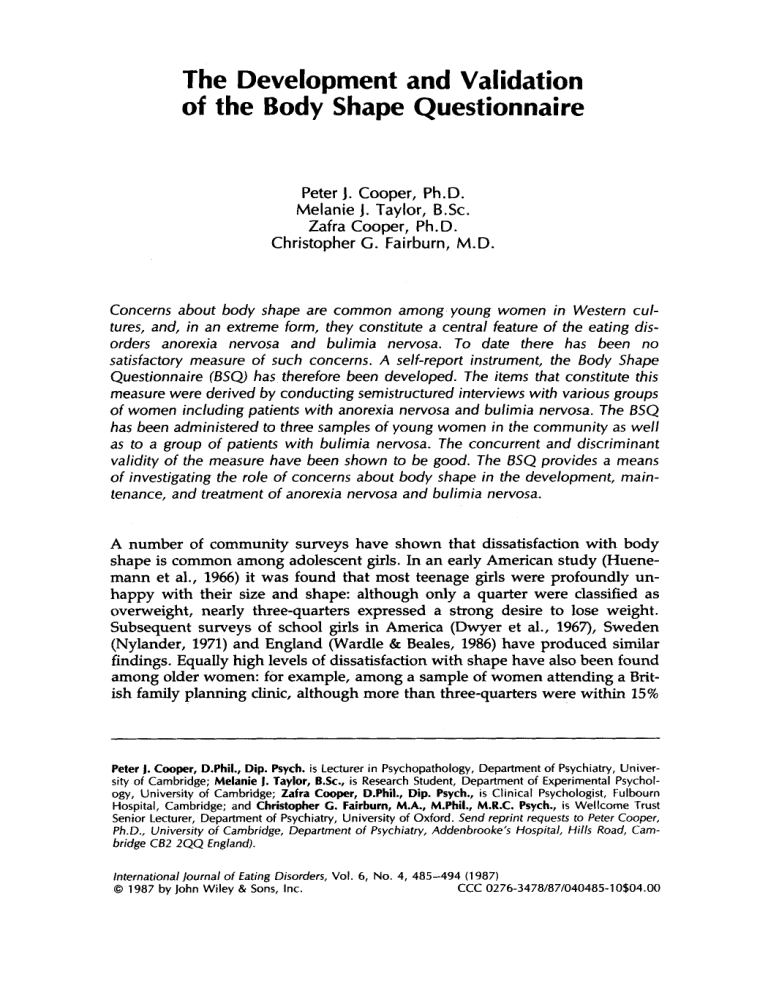
The Development and Validation of the Body Shape Questionnaire Peter 1. Cooper, Ph.D. Melanie 1. Taylor, B.Sc. Zafra Cooper, Ph.D. Christopher G. Fairburn, M.D. Concerns about body shape are common among young women in Western cultures, and, in an extreme form, they constitute a central feature of the eating disorders anorexia nervosa and bulimia nervosa. To date there has been no satisfactory measure of such concerns. A self-report instrument, the Body Shape Questionnaire (SSQ, has therefore been developed. The items that constitute this measure were derived by conducting semistructured interviews with various groups of women including patients with anorexia nervosa and bulimia nervosa. The SSQ has been administered to three samples of young women in the community as well as to a group of patients with bulimia nervosa. The concurrent and discriminant validity of the measure have been shown to be good. The SSQ provides a means of investigating the role of concerns about body shape in the development, maintenance, and treatment of anorexia nervosa and bulimia nervosa. A number of community surveys have shown that dissatisfaction with body shape is common among adolescent girls. In an early American study (Huenemann et al., 1966) it was found that most teenage girls were profoundly unhappy with their size and shape: although only a quarter were classified as overweight, nearly three-quarters expressed a strong desire to lose weight. Subsequent surveys of school girls in America (Dwyer et al., 1967), Sweden (Nylander, 1971) and England (Wardle & Beales, 1986) have produced similar findings. Equally high levels of dissatisfaction with shape have also been found among older women: for example, among a sample of women attending a British family planning clinic, although more than three-quarters were within 15% Peter J. Cooper, D.Phil., Dip. Psych. is Lecturer in Psychopathology, Department of Psychiatry, University of Cambridge; Melanie J. Taylor, B.Sc., is Research Student, Department of Experimental Psychology, University of Cambridge; Zafra Cooper, D.Phil., Dip. Psych., is Clinical Psychologist, Fulbourn Hospital, Cambridge; and Christopher C. Fairburn, M.A., M.Phil., M.R.C. Psych., is Wellcome Trust Senior Lecturer, Department of Psychiatry, University of Oxford. Send reprint requests to Peter Cooper, Ph.D., University of Cambridge, Department of Psychiatry, Addenbrooke's Hospital, Hills Road, Cambridge C62 2QQ England). international journal of fating Disorders, Vol. 6,No. 4,485-494 (1 987) 10804.00 CCC 0276-3478/87/0404850 1987 by John Wiley & Sons, Inc. Cooper et al. 486 of average body weight, 39% reported that they thought themselves to be significantly overweight, and 60% reported persistently feeling fat (Cooper & Fairburn, 1983). A disturbance of body image has long been recognized as a central feature of anorexia nervosa (Bruch, 1962, 1973). Indeed such a disturbance is included as a necessary feature of the disorder in the diagnostic criteria specified in the third edition of the Diagnostic and Statistical Manual of the American Psychiatric Association (1980). However, the notion of body image disturbance is a complex one and may be considered to encompass two related but conceptually distinct aspects, namely concern about body shape and body size overestimation (Garner & Garfinkel, 1981). The latter feature, which reflects an inability to estimate body size accurately, has been extensively studied; but there has been little systematic research into the former aspect. This is unfortunate since concern about body shape is a well recognized feature of both anorexia nervosa (Bruch, 1973) and bulimia nervosa (Fairburn & Cooper, 1984). It may vary in intensity from mild dissatisfaction with particular regions of the body to extreme body shape disparagement in which patients find their body loathsome and revolting. A major reason for the dearth of systematic research into concerns about body shape is the absence of an appropriate method for measuring this phenomenon. Although a number of