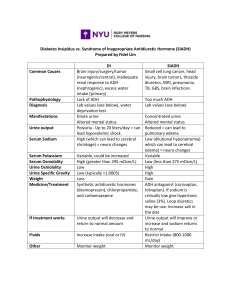
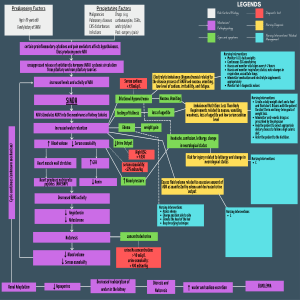
Hinkle & Cheever 14th ed. Chap 52, pp. 1509-1524 Excessive secretion of antidiuretic hormone from the pituitary gland despite low serum osmolality level 1. List five essential assessments that should be done for a client with SIADH. assessments necessary? Why are these Nursing Management 1. Close monitoring of fluid intake and output Patients with SIADH cannot excrete a dilute urine causing a low urinary output (oliguria), and retain fluids. 2. Daily Weights>For a baseline. To see if they are experiencing weight gain, and if the condition is getting worse 3. Urine Chemistry> Urine will have a high urine osmolality. Normal urine osmolality 500850. Also, Specific gravity will be >1.005…high from the image above is 1.030+ (possibly when urine is thick and sticky) 4. Blood Chemistry> Serum sodium-For the development a sodium deficiency known as dilutional hyponatremia. Your blood osmolality will be low (Hyposmolality) because the sodium in your bloodstream will be diluted due to the increased fluid retention. Normal serum osmolality 280-295 and Normal Sodium 135-145. Since the two electrolytes are tied together, there will also be hypochloremia. Normal range is 95-105 BUN- Should see normal renal function Creatinine- Should see normal renal function Hgb-inappropriate release of ADH increases free water reabsorption, which increases circulating blood volume, and lowers Hemoglobin Hct- inappropriate release of ADH increases free water reabsorption, which increases circulating blood volume, and lowers Hemoglobin 5. Neurologic Status> When sodium levels in the blood are too low, extra water goes into body cells causing them to swell. This swelling can be especially dangerous for brain cells, resulting in neurological symptoms such as: Headache is the early sign, Confusion, Seizures, and Coma are caused by Hyponatremia. Low sodium OR 1. 2. 3. 4. 5. Blood pressure for increase Respiratory rate O2 Sat Monitor for fluid overload by listening to lungs Assess Urine 2. What are four neurological signs and symptoms of SIADH? Headache is the early sign, Confusion, Seizures, and Coma 3. Explain, why it is important to monitor a client with SIADH or Diabetes Insipidus serum sodium and urine sodium. With SIADH, Decreased Serum sodium will be < 134 mEq/L and Urine Sodium/Osmolality will be increased Normal Urine osmolality will be 500-850 With Diabetes Insipidus, Serum sodium will be>145 and Urine Sodium/Osmolality will be decreased <100mOsm/kg Normal Urine osmolality will be 500-850) 4. In the treatment of SIADH, correlate the therapeutic use of a 3% hypertonic saline. If serum sodium < 120 mEq, Hypertonic saline 3-5% slow infusion. It will block the effect of ADH on the renal tubules, thereby allowing more dilute urine. Hypertonic solution will block ADH from allowing Aquaporins from putting more and more water back into the bloodstream. It will increase the amount of sodium in the bloodstream, which will go into the urine, allowing water is already in the in bloodstream to follow the sodium via the concentration gradient, diluting more of the urine. 5. The physicians orders Lasix 40 mg IVP for your client with SIADH. You review your labs and notice that their serum sodium is only 124 mEq/L. What should be your nursing intervention and why? You want to hold the med and contact the doctor about the lab results. The patient is hyponatremia and you don’t want to cause any neurological complications. 6. When positioning a client with trauma (head) induced SIADH, which position should the client maintain? Explain why. Positioning: HOB no more than 10 degrees ( venous return to heart & atrial filling pressure which ADH ? 7. When assessing your client being treated with Demeclocycline what symptoms would you assess for to determine that the treatment is effective? Demeclocycline has been used in treatment of the syndrome of inappropriate antidiuretic hormone (ADH) secretion (SIADH), as it acts on collecting tubule cells to diminish their responsiveness to ADH, in effect essentially inducing nephrogenic diabetes insipidus. ? 8. What diet constraints does a client with SIADH have? NO FLUIDS Hinkle & Cheever 14th ed. Chap 52, pp. 1509-1524 9. What is Nephrogenic DI (NDI)? Another cause of DI is failure of the renal tubules to respond to ADH; this nephrogenic form may be related to hypokalemia, hypercalcemia, and a variety of medications (e.g., lithium, demeclocycline [Declomycin]). 10.A client asks what is the “Water deprivation test?” What would you explain to him? The fluid deprivation test is carried out by withholding fluids for 8 to 12 hours or until 3% to 5% of the body weight is lost. The patient is weighed frequently during the test. Plasma and urine osmolality studies are performed at the beginning and end of the test. The inability to increase the specific gravity and osmolality of the urine is characteristic of DI. The patient continues to excrete large volumes of urine with low specific gravity and experiences weight loss, increasing serum osmolality, and elevated serum sodium levels. 