia
•
Hematuria w/acanthocytes
•
Generalised oedema
•
RBC casts in urine
•
Hyperlipidemia & fatty casts in
urine → frothy urine
•
Mild-moderate oedema
•
Oliguria
•
HT
•
Azotemia
•
↑ Risk of thromboembolism (via
•
HT
loss of antithrombin III)
•
Sterile pyuria
•
↑ Risk of infection (via loss of IgG
and tissue oedema which
compromises local blood supply
and immune response)
Pathophysiology
Damage to podocytes → structural
damage of glomerular filtration barrier →
massive renal loss of protein
Inflammatory response w/in glomeruli →
glomerular BM disruption → loss of renally
excreted RBCs (acanthocytes) and ↓ GFR
→ hematuria, oliguria, azotemia, and ↑ renin
→ oedema and HT
Causes
•
MCD
•
Post-streptococcal GN
•
FSGS
•
IgA nephropathy
•
Membranous nephropathy
•
Goodpasture syndrome
•
Diabetic nephropathy
•
Alport syndrome
•
Amyloidosis
•
RPGN
•
Lupus nephritis
•
Lupus nephritis
•
Microscopic polyangiitis
•
Granulomatosis w/polyangiitis
VIII.Toxicology and Allergology
122) Toxicodynamics and toxicokinetics of exogenous poisons
Toxicology
•
Definition = the branch of science that deals w/poisons, which themselves are
chemical/physical agents that produce adverse responses in the organism. The state of being
poisoned is a condition of organisms resulting from physical and chemical changes leading to
disturbances of the organism under influence of toxic substances.
•
Poisons can be defined as exogenous or endogenous. Poisoning can be acute or chronic,
have non-specific or specific symptoms, cause long-term effects, or even lead to addiction.
•
Common causes of toxicity include drugs, industrial chemicals, household chemicals,
environmental agents, natural toxins, and food additives
Toxicodynamics
•
Definition = describes the dynamic interactions of a toxicant w/a biological target and its
biological effects.
•
A biological target (site of action) can be binding proteins, ion channels, DNA, or a variety of
other receptors. When a toxicant enters an organism, it can interact w/these receptors and
produce structural or functional alterations.
•
The mechanism of action of the toxicant, as determined by a toxicant’s chemical properties,
will determine what receptors are targeted and the overall toxic effect at the cellular level and
organismal level
•
The toxic effects are generally the result of enz. damage, protein synthesis disruption, DNA
damage, or modification of biochemical function.
•
Toxins can have 2 types of impact on the organism = quantal dose response (all-or-none
response, i.e., up to a certain dose there is no response) or the graded dose response (when
dose ↑, the response ↑)
•
We can also consider the effect that different toxins have on an organism based on how they
impact each of the systems
Interfere w/O2 transport in blood (e.g. CO, cyanide)
Depression of the CNS (e.g. sedative-hypnotics)
Attack the ANS (e.g. organophosphates, insecticides)
Damage to the lungs by aspiration (e.g. hydrocarbons)
Affect the CVS through myocardial dysfunction, dysarrhythmias, BP changes,
Local tissue damage
Damage to kidney/liver function
Toxicokinetics
•
Definition = describes the changes in the conc. of a toxicant over time due to the uptake,
biotransformation, distribution, and elimination of toxicants (ADME model)
•
Absorption = oral (GI tract), dermal, and inhalational route. It depends on the route of
administration, its ability to become ionised, its solubility, its conc., blood flow to the site of
admin, and the area of the absorptive site
•
Distribution = the apparent volume in which a substance is distributed. VD (dose/plasma conc.)
is important as it helps predict the peak blood conc. of the chemical taken and allowing us to
better understand the dose taken. Distribution depends on protein binding, plasma conc.,
physiological barriers, and the affinity of chemicals to certain tissues
•
Metabolism = can produce metabolites that are pharmacologically active and toxic. The liver is
the most common site of metabolism. There are 2 processes – phase 1 (drug is converted to
a more polar compound by oxidation, reduction, hydrolysis etc.) and phase 2 (conjugation
w/an endogenous substance by CYP450).
•
Notable inducers (↓ drug conc.) = phenytoin, carbamazepine, barbiturates, rifampicin, alcohol,
sulphonylureas
•
Notable inhibitors (↑ drug conc.) = allopurinol, omeprazole, disulfiram, azithromycin, valproate,
isoniazid, ciprofloxacin, ethanol, sulphonamides
•
Excretion = via kidneys, lungs, saliva, tears, milk, bile and/or faeces
123) Treatment of acute exogenous poisoning
The fundamental of poisoning management = supportive care, prevention of further poison
absorption, enhancement of poison elimination, administration of antidotes, and prevention of reexposure.
Supportive care
•
Goal of supportive therapy is to maintain physiologic hemostasis until detoxification is
accomplished and to prevent and treat secondary complications such as aspiration, bedsore,
cerebral and pulmonary oedema, renal failure, pneumonia etc.
•
ABCDEs are very important! Must always first clear the airway and ensure patient is well
ventilated. Endotracheal intubation may be indicated for unconscious patients or for protection
against aspiration of GI contents
•
Oxygenation/ventilation
•
Treatment of arrhythmias = mil/moderate supraventricular tachycardia treated
w/benzodiazepines or further combined treatment w/labetalol, CCB, or combo of BB and a
vasodilator
•
Hemodynamic support = if hypotensive then give IV fluids; administer adrenaline or high-dose
dopamine if unresponsive to this.
•
Treatment of seizures
•
Correction of temp. abnormalities
•
Correction of metabolic derangements
•
Prevention of secondary complications
Prevention of further poison absorption
•
GI decontamination (should be done w/in 1st 4 hours) = previously gastric lavage was
indicated however it is no longer common. It is sometimes considered for life-threatening
poisons that can’t be treated effectively w/other decontamination or elimination therapies
•
Activated charcoal is the preferred method of GI decontamination in most cases – has
comparable or greater efficacy; has fewer contraindications and complications; and is <
aversive and invasive than ipecac or gastric lavage. Recommended dose is 1 g/kg of body
weight
•
Whole bowel irrigation is performed by administering a bowel cleansing solution containing
electrolytes and polyethylene glycol orally or by gastric tube at a rate of 2 L/h (0.5 L/h in
children) until rectal effluent is clear. It is most appropriate for those who have ingested FBs,
packets of illicit drugs, and agents that are poorly absorbed by charcoal (heavy metals). It is
contraindicated in ileus, bowel obstruction, and hemodynamic instability.
•
Dilution (drinking water/milk at a volume of f ml/kg of body weight) is recommended only after
ingestion of corrosives.
•
Decontamination of other sites = eye, skin, and body cavity decontamination
Enhancement of poison elimination
•
Multiple-dose activated charcoal
•
Urinary alkalinisation = ion trapping via alteration of urine pH may prevent the renal absorption
of poisons that undergo excretion by glomerular filtration and active tubular secretion
•
Extracorporeal removal (haemodialysis, charcoal/resin hemoperfusion, hemofiltration,
plasmapharesis) = capable of removing toxin from the bloodstream; in cases of severe
poisoning w/carbamazepine, ethylene glycol, isopropyl alcohol, lithium, theophylline, and
salicylates.
•
Elimination of heavy metals can be enhanced by chelation, and the removal of CO can be
accelerated by hyperbaric oxygenation
Administration of antidotes
•
Antidotes counteract the effects of poisons by neutralising them or by antagonising their
physiologic effects.
•
IV lipid emulsion has been shown to be a successful antidote for poisoning from various
anaesthetics and membrane-active agents (cyclic antidepressants)
Agent
Indication
Activated charcoal with sorbitol
used for many oral toxins
Beta-blockers
theophylline poisoning (used in therapy for respiratory
diseases such as COPD and asthma)
Calcium chloride
CCBs, black widow spider bites
Glucagon
beta-blocker and CCB poisoning
Insulin with glucagon
beta-blocker and CCB poisoning
Flumazenil
benzodiazepine poisoning
Naloxone
Opiate poisoning
N-acetylcysteine
paracetamol (acetaminophen)
Sodium bicarbonate
aspirin overdose
Fomepizole or ethanol
methanol and ethylene glycol poisoning
Atropine
organophosphate, nerve agents, some mushrooms
Pralidoxime chloride
organophosphate insecticides, followed by atropine
100% oxygen or hyperbaric oxygen
therapy (HBOT)
carbon monoxide poisoning
Hydroxocobalamin
Cyanide poisoning
Prevention of re-exposure = adult education; childproofing; notification of regulatory agencies;
psychiatric referral
124) Acute exogenous poisoning w/medicines used to treat
cardiovascular diseases, benzodiazepines, antipsychotics,
antidiabetic, antipyretic, analgesics, and antiemetic agents
Cardiovascular drugs
ARBs
•
Used for treatment of HT, HF, and those w/previous MI
•
Mechanism = directly inhibit the action of angiotensin II
•
Pharmacokinetics = low VD, parent drugs are rapidly converted to active metabolites
•
Presentation = hypotension, bradycardia, hyperkalemia (especially in those w/renal
insufficiency and in combo w/NSAIDs)
•
Diagnosis = history of exposure, no specific bloods
•
Treatment = no specific antidote; consider oral charcoal
ACEI
•
Used for treatment of HT, HF, and those w/previous MI
•
Mechanism = blocks conversion of angiotensin I to angiotensin II thereby ↓ VC and
aldosterone activity. Additionally, can cause angioedema and cough, mediated by bradykinin
(which is normally broken down by ACE)
•
Pharmacokinetics = low VD, parent drugs are rapidly converted to active metabolites
•
Presentation = dry cough, hypotension, hyperkalemia, acute angioedema involving the
tongue, lips, and face which may lead to airway obstruction
•
Diagnosis = history of exposure, no specific bloods
•
Treatment = no specific antidote; consider oral charcoal to decontaminate
o
o
o
if hypotension occurs, treat it with supine positioning and IV fluid
treat angioedema with diphenhydramine or corticosteroids + discontinue ACEIs
treat hyperkalaemia if it occurs
CCBs
•
Used for treatment of HT, tachycardia, anti-arrythmic, and angina
•
Types: DHP’s – Amlodipine, Non-DHP’s - Verpamil
•
Mechanism = disrupt movement of Ca2+ through Ca2+ channels, limiting intracellular Ca2+
which ↓ excitation of skeletal, smooth, and cardiac muscle leading to VD and bradycardia,
reduce the force of contraction of heart
•
Toxicokinetics = good bioavailability, peak conc. after 1-2 hours; large VD, highly protein
bound
•
Toxicodynamics = cardiotoxic syndrome > likely if co-ingested w/other drugs acting on CVS.
Presents w/in 6-8 hours
o Clinical features are mostly in the CVS and include bradycardia, bradyarrhythmia (wide
QRS complexes), reduced contractility (long QT) and peripheral VD leading to
hypotension. Lactic acidosis can occur in patients w/significant hypotension;
hyperkalemia and hypocalcaemia may also occur.
•
Treatment = oral charcoal if presenting in 1st hour after ingestion.
o If bradycardic give atropine
o temporary pacing may be required if significant heart block.
o
Fluids for hypotension; add in IV Ca2+ if no response
Benzodiazepines
•
Benzodiazepines are sedative-hypnotic drugs prescribed for their sedative and anxiolytic
effects; also treat convulsions
•
E.g. midazolam, triazolam (short acting); temazepam (intermediate acting); lorazepam,
diazepam (long acting)
•
They are indirect GABA-A receptor agonists → ↑ affinity of GABA to bind to GABA-A
receptors → ↑ GABA action → ↑ opening frequency of chloride channels → hyperpolarisation
of the postsynaptic neuronal membrane → ↓ neuronal excitability
•
They also ↓ the duration of N3 phase in REM sleep, thereby ↓ the occurrence of sleepwalking
and night terrors.
•
Overdose = CNS depression (lethargy, somnolence, respiratory depression – intensifies when
combined w/other respiratory depressants like alcohol or barbiturates), mild hypotension,
hypotonia and hyporeflexia, ataxia, slurred speech
•
Benzodiazepines have a wider margin of safety than barbiturates and, consequently, a lower
risk of coma and respiratory depression
•
Diagnosis = history, clinical findings, urine screening for metabolites
•
Treatment = supportive therapy (oral charcoal, endotracheal intubation if GCS ≤8, fluid
resuscitation for hypotension); antidote = flumazenil – competitive antagonism at GABA
receptor (indicated for severe respiratory depression or overdose in accidental ingestion by
children). Overuse of flumazenil has risk of seizures and it induces a state of acute
benzodiazepine withdrawal
Antipsychotics
•
A heterogeneous group of substances used primarily to treat schizophrenia, psychosis,
mania, delusions, and states of agitation.
•
1st gen/typical antipsychotics (haloperidol, fluphenazine, chlorpromazine) = block D2 receptor
→ ↑ cAMP
•
2nd gen/atypical antipsychotics (clozapine, olanzapine, risperidone) = most are 5HT2 and D2
antagonists w/varying α and H1 receptor effects
•
Anti-dopaminergic effects (1st gen drugs) have strong extrapyramidal symptoms – a collection
of movement disorders that are typically due to disruption of dopaminergic pathways, resulting
in bradykinesia, rigidity, dystonia, athetosis, chorea, ballismus, tics, and tremors.
•
Anti-cholinergic effects (2nd gen) = dry mouth, constipation, blurred vision, mydriasis, urinary
retention, tachycardia.
•
The older drugs are absorbed slowly, w/erratic peak conc. often taking hours. Most drugs are
lipid soluble, w/large VD and are eliminated by hepatic metabolism w/long HL. Most have
metabolites which may contribute to toxicity
•
Risk factors for toxicity = young, F sex, patients w/liver disease, co-ingestion of drugs w/CNS
depressant activity
•
Treatment = supportive (activated charcoal w/in the 1st 4 hours), dystonic rxns should be
managed w/anticholinergics (procyclidine 5-10 mg IV/IM) if required
Anti-diabetics
Insulin
•
Has different preparations that vary based on their uptake and action time
•
Iatrogenic toxicity may arise as an error or patients may overdose to attempt to lose weight
•
Profound hypoglycemia may occur w/agitation, sweating, slurred speech, tachycardia,
seizures, and ↓ level of consciousness
•
Treat w/IV dextrose or glucose; treat any metabolic imbalances (hypokalemia is notable)
Metformin
•
Toxicity is due to inhibition of lactate dehydrogenase and development of severe lactic
acidosis. Metformin ingestion alone does not cause significant hypoglycemia
•
Symptoms = abdominal pain, N/V, diarrhoea, metabolic disturbance and severe lactic acidosis
•
Treatment = manage urea, electrolytes, creatinine, and lactate carefully; correct hypoxia and
any hypovolemia
Anti-pyretics
•
NSAIDs (ibuprofen, aspirin, diclofenac) reversibly inhibit COX-1 and COX-2 enz. → ↓
prostaglandin synthesis (involved in regulating pain receptor sensitivity, body temp., renal
blood flow, and inflammatory processes). Aspirin is the exception because it leads to
irreversible inhibition.
•
Effects = analgesic, antipyretic, anti-inflammatory
•
NSAIDs are rapidly absorbed and have low VD due to their plasma protein binding. Most have
a short HL
•
Overdose managed w/activated charcoal (w/in 1st hour). Otherwise, symptomatic treatment
Side effects
•
Gastric and duodenal ulcers w/risk of GI bleeding and perforation (inhibition of COX disrupts
the production of protective gastric mucosal prostaglandins)
•
↑ Risk of MI and stroke (w/the exception of aspirin and naproxen)
•
Renal function impairment = prostaglandins normally maintain renal blood flow by inducing VD
of the afferent arterioles. NSAIDs inhibit prostaglandin synthesis, which leads to harmful
hypoperfusion of the kidneys and ↓ GFR → electrolyte and fluid abnormalities (oedema,
hyperkalemia, hyponatremia), worsening of HT, acute renal failure in rare cases
•
Prolonged NSAID use results in tubulointerstitial nephritis and papillary necrosis
•
Pseudoallergic rxns = urticaria and angioedema, asthma, aspirin-exacerbated respiratory
disease
•
In very large doses, CNS and hepatic effects can be seen, however these are uncommon
Analgesics
•
Paracetamol is a commonly used analgesic and anti-pyretic
•
Minimum toxic dose = 7.5 g/day in adults
•
Exhaustion of hepatic metabolic pathways (CYP450) causes ↑ formation of a toxic metabolite
of paracetamol, N-acetyl-p-benzoquinoneimine (NAPQI) → irreversible oxidative hepatocyte
injury → hepatocellular necrosis
•
Clinical = non-specific (N/V, pallor, lethargy) or asymptomatic in the 1st 24 hours; progressive
liver impairment (RUQ pain, hepatomegaly, tenderness, abnormal LFTs); AKI occurs in ~50%
of patients w/acute hepatic failure
•
Treatment = activated charcoal (w/in 1st 4 hours); antidote PO/IV N-acetylcysteine, which
replenishes glutathione stores in the liver (this usually inactivates NAPQI); treatment of liver
failure; liver transplant in severe cases
Anti-emetic agents
•
Used to treat cases of N/V
•
Dopamine antagonists (metoclopramide – central anti-emetic effect); serotonin receptor
antagonist (ondansetron, granisetron – strong central anti-emetic, also peripheral effect via
inhibition of vagus n.); anti-cholinergics (scopolamine – non-specific muscarinic antagonist)
•
Metoclopramide overdose can cause neurological manifestations (drowsiness and confusion;
reversible extrapyramidal syndrome).
125) Acute exogenous poisoning w/alcohols: ethanol, methanol,
ethylene glycol
Alcohol intoxication = a temporary condition in which excessive consumption of alcohol alters a
person’s consciousness, cognition, perception, judgement, affect, and/or behaviour
Etiology
Ethanol (AKA ethyl/grain/drinking alcohol)
•
Simple alcohol w/chemical structure C2H6O
•
It is a psychoactive substance, recreational drug, and the active ingredient in alcoholic drinks.
•
It is naturally produced by the fermentation of sugars by yeasts or via petrochemical
processes such as ethylene hydration
Methanol
•
Chemical structure CH3OH
•
More toxic than ethanol; lethal in quantities as small as 10-15 ml (2-3 tbsp)
•
Sources of exposure = fuels (highly flammable), ingested as ethanol substitute by alcoholics,
improper distillation of spirits, self-harm attempts, accidental ingestion
Ethylene glycol (anti-freeze)
•
Colourless, odourless, sweet-tasting alcohol that is primarily used in radiators to raise the
boiling point and lower the freezing point
•
Sources of exposure = ingested as ethanol substitute by alcoholics, self-harm attempts,
accidental ingestion
Pathophysiology
Ethanol
•
Ethanol is metabolised in the liver and broken down by alcohol dehydrogenase where it is
converted to acetaldehyde which itself is catabolised into acetate by acetaldehyde
dehydrogenase. Acetate → acetyl-CoA
•
Alcohol works in the brain primarily by ↑ the effects of GABA which is the main inhibitory NT in
the brain. By facilitating its actions, alcohol suppresses the activity of the CNS
•
The substance also directly affects a n.o of other NT systems including glutamate, glycine,
ACh, and serotonin
•
The pleasurable effects of alcohol are the result of ↑ levels of dopamine and endogenous
opioids in the reward pathways of the brain
Methanol
•
Methanol has low toxicity and adverse effects of its ingestion are due to its metabolites
•
Metabolism of methanol in the liver → accumulation of formaldehyde and formic acid in the
blood (slow metabolism which allows it to accumulation) → anion gap metabolic acidosis
(acidemia) → cellular toxicity
•
Max effect = 48 hours after intoxication
•
Delayed toxicity = coingestion of methanol w/another alcohol will delay the metabolism of
methanol, and, therefore, the onset of toxicity
Ethylene glycol
•
The toxic mechanism of ethylene glycol poisoning is mainly due to its metabolites
•
Initially it is metabolised by alcohol dehydrogenase to glycolaldehyde, which is then oxidised
to glycolic acid by aldehyde dehydrogenase. The ↑ in metabolites may cause encephalopathy
or cerebral oedema. The metabolic effects occur 12-36 hours post ingestion, causing primarily
metabolic acidosis which is mainly due to accumulated glycolic acid.
•
Glycolic acid is then metabolised to glyoxylic acid and finally to oxalic acid. Oxalic acid binds
to Ca2+ → calcium oxalate crystals which deposit and cause damage to the brain, heart,
kidneys, and lungs.
Clinical manifestations
Ethanol
•
Short-term effects range from ↓ in anxiety and motor skills at lower doses to unconsciousness,
anterograde amnesia, and CNS depression at higher doses. Alcohol disrupts sleeping
patterns thereby ↓ sleep quality and can greatly exacerbate sleep problems.
•
Chronic heavy use of alcohol damages nearly every organ and system in the body. Risks
include liver cancer, malnutrition, chronic pancreatitis, cirrhosis, hepatitis, damage to the CNS
and peripheral NS (neuropathy), alcoholic cardiomyopathy.
Methanol
•
Nausea, abdominal cramps
•
Headache, altered mental status
•
Severe acidosis
•
Tachypnoea, hyperpnoea
•
Optic neuropathy = loss of visual acuity, scotoma, blindness
•
↑ Osmolar gap
Ethylene glycol
•
Sweet-smelling breath
•
Altered mental status, hallucinations, seizures
•
Tachypnoea, hyperpnoea
•
Calcium oxalate deposition in the kidneys → flank pain, hematuria, oliguria, and AKI
•
Signs of tetany due to hypocalcaemia
•
↑ Osmolar gap
Diagnosis = history and clinical findings; blood alcohol level; electrolytes; osmolar gap
Treatment
•
Supportive care – withdrawal of alcohol, hydration, gastric lavage
•
General =
o secure airways,
o oxygenation,
o
o
o
o
•
fluid resuscitation,
check serum electrolytes and osmolality,
crystalloid infusions for enhanced renal elimination
haemodialysis for severe metabolic acidosis and renal failure
Antidotes exist for methanol and ethylene glycol = fomepizole and ethanol – both prevent
the conversion of formaldehyde to formic acid.
o Fomepizole (1st line) competitively binds to alcohol dehydrogenase; ethanol (2nd line)
binds alcohol dehydrogenase w/higher affinity, thereby competitively inhibiting their
metabolism into toxic metabolites
•
Sodium bicarbonate for anion gap metabolic acidosis in methanol poisoning
•
Methanol = folic acid (accelerates the breakdown of formic acid)
•
Ethylene glycol = calcium gluconate for hypocalcaemia
•
Thiamine 100mg IV/IM to prevent neurologic injury
•
Hemodialysis in severe refractory cases or no improvement
126) Acute exogenous poisoning w/psychoactive substances
Ecstasy (Methylenodioxy-methamphetamine – MDMA)
•
A drug related to amphetamines that produces feelings of euphoria and empathy in users 30
mins – 1 hour after ingestion.
•
It is a sympathomimetic (stimulant) that ↑ the release and ↓ the reuptake of sympathetic
amines (noradrenaline, serotonin, dopamine).
•
Forms of preparation = pills or as loose powder dabbed on the gums
Patho
•
5HT2A-serotonin receptor and D2-receptor agonists and serotonin and dopamine reuptake
inhibitors = ↑ serotonin and dopamine conc. in the synaptic cleft → hallucinations
•
MDMA ↑ secretion of ADH → thirst → ↑ water intake w/out electrolyte repletion →
hyponatremia
Symptoms
•
Grinding teeth (bruxism)
•
Hyponatremia w/↑ risk of seizures and life-threatening cerebral and pulmonary oedema;
diaphoresis
•
Mental changes = euphoria and hyperactivity followed by severe agitation, anxiety, and
paranoia
•
Perceptive changes = distorted time and sensory perception, hallucinations
•
Cold extremities (due to peripheral VC); hyperthermia
•
Tachycardia w/arrhythmias, HT
Cocaine (AKA crack cocaine, coke, crack cocaine – free base form of cocaine)
•
A recreational drug used for stimulation
•
Forms of preparation = powder or rocks that are insufflated, smoked, or injected IV
Patho
•
Inhibition of dopamine, serotonin, and noradrenaline uptake → ↑ dopamine in the synaptic
cleft
•
Inhibition of Na+ channels causes local anaesthetic action by blocking n. AP transmission
Symptoms
•
Snorting can cause damage to the nasal vessels → nosebleeds. Local VC may cause
ischemic necrosis → perforated nasal septum
•
Intoxication = euphoria, arousal, ↑ vigilance, impaired judgment; sweating, tachycardia, HT,
chest pain; mydriasis; tachyarrhythmias; can result in sudden cardiac death; paranoia,
hallucinations; malignant hyperthermia
LSD (lysergic acid diethylamine) (AKA acid) = a recreational hallucinogenic drug
•
Patho = 5HT2A-serotonin receptor agonist (↑ serotonin and dopamine conc. in the synaptic
cleft → hallucinations)
•
Symptoms: Mental changes = marked anxiety and paranoia, psychosis
•
Perceptual changes = depersonalisation, visual and/or auditory perceptual distortion, and
synthesia are particularly noticeable
•
Flashbacks
•
Mydriasis
Cannabis (AKA weed, pot, skunk, grass, ganja)
•
Forms of preparation = most commonly smoked; vapourised; ingested orally via pills,
capsules, oil, or food
•
Marijuana is the dried leaves and buds of the cannabis plant; hashish/hash is the resin of the
cannabis plant
•
Medical marijuana (dronabinol) is used to ↑ appetite and treat N/V in terminally ill patients and
in those w/AIDS; it also relieves pain in cancer patients and ↓ intraocular pressure in
individuals w/glaucoma
Patho= tetrahydrocannabinol (THC; main active component) interacts w/the cannabinoid
receptors CB1 and CB2 → inhibition of adenylate cyclase (enz. that synthesises the 2nd
messenger cAMP)
Symptoms
•
Any of the following behavioural/mental disturbances must occur during/shortly after
consumption = euphoria, perceptual disturbances, impaired rxn time/conc./motor coordination, social detachment, impaired judgment, joviality, anxiety, panic
•
At least 2 of the following must be present w/in 2 hours after consumption = tachycardia,
conjunctival injection (red eyes), mydriasis, ↑ appetite, dry mouth
•
Additional features = paranoid delusions, hallucinations, ↑/↓ BP
Diagnosis = history and clinical features; blood/urine analysis
Treatment = withdrawal of the drug and treatment of intoxication w/benzodiazepines; supportive care
for withdrawal symptoms (usually resides w/in 72 hours); psychotherapy and group programs for drug
abuse; symptomatic treatment (external cooling for hyperthermia, antipsychotics for psychoses)
Complications = serotonin syndrome (MDMA), flashbacks, hallucinogen persisting perception
disorder (LSD); cocaine-induced vasospasm → MI, cerebrovascular accident, or ischemic colitis
(cocaine); cannabis-induced psychosis, anxiety/sleep disorders (cannabis)
Opioids
Classification:
•
Natural→ alkaloids contained in opium poppy: morphine, codeine
•
Semi-synthetic→ created from natural opioids: hydromorphone, diacetylmorphine(heroine)
•
Fully synthetic→ fentanyl, pethidine, methadone
Mechanism of action:
•
They reduce pain by binding to receptor sites in the CNS and PNS. They also inhibit the
release of many neurotransmitters including acetylcholine, NE, glutamate, and serotonin.
•
Opioids relieves severe pain in acute, chronic and terminal illnesses → also used to treat
anxiety, control diarrhoea and supress coughing
Adverse effects:
•
in acute cases they cause miosis, respiratory depression, nausea and vomiting, sedation
•
in chronic cases they cause tolerance, physical dependence and apnoea (in new-borns)
Clinical characteristics of toxicity
•
opiate toxicity should be suspected when following clinical triad is present:
-
CNS depression
respiratory depression (most specific sign)
pupillary miosis (not always present)
•
drowsiness, conjunctival infection and euphoria are present frequently
•
needle tracks are observed frequently
•
ventricular arrhythmias, acute mental status changes and seizures
•
bradypnea and hypopnea
•
use of opioids with other drugs that decrease respiration such as alcohol, sedatives, hypnotics
and anaesthetics, increase the risk of severe respiratory depression
Treatment
•
airway control and adequate oxygenation
•
endotracheal intubation in patients who cannot protect their airways
•
Naloxone (0.4-2mg IV) is administered for significant CNS and/or respiratory depression
•
in chronic opioid users slowly administer 0.1-0.2 mg IV aliquots every 1-2minute
•
in patients with non-opiate addiction, naloxone is administered by continuous IV infusion →
repeated dose of 2mg can be given every 3-5 minutes up to a total of 10mg (in addicted
patients this is dangerous because of concern for precipitating opiate withdrawal)
•
assisted bag-valve mask breathing can be provided until patient is ventilating adequately
127) Acute exogenous poisoning w/organophosphate compounds
Etiology = organophosphates are used as insecticides (malathion, parathion), herbicides, and n.
agents (soman, sarin)
Pathophysiology
•
Absorbed through the skin, RT, or GI tract
•
Irreversible inhibition of AChE → ↑ ACh levels → overstimulation of muscarinic and nicotinic
ACh receptors
•
Result = life-threatening activation of the PNS
Clinical manifestations
Acute cholinergic crisis and paralysis
•
CVS = bradycardia, hypotension
•
GI = N/V, diarrhoea, abdominal pain
•
Respiratory = bronchospasm
•
CNS = lethargy, seizures, tremor, possibly coma
•
Musculoskeletal = fasciculations, weakness, spasms, paralysis
•
Ocular = miosis, lacrimation
•
Uncontrolled urination; ↑ sweating and salivation
Chronic low-dose exposure = chronic organophosphate-induced neuropsychiatric disorder
characterised by fatigue, depression, impaired memory, extrapyramidal symptoms, peripheral
neuropathy, and autonomic dysfunction.
MNEMONIC = SLUDGEM (cholinergic crisis, Q9) or DUMBBELLS – diarrhoea, urination, miosis,
bronchospasm/bradycardia, emesis, lacrimation/lethargy, sweating/salivation
Diagnosis = history, clinical features (muscarinic toxidrome w/prominent respiratory findings, pinpoint
pupils, muscle fasciculations, and weakness); RBC cholinesterase levels (↓)
Treatment
•
Patient decontamination (e.g. remove clothes, wash skin)
•
Secure airways, O2 therapy, ECG
•
Meds = atropine; pralidoxime (2-PAM), obidoxime (regenerate AChE by dephosphorylation;
function peripherally on both muscarinic and nicotinic receptors); benzodiazepines (diazepam)
– to control organophosphate-induced seizures
128) Acute exogenous poisoning w/carbon monoxide
Etiology
•
CO poisoning, one of the most common fatal poisonings, occurs by inhalation.
•
CO is a colourless, odourless gas that results from incomplete combustion of hydrocarbons.
•
Common sources = house fires and improperly vented automobiles, gas heaters, furnaces,
hot water heaters, wood- or charcoal-burning stoves, and kerosene heaters.
•
CO is produced when natural gas (methane/propane) burns
•
Inhaling tobacco smoke results in CO in the blood but not enough to cause poisoning
Pathophysiology
Mechanisms of CO toxicity are not completely understood but they appear to involve:
•
Displacement of O2 from Hb (because CO has a greater affinity for Hb than does O2)
•
Shifting of the O2-Hb dissociation curve to the L (↓ release of O2 from Hb to tissues → tissue
hypoxia)
•
Binds to myoglobin which may impair its ability to utilise O2 → ↓ CO (cardiac output) and
hypotension → brain ischemia
•
Inhibition of mitochondrial respiration
•
Possibly direct toxic effects on brain tissue
Clinical manifestations
•
Early, non-specific = headache, nausea, malaise, fatigue
•
Levels >20% = vague dizziness, generalised weakness, difficulty concentration, impaired
judgement
•
Levels >30% = dyspnoea during exertion, chest pain, confusion
•
Higher levels can cause syncope, seizures and seizures
•
Hypotension, coma, respiratory failure, and death may occur, usually when levels are >60%.
•
CVS = tachycardia, hypotension, cardiac arrhythmia
•
CNS symptoms = delirium, hallucinations, dizziness, unsteady gait, confusion, seizures, CNS
depression, unconsciousness, respiratory arrest, and death
•
Less common symptoms of acute CO poisoning = myocardial ischemia, A-Fib, pneumonia,
pulmonary oedema, hyperglycemia, lactic acidosis, muscle necrosis, AKI, skin lesions, and
visual and auditory problems
•
Severe delayed neurological manifestations = short-term memory loss, dementia, amnesia,
psychosis, irritability, gait abnormalities, speech disturbances, Parkinson’s disease-like
syndromes, cortical blindness, depression.
Diagnosis = carboxy-Hb level in the blood (venous sample); CO-oximeter
DDx = cyanide toxicity, alcoholic ketoacidosis, aspirin poisoning, URT infection
Treatment = 100% O2 w/non-rebreather O2 mask); treat complications (hypotension, acidosis,
seizures, arrhythmias)
129) Snake venom poisoning
Etiology
•
In the developing world most snakebites occur in those who work outside such as farmers,
hunters, and fishermen. They often happen when a person steps on the snake or approaches
it too closely. In the US and EU snakebites most commonly occur in those who keep them as
pets.
•
The type of snake that most often delivers serious bites depends on the region of the world.
