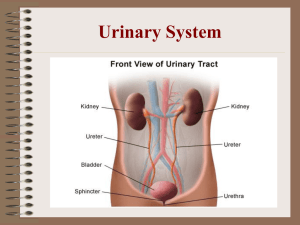
EXCRETION Ms Henning Life Sciences Grade 11 Abbotts College 2023 The average person urinates about 2500 times per year The average person produces about 140 kg of faeces per year Most people, on average, would breathe about 6286920 times in their lifetime. The average adult bladder can hold 500-700 ml of urine DON’T GET CONFUSED Excretion: getting rid of metabolic wastes Egestion: undigested remains (defaecation) Secretion: release of useful substances Excretory Waste products Organ Origin of waste Lungs Cellular respiration Kidneys and bladder Liver and intestines Skin CO2, water vapour, heat Water, mineral salts, nitrogenous waste: urea, uric acid, creatinine Urea Bile pigments Water Salts urea Cellular respiration, drinking Food Degradation of excess amino acids Degradation of nucleic acids (DNA, RNA) Degradation of creatine phosphate (energy carrier in muscles) Excess amino acids degraded Haemoglobin breakdown Cellular respiration, drinking Food Excess amino acids THE URINARY SYSTEM A Nitrogenous waste removed: Urea Uric acid Creatinine Regulates: B C D E F Water (Osmoregulation) Salt content pH G H THE URINARY SYSTEM A. Renal artery B. Renal vein C. Kidney D. Vena cava E. Aorta F. Ureter A B C D E F G. Bladder H. urethra G H STRUCTURE OF THE URINARY SYSTEM Two kidneys located near the middle of the back just below the diaphragm, on either side of the spine. Renal artery – carried blood to each kidney to be filtered. Renal vein – remove the filtered blood. Two ureters – tubes which carry urine from the kidneys to the bladder. Bladder – stores urine temporarily. Urethra – tube through which urine passes from the bladder to the outside. THE KIDNEY (EXTERNAL STRUCTURE) • External structure: – Renal capsule – Renal pelvis – ureter – (Adrenal Gland) A B C D MACRO-STRUCTURE OF THE KIDNEYS Kidneys are about the size of an adult fist and are surrounded by a thick layer of adipose tissue (fat) which acts as a shock absorber. Each kidney is enclosed in a renal capsule made of fibrous connective tissue. Renal cortex – outer region, beneath the capsule; grainy appearance. Renal medulla – made up of about seven cone-shaped renal pyramids; striped appearance. Pelvis – hollow inner chamber in which urine collects before it is carried via the ureter to the bladder. Hilum – where the renal artery enters the kidneys, and the renal vein and the ureter leave the kidney. INTERNAL STRUCTURE (MACROSCOPIC – P 2.43) A Draw a labelled biological drawing of the internal structure of the kidney. B C D E F G Internal structure (macroscopic – p 2.43) CORTEX A (red in colour – lots of blood capillaries. Region of filtration) B RENAL PELVIS (collects urine from the calyces) CALYX C (collects urine from the pyramids) D RENAL PYRAMID (made of hundreds of tubes, draining waste from capillaries to pelvis) E RENAL CAPSULE F MEDULLA (region that is whitish in colour – contains kidney tubes) G URETER (INTERESTING ASIDE) The bladder holds the distinction of being the first complex human organ to be rebuilt in a laboratory and placed in human patients. The patients' own cells were used to build the bladders. These cells were harvested during an operation to remove bladder damage and then placed on scaffolding that shaped the growing cells. The new bladders were ready in seven weeks, and in 1999, doctors performed the first operation to sew the new bladder to the existing one. The researchers performed seven such surgeries and followed the patients for a minimum of two years before announcing their success. This advancement holds tremendous promise for replacement organs. So many people die each year waiting for a transplant, but now it may be possible to harvest organs for those people before time runs out. http://health.howstuffworks.com/human-body/parts/10-body-parts-that-can-be-rebuilt10.htm calyces WHAT DOES A FILTER DO? WHAT IS IN BLOOD? • Things to remove: • Excess water • Nitrogenous wastes • Excess salt • Toxins • Things to leave in: • Plasma proteins, water, salts, blood cells, antibodies, etc OVERVIEW OF WHAT KIDNEYS DO STEP1: size filter (ultrafiltration) Plasma without blood cells and big proteins blood cells, big proteins and some plasma stay behind Waste to bladder as urine STEP2: reabsorption Useful substances reabsorbed FUNCTIONAL UNIT OF THE KIDNEY: THE NEPHRON • Each kidney has about 1 million nephrons • Each one is a microscopic filter and absorber STRUCTURE OF THE NEPHRON Each nephron is composed of 4 parts: 1. Bowman's capsule Bowman was an English surgeon who identified “Bowman’s capsule” in the nephron in 1841, at the age of 25. 