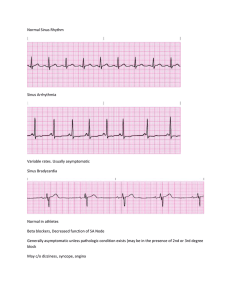
NORMAL SINUS RHYTHM Definition Reflects normal conduction of the sinus impulse through the atria and ventricles Rate Atrial and ventricular rates are the same and range from 60–100 bpm Rhythm Rhythm is regular or essentially regular P Wave Normal PR Interval Normal QRS Complex Normal QT Interval Normal T Wave Normal Conduction Normal Causes Occurs in healthy cardiac systems Symptoms No symptoms; patient is hemodynamically stable Medication None required Treatment None required Distinguishing N/A feature SINUS TACHYCARDIA Definition Sinus tachycardia results when the SA node fires faster than 100 bpm. It is a normal response to stimulation of the sympathetic nervous system Rate Both atrial and ventricular rate >100 bpm, my even be as fast as 180 bpm Rhythm Gradual onset; Regular or essentially regular P Wave Normal; may be hidden in T wave is rate is too fast PR Interval Normal QRS Complex Normal QT Interval May shorten T Wave Normal; may overcome the P waves in rapid rates Conduction Normal Causes Hyperthyroidism, hypovolemia, HF, anemia, exercise, use of stimulants, fever, sympathetic response to fear/pain, anxiety, inotropic meds, caffeine Symptoms HR may CO d/t shorter filling times for the ventricles Medication None specifically (antipyretics if caused by fever, pain medication if caused by pain) Treatment Tx depends on context (Sinus tachy may be a normal response). Treat underlying cause (ceasing/starting medication, replacing blood or fluids, etc.) Distinguishing This is a normal fast rate. P’s may not be present and that’s ok, they may just be feature hiding within a T wave SINUS BRADYCARDIA Definition Sinus bradycardia may be normal for athletes or may occur during sleep. Although this may be asymptomatic, it may cause instability. Assess for instability in pt Rate Both atrial and ventricular rates <60 bpm Rhythm Regular or essentially regular P Wave Normal PR Interval Normal QRS Complex Normal QT Interval Might be prolonged T Wave Normal Conduction Decreased in SA node (looks like NSR but at a slower rate) Causes [Normal in athletes and during sleep] ICP, hypoxia, hypothermia, heart disease, excessive inhibitory vagal (vomiting, BM), drug induced (digoxin, Inderal), Ca channel blockers, Beta Blockers Symptoms A slowed heart rhythm may cause a decrease in CO, resulting in hypotension and decreased organ perfusion; changes in LOC, chest discomfort, SOB/resp. distress, pulmonary congestion/crackles, rapid/slow/weak pulse, dizziness, syncope, fatigue, restlessness Medication Atropine (IVP, most common drug for low HR, one-time dose); Isuprel (IV drip, cont. infusion, not a permanent fix) Treatment None if mild; observation; pacing/pacemaker Distinguishing A normal slow feature SINUS ARRYTHMIA Definition A cyclical change in heart rate that s associated with respiration. HR increases with inspiration, slows with expiration d/t changes in vagal tone. Rate Atrial and ventricular rates between 60–100 bpm Rhythm Regularly irregular; pattern of increasing and decreasing P Wave Normal PR Interval Normal QRS Complex Normal QT Interval Normal T Wave Normal Conduction Normal Causes Usually associated with respirations Symptoms This rhythm is tolerated well Medication None necessary Treatment None necessary Distinguishing Alternating patterns of slow and fast HR (within the 60-100 range) feature PREMATURE ATRIAL CONTRACTIONS (PAC) Definition A single ectopic beat arising from atrial tissue, not the SA node. The PAC occurs earlier than the next normal beat and interrupts the regularity of the underlying rhythm. PACs are common, but denote an irritable area in the atria that has developed the property of automaticity Rate The rate matches that of the underlying rhythm (usually within normal range) Rhythm Irregular d/t early beat; usually the pause is noncompensatory (doesn’t resume original rhythm after the funny little beat) P Wave Usually different than normal because it arises from a different area of the atria; It may follow or be in the T wave PR Interval Usually shorter QRS Complex Normal or wide; a non-conducted P wave may not be followed