UK = vipers – specifically the common EU viper (adder)
Bulgaria = vipers – horned viper and common EU viper
Africa = mamba, Egyptian cobras, puff adders, and carpet vipers
North America = rattlesnakes
Asia = elapids, vipers, pit vipers
Pathophysiology
•
Since envenomation is voluntary, all venomous snakes are capable of biting w/out injecting
venom into a person (“dry bite”)
•
Venom affects virtually every organ system and can be a combo of many toxins including
cytotoxins, hemotoxins, neurotoxins, and myotoxins, allowing for an enormous variety of
symptoms
•
The strength of venom differs between species and even more so between families, as
measured by median lethal dose (LD50) in mice.
Clinical manifestations
•
“Dry bites” (bites w/out envenomation) = minor local symptoms – pain, swelling, bruising,
inflammation, lacerations to the skin
•
Envenomation leads to varying degrees of local and systemic symptoms that depend on the
amount and toxicity of the venom.
Rattlesnakes
Venom
Coral snakes
•
Cytohemoneurotoxic
•
Neurotoxin
•
↑ Permeability of the
•
Causes competitive
cell membrane
Local
clinical
features
Systemic
clinical
features
•
Fibrinolytic and protein
C-activation effect
•
Severely painful bite
•
Swelling, ecchymoses,
erythema
•
Bite painless or
mildly painful
•
Swelling and
paresthesia
Tissue necrosis
•
N/V
•
N/V, abdominal pain
•
Coagulopathy = can
lead to DIC and
bleeding
•
Neurotoxicity =
descending
paralysis
(dysphagia,
dysarthria, bulbar
paralysis),
respiratory
depression
Thrombocytopenia
•
Hemodynamic
instability (tachycardia,
hypotension,
distributive shock)
•
Neurotoxicity
(paresthesia, altered
mental status,
seizures)
•
Dendrotoxin = K+
channel blockage and
↑ release of ACh at
the NMJ
•
Multiple bite sites
•
No local swelling and
minimal tingling
sensation
•
Non-specific =
inhibition of pre- and
postsynaptic
muscarinic AChR
•
•
Black mamba
•
metallic taste, N/V,
abdominal pain
•
Neurotoxicity = ptosis,
bulbar palsy,
paresthesia
•
Autonomic symptoms
= hypersalivation,
diarrhoea, sweating,
miosis
Autonomic
symptoms
(hypersalivation,
miosis)
•
Can lead to loss of
consciousness and
respiratory paralysis
Diagnosis = history and clinical features
Treatment
•
First aid = remove tight clothing from limb; pressure immobilisation and/or tourniquets are not
recommended in USA as it can worsen local tissue damage
•
Give specific antivenom (hyper-immune animal serum Ig’s) administered w/IV
infusion/injection
•
Patients must be closely watched for signs of cardiovascular instability and respiratory
compromise.
•
Respiratory failure will require endotracheal intubation; AKI may necessitate dialysis; treat
hypovolemic shock supportively
•
Wound infection/necrotic tissue may be treated w/surgery
130) Acute exogenous poisoning w/mushrooms
Definition = harmful effects from ingestion of toxic substances present in a mushroom.
Etiology
The majority of fatal poisonings are attributable to the Amanita phalloides mushroom. Of the most
lethal mushrooms, five – the death cap (A. phalloides), the 3 destroying angels (A. virosa, A.
bisporigera, and A. ocreata), and the fool’s mushroom (A. verna) – belong the genus Amanita, and 2
more – the deadly webcap and the fool’s webcap – are from the genus Cortinarius
•
The death cap mushroom (A. phalloides) contains phalloidin and α-amanitin (blocks RNA
polymerase → inhibition of mRNA transcription and protein synthesis → apoptosis)
Clinical features
Death cap mushroom
•
For 6 hours = no symptoms
•
After 6-24 hours = GI symptoms (diarrhoea, N/V, abdominal cramps) that resolve 24-36 hours
after ingestion. This stage is caused primarily by the phallotoxins (found in various
mushrooms)
•
After 2-4 days = renal and liver failure
Orellanine toxin (Cortinarius genus)
•
Asymptomatic for 3-20 days after ingestion
•
Around day 11, the process of kidney failure begins, and is usually symptomatic by day 20.
Symptoms include pain in the kidney area, thirst, N/V, headache, and fatigue.
Muscarine (Omphalotus genus – Jack o’ lantern mushrooms)
•
Stimulates the muscarinic receptors of the nn. and muscles
•
Symptoms = cholinergic toxicity/crisis/SLUDGE syndrome – salivation, lacrimation, urination,
defecation, GI distress, and emesis (additionally miosis and muscle spasm)
•
NB! Features of anti-cholinergic syndrome would be remembered w/”Blind as a bat
(cycloplegia & mydriasis), mad as a hatter (delirium & hallucinations), red as a beet
(cutaneous VD), hot as hell (hyperthermia), dry as a bone (anhidrosis & xerophthalmia), the
bowel and bladder lose their tone (urinary retention & absent bowel sounds), and the heart
runs alone (tachycardia)”
Neurotoxins
•
Ibotenic acid is an excitotoxin which decarboxylates into muscimol upon ingestion which
causes CNS depression and hallucinations. Other symptoms include N/V, confusion,
euphoria, drowsiness, sweating, and chills.
Diagnosis = history and clinical features
Treatment
•
Supportive care – monitoring for hypoglycaemia and possibly repeated doses of activated
charcoal
•
Gastric decontamination w/in 1st hour after ingestion if patient has not vomited yet (e.g.
medically induced vomiting, gastric lavage and suction)
•
Suggested therapies = N-acetylcysteine, penicillin G, IV fat emulsion, silibinin
•
Treatment of liver/kidney failure may require transplantation
•
Neurotoxic symptoms are treated w/pyridoxine 70 mg/kg slow IV infusion over 4-6 hours
131) Hereditary angioedema (HAE)
Definition = a disorder characterised by recurrent attacks of angioedema (a self-limited, localised
swelling of the dermis, SC tissues, and/or submucosal tissues caused by fluid leakage into the
interstitial tissue).
Classification
Angiodema can be classified as:
•
Histamine-mediated angioedema = direct mast cell activation (non-IgE mediated) or allergic
rxns (IgE mediated)
•
Bradykinin-mediated angioedema = hereditary, acquired, or ACE inhibitor-induced
•
Angioedema of unknown cause = idiopathic angioedema, infections, drug-induced (CCBs,
immunosuppressive agents)
Etiology
AD disease due to:
•
Type 1 (85%) = inherited C1-esterase inhibitor (C1-INH) deficiency, a protein responsible for
complement regulation. A lack of C1-INH allows activation of kallikrein and subsequent
overproduction of bradykinin, which can trigger bradykinin-mediated angioedema.
•
Type 2 = dysfunctional protein
•
Type 3 = C1-INH function is normal and the
causal lesions is a mutant form of factor XII,
which leads to generation of excessive
bradykinin.
Types 1 and 2 are caused by a mutation in the
SERPING1 gene, which makes the C1-inhibitor
protein, while type 3 is often due to mutation in the
F12 (factor XII) gene.
Clinical manifestations in childhood and adolescence.
Possible triggers for HAE = oestrogen fluctuations
(oral contraceptives, hormone replacement,
menstruation, ovulation, pregnancy); infection,
mental stress/fatigue, physical exertion, trauma,
surgical and dental procedures, weather changes, drugs (ACEIs)
Pathophysiology
Bradykinin-mediated angioedema is triggered by ↑ levels of the proinflammatory VD bradykinin, which
can build up via several different mechanisms:
•
In type 1 and 2, the normal inhibitory function of C1-INH on the kallikrein-kinin system is ↓,
resulting in ↑ bradykinin generation
•
In type 3, a factor XII mutation leads to ↑ factor XIIa activity, which leads to ↑ bradykinin
generation.
Clinical manifestations
•
Facial oedema (mouths, eyelids, tongue)
•
Laryngeal involvement = dyspnoea and inspiratory stridor
•
Possible swelling of extremities and urogenital area (e.g. hands/feet, scrotum)
•
Family history often present (though not requires, since up to 25% of cases are due to
spontaneous mutations)
•
Abdominal symptoms (due to bowel wall involvement) = colicky abdominal pain, N/V,
diarrhoea
•
Angioedema of the extremities or trunk
•
Not associated w/urticaria or pruritus
Diagnosis
Diagnosis is mainly based on history and clinical findings. A flexible fiberoptic laryngoscopy should be
performed if there is no clear obstruction but clinical suspicion of angioedema is high.
Lab findings in HAE:
Type I
Type II
Type III
C1-INH level
↓
Normal
Normal
CI-INH function
↓
↓
Normal
C4 level
↓ during acute attacks
↓ during acute attacks
Normal
C1q level
Normal
Normal
Normal
C4 level is a sensitive screening test for C1-INH deficiency; C1q level is important to differentiate
between hereditary and acquired C1-INH deficiency (↓ in acquired C1-INH deficiency)
DDx = anaphylaxis
Treatment
•
Emergency management = treat anaphylaxis, if present; airway management; stop any
potential triggers
•
Administer one of the following targeted therapies = purified C1-INH concentrate (protein
replacement) – plasma derived/recombinant; kallikrein inhibitor (ecallantide); bradykinin-B2
receptor antagonist (icatibant)
•
2nd line or suspected ACEI induced etiology = fresh frozen plasma (FFP)
NB! Adrenaline, glucocorticoids, and antihistamines are usually not effective in acute HAE. If these
have been given empirically (e.g. for suspected anaphylaxis w/airway compromise) and there is a
poor response, then targeted therapy for bradykinin-mediated angioedema should be considered as
the next step (C1-INH replacement)
132) Asthma: epedimiology, pathogenesis, clinical features, diagnosis
and differential diagnosis
Definition = chronic inflammatory disease of the RT characterised by bronchial hyperresponsiveness,
episodic exacerbations (asthma attacks), and reversible airflow obstruction; manifests w/a reversible
cough, wheezing, and dyspnoea
Epidemiology
•
Prevalence = 5-10% of US population; black > white population; prevalence has been ↑ over
the past 20 years
•
Sex differs depending on age = M > F in patients < 18 years; F > M in patients > 18 years
•
Age of onset = childhood onset in allergic asthma; >40 years for non-allergic asthma
Classification
•
Allergic asthma (most common) = begins w/intermittent symptoms in childhood and is
usually associated w/atopy (genetic predisposition to produce IgE after Ag exposure – e.g.
eczema, rhinitis) and a good response to treatment
•
Non-allergic asthma = an uncommon type of asthma that is not related to atopy and is
typically associated w/a poor response to standard treatment
Etiology
Exact cause is unknown. Risk factors include = family history of asthma, past history of allergies,
atopic dermatitis, low socioeconomic status
Several factors can trigger an initial asthma attack or cause acute asthma exacerbations:
•
Allergic (intrinsic) asthma = atopy (cardinal risk factor); environmental allergens (pollen, dust
mites, mold spores); allergenic occupational asthma (flour dust)
•
Non-allergic (extrinsic) asthma = viral RT infections (most common stimuli, especially in
children); cold air; physical exertion (exercise-induced asthma); GERD (often exists
concurrently w/asthma); chronic sinusitis/rhinitis; meds (aspirin/NSAIDs, BBs); stress; irritantinduced asthma (solvents, tobacco smoke)
Pathophysiology
Asthma is an inflammatory disease driven by TH2 cells that manifest in individuals w/a genetic
predisposition. It consists of the following 3 pathophysiologic processes:
•
Bronchial hyperresponsiveness
•
Bronchial inflammation = overexpression of TH2 cells → inhalation of Ag results in production
of cytokines (IL 3-5, IL-13) → activation of eosinophils and induction of cellular response (B
cell IgE production) → bronchial submucosal oedema and SM contraction → bronchioles
collapse
•
Endobronchial obstruction = ↑ parasympathetic tone (reversible bronchospasm, ↑ mucus
production, mucosal oedema); hypertrophy of SM cells
Some forms have specific pathophysiologies:
•
Allergic asthma = IgE-mediated type I HS rxn; characterised by mast cell degranulation and
release of histamine after a prior phase of sensitisation
•
Non-allergic asthma:
Irritant asthma = irritant enters lung → ↑ release of neutrophils → submucosal oedema
→ airway obstruction
Aspirin-induced asthma is characterised by the Samter triad = inhibition of COX-1 → ↓
PGE2 → ↑ leukotrienes and inflammation → submucosal oedema → airway
obstruction; chronic rhinosinusitis w/nasal polyposis; asthma symptoms
Clinical manifestations
•
Persistent, dry cough that worsens at night, w/exercise, or on exposure to triggers/irritants
•
End-expiratory wheezes
•
Dyspnoea
•
Chest tightness
•
Prolonged expiratory phase on auscultation
•
Hyperresonance to lung percussion
•
Features of common comorbid conditions = e.g. chronic allergic rhinitis w/nasal congestion
Diagnosis
•
Peak flow meter = ↓ PEFR during asthma exacerbations; excessive variability in PEFR. It is a
portable device which allows rapid serial measurement of PEFR, however it is < accurate than
spirometry
•
Spirometry = ↓ FEV1 and Tiffeneau index (FEV1/FVC ratio); obstruction is reversible
w/bronchodilators
•
Bronchial provocation test = evidence of bronchial hyperresponsiveness after inhalation of
methacholine; +ve if FEV1 reduced by ≥ 20%
•
CXR = indicated in severe asthma to exclude DDx (pneumonia, pneumothorax)
•
In allergic asthma = ↑ total IgE and allergen specific IgE; possibly eosinophilia
DDx = COPD
Asthma
COPD
Age at diagnosis
Childhood/adolescence OR > 40 years (nonallergic)
Typically >40 years
Etiology
Allergic and non-allergic types
Smoking (90%)
Clinical features
Episodic (i.e. acute asthma exacerbations
w/asymptomatic phases in-between)
Insidious onset; chronic
progression over years
Bronchial obstruction
Reversible
Persistent
Meds
Good response to long-term ICS
Good response to
muscarinic antagonists
Asthma: management
Overview of asthma medications
Class
Beta-2 agonists
Examples
•
Short-acting β-2
agonists (SABA) =
albuterol, terbutaline
•
Long-acting β-2
Mechanism
Primary use
Dilate bronchial smooth
muscles
SABA = acute
exacerbations
LABA = long-term
maintenance treatment
Inhibit transcription factors → ↓
expression of pro-inflammatory
genes
Long-term maintenance
treatment (1st line)
Prevent leukotrienes from
binding to their receptors → ↓
bronchoconstriction
Long-term maintenance
treatment (particularly in
children).
Exercise-induced and
aspirin-induced asthma
agonists (LABA) =
salmeterol, formoterol
Inhaled
corticosteroids
(ICS)
Leukotriene
receptor
antagonist (LRA)
•
Beclomethasone
•
Fluticasone
•
Budesonide
•
Mometasone
Montelukast
•
Muscarinic
antagonists
Short-acting muscarinic
antagonists (SAMA) =
Ipratropium bromide
•
Methylxanthines
Mast cell
stabilisers
Long-acting muscarinic
antagonists (LAMA) =
Tiotropium bromide
Theophylline
•
Cromolyn sodium
•
Nedocromil sodium
Competitively inhibit
postganglionic muscarinic
receptors in bronchial smooth
Option for long-term
maintenance treatment
muscles → bronchodilation
Inhibits phosphodiesterase
(PDE) → ↑ cAMP levels →
anti-inflammatory and mild
bronchodilatory effect
Limited used (cardiotoxic,
neurotoxic)
Prevents release of
inflammatory mediators from
mast cells
Preventive treatment prior
to exercise or unavoidable
exposure to known
allergens in patients ≥55
years old
Oral
corticosteroids
•
Methylprednisolone
•
Prednisone
Biological agents
•
Omalizumab (1)
•
Mepolizumab (2)
Similar to ICS
•
Anti-IgE AB that binds
to serum IgE = ↓ serum
IgE prevents binding of
IgE to high affinity IgE
receptor on mast cells
and basophils → the
inflammatory cascade
triggering asthma is
inhibited. Long-term
reduction in serum IgE
will ↓ surface
expression of IgE
receptor on mast cells
and basophils. (1)
•
Used in severe and
refractory cases
Additional medication for
severe eosinophilic
asthma that is not
sufficiently controlled
w/other measures
Monoclonal AB against
IL-5 = potent
chemoattractant for
eosinophils (2)
•
Reliever (“rescue”) medications = provide relief of asthma symptoms by quickly opening up
the airways and are taken as needed when symptoms are present. E.g. SABA
•
Controller (“preventer”) medications = reduce the inflammation in the lungs, preventing
asthma symptoms over the long term. Controllers usually have steroids in them, and are used
every day – even if you don’t have any acute symptoms.
Treatment regime (NICE) (persons aged 17+)
•
Offer a SABA as a reliever therapy for adults w/newly diagnosed asthma. In patients
w/asthma who have infrequent, short-lived wheeze and normal lung function, occasional use
of a SABA might be the only treatment necessary
•
Offer a low dose of an ICS as the 1st line maintenance therapy to adults w/symptoms that
clearly indicate need for maintenance therapy (symptoms 3X per week or more, or causing
waking at night) OR asthma is uncontrolled w/a SABA alone
•
If asthma is uncontrolled on a low dose of ICS as maintenance therapy, offer a LTRA in
addition to the ICS and review the response to treatment in 4-8 weeks
•
If the asthma is still uncontrolled, offer a LABA in combo w/the ICS, and review LTRA
treatment
•
If the asthma is still uncontrolled, offer to change the person’s ICS and LABA maintenance
therapy to a maintenance and reliever therapy (MART) (a form of combined ICS and a fastacting LABA, is used for both daily maintenance therapy and relief of symptoms as required)
regimen w/a low maintenance ICS dose
•
If asthma is still uncontrolled, consider:
↑ the ICS to a high maintenance dose (this should only be offered as part of a fixeddose regimen, w/a SABA used as a reliever therapy) or
A trial of an additional drug (e.g. LAMA or theophylline) or
Seeking advice from a healthcare professional w/expertise in asthma
Treatment regime (GINA guidelines – global initiative for asthma)
•
Shift in treatment paradigm as of 2019
•
Previously = as-needed SABA reliever inhaler was the mainstay of intermittent asthma
treatment
•
New recommendation = all adults and adolescents’ w/asthma should receive ICS-containing
controller treatment to ↓ their risk of serious exacerbations and to control symptoms. New ICS
controller options include:
(for mild asthma) As-needed low dose ICS-formoterol or, if not available, low dose ICS
taken whenever SABA is taken, or
Regular ICS or ICS-LABA every day, plus as-needed SABA, or
Maintenance therapy and reliever treatment w/ICS-formoterol
•
Reasoning = ICS addresses the underlying problem of airway inflammation → reduces both
frequency of symptoms and risk of severe asthma exacerbations. SABAs only provide quick
relief of symptoms and SABA only treatment is associated w/↑ risk of severe exacerbations
and lower lung function. Regular use of SABA ↑ allergic responses and airway inflammation
and ↓ the bronchodilator response to SABA when it is needed
Severity
Treatment
Mild intermittent
Mild persistent
Moderate
persistent
Preferred
reliever
•
As-needed low dose ICS-formoterol or SABA
Preferred
controller
•
As-needed
low-dose
•
Daily low-dose
ICS
ICSformoterol
•
OR as-needed
low-dose ICSformoterol
OR low-dose
•
OR LTRA
ICS
whenever
SABA is
taken
•
OR low-dose
ICS whenever
SABA is taken
Alternative
and add-on
controllers
•
•
Severe persistent
•
Daily medium/highdose ICS-LABA
OR low-
•
OR high-dose ICS
dose ICS +
LTRA
•
± LAMA
•
± LTRA
•
± Low-dose OCS
•
± Omalizumab or
mepolizumab in
Daily lowdose ICSLABA
•
•
OR
mediumdose ICS
refractory cases
133) Insect allergy
Definition = allergic response to the bite or sting of an insect
Etiology
•
The most common cause of insect allergies are the families of the Apidae (honeybees and
bumblebees), Vespidae (hornets, wasps), and Formicidae (fire ants).
•
Most rxns to biting and stinging insects are limited to a primary lesion isolated to the area of
the bite and do not represent an allergic response. Occasionally, bites and stings induce
pronounced localised rxns or systemic rxns that may be based on immediate or delayed HS
rxns. Systemic allergic responses are attributed most typically to IgE-mediated responses,
which are caused primarily by stings from venomous insects of the Hymenoptera (bees,
wasps etc.) order, and more rarely from ticks, spiders, and kissing bugs.
Pathophysiology
•
Localised skin responses to biting insects are caused primarily by vasoactive or irritant
materials derived from insect saliva, and rarely occur from IgE-mediated responses
•
Systemic IgE-mediated allergic rxns to salivary proteins of biting insects are reported but
uncommon
•
IgE-mediated allergic responses to particular matter carrying insect emanations contribute to
season and perennial symptoms affecting the upper and lower airways
Clinical manifestations
Insect bites are usually urticarial but may be papular and vesicular. Clinical rxns to stinging venomous
insects are categorised as:
•
Simple local = involve limited swelling and pain, generally last <24 hours
•
Large local reactions = develop over hours to days; involve swelling of extensive areas (>10
cm) that are contiguous w/the sting site; may last for days
•
Generalised cutaneous = typically progress w/in minutes and include cutaneous symptoms of
urticaria, angioedema, and pruritus beyond the site of the sting.
•
Systemic = identical to anaphylaxis from other triggers and may include symptoms of
generalised urticaria, laryngeal oedema, bronchospasm, and hypotension
•
Toxic = stings from a large no of insects at once may result in toxic rxns of fever, malaise,
N/V, owing to the chemical properties of the venom in large doses
•
Delayed/late = serum sickness, nephrotic syndrome, vasculitis, neuritis, encephalopathy
Diagnosis = history of exposure, typical symptoms, physical findings; skin prick testing
Treatment
•
Avoidance of the insect
•
Stingers should be removed promptly by scraping, w/caution not to squeeze the venom sac
because doing so could inject more venom
•
For local cutaneous rxns = cold compresses, topical meds to relieve itching, NSAIDs
o Severe cases: Oral prednisone to reduce significant swelling
•
Treat anaphylaxis if present = IM Epinephrine, O2, IV saline, steroids, antihistamines, CorticoS
•
Venom immunotherapy = a prophylactic treatment against bite and sting allergic rxns; ↓ the
risk of severe systemic rxns
134) Food allergy
Definition = HS rxns to allergens contained in food. They are the most common cause of anaphylaxisrelated emergency admissions. Young children are commonly affected, usually beginning in the 1st 2
years of life.
Etiology = HS rxn against select ingredients in food. The most common food allergens are cow’s milk,
eggs, nuts, peanuts, seafood, soy, wheat, and fruits.
Risk factors – family history, vitamin D deficiency, obesity, high levels of cleanliness
Pathophysiology = commonly IgE mediated (type 1 HS rxn) – immediate onset, w/in mins – 2 hours of
ingestion. Mixed IgE/non-IgE-mediated and non-IgE-mediated rxns are also possible – delayed
onset, hours – days after ingestion.
Clinical manifestations
•
Skin (most common) = pruritus, urticaria, exanthema, angioedema, atopic dermatitis
•
Respiratory = rhinitis (often w/sneezing), nasal congestion, dyspnoea, wheezing, laryngeal
oedema
•
GI = oral allergy syndrome (oral pruritus, tingling numbness, and swelling of the lips, tongue,
palate, and throat); N/V, abdominal pain, diarrhoea
•
CVS = hypotension, tachycardia, arrhythmia
•
CNS = headache
Diagnosis
•
Patient history = determine type of food, time and amount of ingestion, and the type of rxn
•
Suspected IgE-mediated rxn = IgE skin prick test or RAST (radioallergosorbent test) – IgE
serum levels are measured in response to predetermined food allergens
•
If above tests are inconclusive or suspected food is not a common allergen = elimination diet
(eliminate suspected allergen from diet and observe for improvement of symptoms) or oral
food challenge (the effect of potential allergens on the mucous membranes is tested.
DDx = food intolerance, celiac disease, food poisoning
Treatment
•
Avoid allergens
•
In case of emergency, treat anaphylaxis
•
Oral immunotherapy (ingestion of ↑ doses of the allergen in a controlled setting, to desensitise
the immune system) is a novel approach, that is still being studies and not widely available.
135) Drug allergy: type I, II, III
Definitions
•
Hypersensitivity rxn (HS rxn) = exaggerated/inappropriate immune responses against an
Ag/allergen
•
Allergy = an abnormal immunological response to an otherwise harmless environmental
stimulus (e.g. food, pollen)
•
Autoimmune disease = an abnormal immunological response directed against an Ag that is
actually part of the body itself (self-Ag)
Stages of HS rxn = sensitisation (initial asymptomatic contact w/an Ag) and effect (harmful immune
response following sensitisation and subsequent Ag contact)
Mnemonic to remember the HS rxns = ACID – Allergic/Anaphylactic/Atopy (I), Cytotoxic (II), Immune
complex deposition (III), and Delayed (IV)
Type 1 HS rxn
Definition = IgE mediated/anaphylactic rxn. It is an allergic rxn provoked by re-exposure to a specific
type of Ag referred to as an allergen. Exposure may be by ingestion, injection, or direct contact. They
are immediate rxns and are AB-mediated
Ag = food, pollen, dust mites, drugs. AB = IgE
Etiology/examples
•
Allergic/anaphylactic transfusion rxns
•
Anaphylaxis
•
Drug rxn (e.g. penicillin, muscle relaxants)
•
Food allergies (e.g. nuts, shellfish, eggs, soy, wheat)
•
Rxns to inhaled/other environmental allergens (e.g. dust mites, animal fur, pollen) → asthma,
allergic rhinitis, atopy
Pathophysiology
First exposure (sensitisation)
•
Allergen enters the body and the Ag is phagocytosed by dendritic cells
•
Dendritic cell (APC) expresses the Ag to naive T cells → TH2 activated
•
TH2 (CD4+ cells) releases IL-4, 5, and 6 which activate B cells → plasma cells → release of
IgE
•
IgE AB binds to FcεRI receptors on mast cells which act as specific receptors
•
Mast cells are now sensitised and remain in the body, ready to attack the Ag
Subsequent exposure
•
Ag enters the body once more. Mast cells w/IgE AB now bind to the Ag
•
This causes mast cell degranulation and release of inflammatory mediators
•
Release of histamine → VD, bronchoconstriction, ↑ permeability of vessel walls = early
response
•
Cytokine release = recruitment and activation of inflammatory cells.
Leads to secondary late response = mucosal oedema, leukocyte infiltration, epithelial
damage, bronchospasm
Summary
1) IgE is formed as a result of prior desensitisation (i.e. previous contact w/the Ag) and coats
mast cells and basophils
2) Subsequent encounter w/Ag results in an IgE-mediated rxn by preformed IgE ABs = free Ag
binds to 2 adjacent IgE AB (crosslinking) → degranulation of cells
3) Release of histamine and other mediators (e.g. prostaglandin, PAF, leukotrienes, heparin,
tryptase) leading to = ↑ SM contraction (→ bronchospasm, abdominal cramping); peripheral
VD and ↑ vascular permeability (→ hypovolemia, hypotension); extravasation of capillary
blood (→ erythema); fluid shift into the interstitial space (→ oedema, pulmonary oedema);
pruritus
4) Mast cell secretion of cytokines and other pro-inflammatory mediators → eosinophil and
neutrophil chemotaxis → late-phase rxn (erythema, rhinorrhoea, sneezing, coughing,
wheezing) → inflammation and tissue damage
Clinical manifestations
•
Immediate rxn = allergic rxn w/in minutes of contact w/the Ag
•
Late-phase rxn = occurs hours after immediate rxn for a duration of 24-72 hours (primarily
cell-mediated, especially by eosinophils)
•
Main symptoms = pruritus, oedema, rash, rhinitis, bronchospasm, and abdominal cramping
Diagnosis
In vivo skin testing = small amounts of allergens are introduced into the skin to test for a local
allergic rxn; evaluation = skin reddening and size of wheals. E.g. skin prick test, scratch test,
intradermal test
In vitro testing (blood tests) = tryptase in serum (specific marker of mast cell activation), allergenspecific IgE (quantatively assessed using ELISA; indicated in patients w/known allergic triggers and
symptoms), total IgE.
Treatment = depends on the etiology of the rxn
•
Urticaria = avoid offending agent, H1-receptor blocker, glucocorticoids
•
Drug rxns = remove offending drug, monitoring, antihistamines, glucocorticoids (moderate
rxns)
•
Allergen immunotherapy (desensitisation) = the only causal therapy for long-term prevention
of allergic diseases. Indicated for documented IgE-mediated allergy (only available for some
allergens but can be quite effective)
Type 2 HS rxn
Definition = tissue-specific/cytotoxic HS. In type 2 HS, the ABs produced by the immune response
bind to Ag’s on the patient’s own cell surfaces. The Ag’s recognised may either be intrinsic or
extrinsic
Ag = drugs (penicillin); can be endogenous molecule. AB = IgM & IgG
Etiology/examples
•
Destruction of cells = acute hemolytic
transfusion rxn, autoimmune hemolytic
anaemia, hemolytic diseased of the fetus and
newborn, immune thrombocytopenia, druginduced neutropenia and agranulocytosis
(TMP/SMX, methimazole), pernicious anaemia
•
Inflammation = Goodpasture syndrome,
rheumatic fever, hyperacute transplant
rejection
•
Impaired cellular function = Graves disease,
bullous pemphigoid, myasthenia gravis
Pathophysiology
IgM and IgG mistakenly bind to surface Ag’s of the cells in the body, which results in:
•
Cellular destruction = AB-dependent cell-mediated cytotoxicity (NK cells or macs); target cell
opsonisation → phagocytosis and/or complement activation; e.g. autoimmune hemolytic
anaemia, acute hemolytic transfusion rxn
•
Inflammation = Fc-receptor mediated immune cell activation; AB bind to cellular surfaces →
activation of the complement system; e.g. Goodpasture syndrome
•
Impaired cellular function = AB bind to cell surface receptors → inhibition or activation of
downstream signalling pathways → impaired cellular function; e.g. Graves disease
Summary
•
Ag enters the body and binds to an APC → activation of B cells
•
Subsequent exposure = plasma cells are activated and large amounts of allergen-specific IgM
and IgG are formed and are densely bound to the allergenic cell surface (opsonification)
•
This forms an Ag-AB complex on the cell surface → activates complement system
•
The complement system then triggers the hemolysis of the cell, leading to tissue damage
Clinical manifestations, diagnosis, and treatment = depend on the underlying etiology
Diagnosis = may involve AB testing and the Coombs test
Type 3 HS rxn
Definition = immune complex mediated type of HS. Type 3 occurs when there is an accumulation of
immune complexes (Ag-AB complexes) that have not been adequately cleared by innate immune
cells, giving rise to an inflammatory response and attraction of leukocytes.
Ag = can be drugs, endogenous/exogenous molecules or proteins. AB = IgM & IgG
Etiology/examples
•
Serum sickness
•
Drug-induced HS vasculitis
•
Hypersensitivity pneumonitis
•
Polyarteritis nodosa (PAN)
•
Post-streptococcal glomerulonephritis
•
IgA nephropathy
•
Membranous nephropathy
•
Lupus
Pathophysiology
An excess of soluble Ag’s (as opposed to those in type II HS which are bound to cell surfaces) leads
to small immune complexes being formed that fix complement and are not cleared from the
circulation
•
When these Ag’s bind ABs, immune complexes of different sizes form. Large complexes can
be cleared by macs but they have difficulty in the disposal of small immune complexes.
