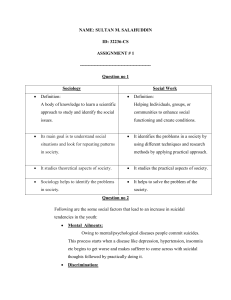
The Suicidal Client Chapter 16 Introduction ▪ Suicide is not a diagnosis or a disorder; it is a behavior. ▪ More than 90% of individuals who attempt or commit suicide have a diagnosed mental disorder. Suicide Statistics ▪ Suicide is the 10th leading cause of death in the US ▪ Each year 44,193 Americans die by suicide ▪ For every suicide - 25 attempts are made ▪ Suicide costs the US $ 51 Billion annually (American Foundation for Suicide Prevention, 2017) ▪ ▪ ▪ ▪ ▪ ▪ Epidemiological Factors The annual age-adjusted suicide rate is 13.26 per 100,000 individuals. Men die by suicide 3.5x more often than women. On average, there are 121 suicides per day. White males accounted for 7 of 10 suicides in 2015. Firearms account for almost 50% of all suicides. The rate of suicide is highest in middle age — white men in particular. (American Foundation for the Prevention of Suicide, 2017) Risk Factors ▪ Marital status ▪ The suicide rate for single persons is twice that of married persons. ▪ Gender ▪ Women attempt suicide more often, but more men succeed. ▪ Men commonly choose more lethal methods than women. Risk Factors ▪ Age -Suicide risk and age are positively correlated. ▪ Risk of suicide increases with age, particularly among men. ▪ Suicidal rates rise sharply during adolescence. ▪ White men older than 80 years are at the greatest risk of all age/gender/race groups. Risk Factors ▪ Religion ▪ Affiliation with a religious group decreases risk of suicide. ▪ Catholics have lower rates than Protestants or Jews. ▪ Socioeconomic status ▪ Individuals in the very highest and lowest social classes have higher suicide rates than those in the middle class. Risk Factors ▪ Ethnicity ▪ Whites are at highest risk for suicide, followed by Native Americans, African Americans, Hispanic Americans, and Asian Americans. Other Risk Factors ▪ Psychiatric illness: mood disorders are the most common psychiatric illnesses that precede suicide. Other psychiatric disorders that account for suicidal behavior include: ▪ Substance-related disorders ▪ Schizophrenia or psychosis with command hallucinations ▪ Personality disorders ▪ Anxiety disorders Other Risk Factors ▪ Severe insomnia ▪ Affliction with a chronic painful or disabling illness ▪ Homosexual individuals have a higher risk of suicide than their heterosexual counterparts ▪ Personal stressors ▪ Losses (personal or financial) ▪ Bullying (perpetrators and victims) Higher Risk Factors ▪ Family history of suicide ▪ Having attempted suicide previously increases the risk of a subsequent attempt ▪ About half of those who ultimately commit suicide have a history of a previous attempt Predisposing Factors: Psychological Theories of Suicide ▪ Anger turned inward ▪ Hopelessness ▪ Desperation and guilt ▪ History of aggression and violence ▪ Shame and humiliation ▪ Developmental stressors Nursing Process: Assessment ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ Age Gender Ethnicity Martial status Socioeconomic status Occupation Lethality and availability of method Religion Family history of suicide Chronic and terminal physical illnesses Nursing Process: Assessment ▪ Presenting symptoms/medical-psychiatric diagnosis ▪ Suicidal ideas or previous attempts ▪ Seriousness of intent ▪ Plan ▪ Means ▪ Verbal and behavioral clues ▪ Interpersonal support system Nursing Process: Assessment ▪ Analysis of the suicidal crisis ▪ The precipitating stressor ▪ Relevant history ▪ Life-stage issues ▪ Psychiatric/medical/family history ▪ Coping strategies Nursing Process: Diagnosis / Outcome Criteria Nursing diagnoses for the suicidal patient may include: ▪ Risk for suicide ▪ Hopelessness Outcome Criteria – The patient: ▪ 1. Has experienced no physical harm to self. ▪ 2. Sets realistic goals for self. ▪ 3. Expresses some optimism and hope for the future. Nursing Process: Planning/Implementation - Inpatient ▪ Ask client directly: “Have you thought about harming yourself in any way? ▪ Create a safe environment. ▪ Formulate a short term verbal or written contract for safety. ▪ Maintain close observation. ▪ Maintain special care with medication administration. ▪ Make rounds at frequent, irregular intervals. ▪ Encourage expression of honest feelings. Nursing Process: Planning/Implementation Guidelines for treatment of the suicidal patient on an outpatient basis: ▪ Do not leave the person alone. ▪ Establish a no-suicide contract with the person. ▪ Enlist the help of family or friends. ▪ Schedule frequent appointments. ▪ Establish rapport and promote a trusting relationship. Nursing Process: Planning/Implementation Guidelines for treatment of the suicidal patient on an outpatient basis ▪ Ask patient directly if they are having thoughts about harming themselves in any way. ▪ Discuss the current crisis situation in the patient’s life. ▪ Identify areas of self-control. ▪ Antidepressant medications may be prescribed. Nursing Process: Planning/Implementation Crisis counseling with the suicidal client: ▪ Focus on the current crisis and how it can be alleviated. ▪ Note client’s reactivity to the crisis and how it can be changed. ▪ Work toward restoration of the client’s self-worth, status, morale, and control. ▪ Introduce alternatives to suicide ▪ Rehearse more positive ways of thinking. Nursing Process: Planning/Implementation ▪ Crisis counseling with the suicidal client ▪ Identify experiences and actions that affirm self-worth and self-efficacy. ▪ Encourage movement toward the new reality. ▪ Be available for ongoing therapeutic support and growth. Nursing Process: Planning/Implementation Information for family and friends of the suicidal patient: ▪ Take any hint of suicide seriously. ▪ Do not keep secrets. ▪ Be a good listener. ▪ Communicate to the person the importance of having them in your life. ▪ Know about suicide intervention resources. ▪ Restrict access to firearms or other means of self-harm. Nursing Process: Evaluation ▪ Develop and maintain a more positive self-concept. ▪ Learn more effective ways to express feelings to others. ▪ Achieve successful interpersonal relationships. ▪ Feel accepted by others and achieve a sense of belonging. Nursing Process: Planning/Implementation Information for family and friends of the suicidal patient: ▪ Acknowledge and accept the person’s feelings. ▪ Provide a feeling of hopefulness. ▪ Do not leave him or her alone. ▪ Show love and encouragement. ▪ Help them seek professional help. ▪ Assess the safety of children in the home. ▪ Do not judge or show anger toward the person, or provoke guilt in him or her. Nursing Process: Planning/Implementation Interventions with family and friends of suicide victims ▪ Encourage the person to talk about the suicide. ▪ Assess emotional reaction. ▪ Discourage blaming and scapegoating. ▪ Listen to feelings of guilt and self-persecution. ▪ Talk about personal relationships with the victim. ▪ Recognize differences in styles of grieving. ▪ Assist with development of adaptive coping strategies. ▪ Identify resources that provide support. References American Foundation for Suicide Prevention. (2017). Suicide statistics. Retrieved from https://afsp.org/about-suicide/suicide-statistics/ Townsend, M. C. (2015). Psychiatric mental health nursing: Concepts of care in evidenced-based practice (8th ed.). Philadelphia: F.A. Davis Company