by a QRS (the ventricles may not have been able to full repolarize before the ectopic beat occurred, therefore not firing and producing a QRS complex) QT Interval Normal, unless the T wave has been affected by a premature P wave T Wave Usually normal unless the P wave occurs within the T wave, then the T wave will present abnormal Conduction Originates from a different location other than the SA node; a different area in the atria has been irritated and is producing automaticity Causes HF, anxiety, caffeine, nicotine, tobacco, enlarged atria, electrolyte imbalances, digoxin, Low K or Mg myocardial hypertrophy/dilation, ischemia, lung disease, may be a normal variant Symptoms Usually well tolerated, though the pt may complain of palpitations Medication None necessary Treatment Not usually necessary; increasing numbers of PACs (Paroxysmal Atrial Tachycardia: 3+ PACs in a row, a run; pt bursts in and out of this) can evolve into A fib or A flutter – observe and assess Distinguishing The beat comes in earlier, and the rhythm comes back noncompensated feature ATRIAL FLUTTER Definition Arises from a single irritable focus in the atria; extremely fast Rate Atrial rate is between 240-320 bpm, typically 300 bpm; Ventricular rate is determined by the conduction ratio of the flutter waves, usually 150 bpm Rhythm Atrial rhythm regular, ventricular may or may not be P Wave Flutter waves, sawtooth; rapid fire, usually a pattern of P waves to QRS 2:1, 3:1, 4:1, 5:1 PR Interval No PR interval present QRS Complex May not be regular (depends on if any conduction comes thru the AV node from the P wave) QT Interval Normal, unless distorted by a flutter wave T Wave May not be regular (depends on if any conduction comes thru the AV node from the P wave) Conduction Possible rapid-fire ectopic focus (hijacks electrical activity of heart) Causes Lung disease, ischemic heart disease, hyperthyroidism, hypoxemia, HF, alcoholism, digoxin toxicity, SA or atrial damage Symptoms Atrial quivering: doesn’t fill properly, 25% decrease in CO and loss of atrial kick; pt is usually asymptomatic Medication Anticoagulant therapy (quivering doesn’t push all blood out of atrium, blood pools and can clot); beta blockers (slows/controls HR); digoxin; Ca channel blockers Treatment Cardioversion, ablation Distinguishing Sawtooth pattern feature ATRIAL FIBRILLATION Definition The most common dysrhythmia. Atrial fibrillation arises from multiple ectopic foci in the atria, causing chaotic quivering of the atria and ineffectual atrial contraction. AV node is bombarded with hundreds of atrial impulses and conducts these impulses in an unpredictable manner to the ventricles. When A fib occurs sporadically, it is called Paroxysmal Atrial Fibrillation Rate If the rate is normal it is called “controlled A fib,” Otherwise, 150-300 bpm. Atrial rate may be as high as 700 bpm Rhythm Totally irregular (irregularly irregular) P Wave Wavy isoelectric line, no discernable P waves PR Interval None QRS Complex Normal; wide if a bundle branch block exists QT Interval Normal; wide if a bundle branch block exists T Wave Should be present, visible in a different lead perspective Conduction Chaotic conduction. AV node conducts hundred of impulses sporadically Causes Ischemic heart disease, valvular heart disease, hyperthyroidism, lung disease, heart failure, aging, stress, alcohol, caffeine, COPD Symptoms Poor ventricular filling d/t loss of atrial kick, stable or decreased CO, possible dizziness, clots may form in atria, Pt may or may not be aware of A fib., worsening of heart failure symptoms Medication Anticoagulants, amiodarone, digoxin, Inderal, verapamil, beta blockers, antithrombotic Treatment Cardioversion, ablation Distinguishing Isoelectric line with QRS/T present feature JUNCTIONAL RHYTHMS (ESCAPE, ACCELERATED, & TACHY) Definition Junctional rhythms are dysrhythmias of the AV node d/t disease or impairment of the SA node. Rate Junctional escape rhythm: 40-60 bpm; Accelerated Junctional: 60-100 bpm; Junctional Tachycardia: >100 bpm Rhythm Regular P Wave P wave will be inverted (before the QRS), absent (hidden in the QRS), or late