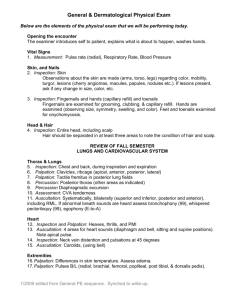
Health Assessment and Physical Examination STUDENT LEARNING OUTCOMES (SLOS): The student learner will be able to: 1. Demonstrate understanding of theoretical foundations of nursing practice. 3. Understand the components of the nursing process and their relevance in providing individualized client care across the lifespan. 5. Provide effective client/family education in relation to health promotion & maintenance. 6. Recognize potential safety risks and intervene appropriately to maintain safety for clients of all ages. 8. Utilize therapeutic communication in communicating with clients across the lifespan. 12. Demonstrate an understanding of technique, risk factors, complications, and effectiveness of basic nursing skills. PURPOSES OF THE PHYSICAL EXAMINATION • Establish the patient’s current condition • Supplement, confirm, or refute subjective data obtained. • Identify and confirm diagnoses. • Make clinical decisions about a patient's changing health status and management. • Evaluating the effectiveness of nursing intervention CULTURAL SENSITIVITY • Respect cultural differences • Be culturally aware and avoid stereotyping LEVELS OF PHYSICAL ASSESSMENT • Comprehensive health assessment • Focused assessment • Initial head-to-toe shift assessment WHEN PHYSICAL ASSESSMENT IS PERFORMED • On admission • At the beginning of each shift • When patient condition changes • When evaluating the effectiveness of nursing care • Any time things do not feel right ASSESSMENT TECHNIQUES • Interviewing (subjective data) • Inspection or observation • Palpation • Percussion • Auscultation PREPARATION FOR EXAMINATION • Infection control • Environment • Equipment • Physical preparation of patient • Positioning • Psychological preparation of patient • Assessment of age groups ORGANIZATION OF THE EXAMINATION • Assessment of each body system • Systematic and organized • Head-to-toe approach • Compare sides for symmetry • Assess body systems most at risk for being abnormal • Offer rest periods as needed • Perform painful procedures at the end • Be specific when recording assessments • Record quick notes during the examination; complete larger notes at the end of the examination INSPECTION • Use adequate lighting. • Use direct lighting to inspect body cavities. • Inspect each area for size, shape, color, symmetry, position, and abnormality. • Position and expose body parts as needed so all surfaces can be viewed but privacy can be maintained. • When possible, check for side-to-side symmetry. • Validate findings with the patient. PALPATION • Uses touch to gather information. • Use different parts of hands to detect different characteristics. • Hands should be warm, fingernails short. • Start with light palpation; end with deep palpation. PALPATION PERCUSSION • Tap skin with fingertips to vibrate underlying tissues and organs • Sound determines location, size, and density of structures • The denser the tissue, the quieter is the sound AUSCULTATION • Requires • Sound characteristics • Good hearing • Frequency • A good stethoscope • Loudness • Knowledge • Quality • Concentration and practice • Duration GENERAL SURVEY • General appearance and behavior • Gender, race, age, signs of distress, body type, posture, gait, movements, hygiene, dress, mood, speech, signs of abuse, substance abuse • Vital signs • Height and weight SKIN, HAIR, AND NAILS • Hair and scalp • Hair: color, distribution, quantity, thickness, texture, and lubrication • Scalp: lesions, lumps, dandruff, lice • Nails • Inspection and palpation • Clubbing HEAD • Inspection and palpation • Inspect the patient’s head, noting the position, size, shape, and contour. • Examine the size, shape, and contour of the skull. • Palpate the temporomandibular joint (TMJ) space bilaterally. EYES • Visual acuity • Extraocular movements • Nystagmus • Visual fields • External eye structures • Internal eye structures EARS • Auricles • Ear canals and eardrums • Size • Color • Shape • Discharge • Symmetry • Scaling • Landmarks • Lesions • Position • Foreign bodies • Color • Cerumen • Discharge • Hearing acuity NOSE AND SINUSES • Nose • Excoriation • Polyps • Sinuses • Palpation MOUTH AND PHARYNX • Lips • Buccal mucosa • Gums • Teeth • Tongue • Floor of mouth • Palate • Pharynx NECK • Neck muscles • Anterior triangle • Posterior triangle • Lymph nodes • Thyroid gland • Carotid and jugular vein • Trachea LYMPH NODES NEUROLOGICAL SYSTEM • Full assessment requires time and attention to detail. • Many variables must be considered during evaluation: level of consciousness (LOC), physical status, chief complaint. • Collect all