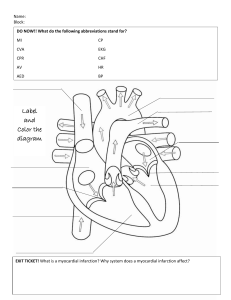
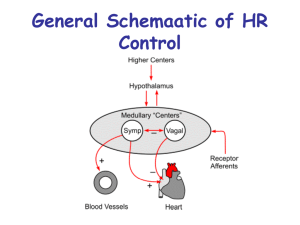
• • • • • • • Cardiac output (CO) is the quantity of blood pumped into the aorta each minute by the heart Determinants: • Stroke Volume • Preload • Afterload • Myocardial contractility • Heart rate Stroke Volume Blood Pressure – indirect measure for tissue blood flow BP = CO x SVR • SVR - determined largely by the tone of the smooth muscle cells lining the arterioles • Vasoconstriction or vasodilation alters SVR and regulates local tissue blood flow 𝛂 β 𝛂1 • 𝛂2 • • • β • ↑ • • • • • • • β • • Inotropes: Effect on the strength of myocardial contractility Vasopressor: Alters blood pressure by increasing vascular tone Chronotropy – rate of firing of sinoatrial node Heart rate Lusitropy - rate of myocardial relaxation • Hemodynamic instability is a common problem in neonates • Inotropes and vasopressors are commonly used to treat low blood pressure or poor perfusion • Limited evidence to guide optimal management in specific clinical situations particularly in neonates • Preterm myocardium contains less contractile tissue • Immature myocardium has a higher basal contractile state and has higher sensitivity to changes in the afterload • • Shock - Imbalance between oxygen delivery and oxygen demand in the tissues leading to tissue hypoxia In the initial compensated phase, blood flow and O2 supply to vital organs are maintained May present with tachycardia, prolonged CRT and decreased UO In the uncompensated phase, decrease in both vital and nonvital organ perfusion leads to the development of lactic acidosis causing irreversible damage Early recognition and identification of the underlying etiology is key to management of shock Factors leading to neonatal shock include: • • • • • Dose Receptor Action 0.5 – 2 mcg/kg/min Dopaminergic receptors Positive chronotropy Renal vasodilation 5 – 10 mcg/kg/min (2 – 6 mcg/kg/min) β1, β2 > ⍺ Positive inotropy Peripheral vasodilation 10 mcg/kg/min 6 – 10 mcg/kg/min ⍺ β1, β2 Peripheral vasoconstriction Positive inotropy Positive contractility • • ⍺ β Benefits Limitations Transition Period ↑ myocardial contractility ↑ MAP ↑ SVR ↑ CBF and tissue oxygenation May have impairment in cardiac contractility due to ↑ SVR Septic Shock ↑ myocardial contractility ↑ MAP ↑ SVR PPHN ↑ myocardial contractility ↑ MAP ↑ SVR • • ↑ PA pressure a(all doses) ↑ PVR (high doses) Dose Receptor Action 2 – 10 mcg/kg/min β1, β2 Increased myocardial contractility Peripheral vasodilation 1 – 20 mcg/kg/min Β1 > β2, ⍺ Positive inotropy Peripheral vasodilation • • • Transition Period Septic Shock • • Benefits Limitations ↑ myocardial contractility (CO) ↑ CBF ↑ renal perfursion Decreased peripheral vascular tone ↑ myocardial contractility No change in mean arterial presure Decreased SVR • • ⍺ β Dose Receptor Action 0.01 – 0.1 β1, β2 > ⍺ Positive inotropy Peripheral vasodilation > 0.1 ⍺ β1, β2 Peripheral vasoconstriction Positive inotropy Positive contractility β Benefits Limitations Transition Period ↑ myocardial contractility ↑ MAP ↑ SVR ↑ CBF ↑ HR ↑ lactate And plasma glucose Septic Shock ↑ myocardial contractility ↑ MAP ↑ SVR PPHN ↑ myocardial contractility ↑ MAP (high dose) ↑ SVR (high dose) • • No change in PA pressure and PVR Dose Receptor 0.05 – 0.5 mcg/kg/min • • • β1, β2 Peripheral vasoconstriction Positive inotropy Benefits Limitations Transition Period ↑ myocardial contractility (CO) ↑ MAP (high dose) ↑ SVR ↑ tissue oxygenation May have impairment in cardiac contractility due to ↑ SVR Septic Shock ↑ myocardial contractility (CO) ↑ MAP (high dose) ↑ SVR ↑ tissue oxygenation May have impairment in cardiac contractility due to ↑ SVR • • ⍺ Action PPHN ↑ MAP (high dose) ↑ SVR ↑ LV output Decreased FiO2 requirement and Pulmonary to systemic pressure ratio Can cause peripheral ischemia and acidosis at high doses Dose Receptor 0.25 – 0.75 mcg/kg/min • • • • PPHN Action Positive inotropy Peripheral vasofilation Lusitropy Benefits Limitations ↑ myocardial contractility and oxygenation Decreased MAP Decreased ductal shunting and lactic acidosis