•
These immune complexes insert themselves into small blood vessels, joints, and glomeruli →
activation of classical pathway
•
Such depositions can induce an inflammatory response and can cause damage when they
precipitate
•
Damage is to anaphylotoxins (C3a and C5a) which mediate the induction of granule release
from mast cells, and recruitment of inflammatory cells into the tissue → tissue damage
(vasculitis) → serum sickness
Summary
•
Ag binds to IgG to form an immune complex (Ag-AB complex)
•
Immune complexes are deposited in tissue, especially blood vessels → initiation of
complement cascade → release of lysosomal enz. from neutrophils → cell death →
inflammation → vasculitis
Clinical manifestations, diagnosis, and treatment = depend on the underlying etiology
Serum sickness
•
Definition = a classic e.g. of type 3 HS rxn which usually develops as a complication of
antitoxin or antivenom administration
•
Etiology = antivenom or antitoxin containing animal proteins or serum (→ “serum” sickness);
meds (e.g. penicillin, amoxicillin, TMP/SMX); infections (hep B)
•
Clinical features = symptoms appear 1-2 weeks following initial exposure (because ABs take
several days to form), and usually resolve w/in a few weeks after discontinuation of the
offending agent – fever; rash; arthralgia, myalgia; lymphadenopathy; headache, blurred vision;
abdominal pain, N/V, diarrhoea
•
Diagnosis = urinalysis may show mild proteinuria
•
Treatment = stop offending agent
136) Drug allergy: type IV a, b, c, d
Definition = delayed type/T-cell mediated HS. Unlike the other types, type 4 is cell-mediated and is a
delayed response (the 1st 3 HS rxns are AB mediated and are immediate)
Ag = some metals (e.g. nickel, chromium), cosmetics, detergents, organ transplants
Etiology/examples
•
Acute and chronic transplant rejection
•
Graft vs. host disease
•
Contact dermatitis (e.g. nickel, chromium, poison ivy, rubber gloves, cosmetics)
•
Mantoux tuberculin skin test for latent TB
•
Candida skin test
•
Drug rxns, including Steven-Johnson syndrome, DRESS syndrome, and toxic epidermal
necrolysis
•
Multiple sclerosis
•
Diseases w/auto-AB present = Guillain-Barre syndrome, Hashimoto’s thyroiditis, RA, DM1
Classification
•
Type 4a = T lymphocyte-mediated mac inflammation. Key immune mediators are IFN-γ, TNFα, and TH1 cells. E.g. contact dermatitis
•
Type 4b = T lymphocyte-mediated eosinophil inflammation. Key immune mediators are IL-4,
IL-5, IL-13, TH2 cells, and eosinophils. E.g. DRESS syndrome
•
Type 4c = T lymphocyte-mediated cytotoxic T lymphocyte inflammation. Key immune
mediators are cytotoxic T cells, granzyme, perforin, granulysin (for Steven-Johnson syndrome
only). E.g. Steven-Johnson syndrome, toxic epidermal necrolysis
•
Type 4d = T lymphocyte-mediated neutrophil inflammation. Key immune mediators are
neutrophils, IL-17, and GM-CSF. E.g. acute generalised exanthematous pustulosis
Pathophysiology
•
T-cell sensitisation = skin penetration by the Ag → uptake of the Ag by Langerhans cell →
migration to lymph nodes → formation of sensitised T lymphocytes (this process takes >5
days)
•
Presensitised T cell response (after repeated contact w/the Ag)
CD4+ T cells (Th1 or Th2) recognise Ag on APCs → release of inflammatory
lymphokines, cytokines (e.g. IFN-γ, TNF-α) → mac activation → phagocytosis of target
cells
CD8+ T cells (Tc) recognise Ag on somatic cells → cell-mediated cytotoxicity → direct
cell destruction
Summary = T helper cells (CD4+ cells) mainly act by cytokine-mediated recruitment of
inflammatory cells to the site of target cells. Cytotoxic T cells (CD8+ T cell) mainly act
by inducing apoptosis of the target cells
Summary = initial contact of Ag’s → sensitisation – sensitised T cells → TH1 → release of chemokines
= ↑ phagocytosis by macs → inflammation after 1-3 days and tissue damage
Clinical manifestations, diagnosis, and treatment = depend on the underlying etiology
Allergic contact dermatitis
•
Definition = a condition that makes skin red/inflamed after contact w/an allergen or an irritant
•
Etiology = poison ivy/oak; latex/rubber gloves; nickel, chromium, cobalt; perfumes, soaps,
cosmetics; topical meds (hydrocortisone, topical anti-B)
•
Pathophysiology = first contact w/allergen → sensitisation; repeated contact w/allergen →
development of a rash after 12-48 hours
•
Clinical features = intensely pruritic, erythematous, papular; vesicles and serous oozing in
severe cases; can spread to other parts of the body through Ag transfer by the hands or in the
circulation
•
Diagnosis = based on clinical findings; patch test (testing for specific allergens in allergic
contact dermatitis) – allergen is fixed on a patch and then attached to the arm/back, rxn
recorded at 48 hours and after 4-5 days, +ve result is erythema, papules, and vesicles under
the area of contact
•
Treatment = avoidance of the allergen; mild-moderate cases can use topical corticosteroids,
oatmeal baths, topical antihistamines, wet dressings, soothing lotions; severe cases can use
systemic corticosteroids and antihistamines
DRESS syndrome (drug rash w/eosinophilia and systemic symptoms; AKA drug-induced HS
syndrome – DIHS)
•
Definition = delayed HS rxn to a drug (w/in 1-8 weeks following administration)
•
Etiology = allopurinol, antiepileptic drugs (phenytoin, carbamazepine), anti-B (sulphonamide)
•
Clinical features = fever, pruritic morbilliform rash, facial oedema, hepatomegaly, diffuse
lymphadenopathy, possible multiorgan failure
•
Diagnostics = lab studies – eosinophilia, thrombocytopenia, atypical lymphocytosis
•
Treatment = drug withdrawal; corticosteroids are often used as symptomatic treatment, but
their effects are disputed
137) Anaphylaxis
Definition
•
Anaphylaxis = an acute, severe type 1 HS rxn that can cause life-threatening and
multisystem effects due to IgE-mediated mast cell activation.
•
Anaphylactoid rxn = a rxn that is clinically similar to anaphylaxis but is mediated by direct
non-immune-mediated activation of either mast cells or the complement cascade
•
Anaphylactic shock = a type of distributive shock that results from anaphylaxis
Etiology
Trigger is idiopathic is 20% of patients. The most common triggers leading to fatal anaphylaxis:
•
Younger patients = food allergies (e.g. peanuts, tree nuts), insect stings (e.g. bee stings)
•
Older patients = drug rxns, radiocontrast media
•
Hospitalised patients = food, meds (e.g. anti-B, NSAIDs), latex
Pathophysiology
Anaphylaxis (type 1 HS rxn – preformed IgE AB coating mast cells and basophils are crosslinked by
contact w/free Ag) → degranulation of mast cells → massive histamine release → systemic VD → ↑
capillary leakage → anaphylactic shock
Clinical manifestations
In general, the onset of symptoms is acute (w/in mins-hours of exposure to a likely Ag)
•
Skin/mucous membranes = flushing, erythema; urticaria, pruritus; swelling of the eyelids,
angioedema; nasal congestion, sneezing
•
Respiratory = cough, hoarseness; chest tightness; dyspnoea (due to bronchospasm or
laryngeal oedema), tachypnoea; stridor, wheezing; hypoxia, cyanosis
•
GI = N/V (especially in food allergies); abdominal pain, diarrhoea
•
CVS = hypotension; tachycardia, weak peripheral pulses; signs of end-organ dysfunction
(altered mental status, syncope; ↓ urine output/anuria; skin changes – mottling; low temp;
delayed capillary refill; ischemic chest pain)
Diagnosis (clinical diagnosis)
If any of the following criteria are fulfilled, anaphylaxis is likely. The onset of symptoms must be acute
(mins-hours)
•
Known allergen exposure w/hypotension (SBP <90 mmHg OR ≥ 30% ↓ from baseline)
•
Acute illness w/skin and/or mucosal symptoms AND ≥1 of the following = CVS or respiratory
symptoms (see above)
•
Suspected allergen exposure AND ≥2 of the following = skin, respiratory, GI, or CVS
symptoms (see above)
Treatment
•
Stabilise the patient (ABCDE approach)
Airway assessment and management
Rapid sequence intubation (RSI) for airway compromise (ketamine is preferred)
For severe bronchospasm = administer a bronchodilator (SABA – albuterol nebuliser
OR albuterol MDI; consider a muscarinic antagonist additionally)
Oxygen = provide FiO2 of 100% (e.g. high-flow O2 by non-breather mask)
Aggressive IV fluid resuscitation if hypotension is present (1-2 L 0.9% saline IV bolus)
Position the patient supine
•
Remove the inciting allergen
•
Administer epinephrine (adrenaline) IM 1:1000 (1 mg/mL) into the anterolateral thigh (repeat
every 5-15 mins as needed)
•
Refractory shock = continuous IV epinephrine infusion 1:1,000,000 (1 μg/mL). if patient is still
refractory = administer IV glucagon, especially if the patient is on a BB; consider other
vasopressors (vasopressin, noradrenaline, dopamine); ensure adequate fluid status; consider
consulting specialist team if above measures fail
•
Consider adjunctive treatment = antihistamines (H1-antagonists – diphenhydramine, or H2antagonists – ranitidine); corticosteroids (Methylprednisolone OR prednisone)
•
Continuous telemetry (monitoring of electrical activity of the heart) and pulse oximetry
•
Transfer to ICU or medical service if patient is not responding well
Complications = biphasic anaphylactic rxns (recurrence of anaphylaxis symptoms despite initially
successful treatment and w/out re-exposure to an Ag)
138) Hypersensitivity pneumonitis (AKA extrinsic allergic alveolitis)
Definition = HS rxn following exposure to environmental allergens
Etiology
•
Combined type 3 and type 4 HS rxn w/genetic predisposition
•
Inhalation of organic particles, primarily through occupational exposure
•
Farmers are frequently affected
•
Types of diseases = pigeon breeder’s lung (avian proteins), farmer’s lung (actinomycetes
spores), chemical worker’s lung (isocyanates) etc.
Pathophysiology
The exact pathogenesis is unclear but it is thought to be a cell mediated rxn. The cellular infiltrate
consists of lymphocytes, plasma cells, and neutrophils, w/non-caseating granulomas and activated
macs found. The inflammation tends to be bronchocentric or bronchiolocentric.
Clinical manifestations
Acute (4-8 hours after exposure) = flu-like symptoms (fever, chills, malaise, cough, headache);
dyspnoea w/out wheezing; chest tightness; diffuse fine crackles upon auscultation; symptoms
subside after 12 hours to several days (in the absence of additional exposure)
Chronic (moths after continuous exposure) = insidious onset of fatigue, productive cough,
progressive dyspnoea, and cyanosis; bilateral rales; weight loss; clubbing of the digits
Diagnosis
Mainly a clinical diagnosis based on history of exposure and typical clinical presentation, which is
supported by the presence of one of the following:
•
Positive serology = IgG, IgA, and/or IgM AB
•
CXR/CT = patchy reticulonodular/diffuse infiltrates in mid – upper zone (acute); ground-glass
attenuation w/honeycombing (fibrotic changes) w/ or w/out emphysema, traction
bronchiectasis, and thickening of the alveolar septa (chronic)
•
Pulmonary function test = restrictive pattern
•
Bronchoalveolar lavage (highly sensitive) = lymphocytic predominance
•
Lung biopsy = histopathological confirmation (non-caseating granulomas w/lymphocytes and
polymorphonuclear giant cells)
Treatment
•
Ag avoidance
•
Glucocorticoid therapy (symptomatic therapy)
•
Anti-fibrotic drugs (e.g. nintedanib, pirfenidone)
•
Last resort = lung transplant for persistent cases that are not responsive to medical therapy
Complications = respiratory failure; pulmonary heart disease
IX.Oncologic Diseases
139) Renal tumors
Benign renal tumours
1) Renal cysts - most common, rarely symptomatic and treated by percutaneous aspiration or
surgical cystectomy when indications are present
a. Classified according to Bosniak classification system.
2) Cortical adenoma – benign tumour of the adrenal cortex, and can present with
a. Cushing’s syndrome or primary hyperaldosteronism they may also secrete androgens,
causing hyperandrogenism
3) Oncocytoma – more common in males, hard to distinguish from malignant lesion in CT/MRI
a. arise from intercalated cells of the collecting duct, and accounts for 3-7% of renal
tumours occurs simultaneously with renal cell carcinoma in 7-32% of cases they are
spherical, capsulated and brown/tan-coloured (50% have a central scar) – and may be
multifocal and bilateral
b. often presents as an incidental finding, or with loin pain and haematuria
c. percutaneous biopsy recommended if there is high degree of suspicion if proven by
biopsy, then surveillance is adequate where the diagnosis is in doubt, partial
nephrectomy is indicated minimally invasive techniques e.g. radiofrequency ablation
may be considered for smaller tumours (where the possibility of renal cell carcinoma is
notexcluded)
4) Angiomyolipoma
a. benign mesenchymal tumour that occurs sporadically, mostly in middle-aged females
b. composed of perivascular epithelioid cells containing blood vessels, immature smooth
muscle and fat
c. frequently present as incidental findings on ultrasound or CT may present with flank
pain, palpable mass or painless haematuria
d. massive and life-threatening retroperitoneal bleeding occurs in 10% of cases
(Wunderlich’s syndrome)
e. Asymptomatic cases followed by serial ultrasound (if <4cm), those bleeding or of >4cm
require treatment (selective renal embolization or partial/total nephrectomy)
f. In tumours >3cm, mTOR inhibitor everolimus can reduce tumour volumes in some
patients
g. Cystic nephroma – in children – abdominal pain, hematuria, infections. Hypertension in
adults (especially women)
5) Leiomyoma – slow growth from renal capsule and rarely from renal vein.
Malignant renal tumours
1) Renal cell carcinoma (RCC)
a. adenocarcinoma of the renal cortex, arising from proximal convoluted tubule
b. 1-2% are bilateral, 7% are multifocal, 10-20% contain calcification or cysts
c. Histological subtypes:
i. Clear cell (80%) – highly vascular with clear cells or granular prognosis is
ii. relatively poor
iii. Papillary (10-15%) – well-circumscribed with a pseudocapsule and frequent
iv. necrosis
v. Chromophobe (5%) – arise from cortical portion of the collecting duct
relatively
vi. good prognosis
vii. Collecting duct (Bellini) – rare, in young patients and very poor prognosis
viii. Medullary cell – rare, arises from calyceal epithelium and often seen in young
sickle-cell sufferers
d. Etiology and risk factors
i. Sporadic - Males are affected 1.5x as commonly as females, and 50% present
at
ii. >70yrs old
1. Lifestyle- Smoking,Obesity
2. Associated conditions- Sickle cell disease, Acquired cystic kidney
disease ,Renal pelvic stones,Hypertension, Immunodeficiency, Chronic
hepatitis C infection
3. Substance exposure
iii. Occupational exposure to: Cadmium, Asbestos
iv. Petroleum by-products such as trichloroethylene (a degreasing agent)
v. Chemotherapeutic agents (e.g., cisplatin) during childhood
vi. Chronic analgesic use (acetaminophen, aspirin)
e. Inherited - 2-4% of renal cancers:
i. Von Hippel-Lindau syndrome – 50% of patients with this AD syndrome
(characterised by phaeochromocytoma, renal and pancreatic cysts, and
cerebellar haemangioblastoma) develop RCC
1. Hereditary pRCC (papillary) – AD condition characterised by trisomy 7
and 17, with activation of the proto-oncogene c-MET (receptor TK for
f.
hepatocyte growth factor, which regulates epithelial proliferation and
differentiation)
ii. Birt-Hogg-Dubé syndrome – mutation of FLCN gene on chr17p, and it is
characterised by benign tumours of hair follicles, pulmonary cysts,
pneumothorax and renal tumours (oncocytomas and RCC)
Clinical presentation
i. At least half of all RCC’s are detected incidentally on abdominal imaging
carried out
ii. for unrelated symptoms. Mostly asymptomatic in early stages.
iii. for symptomatic RCC:
1. 50% have haematuria
2. 40% have flank pain,
3. 25% palpable mass
4. Constitutional symptoms – Fever, weight loss, night sweats, fatigue
5. Signs of complications of RCC
iv. 30% have signs of metastatic disease
1. Lung - dyspnoea, hemoptysis
2. Bone – Bone pain, pathological fractures
v. Paraneoplastic syndromes due to ectopic hormone secretion by the
1. tumour occurs in 20% of patients
2. EPO - Polycythaemia
3. Renin – HT
4.
5.
6.
7.
8.
ACTH – Cushing’s disease
PTHrP – Hypercalcemia
Anaemia – Haematuria
Insulin - Hypoglycaemia
Stauffer's syndrome- 3% to 20% of cases.
a. Presents w/ hepatic dysfunction, fever, anorexia. Resolves after
nephrectomy.
vi. rarely, invasion of the left renal vein compresses left testicular vein,
causing a varicocele
vii. Budd-Chiari syndrome if Inferior Vena Cava involvement
viii. Metastasis is by:
1. direct extension to the adrenal gland, through the renal capsule (25%),
into the renal vein (44%), IVC (5%) and right atrium
2. by lymphatics to hilar and para-aortic lymph nodes
3. haematogenously to lungs, bone, liver and brain
4. 25% have metastases at presentation
g. Diagnosis
i. Anamnesis and physical exam – palpable abdominal mass
ii. FBC – polycythaemia from EPO secretion, anemia, thrombocytosis, Serum
creatinine, U&E, clotting profile, LFTs including ALP (bony mets), glucose
levels, Ca2+ level
iii. Urine cytology and culture – should be normal
iv. Imaging –
1. Renal ultrasound,
2. CT or MRI in those with contrast allergy or renal failure
3.
4.
5.
6.
7.
8.
Renal angiography
Retrograde pyelography
CXR shows ‘cannon ball’ metastases
Doppler ultrasound - any suggestion of renal vein or IVC involvement
CT may be further investigated with or MRI
Bone scan if metastasis suspected
h. Staging
i. T
1.
2.
3.
4.
5.
T0: No evidence of primary tumor
Tla: Tumor ≤ 4.0 cm and confined to the kidney
Tlb: Tumor > 4.0 cm and ≤ 7.0 cm and confined to the kidney
T2: Tumor > 7.0 cm and confined to the kidney
T3a: Tumor invades adrenal gland or perinephric fat but not beyond
Gerota's fascia
6. T3b: Tumor extents into the renal vein (or its segmental branches) or
vena cava below diaphragm
7. T3c: Tumor extends into the vena cava above the diaphragm or invades
the wall of the vena cava
8. T4: Tumor invades beyond Gerota's fascia
ii. N: Regional lymph nodes
1. N0: No regional lymph nodes metastasis
2. N1: Metastasis in a single regional lymph node
i.
3. N2: Metastases in more than one regional lymph node
iii. M: Distant metastases
1. M0: No distant metastasis
2. M1: Distant metastasis present
Management
i. Surgery is the mainstay of curative treatment for operable RCC (localized
tumours). Types – Open, Robotic, Laparoscopic surgery. For cT1 tumours,
partial nephrectomy
ii. Indications: solitary kidney; Localised unilateral RCC and healthy contralateral
iii.
iv.
v.
vi.
vii.
kidney
T1a,b tumours (up to 7cm) with a normal contralateral kidney)If RCC invades
IVC consider – Robotic/Laparoscopic surgery
For T2-T4 RCC and T1 in patients unsuitable for partial nephrectomy, Radical
nephrectomy performed
Done laparoscopically, with a transperitoneal or extraperitoneal approach
advantages over open surgery = less blood loss, reduced hospital stays and
quicker return to normal capacity
Open surgery is necessary only for large or locally advanced non-metastatic
RCC
Alternatives to surgical treatment (localised RCC)
1. Active surveillance – for small, solid renal masses (T1a, <4cm), serial
abdominal imaging (contrast-enhanced CT or ultrasound) can be done
2. Renal artery embolization – for patients with gross haematuria who are
unfit for curative surgery
3. Percutaneous minimally invasive treatment e.g. cryosurgery, image-
guided percutaneous radiofrequency ablation, high-intensity ultrasound
ablation – for those patients unfit or unwilling to undergo surgery
j. Contraindications:
i. life expectancy <1y,
ii. multiple metastasis, tumour localization in renal hilus, proximal ureter
iii. Coagulopathies, sepsis
k. RCC is resistant to chemotherapy and radiotherapy – (MDR-1 protein produced by
RCC)
i. For unresectable or metastatic disease,
1. Immunotherapy (as RCC is an immunogenic tumour expressing
numerous antigens)
ii. Cytokines
1. IL-2 only clear cell RCC
2. INF-alpha
iii. Targeted therapy
1. Tyrosine kinase inhibitors (VEGF inhibitors)
a. Sorafenib
b. Sunitinib
c. Pazopanib
2. mTOR inhibitors e.g., everolimus, temsirolimus
3. EGFR inhibitor - axitinib
4. Anti-VEGF antibodies: bevacizumab
l.
Prognosis
i. Overall prognosis is determined by the anatomic extent of the disease (stage
of cancer at diagnosis) and the histopathology of the tumour.
ii. Targeted therapies have significantly prolonged survival time.
iii. Early stage RCC with tumour growth limited to the kidney generally has a good
prognosis.
iv. 5yr survival - Stage 1/2 – 85%, Stage 3 – 60%, Stage 4 – 9%
2) Wilms’ tumour (nephroblastoma)
a. childhood tumour (soft, pale grey tumour) of the primitive renal tubules and
mesenchymal cells
b. Affecting 1 in 10,000 children, and is the main abdominal malignancy in
c. children (typically presents in children under 5yrs old
d. Etiology - Associated with mutations in WT1, WT2 and WTX genes
i. Can have associations with:
1. hemihypertrophy/macroglossia (Beckwith-Wiedemann syndrome)
2. aniridia, mental retardation (part of WAGR syndrome – Wilms’
tumour/Anirida/Genitourinary anomalies/mental Retardation)
3. foetal overgrowth (Perlman’s syndrome)
e. Clinical features include: palpable abdominal mass, painless haematuria,
abdominal/loin pain (unilateral in 95%of cases). hypertension may also occur.
f. Diagnosis is by ultrasound or CT
g. Treatment – staging nephrectomy,with or without preoperative/postoperative
chemotherapy (vincristine,doxorubicin)
h. Prognosis – 92% overall survival
i.
Staging
i. Stage I: The tumor is found in 1 kidney and can be completely removed with
surgery.
ii. Stage II: Cancer is found in the kidney and in the fat, soft tissue, or blood
vessels near the kidney. It may have spread to the renal sinus. The tumor can
be completely removed with surgery.
iii. Stage III: Cancer is found in areas near the kidney and cannot be completely
removed with surgery. The tumor may have spread to nearby organs and blood
vessels or throughout the abdomen and to nearby lymph nodes. Stage III
cancer has not spread outside the abdomen.
iv. Stage IV: Cancer has spread to other more distant organs, such as the lungs,
liver, bones, and brain, or to lymph nodes outside the abdomen.
v. Stage V: Cancer cells are in both kidneys at the same time. The tumor in each
kidney is staged separately.
140) Lung cancers
Definition = malignant tumour afflicting the bronchi (99%) or the alveoli (1%)
Etiology
•
Smoking = associated w/development of ~90% of lung cancers; weaker association w/lung
adenocarcinoma
•
Occupational and environmental exposure to carcinogens = passive smoking; radon (2nd
leading cause) and uranium; asbestos; occupational carcinogens (arsenic, chromium, nickel);
environmental air pollution
•
Family history (genetic predisposition)
•
Other risk factors = pulmonary scarring, previous radiation, pulmonary fibrosis, chronic
infections (e.g. TB, HIV)
Classification
TNM staging to stage the cancer (tumour, node, metastases)
Variants of lung cancer
•
Pancoast tumour = an apical lung carcinoma
•
Located in the sup. sulcus of the lung
•
Predominantly NSCLC
•
May lead to development of Pancoast syndrome = a constellation of symptoms secondary to
the mass effect of the tumour on surrounding structures
•
Lymphangitic carcinomatosis = spread of cancer cells along lymphatic vessels
Clinical manifestations
Symptoms may be related to the local effects of the tumour in the lung of spread of disease beyond
the chest. Lung cancer often only becomes symptomatic in late stages, generally affecting prognosis
negatively
Pulmonary symptoms = cough, hemoptysis, progressive dyspnoea, wheezing, chest pain
Extrapulmonary symptoms
•
Constitutional symptoms = weight loss, fever, weakness
•
Signs and symptoms of tumour infiltration and/or compression of neighbouring structures:
SVC syndrome = compression of the SVC impairs the venous backflow to the R
atrium, resulting in venous congestion in the head, neck, and upper extremities
Hoarseness = paralysis of the recurrent laryngeal n.
Dyspnoea and diaphragmatic elevation = paralysis of the phrenic n.
Dullness on percussion, ↓ breath sounds = malignant pleural effusion on the affected
side
Post-obstructive pneumonia
Dysphagia = oesophageal compression
Metastases
•
Common sites of metastases = brain, liver, adrenal glands, bone (BLAB)
•
Brain = headaches, seizures, focal motor deficits, behavioural changes
•
Liver = typically asymptomatic but may manifest w/nausea, jaundice, ascites
•
Adrenals = typically asymptomatic
•
Bone = bone pain, ↑ alkaline phosphatase and Ca2+
Diagnosis
•
Labs = CBC – anaemia, thrombocytopenia, neutropenia
•
CXR = < sensitive than CT; indirect signs of malignancy – atelectasis, post-obstructive
pneumonia, pleural effusion, mediastinal widening, cavitary lesions
•
CT (w/IV contrast preferable) = allows for the delineation of the primary tumour and the
assessment of mediastinal lymph node involvement; relatively insensitive for lymph node
metastases
•
PET/CT = useful for detecting occult lymph node involvement and extrathoracic metastases
•
Tissue biopsy = confirmatory test required for the diagnosis of lung cancer. Non-surgical
method involves bronchoscopy w/transbronchial biopsy for central nodules; CT-guided
transthoracic biopsy for peripheral nodules. Surgical procedures involve mediastinoscopy or
video-assisted thoracoscopy
Treatment
•
Surgical resection w/ or w/out chemo is the standard of care for early stage (stage I and IIA)
lung cancers.
•
Radiotherapy is the treatment of choice for patients w/inoperable early-stage disease (either
due to poor pulmonary reserve of medical comorbidities).
•
Treatment of locally-advanced NSCLC and limited stage SCLC (stage IIB-IIIC) requires a
multimodal approach w/chemo, radiotherapy, surgical resection, and immunotherapy.
•
Most cases of lung cancer are diagnosed at an advanced stage and are therefore treated
palliatively w/chemo and immunotherapy.
141) Esophageal cancer
Definition = neoplastic disorder originating from epithelial cells of the oesophagus – can be
benign/malignant and epithelial/non-epithelial.
Types
•
Oesophageal squamous cell carcinomas (ESCC) = arises from the epithelial cells that line the
oesophagus
•
Oesophageal adenocarcinoma (EAC) = arises from glandular cells present in the lower 1/3 of
the oesophagus
•
Usually, a cancer in the upper 2/3 is likely to be ESCC and one in the lower 1/3 EAC
•
Premalignant conditions = Plummer-Vinson syndrome, achalasia, oesophageal strictures,
oesophageal diverticula, Barrett’s oesophagus
•
Unusual types = neuroendocrine carcinoma, melanoma, carcinosarcoma, sarcoma
Etiology
•
Major risk factors for ESCC = smoking and alcohol; diet poor in fruit and veg; radiation,
chronic dysphagia, caustic ingestion, chronic oesophagitis, nutritional deficiencies
•
Major risk factors for EAC = GERD (long term erosive effects of acid reflux), western diet, ↑
risk of acid suppressing meds, smoking, achalasia, obesity. Long-standing GERD is
associated w/Barrett’s oesophagus
Clinical findings
•
Early = asymptomatic. Usually > 2/3 of the lumen has to be obstructed (stenosis), due to
physical presence of the tumour, before onset of symptoms
•
Most common symptoms = dysphagia, weight loss, retrosternal chest/back pain, anaemia
(caused by chronic blood loss)
•
Other symptoms can include = N/V, regurgitation, ↑ risk of aspiration pneumonia, cough, SOB
•
Less common = haematemesis, melena, hoarseness
•
Symptoms of metastatic spread = jaundice and ascites (liver); pleural effusion and SOB
(lungs)
•
Common sites of spread include nearby lymph nodes, liver, lungs, and bone
Diagnosis
•
EGD (best initial and confirmatory test) = direct visualisation of the tumour; w/biopsy of any
suspicious lesions
•
Barium swallow = asymmetrical and irregular borders of the oesophagus w/characteristic
stenosis and prox. dilation (apple core lesion)
•
Staging = transoesophageal endoscopic US (to determine infiltration depth and register
regional lymph node disease); chest and abdominal CT/MRI and/or PET
•
TNM staging – tumour, nodes, metastasis
DDx = non-erosive reflux disease (NERD) (no visible injury to oesophageal mucosa), achalasia,
oesophageal strictures, gastric stasis, sensitisation to foods
Treatment
•
Small tumours only involving the mucosa may be removed by endoscopic mucosal resection
(EMR)
•
Larger tumours that are resectable are removed by oesophagectomy – removal of a segment
of the oesophagus; as this shortens the length of the remaining oesophagus, some other
segment of the digestive tract is pulled up through the chest cavity and interposed (usually the
stomach or part of the LI or jejunum)
•
Chemotherapy and radiotherapy
Complications = cahexia, malnutrition, distant metastasis, aspiration pneumonia
142) Gastric cancer
Definition = malignant tumour of the stomach. high incidence in South Korea and Japan, declining
incidence in USA and EU
Etiology
Exogenous risk factors = diet rich in nitrates and/or salts, nicotine use, low socioeconomic status
Endogenous risk factors
•
Diseases associated w/a higher risk of gastric cancer = atrophic gastritis, H. pylori infection,
gastric ulcers, partial gastrectomy, GERD
•
Hereditary factors = +ve family history, hereditary non-polyposis colorectal cancer
•
Higher incidence in individuals w/blood type A
Clinical manifestations
Gastric cancer is often asymptomatic. Early signs are non-specific and often go unnoticed. At later
stages the following symptoms may occur:
•
General signs = weight loss, chronic IDA (pallor, fatigue, headaches)
•
GI signs = abdominal pain, early satiety, N/V, dysphagia, acute gastric bleeding
(haematemesis or melena)
•
Late stage gastric cancer = palpable tumour in epigastric region, gastric outlet obstruction,
hepatomegaly, ascites, malignant acanthosis nigricans
•
Virchow’s node = L supraclavicular lymphadenopathy, located where the thoracic duct joins
the subclavian v. at the venous angle – sign of metastatic gastric cancer
•
Sister Mary Joseph’s node = umbilical node indicating metastasis from a GI or
abdominopelvic malignancy
Metastases
•
Lymphangitic spread = all local nodes (lesser and greater curvature); celiac, paraaortic, and
mesenteric nodes; carcinoma of the cardia may spread to mediastinal lymph nodes
•
Hematogenous spread = liver, lungs, brain, bones
•
Local invasion of adjacent structures = peritoneal carcinomatosis, oesophagus, transverse
colon, pancreas
•
Direct seeding = to the ovaries (Krukenburg tumour), to the pouch of Douglas
Diagnosis
•
Upper endoscopy w/biopsy (best initial test) = take several biopsies
(~7) to make sure you don’t miss anything
•
Barium upper GI series may be considered and would show loss of
intestinal folds and stenosis
•
Labs = IDA
•
Staging = abdominal US; endoscopy (endoscopic US) to assess
tumour depth and local lymph nodes, abdominal and pelvic
CT/MRI, PET-CT, diagnostic laparoscopy
•
Tumour marker for treatment follow-up and monitoring = CA 72-4
Pathology
•
Adenocarcinoma (90% of cases) = typically localised, exophytic lesion +/- ulceration; arise
from glandular cells in the stomach; usually located on the lesser curvature of the stomach
•
Signet ring cell carcinoma = diffuse growth; multiple signet ring cells (round cells filled
w/mucin, w/a flat nucleus in the cell periphery)
•
Less common = Adenosquamous and squamous cell carcinomas
Lauren classification of gastric adenocarcinomas
•
Intestinal type (~50%) = polyploid, glandular formation, expanding (not infiltrative) growth
patter; clear border
•
Diffuse type (~40%) = infiltrative growth and diffuse spread in the gastric wall, no clear border
•
Mixed type (~10%)
Treatment
•
Chemo and radiotherapy – may be adjuvant (after surgery) or neoadjuvant (before surgery)
•
Endoscopic resection = only for tumours diagnosed at a very early stage, when they are
limited to the inner lining layer of the stomach
•
Surgery = radical gastrectomy and lymphadenectomy – resection of the lesser and greater
omentum and radical lymphadenectomy. An alternative would be subtotal gastrectomy
•
Decide which surgery to do based on size and location of tumour. If it is > distal (in pylorus)
should do 5 cm proximally (subtotal gastrectomy). If it is in the middle or upper part of the
stomach = anterior gastrectomy
•
2nd goal is to remove lymph nodes = lymph node dissection – all nodes around the stomach.
•
Roux-en-Y gastric bypass = surgeon separates the proximal jejunum from the duodenum and
creates an end-to-end anastomosis of the jejunum w/the remaining part of the stomach
(gastrojejunostomy), or in the case of a total gastrectomy, w/the oesophagus
(oesophagojejunostomy)
•
The duodenal stump is connected distally w/the jejunum using and end-to-side anastomosis
143) Tumors of the colon
Definition = development of cancer from the colon or rectum (LI)
Etiology (risk factors)
•
Advanced age: >40yrs
•
Hereditary syndromes = family history of CRC; familial adenomatous polyposis, (GS, TS, PJS,
JPS); hereditary nonpolyposis colorectal cancer
•
Associated conditions = colorectal adenomas and serrated polyps.
o IBD (chronic inflammation → hyperplasia → non-polypoid dysplasia → neoplasia).
(↑risk esp. w/ UC and PSC)
o DM-2
o Endocarditis from S.Gallolyticus
•
Lifestyle = smoking, alcohol
•
Diet = obesity, processed meat, high-fat and low-fiber
o Protective factors: long term use of NSAIDs, aspirin; physical activity, diet
Classification = proximal (caecum, ascending and transverse colon) and distal (descending and
sigmoid colon, rectum)
Most common type is adenocarcinoma w/4 types = polypoid, ulcerous, solitary, and infiltrative. Less
common types include = mucinous adenocarcinoma; signet ring cell, small cell, and Adenosquamous
carcinomas
Clinical manifestations
•
Often times asymptomatic, particularly during the early stages
•
Constitutional symptoms = weight loss, fever, night sweats, fatigue, abdominal discomfort
(symptoms similar to diverticulitis, especially in carcinoma of the rectosigmoid and descending
colon)
•
Symptoms of R side carcinomas (cecum, ascending, and transverse colon) = occult
bleeding/melena, IDA (due to chronic bleeding), diarrhoea, mostly exophytic mass
o IDA in >50y men/post-menopausal women – think of CRC!