assessment procedures have been developed that deal with certain aspects of body image, none has provided a specific assessment of the phenomenal experience of concerns about body shape together with their antecedents and consequences. Most measures simply assess dissatisfaction with various body parts, such as the Body Cathexis Scale (Secord & Jourard, 1953), the Body Image Satisfaction Scale (Marsella et al., 1981), the Body Image Questionnaire (Berscheid et al., 1972), and the Body Dissatisfaction subscale of the Eating Disorder Inventory (Garner et al., 1983). Other measures, although containing some items concerned with bodily appearance, do not specifically deal with body shape concerns. For example, the Body Distortion Questionnaire (Fisher, 1970) is largely concerned with unpleasant bodily sensations; the "Appearance" subscale of the Food, Fitness and Looks Questionnaire (Hall et al., 1983) mainly covers cosmetic appearance; and the "Appearance" subscale of the Body Self Relations Questionnaire (Winstead & Cash, 1984) is principally concerned with physical attractiveness. One measure that does address attitudes to body shape is the Eating Disorder Examination (Cooper & Fairburn, 1987), but this is a research interview that was designed to assess the full range of the specific psychopathology of anorexia nervosa and bulimia nervosa and not concern with body shape per se. Thus, there is a need for a specific measure of concerns about body shape. To meet this need, a self-report measure was developed. QUESTIONNAIRE DEVELOPMENT The Derivation of Items Subjects who would be expected to show various degrees of concern about their shape were interviewed using an open-ended schedule. These subjects were encouraged to elaborate upon the experience of "feeling fat," to describe Body Shape Questionnaire 487 the specific circumstances that provoke such feelings, and to provide an account of the behavioral and emotional consequences of such feelings. This interview was administered to 28 young women: 6 patients with bulimia nervosa, 4 patients with anorexia nervosa, 7 women on weight-reducing diets, 3 women attending an exercise class, and 8 female university students. Having completed these 28 interviews it was apparent that no new information was emerging. The interviews, which lasted approximately an hour each, were tape recorded and transcribed. The transcribed material was organized into conceptual categories, and questions were formulated to reflect their content. There were 51 separate questions thereby derived, and a self-report questionnaire was constructed with a 6-point Likert scale (“never”, “rarely,” ”sometimes,” “often,” “very often,” “always”). All questions referred to the subject’s state over the previous 4 weeks. Item Elimination and Questionnaire Validation The Samples The 51-item questionnaire was administered to four samples of women. 1. Patients with bulimia nervosa. The questionnaire was completed by a consecutive series of 19 female patients with bulimia nervosa attending a psychiatric outpatient clinic in Cambridge and a consecutive series of 19 female patients with bulimia nervosa attending a similar clinic in Oxford. All these patients fulfilled either Russell’s (1979) diagnostic criteria for bulimia nervosa or the proposed DSM-111-R criteria for bulimic disorder (American Psychiatric Association, 1985). 2. Family planning clinic attenders. A consecutive series of 371 women attending two family planning clinics in Cambridge over a 4-week period were asked to complete the questionnaire: 13 refused, 276 (95.5%) completed the questionnaire while waiting to see the doctor, and 82 were unable to complete the questionnaire while waiting and were asked to return it by mail and 55 (67.1%)complied. Although the response rate was low among those returning their questionnaire by mail, since their BSQ responses did not differ from the remainder, the complete sample of 331 questionnaires was considered together. 3. Occupational therapy students. The questionnaire was administered to 132 female occupational therapy students, the total number in two training classes, of whom 119 (90.27) returned it satisfactorily completed. 