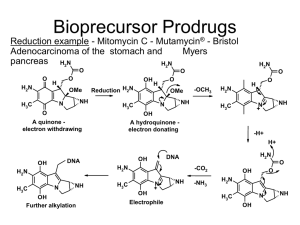
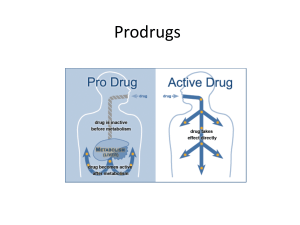
Chapter 9 Prodrugs Zeynep Ates-Alagoz1,2 and Adeboye Adejare2 1 Department of Pharmaceutical Chemistry, Faculty of Pharmacy, Ankara University, Ankara, Turkey, 2Department of Pharmaceutical Sciences, Philadelphia College of Pharmacy, University of the Sciences, Philadelphia, PA, United States 9.1 Introduction The term “prodrug” was first used by Albert (1958) to indicate pharmacologically inactive compound that is broken down in vivo to give the active drug. It could be used instead of the drug to achieve desired physicochemical properties that can increase usefulness and/or decrease associated toxicity (Sriram and Yogeeswari, 2010). Medicinal chemists have used this concept as a tool to solve issues with problematic drugs. In order to exert desired pharmacological actions, prodrugs must undergo chemical or enzymatic biotransformation to the active forms and promoieties within the body (Rautio et al., 2008b) (Fig. 9.1). The promoiety is carefully selected to pass on a desirable property to the drug resulting in prodrug with desired physicochemical properties. The prodrug should be safe and rapidly excreted from the body. It is not necessary for pharmacologic activity (Andurkar, 2007). Prodrugs can exist naturally or they can result from synthetic or semisynthetic processes produced intentionally as part of a rational drug design or unintentionally during drug development (Wu, 2009). Release of the active drug can be controlled depending upon the purpose for which prodrug is designed (Sinkula and Yalkowsky, 1975; Stella et al., 1985). The major goal in prodrug design is to overcome the various physicochemical, pharmaceutical, biopharmaceutical, and pharmacokinetic limitations of parent drug, which otherwise could hinder its clinical use (Stella et al., 2007; Sherwood, 1996; Stella, 2004, 2006; Stella and Nti-Addae, 2007; Oliyai, 1996). For example, prodrugs provide possibilities for overcoming drug-delivery challenges, such as poor aqueous solubility, formulation, insufficient oral absorption, chemical instability, inadequate brain penetration, toxicity, and local irritation. Prodrugs can also improve drug targeting, and the development of a prodrug of an existing drug with improved properties may represent a life-cycle management opportunity (Rautio et al., 2008a). The prodrug concept has found a number of useful applications in drug discovery and development. There are a number of subcategories of prodrugs. The most common category is one in which additional chemical substituents have been attached covalently to the drug molecule. Release of the free drug is then accomplished either enzymatically or chemically (Rautio et al., 2008a). Earlier examples of prodrugs include methanamide (hexamine), aspirin, and prontosil (Fig. 9.2; Stella, 2007). Methanamide was used in 1899 as a urinary tract prodrug that delivers the antibacterial formaldehyde. It is a stable inactive compound at pH greater than 5. However, in acidic environment, the compound disintegrates to form formaldehyde. Aspirin (acetyl salicylic acid) is a common nonsteroidal antiinflammatory drug used for the treatment of pain and arthritis; a less irritating form of sodium salicylate (Stella et al., 2007; Supernaw, 2007). In the body, aspirin is rapidly deacetylated to form salicylic and acetic acids. Aspirin and salicylic acid have been proposed as antiinflammatory agents (Kuehl et al., 2006). Acetic acid can be acted on rapidly by metabolic enzymes, thus, is basically a nontoxic byproduct (Fuchs, 2007). Prontosil is an example of accidental prodrugs. It is the first commercially available antibacterial antibiotic and a prodrug of sulfanilamide. Prontosil is inactive as an antibacterial, but it is turned FIGURE concept. Remington. DOI: https://doi.org/10.1016/B978-0-12-820007-0.00009-X Copyright © 2021 University of the Sciences in Philadelphia. Published by Elsevier Inc. All rights reserved. 9.1 Illustration of prodrug 169 170 SECTION | 3 Pharmaceutical Chemistry FIGURE 9.2 Methanamide (A), prontosil (B), and acetyl salicylic acid (C). in vivo to pharmacologically active sulfanilamide by the enzyme azoreductase. These studies led to discovery of the sulfonamides as antibacterial agents (Andurkar, 2007). There are a number of ways that drugs can be modified. What is necessary is that the parent drug has a functionality that is amenable to modification. Functional groups that are amenable to prodrug design include carboxylic, hydroxyl, amine, phosphate, and carbonyl groups. Modifications of these groups can lead to esters, carbonates, carbamates, amides, phosphates, and oximes. These functional groups lead to prodrugs which can provide drug release triggered by esterases, phosphatases, proteases, hypoxia, pH changes, reducing, oxidizing, and light conditions (Rautio et al., 2008a). There are currently a number of prodrugs in clinical trials. Classification of them can be based on the therapeutic categories, for example, anticancer, antiviral, antibacterial, nonsteroidal antiinflammatory, and cardiovascular; or based on the categories of moiety that attach to the active drug, for example, esters, carbonates and carbamates, amides, and oximes prodrugs (Han and Amidon, 2000; Hu, 2004; Liederer and Borchardt, 2006); or based on the delivery method, for example, oral, topical, or parenteral delivery. This review will start with an overview of the delivery systems, functional groups, and then more into prodrug approaches for anticancer drugs. 9.2 Prodrug approaches based on drug delivery Oral delivery, the most desirable route of administration, is the most difficult to attain as bioavailability by this route is usually least efficient compared to other routes (Lee, 1995). It is very important to be aware of the physicochemical and biological factors that are restraining the oral bioavailability of a drug before starting a prodrug strategy. Aqueous solubility, low permeability, tendency to be an efflux substrate, rapid hepatic metabolism, and biliary excretion are important physicochemical and biological factors that may limit oral delivery (Rautio et al., 2008a). The rationale behind the prodrug strategy for hydrophilic and/or charged compounds is to introduce lipophilicity and mask hydrogen-bonding groups by the addition of another moiety (Beaumont et al., 2003). These prodrugs are often carboxylic acid esters, or phosphonic acid esters, of poorly permeable but aqueous soluble parent drugs (Rautio et al., 2008a). Use of carrier-mediated absorption is one of the prodrug approaches for improving oral drug delivery. This prodrug approach uses transporters that facilitate membrane transport of polar and charged nutrients such as amino acids and peptides. Therefore targeting specific membrane transporters is particularly important when prodrugs are polar or charged. There have been many attempts to improve drug absorption by targeting specific membrane transporters, including amino acid, peptide, and glucose transporters. Among the various membrane transporters, peptide transporters are attractive targets in prodrug design to improve oral drug absorption because of several advantages such as broad substrate specificity and high capacity. They have been extensively studied (Incecayir et al., 2016). When a drug cannot be taken orally due to oral absorption limitations or when immediate action of drug is required, such as in anaphylactic reaction, parenteral drug dosing is the desired route of administration. Most phosphate esters used in parenteral formulations are watersoluble prodrugs of poorly water-soluble parent drugs. Phosphate esters are ionizable and have considerably higher aqueous solubility than the parent compounds, and they are rapidly hydrolyzed by phosphatases yielding the parent drugs (Hemenway and Stella, 2007; Heimbach et al., 2003). The ocular absorption of topically applied drugs is limited by the corneal epithelium barrier, the rapid precorneal drug elimination and systemic absorption from the conjunctival. Prodrugs were introduced to ophthalmology about 35 years ago when ocular absorption of epinephrine was substantially improved by its prodrug (Jarvinen and Jarvinen, 1996). Dipivefrine (Fig. 9.3) is a dipivalic acid ester prodrug of epinephrine which is able to release the parent drug within the eye at a rate that meets therapeutic need. Dipivefrine penetrates cornea 17 times better than epinephrine due to its higher lipophilicity at pH 7.2 (Jarho et al., 1997). Dermal drug delivery has some advantages over more conventional treatments such as delivery of therapeutic level of drug to the application site in a more effective and safer way (Rautio et al., 2000). Thus it has been getting Prodrugs Chapter | 9 171 FIGURE 9.3 In vivo conversion of dipivefrine to epinephrine. increasing popularity. But, most drugs present inappropriate physicochemical properties to efficiently penetrate the skin. Therefore many attempts have been carried out to increase drug permeation through the skin (Bonina et al., 2001). Drugs containing polar functional groups have problems of membrane permeability and biphasic solubility which limit their dermal delivery. The prodrug approach can mask these polar functional groups as esters which then hydrolyze to the parent drug either enzymatically or chemically (Majumdar and Sloan, 2006). Recent studies have shown that prodrug needs to have adequate lipid as well as water solubility to permeate the skin effectively because the skin represents a lipid-aqueous biphasic barrier to permeation due to nature of the stratum corneum. Thus prodrugs should increase not only lipid but also aqueous solubility as need be (Sloan and Wasdo, 2003, 2007). 