•
Symptoms of L side carcinomas (splenic flexure, descending and sigmoid colon, rectosigmoid
junction) = changes in bowel habits (size, consistency, frequency), blood-streaked stools
(visible/occult), colicky abdominal pain (due to obstruction), mostly infiltrating mass
o Bowel obstruction is the earliest sign due to smaller lumen and more solid fecal matter
on L side of colon
•
Symptoms of rectal carcinomas = hematochezia (passage of bright red, fresh blood in or
w/stools), ↓ stool calibre (pencil-shaped), rectal pain, tenesmus (urge to empty the
rectum/bladder), flatulence w/involuntary stool loss, fecal incontinence (involuntary).
o Consider CRC in any patient with Hematochezia!
•
Symptoms of advanced disease = palpable abdominal mass, intestinal obstruction or
perforation
•
Metastasis to liver (abdominal distension, hepatomegaly, RUQ pain, ascites, jaundice), or
lung (dyspnoea, cough, hemoptysis, pleural effusion). Less commonly to peritoneum w/ worse
prognosis (ascites, ab distension, diffuse ab pain, bowel obstruction). Rarely – Virchow node
(supraclavicular lymph node)
Diagnosis
Initial work-up
•
Digital rectal examination (with LGI symptoms) = distal rectal cancers are palpable
•
Complete colonoscopy (gold standard) + biopsies
o
o
Ulceroproliferative friable mass
Alternatives: CT colonography, capsule endoscopy
•
Flexible sigmoidoscopy +/- anoscopy: who are <40yrs, no RF’s/ red flags for CRC.
o Rule out hemorrhoids, fissures
•
Double-contrast barium enema (uncommon) = only if colonoscopy is incomplete. Shows
characteristic apple core lesion = a filling defect due to constriction of the colonic lumen by a
stenosing colon carcinoma
Staging and additional tests
•
Staging = endorectal US (depth of tumour), CT (abdomen, pelvis, and chest), MRI, PET-CT
•
Labs: CEA, CBC (IDA)), LFT’s (abnormal if metastasized)
•
Prognostic monitoring via carcinoembryonic antigen (CEA) = tumour marker – monitor levels
during course of treatment and the follow-up period to evaluate treatment response and
recurrence. Not useful in screening. Can also use CA19-9
AJCC staging for CRC
TNM
0
Tis, N0, M0
I
Up to T2, N0, M0
II
Up to T4, N0, M0
III
Any T, N1/N2, M0
IV
Any T, any N, M1
Description
Tumor in situ – no invasion
Tumor invasion
•
T1: submucosa
•
T2: muscularis propria
•
T3: subserosa
•
T4a: visceral peritoneum
•
T4b: adjacent tissue or organs
Regional LN involvement
•
N1: 1-3 LN
•
N2: 3-7 LN
Distant metastases
•
M1a: affecting only one organ or site
•
M1b: affecting more than one organ or site
•
M1c: peritoneal metastases (regardless of
metastasis to other organs)
Treatment
Treatment mainly depends on the location of the tumour and the TNM stage.
•
Curative approach = any primary tumour w/ or w/out regional spread; treatment involves
surgical resection and adjuvant chemo
•
Palliative approach = distant metastasis beyond the liver and/or lung; patient is not a surgical
candidate due to poor general health; treatment involves palliative chemo and palliative
surgery (to manage complications of the primary tumour such as obstruction)
Surgery options
•
Colon cancer
o Types
R hemicolectomy = Resection of part of the distal ileum, the ileocecal valve,
cecum, ascending colon, hepatic flexure, and proximal third of the transverse
colon w/end-to-end/end-to-side ileocolonic anastomosis. T in cecum/ascending
colon
Extended RHC RHC + transverse colon w/end-to-end/end-to-side
ileocolonic anastomosis. T = in proximal/middle transverse colon
L hemicolectomy = distal 1/3 of the transverse colon, the splenic flexure,
descending colon, and sigmoid colon. Perform a colorectal anastomosis.
Sigmoid colectomy
Transverse colectomy
Total abdominal colectomy = indicated for hereditary and multifocal carcinomas
o
Stages
I Curative surgery
II, III Curative surgery + Adjuvant chemotherapy
•
IV Neoadjuvant chemo, if Resectable: CS +AC; Unresectable: palliative
chemo/surgery
Rectal cancer =
o
o
Types
Transanal excision (early, localised disease- Stage I),
Low ant. resection (locally advanced disease; Stage II-III): Sphincter-preserving
resection of the rectum and sigmoid/ Total mesorectal excision
Abdominoperineal resection – Stage IV (if the distal margin to the rectum
cancer is < 2-5 cm to the anus – resection of rectum, sigmoid, and anus)
Stages
I Curative surgery
II, III Neoadjuvant chemo and/or radiotherapy, Curative surgery, Adjuvant
chemotherapy, consider adjuvant radiotherapy
IV Neoadjuvant chemo, if Resectable: CS +AC/AR; Unresectable: palliative
chemo/surgery
•
The surgery option depends on the blood supply. Before resection, the arteries have to be
ligated. Also surrounding lymph nodes must be removed as they are near the blood supply.
•
Regional lymph node dissection
•
Resection of metastases in the liver and/or lung
•
Palliative surgery = intestinal bypass (ileocolonic anastomosis, colostomy), enteral stenting,
resection, colostomy
Systemic therapy
•
Chemotherapy –
o
o
o
FOLFOX/FOLFIRI (FOLinic acid + 5-FU + OXaliplatin or IRInotecan);
CAPOX (CAPecitabine + OXaplatin).
Radiotherapy is not standard treatment choice in colon cancer due to adverse effects
on the SI, leading to enteritis and strictures.
•
Rectal cancer = neoadjuvant radio (locally advanced disease), adjuvant and palliative chemo
•
Biological treatment: anti-VEGF AB: Bevacizumab; EGFR AB: Cetuximab
144) Liver tumors
Benign tumours of the liver
Definition = abnormal growth of neoplastic cells on or in the liver
Classification
•
Hepatic/cavernous haemangioma (most common) = composed of endothelium-lined bloodfilled sinuses
•
Focal nodular hyperplasia (FNH)
•
Hepatocellular adenoma (rare) = benign proliferation of hepatocytes in the context of a normal
liver
Epidemiology
•
Usually F>M
•
Most often an incidental finding on imaging tests
•
Haemangioma at 30-50 years; FNH at any age (usually 30-40 in F; later in M); adenoma at
15-45
Etiology
•
Haemangioma = possible hormonal component; oestrogen therapy associated w/↑ growth
•
FNH = mostly unknown
•
Adenoma = oral contraceptives and anabolic steroids
Clinical manifestations
•
Usually asymptomatic
•
Large masses (especially adenoma) may present w/abdominal pain, fullness, N/V
•
Could cause abnormalities in liver function
Pathology
•
Haemangioma = epithelium-lined blood-filled spaces separated by fibrous septa
•
FNH = contains cords of benign-appearing hepatocytes divided by multiple fibrous septa
originating from a central scar. The central scar often contains large a. that branches out into
multiple smaller aa. in a spoke wheel pattern
•
Adenoma = composed of cords of benign hepatocytes containing ↑ glycogen and fat.
Haemorrhage and necrosis are commonly seen
Diagnosis
US (best initial test) = haemangioma is seen as well-defined hyperechoic lesions; FNH has variable
appearance of scar and nodular lesions; adenoma is seen as a solitary, well demarcated,
heterogeneous mass
Other imaging (to differentiate between the different types and reach a definitive diagnosis) =
contrast-enhanced CT, MRI, biopsy to confirm diagnosis (contraindicated in haemangioma as it may
cause bleeding)
Treatment
•
Conservative treatment is often sufficient for hemangioma and FNH
•
Surgical resection if symptomatic and/or complications arise
•
For adenoma = discontinue oral contraceptives; surgical resection in all M and for
symptomatic F w/tumour >5 cm because of ↑ risk of rupture, bleeding, or malignant
transformation.
Complications = risk of malignant transformation, and rupture and bleeding (adenoma)
Liver cancer
Definition = malignant neoplasms of the liver. 5th most common malignancy worldwide; M>F; highest
incidence in SE Asia and Africa.
Classification
Primary malignant tumours = hepatocellular carcinoma (HCC) (75%), intrahepatic cholangiocellular
carcinoma (CCC) (2nd most common), hepatic angiosarcoma
Secondary tumours/metastatic liver tumours = very common since the liver is usually the 1st site
of metastatic disease. Typical primary tumour site = GI (colon, stomach, pancreas), lungs, and breast
Etiology
HCC
•
Liver cirrhosis (80%)
•
Risk factors independent of cirrhosis = chronic hep B/C, alcoholic liver disease, NASH,
hemochromatosis, Wilson’s disease, α-1 antitrypsin deficiency, glycogen storage disease,
chronic ingestion of food contaminated w/aflatoxin (carcinogen produced by Aspergillus
flavus) – leads to inactivating mutation of TP53 gene
CCC = associated w/primary sclerosing cholangitis, parasitic biliary infestation, and choledochal cysts
Clinical manifestations
•
Usually asymptomatic apart from symptoms of underlying disease (mostly cirrhosis or
hepatitis)
•
Possible symptoms of advanced disease = weight loss/anorexia, hepatomegaly and RUQ
tenderness (caused by distention of the hepatic capsule), jaundice, ascites.
•
Metastasis (hematogenous) = rare, usually occurs in advanced stages – lungs, abdomen,
bones)
Diagnosis
Labs
•
↑ Serum α-fetoprotein (AFP) = in patients w/cirrhosis or chronic hepatitis, AFP is used as a
screening test for HCC
•
Lab studies consistent w/hepatitis and cirrhosis (↑ transaminases, +ve hepatitis serologies, ↓
coagulation factors)
•
Paraneoplastic syndromes = ↑ RBC (due to tumour EPO production), hypoglycaemia,
hypercalcaemia
Imaging
•
US (best initial test) = irregular mass borders; variable echogenicity; vascular invasion of the
tumour and underlying cirrhosis may be visible
•
Abdominal CT/MRI (w/contrast) (confirmatory test) = hypodense lesions; irregular mass
borders; possible local invasion
•
Chest CT = detection of pulmonary metastases (rare)
•
Bone scintigraphy = detection of bone metastases (rare)
Biopsy = can provide definitive diagnosis but carries risk of bleeding and tumour spread.
Treatment
Curative options = potentially for patients w/retained liver function
•
Surgical resection
•
Liver transplant = waiting time depends on donor availability. Bridging methods used to
prevent tumour progression include downsizing w/ablative therapies and chemoembolisation
•
Ablative therapies (mostly palliative, but can also be curative) result in shrinking and scarring
of the tumour
Radiofrequency ablation (RFA) = catheter placed w/in the tumour to induce heat
necrosis via pulsed release of high-frequency waves
Transcatheter arterial chemoembolisation (TACE) = local application of chemo and
embolic agents
Percutaneous ethanol injection
Selective internal radiation therapy
Follow-up = vaccination against HBV in high-risk individuals; surveillance w/US in patients
w/cirrhosis or chronic hep B
Palliative care = primarily for decompensated disease, unresectable, multinodular disease, or
metastatic disease.
Complications = Budd-Chiari syndrome (hepatic v. obstruction that leads to hepatomegaly, ascites,
and abdominal discomfort) – when the tumour compresses the hepatic vv., leading to obstruction of
the blood outflow and thus hepatic congestion
145) Pancreatic cancer
Definition = malignant neoplasm of the pancreas. It is the 4th leading cause of cancer deaths in the
USA and typically affects older individuals (60-80 years). High risk groups include African-Americans
and Ashkenazi Jewish descent.
Etiology
Exogenous risk factors = smoking, chronic pancreatitis, high alcohol consumption, DM2, obesity,
occupational exposure to chemicals, possibly infections w/H. pylori or HBV.
Endogenous risk factors = age >50 years; inherited genetic syndromes (10% of pancreatic
cancers) – familial atypical multiple mole melanoma syndrome, hereditary breast and ovarian cancer
syndrome, Lynch syndrome, NF type 1, MEN1, hereditary pancreatitis.
Clinical manifestations
Asymptomatic in early stages
General = poor appetite, weight loss, weakness
GI symptoms
•
Belt-shaped epigastric pain which may radiate to the back
•
N/V
•
Malabsorption, diarrhoea (possible steatorrhoea secondary to exocrine pancreatic
insufficiency)
•
Jaundice caused by obstruction of extrahepatic bile ducts (especially in tumours of the
pancreatic head) = Courvoisier sign (enlarged, non-tender gallbladder and painless jaundice);
pale stools, dark urine, and pruritus
•
Impaired glucose tolerance (rarely)
Hypercoagulability
•
Trousseau syndrome = super. thrombophlebitis – recurring thrombophlebitis in changing
locations (migratory); red, tender extremities; classically associated w/pancreatic cancer
•
Thrombosis (e.g. phlebothrombosis, splenic v. thrombosis)
Metastases (lymphogenic and hematogenous) = often already present at time of diagnosis; early
stage in nearby lymph nodes and liver; late stage in surrounding visceral organs (duodenum,
stomach, colon) and lungs
Diagnosis
•
Tumour markers to monitor progression of cancer and treatment efficacy = CA 19-9, CEA (<
specific)
•
Abdominal US (1st test) = if US reveals a pancreatic mass → contrast-enhanced CT; poorly
defined, hypodense and hypovascular mass; Double-duct sign (w/↑ size, tumours of the
pancreatic head may block bile drainage in both the common bile and pancreatic ducts,
leading to dilatation of both structures)
•
ERCP/MRCP = to rule out choledocholithiasis; to assess if biliary decompression is indicated
•
Endoscopic US = when other tests are inconclusive
•
Fine needle aspiration (can be done via endoscopic US or percutaneously) = help differentiate
cancer from pancreatitis
DDx = pancreatic cyst, pancreatitis, pancreatic pseudocyst, metastasis (breast)
Pathology
Location = pancreatic head (65%), pancreatic body and tail (15%), diffuse (20%)
Pancreatic exocrine tumours (95% of tumours) = ductal adenocarcinoma (most common); less
common = acinar adenocarcinoma (acinar cells produce digestive enz.), mucinous
cystadenocarcinoma
Pancreatic endocrine tumours (neuroendocrine tumours/NET) = insulinomas (result in
hypoglycaemia), glucagonomas, somatostatinomas, gastrinomas, VIPomas, pancreatic polypeptidesecreting endocrine tumours
Treatment
The only curative option is surgical resection. If surgery is not possible or distant metastasis is
present, a palliative approach is chosen.
Pancreatic head carcinoma
•
Pancreaticoduodenectomy (Whipple procedure) = resection of pancreatic head, distal
stomach, duodenum, gallbladder, and common bile duct
•
Lymphadenectomy
•
4 anastomosis = gastrojejunostomy, pancreaticojejunostomy, hepaticojejunostomy (common
bile duct to the jejunum), and enteroenterostomy (between the afferent and efferent jejuna
loop). The blind prox. end of the jejunum is closed.
• Pylorus-preserving pancreaticoduodenectomy (Traverso-Longmire procedure)
Pancreatic body and tail carcinoma
•
Resection of the L side of the pancreas w/splenectomy
•
In some cases, duodenopancreatectomy w/splenectomy (if partial removal of the pancreas is
insufficient)
Palliative approach (patients w/advanced/metastatic cancer)
•
Palliative chemo
•
Pain management = analgesia according to WHO step-by-step plan; radiotherapy (patients
w/symptomatic metastasis; celiac ganglion block
•
Management of GI complications = cholestasis (ERCP w/stent implantation, percutaneous bile
duct drainage), gastric outlet stenosis (gastroenterostomy), ileus (percutaneous endoscopic
gastrostomy tube), cachexia (nutrition counselling)
146) Carcinoma of the biliary duct
Cancer of the biliary system/Cholangiocarcinoma [Rare]
• Originates in the bile ducts and are classified based on their anatomical site of origin
• It can occur at any site along the biliary tree, although predominantly arises in the extrahepatic
biliary system.
• The most common site for bile duct cancers is at the bifurcation of the right and left hepatic
ducts (Klatskin tumors).
• Slow-growing and invades locally and metastases to local lymph nodes, before spreading
distally to the peritoneal cavity, lung and liver.
• Genetics – KRAS, p53
RF:
• Primary sclerosing cholangitis
• Ulcerative colitis
• Infective – liver flukes, HIV, chronic hepatic virus
• Toxins – chemicals in rubber and aircraft industry
• Congenital – choledochal cyst, Caroli’s disease
• Cirrhosis
• Choledocholithiasis – both with and without hepatic duct involvement
• Alcoholism
• DM
CF:
• Intrahepatic cholangiocarcinoma - generally ASx until a late stage in the disease, nonspecific
Sx – weight loss, nausea, fever, weakness, fatigue, dull abdominal pain (RUQ/epigastric)
• Extrahepaic cholangiocarcinoma - Post-hepatic jaundice, pruritus with pale stools and dark
urine, Courvoisier sign
• Physical Exam: jaundice, cachexia
• Courvoisier’s Law
o In the presence of jaundice and an enlarged or palpable gallbladder, malignancy of the
biliary tree or pancreas should be suspected
Dx:
• Biochemical investigations e.g. elevated Br, ALP and GGT – obstructive jaundice (parameters
of cholestasis)
• Liver FTs – possible INR, ALT and AST elevation – chronic biliary obstruction and eventual
hepatic dysfunction
• CEA, CA19-9 elevated
• Transabdominal US
•
•
•
•
•
MRCP – definitive Dx
ERCP – site of obstruction
Chest CT – staging of disease
Biopsy – only for cholangiocarcinoma
Angiography – pre-operative planning to image the hepatic arteries or portal vein
•
•
•
Complete surgical resection
Intrahepatic or Klatskin tumours – partial hepatectomy and reconstruction of the biliary tree
Extrahepatic or Distal common duct tumours – pancreaticoduodenectomoy (Whipple’s).
Regional lymphadenopathy
RT
Palliative = stenting via ERCP, surgery – bypass, medical – CT e.g. cisplatin and gemcitabine.
Transarterial chemoembolization – local application of CT
Tx:
•
•
Cx:
•
•
Increased risk of biliary tract sepsis
Secondary biliary cirrhosis
147) Tumor of the thyroid gland
Thyroid cancer arises from either the thyrocytes or the parafollicular cells of the thyroid gland. It is
more common in women, especially between 30–50 years of age.
Risk factors for thyroid cancer are a
1. history of childhood irradiation to the head and neck papillary carcinoma
2. a family history of thyroid cancer. (Genetic factors)
Papillary carcinoma is the most Prevalent type of thyroid cancer, it features Palpable lymph nodes,
and it has the best Prognosis compared to all other types of thyroid cancer.
Benign thyroid nodules (∼ 95% of cases)
Thyroid adenomas
1. Follicular adenoma (most common)
2. Hürthle cell adenoma
3. Toxic adenoma
4. Papillary adenoma (least common)
Thyroid cysts
Dominant nodules of multinodular goiters
Hashimoto thyroiditis
Malignant thyroid nodules (∼ 5% of cases)
Types:
1. Thyroid carcinoma
2. Thyroid lymphoma
3. Metastatic cancer from breast/renal carcinoma (rare)
In addition to red flags for thyroid cancer, a solid nodule on thyroid ultrasound or a cold
nodule on thyroid scintigraphy should raise suspicion for thyroid cancer
CLINICAL FEATURES:
Thyroid carcinoma may be asymptomatic (e.g., thyroid incidentaloma) or manifest with any or all of
the following clinical features:
1) Thyroid nodule
o Firm to hard consistency
o Typically, painless - larger nodules may be painful or cause a globus sensation.
2) Features of local infiltration or compression
o Fixed thyroid nodule - I.e., the nodule does not move with deglutition. This indicates
infiltration into adjacent tissue.
o Recent onset of any of the following:
1* Hoarseness of voice (vocal cord paresis)
2* Dyspnea
3* Dysphagia
4* Horner syndrome (rare)
5* Venous obstruction (very rare): IJV thrombosis, SVC syndrome
3) Painless cervical lymphadenopathy
o More common in papillary thyroid cancer and anaplastic thyroid cancer
4) Signs of distant metastasis
o More common in follicular thyroid cancer and anaplastic thyroid cancer
o Examples include:
i. Pulmonary metastases: coughing, hemoptysis, dyspnea
ii. Bone metastases: bone pain, pathologic fractures
iii. Brain metastases: focal neurologic deficit, seizures
5) Paraneoplastic syndrome: diarrhea and facial flushing
=>(typically seen in advanced medullary carcinoma)
DIAGNOSTICS
Laboratory studies and ultrasound
Serum TSH and ultrasound should be obtained in all patients with thyroid nodules.
1- TSH : typically normal or mildly elevated
2- Thyroid ultrasound: to assess for sonographic signs of thyroid malignancy;
o Solid or mostly solid hypoechoic nodule(s)
o Irregular margins
o Microcalcifications within nodules
o Nodules that are taller than wide
o Extrathyroidal growth => Signifying growth unrestricted by anatomic planes
Ultrasound alone cannot confirm malignancy but guides the decision of whether to obtain cytology via
FNAC.
Thyroid Scintigraphy
Indications
1. Thyroid nodule(s) with ↓ TSH levels
2. Multinodular thyroids (to identify nodules that require FNAC) 3. Prior to RAIA to evaluate eligibility for adjuvant treatment of well-differentiated thyroid cancer
Contraindications: pregnant and breastfeeding women
Supportive findings: decreased or no radiotracer uptake (i.e., hypofunctioning or nonfunctioning
nodules, referred to as cold nodules)
➢ Nodules that appear hypoechoic on thyroid ultrasound and cold on thyroid scintigraphy should
increase suspicion for malignancy
➢ Hyperfunctioning nodules (hot nodules) are rarely malignant and typically do not require
further evaluation for malignancy.
Fine-needle aspiration cytology (FNAC)
Indications: sonographic signs of thyroid cancer
Intraoperative frozen-section: Consider if FNAC cannot reliably rule out malignancy in high-risk
patients.
ADDITIONAL STUDIES AFTER CONFIRMED DIAGNOSIS
Thyroid cancer tumor markers
The specific tumor markers depend on the histological type of the cancer.
A. Follicular or papillary thyroid cancer
Thyroglobulin (Tg): precursor of thyroid hormones; produced exclusively by the thyroid gland
o Indicated after total thyroidectomy or RAIA therapy
B. Medullary carcinoma
Calcitonin: A hormone secreted by parafollicular cells, which is the tissue of origin of medullary
carcinoma
o Indicated preoperatively if FNAC is suspicious for medullary carcinoma (supportive
diagnostic marker) Very high calcitonin levels before total thyroidectomy or RAIA may
indicate metastatic disease.
o Used to monitor response to therapy
Carcinoembryonic antigen (CEA): nonspecific marker, used in combination with calcitonin to monitor
response to therapy
Elevation of tumor markers after total thyroidectomy or RAIA indicates persistent disease,
recurrence, or metastasis.
STAGING includes
I. Preoperative assessment of cervical lymph nodes
1* Neck ultrasound in all patients with confirmed diagnosis
2* FNAC of lymph nodes with signs of metastases
II. Assessment of distant metastases: based on clinical suspicion
1* Chest x-ray or CT
2* Bone scintigraphy
3* CT or MRI head -> In anaplastic carcinoma, to assess for brain metastases.
Pathology – not included
DDx:
• Thyroid nodules
• Thyroid Cyst anechoic round mass
TREATMENT
a) Surgical
i.
Well-differentiated thyroid cancer
• Standard management (regardless of nodal or distant metastases): total thyroidectomy
(with neck dissection as needed) + RAIA + TSH suppression therapy
• Small cancers without nodal or distant metastases: Consider hemithyroidectomy +
TSH suppression therapy.
• Papillary microcarcinoma in low-risk patients I.e., Patients with no risk factors for
tumor recurrence (e.g., age > 45 years, no family history of thyroid cancer, no history
of head and neck irradiation): Consider active surveillance.
ii.
Poorly-differentiated thyroid cancer
• Medullary carcinoma: total thyroidectomy+ neck dissection ± radiation therapy and/or
systemic chemotherapy as needed.
• Anaplastic carcinoma
o Resectable cancer: total thyroidectomy + neck dissection + radiochemotherapy
o Unresectable or metastatic cancer: palliative care
• Thyroid hormone replacement will be required after total thyroidectomy.
Complications of surgery
1) Hypocalcemia: as a result of accidental removal of parathyroid glands
2) Dysphonia (hoarseness) and/or dysphagia: as a result of transection of the superior
and recurrent laryngeal nerve
b) ADJUVANT THERAPY
i. Well-differentiated thyroid cancer
• Radioactive iodine ablation (RAIA): conducted 4– 6 weeks after total thyroidectomy to
destroy remaining thyroid tissue or metastases
• Only differentiated thyroid carcinomas take up iodine; for this reason, only they
respond to radioiodine therapy. Thyroid scintigraphy is recommended before RAIA to
identify which patients are likely to benefit
• TSH suppression therapy:
o Administration of L-thyroxine to suppress serum TSH to subnormal levels to
minimize the risk of tumor recurrence
o Administered after completion of RAIA in patients who have undergone total
thyroidectomy
o L-thyroxine also serves as hormone replacement therapy after surgery and RAIA.
ii. Poorly differentiated thyroid cancer:
o adjuvant radiation therapy and/or chemotherapy as needed
c) NONOPERATIVE MANAGEMENT
• Active surveillance
o Papillary microcarcinoma (i.e., < 1 cm) with no nodal or distant metastasis in low-risk
patients
o Multimorbid patients with high surgical risk or short life expectancy
• Palliative therapy: Palliative radiation therapy and/or chemotherapy may be considered
for advanced anaplastic thyroid cancer (transcutaneous gastrostomy for esophageal
obstruction, tracheostomy for airway compression, and palliative thyroidectomy for symptom
control.
FOLLOW UP:
● Physical exam.
● Biochem. Tests - E.g., tumor markers such as thyroglobulin for differentiated thyroid cancers
● Neck US
● Further imaging id relapse is suspected E.g., iodine-123 or iodine-131 scintigraphy in
papillary/follicular malignancies while pausing thyroid hormone therapy
PROGNOSIS – 5yr survival rate:
• Papillary - >90%
• Follicular – 50-70%
• Medullary – 50 %
• Anaplastic – 5-14%
• OTHER SUBTYPES/VARIANTS
1) Hurthle cell carcinoma
a. 3–10% of all well-differentiated thyroid cancers
b. Often classified as subtype of follicular carcinoma
2) B-cell lymphoma: usually develops from Hashimoto thyroiditis
3) Sarcoma: rare
4) Metastatic (e.g., breast, renal, melanoma): rare
X.Principles of Treatment
148) Treatment of peptic diseases of the gastrointestinal tract
Therapeutic approach
Clinical scenario
Management
All patients
Nonpharmacological measures: E.g., avoid NSAIDs, restrict
alcohol.
Follow-up to confirm treatment success and possibly endoscopic
surveillance (see “Follow-up” for more details)
H.pylori +ve
(test and treat strategy)
H. pylori eradication therapy with antibiotics and a PPI
Continue acid suppression medication (i.e., PPIs) for 4–8 weeks.
H.pylori -ve
Trial of acid suppression medication (i.e., PPIs) for 4–8 weeks,
followed by reevaluation
Medically refractory symptoms
Consider elective surgery.
Inability to tolerate or adhere to
medical treatment
Confirmed upper GI malignancy
•
Complications
Active bleeding: hemodynamic support (e.g., transfusion)
and urgent endoscopy with possible subsequent surgery
(see “GI bleeding”)
•
Perforation: empiric antibiotics for intraabdominal infection
and urgent surgery consult (see “Secondary peritonitis”
and “Gastrointestinal perforation”)
•
Subhepatic abscess, fistulas, or gastric outlet obstruction:
See “Complications.”
MEDICAL TREATMENT OF PUD
•
Pharmacologic therapies for uncomplicated PUD include a trial of acid suppression therapy
and, if H. pylori is detected, eradication therapy. These may be complemented with antacids
for rapid symptom relief, and in some cases with cytoprotective agents for mucosal
protection. All patients should also be counseled on lifestyle and risk factor modification.
Acid suppression medications and antacids
•
Acid suppression:
o PPIs- Omeprazole: 20-40 mg/day
o Pantoprazole: 40mg/day
Decrease acid production in the stomach by irreversibly inhibiting
hydrogen/potassium ATPase. Adverse effects: Osteoporosis (long term use),
micronutrient malabsorption (iron deficiency, B12 def.), CYP 450 inhibition.
Onset of action: 2-6 hours after administration. Takes 2-5 days for gastric acid
secretion to return to normal levels once the drug has been discontinued. PPIs
should be administered before taking a meal and the PPIs may interfere with
absorption of drugs such as Ketoconazole, Ampicillin and Digoxin.
H2 receptor blockers –
Ranitidine(300mg),
o
●
Famotidine (40mg/day)
Cimetidine (800mg)
SI-reversible gynecomastia, impotence, increase aminotransferases
o Antacids:
Calcium carbonate, Magnesium hydroxide, Aluminum hydroxide
Neutralize acid: mainly used w/ acid suppression for rapid symptom relief
Recommended duration of acid suppression for PUD
○ Duodenal ulcers: ≥ 4 weeks
○ Gastric ulcers: ≥ 8 weeks
○
○
Unknown location: Consider 8 weeks of empiric treatment.
Select patients (e.g., those with idiopathic ulcers) may benefit from maintenance acid
suppression therapy to prevent recurrence.
●
Antibiotics: e.g., clarithromycin triple therapy (combined with amoxicillin and a PPI). See “H.
pylori eradication therapy” for other treatment regimens.
●
Cytoprotective agents (gastrointestinal mucosal protection)
○ Sucralfate: a sucrose sulfate-aluminum complex that reacts with HCl in an acidic
environment to create a protective barrier over the gastric/duodenal mucosa
■ Acts as an acid buffer and promotes HCO3 production
■ Mostly used to promote ulcer healing in patients with duodenal ulcers
■ Should not be taken simultaneously with a PPI or H2 blocker
○ Misoprostol: used for PUD prevention for frail/elderly patients taking NSAIDs that
cannot he discontinued
○ Bismuth-bismuth subsalicylate, bismuth subcitrate
Bismuth does not inhibit or neutralize gastric acid. The most dramatic action of bismuth
salts is the suppression of H. pylori and other actions that promotes ulcer healing.
●
Nonpharmacological measures
○ Restrict alcohol, smoking, and caffeine, and avoid stress.
○ Avoid medications that may cause or worsen PUD (e.g., discontinue NSAIDs, reduce
or stop corticosteroids if possible).
○ Avoid eating before bedtime.
149) Treatment of Helicobacter pylori infection
Before you prescribe check if patient is allergic to Amoxicillin, did the patient take macrolide before?
(think of resistance)
Giving probiotics doesn’t help in eradication but they decrease the side effects of the medication.
New therapeutic approaches: 5 days of amoxicillin with PPIs followed by 5 days of PPIs, Tinidazole
and Clarithromycin
First-line options for H.pylori eradication therapy
Clarithromycin triple therapy
Preferred in areas with low levels (< 15%) of
•
clarithromycin resistance
•
PPIs at standard or double dose twice
daily (e.g., omeprazole: 20-40mg/12hrs)
PLUS clarithromycin 500mg/12hrs
•
PLUS amoxicillin (1g/12hrs) OR
metronidazole (500mg/8hrs)
Clarithromycin-based concomitant therapy
Bismuth quadruple therapy
Preferred in areas with high levels (≥ 15%) of
clarithromycin resistance.
•
Duration: 14 days
•
PPIs at standard dose twice daily (e.g.,
omeprazole)
•
PLUS clarithromycin
•
PLUS amoxicillin
•
PLUS metronidazole OR tinidazole
(500mg/12hrs)
•
Duration: 10–14 days
•
PPIs at standard dose twice daily (e.g.,
omeprazole)
•
PLUS bismuth (e.g., bismuth subcitrate:
420mg/6hrs OR bismuth subsalicylate)
•
PLUS tetracycline (500mg/6hrs)
•
PLUS metronidazole
•
Duration: 10–14 days
Triple therapy:
1. Omeprazole: Standard dose or double dose. 20-40 mg every 12 hrs
2. Clarithromycin: 500 mg PO/12 hrs
3. Amoxicillin: 1 g PO/12 hrs OR Metronidazole: 500 mg/8 hrs
Quadruple therapy:
1. PPI standard dose 20 mg every 12 hrs
2. Bismuth salicylate 525 mg PO every 6 hrs or Bismuth substrate 420 mg PO every 6 hrs
3. Tetracycline 500 mg PO every 6 hours
4. Metronidazole 250-500 mg PO every 6-8 hrs
Second-line treatment options
● Choose different antibiotics to those used as first-line therapy.
