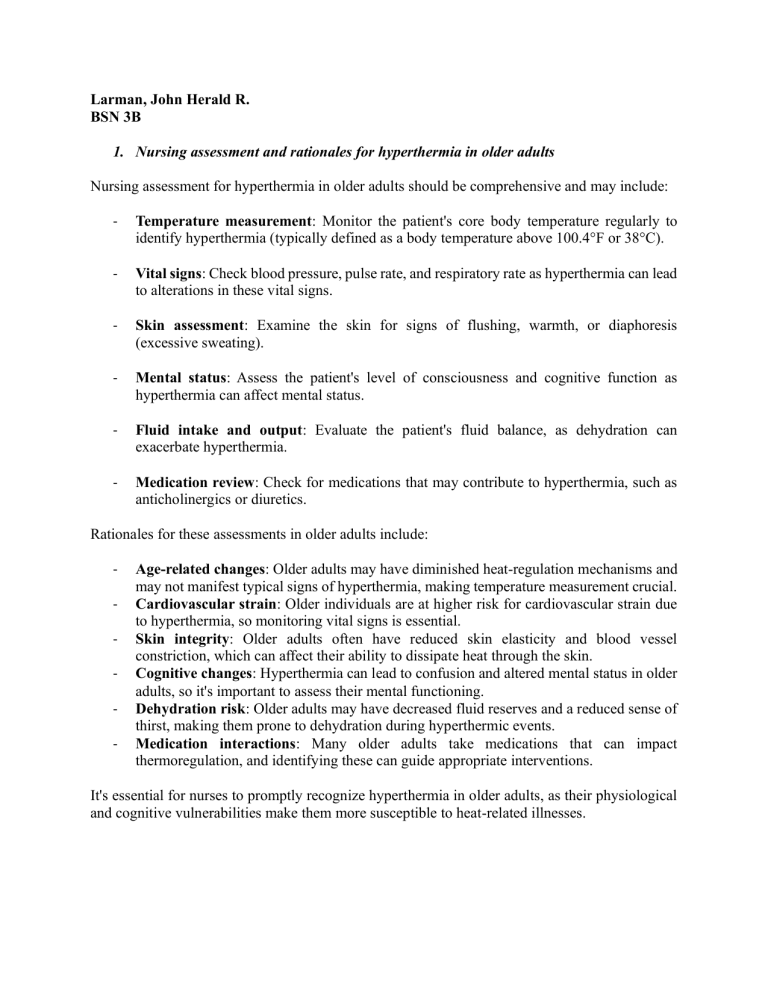
Larman, John Herald R. BSN 3B 1. Nursing assessment and rationales for hyperthermia in older adults Nursing assessment for hyperthermia in older adults should be comprehensive and may include: - Temperature measurement: Monitor the patient's core body temperature regularly to identify hyperthermia (typically defined as a body temperature above 100.4°F or 38°C). - Vital signs: Check blood pressure, pulse rate, and respiratory rate as hyperthermia can lead to alterations in these vital signs. - Skin assessment: Examine the skin for signs of flushing, warmth, or diaphoresis (excessive sweating). - Mental status: Assess the patient's level of consciousness and cognitive function as hyperthermia can affect mental status. - Fluid intake and output: Evaluate the patient's fluid balance, as dehydration can exacerbate hyperthermia. - Medication review: Check for medications that may contribute to hyperthermia, such as anticholinergics or diuretics. Rationales for these assessments in older adults include: - Age-related changes: Older adults may have diminished heat-regulation mechanisms and may not manifest typical signs of hyperthermia, making temperature measurement crucial. Cardiovascular strain: Older individuals are at higher risk for cardiovascular strain due to hyperthermia, so monitoring vital signs is essential. Skin integrity: Older adults often have reduced skin elasticity and blood vessel constriction, which can affect their ability to dissipate heat through the skin. Cognitive changes: Hyperthermia can lead to confusion and altered mental status in older adults, so it's important to assess their mental functioning. Dehydration risk: Older adults may have decreased fluid reserves and a reduced sense of thirst, making them prone to dehydration during hyperthermic events. Medication interactions: Many older adults take medications that can impact thermoregulation, and identifying these can guide appropriate interventions. It's essential for nurses to promptly recognize hyperthermia in older adults, as their physiological and cognitive vulnerabilities make them more susceptible to heat-related illnesses. 2. General interventions for hyperthermia in older adults. - Hyperthermia, an elevated body temperature due to various causes, is a significant concern in older adults because of age-related physiological changes that affect thermoregulation. Older adults often exhibit atypical symptoms, so vigilant assessment is essential. General interventions for hyperthermia in older adults include cooling the environment, encouraging hydration, using cooling techniques, adjusting medications, treating underlying causes, and educating patients and caregivers on heat prevention. Educating the patient and their caregivers is crucial. Ensure they are aware of the importance of staying cool, staying hydrated, and seeking medical attention if necessary. In summary, hyperthermia in older adults demands a multifaceted approach. Timely recognition, cooling measures, medication management, and addressing underlying causes are fundamental. Nursing care in hyperthermia cases for older adults should be vigilant, tailored to individual needs, and mindful of the unique challenges posed by aging-related changes in thermoregulation. 3. Interventions for malignant hyperthermia. Malignant hyperthermia is a rare but life-threatening condition triggered by certain drugs used during anesthesia. Immediate interventions include: 1. Stop Triggering Agents: Discontinue the anesthesia agents like succinylcholine and inhalational anesthetics. 2. Administer Dantrolene: Dantrolene is the specific antidote for malignant hyperthermia. It helps to reduce muscle contractions and hyperthermia. 3. Cooling Measures: Lower the patient's body temperature with cooling blankets or ice packs to prevent hyperthermia. 4. Supportive Care: Provide supportive care, including intravenous fluids, electrolyte correction, and medications to stabilize the heart and blood pressure. 5. Monitor: Continuously monitor vital signs, ECG, and arterial blood gases. Seek immediate medical attention in suspected cases of malignant hyperthermia, as it can be lifethreatening if not treated promptly. 4. What is the difference between senescence and senility? Senescence and senility are related terms, but they refer to different concepts: Senescence is a natural biological process of aging that occurs in all living organisms, including humans. It is the gradual and progressive deterioration of cells and organs over time. Senescence is a normal part of the aging process and involves various age-related changes in the body, such as reduced physical and cognitive abilities. On the contrary, senility is not a commonly used medical term today. Historically, it was used to describe the mental and physical infirmities or disabilities that were often associated with old age. It is an outdated and somewhat pejorative term, and healthcare professionals now use more specific and less stigmatizing terms to describe age-related conditions, such as dementia, cognitive decline, or physical frailty. In summary, senescence is the natural process of aging, while senility, which is an antiquated term, used to refer to the mental and physical decline often seen in old age. It's important to use more precise and respectful terminology when discussing age-related health issues.