9.3 Prodrug approaches based on functional groups Amines are highly ionized functional groups under physiological conditions (pH 5 18). However, this functional group is found in many drug molecules (Sloan and Wasdo, 2007; Simplı́cio et al., 2008). Drug molecules that contain basic amine functional groups may actually permeate skin better than expected, and basic amine groups incorporated into a prodrug may enhance its skin permeation (Sloan et al., 1984). Derivatizations of amines can result in reduction in basicity. That could be favorable for improving the rate of diffusion across biological membranes. Physicochemical and structural properties of the promoiety that is incorporated into a drug molecule are important. Hydrophilic promoieties are designed to improve water solubility and lipophilic ones are designed to improve membrane permeability of the parent drugs (Krise and Oliyai, 2007). Ester formation is the most common prodrug design strategy to increase lipophilicity by masking carboxylic acids, phosphates, and other charged groups (Taylor, 1996). Such prodrug is activated by enzymatic (esterase) or chemical hydrolysis (Ettmayer et al., 2004). Ester prodrugs are most often used to enhance oral absorption and thus passive membrane permeability of poorly permeable compounds (Beaumont et al., 2003). Acylation or alkylation of alcohols or phenols could lead to a less polar prodrug, while phosphorylation can lead to a more water-soluble prodrug. Drugs containing hydroxyl groups, including alcohols and phenols, can have a variety of physical/chemical properties that have advantages and disadvantages. Esterification of the hydroxyl group has been one of the preferred prodrug strategies to mask polar groups within a drug molecule and thereby promote membrane permeability. Acyl groups that have been incorporated to form promoieties for the hydroxyl group range from lower alkyl groups to long-chain fatty acids (Dhareshwar and Stella, 2007). Phosphate ester prodrugs present several advantages for the formulation and development of poorly watersoluble compounds. They are chemically stable, need only a hydroxyl moiety, and enhance aqueous solubility to allow oral or parenteral administration. Phosphate ester prodrugs (Fig. 9.4) are readily hydrolyzed by endogenous phosphatases to release the pharmacologically active parent compounds and phosphates (Kearney and Stella, 1993; McComb et al., 1979; Heimbach et al., 2007). Phosphorus is an essential mineral for normal body function and is found as phosphate in the body (Food and Nutrition Board, Institute of Medicine, 1997). Phosphates are extremely important in living cells. Phosphates are FIGURE 9.4 Illustrative in vivo conversion of phosphate ester prodrugs to their active parent compound. 172 SECTION | 3 Pharmaceutical Chemistry FIGURE 9.5 General structure of phosphates, phosphonates, and phosphinates. FIGURE 9.6 Illustration of how phosphorous ester prodrug moiety is cleaved by an enzymatic and/or chemical process to active parent compound. extensively circulated in the body and excreted in the urine and feces and must be replaced in the diet (Food and Nutrition Board, Institute of Medicine, 1997). Phosphates, phosphonates, and phosphinates (Fig. 9.5) are prominently represented pharmacophores in various classes of biological agents. It is generally well recognized that the therapeutic potential of drugs containing a phosphate, phosphonate, or phosphinate group is limited by their inadequate membrane permeation and oral absorption. These groups carry one or two negative charges making them ionic. They do not readily undergo passive diffusion across cell membranes. These compounds exhibit a low volume of distribution and efficient renal clearance because of the ionization (Krise and Stella, 1996; He et al., 2007). To overcome these problems, a variety of promoieties to mask ionizable phosphate, phosphonate, or phosphinate groups have been designed by medicinal chemists. They usually use phosphorus-coupled oxygen to form neutral ester, which will decrease the polarity by increasing the lipophilicity of the compound. Once the ester prodrug gets into the target issues, moiety can be cleaved by an enzymatic and/or chemical process to release free drug to achieve the desired biological effect (He et al., 2007) (Fig. 9.6). This process will be illustrated with several examples, including nucleotides. The monoalkyl/aryl ester analogs of phosphates failed to act as efficient prodrugs for the delivery of nucleosidemonophosphate analogs intracellularly due to high degree of polarity and lack of conversion of the monoalkyl esters in vivo back to the parent nucleoside (Krise and Stella, 1996). Serafinowska et al. have synthesized a series of dialkyl prodrugs of 9-[2-(phosphonomethoxy)ethoxy]adenine (Fig. 9.7) to improve the poor bioavailability. Short-chain FIGURE 9.7 General structure of dialkyl prodrugs of 9-[2-(phosphonomethoxy) ethoxy] adenine. FIGURE 9.8 General structure 1-naphthalenemethylphosphonate. of 3-phthalidyl esters of diesters, being chemically stable, were predominantly detected unchanged in the serum after oral administration (Serafinowska et al., 1995). In order to completely mask the negative charge on phosphorous, a wide variety of tri-ester prodrugs have been synthesized (Jones et al., 1989; McGuigan et al., 1989, 1990, 1991). Generally, simple alkyl tri-esters are too stable to be useful as prodrugs and the resulting phosphorous esters are inactive. However, aryl esters and activated alkyl esters are capable of functioning as nucleotide prodrugs (Jones and Bischofberger, 1995). Dang et al. synthesized a series of 3-phthalidyl esters of 1-naphthalenemethylphosphonate (Fig. 9.8) as a potential Prodrugs Chapter | 9 prodrug approach to improve intracellular delivery of phosphonates. These 3-phthalidyl esters successfully delivered 1-naphthalenemethylphosphonate intracellularly in rat hepatocytes and were further optimized to give higher plasma stability. Advantages possessed by this prodrug approach over the traditional acyloxymethyl prodrug approach include that these prodrugs do not generate formaldehyde and have improved plasma stability (Dang et al., 1999). Nucleoside and nucleotide analogs have great therapeutic potential for the treatment of viral diseases and cancer (Robins, 1984). Nucleosidic drugs depend on kinasemediated activation to create the phosphorylated nucleotide and exhibit biological activity. Monophosphate formation is the first step in phosphorylation and known to be highly specific and often causes the development of resistance (Johnson et al., 1988). In contrast to nucleosides, nucleotides are phosphorylated species and do not require that first step in their metabolic activation (Jones and Bischofberger, 1995). Nucleotides, however, have some disadvantages over nucleosides. They go into cells very poorly (Posternak, 1974) and show usually low or no activity in vitro, because of their charge. Another disadvantage especially for nucleoside phosphate analogs is their low stability in biological media, due to rapid dephosphorylation (Krise and Stella, 1996; LePage et al., 1975; Cohen and Plunkett, 1975). Nucleotide prodrugs can potentially overcome these difficulties, and they were successfully used to increase oral absorption of nucleotides in vivo by masking the negative charge (s) on the phosphorous with suitable functionalities. These prodrugs can be converted chemically or biologically to the parent nucleotide. They have been utilized to increase intracellular delivery and alter pharmacokinetic properties. They have also been used for tissue-specific delivery of the nucleotides in vivo resulting in altered selectivity and reduced toxicity (Jones and Bischofberger, 1995). 9.4 Prodrug approaches for anticancer drugs Cancer is still a major cause of death in the world; thus the urge to discover novel and effective therapeutic FIGURE 9.9 In vivo conversion of miproxifene phosphate to miproxifene. 