● Bismuth quadruple therapy: if first-line clarithromycin triple therapy was unsuccessful
● Levofloxacin-containing therapy: e.g., levofloxacin triple therapy
○ PPIs at standard dose twice daily (e.g., omeprazole)
○ PLUS levofloxacin (500mg/24hrs)
○ PLUS amoxicillin
○
Duration: 10–14 days
Follow-up: Confirm H.pylori eradication
● Confirm that H. pylori has been eradicated 4–6 wks after completion of the treatment regimen.
● Preferred modalities: Urea breath test, stool antigen test, or biopsy
● Stop PPIs at least 2 weeks before the urea breath test is performed for accurate results.
● Serology is not recommended to confirm eradication, as H. pylori antibodies may still be
present for weeks or months after eradication.
● Acid suppression medication can be discontinued once eradication is confirmed
150) Principles in treatment of chronic liver disease
Chronic liver disease is a progressive deterioration of liver functions for > 6 months, which includes
synthesis of clotting factors, other proteins, detoxification of harmful products of metabolism and
excretion of bile.
It is a continuous process of inflammation, destruction and regeneration of liver parenchyma which
leads to fibrosis and cirrhosis.
Treatment goal is to STOP the progression of the disease and complications and require a
multidisciplinary approach. The principle of management is mainly underlying cause correction,
Portal hypertension management, and specific treatments for individual disease.
Etiology of chronic hepatitis:
•
Alcoholic Liver Disease
•
Non-alcoholic Fatty Liver Disease (NAFLD/NASH)
•
Chronic Viral Hepatitis: HBV, HCV
•
Genetic Causes-Alpha-1 antitrypsin deficiency, Hereditary hemochromatosis, Wilson disease
•
Autoimmune Causes-Primary biliary cirrhosis, Primary Sclerosing Cholangitis, Autoimmune
hepatitis.
•
Other Causes of Chronic Liver Diseaseo Drugs - amiodarone, isoniazid, methotrexate, phenytoin, nitrofurantoin.
o Vascular - Budd-Chiari syndrome.
o Idiopathic/cryptogenic: around 15%
General principles:
•
Lifestyle changes: Avoid alcohol, optimize diet, encourage physical activity
•
Avoid hepatotoxic drugs (e.g., NSAIDs and aspirin) & adjust dosage for certain drugs
•
Vaccinations: Vaccination against hepatitis A and B virus infection for those who are not
already immune can help prevent superimposed insults to the liver. Other vaccinations, such
a yearly influenza vaccination, are also recommended
•
Hepatoprotectors: silymarin
•
Identify and treat the underlying cause of chronic liver disease
•
Treat cirrhosis and its complications
•
Liver transplant
Patients with chronic liver disease mostly present with one of the complications:
•
Esophageal varices,
•
Hepatic encephalopathy and
•
Hepatorenal syndrome. (Look at Q 152 for treatments for this)
Hepatocellular carcinoma (HCC) - Treatment is based on the Barcelona clinic liver cancer
staging system in the management of HCC:
•
Initial stage (single HCC lesion): Resection and ablation.
•
Intermediate stage: Trans arterial chemoembolization and radio-embolization.
•
Metastatic disease: Sorafenib
SPECIFIC TREATMENT
Viral Hepatitis (Look at Q. 151)
•
Continuous viral suppression with nucleoside and nucleotide analogs
•
Direct-acting antivirals achieving HCV eradication
•
Interferon-alpha
Alcoholic liver disease:
•
Immediate cessation of alcohol use
•
In some cases, glucocorticoids (e.g., prednisolone in severe disease)
Non-alcoholic fatty liver disease: Treatment of metabolic syndrome components
•
Therapy
o
o
o
o
Weight loss, optimization of diabetic treatment (Metformin)
Discontinue responsible medication
Studies suggest that ursodeoxycholic acid may have anti-inflammatory and antiapoptotic effects in the liver
Vitamin E may decrease oxidative stress and improve aminotransferase levels in
NASH patients.
Hereditary Hemochromatosis (primary hemochromatosis):
•
Therapeutic phlebotomy (first-line treatment)
•
Drug-induced iron chelation
o
o
•
Agents: deferoxamine, deferasirox, or deferiprone
Indication: particularly when phlebotomy is contraindicated, e.g., in cases of anemia,
severe heart disease, or difficult venipuncture
Dietary changes
o Diet low in iron
o Restriction of alcohol and vitamin C supplements
o Consumption of tea
Wilson’s diseaseGeneral management
•
Low-copper diet: avoid foods such as organ meats, shellfish, nuts, and chocolate
•
Liver transplantation in cases of fulminant liver failure
Medical therapy
•
Initial therapy: chelating agents
•
Penicillamine
•
Maintenance therapy: zinc salts
Alpha-1-antitrypsin deficiency: Liver transplant
Autoimmune hepatitis: Corticosteroids and other immunosuppressive drugs
•
Immunosuppressive medications
o
o
Induction therapy
First-line: Prednisone with or without Azathioprine
Second-line: Mycophenolate, Cyclosporine, Tacrolimus
Maintenance therapy: low doses of Azathioprine or Prednisone
Primary Biliary Cirrhosis (PBC):
•
No cure: treatment consists of slowing disease progression and alleviating symptoms;
•
Liver transplant is the only definitive treatment
•
Symptomatic =
o
o
•
1st line= Ursodeoxycholic acid/ Ursodiol (slows disease progression + improves clinical
symptoms; delayed need for transplantation); treatment of pruritus
2nd line= Obeticholic acid (inhibits cholesterol synthesis)
Liver transplant necessary if liver cirrhosis is advanced
Primary Sclerosing Cholangitis: Transplant
•
Symptomatic: Ursodeoxycholic acid + Tacrolimus (immunosuppressive, which may ↓
cholestasis parameters: ALP, ASAT, ALAT, bilirubin).
o Doesn’t prevent disease progression
•
Treatment of pruritus (e.g., cholestyramine, rifampicin, naltrexone)
•
Supplementation of fat-soluble vitamins (ADEK);
•
In case of bile duct stenosis: ERCP w/duct dilation= potentially stent placement
•
Surgical = Liver transplantation is the only curative option; performed in case of advanced
liver cirrhosis
Budd-Chiari syndrome:
•
Anticoagulation,
•
Thrombolysis or
•
Angioplasty with or without stenting,
•
TIPS, or Liver transplant
151) Treatment of chronic viral hepatitis
TREATMENT FOR CHRONIC HBV AND HCV
Lifestyle changes: for both
•
Weight loss and diet
•
Cessation of substance use (including alcohol)
•
Discontinuation of hepatotoxic medication
Chronic hepatitis B (The diagnosis of chronic HBV infection is based upon the persistence of
hepatitis B surface antigen (HBsAg) for greater than six months)
1. Nucleoside/nucleotide analogs (NAs): Indicated in patients with both decompensated and
compensated liver disease and patients who do not respond to interferon treatment
o Tenofovir 300mg PO- is preferred due to:
High efficiency
Low rates of drug resistance
o Entecavir 0.5 mg daily
o Telbivudine, lamivudine 600mg, and adefovir 10mg are no longer preferred due to
(High rates of drug resistance, Lower antiviral potency, > severe side effects)
2. Pegylated interferon alfa (PEG-IFN-α): recombinant interferon alpha conjugated with
polyethylene glycol (PEG) with antiviral and antineoplastic properties.
•
Treatment duration: shorter than nucleoside/nucleotide analogue regimen
•
Contraindications for PEG interferon alfa:
o Decompensated cirrhosis
o Psychiatric conditions
o
Pregnancy
Liver transplantation indications
o End-stage liver disease due to HBV
o Fulminant hepatic failure (emergency transplantation)
If patient has concomitant HIV:
o The foundation of this therapy should be tenofovir (TDF or TAF) PLUS either
lamivudine or emtricitabine
Drug of choice in pregnancy:
o Tenofovir (Interferon therapy is contraindicated during pregnancy!)
Coinfection with HDV:
o PEG-IFN-α, Nucleoside/nucleotide analogs
Treatment of chronic Hepatitis C
There is neither a pre-exposure or postexposure prophylaxis nor a vaccine for HCV.
Treatment goals
•
Complete cure
•
Eradication of HCV RNA in serum as defined by sustained virologic response (SVR)
Treatment regimens
•
Chronic HCV infection is always treated with a multidrug approach (no antivirals are
approved as monotherapy).
•
Chosen based on the history of antiviral treatment, degree of liver fibrosis, viral genotype, and
viral load
•
Combination of two direct-acting antivirals (DAAs): Antivirals target and inhibit HCVencoded proteins that are essential for the HCV replication cycle.
o Ledipasvir PLUS sofosbuvir (genotypes 1, 4, 5, and 6) = HARVONI
o Sofosbuvir PLUS velpatasvir (all 6 genotypes) = EPCLUSA
o Elbasvir PLUS grazoprevir
o Glecaprevir PLUS pibrentasvir (all genotypes)
o Sofosbuvir PLUS daclatasvir
•
Interferon PLUS ribavirin
o
o
Interferon-based treatment is still used as a last resort in cases of treatment failure.
Can be used in the treatment of all genotypes
•
Ribavirin on its own may be combined with DAAs to increase antiviral effect. Interferon
and ribavirin are associated with severe adverse effects (e.g., arthralgias, thrombocytopenia,
leukopenia, depression, and anemia) and are teratogenic.
•
Vaccinations for hepatitis A and B should be given in addition to any treatment regimen.
Simplified Pangenotypic algorithm for the treatment of HCV
Elegibility criteria
Without
cirrhosis
•
•
•
•
Age > 18 years
Any genotype
No evidence
of cirrhosis
No previous
Regimens
•
•
Contraindications
Glecoprevir
PLUS pibrentasvir for
•
Concomitant HIV or HBV
infection
8 weeks
Sofosbuvir PLUS vel
patasvir for 12 weeks
•
Hepatocellular carcinoma
History of liver
transplantation
•
treatment
for HCV infection
•
With
compensated
cirrhosis
(Child-Pugh
class A)
•
•
•
Age > 18 years
Any genotype
No previous
treatment
for HCV infection
Evidence
of cirrhosis (see
“Diagnostics”
section in
“Cirrhosis”)
•
•
Genotype 16: glecaprevir PLUS
pibrentasvir for 8
weeks
Genotype 1, 2, 4, 5,
or
6: sofosbuvir PLUS
velpatasvir for 12
weeks
•
Pregnancy
•
Concomitant HIV or HBV
infection
Hepatocellular carcinoma
History of liver
transplantation
Pregnancy
Decompensated cirrhosis
ESRD
•
•
•
•
•
Treatment algorithm for patients with decompensated cirrhosis (Child-Pugh class B or C)
•
Refer to a medical professional with expertise and/or liver transplant center
•
Regimens
o
o
o
Ledipasvir PLUS sofosbuvir PLUS ribavirin for 12 weeks (genotype 1, 4, 5, or 6)
Sofosbuvir PLUS velpatasvir PLUS ribavirin for 12 weeks (all genotypes)
If ribavirin is contraindicated: administer the DAAs for 24 weeks
•
Interferon is contraindicated (high risk of worsening cirrhosis decompensation)
•
End stage liver failure: liver transplantation
152) Treatment of the liver cirrhosis complications: esophageal
varices, ascites, spontaneous bacterial peritonitis, hepato-renal
syndrome, encephalopathy
Esophageal varices
•
Resuscitation and stabilization
o Bring patient into shock position
o Place (at least) two peripheral venous catheters
o
o
o
o
o
•
Substitute crystalloids to maintain plasma volume
Intubate patient (with decreased consciousness) to prevent the possibility of aspiration
or airway obstruction
Place a stomach tube → helps to remove the blood
Intensive care monitoring
Transfuse blood or blood products to stabilize coagulation, if indicated
Medical therapy
o Octreotide for 3–5 days → inhibits secretion of vasodilative hormones, e.g., glucagon
→ indirect splanchnic vasoconstriction → reduces splanchnic blood flow
o Vitamin K is indicated for patients with coagulation disorders
o
•
Antibiotic prophylaxis for 7 days: prevention of infections (SBP, urinary tract
infection, pneumonia) and of septic complications due to bacteremia, as well as colon
decontamination to reduce ammonia production of gut flora
First-line: IV ceftriaxone
Alternative: oral ciprofloxacin
Endoscopic management
o
o
Erythromycin (a strong prokinetic agent) may be administered before gastroscopy.
Procedures
1. Endoscopic band ligation (procedure of choice)
•
Hemostasis
•
Used for primary prophylaxis and prevention of recurring hemorrhage
2. Alternative: Injection sclerotherapy, absolute alcohol, and fibrin glue, as well
as cyanoacrylate, to stop acute variceal bleeding
3. Balloon tamponade using a Sengstaken-Blakemore tube or Minnesota tube
•
Bleeding prevention
o Primary prophylaxis
Non-selective beta-blockers (e.g., propranolol, nadolol) - Medication to lower
portal pressure, irrespective of variceal grading.
Endoscopic esophageal variceal ligation: only indicated for patients with a
o
high risk of bleeding
Secondary prophylaxis
Combine endoscopic variceal ligation and medication (e.g., propranolol) to
reduce portal pressure for residual varices
If bleeding occurs despite secondary prophylaxis → placement of TIPS
Ascites
1. Treatment of cirrhosis, including sodium restriction, diuretics, and avoidance of certain
medications, such as NSAIDs and ACE inhibitors
2. Tense or large ascites: therapeutic paracentesis (first line); followed by diuretic therapy and
dietary sodium restriction
3. Refractory ascites o Consider the following treatment options:
a) Optimize medications and ensure adherence to a low-sodium diet.
b) Serial paracentesis (with IV albumin for large-volume paracentesis)
c) Evaluate for advanced therapies (e.g., TIPS, liver transplant).
•
Medical and supportive therapy
o
o
•
Salt and fluid restriction
Dietary sodium restriction: 2 g/day or 88 mEq/d (2 g of sodium = 5 g of salt)
Fluid restriction: 1 L/day (only if serum Na+ < 125 mEq/L)
Diuretics
Monotherapy with Spironolactone: 25mg x4/day may be preferable for newonset ascites, mild ascites, moderate ascites, and outpatients.
Combination therapy with spironolactone PLUS furosemide 20-80mg may be
preferable for recurrent gross ascites or when faster resolution of ascites is
required (e.g., in hospitalized patients).
Diuretics should be used w/ caution in patients w/ severe hyponatremia,
hepatic encephalopathy, and/or renal function deterioration.
Therapeutic paracentesis
o
Indications
Tense ascites (first line)
o
•
Refractory ascites (can be repeated every ∼ 2 weeks)
Malignancy-related ascites
Contraindications for diuretic therapy
Important considerations
Consider performing the procedure under ultrasound guidance to minimize the
risk of complications.
Administer albumin in patients undergoing large-volume paracenteses (> 5 L).
(8g/L)
Advanced therapies
o Liver transplant: cirrhosis with new-onset ascites
o Transjugular intrahepatic portosystemic shunt (TIPS): refractory ascites
o Peritoneovenous shunt: patients with refractory ascites who are not candidates for
paracenteses, TIPS, or liver transplant
Spontaneous Bacterial Peritonitis
•
Is a bacterial infection of ascitic fluid that occurs in the absence of an identifiable
intraabdominal source of infection.
•
Antimicrobial therapy
o
o
o
o
o
o
•
Indications (presence of any of the following in a patient with cirrhosis and ascites):
Abdominal pain and/or tenderness
Fever > 37.8°C (100°F)
Ascitic fluid neutrophil count ≥ 250/mm3
Most common isolates: Escherichia coli, Streptococcus spp., Staphylococcus spp.,
and Klebsiella
Duration
Narrow antibiotic coverage according to bacterial susceptibility.
Continue antibiotic therapy for at least 5–7 days.
Community-acquired infection and no recent beta-lactam antibiotic exposure First-line: 3rd-gen cephalosporin IV, preferably cefotaxime 2g every 8h iv
Alternative: oral ofloxacin 400mg x2/day
Healthcare-associated infection, suspected resistant pathogen, and/or recent betalactam antibiotic exposure In areas with a low prevalence of multidrug-resistant pathogens: Piperacillintazobactam 3.75-4.5g iv every 8h
In areas with a high prevalence of ESBL-producing Enterobacteriaceae:
Low prevalence of gram-positive MDR bacteria: Meropenem 1g iv every 8h
High/ unknown prevalence of gram-positive MDR bacteria (e.g., MRSA, VRE):
•
Meropenem PLUS, one of the following:
•
Vancomycin
•
Linezolid
•
Daptomycin
Adjunctive therapy
o
o
o
IV albumin supplementation
Consider discontinuing beta blockers
Discontinue diuretics.
o
o
•
Avoid potentially nephrotoxic medications (e.g., NSAIDs).
Consider discontinuing proton-pump inhibitors
Supportive therapy
o
o
o
o
Electrolyte repletion
Analgesics as needed
Antipyretics as needed
IV fluids: Use caution in patients who are volume overloaded
Hepato-renal syndrome
Def: Deterioration of kidney function in patients with advanced liver disease
Treatment
•
General measures: improvement of liver function if possible (e.g., cessation of alcohol use,
avoid nephrotoxic drugs)
•
Pharmacotherapy
o
o
•
Non critically ill individuals:
a combination of midodrine (is a systemic vasoconstrictor), octreotide
(inhibitor of endogenous vasodilator release, produces splanchnic
vasoconstriction), and albumin
Critically ill individuals:
a combination of norepinephrine and albumin
Surgical/interventional procedures
o Renal replacement therapy (dialysis)
o Placement of a transjugular intrahepatic portosystemic shunt (TIPS)
o A liver transplant is the only curative option.
Hepatic encephalopathy
Definition: Fluctuations in mental status and cognitive function in the presence of severe liver
disease (e.g., cirrhosis)
Treatment:
•
General measures
o
o
•
Avoidance and correction of precipitating factors (e.g., hepatotoxic medication,
alcohol, hypovolemia, electrolyte disturbances)
Treatment of further complications that might aggravate the encephalopathy
Pharmacotherapy
o Lactulose: a synthetic disaccharide laxative
First-line treatment for hepatic encephalopathy
Improves hepatic encephalopathy by decreasing absorption of ammonia in the
o
o
bowel: lactulose is converted to lactic acid by intestinal flora → acidification in
the gut leads to conversion of ammonia (NH3) to ammonium (NH4+) →
ammonium is excreted in the feces → decreased blood ammonia concentration
Rifaximin: a broad-spectrum, nonabsorbable oral antibiotic
Reduces the number of ammonia-producing intestinal bacteria
May be added to lactulose to prevent recurrent episodes of hepatic
encephalopathy after a second episode
LOLA- L Ornithine L Aspartate (Hepa merz): 20-40g/day IV
153) Treatment of chronic cholestasis
Definitions
•
Cholestasis: impaired production, secretion, or outflow of bile
•
Nonobstructive intrahepatic cholestasis: impaired bile formation or secretion
•
Obstructive intrahepatic cholestasis: biliary obstruction within the liver
•
Obstructive extrahepatic or posthepatic cholestasis: obstruction of the biliary ducts between
the liver and the duodenum
Treatment based upon etiology:
•
Primary Biliary Cirrhosis (PBC):
o Liver transplant is the only definitive treatment
o Symptomatic =
1st line= Ursodeoxycholic acid (slows disease progression + improves clinical
symptoms; delayed need for transplantation); treatment of pruritus
2nd line= Obeticholic acid (inhibits cholesterol synthesis)
Liver transplant necessary if liver cirrhosis is advanced
o
•
Primary Sclerosing Cholangitis: Transplant
o Symptomatic: Ursodeoxycholic acid + Tacrolimus (immunosuppressive, which may
↓ cholestasis parameters: ALP, ASAT, ALAT, bilirubin).
Doesn’t prevent disease progression
o Treatment of pruritus (e.g., cholestyramine, rifampicin, naltrexone)
o Supplementation of fat-soluble vitamins (ADEK)
o In case of bile duct stenosis: ERCP w/duct dilation= potentially stent placement
o
Surgical = Liver transplant necessary if liver cirrhosis is advanced
•
Malignant extrahepatic biliary obstruction:
o Bile duct stenting
•
Biliary cyst
o Surgical excision
•
Drug-induced cholestasis:
o Discontinuation of the offending medication
•
Invasive intervention for select patients with symptomatic gallstones, biliary strictures, or
other obstructing masses:
o Cholecystectomy, ERCP
Symptomatic treatment
•
Treatment of pruritus — Depends on the severity of symptoms
o
o
Mild: emollient solutions for skin hydration
Moderate/ severe: Cholestyramine, Rifampin, opioid antagonists, ursodeoxycholic acid
•
Supportive therapy:
o Dietary modifications and spasmolytics (Dicyclomine),
o Analgesics (NSAIDs, opioids)
•
Treatment of fat malabsorption principally involves dietary substitution.
o
o
In older patients, a diet that is rich in carbohydrates and proteins can be substituted for
a diet containing long-chain triglycerides.
Oral absorbable, fat-soluble vitamin A, D, E, and K supplementation and monitor
response to prevent fat-soluble vitamin deficiencies,
•
If untreated Vit D deficiency → Increased risk of osteoporosis can be treated
with Bisphosphonates
Ursodeoxycholic acid
o
Decreases the cholesterol content of bile and therefore reduces bile stone and
sludge formation.
154) Antibacterial treatment of the biliary tract infection
•
Definition: Acute cholangitis is caused primarily by bacterial infection in a patient with biliary
obstruction. The organisms typically ascend from the duodenum.
•
Treatment
•
In general, empiric regimens for intra-abdominal infections include antimicrobials with activity
against enteric streptococci, coliforms, and anaerobes.
•
The choice of antibiotics should take into consideration whether the infection is communityacquired versus healthcare-associated, as well as individual risk factors for infection with
resistant bacteria and risk for adverse outcomes.
•
Community-Acquired Acute Cholangitis
o
Low to-moderate risk.
One of the following:
•
Cefazolin 1-2 g IV every 8 hours
•
Ceftriaxone 2 g IV once daily
• Ciprofloxacin 400 mg IV every 12 hours or 500 mg PO every 12 hours
PLUS
•
o
Metronidazole 500 mg IV or PO every 8 hours
High risk
Single- agent regimen:
•
Meropenem 1g IV every 8 hours
•
Piperacillin-tazobactam 4.5g IV every 6 hours
Combination regimen with metronidazole:
•
ONE of the following:
o Cefepime or Ceftazidime (have same dose: 2 g IV every 8hrs)
•
PLUS:
o
•
•
Metronidazole 500 mg IV or PO every 8 hours
Healthcare-associated acute cholangitis:
o Single agent regimen:
Meropenem 1g IV every 8 hours
Piperacillin-Tazobactam 4.5 g IV every 6 hours
o Combination regimens:
Cefepime or Ceftazidime 2 g IV every 8 hours
Plus, Metronidazole 500 mg IV or PO every 8 hours
PLUS, one of the following, in some cases*
•
Ampicillin 2 g IV every 4 hours
•
OR Vancomycin 15-20 mg/kg IV every 8-12hrs
The chosen antimicrobial agents should subsequently be tailored to culture and susceptibility
results when they become available.
•
The duration of antibiotics depends on the adequacy of control of infection and the clinical
stability of the patient.
•
Once the source of infection is controlled, antimicrobial therapy for patients with acute
cholangitis is continued for an additional duration of four to five days.
155) Treatment principles in poisoning
The fundamentals of poisoning management =
1) Supportive care,
2) Prevention of further poison absorption,
3) Enhancement of poison elimination,
4) Administration of antidotes,
5) Prevention of re-exposure.
Supportive care: Is the most important aspect of treatment and frequently is sufficient to effect
complete patient recovery.
●
Goal of supportive therapy is to maintain physiologic hemostasis until detoxification is
accomplished and to prevent and treat secondary complications such as aspiration, bedsore,
cerebral and pulmonary oedema, renal failure, pneumonia etc.
●
ABCDEs are very important! Must always first clear the airway and ensure the patient is well
ventilated. Endotracheal intubation may be indicated for unconscious patients or for
protection against aspiration of GI contents
●
Oxygenation/ventilation
●
Treatment of arrhythmias =
o Bradyarrhythmia – Bradyarrhythmias associated with hypotension should be treated
in the standard fashion with atropine and/or temporary pacing.
However, in patients with CCB or BB intoxication, the administration of
calcium, glucagon, vasopressors, isoproterenol, high-dose insulin, or other
therapies may obviate(remove) the need for a temporary pacemaker.
Ventricular tachycardia – Sodium bicarbonate is first-line therapy for ventricular
▪
o
tachycardias when they occur in the context of intoxication from a drug with sodium
channel-blocking properties (eg, tricyclic antidepressants, carbamazepine, cocaine).
●
Hemodynamic support =
a) if hypotensive then give boluses of isotonic IV fluids.
b) administer adrenaline or high-dose dopamine if unresponsive to this.
●
Treatment of seizures - benzodiazepines, followed by barbiturates if necessary
●
Hypertension –
o in agitated patients is best treated initially with nonspecific sedatives such as
Benzodiazepines.
o When hypertension necessitates specific therapy because of associated end-organ
dysfunction, preferred treatments include CCB’s, Phentolamine, Labetalol, or
Nitroprusside.
o The use of beta-blockers alone for patients with sympathetic hyperactivity (e.g.,
cocaine intoxication) is generally not recommended.
●
Correction of temp. abnormalities.
o
Hyperthermia may require aggressive treatment, including ice water immersion
●
Correction of metabolic derangements
●
Prevention of secondary complications
Prevention of further poison absorption
•
GI decontamination (should be done w/in 1st 4 hours) =
o
o
•
Previously gastric lavage was indicated however it is no longer common. It is
sometimes considered for life-threatening poisons that can’t be treated
effectively w/other decontamination or elimination therapies
Activated charcoal is the preferred method of GI decontamination in most
cases – has comparable or greater efficacy; has fewer contraindications and
complications; and is < aversive and invasive than ipecac or gastric lavage.
Recommended dose is 1 g/kg of body weight
Whole bowel irrigation
o performed by administering a bowel cleansing solution containing electrolytes
and polyethylene glycol orally or by gastric tube at a rate of 2 L/h (0.5 L/h in
children) until rectal effluent is clear.
o
o
It is most appropriate for those who have ingested FBs, packets of illicit drugs, and
agents that are poorly absorbed by charcoal (heavy metals). It is contraindicated in
ileus, bowel obstruction, and hemodynamic instability.
Whole bowel irrigation (WBI) refers to the administration of osmotically balanced
polyethylene glycol electrolyte solution (PEG-ES) to induce liquid stool and
mechanically flush pills, tablets, or drug packets from the GI tract.
•
Dilution (drinking water/milk at a volume of f ml/kg of body weight) is recommended only
after ingestion of corrosives.
•
Decontamination of other sites = eye, skin, and body cavity decontamination
Enhancement of poison elimination
•
Multiple doses of activated charcoal
•
Urinary alkalinization: ion trapping via alteration of urine pH may prevent the renal
absorption of poisons that undergo excretion by glomerular filtration and active tubular
secretion
•
Extracorporeal removal: capable of removing toxin from the bloodstream; in cases of
severe poisoning w/carbamazepine, ethylene glycol, isopropyl alcohol, lithium,
theophylline, and salicylates.
o Hemodialysis,
o Charcoal/resin hemoperfusion,
o Hemofiltration,
o Plasmapheresis
•
Elimination of heavy metals can be enhanced by Chelation, and the
o
Removal of CO can be accelerated by Hyperbaric Oxygenation
•
Forced diuresis
•
Exchange transfusion
Administration of antidotes
Antidotes counteract the effects of poisons by neutralizing them or by antagonizing their physiologic
effects.
1) IV lipid emulsion has been shown to be a successful antidote for poisoning from various
anesthetics and membrane-active agents (cyclic antidepressants)
2) Activated charcoal with sorbital - used for many oral toxins
3) Atropine - organophosphate poisoning
4) Ethanol or fomepizole - Ethylene glycol poisoning and methanol poisoning
5) Naloxone - opioid
6) N-acetylcysteine - Paracetamol (acetaminophen) poisoning
7) Beta blocker- Theophylline
8) Calcium chloride- calcium channel blockers, black widow spider bites
9) Chelators such as
a) EDTA, dimercaprol, penicillamine, and 2,3-dimercaptosuccinic acid- heavy metal
poisoning
10) Deferoxamine -Iron poisoning
11) Digoxin Immune Fab antibody (Digibind and Digifab)-digoxin poisoning
12) Flumazenil- benzodiazepine poisoning
13) Glucagon- beta blocker poisoning and calcium channel blocker poisoning
14) 100% oxygen or hyperbaric oxygen therapy- carbon monoxide and cyanide poisoning
15) Leucovorin-methotrexate and trimethoprim
16) Octreotide-oral hypoglycemic agents
17) Protamine sulfate- Heparin poisoning
18) Physostigmine sulfate- Anticholinergic poisoning
19) Pyridoxine- Isoniazid poisoning, ethylene glycol
20) Phytomenadione (vitamin K) and fresh frozen plasma-warfarin poisoning and indanedione
21) Sodium bicarbonate- TCAs
Prevention of re-exposure =
●
Adult education,
●
Childproofing,
●
Notification of regulatory agencies,
●
Psychiatric referral
156) Treatment of urinary tract infection
General principles:
•
Antibiotic treatment is recommended for all patients with symptomatic UTI.
•
The Initial treatment is with an empiric regimen, which is maintained for uncomplicated
cases. But in unclear or complicated cases, the regimen may subsequently have to be
adjusted based on urine culture data.
•
In addition to the antibiotic treatment, we can consider also supportive treatment:
o
o
Phenazopyridine, a urinary analgesic, can be used for symptomatic relief for a
maximum of 2 days.
Also, oral analgesia, e.g., with NSAIDs, can provide additional relief.
Uncomplicated lower UTI treatment:
Treatment can be in an outpatient setting with oral antibiotics.
Treatment duration depends on the chosen antibiotic agent.
Symptom relief can be expected to occur after an average of 36 hours.
(If symptoms persist despite the antibiotic therapy, it might be a complicated case or you
need to change the empiric antibiotic)
● First-line treatment
○ Fosfomycin (single dose) 3g PO ONCE
○ Nitrofurantoin (100 mg PO every 12 hours) for 5 days
○ Trimethoprim/sulfamethoxazole for 3 days (160/800 mg PO every 12 h)
● Second-line treatment: beta-lactam antibiotics for 5–7 days
○ Aminopenicillins plus beta-lactamase inhibitors, e.g., amoxicillin/clavulanic acid (500
mg/12hrs PO)
○ Oral cephalosporins, e.g., cefpodoxime, cefdinir, or cefaclor
● Alternatives: Consider fluoroquinolones, e.g., ciprofloxacin for 3 days (250 mg PO every
12 hours) for patients with previous infections with bacteria resistant to other drug classes.
Complicated lower UTI treatment:
● The empiric antibiotic therapy should have broad-spectrum activity against the expected
uropathogens.
● Because UTIs in men can involve the prostate, antibiotics should be able to penetrate
prostate tissue (e.g., fluoroquinolones, TMP/SMX).
● In addition to antibiotic therapy, complicating factors (e.g., obstruction) should be treated, if
possible.
● Hospitalization and initial intravenous treatment may be necessary in the following
cases:
○ Severe systemic symptoms, e.g., signs of shock
○ Inability to tolerate oral antibiotics
○ Severe comorbidities, e.g., immunocompromised or heart failure
● Options for the initial empiric treatment of complicated lower UTIs include:
Antibiotic therapy is commonly given for 7-14 days.
○ Fluoroquinolones PO or IV:
■
■
levofloxacin (750 mg PO or IV every 24 hours)
or ciprofloxacin (500mg/12hrs PO OR 400mg/12hrs IV)
○ Beta lactams
■
■
Second-generation or third generation cephalosporins:
● e.g., ceftriaxone (1g/ 24hrs IV)
Extended-spectrum penicillins: e.g., ampicillin/sulbactam (1.5–3g/ 6hrs IV)
○ Aminoglycosides (e.g., gentamicin 5 mg/kg/24hrs IV or IM): treatment option if
fluoroquinolones or beta lactams are contraindicated or as an addition to beta lactams.
Uncomplicated pyelonephritis:
Empiric antibiotic therapy for uncomplicated pyelonephritis
● Most patients can be treated with an oral fluoroquinolone for 5–7 days
○ levofloxacin (750 mg/ 24hrs PO)
○ ciprofloxacin (500 mg PO every 12 hours)
● Alternatives
○ Trimethoprim-sulfamethoxazole, for 10–14 days (only recommended if susceptibility is
known)
○ Amoxicillin-clavulanate for 10–14 days (500 mg PO three times daily)
○ Cefpodoxime for 10–14 days
● Consider a single dose of a broad-spectrum parenteral antibiotic prior to the
administration of oral antibiotics:
■
■
Ceftriaxone 1 g IV once
OR gentamicin 5–7 mg/kg IV once
● Supportive care
○ Encourage the patient to drink adequate amounts of fluids.
○ Consider an IV fluid bolus in patients with dehydration.
○ Analgesia for pain
○ Antiemetics in patients with nausea and vomiting
Complicated pyelonephritis:
•
Patients with complicated acute pyelonephritis should be admitted to the hospital and
started on parenteral empiric antibiotic therapy for 10-14 days as soon as possible.
