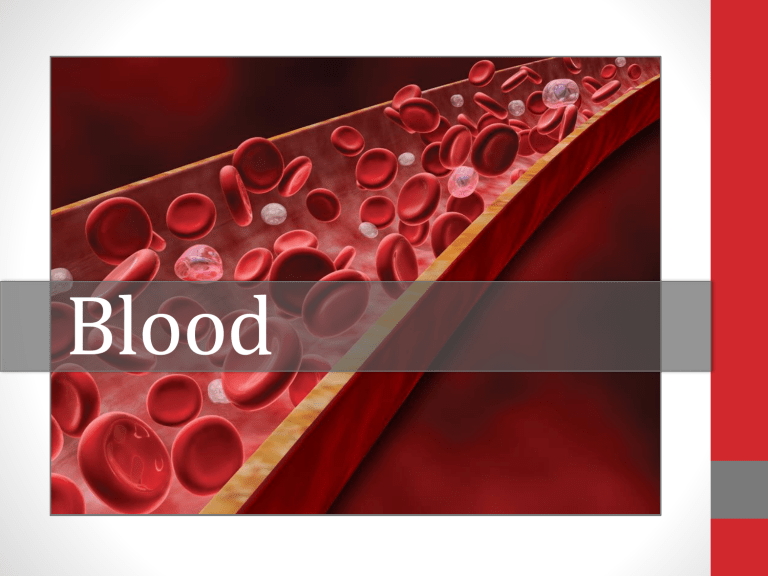
Blood STRUCTURE AND FUNCTION 2 Facts about Blood • The only fluid tissue in the body • Sticky, opaque fluid • Metallic, salty taste • Alkaline pH between 7.35-7.45 • Temperature is 38° C (100.4° F) • Volume in healthy adult male is 5-6 liters; about 8% of body weight 1 2 3 4 5 Venous blood, 1 & 2, is slightly darker due to low oxygen content. Oxygen gives arterial blood, 3, 4 & 5, a much brighter color. 3 Functions of Blood • Blood transports substances throughout the body through blood vessels • Carries nutrients, respiratory gases, and other substances throughout the body • Distributes body heat 4 Components of Blood 1. Solid Component or Formed Elements (living): • red blood cells • white blood cells • platelets 2. Liquid Component (non-living): plasma 5 Erythrocytes Thrombocytes 6 Leukocytes Hematocrit • Blood samples are spun in a centrifuge • Formed elements settle at the bottom & plasma rises to the top The ratio of red blood cells to total blood volume is the hematocrit. 7 Plasma • Liquid portion of blood, 90% water • Makes up 55% of blood volume • Contains over 100 dissolved substances including nutrients, salts (electrolytes), respiratory gases, hormones, plasma proteins, and various wastes Albumin is the most abundant plasma protein found in blood. It helps maintain osmotic pressure of blood by keeping water in the bloodstream. 8 Formed Elements Red blood cells are the most numerous blood cells; white blood cells are the largest • Together, make up about 45% of blood • Red blood cells carry oxygen & CO2 • White blood cells play a role in immunity • Platelets are responsible for blood clotting 9 Red Blood Cells: Erythrocytes • 44% of blood volume • Function to carry oxygen • Shaped like a biconcave disk, increases surface area • No nucleus • Live 100-120 days; old cells are destroyed in liver or spleen • Low number or reduced function is anemia 10 Hemoglobin • An iron-bearing protein that carries oxygen and gives blood its red color • A single RBC contains about 250 million hemoglobin molecules • Each hemoglobin molecule can carry 4 molecules of oxygen 11 White Blood Cells: Leukocytes • Defend the body against • • • • Bacteria Viruses Parasites Tumor cells • Less than 1% of total blood volume • Leukocytosis is the increase in wbc production to fight infection 12 Types of Leukocytes 13 Phagocytosis • The process of engulfing and destroying microorganisms, cellular debris, and other foreign or toxic substances • Leukocytes can leave the circulatory system and move around inside body tissues to fight invaders such as bacteria • They respond to certain chemicals released by damaged cells Most phagocytosis is performed by neutrophils 14 Macrophage • Monocytes change into macrophages when they enter infected tissues • They recognize, engulf and destroy target cells • Image shows macrophages in infected lung tissue 15 Pus A collection of dead leukocytes at the site of an infection. 16 Platelets: Thrombocytes • Cell fragments • Necessary for blood clotting process • A blood clot on the surface of skin forms a scab • Bruises are caused by bleeding under the skin 17 HEMATOPOIESIS 18 All Blood Cells Differentiate from Stem Cells in Bone Marrow 19 Hematopoiesis • Blood cell formation • Occurs in red bone marrow • All formed elements come from a type of stem cell called a hemocytoblast • Most blood cells are formed in the red marrow of the vertebrae and pelvis 20 Hemocytoblasts are Stem Cells that develop into Blood Cells 21 HEMOSTASIS 22 Hemostasis • Hemostasis is the process of stopping blood flow • A series of reactions triggered by a break in a blood vessel wall • Response is fast and localized 23 3 Stages of Hemostasis 1. Vascular Spasms 2. Platelet Plug Formation 3. Coagulation Events 24 Vascular Spasms • Damaged blood vessels constrict to reduce blood loss • Most effective in smaller vessels 25 Platelet