and inverted (after the QRS) PR Interval < 0.12 sec. if present QRS Complex Usually normal QT Interval Normal T Wave Normal Conduction The SA node may be impaired, so the impulse originates from the AV node. This impulse may jump back into the atria Causes The escape rhythm may be caused by loss of SA node activity. Accelerated/Tachy may be caused by sinoatrial node disease, ischemic heart disease, electrolyte imbalances, digitalis toxicity, hypoxemia Symptoms Escape: when it’s bradycardia, not dangerous on its own. Assess pt tolerance. Accelerate/Tachy: Pt my have decreased CO and hemodynamic instability, depending on the rate Medication Escape: if symptomatic, give atropine, dopamine, epinephrine infusions Treatment Escape: transcutaneous pacing Accelerate/Tachy: assess and treat the tachycardia if the pt is hemodynamically unstable Distinguishing Inverted or absent P waves feature PREMATURE JUNCTIONAL CONTRACTIONS (PJC) Definition Irritable areas in the AV node and junctional tissue can generate premature beats that are earlier than the next expected beat. Like PACs but with characteristics of a junctional beat Rate The rate is that of the underlying rhythm Rhythm Premature beat, interruption of rhythm (may or may not be compensatory) P Wave May be before/inverted, within, or after QRS PR Interval Short on the PJC beat QRS Complex Normal QT Interval Normal T Wave Normal; followed very closely by the PJC beat Conduction AV node usurps and gains control of conduction Causes May be a normal variant, increased vagal tone, digitalis toxicity, HF, edema, ischemic or valvular heart disease, response to endogenous or exogenous catecholamines, such as epinephrine Symptoms This rhythm is well tolerated, but the patient may experience palpitations if the PJCs occur frequently Medication Quinidine, hold Dig Treatment Stop stimulants; No treatment usually necessary Distinguishing Like a PAC, except the P is inverted feature PAROXYSMAL SUPRAVENTRICULAR TACHYCARDIA (SVT) Definition Occurs above the ventricles and it has an abrupt onset and cessation. It is initiated by either a PAC or a PJC. An abnormal conduction pathway around the AV node or an accessory pathway around the AV node results in extreme tachycardia. Paroxysmal: abrupt onset and end Rate HR is 150-250 bpm Rhythm Regular P Wave Absent, cannot be visualized. If present, it shortens the PR interval PR Interval If P wave present, the PR interval is shortened QRS Complex Narrow, normal QT Interval Normal T Wave Normal Conduction Above the ventricles Causes Catecholamines, heart disease, stimulants, anatomic abnormalities, electrolyte imbalance, congenital. Can occur in healthy, young adult w/o structural heart disease Symptoms Patient may be asymptomatic or symptomatic, dizzy, hypotensive Medication Adenosine (IVP, rapid action) Treatment Vagal maneuvers (causes decrease in HR), cardioversion Distinguishing Rapid pace, absent P feature PREMATURE VENTRICULAR CONTRACTIONS (PVC) Definition A common ventricular dysrhythmia. PVCs are early beats that interrupt the underlying rhythm. Originating from one focus: identical PVCs. Originating from multiple foci: unidentical PVCs. Bigeminy: every other beat. Unifocal: just one beat. Couplets/Pair: two paired together. Runs: grouping of a few (6+ can cause VTach). Fused: simultaneous with a normal beat. Multifocal: frequent, rare, occasional. R on T phenomenon: when the R wave of PVC falls on the T wave of a normal beat Rate Not significant, doesn’t matter. The underlying rhythm doesn’t change Rhythm PVC is a premature beat; The PVC doesn’t interrupt the underlying rhythm (compensatory rhythm). P Wave Usually not identified. May be buried in the QRs or the T PR Interval None QRS Complex Longer than 0.12 seconds. The QRS complex of the PVC is wide and bizarre QT Interval May be distorted or unidentified if warped by the PVC. Would be normal in the other normal beats T Wave T wave may be oriented opposite direction of the QRS. If a PVC occurs during a T wave, VTach may occur. The peak of the T wave through the downslope of the T wave is considered the vulnerable period, which coincides with