173 agents continues. Only 20% of the cancer patients can benefit from surgical- or radiation-based therapies, and that is why chemotherapy is the primary choice for cancer treatment (DeSantis et al., 2014). However, current therapeutics may suffer from low bioavailability, high toxicity, and drug resistance (Perkins et al., 2003). Prodrugs provide possibilities for overcoming drugdelivery challenges, such as poor aqueous solubility, formulation, insufficient oral absorption, chemical instability, inadequate brain penetration, toxicity, and local irritation (Rautio et al., 2008a). Miproxifene phosphate (TAT-59, Fig. 9.9) is a triphenylethylene analog of tamoxifen. After oral administration, TAT-59 is immediately metabolized in the digestive tract to its active form DP-TAT-59 which has a high affinity for estrogen receptors. DP-TAT-59 suppresses the proliferation of human breast carcinoma cells even at concentrations lower than 1/30th of the level required for tamoxifen exhibiting this action (Toko et al., 1995; Shibata et al., 2000). Unlike other phosphate esters, TAT-59 exhibits unusually low water solubility. The prodrug was successful because its solubility and dissolution rate were significantly higher than those of the parent drug (Heimbach et al., 2007). Estramustine phosphate (Fig. 9.10) is a phosphate ester prodrug of the practically insoluble, nonionizable parent drug estramustine. It is a cytotoxic drug that has been used in the treatment of advanced prostatic carcinoma (Heimbach et al., 2007). A phosphate group was added at the 17-β position of the steroid D ring to increase the water solubility of the compound. Estramustine phosphate sodium is immediately dephosphorylated in the gastrointestinal tract, producing the main cytostatic metabolite estramustine (Nicholson et al., 2002). Etoposide (Fig. 9.11), a semisynthetic derivative of podophyllotoxin, is an important chemotherapeutic agent (CA) in the treatment of select patients with germ cell tumors, lymphomas, and small cell lung cancer (Greco et al., 1991; Greco and Hainsworth, 1995). The clinical use of etoposide is adversely affected by its very poor water solubility and is formulated in polysorbate-80, polyethylene glycol, and alcohol. Because of its poor solubility, even 174 SECTION | 3 Pharmaceutical Chemistry FIGURE 9.10 In vivo conversion of estramustine phosphate to estramustine. FIGURE 9.11 In vivo conversion of etoposide phosphate to etoposide. with this formulation, etoposide must be diluted to avoid precipitation. This dilution may cause fluid overload problems in patients receiving high doses of this agent and requires prolonged nursing supervision, higher expenses, and patient inconvenience and discomfort (Saulnier et al., 1994). In addition, hypersensitivity and hypotensive reactions have been reported. Etoposide phosphate, a water-soluble prodrug of etoposide, has several potential advantages, including easier and more rapid administration, avoidance of large fluid loads, and elimination of hypersensitivity reactions and other problems related to the solubilizer (Saulnier et al., 1994). The anticancer drug CPT-11 (irinotecan, 7-ethyl-10[4-(1-piperidino)-1-piperidino] carbonyloxycamptothecin, Fig. 9.12), is a prodrug that is activated by esterases to yield SN-38 (7-ethyl-10-hydroxycamptothecin), a potent topoisomerase I poison (Hatfield et al., 2011; Hyatt et al., 2005). Irinotecan is a semisynthetic water-soluble camptothecin produced in an attempt to reduce the toxicity and improve the therapeutic efficacy of the drug (Escoriaza et al., 2000). Irinotecan shows encouraging activity in the treatment of several types of tumors such as nonsmall cell lung cancer, colorectal adenocarcinoma, and cancer of the cervix. SN-38 has been shown to be 1001000 times more potent than CPT-11 in in vitro and in vivo tests of cytotoxicity (Rivory et al., 1996). Irinotecan’s clinical utility is limited due to the drawbacks such as poor bioconversion to the active drug SN-38, severe toxicities, and the function of SN-38 as a substrate of the breast cancer resistance protein efflux pump (Ohwada et al., 2009). Ohwada et al. reported the syntheses and biological activities of water-soluble prodrugs of hexacyclic camptothecin analog, CH0793076 (Fig. 9.13). It exhibits pH-dependent conversion to parent compound and showed better anticancer activity than irinotecan. Among the prodrugs synthesized, TP300 is highly water-soluble and rapidly generates CH0793076 at physiological pH in vitro. TP300 showed a broader antitumor spectrum and more potent antitumor activity than irinotecan in various human cancer xenograft models (Ohwada et al., 2009). 5-Fluorouracil (5-FU, Fig. 9.14) is an antimetabolite with a broad spectrum of activity against solid tumors (Calabresi and Parks, 1985). However, its administration is accompanied by severe toxic side effects and delivery problems. In order to solve these problems, low- and Prodrugs Chapter | 9 175 FIGURE 9.12 In vivo conversion of irinotecan to SN-38. FIGURE 9.13 In vivo conversion of TP300 to CH0793076. FIGURE 9.14 In vivo conversion of capecitabine to 5-fluorouracil. macromolecular prodrugs of 5-FU have been developed. In most instances the antitumoral activity of the polymeric prodrugs is due to the free 5-FU released by a nonspecific chemical hydrolysis of the ester (Akashi and Takemoto, 1990; Ouchi et al., 1990b), carbamate (Ouchi et al., 1992), carbamoyl (Ouchi et al., 1990a,b, 1992), or amide (Ouchi et al., 1990b, 1992) bonds between the Nl-pyrimidine atom of the drug and the polymer backbone or an alkylene type spacer (Nichifor et al., 1996). Capecitabine is a commercially available prodrug of 5-FU and it was first approved in the United States in 1998 for the treatment of metastatic breast cancer. This prodrug was designed to improve oral bioavailability and selectivity of 5-FU to tumor cells. Capecitabine passes intact through the intestinal mucosa and selectively delivers 5-FU to tumor tissue by enzymatic conversion (Shimma, 2007). To enhance therapeutic index, and reduce the toxicity issues of cytotoxic chemotherapy, targeted prodrug approaches are new directions in the treatment of cancer (Gonzalez-Mendez et al., 2019). These directions are 176 SECTION | 3 Pharmaceutical Chemistry FIGURE 9.15 Enzymatic activation of IQ-FdUrd under hypoxic conditions. IQ-FdUrd, 5-Fluorodeoxyuridine prodrug bearing an indolequinone unit. FIGURE 9.16 Mechanism of releasing Dox from prodrug induced by pH. Dox, Doxorubicin. receiving big attention for adjustment of physical properties of drugs such as the charges, lipophilicity, or reactivity by alteration of leads to selective delivery of the drugs to cancer cells and tissues. Therefore prodrugs concentrate at their target cells and show their activities there in a selective way (Jiho et al., 2019). Significant strategies to accomplish the local activation of prodrugs include enzymatic activation of prodrugs in hypoxic cells (Sriram and Yogeeswari, 2010, Han and Amidon, 2000), the use of pH-sensitive conjugates (Hong et al., 2019), antibodydrug conjugates (Cho et al., 2019), hydrophobic drug self-delivery systems (Xue et al., 2019), and integration of prodrugs with nanotechnology-based drug delivery. Jiho et al. recognized an enzymatic one-electron reduction as a useful reaction that can be applied in the design of tumor hypoxia-targeting drugs. The enzymatic reaction of 5-fluorodeoxyuridine (FdUrd) (Fig. 9.15) prodrug bearing an indolequinone unit (IQ-FdUrd) is a substrate of reductases that were characterized by them. Release of FdUrd under hypoxic conditions after treatment with cytochrome NADPH P450 reductase and IQFdUrd was achieved. They also confirmed that IQ-FdUrd showed selective cytotoxicity in hypoxic tumor cells (Jiho et al., 2019). Doxorubicin (Dox) is a potent anticancer drug, but it causes dose-dependent cardiotoxicity. To overcome this problem, Gonzalez-Mendez et al. designed pH-sensitive prodrugs (Fig. 9.16) for improving its selectivity and reducing the toxic effects of the free drug. They examined Dox attached to adamantane (Ad) using three different pH-sensitive linkers; ester, amide, and hydrazone to reduce the toxicity of free drug. Kinetics of the in vitro hydrolysis of the three proposed linkers was evaluated at different pH values, considering the acid microenvironment that characterizes tumors. The cytotoxic activity of the prodrug with the best release profile displayed a similar behavior to the free drug, illustrating use of appropriate linker in the design of pH-sensitive Dox prodrugs (Gonzalez-Mendez et al., 2019). A novel strategy named radiation-induced apoptosistargeted chemotherapy (RIATC) that could specifically deliver cytotoxic agents to the tumor guided by radiotherapy was proposed by Chung et al. They synthesized a novel albumin-binding prodrug MPD02 (Fig. 9.17) by