Plug Formation • Platelets detect damage, become sticky and cling to the damaged area • Anchored platelets release chemicals that attract more platelets • A small mass is formed called a platelet plug platelet plug 26 Coagulation • A complex series of reactions that eventually convert a soluble protein called fibrinogen into an insoluble fiber called fibrin • A fibrin mesh forms to strengthen the platelet plug and trap red blood cells blood clot 27 Fibrin Mesh 28 Scab Scabs fall off when the underlying skin is fully healed. • Protective crust that forms over an injury • Once a platelet plug is no longer needed, it begins to dry out and form a scab • The scab protects underlying tissues as they are regenerated 29 BLOOD GROUPS & TRANSFUSIONS 30 Blood Types • 4 inherited blood types exist in the human population • Type O is most common • Type AB is least common 31 ABO Blood Groups • Differences in blood type are due to the presence or absence of proteins (antigens) on the surface of red blood cells • Antigens will determine the type of antibodies produced in the plasma Red blood cells have either: • A antigens • B antigens • Both A & B • Neither A nor B 32 Antigens & Antibodies 33 Determining Blood Type • A blood sample is mixed with • Anti-A • Anti-B • Anti-Rh • Clumping or agglutination indicates the presence of the antigen Anti-A - Anti-B Anti-Rh + + Results: • A antigen NOT present • B antigen present • Rh antigen present Conclusion: Type is B+ 34 Blood Transfusions If blood of an incompatible type is introduced, the patient’s plasma (serum) antibodies will react with red blood cell antigens, and aggregation or clumping will occur. 35 Complications of Transfusing Incompatible Blood • Aggregation or agglutination of blood in the body leads to: • Clogging of small blood vessels • Destruction of erythrocytes • Free hemoglobin molecules can cause fatal kidney damage 36 Rh Factor The Rh factor was first discovered in the blood of Rhesus monkeys. • Another type of protein sometimes found on the rbc • Rh- people do not automatically have antibodies against Rh • First exposure of Rhperson to Rh+ antigens will cause the production of antibodies • Second exposure will result in recipient’s antibodies attacking and rupturing donor’s Rh+ red blood cells 37 Rh Factor Complications during Pregnancy • When Rh- mother carries her first Rh+ baby, her body will produce antibodies, but baby is not affected • The second pregnancy will result in her antibodies crossing the placenta and attacking the baby’s red blood cells 38 Universal Donor & Recipient • The absence of rbc antigens makes those with type O- blood able to donate to any other type: universal donor • The absence of plasma antibodies makes those with type AB+ blood able to receive transfusions from any other type: universal recipient Type O-: no antigens Type AB+: no antibodies 39 DISEASES & CONDITIONS 40 Anemia • Reduced ability of the blood to carry oxygen • Several different types of anemia exist Common symptoms of anemia: • May result from: • Pale or sallow skin • Low number of rbc • Abnormal or deficient hemoglobin content • General fatigue • Weakness • Shortness of breath 41 Sickle Cell Anemia • Inherited form of anemia • Hemoglobin does not form properly giving red blood cells a sickle shape • Abnormal red blood cells rupture easily and get clogged in small vessels 42 Hemophilia • A sex-linked genetic blood disorder in which blood does not clot properly • May lead to excessive internal or external bleeding • Can be treated with IV clotting factors 43 Leukemia Red bone marrow becomes cancerous and produces large numbers of abnormal white blood cells that do not function properly. 44 Undesirable Clots • A blood clot that forms in a blood vessel and does not move to another area of the body is called a thrombus. • If the clot moves to another part of the body, it is called an embolus. 45 The End 46