2. The proximal convoluted tubule 3. The loop of Henle 4. The distal convoluted tubule Each nephron has its own blood supply Henle was a German physician of the late nineteenth century who discovered many structures in the human body, including the loop of Henle. MICROSCOPIC STRUCTURE OF A NEPHRON Malpighian Body: Ultrafiltration Renal Tubule: Reabsorption Collecting duct: transport of waste Efferent arteriole Nephrons isolated from kidney material FUNCTIONING OF THE NEPHRONS Nephrons, the functional units of the kidneys, are responsible for filtering the blood and producing urine. Water and solutes pass from the blood into the nephrons, forming a filtrate. Useful substances are reabsorbed back into the blood from the filtrate. When the filtrate leaves the nephrons via the collecting ducts it is known as urine. Urine production in the nephrons consists of three processes: ultrafiltration, reabsorption, and tubular excretion. GLOMERULAR FILTRATION • Blood in afferent arteriole enters glomerulus under pressure as efferent arteriole narrower • Small substances including water filtered through capillary walls with pores and tiny slits through podocytes into Bowman’s capsule as glomerular filtrate • Large substances e.g. blood cells and proteins remain in glomerulus • Formation of this filtrate is not selective and many useful substances (e.g. glucose) are found in the filtrate together with waste MALPIGHIAN BODY IN DETAIL Glomerular filtration: • Pressure from difference in diameter between afferent and efferent arterioles • Filtrate passes through pores in capillary endothelium and slits between podocytes into Bowan’s capsule cavity • Blood cells and large proteins stay in glomerulus – leave via efferent arteriole podocyte MALPIGHIAN BODY SUITED FOR ITS FUNCTION wider afferent arterioles for high pressure in glomerulus large surface area of capillary network endothelium and podocytes form a fine filter 1. endothelium has pores 2. podocytes have filtration slits 26 TUBULAR REABSORPTION • As glomerular filtrate passes proximal convoluted tubule, all useful substances (e.g. glucose, amino acids, glycerol and salts) are actively reabsorbed into peritubular capillaries • Water (65%) follows these substances by osmosis 27 REABSORPTION OF WATER AND THE LOOP OF HENLE • Filtrate entering the loop of Henle is still considered dilute with too much water. • The loop of Henle ensures medulla tissue has a high sodium ion concentration and therefore hypertonic (low water potential) • The descending limb of the loop is permeable to water and water moves out by osmosis into the blood • Sodium ions are actively pumped out of the ascending limb into the tissue fluid of the medulla • This process needs energy and is called the sodium pump. Chloride ions follow passively. 28 • Water does not follow the sodium ions at this stage as the ascending limb is impermeable to water. • Sodium ions slowly get transported in the medulla back to the peritubular network to prevent the concentration becoming too high. • further reabsorption of useful substances occurs in the distal convoluted tubule. 29 TUBULAR EXCRETION • Cells in the tubules don’t only reabsorb, they also excrete wastes (e.g. creatinine, drugs, hydrogen and potassium ions, colourants, preservatives and other foreign substances) • From the peritubular capillaries into the proximal and distal convoluted tubules FORMATION OF URINE The filtrate which enters the collecting duct is known as urine. Urine consists of urea and excess water and salts. All useful substances such as glucose, amino acids and some salts have been reabsorbed back into the blood. The collecting ducts carry urine through the renal medulla and into the renal pelvis, from where it passes into the ureter. Urine travels down the ureter into the bladder, where it is stored until it can be released through the urethra during urination. About 1 to 2 litres of urine is produced each day. URINE Contains: Water Inorganic salts (calcium, chloride, sulphate, sodium & magnesium ions) Metabolic wastes (urea, uric acid, creatinine) Foreign substances (flavourants, colourants, drugs, preservatives) OSMOREGULATION Osmoregulation is the name for the active maintenance of the correct balance of water and solutes in the body fluids (i.e. blood