4. Female university undergraduate students. There were 85 female university undergraduate students who were approached and asked to complete the questionnaire. All agreed. In addition to completing the 51-item questionnaire, the 3 nonpatient samples also completed a background information sheet that included questions about their demographic characteristics, weight and eating history, and the importance the subject placed on being slim and on her attitude towards becoming fat. The patients with bulimia nervosa and the occupational therapy students also completed the Eating Attitudes Test or EAT (Garner & Garfinkel, 1979). Considerable additional information was obtained on the patients, including their responses to the Eating Disorder Inventory. The age and weight distributions of the four samples are shown in Table 1. Cooper et al. 488 Table 1. Age and current weight (% matched population mean weight; Geigy Pharmaceuticals, 1962) of the four samples of women. Bulimia Nervosa Patients (n = 38) Age (years) Weight (% mpmw) Undergraduate Students (n = 85) Occupational Therapy Students (n = 119) Family Planning Clinic Attenders (n = 331) Mean SD Mean SD Mean SD Mean SD 22.2 102.8 4.1 13.9 20.0 99.8 1.1 10.8 21.3 98.9 3.2 8.9 23.8 97.7 6.3 11.6 Item Elimination Since a brief questionnaire was considered desirable, a number of items were eliminated. First, using a one to six scoring method (“never” = 1, ”always” = 6) all 51 items were intercorrelated (Pearson’s T ) separately for the 38 patients and for the 535 other women. Items correlating at 0.60 or above for both samples were examined. In six cases, where the content of the questions was considered to be closely related, one of the items was eliminated. Second, the patients and the nonpatients were compared on each item using Student’s ftest. There were six items eliminated because the difference between the two groups failed to reach the 0.001 level of significance. Finally, a further five items were eliminated because they fell below an arbitrary rarity threshold: fewer than 25% of patients and fewer than 5% of nonpatients rated them as occurring at least “often” in the past 4 weeks. The final set of 34 questions was termed the Body Shape Questionnaire, or the BSQ (Appendix). Questionnaire Validation For each subject a total BSQ score was derived based on the one to six scoring system. Figure 1 shows the BSQ distributions for the patients and the nonpatients. It is apparent that the BSQ scores of the patients were significantly higher than those of the nonpatients (t = 11.7, df = 571, p < .OOO). Clearly, the fact that the BSQ scores of patients and nonpatients differ markedly does not in itself constitute validation since items were, in part, chosen by their power to differentiate these two groups. To test for concurrent validity, the BSQ was correlated with the Body Dissatisfaction subscale of the ED1 and with the total EAT score among the patients with bulimia nervosa; and with the EAT total score among the occupational therapy students. The results are shown in Table 2. Among patients the BSQ correlated moderately highly with the score on the EAT and very highly with the ED1 Body Dissatisfaction score. Among the occupational therapy students, the BSQ correlated very highly with the score on the EAT. For a second assessment of validity, two groups were derived from the nonpatient sample. First, a group of women concerned about weight and shape were identified as those who rated slimness as “moderately” or ”extremely” important, and their fear of fatness as “moderate” or “marked,” and who were currently dieting to lose weight; 95 women fulfilled these criteria. Second, a group of women unconcerned about weight and shape were identified as those Body Shape Questionnaire 489 Community 101 S a m p l e Bulimia N e r v o s a Patients 8% 6- 42- 36 BSQ Score 187 Figure 1. Distribution of BSQ scores for patients with bulimia nervosa (Mean = 136.9, SD = 22.5) and women in the community (Mean = 81.5, SD = 28.4). who rated slimness as "not at all" or only "slightly" important and their fear of fatness as "not at all" or only "slight" and who were not currently dieting; 79 women fulfilled these criteria. The mean BSQ score of the "concerned" group was 109.0 (SD = 21.2); and the mean for the unconcerned group was 55.9 (SD = 14.4). These scores are significantly different (t = 19.6, df = 172, p < .000). For the final assessment of validity, two further groups were derived from the community samples. The first group comprised individuals who fulfilled self-report diagnostic criteria for bulimia nervosa. These criteria were the current occurrence of bulimic episodes (defined as episodes of excessive uncontrolled overeating) at least once fortnightly; the current occurrence of compensatory vomiting or laxative use; and a fear of becoming fat rated as "marked," the most extreme point on the scale provided; 10 subjects fulfilled these criteria and were classed as "probable cases" of bulimia nervosa. The BSQ scores of these 10 subjects were compared with those of the 316 women who were classified as "definite non-cases" (ie., they did not binge, vomit, or Table 2. Correlations (Pearson's r) between the BSQ and the EAT total score and the Body Dissatisfaction (BD) subscale of the EDI. Bulimia Nervosa Patients (n = 38) Occupational Therapy Students (n *p < .02. "'p < .001. = 119) BSQ vs. EAT BSQ vs. BD 0.35' 0.66'' 0.61'' - Cooper et al. 490 use purgatives). This comparison is shown in Table 3. It can be seen that the two groups differed markedly on the BSQ. It can also be seen from the table that the mean BSQ score for the 10 “probable cases” of bulimia nervosa was not significantly different from that of the 38 patients with bulimia nervosa mentioned earlier. DISCUSSION The Body Shape Questionnaire is a self-report measure of concerns about body shape, in particular the phenomenal experience of “feeling fat.” Items were empirically derived by interviewing both patients with eating disorders and other women. It is simple to fill in and can be completed in about 10 minutes. Significant correlations between the BSQ and the total score on the EAT and the Body Dissatisfaction subscale of the ED1 establishes its concurrent validity. Its discriminant validity has also been shown to be satisfactory. Among a community sample of women, those who independently declared themselves as concerned about weight and shape had significantly higher BSQ scores than those who were unconcerned about such matters. Similarly, community “cases” of bulimia nervosa were found to have significantly higher BSQ scores than ”non-cases.” There was a certain amount of overlap between the BSQ scores of patients with bulimia nervosa and women in the community (as shown in Fig. 1).However, this is to be expected given that the BSQ measures a psychological dimension that is known to vary considerably in intensity both within patient populations and within community samples. As such, the BSQ should be regarded as providing a measure of the extent of psychopathology rather than a means of case detection. The significance of concerns about body shape in the development and maintainence of anorexia nervosa and bulimia nervosa is unclear. It is also unclear how this aspect of these disorders relates to other features of their specific psychopathology, such as body size overestimation; or how it relates to aspects of their general psychopathology, such as depression. It is also not known whether concerns about body shape relate to response to treatment. The BSQ provides a means of investigating these issues. Table 3. BSQ scores of ”probable cases” of bulimia nervosa compared with BSQ scores of ”probable non-cases” of bulimia nervosa. Patients with Bulimia Nervosa (n = 38) ”Probable Cases“ of Bulimia Nervosa (n = 10) “Definite Non-cases“ of Bulimia Nervosa (n = 316) “Probable Cases” vs. ”Definite Non-cases” “Probable Cases” vs . Patients with Bulimia Nervosa Mean SD Mean SD Mean SD (t) (4 136.9 22.5 129.3 17.0 71.9 23.6 7.62* 1.00 ‘ p < ,000. Body Shape Questionnaire 491 We are grateful