11. What are your nursing responsibilities for the fluid deprivation test? The patient’s condition needs to be monitored frequently during the test, and the test is terminated if tachycardia, excessive weight loss, or hypotension develops. . 12. Desmopressin acetate (DDAVP) is the drug of choice when treating a client with Diabetes Insipidus. What is the action of this drug and what nursing responsibilities are important when administering it? Desmopressin (DDAVP), a synthetic vasopressin without the vascular effects of natural ADH and works on the kidneys to reduce urine volume and serum osmolality in patients with diabetes insipidus. It increases the reabsorption of water by the kidney. Desmopressin increases cyclic adenosine monophosphate (cAMP) in the cells of the renal tubule to increase the water permeability, decreasing urine volume and increasing its osmolality. It is particularly valuable because it has a longer duration of action and fewer adverse effects than other preparations previously used to treat the disease. It is given intra-nasally; the patient sprays the solution into the nose through a flexible calibrated plastic tube. One or two administrations daily (i.e., every 12 to 24 hours) usually control the symptoms. Adverse effects of desmopressin reportedly occur in less than 5% of cases. The most common effects are erythema, swelling, and burning of the parenteral injection site. Other adverse effects include drowsiness, headache, dizziness, lethargy, shortness of breath, gastric irritation with heartburn, abdominal cramping, vulval pain, nasal congestion, and nasal irritation. Vasopressin causes vasoconstriction; thus, it must be used cautiously in patients with coronary artery disease. A Creatinine clearance less than 50 mL/minutes contraindicates the use of desmopressin. Black box warning; the drug can cause decreased urinary output, which can lead to hyponatremia which can lead to death by headache, seizures, and death. Another black box warning stipulates that changes in fluid volume status may result in cardiac arrest in patients with known cardiovascular disease. Water intoxicantion Administering the Medication Guidelines for administration are as follows: Use the IM, IV, and subcutaneous preparations for central diabetes insipidus. Withdraw the dosage from the ampule and administer it using a small gauge needle and syringe (e.g., an insulin syringe). For intranasal administration, ensure that nasal passages are intact, clean, and free of obstruction before giving intranasally. The nasal spray pump delivers only doses of 10 mcg DDAVP. If doses other than these are necessary, use the nasal tube delivery system as directed below. Insert the top of the dropper into the tube in a downward position. Then squeeze the dropper until the solution reaches the desired calibrated dose and disconnect the dropper. Hold the tube 3/4 inch from the end and insert one end into the nostril until the fingertips reach the nostril. Place the opposite end into the patient’s mouth while the patient holds his or her breath. Have the patient tilt the head back and blow into the tube, and into the nostril, with a strong, short puff. (In children, the nurse or an adult needs to blow into the tube.) 13. List three (3) routes in which DDAVP can be administered. For Central Diabetes Insipidus, use SQ, IV, or IM from Pharm book (Pages 874-876) The Med surgical book mentions intranasal (Page 1510) ?14. Why is it important to monitor a client with DI vital signs, UOP, weight, and LOC so closely? To prevent death 15. What diet constraints does a client with DI have? Eat a diet that is low in salt and protein to help your kidneys make less urine. 16. When assessing a client with neurogenic diabetes insipidus, which finding would indicate the need for intervention? a. Edema b. Increased head circumference c. Weight gain d. Weight loss 17. In a client with diabetes insipidus, a nurse could expect which characteristics of the urine? a. Pale in color; specific gravity less than 1.006 b. Concentrated; specific gravity less than 1.006 c. Concentrated; specific gravity greater than 1.010 d. Pale in color; specific gravity more than 1.025 18. Which is the best monitoring method for a client newly diagnosed with DI? a. Measuring I&O’s, and urine specific gravity b. Measuring abdominal girths every day c. Checking daily weights and measuring intake d. Checking pitting edema in the lower extremities 19. Which clinical manifestations should the nurse report in a client with SIADH? a. Serum calcium of 10mg/dL and tented tissue turgor. b. Serum magnesium of 1.2 mg/dL and large urinary output. c. Serum sodium of 112 m Eq/L and a headache. d. Serum potassium of 5.2 mEq/L and weight loss 20. What findings indicate that the treatment a client’s is receiving for SIADH is effective? (Select all that apply) a. Decrease in body weight b. Rise in blood pressure; drop in HR c. Absence of wheezes in the lung d. Decrease in urine osmolarity 21. Which laboratory value is the most important to monitor in a client with SIADH? a. Glucose b. Hemoglobin c. Creatinine d. Sodium