conjugating cytotoxin monomethyl auristatin E (MMAE) to the C-terminus of the KGDEVD peptide via self-eliminating linker and introduced a maleimide group to the Lys side chain of the peptide. They found that MPD02 metabolized Prodrugs Chapter | 9 177 FIGURE 9.17 Mechanism of releasing MMAE from prodrug induced by caspase-3. MMAE, Monomethyl auristatin E. FIGURE 9.18 Mechanism of releasing Dox and CA4 induced by light. CA4, Combretastatin A4; Dox, doxorubicin. into a highly potent MMAE on caspase-3-mediated activation, showing a highly potent anticancer effect with good safety profile in two different triple negative breast cancer (TNBC) xenograft models (Chung et al., 2019). Same researchers improved an RIATC prodrug by introducing an apoptotic cell-binding moiety, ApoPep-1, which binds to histone H1 translocated on the surface of apoptotic cells. The prodrug named AP1-DEVD-S-Dox was prepared by conjugating ApoPep-1 and Dox via a caspase-3-cleavable linker, allowing cytotoxic Dox to be released in the presence of caspase-3. Results showed that prodrug AP1-DEVD-S-Dox was able to selectively deliver Dox to the tumor with less systemic cytotoxicity (Cho et al., 2019). Since light is noninvasive external stimulus that can be manipulated, photoremovable protection groups (PPGs) have received much attention in recent years for clinical applications (Döbber et al., 2017; Ieda et al., 2016). Inactive prodrugs were prepared by conjugation of active drug to PPGs with covalent bonds to achieve maximum activity and minimum toxic effects by controlled release of active drug in the target region by light irradiation. Recently, various PPGs have been explored, but most of them were investigated to deliver a solo drug molecule (Ahmed and Fruk, 2013; Klan et al., 2013). Liu et al. synthesized a photoresponsive hybrid prodrug that has both Dox and combretastatin A4 (CA4) (Fig. 9.18) to explore the application of PPGs in the field of combination chemotherapy. They found that Dox release was achieved with 405 nm light and CA4 release with mostly 365 nm light. Cell viability assessment confirmed that the prodrug had greater toxicity to MDA-MB-231 TNBC cells compared to individual drugs, and a synergistic effect was achieved (Liu et al., 2019a). Gemcitabine (Gem), an anticancer agent, has a low therapeutic effect due to its short circulation time and rapid metabolism. To increase antitumor activity, a new Z-GP-Gem prodrug was developed by modifying the 4-amino group of Gem by Sun et al. This prodrug can effectively release Gem in the tumor through cleavage by FAPα enzyme activation. Compared to Gem, the Z-GPGem prodrug showed significant inhibition on both tumor growth and pulmonary metastasis in BALB/c mice bearing orthotopic breast 4T1 tumors. As Z-GP-Gem prodrug had a long circulation time and a high tumor uptake, it led to a remarkable improvement in systemic toxicity and inhibition of tumor growth in 4T1 cells. Also, in the animal model, depletion of tumor-associated fibroblast was 178 SECTION | 3 Pharmaceutical Chemistry observed during the treatment of Z-GP-Gem prodrug. Thus these findings showed that FAPα-activated prodrug would be a desirable approach for tumor treatment (Sun et al., 2019). High toxicity of colchicine limited its medical application in cancer therapy (Lin et al., 2013). Colchicine prodrugs and codrugs have been prepared to decrease toxicity and increase therapeutic properties (Huczynski et al., 2015; Nishiyama et al., 2014; Kurek et al., 2014; Singh et al., 2015). Recently, many efforts focused on colchicine nanoformulation, as well as chemical synthesis of colchicine prodrugs and codrugs with different linkers. Classification of colchicine prodrugs based on type of conjugates is noted as biopolymers prodrugs, fluorescent prodrug, metal complexes prodrug, metal-labile prodrug, and bioconjugate prodrug by Ghawanmeh et al. They summarized the biological importance of colchicine nanoformulation, colchicine prodrugs, and codrugs (Ghawanmeh et al., 2018). Methotrexate (MTX) is a CA used clinically for the treatment of different types of cancer, rheumatoid arthritis, psoriasis, and other autoimmune diseases (Chen et al., 2014; Khan et al., 2012; Tondwal and Singh, 2015; Yang et al., 2012). The therapeutic effect of MTX is reduced by its low tumor cell uptake, and it can cause severe side effects at therapeutic doses (Chatterjee et al., 1997). MTX also has low permeability, poor aqueous solubility, and poor bioavailability. To address all these limitations, an ionic liquid (IL) formulation of MTX has been prepared by Moshikur et al. (2019). An IL formulation of active pharmaceutical ingredients (APIs) was used to address the issue of polymorphisms (Furukawa et al., 2016; Ferraz et al., 2011; Shamshina and Rogers, 2014), which is often responsible for reducing therapeutic efficiency, bioavailability and thermal stability (Ferraz et al., 2011; Shamshina and Rogers, 2014; Yan et al., 2018). They synthesized a series of IL-APIs using MTX, and biocompatible IL-forming cations (choline and amino acid esters) as potential anticancer prodrugs. A mammalian cell line (HeLa cells) was used to evaluate their cytotoxicity. MTX-ILs showed 5000 times more water solubility than free MTX, and more solubility in both water and imitated body fluids, compared to a sodium salt of MTX. Proline ethyl ester MTX prodrug showed similar solubility to MTX sodium salt, but better in vitro antitumor activity. These results show that newly synthesized API-ILs are promising (Moshikur et al., 2019). Another advanced drug-delivery opportunity for prodrugs design is called enzyme prodrug therapy (EPT). A prodrug designed for it undergoes bioconversion by a specifically identified enzyme placed in a specific place in the body. Unlike general prodrugs, quantitative drug recovery is less important, and the main objective is to provide site-specific recovery. The localization of the enzyme at the desired site can be accomplished in various ways, with various degrees of success, and laboratory-to-clinic progression. Historically, antibodydirected EPT (ADEPT) is the earliest known success of EPT (Bagshawe et al., 1994). An antibody developed against a tumor antigen binds to an enzyme and is injected into the blood, thereby, causing selective binding of the enzyme within the tumor. The second step is to administer the prodrug after cleansing the free antibodyenzyme conjugate from the blood stream. In such a case the enzyme-mediated prodrug activation is carried out only by the antigen-bound enzyme thus providing localized drug delivery. Alkaline phosphatase is a member of phosphoesterases and was the first enzyme used in ADEPT (Senter, 1990; Springer et al., 1990). The first drugs used in ADEPT were clinically approved anticancer drugs, etoposide, mitomycin, and Dox (Senter, 1990). Such EPTs in medicinal chemistry are discussed in detail by Walther et al. (2017). Gene-directed EPT (GDEPT) has also received big attention because it limits toxicity at healthy cells and increases tumor cell uptake for cancer therapies (Bhaumik et al., 2012). GDEPT has two steps. First is transfer of the enzyme gene to the tumor cell by loading the carrier vector and expression of this gene in the tumor cell (Denny, 2002; Dachs et al., 2005). Second step is conversion of nontoxic prodrug to cytotoxic drug by enzyme catalysis. After all, the active drug is transported to other cancer cells (Zhang et al., 2017a). Nitroreductases (NTR) catalyze the reduction of nitro compounds by using NAD(P) H. The use of NTR in GDEPT studies is extraordinary. For discovery of new prodrug/NTR combinations, nitrocontaining aromatic amides (A1-A23) (Denny, 2002) were designed and synthesized in silico ADMET and molecular docking experiments were then performed by Güngör et al. (2019). Reduction potentials of prodrug candidates were studied using Ssap-NtrB by HPLC system. Cyototoxic properties of prodrugs were investigated using different cancer cell lines such as Hep3B and PC3. As a result of biological studies, it was determined that combinations of A5, A6, and A20 (Fig. 9.19) with Ssap-NtrB can be suggested as potential prodrugs/enzyme combinations in NTR-based cancer therapy (Güngör et al., 2019). Paclitaxel (PTX) is an anticancer drug mostly used for breast cancer, and ovarian cancer (Schiff et al., 1979). It has a unique microtubule mechanism during mitosis, but the long-term use can lead to the development of resistance that further limits its applications (Dowdy et al., 2006). To address this limitation, it is important to increase drug accumulation in tumor tissues and reduce their resistance. Histone deacetylase inhibitors (HDACIs) have shown good activity in multiple cancers, either alone or by combination with conventional anticancer drugs (Huang and Geng, 2017; Fallkenberg and Johnstone, 2014). Prodrugs Chapter | 9 179 