to the Cambridge Family Planning Service and Dorset House School of Occupational Therapy in Oxford for their help with this study. The Cambridge patient sample was collected in the course of conducting a treatment study funded by the East Anghan Regional Health Authority, and the Oxford patient sample was collected in the course of a treatment study funded by the Wellcome Trust. Melanie Taylor was supported by a Research Studentship from the Science and Engineering Research Council. APPENDIX BSQ We should like to know how you have been feeling about your appearance over the PAST FOUR WEEKS. Please read each question and circle the appropriate number to the right. Please answer all the questions. OVER THE PAST FOUR WEEKS: Very Never Rarely Sometimes Often Often Always 1. Has feeling bored made you brood about your shape?. . . . . 1 3 4 5 2 6 2. Have you been so womed about your shape that you have been feeling that you ought to 2 diet? . . . . . . . . . . . . . . 1 3 4 5 6 3. Have you thought that youi thighs, hips or bottom are too large for the rest of you?. . . . . 1 2 3 4 5 6 4. Have you been afraid that you might become fat (or fatter)? . . . 1 4 6 2 3 5 5. Have you womed about your flesh not being firm enough? . . . 1 2 3 4 5 6 6. Has feeling full (e.g., after eating a large meal) made you feel fat? . . . . . . . . . . . . . . 1 2 4 5 3 6 7. Have you felt so bad about your shape that you have cried?. . . . 1 2 3 5 6 4 8. Have you avoided running because your flesh might wobble? . . . . . . . . . . . . 1 2 4 5 3 6 9. Has being with thin women made you feel self-conscious about your 4 2 5 shape? . . . . . . . . . . . . . 1 6 3 10. Have you worried about your thighs spreading out when sitting 2 4 5 down? . . . . . . . . . . . . . 1 3 6 11. Has eating even a small amount of food made you feel fat? . . . . 1 2 3 4 5 6 12. Have you noticed the shape of other women and felt that your own shape compared 2 3 4 5 6 unfavourably?. . . . . . . . . . 1 Cooper et al. 492 very Never Rarely Sometimes Often Often Always 13. Has thinking about youz shape interfered with your ability to concentrate (e.g., while watching television, reading, listening to conversations)? . . . . . . . . . 14. Has being naked, such as when taking a bath, made you feel fat? . . . . . . . . . . . . . . 15. Have you avoided wearing clothes which make you particularly aware of the shape of your body? . . . . . . . . . . . . . . 16. Have you imagined cutting off fleshy areas of your body? . . . . 17. Has eating sweets, cakes, or other high calorie food made you feel fat? . . . . . . . . . . . . . . 18. Have you not gone out to social occasions (e.g., parties) because you have felt bad about your shape? . . . . . . . . . . . . . 19. Have you felt excessively large and rounded?. . . . . . . . . . 20. Have you felt ashamed of your body? . . . . . . . . . . . . . 21. Has worry about your shape made you diet? . . . . . . . . . 22. Have you felt happiest about your shape when your stomach has been empty (e.g., in the morning)? . . . . . . . . . . . 23. Have you thought that you are the shape you are because you lack self-control? . . . . . . . . 24. Have you worried about other people seeing rolls of flesh around your waist or stomach? . . . . . 25. Have you felt that it is not fair that other women are thinner than you?. . . . . . . . . . . . 26. Have you vomited in order to feel thinner? . . . . . . . . . . . . 27. When in company have you worried about taking up too much room (e.g., sitting on a sofa or a bus seat)?. . . . . . . . . . . . 28. Have you womed about your flesh being dimply? . . . . . . . 29. Has seeing your reflection (e.g., in a mirror or shop window) made you feel bad about your shape? . . . . . . . . . . . . . 1 2 3 4 5 6 1 2 3 4 5 6 1 2 3 4 5 6 1 2 3 4 5 6 1 2 3 4 5 6 1 2 3 4 5 6 1 2 3 4 5 6 1 2 3 4 5 6 1 2 3 4 5 6 1 2 3 4 5 6 1 2 3 4 5 6 1 2 3 4 5 6 1 2 3 4 5 6 1 2 3 4 5 6 1 2 3 4 5 6 1 2 3 4 5 6 1 2 3 4 5 6 Body Shape Questionnaire 493 Very Never Rarely Sometimes Often Often Always 30. Have you pinched areas of your body to see how much fat there is?. . . . . . . . . . . . . . . 