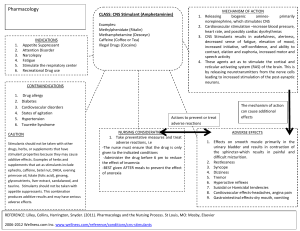
Sunga, Saara Paula Bianca B. BSN 2-Y1-6 Drug Study – NCMA 216 Using the Drug Handbook: Search for the Assigned drug classification showing its drug action/s and indication/s. I. CNS Stimulants 1. Amphetamines (Drug Classification: ADHD Agents, Stimulants) THERAPEUTIC SIDE EFFECTS ACTION Amphetamine is a CNS: Overstimulation, central nervous (CNS) restlessness, dizziness, system stimulant that insomnia, dyskinesia, functions by increasing euphoria, tremor, changes in the amounts of dopamine, norepinephrine, libido. In children, manifestation of vocal and and serotonin (to a lesser motor tics and Tourette’s extent) in the synaptic cleft through a variety of syndrome. GI: N&V, cramps, dry mouth, mechanisms. Amphetamine enters the diarrhea, anorexia. CV: palpitations, dyspnea, presynaptic axon increased BP, reflex terminal through decrease in HR, pulmonary diffusion or uptake by hypertension, precordial the monoamine transporters DAT, NET, and pain. DERMATOLOGIC: SERT. Once inside the symptoms of allergy ADVERSE EFFECTS The association between amphetamine and severe cardiovascular events is controversial. There have been reports of severe cardiovascular events such as myocardial infarction and sudden cardiac death in patients (including children) treated with stimulants. The use of amphetamine with other serotonergic agents and/or CYP2D6 inhibitors (including fluoxetin e, paroxetine, and bupropion) can increase the NURSING CONSIDERATION 1. If prescribed to suppress appetite administer 30 min before anticipated meal time. 2. Use a small initial dose; then increase gradually as necessary. Use lowest effective dose. 3. Unless otherwise ordered, give last dose of day at least 6 hr. before bedtime. 4. When used for attention deficit disorder in children, interrupt therapy on occasion presynaptic terminal, amphetamine increases the amounts of monoamine neurotransmitters in the cytosol through the inhibition of vesicular monoamine transporter 2 (VMAT2) as well as through disruption of the electrochemical gradients necessary for vesicular transporter function. including rash, burning, pallor. GU: urinary frequency, dysuria. ENDROCRINE: changes in libido, menstrual irregularities, gynecomastia. OPHTHALMOLOGIC: blurred vision, mydriasis. HEMATOLOGIC: leukopenia. risk of serotonin syndrom e. Amphetamine should be started cautiously in patients taking these medications, with close monitoring for signs and symptoms of serotonin syndrome. to determine necessity for continued therapy. 5. If tolerance develops, do not exceed the recommend dose in an attempt to increase the effect; rather, discontinue the drug. 2. Anorexiants (Drug Classification: CNS Stimulants THERAPEUTIC SIDE EFFECTS ACTION Anorectic drugs act CNS: Bad/metallic taste mainly on the satiety in the mouth, diarrhea, center in the headache, nausea, hypothalamus to produce vomiting, dry mouth, anorexia. They also have drowsiness, tiredness. GI: various metabolic effects Constipation, abdominal involving fat and or stomach pain, inability carbohydrate metabolism, to hold bowel movement, but many of these may be increases in bowel ADVERSE EFFECTS Many of the weight loss drugs known as sympathomimetic amines can stimulate the heart and lead to high blood pressure and a fast heart rate (tachycardia). Amphetamine-derivative, stimulant type weight loss drugs may be associated NURSING CONSIDERATION 1. Weigh the patient and take the blood pressure, pulse, and respiratory rate before starting drug therapy 2. Carefully monitor the patient's respiratory rate and the pattern until the respirations return to normal secondary to loss of weight. movements, loss of bowel control, oily bowel movements. OPHTHALMOLOGIC: blurred vision DERMAT OLOGIC: Sensitivity of the skin to sunlight. with constipation, dry mouth, restlessness, withdrawal effects, or insomnia (difficulty falling asleep), drug abuse and addiction. 3. Analeptics (Drug Classification: General CNS Stimulants THERAPEUTIC ACTION Analeptics can also be used as convulsant, with low doses causing patients to experience heightened awareness, restlessness, and rapid breathing. The primary medical use of these drugs is as an anesthetic recovery tool or to treat emergency respiratory depression. II. SIDE EFFECTS CNS: Depersonalization (a feeling that you are an observer of yourself), dizziness, facial tics, headaches, inability to sleep, increased blood pressure, increased rate of breathing, irritability. GI: Gastrointestinal irritation ADVERSE EFFECTS Abnormalities of cerebellar structure and function in alcoholism, fragile X syndrome, cancer, neurologic disease NURSING CONSIDERATION 1. Monitor vital irregularities signs 2. Record height, weight, and growth. 