FIGURE 9.19 Structures of nitro-containing aromatic amides A5, A6, and A20. FIGURE 9.20 PTXSAHA coprodrugs with Gly (1a) and succinic acid (1b) linkers. Gly, Glycine; PTX, paclitaxel; SAHA, suberoylanilide hydroxamic acid. Suberoylanilide hydroxamic acid (SAHA) is an HDACI that has strong anticancer effects in hematological tumors (Duvic and Vu, 2007). It has been shown that SAHA could potentiate PTX-induced antitumor effects against some cancers (Cooper et al., 2007; Modesitt and Parsons, 2010; Shi et al., 2010). Liu et al. (2019b) improved the stability of SAHA and decreased drug resistance after cellular uptake of the PTXSAHA coprodrugs by conjugating them in a cleavable way. They attached the hydroxamic acid group of SAHA and the 20 -OH of PTX to create a coprodrug and further formed the coprodrug nanomicelles with mPEG2000PLA1750 as the carrier (Sankar and Ravikumar, 2014). They used glycine (Gly) and succinic acid as the linker of PTXSAHA coprodrugs (Fig. 9.20). The releasing mechanism of coprodrugs is hydrolysis of the carbonic ester bound to SAHA by hydrolysis or enzymolysis first. Subsequently, the rate of release of PTX depends essentially on the stability of the remaining complex. It has been found that PTX20 -Gly is unstable when exposed to water and the other is more stable under the same conditions (Greenwald et al., 2003; Wong and Choi, 2015). They examined the stability of coprodrugs and in vitro cytotoxicity in human colorectal cell line HCT-116, breast cancer cell lines MCF-7 and MCF-7/ADR. It was found that 1a effectively releases PTX and SAHA and had better cytotoxicity than 1b. Comparing free PTX and 1a coprodrug, 1a coprodrug increased the anticancer efficacy and effectively reversed PTX resistance in cancer treatment (Liu et al., 2019). Phosphoinositide 3-kinase (PI3K) inhibitors have been considered as adjuvant therapy for advanced prostate cancer. But, expected results have not been achieved in the clinic. Increasing the effectiveness of PI3K inhibitors against prostate cancer by the conversion of the inhibitor to an inactive prodrug through adding a separable specific prostate-specific antigen (PSA) peptide (Abet et al., 2017) has been explored. In systemic circulation, PSA is inactive and protease activity is limited to prostate or prostate-derived cancer cells. The cleavable peptide has the sequence Mu-LEHSSKLQL (N-(4morpholinylcarbonyl)-Leu-Glu-His-Ser-Ser-Lys-Leu-GlnLeu), and HSSKLQ is the substrate for PSA. Therefore activation of the water-soluble prodrug yields the active drug, a PI3K inhibitor LY294002-analog, which minimizes systemic toxicity and increases delivery to the tumor site (Fig. 9.21; Abet et al., 2017; Morales et al., 2013; Baiz et al., 2012). The primary cause of melanoma, the most dangerous type of skin cancer and which develops from melanocytes, is ultraviolet (UV) light exposure. Melanintargeting probes (MTPs) are a group of arylcarboxamide families with high affinity for melanins which contain molecular targets detected in more than 90% of primary melanoma cases and 30%50% of metastatic lesions. 180 SECTION | 3 Pharmaceutical Chemistry FIGURE 9.21 Conversion of water-soluble prodrug to active drug. FIGURE 9.22 Conversion of the prodrug to the active drug by cleavation of the disulfide bond. The use of such MTPs to transport an anticancer drug into the melanoma tumor site was explored by El Aissi et al. (2015). They reported synthesis and evaluation of a prodrug (Fig. 9.22) for pigmented melanoma therapy. It contains an MTP conjugated to the antimetabolite 5-iodo20-deoxyuridine. The fragments were linked by a binder comprising a disulfide bond that is stable in plasma but is cleaved effectively by intracellular reduction systems found in hypoxic tumor cells. The resulting thiol undergoes cyclization to provide free anticancer agent (Abet et al., 2017; El Aissi et al., 2015; Vivier et al., 2008). Nitrogen mustards are anticancer drugs that act by alkylating DNA in purine rings. However, they have very important side effects in noncancerous tissues and cells resulting from nondiscriminatory alkylation of biomolecules. Also, aziridinium ion formation is suppressed in the presence of electron withdrawing groups in N-aryl nitrogen mustard and, by contrast, increases with donating groups on the aryl ring. Johnson et al. (2014) reported that a new nitrogen mustard prodrug was prepared in which mustard binds to Tirapazamine, a heterocyclic di-N-dioxide that undergoes enzymatic deoxygenation in hypoxic solid tumor cells to produce mono-N-oxide metabolite (Fig. 9.23). This method resulted in significant increase in the reactivity of the mustard unit and unmasked the bioactive material in the hypoxic cells (Abet et al., 2017). Unsaturated fatty acids (UFAs) have been extensively investigated in the rational design of CA-UFA prodrugs in cancer therapy, with good advantages of biocompatibility and innate tumor targeting effect. In the last few decades, numerous chemotherapeutic CA-UFA prodrugs have been developed (Sun et al., 2017). Among these, Gemelaidic acid conjugate (CP-4126), cytarabinelaidic acid conjugate (CP-4055), and PTXDHA conjugate have successfully entered clinical trials. However, clinical results of the prodrugs lagged behind expectations. Several factors may be responsible for the inadequate clinical outcomes, such as tumor types and heterogeneity, therapeutic program, and drug resistance. To address these problems, prodrug-based nanodrug-delivery system (DDS) combining the advantages of prodrug strategy and nanotechnology has shown great potential in cancer therapy, particularly for promising CA-UFA prodrug-based spontaneous nano-assemblies. The advanced drugdelivery strategies based on UFA conjugates and focusing on recent advances in CA-UFA prodrugs and the emerging CA-UFA prodrug-based nano-DDS were reviewed by Sun et al. (2017). They focused on the rational design of CA-UFA prodrugs in response to multiple barriers to chemotherapy, emphasizing the latest developments in both preclinical and clinical trials. The resulting CA-UFA prodrug-based nano-DDS was also discussed. It emphasized the prospects and potential challenges of CA-UFA prodrug-based drug-delivery strategies in chemotherapy. The emerging multifaceted nano-platform based on CA-UFA conjugates shows significant advantages in drug bioavailability, delivery efficiency and has great potential for clinical applications (Sun et al., 2017). Prodrug-based nanosystems are of great interest as they provide significant benefits such as increased chemical stabilities in vivo, longer drug-release profiles, and low toxicities before degradation takes place (Yu et al., 2018). Researchers are working extensively to find new prodrugs and improve pharmacokinetics and pharmacodynamics in vivo (Zhang et al., 2017b). Prodrugs enhance the therapeutic effects and reduce side effects by placing stimuli-responsive properties such as redox, pH, and temperature into the nanoparticles (NPs) (Ma et al., 2018). Such a system was synthesized by Hong et al. They encapsulated a curcumin (CUR) and peptide-Dox (U11Dox) to an NP system (U11-Dox/CUR NPs) to treat lung cancer. Prodrug-based nanosystems showed a remarkable antitumor effect with less toxicity in vivo (Hong et al., 2019). Furthermore, Zhu et al. prepared a novel pH-sensitive and charge-convertible prodrug nanogel to achieve targeted delivery of Dox to enhance the efficacy and reduce side effects. They synthesized an NP system containing a folic acidmodified gelatin (Gel-FA)/pluronic F127chitosan-CAD (F127-CS-CAD)/cis-aconitic anhydrideDox prodrug successfully. It was found that the system had better therapeutic effects on tumors, and the toxic side effects were decreased significantly when compared to free Dox (Zhu et al., 2019). A prodrug of 5-FU (Fig. 9.24) covalently conjugated to low molecular weight chitosan (LMWC) via a photocleavable linker has been synthesized by Horo et al. to improve hydrophilicity as well as increase the biological retention time of the drug. Then, they used ionic gelation technique to the LMWC-5-FU conjugate into NPs for effective penetration into cells. The conjugate was FIGURE 9.23 Conversion of nitro mustard prodrug to a mono-N-oxide metabolite. 182 SECTION | 3 Pharmaceutical Chemistry FIGURE 9.24 Mechanism of releasing 5-FU induced by 365 nm light. 5FU, 5-Fluorouracil. designed to be cleaved under 365 nm UV-A radiation. The conjugate was been found to exhibit greater water solubility compared to LMWC and formed hydrogel (Horo et al., 2019). 