partial repolarization of the ventricles Conduction Impulse arises from a single ectopic foci or multiple foci within the ventricles Causes HF, MI, increased catecholamine, stimulants, hypoxia, excessive digoxin, decreased K or MG (electrolyte imbalances), acid base imbalance, ischemic heart disease Symptoms Occasional or rare, usually well tolerated in patients. PVCs may be experienced as palpitations, pt may become symptomatic if the PVCs occur frequently. Can be a precursor of VTach and no CO. Risking R on T. Lightheadedness Medication Beat blockers, Ca channel blockers, antiarrhythmics (amiodarone, flecainide) Treatment Chart how often PVCs are seen (frequent, rare, occasional). Treat underlying cause if increasing in frequency Distinguishing Compensatory (the PVC doesn’t interrupt the underlying rhythm). Wide, bizarre QRS feature complex. VENTRICULAR TACHYCARDIA Definition A rapid, life-threatening dysrhythmia originating from a single ectopic focus in the ventricles. Characterized by three PVCs in a row Rate > 100 bpm. Usually 150 bpm up to 250 bpm. >250 can be fatal d/t decreased perfusion of the brain. Pt may or may not have a pulse Rhythm The rhythm is regular unless capture beats occur and momentarily interrupt the VT P Wave May be absent b/c the wave of depolarization associated with VT rarely reaches the atria. If present, P waves have no association with QRS. P waves may be firing at a normal rate and show up randomly throughout the strip (AV dissociation). A P wave could “capture” the ventricle b/c of the timing of atrial depolarization, interrupting VT with a single beat, producing an apparently normal QRS; then VT recurs. This helps differentiate VT from wide complex tachycardias PR Interval None QRS Complex Wide, bizarre d/t abnormal depolarization of the ventricles. Greater than 0.12 sec., wider than 0.16 sec. QT Interval None T Wave The polarity of the T wave is opposite to that seen in the QRS Conduction Originates from a single ectopic focus in the ventricles Causes CAD, MI, Digoxin toxicity, HF, electrolyte disturbances (low K is very significant), increased ICP, meth/cocaine, ischemia, chronic sleep apnea, genetic abnormalities, QT prolongation Symptoms Life threatening!! Decreased/no perfusion. If there is enough CO, HR/BP may be present. If CO is impaired, the pt has s/s of low CO and low perfusion. Possible cardiac arrest. Eyes rolling back, no BP, no HR, vomiting possible Medication If pulse is present and BP is stable, treat w/ drugs. IV amiodarone or lidocaine. Mexiletine, sotalol. Drug cardioversion: decreases HR Treatment No pulse: call code, BLS, defibrillate (defib fast and early for best results). Electrocardioversion (delivered on R wave, T wave is avoided) Distinguishing Wide ups and downs. Rapid rate, poor pt tolerance, life threatening! feature VENTRICULAR FIBRILLATION Definition A chaotic rhythm characterized by a quivering of the ventricles, which results in total loss of cardiac output and pulse. Wavy baseline with no PQRST complex. V Fib may be coarse or fine Rate May not be discernable. Could be 300-600 bpm Rhythm Rapid irregular succession of chaotic, bizarre waves, oscillation of baseline P Wave None identifiable PR Interval None identifiable QRS Complex None identifiable QT Interval None identifiable T Wave None identifiable Conduction Uncoordinated muscle fiber contractions. Quivering of ventricles Causes Ischemic and valvular heart disease, electrolyte or acid-base imbalances, QT prolongation, excessive medications (quinidine, procainamide, digoxin), electrocution Symptoms Life-threatening!! This pt is in cardiac arrest. Absent CO, fatal if not corrected within minutes Medication Drugs used during a code (epi, etc.). Meds are taken to decrease future episodes Treatment The more immediate the treatment, the better the odds are for survival. Must assess pt and leads first, as this rhythm may be caused by loose leads or electrical interference. Call code, BLS, defibrillation. May implant ICD (implanted cardioverter defibrillator) Distinguishing Complete chaos, no distinguishable PQRST complex, life threatening!! feature IDIOVENTRICULAR (ESCAPE) RHYTHM Definition An escape rhythm that is produced by the Purkinje fibers. Emerges only when SA and AV nodes fail to initiate an impulse. Because this last pacemaker cell is in the ventricles, the QRS complex appears wide and bizarre with a slow rate. Considered a lethal dysrhythmia b/c if the Purkinje cease firing, the pt will go into asystole. Accelerated Idioventricular Rhythm (AIVR): 40-100 bpm; may be seen after reperfusion of a coronary artery by thrombolytics, after angiography, stent placement, or cardiac surgery Rate 20-40 bpm; 40-100 bpm is accelerated idioventricular rhythm Rhythm Atrial: non or irregular. Ventricle: regular P Wave Usually not present. If present, normal, irregular, or abnormal PR Interval None QRS Complex Wide and bizarre QT Interval None T Wave Follows QRS and shows opposite polarity Conduction Rhythm by default, slow inherent rate of the ventricles. Still base electrical activity but no emptying or filling is happening Causes Failure of the SA/AV nodes, common with MI, heart disease, drug induced (narcotics) Symptoms May have enough rate to maintain perfusion, may progressively worsen. The extreme bradycardia may cause the same s/s as any severe bradycardia. Asystole may occur Medication Atropine, Isuprel Treatment Treat underlying cause, pacing (but pacing only works if there is something to pace – can’t pace dead heart tissue), BLS/ACLS Distinguishing Extremely slow rate, wide QRS feature VENTRICULAR ASYSTOLE (STANDSTILL) Definition Characterized by complete cessation of electrical activity. A flat baseline is seen, without evidence of PQRST complex. Absent pulse, no CO, cardiac arrest has occurred. Occurs following VF. If following Ventricular Escape Rhythm (VER), the asystole is referred to as ventricular standstill Rate None Rhythm None P Wave None PR Interval None QRS Complex None QT Interval None T Wave None Conduction Cessation of electrical activity Causes Lead displacement, electrode coming off (assess pulse) Symptoms Patient is in cardiac arrest. Severe MI, dying heart, severe hypoxia, drug overdose, hyperkalemia, acidosis (always check electrolytes), VF, VER Medication Epinephrine bolus, Vasopressin Treatment ACLS/BLS, call code, CPR Distinguishing Flat line feature FIRST DEGREE AV BLOCK Definition Consistent delayed conduction through the AV node or the atrial conductive tissue. Represented on the ECG as a prolonged QT interval. Common in older adults and in cardiac patients. Rate Normal Rhythm Regular P Wave Normal PR Interval Prolonged PR interval is the key feature of 1st degree AV block QRS Complex Normal QT Interval Normal T Wave Normal Conduction Conduction is delayed at the AV node. An impulse from the SA node has trouble passing through the AV node and to the rest of the ventricles. Causes MI of the inferior wall; dig toxicity. Aging and ischemic and valvular heart disease can cause AV block Symptoms This block is well tolerated. No s/s but can progress to type II or III. Adequate perfusion still exists Medication None required Treatment None required. Possible to treat underlying cause (monitor electrolyte imbalances, medicinal causes, etc.). Observe for possible progression Distinguishing “If the R is far from P, then you have a first degree” feature SECOND DEGREE AV BLOCK TYPE I (MOBITZ I/WENCKEBACH) Definition Mobitz I is a progressive lengthening of the PR Interval until there is a P wave without a QRS. The AV node progressively delays conduction to the ventricles resulting in progressively longer PR intervals until the QRS complex is finally dropped. The PR interval following the dropped QRS is shorter and returns to the original rhythm. The AV node can recover and conduct the next atrial impulse. If the dropped beat occurs frequently, describe the conduction ratio (2:1, 3:1, 4:1, etc.) Rate Atria: normal. Ventricle: depends on the AV node and what is able to come through the AV node Rhythm Atria: normal. Ventricle: usually irregular P Wave More frequent than QRS (because the SA node is fine and conducts a proper beat through the atria) PR Interval Progressive lengthening, then 1 P wave is blocked by the