IF not severely ill and no risk factors for multidrug-resistant bacterial infection:
•
One of the following:
A fluoroquinolone: Levofloxacin 750 mg/ 24hrs IV
An extended-spectrum cephalosporin: Ceftriaxone 1g IV every 24 hours
An extended-spectrum penicillin with a β-lactamase inhibitor (e.g., piperacillintazobactam)
o Consider adding an aminoglycoside until culture results are available.
Gentamicin 5–7 mg/kg/24 hours IV in three equally divided doses every 8hrs
IF severely ill (i.e., septic)
and/or with risk factor(s) for multidrug-resistant gram-negative bacterial infection:
o
o
o
•
One of the following:
o
o
o
A carbapenem: Meropenem 1 g IV every 8 hours
An extended-spectrum cephalosporin: Ceftriaxone 1 g IV every 24 hours
An extended-spectrum penicillin with a β-lactamase inhibitor
(e.g., piperacillin-tazobactam)
•
PLUS consider adding an aminoglycoside until culture results are available.
o Gentamicin 5–7 mg/kg/24 hours IV in three equally divided doses every 8 hours
•
IF Enterococcus or MRSA suspected:
o
•
Consider adding vancomycin 15 mg/kg/12hrs IV; titrate as needed.
Supportive care
o Hydration oral or iv fluids if needed
o Analgesics as needed
o Antiemetics as needed
157) Treatment in glomerulonephritis
Nephritic syndrome
Presentation
•
•
Proteinuria (< 3.5 g/day) (can be in
nephrotic range in severe cases)
Hematuria with acanthocytes
Nephrotic syndrome
•
•
•
Heavy proteinuria (> 3.5 g/day)
Hypoalbuminemia
Generalized edema
•
•
•
•
•
•
Pathophysiology
RBC casts in urine
Oliguria
Mild to moderate edema
•
Azotemia
Hypertension
Sterile pyuria
•
Inflammatory response
within glomeruli → GBM disruption → loss of
renally excreted RBCs (acanthocytes)
and ↓ GFR → hematuria, oliguria, azotemia,
and ↑ renin → edema and hypertension
Causes
1) Poststreptococcal glomerulonephritis
2) IgA nephropathy (Berger disease)
3) Granulomatosis with polyangiitis
4) Eosinophilic granulomatosis with
5)
6)
7)
8)
9)
polyangiitis
Microscopic polyangiitis
Goodpasture syndrome (antiGBM disease)
Alport syndrome (hereditary nephritis)
Thin basement membrane disease
Rapidly progressive
glomerulonephritis (RPGN)
10) Lupus nephritis
Most common causes of nephriticnephrotic syndrome:
1) Membranoproliferative GN
2) Diffuse proliferative GN
•
•
Hyperlipidemia and fatty
casts in urine → frothy urine
Hypertension
↑ Risk of thromboembolism: (via
loss of antithrombin III)
↑ Risk of infection (via loss
of IgG and tissue edema which
compromises the local blood supply
and immune response)
Damage to podocytes → structural damage
of glomerular filtration barrier → massive
renal loss of protein
Due to primary or
secondary podocyte damage
1) Minimal change disease
2) Focal segmental
glomerulosclerosis
3) Membranous nephropathy
Due to secondary podocyte damage
4) Diabetic nephropathy
5) Amyloid light-chain
(AL) amyloidosis, light
chain deposition disease
6) Lupus nephritis
Treatment Nephritic syndrome:
Supportive therapy
● Low-sodium diet
● Water restriction
Medical therapy
•
If proteinuria and/or hypertension: angiotensin-converting enzyme inhibitors or angiotensinreceptor blockers
•
If severe hypertension and/or edema: diuretics
•
Sometimes immunosuppressive therapy is indicated (e.g., in lupus nephritis).
•
If RPGN (Rapidly prog. GN) from anti-GBM antibody disease: plasmapheresis
•
In the case of:
Severe renal insufficiency or kidney failure: renal replacement therapy (e.g.,
hemodialysis, possibly transplantation)
*For specific treatment of underlying diseases look at the end of the question.
o
Management of symptoms and complications of nephrotic syndrome
1. Edema
•
Dietary sodium restriction: < 3 g/day (usually 1.5–2 g/day)
•
Fluid restriction: < 1.5 liters/day
•
Diuretic therapy
o First-line: oral loop diuretic (e.g., furosemide ex. 40 mg once)
o Second-line:
Add oral thiazide or thiazide-like diuretic
AND/OR switch to IV loop diuretic (e.g., IV furosemide)
o Consider adjunctive IV albumin
2. Proteinuria
Elimination or reduction of proteinuria is a major treatment goal for nephrotic syndrome and can lead
to increased serum albumin, decreased edema, attenuation of the metabolic effects of heavy
proteinuria (e.g., hyperlipidemia), reduction in risk of thromboembolism and infection, and slowing of
the progression of chronic kidney disease.
Antiproteinuric therapy
•
RAAS inhibitors: ACEI (Ramipril 2.5-20mg/day) or ARB (losartan 25-100mg/day)
o Reduces proteinuria
o Treats hypertension
o May slow progression of any underlying renal disease (e.g., diabetic nephropathy)
o
Avoid in patients with: AKI, hyperkalemia, or abrupt onset of nephrotic syndrome.
•
Other measures that may be beneficial in combination with an ACEI or ARB:
o Low sodium diet
o Thiazide diuretic (e.g., hydrochlorothiazide 25mg/day)
o Mineralocorticoid receptor antagonist (e.g., spironolactone 25mg/day)
•
Dietary protein: avoid a very high-protein diet but ensure adequate protein intake.
3. Dyslipidemia
• Lipid-lowering therapy (e.g., atorvastatin 10-80mg/day)
4. Hypercoagulability
All patients with nephrotic syndrome are at increased risk of thromboembolism, and this risk becomes
progressively higher as serum albumin drops below 3.0 g/L.
•
Prophylactic anticoagulation
o Unfractionated heparin: 5000units/day
o Low molecular weight heparin: Enoxaparin 40mg/day SC
o Oral warfarin (target INR 2.0–3.0)
5. Infectious risk
•
Preventive measures
o Pneumococcal vaccination
o Annual vaccination for influenza
Disease-specific measures for nephrotic GN
Primary forms of nephrotic glomerulopathies: often treated with immunosuppressive therapy
•
Immunosuppressive therapies may include:
o
o
Glucocorticoids (often used initially)
Additional immunosuppressants in patients with steroid-resistant nephrotic syndrome
or severe disease.
Cyclophosphamide,
Calcineurin inhibitors
•
Management in adults is usually guided by biopsy-based histological diagnosis.
•
Children are often treated initially with empiric corticosteroids for presumed MCD.
• Secondary forms of nephrotic glomerulopathies: Treat the underlying cause.
1. Primary membranous nephropathy
•
Initial management: conservative therapy including an RAAS inhibitor (i.e., ACEI or ARB)
•
Consider immunosuppressive therapy for severe or refractory disease.
o Prednisone AND cyclophosphamide
o Alternatives: cyclosporine, tacrolimus, OR rituximab
2. Primary (idiopathic) focal segmental glomerulosclerosis
•
Initial management: supportive therapy including an RAAS inhibitor (i.e., ACEI or ARB).
•
Consider immunosuppressive therapy for all patients with nephrotic syndrome due to
FSGS.
o Prednisone
o Alternative: calcineurin inhibitor (cyclosporine OR tacrolimus)
3. Primary (idiopathic) minimal change disease
•
Initial management: immunosuppressive therapy
o Prednisone
o Alternative: cyclophosphamide OR calcineurin inhibitor
4. Diabetic nephropathy
•
Strict glycemic control
•
RAAS inhibition (e.g., ACEI or ARB)
•
Optimization of blood pressure control
•
Close surveillance and timely referral to renal replacement therapy if ESRD is anticipated
5. Amyloid nephropathy
•
Treatment of the underlying disease
o AL amyloidosis: treatment of multiple myeloma or other plasma cell dyscrasia
o AA amyloidosis: treatment of underlying inflammatory condition
6. Lupus nephritis
•
Induction and maintenance therapy is generally indicated in patients with class III or IV lupus
nephritis.
•
All patients should receive standard therapy for lupus and individualized management of CKD.
•
Induction therapyo
o
IV glucocorticoids (e.g., methylprednisolone)
PLUS other immunosuppressants (e.g., mycophenolate or cyclophosphamide)
•
Maintenance of remissiono Oral prednisone
o PLUS mycophenolate OR azathioprine
•
Refractory or relapsing disease: Rituximab may be considered.
Specific treatments for nephritic syndrome
1. Poststreptococcal glomerulonephritis
•
In most cases the disease is self-limiting and only supportive treatment focused on the
complications of volume overload is necessary.
•
Monitor electrolytes, renal function parameters, and blood pressure
•
For edema: low-sodium and low-protein diet, loop diuretics
•
For hypertension: ACE-inhibitors/ARBs, calcium channel blockers
•
If persisting streptococcal infection: antibiotic therapy (penicillin G benzathine)
• If severe course/complications: glucocorticoids, temporary need for dialysis
2. IgA nephropathy
•
Patients with isolated hematuria
•
Regularly monitor kidney function and initiate treatment if disease progresses (e.g.,
occurrence of proteinuria).
•
Symptoms resolve spontaneously in 30% of patients.
•
Patients with proteinuria or hypertension: ACE inhibitors/angiotensin II receptor blockers
•
For severe/rapidly progressive disease: glucocorticoids PLUS possibly
cyclophosphamide/azathioprine
3. Membranoproliferative glomerulonephritis
•
Membranoproliferative glomerulonephritis (type 1 and type 2 MPGN)
•
RAAS inhibitors are often added to treatment.
•
Prednisone alone or in combination with
o other immunosuppressants (cyclosporine OR tacrolimus)
158) Diabetes mellitus - treatment with insulin and oral medications
•
Comprehensive medical careo individualized goal and therapeutic plan
o self monitoring of blood glucose
o HBA1c testing (2-4 times a year)
•
Lifestyle managemento
o
o
o
•
•
diabetic self management education and support
nutrition therapy
physical activity
psychological care including evaluation of depression
Detection, prevention and management of diabetic related complications
Management and treatment of diabetic relevant conditions-hypertension,
hyperlipidemia
Pharmacologic treatment of diabetes
Type 1 DM:
•
Intensive insulin therapy has the goal of achieving near-normal glycemia.
•
This requires multiple resources such as patient education, comprehensive recording of
plasma glucose and nutrition intake, and variable insulin regimens Multiple daily injections or
continuous subcutaneous insulin infusion.
short-acting
Onset (h)
Peak (h)
duration (h)
lispro
<0.25
0.5-1.5
2-4
Aspart
<0.25
0.5-1
2-4
Glulisine
<0.25
0.5-1.5
2-4
regular
0.5-1
2-3
3-6
inhaled human insulin
0.5-1
2-3
3
Long-acting
Onset (h)
Peak (h)
duration (h)
Degludec
1-9
42
Detemir
1-4
12-24
Glargine
2-4
20-24
NPH
2-4
4-10
10-16
examples of insulin
combinations
Onset (h)
Peak (h)
duration (h)
75/25- 75% protamine
lispro, 25% lispro
<0.25
10-16
70/30-70% protamine
aspart, 30% aspart
<0.25
15-18
●
●
●
●
●
●
●
Short acting insulins are effective postprandially especially aspart, lispro, glulisine is
prefered over regular insulin for prandial coverage because they have faster onset.
A lower incidence of hypoglycemia especially at night has been reported with insulin glargine
when compared to NPH
Combined insulins tips:
1. mix the different insulin formulations in the syringe immediately before injection.
2. Do not store insulin in a mixture.
3. Follow same routine to standardize the physiologic response
4. Do not mix insulin glargine, detemir, degludec with other insulins.
In all regimens, long acting insulins (NPH, glargine, detemir, degludec) supply basal
insulin, whereas regular insulin aspart, glulisine, lispro provides prandial insulin.
○ Short-acting insulin analogue should be injected just before <10 mins and regular
insulin 30-45mins before
In general individuals with type I DM require 0.4- 1 units/kg/day of insulin, divided into
multiple doses, with 50% given as basal insulin.
Strategies to overcome the persistent dysglycemia on insular regimen
○ Increased Blood Glucose before breakfast → increase the dose of long acting insulin
before bed
○ Increased BG after meal → increase dose of rapid acting insulin before meal
○ Increased BG before lunch/ dinner → increase dose of basal insulin before breakfast
Insulin pumps
○ small computerized device that delivers insulin continuously throughout the day
○ constantly infuse insulin subcutaneously
○
○
○
program amount of insulin to infuse during basal hours and can deliver a bolus of
insulin before meal.
usually aspart or lispro are used in the pump
Is considered the gold standard
Treatment of T2DM
1. Medications that primarily lower glucose levels by their actions on the liver, muscle, and
adipose tissueA. Metformin (Biguanides):
•
Increase insulin sensitivity (enhances effect of insulin)
•
Reduction in insulin resistance via modification of glucose metabolic pathways
•
Decreases glucose production in the liver ↓hepatic gluconeogenesis and intestinal
glucose absorption
•
Increases peripheral insulin sensitivity
•
Lowers postprandial and fasting blood glucose levels
•
Beneficial effect on dyslipidaemia
•
Reduces LDL/triglycerides and free fatty acid concentrations, increases HDL
•
Promotes modest weight reduction or at least weight stabilization
•
No risk of hypoglycaemia
•
Start with a low dose and increase dose gradually to reduce the risk of gastrointestinal
side effects.
•
Dosing
o A common schedule would be one 500 mg tablet three times a day with meals or
one 850 mg or 1 000 mg tablet twice daily at breakfast and dinner. 1500-3000 mg
in normal kidney function.
•
Side effects –
o
o
o
•
Can be used during pregnancy first trimester,
o
•
gastrointestinal, including a metallic taste in the mouth, mild anorexia, nausea,
abdominal discomfort, and soft bowel movements or diarrhea.
Vitamin B12 deficiency, monitor patients B12 levels
Lactic acidosis is an extremely uncommon side effect
but if used during all of pregnancy can cause problems later during childhood. Is
not advised to use during pregnancy. Can treat with insulin instead!
Contraindications
o Renal failure (if creatinine clearance < 30 mL/min)
o Severe liver failure
o Drug interaction: Intravenous iodinated contrast medium (stop at least 24 hours
before test to prevent acute kidney failure and lactic acidosis)
o Pause metformin prior to surgery (ex.opening of thoracic cavity)
o Chronic pancreatitis, starvation ketosis, ketoacidosis, sepsis
o Heart failure (NYHA III and IV), respiratory failure, shock, sepsis
o Alcoholism
B. Thiazolidinediones (Insulin sensitizer)
•
Both rosiglitazone(withdrawn) and pioglitazone 15-45 mg PO, once daily are effective
as monotherapy and in combination with sulfonylureas or metformin or insulin,
•
Glycemic efficacy: lowers HbA1c by 1-2% in 3 months
•
The thiazolidinediones increase insulin sensitivity by acting on adipose, muscle, and, to
a lesser extent, liver to increase glucose utilization and decrease glucose production.
•
Favorable effect on lipid metabolism: ↓ triglyceride, ↓ LDL, ↑ HDL
•
Indications: May be considered as monotherapy in patients with severe renal failure
and/or contraindications for insulin therapy. No risk of hypoglycaemia.
•
Important side effects:
o Fluid retention and edema
o Weight gain, does not cause hypoglycaemia
o
o
o
o
•
Increased risk of heart failure
Increased risk of bone fractures (osteoporosis)
Rosiglitazone: increased risk of cardiovascular complications like cardiac infarction
or death
Pregnancy risk factor C
Contraindications-Congestive heart failure (NYHA III or IV),Liver failure,Pioglitazone:
history of bladder cancer or active bladder cancer; macrohematuria of unknown origin
2. Medications that primarily stimulate insulin secretion by binding to the sulfonylurea
receptor on the beta cell/insulin secretagogues:
A. Sulfonylureas
•
usually given once or twice daily, increase glucose levels throughout the whole
day, more potent in reducing blood glucose
o Glyburide - relatively long half-life
o Glipizide - short acting agent
o Glimepiride - 1-2 mg, once daily per os
•
The primary mechanism of action of the sulfonylureas is to stimulate insulin release from
pan-creatic B cells.
•
Medications require functioning pancreatic B cells to produce their effect on blood glucose.
(So not used in DM1). Low cost.
•
Indications
o Patients who are not overweight, do not consume alcohol, and adhere to a consistent
dietary routine
o Generally not frequently used
•
Side effects: Life threatening hypoglycemia, increased risk in renal failure.
Granulocytopenia, hemolytic anemia, weight gain, alcohol intolerance.
•
Contraindications: Severe cardiovascular comorbidity, obesity, sulphonamide allergy,
severe liver/kidney failure
•
Drug interactions: Ketoconazole, warfarin
•
NB! Beta-blockers may mask the warning signs of hypoglycemia (e.g., tachycardia) and
decrease serum glucose levels even further . Since sulfonylureas also increase the risk of
hypoglycemia, the combination of these two substances should be avoided!
3. Incretin mimetics (incretins are hormones)
(GLP-1 receptor agonists)
• Exenatide - all subcutaneous except for semaglutide
•
Liraglutide: rapid-release formula that is administered daily 0.6mg sc
•
Albiglutide: extended-release formula that is administered once weekly
•
Dulaglutide
• Semaglutide : oral, 3 mg os per day
Clinical characteristics:
o Weight loss, no risk of hypoglycaemia, decrease risk for cardiovascular disease
Side effects
o Gastrointestinal complaints (particularly impaired gastric emptying!)
o Increased risk of pancreatitis and potentially pancreatic cancer :
o Strong feeling of satiety - so decreases weight
Contraindications
o Preexisting symptomatic gastrointestinal motility disorders
o Chronic pancreatitis or a family history of pancreatic tumors
4. Dipeptidyl peptidase-4 inhibitors (DPP-4 inhibitors - gliptins)
1) Sitagliptin - 100 mg per day, orally
2) Saxagliptin
3) Linagliptin
Gliptins indirectly increase the endogenous incretin effect by inhibiting the DPP-4 that breaks
down GLP-1 → increased insulin secretion decreased glucagon secretion, delayed gastric
emptying.
o No risk of hypoglycemia
o Usually no weight changes
Important side effects
o Gastrointestinal symptoms: diarrhea, constipation (milder than in GLP-1 agonist
exposure), Arthralgia, Headaches, dizziness
o Increased feeling of satiety (often favorable) due to delayed gastric emptying
o Nasopharyngitis and upper respiratory tract infection, Increased risk of pancreatitis
o Worsening renal function, acute renal failure
Contraindications- Hypersensitivity, Liver failure, Renal failure
o No synergism between GLP-1 and DPP-4-inhibitors
5. SGLT-2 inhibitors (gliflozins)
1) Dapagliflozin*
2) Empagliflozin 10 mg once daily (jardiance)
3) Canagliflozin
Mechanism: Reversible inhibition of the sodium-dependent glucose co-transporter (SGLT-2)
in the proximal tubule of the kidney → reduced glucose reabsorption in the kidney →
glycosuria and polyuria
Indications: a treatment option used especially in young patients with treatment-compliant
type 2 DM without significant renal failure
Promotes weight loss, reduces blood pressure (decreases CVS risk- because it decreases
Na —> decreased preload)
Side effects: UTI, genital infections, dehydration, severe diabetic ketoacidosis
Contraindications: chronic kidney disease, recurrent UTI's
6. α-glucosidase inhibitors =
Acarbose
Should be given with the first bite to be together with carbohydrates
Doesn’t cause weight gain or hypoglycaemia, cause bloating
Avoid with antacids, don’t prescribe in patients with IBD
Overall approach in T2 DM
1. Target goals: HBA1c
a. < 6.5: low hypoglycemic risk, most patients
b. > 6.5: w/ serious illness
2. Lifestyle + weight loss
Monotherapy
(HBA1c <7.5%)
Dual therapy
(HBA1c >7.5%)
Triple therapy
Symptoms
(HBA1c > 9%)
Metformin
GLP-1
Metformin OR other 1st
line agent
Metformin OR other 1st
line + 2nd line agent
NO
Dual
YES
Insulin
DPP4i
SGLT-2i
TZD
Sulfonylureas
AGi
PLUS
GLP-1
SGLT-2i
TZD
Sulfonylureas
Insulin
PLUS
GLP-1
SGLT-2i
Basal insulin
AGi
Sulfonylureas
Or
Triple
therapy
PLUS
Other
agent
If target HBA1c goal not
reached in 3 months
progress to DUAL
therapy
If target HBA1c goal not
reached in 3 months
progress to TRIPLE
therapy
If target HBA1c goal
not reached in 3
months progress to
INTENSIVE Insulin
ADD or INTENSIVE
insulin therapy
therapy
Insulin in T2DM should
be considered in
lean individuals those
with severe weight loss,
w/ Renal/ Hepatic dis.
Or in hospitalised indivi.
159) Treatment of diabetic complications.
1. Treatment of DKA and HHS (hyperosmolar hyperglycemic state)
DKA
HHS
Treatment
1. Fluid resuscitation
1. Fluid resuscitation
2. Short-acting IV insulin
2. insulin
3. Replacement of potassium
3. Replacement of potassium
4. Glucose supplementation in the
case of hypoglycemia
• Fluid resuscitation
o First hour: isotonic saline solution (0.9% sodium chloride)
o Next 24–48 hours: Adjust IV fluid rate and composition according to CVP,
urine output, blood glucose, and corrected sodium levels.
o (at least 3-4 L in 8 hours)
Check corrected sodium for hyperglycemia.
• If corrected serum sodium ≥ 135 mmol/L: 0.45% NaCl
• If corrected serum sodium < 135 mmol/L: 0.9% NaCl
When serum glucose falls to < 200–250 mg/dL, add 5% dextrose to
infusion.
• Electrolyte repletion
o Potassium
Potassium levels must be ≥ 3.3 mEq/L before insulin therapy
If potassium level is < 3.3 mEq/L, potassium should be repleted and
rechecked prior to giving any insulin
If potassium level is < 5.3 mEq/L, the patient will likely require
potassium repletion once insulin therapy
o *Treat any hypophosphatemia or hypomagnesemia
• Insulin
o The administration of insulin is essential in halting lipolysis and ketoacidosis
in patients with DKA.
o Recommended regimens
IV regular insulin bolus 0.1U\kg , followed by continuous regular
insulin IV infusion 0.1U\kg\h
Or regular insulin continuous IV infusion without a bolus
Both options listed are valid approaches with advantages and
disadvantages. When in doubt, follow hospital standards.
2. Treatment of hypoglycemia
• If the patient is conscious:
Oral glucose 15–20 g
Fast-acting carbohydrates (such as glucose tablets, candy, or juice)
• If the patient is unconscious (or unable to ingest glucose)
IV dextrose 50% 25gr iv once
IM glucagon 0.5-1 mg once: if neither oral or IV routes of administering
glucose are feasible
Monitoring
• Recheck POC glucose after 15 minutes.
3. Treatment of diabetic retinopathy
• Screening
o Type 1 DM: initial dilated and comprehensive eye examination within 5 years after
the onset of diabetes and then annually
Type 2 DM: initial dilated and comprehensive eye examination at the time of the
diabetes diagnosis and then annually
Management
o General measurements
Blood sugar control
Blood pressure and serum lipid control to reduce the risk or slow the
progression of diabetic retinopathy
Invasive treatment
o Laser panretinal photocoagulation over the course of numerous appointments if
the patient has severe nonproliferative retinopathy or proliferative retinopathy
o Intravitreal anti-vascular endothelial growth factor (VEGF) injection
o Vitrectomy rarely done in case of traction retinal detachment and vitreal
hemorrhage
o
•
•
4. Treatment of diabetic nephropathy
• Stringent glycemic control
• Antihypertensive treatment
o ACE inhibitors OR angiotensin-receptor blockers are the first-line
antihypertensive drugs in patients with diabetes
o Second line agents to be added to ACE inhibitors or ARBs to further control
hypertension include diuretics or calcium channel blockers
o Annually test for albuminuria + eGFR, exclude other reasons for albuminuria
o Dose of diabetic drugs should be reduced with the progression of kidney
damage like (metformin, sulfonylureas)
o GLP-I agonist and SGLT1: improve glycemic control and reduce progression
to diabetic kidney disease
o Referral to transplantation evaluation when GFR < 20 ml/min
5. Diabetic neuropathy
• Distal symmetric polyneuropathy
o Treatment
Optimal glycemic control ,smoking cessation, stop alcohol
consumption,vit B12 supplementation
alpha lipoic acid
Pain management
• Anticonvulsants: pregabalin (most effective; usually first-choice),
gabapentin, and sodium valproate
• Antidepressants
o Tricyclic antidepressants: amitriptyline
o SNRI: duloxetine, venlafaxine
• Miscellaneous: lidocaine patch, capsaicin spray, isosorbide dinitrate
spray
• Opioids: dextromethorphan, morphine sulfate, tramadol, and
oxycodone
• Autonomic neuropathy:
o Treatment
Conservative (first-line)
• Glycemic control, dietary modifications
• Prokinetics (e.g., metoclopramide) and antiemetics (e.g.,
diphenhydramine, ondansetron)
Invasive (e.g., decompressive endoscopy): if conservative treatment fails
Surgery (e.g., venting gastrostomy or jejunostomy): refractory symptoms
o
Complications: electrolyte imbalance, malnutrition, increased risk of postprandial
hypoglycemia
6. Treatment of foot ulcers
• regular foot examination,smoking cessation, control of blood pressure and
dyslipidemia,improve glycemic control
• surgical debridement; regular wound dressing mechanical offloading (fitting of therapeutic
footwear or total contact cast); anti-B if foot ulcers become infected; interventional/surgical
revascularization (patients w/underlying peripheral a. disease); amputation if all else fails
or severe life-threatening complications arise
7. Treatment and prevention of macrovascular complications• prevention- smoking cessation, blood pressure control(ACE inhibitors as a first line),
glycemic control(GLP1 analogues and SGLT2 inhibitors have cardioprotective effect), treat
hyperlipidemia (statins) and healthy diet.
• aspirin should be considered
• revascularization procedures
160) Treatment with NSAIDs
Overview of NSAIDS
NSAIDS
COX-2
Other non-opiod
analgesics
Common agents
• Ibuprofen
• Diclofenac
• Indomethacin
• Naproxen
• Ketorolac
• Meloxicam
• Piroxicam
• Sulindac
• Aspirin
• Celecoxib
•
Acetaminophen
Activity profile
• Analgesic
• Antipyretic
• Anti-inflammatory
• Antiplatelet effect
•
•
Analgesic
Anti-inflammatory
•
•
Analgesic
Antipyretic
Ibuprofen:
• 400 mg every 4 to 6 hours or
• 600 to 800 mg every 6 to 8 hours
• Shorter-acting alternative to naproxen 500 mg twice daily.
• useful in patients without cardiovascular risks
Indomethacin:
• 25 to 50 mg every 8 to 12 hours Diclofenac: 50 mg every 8 to 12 hours
Mechanism of action
• Reversible inhibition of the enzymes COX-1 and COX-2 → decreased prostaglandin synthesis
• Aspirin is the exception because it leads to irreversible COX-1 and COX-2 inhibition.
Effects
• Analgesic
• Antipyretic
• Anti-inflammatory (antirheumatic)
• Minor antiplatelet function (with the exception of aspirin)
Side effects
• GI:
o Gastric and duodenal ulcers with the risk of gastrointestinal bleeding and
perforation (inhibition of COX disrupts the production of protective
gastric mucosal prostaglandins)
Risk increases with duration and dose of treatment
Prophylaxis: administration of proton pump inhibitors (in case long-term intake
is needed)
The risk of an ulcer is 10–15 times higher if NSAIDS and glucocorticoids are
administered simultaneously!
• Heart:
o Increased risk of heart attack and stroke (with the exception of aspirin and naproxen)
• Kidney:
o Renal function impairment: Prostaglandins normally maintain renal blood flow by
inducing vasodilation of the afferent arterioles. NSAIDS
inhibit prostaglandin production, which leads to harmful hypoperfusion of
the kidneys and reduced GFR.
o Analgesic nephropathy: prolonged NSAID use results in tubulointerstitial
nephritis and papillary necrosis (↑ urea/BUN ratio, slight ↑ K+)
• Blood:
o Aplastic anemia - indomethacin
• Skin:
o Pseudoallergic reactions
Urticaria and angioedema
Asthma
Aspirin-exacerbated respiratory disease (AERD)
Indications
Acute and chronic pain (particularly musculoskeletal)
o Rheumatoid arthritis
o Inflammatory arthritis
o Kawasaki disease
o Acute gout attack
o Post-operative pain
o Dysmenorrhoea
o Headache, migraine
Fever
Indomethacin: closure of a patent ductus arteriosus
Contraindications
• Gastroduodenal ulcers
• Acute hemorrhage (especially aspirin)
• Renal failure
• Recent myocardial infarction, unstable angina, heart failure
• Surgery: discontinue NSAIDs 1–3 days prior to surgery
• Avoid NSAIDs during pregnancy!
Selective COX-2 inhibitors
Agent
• Celecoxib: 200 mg daily or 100 mg every 12 hours, max dose 400 mg.
o Mechanism of action
Reversible selective inhibition of COX-2 with almost no inhibition of COX-1
• COX-2 is found in:
o Cells that mediate inflammation and pain (e.g., macrophages, leukocytes)
o Vascular endothelial cells (i.e., cells that control vasodilation)
Effects
• Analgesic and anti-inflammatory
• Advantages in comparison to nonselective NSAIDs
o No antiplatelet effect: platelets only possess COX-1 and are therefore not targeted by
selective COX-2 inhibitors. This means that the activity of thromboxane A2 (TXA2) is
not interrupted (TXA2 normally promotes platelet aggregation).
o Gastric mucosal cells express mostly COX-1, which is involved in maintaining a
healthy gastric mucosa, so there are minimal gastrointestinal side effects and a lower
risk of gastric ulcers.
Side effects
• Increased risk of thrombosis, MI, and/or stroke
• Sulfa drug allergic reaction
Indications
Rheumatoid arthritis, osteoarthritis, acute pain, nonrheumatoid joint pain
Especially as an alternative to nonselective NSAIDs for patients with a history of peptic
ulcer disease and platelet disorders (e.g., Glanzmann thrombasthenia
Contraindications
• Severe heart failure, recent myocardial infarction, gastrointestinal bleeding
• Sulfa drug allergy
Clinical pearls:
• NSAIDS should ideally be prescribed for short periods, of no more than 7-10 days. Especially
in elderly patients with preexisting cardiovascular problems and renal diseases.
• If we prescribe non-selective COX inhibitors prescribe PPI
• Renal effects: sodium and water retention
• Treatment initiation: Should be initiated with an agent known to have a low incidence of side
effects like Ibuprofen and Naproxen and if needed maybe continued with more potent agents
ex. Diclofenac, Ketoprofen.
Drug Interactions:
• Steroids - ↑ GI side effects
• Warfarin, DOAC - ↑ GI bleeding
• ACEi, Diuretics - ↑ renal impairment
• NSAID ↓ therapeutic effects of antiHTN medication
Special contraindications:
• Aspirin:
• Children< 16 yrs → Reye Syndrome
• Hypersensitivity
• 3rd TM of pregnancy → patent DA
• Gout → can trigger acute attack
• Use in caution in pts with PUD
161) Treatment in predialysis period of chronic renal failure and
indications for dialysis
Predialysis
eGFR category (mL/min/1.73 m2)
G1: ≥ 90 (normal or high)
G2: 60–89 (mildly low)
G3a: 45–59 (mildly to moderately low)
G3b: 30–44 (moderately to severely low)
G4: 15–29 (severely low)
G5: < 15 (kidney failure)
1. Approach
The goals of treatment are to delay the progression of CKD and prevent and manage
complications.
● Treat the underlying causes of CKD
● Start comprehensive management.
○ Provide recommendations regarding nutrition and vaccinations, and adjust current
medications as required.
○ Manage ASCVD risk factors.
○ Assess for evidence of metabolic complications and start management under
specialist guidance.
● Monitor for CKD progression and continuously evaluate the need for advanced care.
2. Nutritional management
● Fluid intake: Ensure appropriate fluid intake and avoid dehydration.
● Protein and energy consumption
○ Mediterranean diet, ↑ fruit and vegetable intake
○ Protein restriction (e.g., 0.55–0.60 g/kg/day) in patients with CKD category G3–G5
● Electrolytes
○ Sodium restriction (< 2.3 g/day)
○ Potassium intake adjustment
○ Phosphorus intake adjustment
● Micronutrients: Consider multivitamin supplementation for patients with inadequate dietary
vitamin (e.g., vitamin D) intake.
3. Vaccinations
Patients with CKD are at an increased risk of vaccine-preventable infections.
● Live attenuated vaccines: Consider offering the MMR vaccine and varicella vaccine to
patients who have not been vaccinated since infancy or do not have immunity.
● Non-live vaccines
○ Ensure influenza, pneumococcal, and hepatitis B vaccinations are up-to-date.
Patients with CKD may be immunocompromised. Decisions regarding the use of live vaccines should
therefore take into account the patient's current immune status and be made in consultation with a
specialist.