9.5 Summary Prodrugs are usually used with the aim of increasing drug permeation by enhancing lipophilicity or water solubility. The prodrug must exhibit enough aqueous solubility and stability, adequate lipophilicity, sufficient safety, and reasonable conversion to the parent drug in vivo. To enhance therapeutic index, and reduce toxicity issues of cytotoxic chemotherapy, targeted prodrug approaches are new directions in the treatment of cancer. Prodrugs can concentrate at desired cells and show activities there in a selective way. Prodrug-based nanosystems also are of great interest as they can provide significant benefits such as increased chemical stability in vivo, longer drugrelease period, and low toxicity before degradation takes place. Wide-ranging research in this field and growing knowledge of drug delivery should generate more new marketable prodrugs in the future. References Abet, V., Filace, F., Recio, J., Alvarez-Builla, J., Burgos, C., 2017. Prodrug approach: an overview of recent cases. Eur. J. Med. Chem. 127, 810827. Ahmed, I., Fruk, L., 2013. The power of light: photosensitive tools for chemical biology. Mol. Biosyst. 9 (4), 565570. Akashi, M., Takemoto, K., 1990. New aspects of polymer drugs. Adv. Polym. Sci. 97, 107. Albert, A., 1958. Chemical aspects of selective toxicity. Nature 182, 421423. Andurkar, S.V., 2007. Chemical modifications and drug delivery. In: Gibaldi, M. (Ed.), Gibaldi’s Drug Delivery Systems in Pharmaceutical Care. American Society of Health-System Pharmacists, Bethesda, MD. Bagshawe, K.D., Sharma, S.K., Springer, C.J., Rogers, G.T., 1994. Antibody directed enzyme prodrug therapy (ADEPT): a review of some theoretical, experimental and clinical aspects. Ann. Oncol. 5, 879891. Baiz, D., Pinder, T.A., Hassan, S., Karpova, Y., Salsbury, F., Welker, M. E., et al., 2012. Synthesis and characterization of a novel prostate cancer-targeted phosphatidylinositol-3-kinase inhibitor prodrug. J. Med. Chem. 55, 80388046. Beaumont, K., Webster, R., Gardner, I., Dack, K., 2003. Design of ester prodrugs to enhance oral absorption of poorly permeable compounds: challenges to the discovery scientist. Curr. Drug Metab. 4, 461485. Bhaumik, S., Sekar, T.V., Depuy, J., Klimash, J., Paulmurugan, R., 2012. Noninvasive optical imaging of nitroreductase gene-directed enzyme prodrug therapy system in living animals. Gene Ther. 19, 295302. Bonina, F.P., Puglia, C., Barbuzzi, T., de Caprariis, P., Palagiano, F., Rimoli, M.G., et al., 2001. In vitro and in vivo evaluation of polyoxyethylene esters as dermal prodrugs of ketoprofen, naproxen and diclofenac. Eur. J. Pharm. Sci. 14 (2), 123134. Calabresi, P., Parks, R.E., 1985. Antimetabolites. In: Goodman, L.S., Raal, T.W., Murad, F. (Eds.), Pharmacological Basis of Therapeutics. Macmillan, New York, pp. 12681276. Chatterjee, D.J., Li, W.Y., Koda, R.T., 1997. Effect of vehicles and penetration enhancers on the in vitro and in vivo percutaneous absorption of methotrexate and edatrexate through hairless mouse skin. Pharm. Res. 14, 10581065. Chen, J., Huang, L., Lai, H., Lu, C., Fang, M., Zhang, Q., et al., 2014. Methotrexate-loaded PEGylated chitosan nanoparticles: synthesis, characterization, and in vitro and in vivo antitumoral activity. Mol. Pharm. 11, 22132223. Cho, Y.S., Chung, S.W., Kim, H.R., Won, T.H., Choi, J.U., Kim, I.S., et al., 2019. The novel strategy for concurrent chemoradiotherapy by conjugating the apoptotic cell-binding moiety to caspase-3 activated doxorubicin prodrug. J. Control. Release 296, 241249. Chung, S.W., Cho, Y.S., Choi, J.U., Kim, H.R., Won, T.H., Kim, S.Y., et al., 2019. Highly potent monomethyl auristatin E prodrug activated by caspase-3 for the chemoradiotherapy of triple-negative breast cancer. Biomaterials 192, 109117. Cohen, S.S., Plunkett, W., 1975. The utilization of nucleotides by animal cells. Ann. N. Y. Acad. Sci. 255, 269286. Cooper, A.L., Greenberg, V.L., Lancaster, P.S., van Nagell, J.R., Zimmer, S.G., Modesitt, S.C., 2007. In vitro and in vivo histone deacetylase inhibitor therapy with suberoylanilide hydroxamic acid (SAHA) and paclitaxel in ovarian cancer. Gynecol. Oncol. 104 (3), 596601. Dachs, G.U., Tupper, J., Tozer, G.M., 2005. From bench to bedside for gene-directed enzyme prodrug therapy of cancer. Anticancer Drugs 16, 349359. Dang, Q., Brown, B.S., van Poelje, P.D.V., Colby, T.J., Erion, M.D., 1999. Synthesis of phosphonate 3-phthalidyl esters as prodrugs for potential intracellular delivery of phosphonates. Bioorg. Med. Chem. Lett. 9 (11), 15051510. Denny, W.A., 2002. Nitroreductase-based GDEPT. Curr. Pharm. Des. 8, 13491361. DeSantis, C.E., Lin, C.C., Mariotto, A.B., et al., 2014. Cancer treatment and survivorship statistics. CA Cancer J. Clin. 64 (4), 252271. Prodrugs Chapter | 9 Dhareshwar, S.S., Stella, V.J., 2007. Prodrug of alcohols and phenols. In: Stella, V., et al., (Eds.), Prodrugs: Challenges and Rewards. Part 2. AAPS Press/Springer, New York, pp. 3382. Döbber, A., Phoa, A.F., Abbassi, R.H., Stringer, B.W., Day, B.W., Johns, T.G., et al., 2017. Development and biological evaluation of a photoactivatable small molecule microtubule-targeting agent. ACS Med. Chem. Lett. 8 (4), 395400. Dowdy, S.C., Jiang, S.J., Zhou, X.C., Hou, X., Jin, F., Podratz, K.C., et al., 2006. Histone deacetylase inhibitors and paclitaxel cause synergistic effects on apoptosis and microtubule stabilization in papillary serous endometrial cancer cells. Mol. Cancer Ther. 5 (11), 27672776. Duvic, M., Vu, J., 2007. Vorinostat: a new oral histone deacetylase inhibitor approved for cutaneous T-cell lymphoma. Expert Opin. Investig. Drugs 16 (7), 11111120. El Aissi, R., Chezal, J.-M., Tarrit, S., Chavignon, O., Moreau, E., 2015. Melanoma targeted delivery system (part 1): design, synthesis and evaluation of releasable disulfide drug by glutathione. Eur. J. Med. Chem. 101, 668680. Escoriaza, J., Aldaz, A., Castellanos, C., Calvo, E., Giráldez, J., 2000. Simple and rapid determination of irinotecan and its metabolite SN38 in plasma by high-performance liquid-chromatography: application to clinical pharmacokinetic studies. J. Chromatogr. B: Biomed. Sci. Appl. 740 (2), 159168. Ettmayer, P., Amidon, G.L., Clement, B., Testa, B., 2004. Lessons learned from marketed and investigational prodrugs. J. Med. Chem. 47, 23932404. Fallkenberg, K.J., Johnstone, R.W., 2014. Histone deacetylases and their inhibitors in cancer, neurological diseases and immune disorders. Nat. Rev. Drug Discov. 13 (9), 673691. Ferraz, R., Branco, L.C., Prudêncio, C., Noronha, J.P., Petrovski, Ž., 2011. Ionic liquids as active pharmaceutical ingredients. ChemMedChem 6, 975985. Food and Nutrition Board, Institute of Medicine, 1997. Phosphorus. Dietary Reference Intakes: Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. National Academy Press, Washington, DC, pp. 146189. Fuchs, T., 2007. Case study: cefuroxime axetil: an oral prodrug of cefuroxime. In: Stella, V., et al., (Eds.), Prodrugs: Challenges and Rewards. Part 2. AAPS Press/Springer, New York, pp. 497503. Furukawa, S., Hattori, G., Sakai, S., Kamiya, N., 2016. Highly efficient and low toxic skin penetrants composed of amino acid ionic liquids. RSC Adv. 6, 8775387755. Ghawanmeh, A.A., Chong, K.F., Sarkar, S.M., Bakar, M.A., Othaman, R., Khalid, R.M., 2018. Colchicine prodrugs and codrugs: chemistry and bioactivities. Eur. J. Med. Chem. 144, 229242. Gonzalez-Mendez, I., Solano, J.D., Porcu, P., Rui, A., Rojas-Aguirre, Y., Rivera, E., 2019. Optimized synthesis, characterization and in vitro systematic evaluation of adamantane-doxorubicin prodrugs sensitive to pH in breast cancer cells. J. Mol. Struct. 1177, 143151. Greco, F.A., Hainsworth, J.D., 1995. Etoposide phosphate or etoposide with cisplatin in the treatment of small cell lung cancer: randomized phase II trial. Lung Cancer 12 (3), S85S95. Greco, F.A., Johnson, D.H., Hainsworth, J.D., 1991. Chronic oral etoposide. Cancer 67 (S1), 303309. Greenwald, R.B., Zhao, H., Reddy, P., 2003. Synthesis, isolation, and characterization of 20 -paclitaxel glycinate: an application of the Bsmoc protecting group. J. Org. Chem. 68 (12), 48944896. 183 Güngör, T., Önder, F.C., Tokay, E., Gülhan, Ü.G., Hacıoğlu, N., Tok, T. T., et al., 2019. Prodrugs for nitroreductase based cancer therapy-2: novel Amide/Ntr combinations targeting Pc3 cancer cells. Eur. J. Med. Chem. 171, 383400. Han, H.K., Amidon, G.L., 2000. Targeted prodrug design to optimize drug delivery. AAPS Pharm. Sci. 2, 1. Hatfield, M.J., Tsurkan, L., Garrett, M., Shaver, T.M., Hyatt, J.L., Edwards, C.C., et al., 2011. Organ-specific carboxylesterase profiling identifies the small intestine and kidney as major contributors of activation of the anticancer prodrug CPT-11. Biochem. Pharmacol. 81 (1), 2431. He, G.-X., Krise, J.P., Oliyai, R., 2007. Prodrugs of phosphates, phosphonates, and phosphinates. In: Stella, V., et al., (Eds.), Prodrugs: Challenges and Rewards. Part 2. AAPS Press/Springer, New York, pp. 625632. Heimbach, T., Oh, D.-M., Li, L.Y., Rodrı́guez-Hornedo, N., Garcia, G., Fleisher, D., 2003. Enzyme-mediated precipitation of parent drugs from their phosphate prodrugs. Int. J. Pharm. 