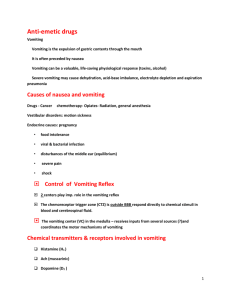
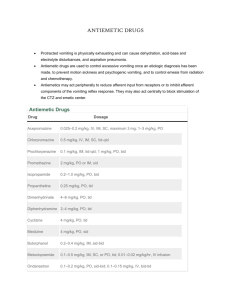
Antiemetic Drugs Dr. Ibrahim El-Shenbaby MD, PhD Clinical pharmacology Mansoura University Horus University Sultan Qaboos University Whats:+2 01007418721 Tel: 93873136 Room: 0007 COMHS, SQU Ext.: 1185 i.elshenbaby@squ.om Objectives 1. Explain the neural pathways and pharmacologic receptors involved in nausea and vomiting in order to understand the mechanisms by which antiemetic drugs act. 2. List 3-4 classes of drugs used to control emesis. 3. Describe the mechanisms of action, clinical applications and main adverse effects of some of the classes of antiemetic agents. Pain,smell, sight Fear &memory Physiology of Emesis Receptors involved in vomiting reflex Muscarinic M1 Histaminergic H1 Dopaminergic D2 Serotoninergic 5HT3 NK1 receptor for substance P Cannabinoids CB1 (agonists) Several classes of antiemetic drugs are available that antagonize these receptors. The antiemetic drugs are classified according to their primary action; some agents affect multiple receptors Receptors involved Antiemetic classes Muscarinic M1 1) Muscarinic blockers Histaminergic H1 2) H1-blockers Dopaminergic D2 3) Dopamine blockers Serotoninergic 5HT3 4) 5-HT3 blockers NK1 receptor for substance P 5) NK1 blockers Cannabinoids CB1 6) CBI partial agonists 7) Others (B6, BDZ, steroids) 1. Muscarinic blockers: Atropine Hyoscine Antiemetic mechanism They block M1 receptors in the vestibulocerebellar pathway, vomiting center, and chemoreceptor trigger zone (CTZ). Uses as antiemetic Prevention and treatment of vomiting due to motion sickness. Adverse effects Blurred vision Glaucoma Dry mouth Urine retention Tachycardia 2. H1-blockers: Diphenhydramine Cyproheptadine Cyclizine Meclizine Antiemetic mechanism They block H1 (also M1) receptors in the vestibulocerebellar pathway, vomiting center, and CTZ. They have sedative action. Uses as antiemetic Vomiting due to motion sickness (diphenhydramine) Vomiting of pregnancy (cyclizine and meclizine) True vertigo: combined with VDs to improve labyrinthine blood flow. Adverse effects Sedation (excitation may occur in children). Atropine-like actions (dry mouth, blurred vision, urine retention). Hypotension 3. 5-HT3 blockers: Ondansetron Granisetron Tropisetron Antiemetic mechanism They block 5HT3 receptors in the GIT, vomiting center, and CTZ. Uses as antiemetic Vomiting due to cancer chemotherapy or radiotherapy. Postoperative nausea and vomiting. Adverse effects Headache, dizziness, and constipation. 4. Dopamine blockers Metoclopramide Domperidone Phenothiazines e.g. Chlorpromazine Haloperidol Antiemetic mechanism They block D2 receptors in the CTZ Uses as antiemetic Vomiting due to cancer chemotherapy. Postoperative nausea and vomiting. Vomiting due to drugs or fevers. Adverse effects Extrapyramidal effects e.g. dystonia and dyskinesia. Hyperprolactinemia Sedation Postural hypotension 5. Neurokinin-1 receptor blockers: Aprepitant Antiemetic mechanism Substance-P induces vomiting through stimulation of NK-1 receptors. Aprepitant blocks this receptor. Uses as antiemetic In combination with 5-HT3 blockers to treat vomiting due to cancer chemotherapy Adverse effects Diarrhea and fatigue 6. Cannabinoid derivatives: Nabilone and Dronabinol Antiemetic mechanism It is a partial agonist at central and peripheral cannabinoid receptors (CB1). The exact mechanism is unclear. Uses as antiemetic Vomiting due to cancer chemotherapy Patients refractory to other antiemetics. Adverse effects Hallucinations Psychotropic effects Drug abuse. Sedation Postural hypotension 7. Vitamin B6 (pyridoxin) Antiemetic mechanism May be related to the balance between GABA (CNS inhibitory transmitter) and glutamate (CNS excitatory transmitter). Uses as antiemetic Vomiting in pregnancy (50 mg at bedtime). Vomiting in children 8. Corticosteroids Dexamethasone Prednisolone Antiemetic mechanism The exact mechanism is unclear. Uses as antiemetic Combined with Vit B6 to treat vomiting in pregnancy. Vomiting due to cancer chemotherapy. Adverse effects Most of these side effects occur after long duration of therapy: a. Iatrogenic Cushing syndrome: occurs if doses up to 100 mg hydrocortisone are used daily for > 2 weeks. It is characterized by moon face, buffalo hump, thin limbs, osteoporosis, hypertension, DM, edema, etc. b. Immune suppression → flaring of infections (especially viral &TB). c. Hypertension due to salt & water retention d. Hyperglycemia. e. Peptic ulcer: due to prolonged inhibition of gastroprotective PGs. f. ↑ IOP (Glaucoma): due to ↓ Aqueous humor drainage. g. Osteoporosis. h. Growth retardation in children. i. Skin atrophy & hypopigmentation after prolonged topical use. j. Sudden withdrawal after prolonged administration causes acute addisonian crisis 9. Benzodiazepines Lorazepam Diazepam Antiemetic mechanism Allosteric facilitation of central GABA inhibitory transmission Uses as antiemetic Stress-related vomiting To controls symptoms in Ménière disease Adverse effects – Physical dependence (treated by gradual withdrawal) – Paradoxical or rebound excitement. – Apnea after rapid i.v. injection (flumazenil is the antidote) – Tolerance.