and tissue fluid). For the body to function properly, the concentration of solutes in the blood and tissue fluid must remain more or less the same. The kidneys, under control of the hormones ADH and aldosterone, help to maintain the correct balance of water and solutes in the body fluids. ROLE OF ADH (ANTIDIURETIC HORMONE) The hormone ADH helps to limit the amount of water lost from the body in the urine, by making the walls of the collecting ducts more permeable to water. ADH is produced by the pituitary gland, under the influence of the hypothalamus, which detects changes in the solute concentration in the blood. If the blood becomes too concentrated, the hypothalamus causes a sensation of thirst so that the person drinks more liquid. At the same time, it stimulates the pituitary gland to secrete ADH, which travels through the blood to the collecting ducts and makes them more permeable to water. Water then moves by osmosis from the urine in the collecting ducts to the tissue fluid in the renal medulla. From here it is reabsorbed into the blood, causing the solute concentration of the blood to return to normal. If the blood becomes too dilute, the hypothalamus stops stimulating the pituitary gland to secrete ADH. Without ADH, the walls of the collecting duct become impermeable to water which passes out in the urine, causing the solute concentration of the blood to return to normal. This is an example of negative feedback, because a change in solute concertation in the blood causes a response (the release of ADH) to counteract change. When the solute concentration of the blood returns to normal, less ADH is released. ROLE OF ALDOSTERONE Aldosterone is a hormone that helps to maintain the balance of salts, especially sodium, in the body fluids. It does this by causing sodium to be actively reabsorbed from the distal convoluted tubules and collecting ducts. Aldosterone is produced by the adrenal glands, under the influence of the kidneys. The body obtains sodium through food and drink, and loses it mainly in sweat and urine. If the levels of sodium ions in the blood and tissue fluid are too low, less water will pass out of the filtrate into the blood by osmosis (that is, to be reabsorbed), causing the volume of the blood and the blood pressure to decrease. If the blood pressure becomes too low to promote ultrafiltration at the glomerulus, the kidneys secrete substances which stimulate the adrenal glands to secrete aldosterone. Aldosterone travels through the blood to the distal convoluted tubules and the collecting ducts. It causes sodium to be actively reabsorbed from the filtrate into the blood and the blood becomes more concentrated. Now more water will pass out of the filtrate into the blood by osmosis, causing a rise in blood volume, and the blood pressure returns to normal. If the level of sodium ions in the blood and tissue fluid are too high, more water will pass out of the filtrate into the blood by osmosis. This means that the volume of the blood, and hence blood pressure, will increase. If the blood pressure increases, aldosterone will not be secreted by the adrenal glands. Without aldosterone, water is not reabsorbed from the distal convoluted tubules and collecting ducts into the blood, so that blood pressure will return to normal. VIDEO TIME Excretion - ADH and Homeostasis - GCSE Biology (9-1) by Mr Exham Biology (02:58) https://www.youtube.com/watch?v=yXWlSve_7Uw&ab_channel=MrExhamBiology The Nephron - Ultrafiltration and Selective Reabsorption - GCSE Biology (9-1) by Mr Exham Biology (05:20) https://www.youtube.com/watch?v=tx9hYFeEd1E&ab_channel=MrExhamBiology KIDNEY STONES • • • • • • when wastes in urine do not dissolve solid crystals can form <4,5mm leave the body with urine >4,5mm can cause blockages of the ureter causing serious pain (renal colic) Blood in urine also can occur due to damage to the epithelium of urinary tubes Risk increased if dehydrated and diet (e.g. lots of animal protein and coke) Removal by surgery or ultrasound to shatter smaller stones EXTRA INFORMATION • Calcium stones. Most kidney stones are calcium stones, usually in the form of calcium oxalate. Oxalate is a naturally occurring substance found in food. Some fruits and vegetables, as well as nuts and chocolate, have high oxalate levels. • Struvite stones. Struvite stones form in response to an infection, such as a urinary tract infection. These stones can grow quickly and become quite large, sometimes with few symptoms or little warning. • Uric acid stones. Uric acid stones can form in people who don't drink enough fluids or who lose too much fluid, those who eat a high-protein diet, and those who have gout. Certain genetic factors also may increase your risk of uric acid stones. • Cystine stones. These stones form in people with a hereditary disorder that causes the kidneys to excrete too much of certain amino acids (cystinuria). • Other stones. Other, rarer types of kidney stones also can occur. 