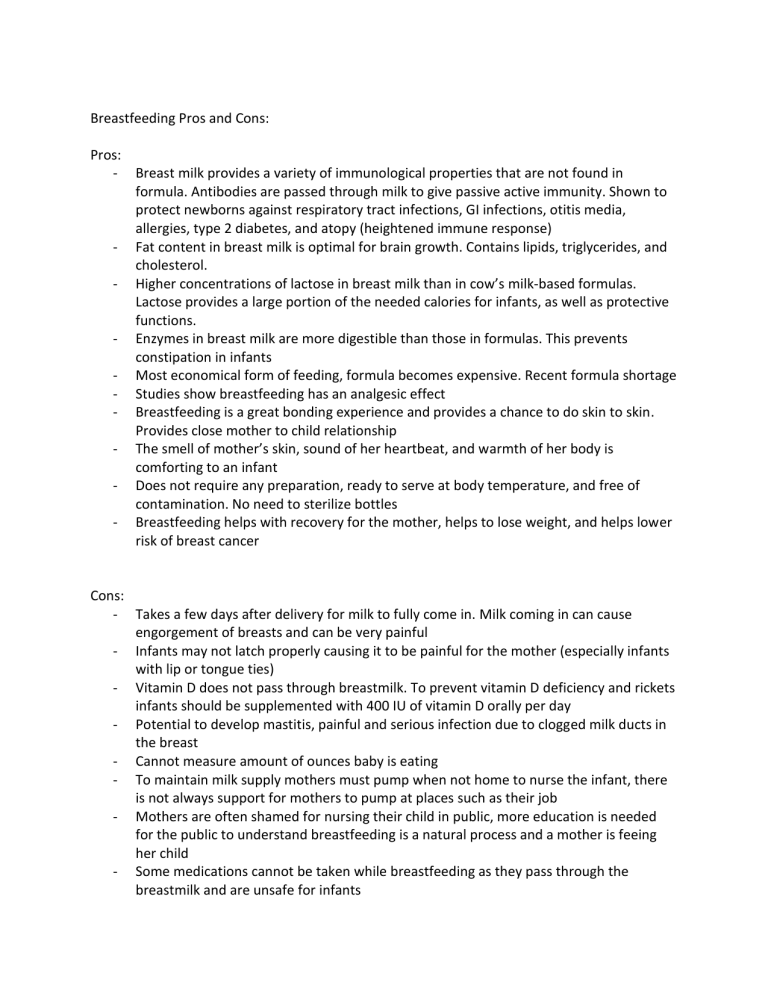
Breastfeeding Pros and Cons: Pros: - Breast milk provides a variety of immunological properties that are not found in formula. Antibodies are passed through milk to give passive active immunity. Shown to protect newborns against respiratory tract infections, GI infections, otitis media, allergies, type 2 diabetes, and atopy (heightened immune response) - Fat content in breast milk is optimal for brain growth. Contains lipids, triglycerides, and cholesterol. - Higher concentrations of lactose in breast milk than in cow’s milk-based formulas. Lactose provides a large portion of the needed calories for infants, as well as protective functions. - Enzymes in breast milk are more digestible than those in formulas. This prevents constipation in infants - Most economical form of feeding, formula becomes expensive. Recent formula shortage - Studies show breastfeeding has an analgesic effect - Breastfeeding is a great bonding experience and provides a chance to do skin to skin. Provides close mother to child relationship - The smell of mother’s skin, sound of her heartbeat, and warmth of her body is comforting to an infant - Does not require any preparation, ready to serve at body temperature, and free of contamination. No need to sterilize bottles - Breastfeeding helps with recovery for the mother, helps to lose weight, and helps lower risk of breast cancer Cons: - Takes a few days after delivery for milk to fully come in. Milk coming in can cause engorgement of breasts and can be very painful - Infants may not latch properly causing it to be painful for the mother (especially infants with lip or tongue ties) - Vitamin D does not pass through breastmilk. To prevent vitamin D deficiency and rickets infants should be supplemented with 400 IU of vitamin D orally per day - Potential to develop mastitis, painful and serious infection due to clogged milk ducts in the breast - Cannot measure amount of ounces baby is eating - To maintain milk supply mothers must pump when not home to nurse the infant, there is not always support for mothers to pump at places such as their job - Mothers are often shamed for nursing their child in public, more education is needed for the public to understand breastfeeding is a natural process and a mother is feeing her child - Some medications cannot be taken while breastfeeding as they pass through the breastmilk and are unsafe for infants - Must limit caffeine or alcohol intake Maternal mental health: mothers are on demand to feed their child every 2-3 hours and may seem overwhelming and feel they have no freedom The mother asks you if it's important for her to breast feed her baby. At 24 hours post-delivery, she doesn't feel she's making enough milk. What should the nurse discuss with this mother? The nurse should explain the stages of breast milk. Breast milk begins as colostrum, a thick sticky milk that is yellowish in color. It is composed of protein, sugars, and is high in antibodies to protect the newborn. It is known as a superfood for infants. With colostrum infants only need 1 ounce of colostrum per day, so the body is not producing large quantities at this time, which is why the mother may feel she is not making enough milk. Production of colostrum lasts for 1-4 days before it becomes transitional milk. This is when the mother will begin to produce larger amounts of milk to feed the infant. Transitional milk begins to change from yellow to white, and has high amounts of proteins, fat, vitamins, and lactulose. At this time, she may experience engorgement or pain while the breasts begin to fill with milk and until the infant learns to properly suck and drink. Feeding regularly is important to help reduce the engorgement. The final form of breastmilk, known as mature milk, does not come in until around 20 days postpartum. Mature milk changes to provide what the baby needs, such as antibodies when they are sick.