4. Medication management
● Renally cleared medications: Adjust dosing based on the patient's eGFR.
● Potentially nephrotoxic substances
○ Avoid use (except when the benefits outweigh the risks).
○ Contrast imaging
■ The risk of contrast-induced nephropathy is highest in patients with eGFR < 30
mL/min/1.73 m2.
Atherosclerotic cardiovascular disease (ASCVD) risk assessment and control of risk factors
● Blood pressure management:
○ Systolic blood pressure (SBP) target < 120 mm Hg is recommended (if tolerated
○ First-line therapy: RAAS inhibitors (i.e., ACEI or ARB)
■ Benefits: nephroprotection and reduced proteinuria
■ Risks: may cause hyperkalemia and/or an initial decline in GFR
Consider combination therapy (e.g., RAAS inhibitor PLUS a calcium channel
blocker and/or a thiazide diuretic):
■ For patients with an initial SBP ≥ 20 mm Hg above target
■ For patients who do not reach the target while on monotherapy at the optimal
dose
○ Second-line agents include:
■ Loop diuretics or thiazide diuretics
■ Calcium channel blockers (CCBs)
■ Beta-blockers: usually reserved for patients with cardiovascular comorbidities
■ Aldosterone receptor antagonists: usually reserved for treatment resistant
hypertension
Lipid management
○ Goal: reduction of ASCVD risk
○ Fasting lipid panel
○ Order at diagnosis and repeat only if the results may alter management.
○ May show dyslipidemia (↑ triglycerides are common)
Statin therapy
Diabetes management
○ Glycemic target (should be individualized)
○ HbA1c of ∼ 7% is appropriate for most patients.
■ Type 1 diabetes mellitus: Insulin therapy is the treatment of choice.
■ Type 2 diabetes mellitus
○ Choose first line antihyperglycemics based on the patient's eGFR category.
■ G1–G3b: metformin PLUS an SGLT-2 inhibitor
■ G4: GLP-1 receptor agonist
■ G5: DPP-4 inhibitor
Antiplatelet therapy
○ Usually indicated for secondary prevention of ASCVD
○ May be considered for primary prevention of ASCVD in high-risk individuals (e.g.,
patients with CKD and diabetes)
○
●
●
●
●
Complications management
● Anemia of chronic kidney disease
○ Consider erythropoietin-stimulating agents for patients with Hb < 10.0 g/dL
Treatment target: usually Hb concentration between 11 and 12 g/dL
○ Avoid blood transfusions: particularly in patients eligible for renal transplantation
(risk of alloimmunization)
○ Treatment with ESAs is not recommended for patients with Hb levels ≥ 10 g/dL
because their use has been associated with increased mortality, stroke, and venous
thromboembolism.
● Chronic kidney disease-mineral and bone disorder
○ Treatment: The goal is to normalize phosphate, calcium, and PTH levels.
■ Treatment of hyperphosphatemia, e.g.:
● Dietary phosphate restriction
● Phosphate binders (e.g., sevelamer)
■ Treatment of hyperparathyroidism, e.g.:
● Cholecalciferol or ergocalciferol supplementation for vitamin D
deficiency or insufficiency
● Calcitriol (not routinely recommended)
● Calcimimetics (e.g., cinacalcet)
● Parathyroidectomy (last-line therapy)
● Renal replacement therapy
○ Indications for dialysis
■
■
Nonoperative (hemodialysis or peritoneal dialysis)
● Indications include:
○ Hemodynamic or metabolic complications that are refractory to
medical therapy, e.g.:
■ Volume overload or hypertension
■ Metabolic acidosis
■ Hyperkalemia
○ Serositis: e.g., uremic pericarditis
○ Other symptoms of uremia: e.g., signs of encephalopathy
○ Refractory deterioration in nutritional status
Operative: kidney transplantation
Mnemonic for indications for dialysis: A-E-I-O-U → Acidosis, Electrolyte abnormalities
(hyperkalemia), Ingestion (of toxins), Overload (fluid), Uremic symptoms
162) Clinical and pharmacological approach in NSAIDs therapy.
SAME AS Q160
163) Treatment of bacterial infection
Goal of antimicrobial therapy:
Minimum = clinical care, prevention of complications, and at a reasonable cost
Maximum = all the above + eradication of the pathogen (prevention of the spread of resistant
bugs
Inappropriate antimicrobial use:
Inappropriate (over) prescription
Prescription not taken correctly
Anti-B for viral infections
Anti-B sold w/out medical supervision
Spread of resistant microbes in hospitals
Exposure to sub-optimal levels of antimicrobials
Before starting anti-B treatment:
1) Diagnosis of infection = localisation, causative agent (putative or proven), and community vs.
hospital acquired infections
2) Patients factors = age, sex, allergies, host defences (clinical state of the patient), renal and
hepatic function, concomitant meds (possible drug interactions) and diseases
3) Drug factors = antibacterial spectrum (narrow/broad), antibiotic potency (MIC90), mechanism
of action (bactericidal/bacteriostatic), PK (ADME), ADRs, drug interactions, convenience, cost
Types of antimicrobial therapy
Etiological/targeted/definitive treatment = treating the specific causative agent – the
causative bacteria is known due to microbiological testing.
Empirical treatment = medical treatment based on experience and, more specifically,
therapy begun on the basis on a clinical “educated guess” in the absence of complete or
perfect information. Thus, it is applied before the confirmation of a definitive diagnosis or w/out
complete understanding of the etiology; treatment is usually w/broad spectrum anti-B
Prophylactic treatment = the use of anti-B before surgery or a dental procedure to prevent a
bacterial infection
Sequential treatment = refers to the practice of limiting the use of IV (parenteral) anti-B to the
early stages of infection and then converting to oral agents for the duration of treatment OR
conversion of parenteral (IV) to oral anti-B treatment using the same medication.
Anti-B
Definition = antimicrobial drugs effective against bacteria
Narrow spectrum = an anti-B that is only able to kill/inhibit limited species of bacteria.
o E.g. natural penicillins, macrolides, lincosamides, oxazolidinones
Broad-spectrum = any anti-B that acts against a wide range of disease- causing bacteria.
E.g. semi-synthetic penicillins, carbapenems, cephalosporins, tetracyclines, quinolones,
sulphonamides
Bactericidal = Kills bacteria at drug serum levels achievable in the patient – drug of choice in
seriously ill patients
Bacteriostatic = arrests the growth and replication of bacteria – stops the bacteria from
reproducing while not necessarily killing them otherwise
As a general rule, agents that inhibit cell wall synthesis are bactericidal (except ethambutol),
while those that inhibit protein synthesis are bacteriostatic (except Tigecycline, rifamycins, and
aminoglycosides)
Anti-B are classified based on their mechanism of action:
Inhibitors of cell wall synthesis = β-lactam anti-B (penicillins, carbapenems,
cephalosporins, and monobactams); others (bacitracin, vancomycin)
Inhibitors of protein synthesis = aminoglycosides, tetracyclines, chloramphenicol,
clindamycin, macrolides
o MNEMONIC = AcTions at 30, CELebrations at 50: Aminoglycosides and Tetracyclines
are 30S inhibitors; Chloramphenicol/Clindamycin, macrolides (e.g. Erythromycin), and
Linezolid, are 50S inhibitors
Inhibitors of nucleic acid synthesis = fluoroquinolones, rifampin and rifabutin, and
metronidazole
Anti-metabolites = sulfonamides, trimethoprim Anti-B classes
1. Beta-Lactam Antibiotics (contain β-lactam ring)
Penicillins = natural (penicillin G and V); penicillinase-resistant (Cloxacillin, methicillin,
Nafcillin); aminopenicillins (amoxicillin, ampicillin); extended- spectrum (Piperacillin, Ticarcillin)
Use
o Gram-positive aerobes (esp. Streptococcus pyogenes, Streptococcus pneumoniae)
o Gram-negative cocci (esp. Neisseria meningitidis)
o Spirochetes (esp. Treponema pallidum)
o Branching gram-positive anaerobes (especially Actinomyces)
Cephalosporins = 1st gen (Cefazolin, cephalexin); 2nd gen (cefuroxime, cefoxitin); 3rd gen
(ceftriaxone, cefotaxime); 4th gen (cefepime);
Use
o Perioperative wound infection (S. aureus) prophylaxis
o Ceftriaxone specifically
Has good CNS penetrance: used to treat meningitis
Also used for gonorrhea and disseminated Lyme disease
Pharmacokinetics = widely distributed in body fluids, elimination mostly renal
Side effects = generally free from toxic effects, most common is allergy.
2. Carbapenem
All contain phenylpropanoid structure
E.g. = IV imipenem, meropenem, ertapenem
Use = as a last resort in life-threatning conditions
o Gram +ve cocci,
o Gram -ve rods- Pseudomonas aeruginosa
o Anerobes
Pharmacokinetics =IV
Side effects = secondary fungal infections, CNS toxicity
3. Monobactams: Aztreonam
Use =
o Effective against gram-negative bacteria only , including nosocomial Pseudomonas, H.
influenzae, and N. meningitidis
o Not effective against gram-positive rods or anaerobes
o Alternative for penicillin-allergic patients (no cross-sensitivity with penicillins)
o Can be used as an alternative to aminoglycosides for patients with renal insufficiency
because it is synergistic with aminoglycosides
o Broad-spectrum coverage in combination with vancomycin or clindamycin
4. Aminoglycosides
All contain an amino sugar substrate
E.g. = streptomycin, Gentamicin, neomycin, tobramycin, amikacin
Use =
o Severe gram-negative rod infections
o Not effective against anaerobes (aminoglycosides require oxygen to be absorbed by
cells)
o Neomycin, which is not absorbed systemically, is administered orally to prepare the
gut for bowel surgery.
o Streptomycin is used as a second-line treatment for Mycobacterium tuberculosis and
M. avium-intracellulare
Pharmacokinetics = highly polar, not absorbed in GI given IM or IV. Cross placenta but not
BBB, penetrate into most fluid compartments
Side effects = serious dose-related toxic effects (nephrotoxicity, ototoxicity), ↑ w/prolonged
treatment.
5. Amphenicols
All contain phenylpropanoid structure
E.g. = chloramphenicol, thiamphenicol, azidamfenicol and florfenicol
Use = effective against bacteria w/resistance to other drugs, cheap, used overseas
o Meningitis caused by H. influenzae, N. meningitidis, and/or S. pneumoniae
Rickettsia infections (e.g., Rocky Mountain spotted fever caused by Rickettsia
rickettsii)
Pharmacokinetics = oral, IV or topical admin
Side effects = severe aplastic anaemia can occur, rarely used as a result
6. Glycopeptides: Vancomycin, Teicoplanin
o
Use =
o especially effective against multidrug-resistant organisms
o Is effective against a wide range of gram-positive bacteria only
MRSA
S. epidermidis
Enterococci (if not vancomycin resistant enterococci)
C. difficile (causing pseudomembranous colitis): administered orally
Pharmacokinetics = oral, IV
Side effects = Nephrotoxicity, Ototoxicity/vestibular toxicity, Thrombophlebitis, DRESS
7. Lincosamides
Compounds isolated from Streptomyces lincolnensis
E.g. = lincomycin, clindamycin and pirlimycin
Use =
o Anaerobes, such as Clostridium perfringens, Bacteroides spp. (clindamycin is less
effective against Bacteroides than other anaerobic species)
Aspiration pneumonia
Lung abscesses
Oral infections
o Group A streptococcus: especially invasive infections
o Partially effective against gram-positive aerobes
Can be used in MRSA infections
Not effective against Enterococci
o Babesia (together with quinine) [45]
Pharmacokinetics = given orally and widely distributed in fluids, doesn’t cross BBB. Active
uptake into leukocytes, HL is 21 hours
Side effects = GI disturbances, lethal condition, pseudomembranous colitis may develop
8. Macrolides
Contain 14-, 15- or 16-membered macrolide ring
E.g. = erythromycin, clarithromycin, azithromycin
Use
o Atypical pneumonia caused by:
Mycoplasma pneumonia
Legionella pneumophila
Chlamydophila pneumoniae
o Bordetella pertussis
o STIs caused by Chlamydia
o Gram-positive cocci especially for the treatment of streptococcal infection in patients
who are allergic to penicillin)
o Neisseria spp.
Second-line prophylaxis for N. meningitidis
Dual therapy with ceftriaxone for N. gonorrhoeae (azithromycin)
o Mycobacterium avium
o
o
o
Prophylaxis: azithromycin
Treatment: azithromycin, clarithromycin
H. pylori (clarithromycin is the part of triple therapy )
Ureaplasma urealyticum
Babesia spp. (azithromycin in combination with atovaquone)
Pharmacokinetics = oral, widely distributed, doesn’t cross BBB. Erythromycin has short HL.
Side effects = GI disturbances, some HS rxns
9. Tetracyclines
Contain 4 adjacent cyclic hydrocarbon rings
E.g. tetracycline, doxycycline, minocycline
Use = wide use, G+ and G-, although ↑ resistance now
o Bacteria that lack a cell wall (e.g, Mycoplasma pneumoniae, Ureaplasma)
o Intracellular bacteria, such as Rickettsia, Chlamydia, or Anaplasma (tetracyclines
accumulate intracellularly and are, therefore, effective against intracellular pathogens)
o Borrelia burgdorferi
o Other: Ehrlichia, Vibrio cholerae, Francisella tularensis
o Cutibacterium acnes (topical tetracycline is used to treat acne) [31]
o Community-acquired MRSA (doxycycline)
Pharmacokinetics = oral, irregular and incomplete absorption (dairy products and iron salts ↓
absorption)
Side effects = GI disturbances most common, hazardous to pregnant women
10. Fluoroquinolones
All have bicyclic core structure related to 4-quinolone (fluoroquinolones)
E.g. = ciprofloxacin, levofloxacin, ofloxacin, norfloxacin, moxifloxacin
Use = broad-spectrum bactericidal, excellent use against G- enterobacteria
o Norfloxacin, ciprofloxacin, and ofloxacin
Gram-negative rods causing urinary and gastrointestinal infections
Some gram-positive pathogens
Genitourinary infections caused by Neisseria gonorrhoeae, Chlamydia
trachomatis, and/or Ureaplasma urealyticum
Ciprofloxacin: Pseudomonas aeruginosa (e.g., malignant otitis externa)
o Levofloxacin, moxifloxacin, and gemifloxacin:
Atypical bacteria (e.g., Legionella spp., Mycoplasma spp., Chlamydophila
pneumoniae)
Also effective against anaerobes
Gemifloxacin is highly potent against penicillin-resistant pneumococci.
Moxifloxacin: 2nd-line treatment of tuberculosis in patients who cannot tolerate
antitubercular drugs and in multidrug resistant tuberculosis
Pharmacokinetics = oral, well absorbed; accumulate in kidney, prostate and lungs, and picked
up by phagocytes
Side effects = infrequent and mild. Most common GI disturbance and skin rashes
11. Sulfonamides
All contain sulfonamide group
E.g. = Sulfadiazine, sulfamethoxazole, Sulfisoxazole
Action = prevent folic acid synthesis in bacteria, therefore preventing DNA replication (inhibit
cell replication)
Usage =
o
o
Common indications include UTIs and acute otitis media.
TMP/SMX
Shigella
Salmonella
Empiric treatment for simple UTI
Prophylaxis and treatment of P. jirovecii
Prophylaxis of toxoplasmosis
Pharmacokinetics = readily absorbed in GI tract, max concentration 4-6 hours. Pass across
BBB and metabolised in the liver
Side effects = N/V, headache, hemolytic and aplastic anaemia, photosensitivity,
12. Nitromedazole: Metronidazole, Tinidazole
E.g. = Oral/ IV: Metronidazole, Tinidazole
Action = Inhibits DNA replication, bactericidal and antiprotozoal effect
Usage =
o Certain protozoa (e.g., Entamoeba histolytica, Giardia, Trichomonas)
o Anaerobes(e.g., C. difficile, Bacteroides spp.)
o Facultative anaerobes
Gardnerella vaginalis
Helicobacter pylori in place of amoxicillin (e.g., in case of penicillin allergy) as
part of a triple therapy regimen#
o Not effective against aerobes
Side effects = headache, disulfiram like reaction w/ alcohol, metal taste, peripheral neuropathy
13. Nitrofurans: Nitrofurantoin
Action = Inhibits protein, DNA, RNA synthesis, bactericidal
Usage =
o Urinary tract pathogens
Gram-positive: Enterococci, Staphylococcus saprophyticus, group B
streptococcus, Staphylococcus aureus, Staphylococcus epidermidis
Gram-negative: E. coli, Enterobacter spp., Shigella spp., Salmonella spp.,
Citrobacter spp, Neisseria spp, Bacteroides spp., Klebsiella spp.
o Not effective against Pseudomonas and/or Proteus
o Clinical indications include:
Treatment and prophylaxis of acute uncomplicated UTIs (e.g., urethritis,
cystitis)
Asymptomatic bacteriuria or symptomatic UTI in pregnant women
Should not be used in (suspected) pyelonephritis because nitrofurantoin does
not achieve adequate concentration in renal tissue
Side effects = Pulmonary fibrosis, Hemolytic anemia in patients with G6PD deficiency, GI
upset, Reversible peripheral neuropathy
164) Treatment with diuretics
Types of diuretics
1) Osmotic
2) Carbonic Anhydrase inhibitors
3) Loop
4) Thiazide
5) Potassium sparing
Osmotic Diuretics
•
Agents
o Mannitol
o Urea
•
Mechanism of action
o Increase the osmolality of:
Serum: ↑ shift of water into the intravascular space → ↑ binding of water → ↓
intracranial and intraocular pressure
Glomerular filtrate: ↑ tubular fluid osmolarity → ↑ binding of water → ↑ urine
production
o No saluresis
•
Side effects
o
o
o
•
Indications
o
o
o
o
•
Dehydration
Initial cardiac volumetric strain
Metabolic and electrolyte imbalances
Effective glomerular filtration → hypernatremia
Ineffective glomerular filtration or administration of very high doses → ↑
plasma osmolality → ↑ extracellular fluid volume → pulmonary
edema, potassium fluctuations, hyponatremia or hypernatremia,
and/or metabolic acidosis
Elevated ICP (e.g., cerebral edema)
Acute glaucoma
Prevention of acute renal injury in cases of oliguria
Forced renal excretion of substances (e.g., drugs or toxins)
Contraindications
o Anuria
o Progressive heart failure
o Severe pulmonary edema
o Severe dehydration
Carbonic Anhydrase Inhibitors Diuretics
•
Agents
o Acetazolamide
•
Mechanism of action
o Inhibition of carbonic anhydrase in the following organs:
•
Kidney (in the proximal convoluted tubule): → ↑ H+ reabsorption and inhibition
of Na+/H+ exchange → ↑ NaHCO3 diuresis and ↑ HCO3- elimination →
compensatory hyperventilation; disinhibition of central chemoreceptors → ↑
oxygenation
Eyes: ↓ production of aqueous humor
Brain: ↓ CSF production
Acid-base effects: alkalinizes urine and acidifies blood
Side effects
o Hyperammonemia with paresthesias
o Proximal renal tubular acidosis → hyperchloremic, nonanion gap metabolic acidosis
o Hypokalemia
o
Sulfonamide hypersensitivity
o
o
•
Indications
o
o
o
o
o
•
Calcium phosphate stone formation (alkaline urine promotes precipitation)
Neuropathy
Acute glaucoma
Altitude sickness (counteracts respiratory alkalosis)
Idiopathic intracranial hypertension
Metabolic alkalosis
Prevention of cystine kidney stones
Contraindications
o Hyperchloremic metabolic acidosis
o Severe renal insufficiency
o Adrenocortical insufficiency
o Hyponatremia, hypokalemia
o Hepatic disease or insufficiency
o
Long-term use in glaucoma
Loop Diuretics
•
Agents
o Sulfonamides: furosemide, torsemide, bumetanide
o Other: ethacrynic acid
•
Mechanism of action
o
o
o
•
Side effects
o
o
o
o
•
Blockage of Na+-K+-2Cl-cotransporter in the thick ascending loop of Henle
Diminishing concentration gradient between the (usually hypertonic) renal
medulla and the cortex → concentration of urine is no longer possible →
increased diuresis
Decreased reabsorption of Ca2+ and Mg2+
Increased PGE release (can be inhibited by NSAIDs)
Dilation of renal afferent arterioles → diuresis
General venodilation (rapid venous pooling) → ↓ cardiac preload
See “Mechanism of blood pH” changes in “Overview of diuretics” for mechanism of
alkalosis.
Metabolic imbalances
Hypokalemia, hypomagnesemia, hypocalcemia, hypochloremia, hyponatremia
(moderate)
Metabolic alkalosis
Hyperuricemia/gout
Hyperglycemia
Ototoxicity (potentially permanent hearing damage): especially high risk with
ethacrynic acid
Dehydration/hypovolemia
Sulfonamide hypersensitivity (except ethacrynic acid, which can be used for diuresis in
patients with allergies to sulfonamides) → rash, interstitial nephritis
Indications
o
o
Hypertension
Edema
Cardiac (acute and congestive heart failure, peripheral edema, lung edema)
o
o
o
o
•
Renal (nephrotic syndrome)
Hepatic (liver cirrhosis)
Renal failure (acute and chronic)
Hypercalcemia
Forced diuresis
Definition: massive diuresis for forced renal elimination of (toxic) substances
Implementation: IV administration of large amounts of fluids in combination with
loop diuretics
Indications: hypercalcemic crisis, severe hyperkalemia, rhabdomyolysis,
intoxication (e.g., lithium)
Sequential nephron blockade
Used to overcome resistance to diuretic treatment
Method: combination of loop diuretics and thiazides → restoration of diuretic
effects
Contraindications
o Furosemide
Anuria
Sulfonamide Hypersensitivity
Thiazide Diuretics
•
Agents
o
o
o
o
•
Mechanism of action
o
o
o
o
o
•
Inhibition of Na+-Cl- cotransporters in the early distal convoluted tubule → ↑ excretion
of Na+ (saluresis) and Cl- → ↓ diluting capacity of nephron and ↑ excretion of
potassium (kaliuresis) and ↓ excretion of calcium → diuresis
Increased reabsorption of Ca2+
Hyperpolarization of smooth muscle cells → vasodilation
Hyperpolarization of pancreatic beta cells → decreased insulin release
See “Mechanism of blood pH” changes in “Overview of diuretics” for mechanism of
alkalosis.
Side effects
o Metabolic Hypokalemia and metabolic alkalosis
o
o
o
o
o
o
o
•
Hydrochlorothiazide (HCTZ)
Chlorthalidone
Chlorothiazide
Metolazone
Hyponatremia
Hypomagnesemia
Hypercalcemia
Hyperglycemia
Hyperlipidemia (↑ cholesterol, triglycerides)
Hyperuricemia
Allergic reactions (sulfonamide hypersensitivity)
Indications
o Hypertension
o Chronic edema secondary to congestive heart failure, cirrhosis, and kidney disease
o Prevention of calcium kidney stones, idiopathic hypercalciuria
o
o
o
•
Contraindications
o
o
o
o
•
Osteoporosis
Nephrogenic diabetes insipidus
Sequential nephron blockade
Hypersensitivity (including hypersensitivity to any sulfonamide medications)
Gout
Anuria
Severe hypokalemia
Interactions
o Glucocorticoids: increased hypokalemia
o Carbamazepine: increased hyponatremia
o Lithium: increased hyponatremia
o ACE inhibitors: hypotension (especially first-dose hypotension)
o Propranolol: increased hyperlipidemia and hyperglycemia
o
o
NSAIDs: decreased diuretic effect
Increased effects of digitalis , methotrexate, and lithium
Potassium Sparing Diuretics
•
Agents
o Aldosterone receptor antagonists: spironolactone, eplerenone
o Epithelial sodium channel blockers: triamterene, amiloride
•
Mechanism of action
o
o
Although the molecular pathways differ, both types of potassium-sparing diuretics
have very similar clinical effects.
Aldosterone receptor antagonists (spironolactone, eplerenone)
Competitively bind to aldosterone receptors in the late distal convoluted tubule
and the collecting duct → inhibition of the effects of aldosterone → decreased
Na+ reabsorption and K+ excretion → diuresis
Decreased H+ excretion → acidosis
Evolving hyperkalemia induces H+/K+-ATPases in all cells to counteract the
increase in serum K+ → K+ enters cells in exchange for H+ → amplifies
acidosis
Spironolactone also acts (nonspecifically) on sex hormone receptors →
endocrine side effects (see section “Gonads” in “General endocrinology” for
more information about hormonal effects of spironolactone)
Epithelial sodium channel blockers (triamterene, amiloride): direct inhibition of the
epithelial sodium channels (ENaC) in the distal convoluted tubule and the collecting
duct → reduced Na+ reabsorption and reduced K+ secretion → diuresis
•
Side effects
o General side effects
Metabolic and electrolyte imbalances, such as hyperkalemia, hyponatremia,
and metabolic acidosis, can lead to cardiac arrhythmias
Gastrointestinal disturbances (nausea, vomiting, diarrhea)
o Spironolactone-specific side effects: endocrine disturbances
Men: antiandrogenic effects (e.g., gynecomastia, erectile dysfunction)
Women: amenorrhea
•
Indications
o
o
o
o
o
o
•
Hypertension (especially if hypokalemia is also present)
Ascites/edema due to congestive heart failure, nephrotic syndrome, or cirrhosis of the
liver (mainly spironolactone)
Hyperaldosteronism (Conn syndrome)
Nephrogenic diabetes insipidus (amiloride)
Hypokalemia
Hyperandrogenic states, e.g., polycystic ovary syndrome (spironolactone)
Contraindications
o
o
General
Anuria and/or renal insufficiency
Preexisting hyperkalemia
Addison disease
Combination with other potassium-sparing diuretics or potassium supplements
Specific
Spironolactone: Use with caution in patients with CHF with either of the
following:
•
GFR < 30 mL/min
• Creatinine ≥ 2.5 mg/dL (men) or ≥ 2 mg/dL (women)
Amiloride: diabetic nephropathy’s
165) Treatment with steroids
Definition:
● Synthetic glucocorticoids are a group of drugs with:
○ antiinflammatory
○ immunosuppressant
○ antiallergic
○ metabolic, and endocrine effects.
● These drugs are structurally and functionally similar to the endogenous glucocorticoid
hormone cortisol.
● Glucocorticoids have immediate effects (e.g., vasoconstriction) that do not depend on DNA
interaction. However, they exert their main antiinflammatory and immunosuppressive actions
by binding to glucocorticoid receptors, which causes complex changes in gene transcription.
● Systemic corticosteroids
○ Corticosteroids that are administered orally, intravenously, or intramuscularly
○ Act systemically as they are distributed throughout the body
● Local corticosteroids (local glucocorticoids)
○ Corticosteroids that are administered topically, intraarticularly, as eye/ear drops, or are
aerosolized and inhaled (inhaled corticosteroids)
○ Act primarily at the site administered; a fraction is systemically absorbed
○ Examples: beclomethasone, budesonide, clobetasol, and fluticasone
● Potency of systemic corticosteroids
○ Hydrocortisone is the synthetic equivalent of endogenous cortisol and its
glucocorticoid and mineralocorticoid potency is considered to be “1” .
○ Relative to hydrocortisone, systemic corticosteroids differ in potency of their
glucocorticoid differ in potency of their glucocorticoid effects (relative glucocorticoid
potency) and mineralocorticoid effects (relative mineralocorticoid potency) for a given
dose.
Indications:
●
Replacement therapy →using doses close to the physiological needs (ie. 20-30mg
hydrocortisone)
○ Adrenocortical insufficiency (Addison disease)
○ Congenital adrenal hyperplasia
○ Hypopituitarism
●
Systemic symptomatic treatment
○ Acute
■ Allergic reactions and anaphylactic shock
■ Asthma
■ Antiemetic treatment
■ Acute exacerbation of autoimmune diseases
■ Gout, calcium pyrophosphate deposition disease
■ Cerebral edema
■ Thyroid storm:cortisol inhibits the peripheral conversion of T4 to T3 (the
inactive byproduct of T4, rT3, increases)
■ Acute pericarditis
○ Long-term
■ Chronic, inflammatory diseases; asthma; chronic obstructive pulmonary
disease; inflammatory bowel disease; vasculitides
■ Rheumatic diseases
■ Graves ophthalmopathy
■ Malignancy (e.g., CLL, non-Hodgkin lymphoma)
●
Local symptomatic treatment:
○ anterior uveitis; dermatoses; tenosynovitis; osteoarthritis
●
Prophylactic
○ Organ transplant
●
Preterm delivery:
○ Glucocorticoids are given to the mother prenatally to induce fetal lung maturity
●
Dosage depends on the treatment approach. There isn’t one fixed dose for all diseases.
Sometimes there is pulse therapy and sometimes there is only one tablett given or inhalation
and sometimes if long term use - they can be given in alternating days (once in 48hrs) etc. (for
pathogenetic therapy with corticosteroids dose is 1 - 2 mg/kg/24hr usually in the morning)
● Pulse therapy = venous infusion of high dose glucocorticoids (eg. 300-1000mg
methylprednisolone in 100-200ml physiological solution for around 20 min for 3-5 consecutive
days). it could be followed by conventional oral glucocorticoid therapy
● toward the end of treatment slowly taper/reduce the dose (eg with 5mg prednisolone every 15
days)
Relative potency of systemic corticosteroids
Duration of action
Drug
Common routes of
administration
Systemic glucocorticoids
Short-acting
Hydrocortisone
Oral
(8–12 hours)
Injectable
Topical
Cortisone
Oral
Injectable
Intermediate-acting
Prednisolone
Oral
(12–36 hours)
Prednisone
Oral
Injectable
Methylprednisolone
Oral
Long-acting
36–72 hours
Dexamethasone
Betamethasone
Systemic mineralocorticoid
Intermediate-acting
12–36 hours
Fludrocortisone
Injectable
Oral
Injectable
Topical
Oral
Injectable
Topical
Oral
Side effects• Skin-Poor wound healing, skin atrophy, and stretch marks due to impaired fibroblast activity
and thus, impaired collagen synthesis, Purpura, Steroid acne, Hypertrichosis, Increased risk
of squamous and basal cell carcinomas
• Cardiovascular system-Hypertension
• Metabolism, electrolytes and endocrine systemo Weight gain with truncal obesity, buffalo hump, and moon face (Cushingoid
appearance)
o Proteolysis and lipolysis: proteolysis contributes to hyperglycemia whereas lipolysis
leads to hyperlipidemia and eventually to redistribution of fat tissue towards the trunk.
o Increased gluconeogenesis, lipolysis, and proteolysis
o Hyperglycemia and ↑ insulin resistance → glucocorticoid-induced diabetes
o Decreased glucose utilization in skeletal muscle and white adipose tissue (due to
antagonization of insulin response)
o Hypocalcemia → PTH activation → secondary osteoporosis
o Women: e.g., amenorrhea, hirsutism, breast atrophy, deep voice, androgenic alopecia
o Men: e.g., gynecomastia, acne, small testes, low sperm density (due to inhibition of the
hypothalamic-pituitary-gonadal axis)
o Adrenocortical atrophy, Acute adrenal insufficiency (predominantly when
glucocorticoids are discontinued suddenly after chronic intake)
• GI systemo Increased appetite, Peptic ulcers and gastrointestinal hemorrhage, Possibly
pancreatitis
o Hepatic damage
• CNS and psyche-Mood disorders, Cognitive disorders ,Psychosis
• Eyes- Cataract, Glaucoma
• Bone, muscle, tendon
o Avascular bone necrosis
o Osteoporosis, osteopenia
o Corticosteroid-induced myopathy
o Tendon ruptures
• Venous thromboembolism
o Growth inhibition in children
o Immunosuppression-Can result in the reactivation of latent infectious diseases (e.g.,
CMV, tuberculosis) and opportunistic infections (e.g., candidiasis),Blood test may
show leukocytosis since white blood cells get demarginalized.
• Cardiovascular: ↑ heart rate, ↑ blood pressure
Systemic administration
★ Tapering to avoid toxicity
★ Sudden discontinuation after chronic use should be avoided because of the risk of adrenal
insufficiency (adrenal crisis) secondary to long-term hypothalamic-pituitary-adrenal axis
suppression.
Contraindications:
● General: hypersensitivity
● Systemic-Systemic fungal infections
● Topical-Dermatological: bacterial, viral or fungal infection of the mouth or throat
(triamcinolone)
● Inhalation: status asthmaticus or acute asthma episode requiring intensive measures
(beclomethasone, budesonide)
● Relative contraindications: Glucocorticoids should be avoided in certain conditions due to
increased risk of toxicity.
○ Adrenocortical atrophy,
○ Cushing syndrome,
○ Diabetes mellitus (steroid diabetes),
○ hyperglycemia,
○ Amenorrhea,
○ Osteoporosis, Avascular necrosis (e.g., of the femoral head),
○ Peptic ulcers,
○ Cataracts,
○ Psychosis
166) Treatment with immunomodulators
Immunosuppressants use heterogeneous mechanisms of action to suppress the body's cellmediated and humoral immune response.