44 BILHARZIA • caused by the Schistosoma parasite (a parasitic flatworm) – – – – – – Flatworms burrow into human skin in contaminated water They grow, mate and lay eggs in blood vessels lining bladder and intestines Eggs rupture the vessels and enter the bladder and intestines A symptom can be painful urination with blood in it Eggs discharged into environment and infect a type of water snail (the secondary host) and the cycle continues Urinary system can be blocked in different parts and eventually result in chronic kidney failure, liver failure and cancer of the bladder. RENAL FAILURE • Kidney is damaged and not functioning • Acute: sudden loss by injury, surgery complications and drug use • Chronic: develops slowly e.g. from diabetes or untreated high blood pressure. • Waste products and excess water accumulate • Toxic to the body and may cause death • Treatments include dialysis or kidney transplant 48 OVERUSE OF PAINKILLERS Some over-the-counter painkillers such as aspirin and ibuprofen can make kidney disease worse in people who already have kidney damage. They can also cause kidney damage in healthy people who use them regularly over a long period of time. Certain other medications, toxins, pesticides and illegal drugs (for example, heroin, and crack cocaine) can also cause kidney failure. Example: drug cause of renal failure • Kidney failure due to overdose – Taking painkillers everyday can cause analgesic nephropathy – Damage builds up over time leading to irreversible kidney failure – E.g. paracetamol and ibuprofen – Important to remain well hydrated when taking any medication and follow dosage instructions Dialysis • removing the blood from a patient • Purification of the blood by a machine • putting the blood back into the patient • Treatment lasts about six hours • regular treatment necessary • serious impact on lifestyle and is not a long term solution 52 Dialysis In order to remove toxic urea, and to maintain the correct balance of salts and water in the body, a patient whose kidneys are not working properly needs to spend many hours a week attached to a dialysis machine. Advantages It can keep a patient alive whilst they are waiting for a suitable donor to be found. It does not involve major surgery. Disadvantages Patients need to follow a carefully controlled diet. Patients need to spend many hours every week attached to a dialysis machine. Dialysis machines are very expensive. Dialysis will only be successful for a certain amount of time. Blood is removed from the patient and flows into the dialyzer where it is kept separated from dialysis fluid by a partially permeable membrane. The dialysis fluid contains the same concentration of glucose and salts as normal blood plasma so there is no net movement of glucose out of the blood by diffusion. Excess salts diffuse into the dialysis fluid. The dialysis fluid contains no urea, so all of the urea diffuses from the blood in to the dialysis fluid from the high concentration in the blood to the lower concentration in the dialysis fluid. The blood and dialysis fluid move in opposite directions across the membrane (a counter current system) in order to maintain concentration gradients all the way along. The clean blood is returned to the patient and the waste dialysis fluid is disposed of. KIDNEY TRANSPLANT Advantages Once the transplant has occurred the patient no longer has diet restrictions. Long periods of time on dialysis are no longer necessary. Although not a life-long cure, a kidney transplant will generally allow the patient to live a fuller life for longer than a patient on dialysis. Disadvantages It is difficult to find a donor organ with a matching tissue type. The risk of organ rejection. Having to take drugs which suppress the immune system, leaving the patient susceptible to contracting other diseases. Regular doctors' appointments to detect signs of organ rejection. Major surgery is required. CONSOLIDATION ACTIVITY