261 (12), 8192. Heimbach, T., Fleisher, D., Kaddoumi, A., 2007. Overcoming poor aqueous solubility of drugs for oral delivery. In: Stella, V., et al., (Eds.), Prodrugs: Challenges and Rewards. Part 1. AAPS Press/Springer, New York, pp. 159199. Hemenway, J., Stella, V.J., 2007. Prodrugs and parenteral drug delivery. In: Stella, V., et al., (Eds.), Prodrugs: Challenges and Rewards. Part 1. AAPS Press/Springer, New York, pp. 219264. Hong, Y., Che, S., Hui, B., Yang, Y., Wang, X., Zhang, X., et al., 2019. Lung cancer therapy using doxorubicin and curcumin combination: targeted prodrug based, pH sensitive nanomedicine. Biomed. Pharmacother. 112, 108614. Horo, H., Das, S., Mandal, B., Kundu, L.M., 2019. Development of a photoresponsive chitosan conjugated prodrug nano-carrier for controlled delivery of antitumor drug 5-fluorouracil. Int. J. Biol. Macromol. 121, 10701076. Hu, L., 2004. The prodrug approach to better targeting. In: Meeting Report of Prodrugs: Effective Solutions for Solubility, Permeability, and Targeting Challenges. June 2829, 2004, Philadelphia, PA. Available from: ,http://www.currentdrugdiscovery.com. (accessed 08.08.09.). Huang, M., Geng, M., 2017. Exploiting histone deacetylases for cancer therapy: from hematological malignancies to solid tumors. Sci. China Life Sci. 60 (1), 9497. Huczynski, A., Rutkowski, J., Popiel, K., Maj, E., Wietrzyk, J., Stefanska, J., et al., 2015. Synthesis, antiproliferative and antibacterial evaluation of C-ring modified colchicine analogues. Eur. J. Med. Chem. 90, 296301. Hyatt, J.L., Tsurkan, L., Morton, C.L., Yoon, K.J.P., Harel, M., Brumshtein, B., et al., 2005. Inhibition of acetylcholinesterase by the anticancer prodrug CPT-11. Chem. Biol. Interact. 157-158, 247. Ieda, N., Yamada, S., Kawaguchi, M., Miyata, N., Nakagawa, H., 2016. (7-Diethylaminocoumarin-4-yl)methyl ester of suberoylanilide hydroxamic acid as a caged inhibitor for photocontrol of histone deacetylase activity. Bioorg. Med. Chem. 24, 2789. Incecayir, T., Sun, J., Tsume, Y., Xu, H., Gose, T., Nakanishi, T., et al., 2016. Carrier-mediated prodrug uptake to ımprove the oral bioavailability of polar drugs: an application to an oseltamivir analogue. J. Pharm. Sci. 105 (2), 925934. Jarho, P., Jarvinen, K., Urtti, A., Stella, V.J., Jarvinen, T., 1997. The use of cyclodextrins in ophthalmic formulations of dipivefrin. Int. J. Pharm. 153, 225. 184 SECTION | 3 Pharmaceutical Chemistry Jarvinen, T., Jarvinen, K., 1996. Prodrugs for improved ocular drug delivery. Adv. Drug Deliv. Rev. 19, 203224. Jiho, Y., Kurihara, R., Kawai, K., Yamada, H., Uto, Y., Tanabe, K., 2019. Enzymatic activation of indolequinone-substituted 5-fluorodeoxyuridine prodrugs in hypoxic cells. Bioorg. Med. Chem. Lett. 29, 13041307. Johnson, M.A., Ahluwalia, G., Connelly, M.C., Conney, D.A., Brodor, S., Johns, D.G., et al., 1988. Metabolic pathways for the activation of the antiretroviral agent 2’,3’-dideoxyadenosine in human lymphoid cells. J. Biol. Chem. 263 (30), 1535415357. Johnson, K.M., Parsons, Z.D., Barnes, C.L., Gates, K.S., 2014. Toward hypoxia-selective DNA-alkylating agents built by grafting nitrogen mustards onto the bioreductively activated, hypoxia-selective DNAoxidizing agent 3-amino-1,2,4-benzotriazine 1,4-dioxide (tirapazamine). J. Org. Chem. 79, 75207531. Jones, R.J., Bischofberger, N., 1995. Minireview: nucleotide prodrugs. Antiviral Res. 27 (12), 117. Jones, B.C., McGuigan, C., Riley, P.A., 1989. Synthesis and biological evaluation of some phosphate triester derivatives of the anti-cancer drug araC. Nucleic Acids Res. 17 (18), 71957201. Kearney, A.S., Stella, V.J., 1993. Hydrolysis of pharmaceutically relevant phosphate monoester monoanions: correlation to an established structure-reactivity relationship. J. Pharm. Sci. 82, 6972. Khan, Z.A., Tripathi, R., Mishra, B., 2012. Methotrexate: a detailed review on drug delivery and clinical aspects. Expert Opin. Drug Deliv. 9, 151169. Klan, P., Šolomek, T., Bochet, C.G., Blanc, A., Givens, R., Rubina, M., et al., 2013. Photoremovable protecting groups in chemistry and biology: reaction mechanisms and efficacy. Chem. Rev. 113 (1), 119191. Krise, J.P., Stella, V.J., 1996. Prodrugs of phosphates, phosphonates, and phosphinates. Adv. Drug Deliv. Rev. 19, 287310. Krise, J.P., Oliyai, R., 2007. Prodrugs of amines. In: Stella, V., et al., (Eds.), Prodrugs: Challenges and Rewards. Part 2. AAPS Press/ Springer, New York, pp. 103124. Kuehl, G.E., Bigler, J., Potter, J.D., Lampe, J.W., 2006. Glucuronidation of the aspirin metabolite salicylic acid by expressed UDPglucuronosyltransferases and human liver microsomes. Drug Metab. Dispos. 34 (2), 199202. Kurek, J., Boczon, W., Myszkowski, K., Murias, M., Borowiak, T., Wolska, I., 2014. Synthesis of sulfur containing colchicine derivatives and their biological evaluation as cytotoxic agents. Lett. Drug Des. Discov. 11, 279289. Lee, H.J., 1995. Biopharmaceutical properties and pharmacokinetics of peptide and protein drugs. In: Taylor, M.D., Amidon, G.L. (Eds.), Peptide Based Drug Design. Controlling Transport and Metabolism. ACS Books, Washington, DC, pp. 6997. LePage, G.A., Naik, S.R., Katakkar, S.B., Khaliq, A., 1975. 9-beta-Darabinofuranosyladenine 5’-phosphate metabolism and excretion in humans. Cancer Res. 35 (11), 30363040. Liederer, B.M., Borchardt, R.T., 2006. Enzymes involved in the bioconversion of ester-based prodrugs. J. Pharm. Sci. 95, 11771195. Lin, Z.-Y., Wu, C.-C., Chuang, Y.-H., Chuang, W.-L., 2013. Anti-cancer mechanisms of clinically acceptable colchicine concentrations on hepatocellular carcinoma. Life Sci. 93, 323328. Liu, W., Liang, L., Zhao, L., Tan, H., Wu, J., Qin, Q., et al., 2019a. Synthesis and characterization of a photoresponsive doxorubicin/combretastatin A4 hybrid prodrug. Bioorg. Med. Chem. Lett. 29, 487490. Liu, S., Zhang, K., Zhu, Q., Shen, Q., Zhang, Q., Yu, J., et al., 2019b. Synthesis and biological evaluation of paclitaxel and vorinostat co-prodrugs for overcoming drug resistance in cancer therapy in vitro. Bioorg. Med. Chem. 27, 14051413. Ma, B., Zhuang, W., Wang, Y., Luo, R., Wang, Y., 2018. pH-sensitive doxorubicin-conjugated prodrug micelles with charge-conversion for cancer therapy. Acta Biomater. 70, 186196. Majumdar, S., Sloan, K.B., 2006. Synthesis, hydrolyses and dermal delivery of N-alkyl-N-alkyloxycarbonylaminomethyl (NANAOCAM) derivatives of phenol, imide and thiol containing drugs. Bioorg. Med. Chem. Lett. 16 (13), 35903594. McComb, R.B., Bowers, G.N.J., Posen, S., 1979. Alkaline Phosphatase. Plenum Press, New York and London, p. 986. McGuigan, C., Tollerfield, S.M., Riley, P.A., 1989. Synthesis and biological evaluation of some phosphate triester derivatives of the antiviral drug AraA. Nucleic Acids Res. 17 (15), 60656075. McGuigan, C., O’Connor, T.J., Nicholls, S.R., Nickson, C., Kinchington, D., 1990. Synthesis and anti-HIV activity of some novel substituted dialkyl phosphate derivatives of AZT and ddCyd. Antivir. Chem. Chemother. 1 (6), 355360. McGuigan, C., Devine, K.G., O’Connor, T.J., Kinchington, D., 1991. Synthesis and anti-HIV activity of some haloalkyl phosphoramidate derivatives of 3’-azido-3’-deoxythymidine (AZT): potent activity of the trichloroethyl methoxyalaninyl compound. Antiviral Res. 15 (3), 255263. Modesitt, S.C., Parsons, S.J., 2010. In vitro and in vivo histone deacetylase inhibitor therapy with vorinostat and paclitaxel in ovarian cancer models: does timing matter? Gynecol. Oncol. 119 (2), 351357. Morales, G.A., Garlich, J.R., Su, J., Peng, X., Newblom, J., Weber, K., et al., 2013. Synthesis and cancer stem cell-based activity of substituted 5-morpholino-7H-thieno[3,2-b]pyran-7-ones designed as next generation PI3K inhibitors. J. Med. Chem. 56, 19221939. Moshikur, R.M., Chowdhury, M.R., Wakabayashi, R., Tahara, Y., Moniruzzaman, M., Goto, M., 2019. J. Mol. Liq. 278, 226233. Nichifor, M., Schacht, E.H., Seymour, L.W., 1996. Macromolecular prodrugs of 5-fluorouracil. 2: Enzymatic degradation. J. Control. Release 39 (1), 7992. Nicholson, K.M., Phillips, R.M., Shnyder, S.D., Bibby, M.C., 2002. In vitro and in vivo activity of LS 4477 and LS 4559, novel analogues of the tubulin binder estramustine. Eur. J. Cancer 38 (1), 194204. Nishiyama, H., Ono, M., Sugimoto, T., Sasai, T., Asakawa, N., Ueno, S., et al., 2014. 4-Chlorocolchicine derivatives bearing a thiourea side chain at the C-7 position as potent anticancer agents. MedChemComm 5, 452458. Ohwada, J., Ozawa, S., Kohchi, M., Fukuda, H., Murasaki, C., Suda, H., et al., 2009. Synthesis and biological activities of a pH-dependently activated water-soluble prodrug of a novel hexacyclic camptothecin analog. Bioorg. Med. Chem. Lett. 19 (10), 27722776. Oliyai, R., 1996. Prodrugs of peptides and peptidomimetics for improved formulation and delivery. Adv. Drug Deliv. Rev. 19 (2), 275286. Ouchi, T., Banba, T., Matsumoto, T., Suzuki, S., Suzuki, M., 1990a. Synthesis and antitumor activity of conjugates of 5-fluorouracil and chito-oligosaccharides involving a hexamethylene spacer group and carbamoyl bonds. Drug Des. Deliv. 