31. Have you avoided situations where people could see your body (e.g., communal changing rooms or swimmingbaths)? . . . . . . 32. Have you taken laxatives in order to feel thinner? . . . . . . . . . 33. Have you been particularly selfconscious about your shape when in the company of other people?. . . . . . . . . . . . . 34. Has worry about your shape made you feel you ought to exercise? . . . . . . . . . . . . 1 2 3 4 5 6 1 2 3 4 5 6 1 2 3 4 5 6 1 2 3 4 5 6 1 2 3 4 5 6 REFERENCES American Psychiatric Association (1980). Diagnostic and Statistical Manual of Mental Disorders (3rd ed.). Washington, D C American Psychiatric Association. American Psychiatric Association (1985). DSM-111-R in Development. Washington, D.C American Psychiatric Association. Berscheid, E., Walster, E., & Bohmstedt, G. (1972). Body Image: A Psychology Today questionnaire. Psychology Today, July 57-65. Bruch, H. (1962). Perceptual and conceptual disturbances in anorexia nervosa. Psychosomatic Medicine, 24, 187-194. Bruch, H. (1973). Eating Disorders: Obesity, Anorexia N m s a and the Person Within. London: Routledge and Kegan Paul. Cooper, P. J., & Fairbum, C. G. (1983). Binge-eating and self-induced vomiting in the community: A preliminary study. British Journal of Psychiatry, 142, 139-144. Cooper, Z., & Fairburn, C. G. (1987). The Eating Disorder Examination: A semi-structured interview for the assessment of the specific psychopathology of eating disorders. lnternational Journal of Eating Disorders, 6, 1-8. Dwyer, J. T., Feldman, J. J., & Mayer, J. (1967). Adolescent dieters: Who are they? Physical characteristics, attitudes and dieting practices of adolescent girls. The American Journal of Clinicat Nutrition, 20, 1045-1056. Fairbum, C. G., & Cooper, P. J. (1984). The clinical features of bulimia nervosa. British Journal of Psychiatry, 144,23%246. Fisher, S . (1970). Body Experience in Fantasy and Behaviour. New York: Appleton-Century-Crofts. Gamer, D. M., & Garfinkel, P. E. (1979). The Eating Attitudes Test: An index of the symptoms of anorexia nerwosa. PsychologiCnl Medicine, 9, 273-279. Gamer, D. M., & Garfinkel, P. E. (1981). Body image in anorexia nervosa: Measurement, theory and clinical implications. International Journal of Psychiatry in Medicine, 11, 263-284. Gamer, D. M., Olmstead, M. P., & Polivy, J. (1983). Development and validation of a multidimensional Eating Disorder Inventory for anorexia nervosa and bulimia. International Journal of Eating Disorders, 2, 15-34. Geigy Pharmaceuticals. (1962). Average weights of adults (Society of Actuaries: Build and Blood Pressure Study, Chicago, 1959), 623, Documenta Geigy. Scientific Tables. Manchester: Geigy Pharmaceuticals. Hall, A., Leibrich, J., & Walkey, F. H. (1983). The development of a Food, Fitness and Looks Questionnaire and its use in a study of "weight pathology" in 204 nonpatient families. In Darby, P. L., Garfinkel, P. E., Gamer, D . M., & Coscina, D. V. (Eds.), Anorexia Nervosa: Recent Dmelopments in Research. New York Alan R. Liss. Huenemann, R. L., Shapiro, L. R., Hampton, M. C., & Mitchell, B. W. (3-966). A longitudinal study of gross body composition and body conformation and their association with food and activity in a teen-age population. American Journal of Clinical Nutrition, 18, 325-338. 494 Cooper et al. Marsella, A. J., Shizuru, L., Brennan, J., & Kameoka, V. (1981). Depression and body image satisfaction. Journal of Cross-Cultural Psychology, 12, 360-371. Nylander, I. (1971). The feeling of being fat and dieting in a school population. Acta Socio-Medica Scandinavia, 1, 17-26. Russell, G . F. M. (1979). Bulimia nervosa: An ominous variant of anorexia nervosa. Psychological Medicine, 9, 429-448. Secord, P. F., & Jourard, S. M. (1953). The appraisal of body-cathexis: Body-cathexis and the self. Iournal of Consulting Psychology, 17, 33-37. Wardle, J., & Beales, S. (1986). Restraint, body image and food attitudes in children from 12-18 years. Appetite, 7, 209-217. Winstead, B. A., & Cash, T. F. (1984). Body-Self Relations Questionnaire, personal communication.