equipment before beginning. • Mental and emotional status • Mini-Mental State Examination (MMSE) • Cultural considerations • Delirium NEUROLOGICAL SYSTEM • Level of consciousness • Glasgow Coma Scale • Behavior and appearance • Nonverbal and verbal • Language • Aphasia • Sensory (receptive) • Motor (expressive) NEUROLOGICAL SYSTEM • Intellectual function • Memory • Knowledge • Abstract thinking • Association • Judgment • Cranial nerve function NEUROLOGICAL SYSTEM • PERLA • Motor function • Coordination • Balance • Romberg’s test • Another test involves asking the patient to walk a straight line by placing the heel of one foot directly in front of the toes of the other foot. NEUROLOGICAL SYSTEM • Grade reflexes: • 0: no response • 1+: sluggish/diminished • 2+: active/expected response • 3+: more brisk than expected, slightly hyperactive • 4+: brisk and hyperactive with intermittent or transient clonus NEUROLOGICAL SYSTEM • Reflexes • Position. • Tap tendon briskly. • Compare corresponding sides. THORAX AND LUNGS • Examination • Inspection and palpation • Diagnostic equipment: x-ray films, magnetic resonance imaging (MRI), computed tomography (CT) scans • Auscultation of lung lobes in relation to anatomical landmarks THORAX AND LUNGS • Posterior thorax THORAX AND LUNGS • Tactile fremitus • Created by vocal cords • Transmitted through lungs to chest wall • Palpation THORAX AND LUNGS • Auscultation • Normal breath sounds • Abnormal or adventitious sounds • Crackles • Rhonchi • Wheezes • Pleural friction rub THORAX AND LUNGS • Lateral thorax • Vesicular sounds • Anterior thorax • Observe accessory muscles. • Palpate muscles and skeleton. • Assess tactile fremitus. • Compare right and left sides. • Auscultate for bronchial sounds. HEART • Compare assessment of heart functions with vascular findings. • Assess point of maximal impulse (PMI). • Locate anatomical landmarks. HEART • Heart sounds • S1 • S2 • S3 • S4 HEART • Inspection and palpation • Patient must be relaxed and comfortable • Inspect and palpate simultaneously • PMI HEART • Auscultation • Normal heart sounds • Dysrhythmia • Extra heart sounds • Murmurs • Grade • Pitch • Quality VASCULAR SYSTEM • Blood pressure • Readings tend to be higher in the right arm. • Always record the higher reading. • Carotid arteries • Reflect heart function better than peripheral arteries • Commonly auscultated VASCULAR SYSTEM • Carotid bruit • Narrowed blood vessel creates turbulence, causes blowing/swishing sound • Pronounced “brew-ee” VASCULAR SYSTEM • Jugular veins • Most accessible • Right internal jugular vein follows more direct path to right atrium. • Note distention. • Assess pressure. VASCULAR SYSTEM • Peripheral arteries • Assess each peripheral artery for elasticity of the vessel wall, strength, and equality. • Pulses • 0: Absent, not palpable • 1: Pulse diminished, barely palpable • 2: Expected • 3: Full, increased • 4: Bounding, aneurysmal VASCULAR SYSTEM • Peripheral arteries • Upper extremities • Radial pulse: thumb side of wrist • Ulnar pulse: little finger side of wrist • Brachial pulse: inside of elbow VASCULAR SYSTEM • Peripheral arteries • Lower extremities • • • • Femoral pulse Popliteal pulse Dorsalis pedis pulse Posterior tibial pulse VASCULAR SYSTEM • Peripheral arteries • Ultrasound stethoscopes • Tissue perfusion • Peripheral veins • Varicosities • Peripheral edema • Pitting edema • Phlebitis LYMPHATIC SYSTEM • Lymphatic system • Lower extremities • Assess during examination of vascular system or genital examination • Upper extremities • Palpate the epitrochlear nodes, located on the medial aspect of the arms • Assess proximal portion during breast examination BREASTS • Assess in both male and female patients. • Male breast: small amount breast of glandular tissue • Female breast: majority of breast is glandular tissue • Breast cancer is second to lung cancer as the leading cause of death in women with cancer. • Early detection is the key to cure. FEMALE BREASTS • Inspection • Size and symmetry • Common for one breast to be smaller • Contour or shape • Color • Nipple and areola • Assess for symmetry while patient raises arms above head FEMALE BREASTS • Palpation • Edge of pectoralis major muscle along anterior axillary line • Chest wall in the midaxillary area • Upper part of humerus • Anterior edge of the latissimus dorsi along posterior axillary line FEMALE BREASTS • Palpation • Lying down with the arm abducted makes the area more accessible • Place pillow or towel under the patient’s shoulder blade to further position breast tissue • Palpate tail of Spence FEMALE BREASTS • Palpation • Use systematic approach: vertical, circular, or radial/wedge technique MALE BREASTS • Inspect the nipple and areola for nodules, edema, and ulceration • Breast enlargement • An enlarged male breast results from obesity or glandular enlargement • Breast enlargement in young males results from steroid use • Men at high risk may be scheduled by their health care provider for routine mammograms ABDOMEN • Complex assessment because of organs located in abdominal cavity • Begin with inspection and follow with auscultation ABDOMEN • Inspection • Skin, umbilicus, contour and symmetry, enlarged organs or masses, movements or pulsations • Auscultation • Bowel motility • Peristalsis • Borborygmi • Vascular sounds • Bruits • Kidney tenderness ABDOMEN • Palpation • Performed last • Detects tenderness, distention, or masses • May be light or deep, as appropriate • Aortic pulsation FEMALE GENITALIA AND REPRODUCTIVE TRACT • Assessment includes both internal and external organs. • Understand cultural sensitivity. • Identify changes across the life span. • Use inspection and palpation. • Preparation of the patient • External genitalia • Speculum examination of internal genitalia MALE GENITALIA • Assesses the integrity of the external genitalia, inguinal ring, and canal. • Have patient void first. • Obtain a thorough history before the examination. • Sexual maturity (adolescence) • Penis • Scrotum • Inguinal ring and canal • Male testicular self-examination RECTUM AND ANUS • Perform after genital examination. • Explain all steps to the patient. • Provide privacy. • Use inspection and digital palpation. MUSCULOSKELETAL SYSTEM • General inspection: • Gait • Posture • Standing • Sitting MUSCULOSKELETAL SYSTEM • Assess for lordosis, kyphosis, or scoliosis. MUSCULOSKELETAL SYSTEM • Palpation • Range of joint motion MUSCULOSKELETAL SYSTEM • Range of motion • Muscle tone and strength • Hypertonicity • Hypotonicity • Atrophy SKIN, HAIR, AND NAILS • Skin • Color • Moisture • Temperature • Texture • Turgor • Vascularity • Edema • Lesions SKIN TURGOR PITTING EDEMA AFTER THE EXAMINATION • Record findings. • Give the patient time to dress; assist if needed. • If findings are serious, consult health care provider before informing the patient. • Delegate cleaning of examination area. • Record complete assessment; review for accuracy and thoroughness. • Communicate significant findings. KEY POINTS • Purposes of physical assessment include establishing a patient’s current condition, establishing a baseline against which future changes may be measured, identifying problems the patient may have or may have the potential to develop, evaluating the effectiveness of nursing interventions, monitoring for changes in body function, and detecting specific body systems that need further assessment or testing. • Techniques of assessment include interviewing, inspection, palpation, percussion, auscultation, percussion, and olfaction. • Assessment is performed in a head-to-toe sequence, beginning with the head and neck, progressing to the chest and abdomen, and then to the four extremities. • Components to be assessed during an initial shift assessment include the following systems: neurological, cardiovascular, respiratory, integumentary, gastrointestinal, genitourinary, and musculoskeletal. Also included in an initial shift assessment are vital signs, including pain and SpO2; appearance; speech; safety risk factors; tubes and equipment; comfort or complaints; and a needs assessment. KEY POINTS • A comprehensive health assessment involves an in-depth assessment of the whole person, including the physical, mental, emotional, cultural, and spiritual aspects of the patient’s health. • You will begin your assessment with subjective data by interviewing and asking questions. The other five techniques involve objective data collected during your assessment. They include inspection or observation, palpation, percussion, auscultation, and olfaction. Percussion is typically performed by the health-care provider unless indicated for further evaluation. • A focused assessment is less encompassing and involves an examination and an interview regarding a specific body system, such as examining solely the integumentary system or the respiratory system. • An initial head-to-toe shift assessment provides you with a quick overall assessment of the patient’s condition to establish a baseline against which you can compare later assessments. • Ways to foster rapport and communication involve talking with a patient; it is important to establish a trusting, professional relationship. • Various adaptations are necessary when assessing patients of different age groups.