● They may be used as transplant rejection prophylaxis or to treat autoimmune disorders
such as lupus, psoriasis, and rheumatoid arthritis
● A common side effect of long-term immunosuppressants use is an increased susceptibility to
infection and malignancy
The main task of this type of treatment is
● to eliminate the immune abnormalities underlying the manifestations of the disease,
● as well as to prevent the subsequent occurrence of such changes.
● In order to achieve it, it is necessary to restore the regulation of the immune response
Classification
1. Cytotoxic agents (classical cytostatics):
• Antimetabolites
o Folic acid analogues (Methotrexate)
o Purine analogues (Azathioprine, Mycophenolate mofetil, etc.)
• Alkylating (Cyclophosphamide, Chlorambucil, etc.)
7. Selectively acting:
o Cyclosporin A, Tacrolimus (calcineurin inhibitors)
3. High doses of immunoglobulin G intravenously
4. Antilymphocytic serum (antilymphocytic and anti-thymocytic antibodies)
5. Monoclonal antibodies
6. Glucocorticoids
7. New immunosuppressants:
• Rapamycin (Sirolimus) which are mTOR Inhibitors,
• 15-Deoxyspergalin, Leflunomid, Mizoribin, Breqinar natrii, Tepoxalin. Are used in organ
transplantions
8. Fish oil. – 8-12g/day – inhibits production of cytokines and eicosanoids
Immunosuppression can be
• specific - an impact on the immune response of the body as a whole.
• nonspecific - effect in relation to a specific immune response and aims to develop an immune
tolerance.
• Most medicines in the group have a small therapeutic index (optimal effect is achieved with a
dose close to the toxic one), therefore strict monitoring of the patient is necessary
• All cytostatic agents that are used as immunosuppressives are usually administered at a
lower dosage than in cancer treatment. They act primarily by inhibiting the clonal expansion of
B and T cells
1. Methotrexate – starting with 7.5 mg/w and adjusted according to the effects
• Mechanism of action: Folic acid antagonist (antimetabolite) by inhibition of dihydrofolate
reductase (DHFR) ↓ pyrimidine and purine nucleotide synthesis → ↓ DNA synthesis
• Uses: Severe psoriasis, RA, gestational choriocarcinoma
• SE: pancytopenia, hepto and nephrotoxic , GI SE folic acid intake 1hr before intake may
decrease the toxicity
2. Azathioprine: - 1.5-2mg/kg for 24hr po
• Mechanism; 1- Purine analog (antimetabolite precursor of 6-mercaptopurine) → ↓ nucleotide
(DNA) synthesis → ↓ proliferation of lymphocytes
o 2- Cytostatic effect at high doses via inhibition of cell proliferation
o 3- Immunosuppressive effect at low doses
• Used for prophylaxis against renal transplant rejection, RA, Crohn’s, GNs and to wean pts off
long term steroid therapy
• SE; hepatotoxic, pancytopenia
3. Mycophenolate mofetil: 1g q12hr
• Mechanism: IMDH/IMPDH inhibitor blockade of purine synthesis→selective inhibition of
lymphocyte proliferation
• Used for: lupus nephritis and rheumatic dis., GNs In combination with cyclosporine for
transplant rejection
• SE: pancytopenia
4. Cyclophosphamide – IV pulse – 1g slow infusion през 7-15 days х 4 times or the same dose 1 time
in 30 days for 6months duration
•
•
•
Mechanism: alkylation of DNA/RNA→ cross-linking and strand breaks→ impaired DNA
synthesis affects mostly T and B cells
Use: SLE, Autoimmune hemolytic anemia, GNs
SE: pancytopenia SIADH , Hemorrhagic cystitis
5. Chlorambucil – 0.15- 0.2mg/kg
• Mechanism: alkylation of DNA/RNA
• Uses: alterantive to cyclophosphamide
6. Calcineurin inhibitors:
• Cyclosporin A – 3-5mg/kg q12hr po
o Mechanism: (Calcineurin inhibitor) 1. Immunosuppression: binding of cyclophilin→
inhibition of calcineurin→ ↓ IL-2 transcription → ↓ activation of T cells
Cytostatic action: binding to multidrug resistance glycoprotein P-170
o Uses: Transplant rejection prophylaxis, Psoriasis, RA, SLE, Vasculitis, GNs,
o SE: nephron and neuro toxic, diabetogenic, gingival hyperplasia, hypertrichosis,
hirsutism, hyperuricemia
• Tacrolimus (FK 506) : 0.15mg/kg q12hr
o Mechanism: (Calcineurin inhibitor) Binding to FK506 binding protein - ↓ IL-2
transcription → ↓ activation of T cells
o Uses: transplant rejection prophylaxis, psoriasis, SLE, resistant nephrotic syndrome
o SE: HTN, hair loss, nephrotoxic
o All of the above are contraindicated in Pregnant, allergic, severe infections and
cytopenia
7. IV Immunoglobulins: - 0.25 – 0.5g/kg divided in 3 parts slowly infused every other day
• Mechanism: block Fc receptors of monocytes, inhibit t and b cell function, inhibit cytokine
production
• Uses; SLE, RA, GNs, alternative therapy for pts that didn’t respond other treatment
• IVIG is Immune globulin derived from the plasma of paid donors is used in the treatment of
an array of disorders, including primary and secondary immune deficiency states and a variety
of autoimmune and inflammatory disorders.
• IVIG – IVIG has a number of immunosuppressive and antiinflammatory properties that include
modulation of immunoglobulin G (IgG) levels, lymphocyte and reticuloendothelial function,
cytokine production, complement regulation, and clearance of pathogenic IgG. IVIG provides
adequate concentrations of antibodies against a broad range of pathogens for patients with
hypogammaglobulinemia, antibody deficiency disorders, other immunodeficiency states, and
certain infections.
8. Monoclonal antibodies:
• SE; General side effects, including: Formation of anti-drug antibodies, Flu-like symptoms,
infections (e.g., nasopharyngitis), ↑ ALT, ↑ AST, Rash, dermatitis,GI upset
• Rituximab: Anti CD20
o Indications: RA, ITP, TTP. MS, AIHA, Bcell non Hodgkin lymphoma – CLL,
• Infliximab – 3mg/kg iv, Adalimumab – 40mg sc (q2 weeks?), Etanercept – 25mg sc 2 times
a week: Anti – TNF-a
o Indications: Refractory-therapy for chronic inflammatory systemic disease: RA
ankylosing spondylitis, psoriasis, psoriatic arthritis. Crohn’s, Ulcerative colitis,
• Tocilizumab: anti IL-6 receptor
o ( which leads to a reduction in cytokine and acute phase reactant production.)
o Indications: Giant cell arthritis, RA, juvenile idiopathic arthritis
• Ustekinumab: anti IL-12, IL-23
o Indications: psoriatic arthritis
•
•
Bevacizumab: anti VEGF (inhibits angiogenesis)
o Indications: proliferative diabetic retinopathy, Colorectal and renal cell carcinoma and
non small cell lung cancer
Denusumab; anti RANKL
o Indications: Osteoporosis
o SE: hypocalcemia
Immunostimulants:
These are immunomodulators with predominantly immunostimulating properties found in the
treatment of chronic infections, immunodeficiency conditions and malignant neoplasms.
1. BCG
• in addition to the specific effect on tuberculous bacterium, it also creates a non-specific
effect on the causative agents of normal infectious diseases.
• It can be injected directly into skin metastases or installations in the bladder in carcinoma
there, as well as administered intrapleural in lye due to metastases.
2. Recombinant Interleukins 2
• Parenteral and local in tumors of bladder, ovaries, melanoma
3. Interferons: a-2a, a-2b, n3… - 1.5- 20 or more million Ul depending on the type of tumor
taken for months
• Increase phagocytic activity of macrophages, N K-cell activity, T-lymphocytic cytotoxicity,
the synthesis of antibodies from B-cells.
• Used for basal cell carcinoma, CML, Kaposi sarcoma, renal cell carcinoma, malignant
melanoma
4. Levamisol
• Increases the production of lymphokinin? Activating proliferation of T lymphocytes
167) Treatment with cytostatics
Cytostatic drugs slow down or stop the growth of specific cells by inhibiting their cell division.
Depending on their specific mechanism of action, cytostatic drugs interfere with cell division in
different ways, for example by disturbing the metabolism or by damaging the DNA of a cell.
Cytostatics do not have a local effect on specific parts of the body but rather affect the whole
organism. Their targets are especially those cells that are growing very fast.
Clinical Use
• Cytostatics are primarily used in cancer treatment. Within chemotherapy they are applied as
active agents to fight against the fast spreading tumor cells and thereby inhibiting tumor
growth totally at best.
Routes of administration
The most common route of administration for chemotherapy is intravenous; other important
methods of delivery include oral, intrathecal, and topical application.
● Topical
○ Used in the treatment of cancerous or precancerous skin lesions
○ Chemotherapeutic agents that can be administered topically include 5-FU and
mitomycin.
● Intrathecal administration
○ The aim of intrathecal administration is to prevent the need for cerebral radiation
therapy and to treat meningeal disseminated diseases (e.g., meningeal
leukemia/lymphoma)
○ Chemotherapeutic agents that can be injected intrathecally include methotrexate and
cytarabine.
● Oral administration
○ Allows for ambulatory treatment, e.g., maintenance therapy, palliative treatment
○ Chemotherapeutic agents that can be administered orally include idarubicin,
capecitabine, temozolomide, etoposide, methotrexate, 6-MP.
Different types of cytostatics:
Alkylating agents:
• These agents act directly on DNA, resulting in its crosslinking and causing DNA strand
breaks, leading to abnormal base pairing, and inhibiting cell division, eventually resulting in
cell death.
• Alkylation of DNA/RNA → cross-links DNA at guanine N–7 → ↓ DNA replication
• Examples:
o Oxazaphosphorines: Cyclophosphamide
Malignancies: Solid tumors (e.g., breast cancer, ovarian cancer, small cell lung
cancer) Leukemias, Lymphomas, Multiple myeloma
Non-Neoplastic conditions: Autoimmune diseases (e.g., systemic lupus
erythematosus, granulomatosis with polyangiitis)
o Nitrogen mustards: Chlorambucil
Chronic lymphocytic leukemia Hodgkin lymphoma Non-Hodgkin lymphoma
o Platinum-based agents: Cisplatin, Carboplatin, Oxaliplatin
Lymphomas, bladder cancer, ovarian cancer, testicular cancer, colorectal
cancer, cervical cancer.
Antitumor antibiotics:
• Bleomycin
o Induces formation of free radicals → breakage of DNA strand
o (squamous cell carcinoma of the head and neck, hodgkin lymphoma, testicular cancer)
• Actinomycin D
o DNA intercalation → interference with DNA transcription → ↓ RNA synthesis
o (childhood tumors(wilms tumor), gestational trophoblastic neoplasia)
• Anthracyclines: doxorubicin
o Inhibition of topoisomerase II → ↑ DNA degradation (dsDNA breaks) and ↓ DNA
replication
o Formation of free radicals → breakage of DNA strands
o DNA intercalation → breakage of DNA strands and ↓ DNA replication
o (breast cancer, metastatic solid tumors, lymphomas, kaposi sarcoma, osteosarcoma)
• Mitomycin
o Cross-linking between DNA strands → ↓ DNA and RNA synthesis
o (bladder cancer, palliative chemotherapy of gastric and pancreatic cancer)
Mitotic inhibitors:
• Mitotic inhibitors interfere with the assembly and disassembly of tubulin into microtubule
polymers. This interrupts cell division, usually during the mitosis phase of the cell cycle
• Types:
o Vinca alkaloids: Vincristine
Binding of β-tubulin → inhibition of β-tubulin polymerization into microtubules→
prevention of mitotic spindle formation → mitotic arrest of the cell in metaphase
(M-phase)
(Hodgkin lymphoma, NHL, ALL, some solid tumors)
o Taxanes: Docetaxel
Hyperstabilization of polymerized microtubules → ↓ mitotic spindles breakdown
→ mitotic arrest in metaphase (not proceeding to anaphase)
(Breast cancer, Ovarian cancer, Prostate cancer, Gastric cancer, Kaposi
sarcoma, NSCLC)
o Non Taxane microtubule inhibitors: Eribulin
Inhibition of mitotic spindle formation → mitotic blockage → cell cycle arrest at
the G2/M phase
(breast cancer, liposarcoma)
Topoisomerase inhibitors:
• Topoisomerase I inhibitors: irinotecan
o Inhibition of topoisomerase I → ↓ DNA unwinding → ↓ DNA replication and DNA
degradation
o Example: topotecan (cervical cancer, small-cell lung cancer, ovarian cancer)
• Topoisomerase II inhibitors- Etoposide
• Inhibition of topoisomerase II → ↑ DNA degradation (dsDNA breaks) and ↓ DNA
replication
• Example: etoposide (lymphomas, leukemias, small-cell lung cancer, testicular cancer)
Antimetabolites:
• Antifolates: Methotrexate
o Competitive inhibition of dihydrofolate reductase via displacement of dihydrofolate →
↓ formation of pyrimidine nucleotides (↓ dTMP) and purine nucleotides → ↓ DNA
synthesis
o Neoplastic conditions
o Leukemias (especially ALL)
o Lymphomas (e.g., cutaneous T-cell lymphoma, non-Hodgkin lymphomas)
o Sarcomas
o Choriocarcinoma
o Breast cancer
o Head and neck cancers (e.g., squamous cell carcinoma)
o Lung cancer
o Immunosuppression for autoimmune diseases (e.g., rheumatoid arthritis,
inflammatory bowel disease, psoriasis, vasculitides)
• Purine antagonists: Azathioprine
o Incorporation of purine analog (thiol analog) into DNA → ↓ DNA synthesis
o For ALL and other non neoplastic disorders: IBD, RA, SLE
• Pyrimidine antagonists: Cytarabine, Fludarabine, 5-fluorouracil
o Incorporation of pyrimidine analog into DNA→ ↓ DNA synthesis
o (leukemias, lymphomas)
• Ribonucleotide reductase inhibitors: Hydroxyurea
o Inhibition of ribonucleotide reductase → ↓ DNA replication (S phase)
o (CML, polycythemia vera, head and neck cancers)
Other cytostatic drugs:
• L-asparaginase:
• Cleavage of the amino acid L-asparagine by L-asparaginase → ↓ asparagine source for
leukemic cells → cytotoxicity specific to leukemic cell (Used for acute lymphoblastic leukemia
Combination therapy
Chemotherapeutic agents are usually used in combination (combined chemotherapy regimens).
● Advantages
○ Increased log-kill
○ Prevention and counteraction of cancer drug resistance
○ Targeting both dividing and resting cells (in combination of cell cycle-specific and cell
cycle-nonspecific agents)
○ Synergistic effects allow for lower doses and, subsequently, less toxicity
● Examples
○ CHOP (or R-CHOP) for the treatment of non-Hodgkin lymphomas
○ ABVD for the treatment of Hodgkin lymphomas
○ FOLFOX, FOLFIRI, or XELOX for the treatment of colorectal cancer.
General side effects of cytostatics that are used in chemotherapy:
Chemotherapeutic agents damage actively dividing cells but can also affect tissues with a low mitotic
potential (e.g., neurons).
•
•
•
•
Gastrointestinal tract
o Chemotherapy-induced nausea and vomiting
o Chemotherapy-induced diarrhea
o Mucositis (soft tissue erythema of the buccal mucosa, gingival bleeding, multiple
shallow ulcerations, and dysphagia)
Blood
o Myelosuppression
o Granulocytopenia and lymphocytopenia (increased risk of infection)
o Thrombocytopenia (increased risk of bleeding)
o Anemia (fatigue)
Skin-Hair loss
CNS
o Centrally induced vomiting
o Chemotherapy-induced peripheral neuropathy
o Pain, burning, tingling, and loss of sensation in the distal extremities that spread from
the hands and feet (stocking-glove pattern).
Sexual organs
o Gonadal damage that may lead to temporary azoospermia, premature ovarian failure,
and infertility
168) Treatment of the thromboembolism
Treatment of pulmonary thromboembolism and DVT
Approach
● Stabilize the patient and provide supportive care.
● Pulseless patient with suspected PE: Start ACLS and consider administration of thrombolytics
(e.g., tPA → Alteplase 50 mg IV push)
● Assess bleeding risk with HASBLED score.
● Consider empiric parenteral anticoagulation while awaiting a definitive diagnosis.
● Risk stratify, patient based on prognostic models.
● Initiate therapy based on risk stratification and bleeding risk.
●
●
Submassive and non-massive PE: anticoagulation or IVC filter
Massive PE: thrombolytic therapy or embolectomy
Supportive care
● Hemodynamic support: in patients with hypotension and obstructive shock
○ IV fluids, Gentle bolus (e.g., normal saline ≤ 500 mL)
● Avoid volume overload, which may be harmful in cases of right ventricular strain
●
●
●
Consider vasopressors (norepinephrine is most commonly used) if there is no improvement
following fluid administration.
Respiratory support
○ Oxygen supplementation in patients with SpO2 < 90%
○ For patients with respiratory failure: airway management and/or mechanical ventilation
Analgesics: for patients with pain
○ Avoid NSAIDs if patient receiving anticoagulation or thrombolytics
○ Consider one of the following: Morphine, Oxycodone
Empiric parenteral anticoagulation for pulmonary embolism
● Indications: consider starting empiric anticoagulation in patients awaiting a definitive
diagnosis, depending on the risk of bleeding, the pretest probability of PE (wells score), and
the expected timing of the diagnostic study.
● High probability of PE
●
Absolute contraindication: high bleeding risk
○ Stable patients:
■ LMWH → Enoxaparin: 1.5 mg/kg SQ daily
○ Unstable patients or patients with renal insufficiency:
■ UFH → Heparin 80 units/kg IV bolus, then 18 units/kg/hour IV infusion
■ with aPTT or anti-Xa monitoring
Treatment of massive pulmonary embolism
Initiate directed therapy based on bleeding risk and the presence of any contraindications to
thrombolytic therapy in massive pulmonary embolism.
Low bleeding risk: systemic thrombolytic therapy
High bleeding risk: catheter-directed thrombolytic therapy
If thrombolytic therapy is contraindicated or unsuccessful: embolectomy
Systemic thrombolysis
•
Thrombolysis, preferably with recombinant tissue-type plasminogen activator (tPA), e.
o
o
•
Alteplase 100 mg IV over 2 hours
Other thrombolytic agents:
Streptokinase (250,000 IU loading dose over 30min, followed by 100,000
IU/hr over 12-24 hrs)
Urokinase
Complication: risk of hemorrhage during thrombolytic treatment
○ In patients receiving anticoagulation - Discontinue anticoagulation prior to
thrombolysis,Check aPTT 2 hours after completion of thrombolysis.
Resume anticoagulation when aPTT is < 2 times the upper normal limit.
Catheter-directed thrombolysis
•
Indication: patients with persistent hypotension who have high bleeding risk,
obstructive shock, and/or failed systemic thrombolysis
•
Procedure: ultrasound-assisted direct infusion of thrombolytics into pulmonary artery via
pulmonary arterial catheter
Embolectomy in pulmonary embolism
•
Last resort when thrombolysis is contraindicated or unsuccessful
•
Procedure: surgical embolectomy (removal of an embolus by opening an artery with an
incision) or catheter-based thrombus removal
Treatment of nonmassive pulmonary embolism and submassive pulmonary embolism
Low to moderate bleeding risk: anticoagulation for pulmonary embolism
High bleeding risk (anticoagulation is contraindicated): Consider IVC filter
●
●
Initial parenteral anticoagulation (first 5–10 days): not required if long-term anticoagulation
is planned with rivaroxaban or apixaban.
○ Low molecular weight heparin (LMWH): Enoxaparin (1.5 mg/kg SQ daily)
○ Fondaparinux 5-10mg once daily (Preferred in patients with normal renal function)
○ Unfractionated heparin (UFH) → Heparin 80 units/kg IV bolus, then 18 units/kg/hour
infusion with aPTT or anti-Xa monitoring; follow local protocols
■ Used for patients with renal failure
Long-term anticoagulation (up to 3 months)
○
○
○
○
DOAC:
■ No initial parenteral anticoagulation required
● Direct factor Xa inhibitors: Rivaroxaban or Apixaban
● (10 mg PO twice daily for 7 days, then 5 mg PO twice daily)
■ Initial parenteral anticoagulation required:
● Direct thrombin inhibitors- Dabigatran (150 mg PO twice daily)
● or Edoxaban
Vitamin K antagonist (warfarin→ initial dose (e.g., 5 mg) based on patient
characteristics; titrate as needed to target INR; follow local protocols),
■ target INR 2–3):
If DOAC cannot be given, VKA is preferred over LMWH.
LMWH: preferred in cancer patients and pregnant women
DVT prophylaxis
VTE prophylaxis refers to the primary prevention of DVT or PE in at-risk individuals and includes
general preventive measures, mechanical VTE prophylaxis, and pharmacological VTE prophylaxis.
VTE prophylaxis should be chosen based on the presence of risk factors for VTE and estimated risk
of bleeding on anticoagulation therapy.
Prophylaxis is usually indicated in seriously ill patients who are hospitalized, patients undergoing
major surgery, patients w/ major trauma and long-distance travelers w/ additional risk factors for VTE.
● General preventive measures
○ Regular exercise
○ Early postoperative mobilization
●
○ Physiotherapy
○ Avoid certain medications (e.g., OCPs) in patients with thrombophilias
Pharmacological VTE prophylaxis (antithrombotics):
○ LMWH,
●
●
●
○ low-dose UFH, and
○ DOACs
Analgesics for pain relief: avoid NSAIDs if the patient is receiving anticoagulation or
thrombolytics
Mechanical VTE prophylaxis
○ Graduated compression stockings: preferred in long-distance travelers
○ Intermittent pneumatic compression device
■ Preferred in seriously ill medical patients and in surgical patients
■ Alternating inflation and deflation of the compression device improve venous
return by simulating the calf pump mechanism.
Duration of prophylaxis in hospitalized patients
○ Mechanical VTE prophylaxis: until the patient is mobile
○ Pharmacological VTE prophylaxis
■ Seriously ill medical patients: at least 7 days; extend to span the duration of
hospitalization
■ Surgical patients: consider extended therapy for > 3 weeks
169) Treatment of pneumonia
Criteria for hospitalisation
Every patient should be assessed individually and clinical judgement is the most important factor. The
pneumonia severity index (PSI) and the CURB-65 score are tools that can help to determine whether
to admit a patient.
CURB-65 score
•
Confusion (disorientation, impaired consciousness)
•
Serum Urea > 7 mmol/L
•
Respiratory rate ≥30/min
•
BP = systolic ≤90 mmHg or diastolic ≤60 mmHg
•
Age ≥ 65 years
•
Each finding is assigned 1 point
•
Score 0 or 1 = patient may be treated as outpatient
•
Score ≥2 = hospitalisation is indicated
•
Score ≥ 3 = consider ICU level of care
•
If serum urea level is not known or unavailable, a score of ≥1 requires hospitalisation
Supportive therapy
•
Sufficient rest (not absolute bed rest) and physical therapy
•
Hydration with PO fluids or IV fluids (see IV fluids)
•
Treat hypoxemia.
•
Supplemental oxygen as needed for hypoxia, mechanical ventilation
•
Incentive spirometer
•
Antipyretics, analgesics as needed (e.g., acetaminophen)
•
Expectorants and mucolytics (N-acetyl cysteine)
•
Antitussives (e.g., codeine)
Empiric anti-B therapy for CAP in an outpatient setting
Patient profile
Recommended empiric anti-B regimen
Previously healthy
patient w/out
comorbidities or risk
factors for resistant
pathogens
Monotherapy w/one of the following:
Patients w/comorbidities
or risk factors for
resistant pathogens
Combo therapy
•
Amoxicillin (500 mg 3X/day)
•
Doxycycline (200 mg on 1st day, then 100 mg 1X/day orally)
•
Macrolide – azithromycin or clarithromycin (500 mg 2X/day)
•
In pregnancy = erythromycin (500 mg 4X/day)
•
An anti-pneumococcal β-lactam (amoxicillin-clavulanate, cefuroxime,
cefpodoxime) PLUS azithro-/clarithromycin or doxycycline
Monotherapy w/a respiratory fluoroquinolone:
•
Gemifloxacin (320 mg 1X/day)
•
Moxifloxacin (400 mg 1X/day)
•
Levofloxacin (750 mg 1X/day)
•
5 days of therapy is usually sufficient for CAP that is treated in the outpatient setting
•
Any patient being treated in a primary care setting should be re-examined after 48-72 hours to
evaluate the efficacy of the prescribed anti-B
Empiric anti-B therapy for CAP in an inpatient setting
Patient profile
Non-severe CAP/non-ICU
treatment
Recommended empiric anti-B regimen
Combo therapy
•
An anti-pneumococcal β-lactam (amoxicillin-sulbactam,
ceftriaxone, cefotaxime) PLUS azithro-/clarithromycin or
doxycycline
Monotherapy w/a respiratory fluoroquinolone:
Severe CAP/ICU treatment
•
Gemifloxacin (320 mg IV 1X/day)
•
Moxifloxacin (400 mg IV 1X/day)
•
Levofloxacin (750 mg IV 1X/day)
Combo therapy
•
An anti-pneumococcal β-lactam (amoxicillin-sulbactam,
ceftriaxone, cefotaxime) PLUS azithro-/clarithromycin or
doxycycline or a respiratory fluoroquinolone
Alternatives for patients w/a penicillin allergy:
•
Aztreonam
•
PLUS a respiratory fluoroquinolone (moxi-/levofloxacin)
Risk factors for MRSA
Add vancomycin (15-20 mg/kg IV every 8-12 hours) or linezolid (600
mg IV/oral every 12 hours, 10-14 days)
Risk factors for pseudomonas
aureginosa
Combo therapy
One of: Piperacillin-tazobactam 4,5 g IV every 6 hours, Cefepime: 2
g IV every 8 hrs, Meropenem 1 g IV every 8 hrs
PLUS a macrolide or fluoroquinolone
•
5-7 days is usually sufficient
•
Consider longer courses in: patients not responding to treatment; suspected or concern for
MRSA or P. aeruginosa infection; concurrent meningitis; unusual pathogens
•
If aztreonam is used instead of β-lactam anti-B (e.g. for penicillin allergy), the addition of
MSSA (methicillin susceptible S. aureus) (e.g. a fluoroquinolone) is necessary
•
Anaerobic coverage is not routinely recommended for suspected aspiration pneumonia
(unless lung abscess or empyema is suspected)
•
Corticosteroids are not routinely recommended as adjunct therapy
Empiric anti-B therapy for hospital-acquired pneumonia
Patient profile
Patients not at high risk for
mortality and w/out risk
factors for MRSA infection
Patients not at high risk for
mortality but w/risk factors for
MRSA infection
Recommended empiric anti-B regimen
Monotherapy:
•
An anti-pneumococcal, anti-pseudomonal β-lactam = imipenem,
meropenem, cefepime, piperacillin-tazobactam
•
OR levofloxacin: 750 mg IV x 1/day
Combo therapy:
•
One of the following anti-B w/MRSA activity = Vancomycin or
Linezolid
PLUS one of the following:
•
Anti-pneumococcal, anti-pseudomonal β-lactam = Piperacillintazobactam: 4.5g/6hrs IV, cefepime 2g/8hrs IV, ceftazidime,
meropenem, imipenem
•
A fluoroquinolone = levo-/ciprofloxacin
•
Aztreonam
Patients at high risk for
mortality and patients
Combo therapy:
w/structural lung diseases
Linezolid
PLUS any two of the following (avoid combining 2 β-lactams):
•
One of the following anti-B w/MRSA activity = Vancomycin or
•
Anti-pneumococcal, anti-pseudomonal β-lactam = Piperacillintazobactam, cefepime, ceftazidime, meropenem, imipenem
•
A fluoroquinolone = levo-/ciprofloxacin
•
An aminoglycoside = Amikacin 15-20mg/kg IV, Gentamicin 57mg/kg IV, tobramycin
•
Aztreonam
•
Empiric anti-B therapy should be narrowed and/or de-escalated as soon as feasible
•
7 days of therapy are usually sufficient
•
Resistance patterns can vary widely; local antibiograms should be considered when starting
empiric treatment
170) Treatment of asthma.
Approach
1. Confirm diagnosis of asthma.
2. Assess severity
3. Initiate antiasthmatic medication based on severity.
4. Manage comorbidities; reduce exposure to asthma triggers
5. Monitor response to therapy.
6. Adjust treatment (step up or step down) based on response to therapy.
7. Schedule frequent follow-ups. Long-term follow-up and reassessment of asthma symptom control
are recommended every 1–6 months.
The goal of treatment is to achieve current control and reduce future risk
Class
Beta-2 agonists
Inhaled
corticosteroids
(ICS)
Leukotriene
receptor
antagonist (LRA)
Examples
●
Short-acting β-2
agonists (SABA) =
albuterol, terbutaline
●
Long-acting β-2
agonists (LABA) =
salmeterol(150mcg
inhaled every 12 h),
formoterol
●
Beclomethasone
●
Fluticasone
●
Budesonide
●
Mometasone
Montelukast
Mechanism
Primary use
Dilate bronchial smooth muscles
SABA = acute
exacerbations
LABA = long-term
maintenance treatment
Inhibit transcription factors → ↓
expression of pro-inflammatory
genes
Long-term maintenance
treatment (1st line)
Prevent leukotrienes from binding
to their receptors → ↓
bronchoconstriction
Long-term maintenance
treatment (particularly in
children).
Exercise-induced and
aspirin-induced asthma
Muscarinic
antagonists
Methylxanthines
Mast cell
stabilisers
●
Short-acting muscarinic
antagonists (SAMA) =
Ipratropium bromide
●
Long-acting muscarinic
antagonists (LAMA) =
Tiotropium bromide
Theophylline
●
Cromolyn sodium
●
Nedocromil sodium
Competitively inhibit
postganglionic muscarinic
receptors in bronchial smooth
muscles → bronchodilation
Option for long-term
maintenance treatment
Inhibits phosphodiesterase (PDE)
→ ↑ cAMP levels → antiinflammatory and mild
bronchodilatory effect
Limited used (cardiotoxic,
neurotoxic)
Prevents release of inflammatory
mediators from mast cells
Preventive treatment prior
to exercise or unavoidable
exposure to known
allergens in patients ≥55
years old
Oral
corticosteroids
●
Methylprednisolone
●
Prednisone
Biological agents
●
Omalizumab (1)
●
Mepolizumab (2)
Similar to ICS
●
Anti-IgE AB that binds to
serum IgE = ↓ serum IgE
prevents binding of IgE to
high affinity IgE receptor
on mast cells and
basophils → the
inflammatory cascade
triggering asthma is
inhibited. Long-term
reduction in serum IgE will
↓ surface expression of
IgE receptor on mast cells
and basophils. (1)
●
Monoclonal AB against IL5 = potent
chemoattractant for
eosinophils (2)
Used in severe and
refractory cases
Additional medication for
severe eosinophilic
asthma that is not
sufficiently controlled
w/other measures
Follow-up
•
Assess response to therapy in 2–6 weeks
•
Good response for ≥ 3 consecutive months: Consider a gradual decrease in pharmacotherapy
(step down).
•
Inadequate response
o Assess treatment adherence, inhaler technique.
o Manage comorbidities and environmental factors
o Consider advancing treatment to the next step (step up).
Adjunctive therapyThese measures should be optimized in all patients to reduce antiasthmatic medication requirements
and decrease the frequency of acute asthma exacerbations.
•
Reducing exposure to triggers or allergens
o Indoor/outdoor allergens (e.g., dust, pollen, dust mites)
o Occupational exposure
o
o
Medications
Consider allergen immunotherapy in allergic asthma.
•
Managing comorbidities
o Obesity
o Rhinosinusitis and nasal polyps
o Anxiety and depression
o PPI if GERD is suspected
•
Reducing the risk of infection-induced exacerbations
o
o
Early treatment of infections in infection-triggered asthma
Immunizations (influenza, pneumococcal vaccines)
•
Lifestyle recommendations
o Provide information and tools for self-monitoring and self-management (e.g., written
action plan, peak flow meter).
o Encourage physical activity, especially in younger patients.
o Smoking cessation
•
Social interventions
•
Encourage normal vaginal birth, breastfeeding and avoidance of paracetamol and antibiotics
use in the first year of life.
Acute asthma exacerbation:
Approach
•
Use appropriate PPE as viral infections are a common trigger for asthma exacerbations.
•
ABCDE approach
•
Signs of life-threatening asthma exacerbation
o Consider early intubation.
o Administer SABA + SAMA + IV corticosteroids; consider IV magnesium
•
No signs of life-threatening asthma at presentation
o Rapidly obtain a focused history, examination, PEFR, and pulse oximetry reading to
assess severity.
o Stratify the severity of asthma exacerbation.
•
Administer initial medical therapy according to severity
o
o
o
Severe asthma exacerbation: Supplemental O2 + SABA + SAMA + oral/IV
corticosteroids; consider IV magnesium
Moderate asthma exacerbation: Supplemental O2 + SABA; consider oral
corticosteroids
Mild asthma exacerbation: SABA; consider oral corticosteroids
•
Monitor closely and escalate treatment accordingly.
•
Consider fluid repletion (preferably oral) in infants and young children
•
Order diagnostic tests as needed once stabilized.