AV node, not allowed to pass, and QRS does not occur QRS Complex Normal when it does appear. The QRS wave will be normal on the complexes that are produced. One will not appear before a P wave where the impulse was blocked QT Interval Normal when they do appear T Wave Normal when it does appear Conduction Defective conduction of an impulse in the AV node Causes Aging, AV nodal blocking drugs, acute inferior MI or right ventricular infarction, ischemic heart disease, digitalis toxicity, excess vagal response Symptoms Usually well tolerated, unless there is underlying bradycardia, or frequently dropped beats. Can progress to higher AV block. Medication None required Treatment No treatment necessarily needed, unless the dropped beats occur very frequently. Treat possible underlying cause. Stop possible contributing medications. Rarely are permanent pacemakers called for Distinguishing “Longer, longer, longer, drop! Then you have a Wenkebach” feature SECOND DEGREE AV BLOCK TYPE II (MOBITZ II) Definition Mobitz II is a more critical type of second-degree heart block that requires early recognition and intervention. This block is often associate w/ with a bundle branch block and a corresponding widened QRS complex; however, QRS complexes can be narrow. This block can progress to the more clinically significant third block and may cause symptomatology Rate HR is slower than the underlying rhythm because of the dropped beats. Ventricular rate less than atrial and is irregular Rhythm Atrial: regular. Ventricular: no regularity, sudden drop of complexes P Wave More numerous than QRS. May not always have an accompanying QRS PR Interval Normal or prolonged, but remains consistent until suddenly one or more wave may occur w/o a QRS QRS Complex Normal or wide. May be missing QT Interval Normal T Wave Normal Conduction The conduction abnormality usually occurs below the AV node, either in the Bundle of His Causes Bundle branch damage, anterior wall MI, heart disease, increased vagal tone, conduction system diseases, ablation of the AV node, inferior and right ventricular infarctions Symptoms Like bradycardia. The pt may tolerate one missed beat, but symptoms may occur if more than one beat is missed Medication Atropine, Isuprel Treatment Pacemaker. Transcutaneous or transvenous pacing for emergent treatment Distinguishing “If some P’s don’t get through (to the ventricles), then you have a Mobitz II)” feature Every QRS has a P, not every P has a QRS THIRD DEGREE AV BLOCK Definition Often called complete heart block b/c no atrial pulses are conducted through the AV node to the ventricles. The atria and ventricles are beating independently of each other because the AV node is completely blocked. The sinus impulse is blocked, and the ventricles receive no impulse. No communication between the atria and ventricle Rate The atria and ventricles beat at different rates. Atria: sinus rhythm. Ventricle: escape rhythm. Atrial rate will be faster than the ventricular rate. Rhythm Each may be regular. Both are firing at random rates. P-P intervals match, R-R intervals match, but they aren’t associated with each other P Wave Normal PR Interval There will be no PR interval in the absence of conduction. If there is one, it happened by chance QRS Complex Often widened greater than 0.12 sec. with a ventricular escape rhythm QT Interval Normal, if not interrupt by a P T Wave Normal, if not interrupt by a P Conduction The block of conduction can occur at the level of the AV node, bundle of His, or the bundle branches Causes Inferior wall MI, myocarditis, electrolyte imbalance, medication (Dig or Inderol toxicity), ischemic heart disease, acute myocardial infarction, and conduction system diseases Symptoms Pt may become symptomatic b/c of the bradycardia of the escape rhythm. Syncope, confusion, dyspnea, CP, risk of death Medication Atropine, Isuprel Treatment Temporary or permanent pacing, emergent action, identify underlying causes and treat or eliminate it (meds, infection, etc.). May implant pacemaker if cause is irreversible Distinguishing “If P’s and Q’s don’t agree, then you have a third degree” feature