6 (4), 281287. Ouchi, T., Fujino, A., Tanaka, K., Banba, Y., 1990b. Synthesis and antitumor activity of conjugates of poly(α-malic acid) and 5-fluorouracils bound via ester, amide or carbamoyl bonds. J. Control. Rel. 12 (2), 143153. Prodrugs Chapter | 9 Ouchi, T., Hagihara, Y., Takahashi, K., Takano, Y., Igarashi, I., 1992. Synthesis and antitumor activity of poly(ethylene glycols)s linked to 5fluorouracil via a urethane or urea bond. Drug Des. Discov. 9, 93105. Perkins, R., Fang, H., Tong, W., Welsh, W.J., 2003. Quantitative structure-activity relationship methods: perspectives on drug discovery and toxicology. Environ. Toxicol. Chem. 22 (8), 16661679. Posternak, T., 1974. Cyclic AMP and cyclic GMP. Annu. Rev. Pharmacol. 14, 2333. Rautio, J., Nevalainen, T., Taipale, H., Vepsäläinen, J., Gynther, J., Laine, K., et al., 2000. Piperazinylalkyl prodrugs of naproxen improve in vitro skin permeation. Eur. J. Pharm. Sci. 11 (2), 157163. Rautio, J., Kumpulainen, H., Heimbach, T., Oliyai, R., Oh, D., Järvinen, T., et al., 2008a. Prodrugs: design and clinical applications. Nat. Rev. Drug Discov. 7, 255270. Rautio, J., Laine, K., Gynther, M., Savolainen, J., 2008b. Prodrug approaches for CNS delivery. AAPS J. 10 (1), 92102. Rivory, L.P., Bowles, M.R., Robert, J., Pond, S.M., 1996. Conversion of irinotecan (CPT-11) to its active metabolite, 7-ethyl-10hydroxycamptothecin (SN-38), by human liver carboxylesterase. Biochem. Pharmacol. 52 (7), 11031111. Robins, R.K., 1984. The potential of nucleotide analogs as inhibitors of retroviruses and tumors. Pharm. Res. 1 (1), 1118. Sankar, R., Ravikumar, V., 2014. Biocompatibility and biodistribution of suberoylanilide hydroxamic acid loaded poly (DL-lactide-co-glycolide) nanoparticles for targeted drug delivery in cancer. Biomed. Pharmacother. 68 (7), 865871. Saulnier, M.G., Langley, D.R., Kadow, J.F., Senter, P.D., Knipe, J.O., Tun, M.M., et al., 1994. Synthesis of etoposide phosphate, BMY40481: a water-soluble clinically active prodrug of etoposide. Bioorg. Med. Chem. Lett. 4 (21), 25672572. Schiff, P.B., Fant, J., Horwitz, S.B., 1979. Promotion of microtubule assembly in vitro by taxol. Nature 277, 665667. Senter, P.D., 1990. Activation of prodrugs by antibody-enzyme conjugates: a new approach to cancer therapy. FASEB J. 4, 188193. Serafinowska, H.T., Ashton, R.J., Baily, S., Harnden, M.R., Sutton, D., 1995. Synthesis and in vivo evaluation of prodrugs of 9-[2-(phosphonomethoxy)ethoxy]adenine. J. Med. Chem. 38, 13721379. Shamshina, J.L., Rogers, R.D., 2014. Overcoming the problems of solid state drug formulations with ionic liquids. Ther. Deliv. 5, 489491. Sherwood, R.F., 1996. Advanced drug delivery reviews: enzyme prodrug therapy. Adv. Drug Del. Rev. 22, 269288. Shi, Y.K., Li, Z.H., Han, X.Q., Yi, J.H., Wang, Z.H., Hou, J.L., et al., 2010. The histone deacetylase inhibitor suberoylanilide hydroxamic acid induces growth inhibition and enhances taxol-induced cell death in breast cancer. Cancer Chemother. Pharmacol. 66 (6), 11311140. Shibata, J., Toko, T., Saito, H., Fujioka, A., Sato, K., Hashimoto, A., et al., 2000. Estrogen agonistic/antagonistic effects of miproxifene phosphate (TAT-59). Cancer Chemother. Pharmacol. 45 (2), 133141. Shimma, N., 2007. Case study: capecitabine: a prodrug of 5-fluorouracil. In: Stella, V., et al., (Eds.), Prodrugs: Challenges and Rewards. Part 2. AAPS Press/Springer, New York, pp. 475482. Simplı́cio, A.L., Clancy, J.M., Gilmer, J.F., 2008. Prodrugs for amines. Molecules 13 (3), 519547. Singh, B., Kumar, A., Joshi, P., Guru, S.K., Kumar, S., Wani, Z.A., et al., 2015. Colchicine derivatives with potent anticancer activity and reduced P-glycoprotein induction liability. Org. Biomol. Chem. 13, 56745689. Sinkula, A.A., Yalkowsky, S.H., 1975. Rationale for design of biologically reversible drug derivatives: prodrugs. J. Pharm. Sci. 64 (2), 181. 185 Sloan, K.B., Wasdo, S., 2003. Designing for topical delivery: prodrugs can make the difference. Med. Res. Rev. 23, 763. Sloan, K.B., Wasdo, S., 2007. Topical delivery using prodrugs. In: Stella, V., et al., (Eds.), Prodrugs: Challenges and Rewards. Part 1. AAPS Press/Springer, New York, pp. 84117. Sloan, K.B., Koch, S.A.M., Siver, K.G., 1984. Mannich base derivatives of theophylline and 5-fluorouracil: syntheses, properties and topical delivery characteristics. Int. J. Pharm. 21 (3), 251264. Springer, C.J., Antoniw, P., Bagshawe, K.D., Searle, F., Bisset, G.M.F., Jarman, M., 1990. Novel prodrugs which are activated to cytotoxic alkylating agents by carboxypeptidase G2. J. Med. Chem. 33, 677681. Sriram, D., Yogeeswari, P., 2010. Chapter 3: Drug metabolism and prodrugs, Medicinal Chemistry, second ed. Pearson, pp. 5574. Stella, V.J., 2004. Prodrugs as therapeutics. Expert Opin. Ther. Pat. 14 (3), 277280. Stella, V., 2006. Prodrug strategies for improving drug-like properties. In: Borchardt, R., Hageman, M., Stevens, J., Kerns, E., Thakker, D. (Eds.), Optimizing the “Drug-Like” Properties of Leads in Drug Discovery. Springer, New York, pp. 221242. Stella, V.J., 2007. A case for prodrugs. In: Stella, V.J., Borchardt, R.T., Hageman, M.J., Oliyai, R., Maag, H., Tilley, J.W. (Eds.), Prodrugs: Challenges and Rewards, vol. 1. Published by AAPS Press and Springer, New York, pp. 333. Stella, V.J., Nti-Addae, K.W., 2007. Prodrug strategies to overcome poor water solubility. Adv. Drug Deliv. Rev. 59, 677694. Stella, V.J., Charman, W.N., Naringrekar, V.H., 1985. Prodrugs. Do they have advantages in clinical practice? Drugs 29 (5), 455473. Stella, V.J., Borchardt, R.T., Hageman, M.J., Oliyai, R., Maag, H., Tilley, J.W., 2007. Prodrugs: challenges and rewards, vol. 12. Published by AAPS Press and Springer, New York. Sun, B., Luo, C., Cui, W., Sun, J., He, Z., 2017. Chemotherapy agentunsaturated fatty acid prodrugs and prodrug nanoplatforms for cancer chemotherapy. J. Control. Release 264, 145159. Sun, J., Yang, D., Cui, S.-H., Zhang, H.-T., Fu, Y., Wang, J.-C., et al., 2019. Enhanced anti-tumor efficiency of gemcitabine prodrug by FAPα-mediated activation. Int. J. Pharm. 559, 4857. Supernaw, R.B., 2007. In Part A: Pharmacologic management of pain. Chapter 111: Simple Analgesics. Pain Manag. 2, 927933. Taylor, M.D., 1996. Improved passive oral drug delivery via prodrugs. Adv. Drug Deliv. Rev. 19 (2), 131148. Toko, T., Shibata, J., Sugimoto, Y., Yamaya, H., Yoshida, M., Ogawa, K., et al., 1995. Comparative pharmacodynamic analysis of TAT-59 and tamoxifen in rats bearing DMBA-induced mammary carcinoma. Cancer Chemother. Pharmacol. 37 (12), 713. Tondwal, R., Singh, M., 2015. Effect of increasing alkyl chain of 1st tier dendrimers on binding and release activities of methotrexate drug: an in vitro study. J. Mol. Liq. 211, 466475. Vivier, M., Rapp, M., Papon, J., Labarre, P., Galmier, M.-J., Sauziere, J., et al., 2008. Synthesis, radiosynthesis, and biological evaluation of new proteasome inhibitors in a tumor targeting approach. J. Med. Chem. 51, 10431047. Walther, R., Rautio, J., Zelikin, A.N., 2017. Prodrugs in medicinal chemistry and enzyme prodrug therapies. Adv. Drug Deliv. Rev. 118, 6577. Wong, P.T., Choi, S.K., 2015. Mechanisms of drug release in nanotherapeutic delivery systems. Chem. Rev. 115 (9), 33883432. Wu, K.-M., 2009. A new classification of prodrugs: regulatory perspectives. Pharmaceuticals 2, 7781. 186 SECTION | 3 Pharmaceutical Chemistry Xue, P., Wang, J., Han, X., Wang, Y., 2019. Hydrophobic drug selfdelivery systems as a versatile nanoplatform for cancer therapy: a review. Colloids Surf., B: Biointerfaces 180, 202211. Yan, Z., Ma, L., Shen, S., Li, J., 2018. Studies on the interactions of some small biomolecules with antibacterial drug benzethonium chloride and its active pharmaceutical ingredient ionic liquid (API-IL) benzethonium L-proline at varying temperatures. J. Mol. Liq. 255, 530540. Yang, F., Kamiya, N., Goto, M., 2012. Transdermal delivery of the antirheumatic agent methotrexate using a solid-in-oil nanocarrier. Eur. J. Pharm. Biopharm. 82, 158163. Yu, J., Li, W., Yu, D., 2018. Atrial natriuretic peptide modified oleate adenosine prodrug lipid nanocarriers for the treatment of myocardial infarction: in vitro and in vivo evaluation. Drug Des. Devel. Ther. 12, 16971706. Zhang, X., You, X.Q., Zhang, X., 2017a. Prodrug strategy for cancer cellspecific targeting: a recent overview. Eur. J. Med. Chem. 139, 542563. Zhang, R., Ru, Y., Gao, Y., Li, J., Mao, S., 2017b. Layer-by-layer nanoparticles co-loading gemcitabine and platinum (IV) prodrugs for synergistic combination therapy of lung cancer. Drug Des. Devel. Ther. 11, 26312642. Zhu, Y., Ma, Y., Zhao, Y., Yang, M., Li, L., 2019. Preparation and evaluation of highly biocompatible nanogels with pH sensitive chargeconvertible capability based on doxorubicin prodrug. Mater. Sci. Eng. C. 98, 161176.