3. Instruct to eat nutritious foods because drug may cause anorexiants effect. CNS Depressants: 1. Sedative-Hypnotics (Anxiolytics) (Drug Classification: CNS Depressants) THERAPEUTIC ACTION SIDE EFFECTS Used to prevent anxiety and treat anxiety related Headache ADVERSE EFFECTS Frequently forgetting losing your memory NURSING CONSIDERATION or report 1. Assess for the mentioned cautions and to several anxiety disorders. These drugs tend to work rather quickly and can be habitforming. Because of this, they're usually only prescribed for short-term use. Hypnotic and sedative medications (henceforth referred to as hypnotics) work, in general, by increasing the activity of gamma- aminobutyric acid (GABA), a neurotransmitter in the brain. Rebound Insomnia Dizziness Drowsiness Nausea Dry Mouth Symptoms of depression, such as fatigue, feeling of hopelessness, or suicidal thought Mental health such as anxiety conditions, Developing a dependency on sedatives that can lead to irreversible effects or withdrawal Liver dysfunction or failure from tissue damage or overdose contraindications to prevent any untoward complication. 2. Perform a thorough physical assessment to establish baseline data before drug therapy begins, to determine effectiveness of therapy, and to evaluate for occurrence of any adverse effects associated with drug therapy. 2. Analgesics (Drug Classification: CNS Depressants) THERAPEUTIC ACTION SIDE EFFECTS Relives pain selectively Constipation without blocking the conduction of nerve Dry Mouth impulse, markedly Dizziness altering sensory perception, or affecting Skin itching consciousness Rash ADVERSE EFFECTS Easy bruising/bleeding Difficulty hearing Signs of kidney problems (such as change in the amount of NURSING CONSIDERATION 1. Determining the nature of the pain and its impact on the resident 2. Identifying factors that affect the resident’s perception and expression of pain Drowsiness Upset Stomach urine) Persistent or severe nausea/ vomiting Unexplained tiredness Dark urine Yellowing eye and skin (Jaundice) 3. Determining when administer analgesics to 4. Using nursing intervention to promote comfort and relive pain 5. Evaluating the effectiveness of the analgesics 3. Anticonvulsants (Drug Classification: CNS Depressants) THERAPEUTIC ACTION The effects of clinically used anticonvulsant drugs on high-frequency sustained repetitive firing (SRF) of action potentials and on postsynaptic responses to iontophoretically applied gammaaminobutyric acid (GABA) have been compared to establish a classification of anticonvulsant SIDE EFFECTS CNS: Psychosis, fatigue, psychological and behavioral disorders. GI: Nausea, metabolic acidosis, weight gain, hepatotoxicity, nephrolithiasis, colitis. DERMATOLOGICAL: Skin rash OPHTHALMOLOGI C: angle closure glaucoma HEMATOLOGIC: ADVERSE EFFECTS Dissociation and hallucination, asthenia, tiredness, and general weakness. Hostility, nervousness, agitation, irritability, and insomnia. Amnesia, aph asia, concentration impairment, confusion, me NURSING CONSIDERATION 1. Shake oral suspensions thoroughly before pouring to ensure uniform mixing. 2. Drug therapy must be individualized according to client needs. 3. Do not discontinue abruptly unless provider approved. To avoid severe, prolonged convulsions, withdraw over a period of days or weeks. drugs based on cellular Anemia, mory impairment, mechanisms of action. thrombocytopenia, purpura, psychomotor slowing, By using concentrations increased white blood cells speech disorder, and in the range of (WBC) count, lymphocytosis. abnormal thinking therapeutic cerebrospinal ENDOCRINE: Menstrual Morbilliform rash Urticaria fluid values in humans, disturbances, sexual Erythema drugs have been problems, fertility difficulties. multif separated into three orme Photosensitivity Acne categories: Phenytoin, form (acne-like) rash carbamazepine, and Purpura valproic acid limited SRF, Morbilliform rash (in 10%) but did not alter GABA Angioedema Pruritus responses (itching) Stevens-Johnson / TEN Anticonvulsant hypersensitivity syndrome 4. If there is a reason to substitute on e anticonvulsant drug for another, withdraw the first drug at the same time the dosage of the second drug is being increased. 5. Be prepared, in case of acute oral toxicity to assist with inducing emesis and with gastric lavage along with other supportive measures such as administration of fluids and oxygen