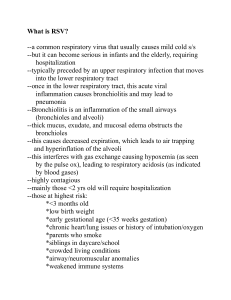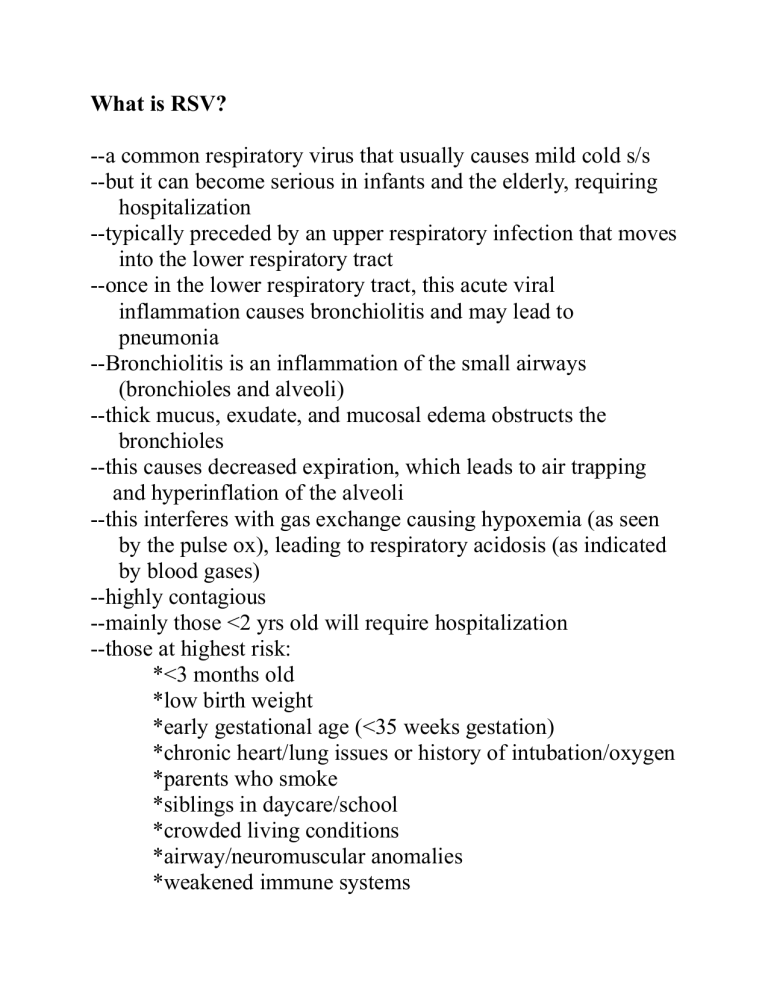
What is RSV? --a common respiratory virus that usually causes mild cold s/s --but it can become serious in infants and the elderly, requiring hospitalization --typically preceded by an upper respiratory infection that moves into the lower respiratory tract --once in the lower respiratory tract, this acute viral inflammation causes bronchiolitis and may lead to pneumonia --Bronchiolitis is an inflammation of the small airways (bronchioles and alveoli) --thick mucus, exudate, and mucosal edema obstructs the bronchioles --this causes decreased expiration, which leads to air trapping and hyperinflation of the alveoli --this interferes with gas exchange causing hypoxemia (as seen by the pulse ox), leading to respiratory acidosis (as indicated by blood gases) --highly contagious --mainly those <2 yrs old will require hospitalization --those at highest risk: *<3 months old *low birth weight *early gestational age (<35 weeks gestation) *chronic heart/lung issues or history of intubation/oxygen *parents who smoke *siblings in daycare/school *crowded living conditions *airway/neuromuscular anomalies *weakened immune systems RSV Season: --starts in the fall --peaks in the winter --length of season and severity vary from community to community and from year to year Prevention: --hand hygiene --cover coughs and sneezes with tissue, shirt sleeve --avoid close contact with others (kissing, shaking hands, sharing cups and utensils, sharing toys) --clean frequently touched surfaces (doorknobs, phones) --RSV vaccine Signs & Symptoms --Early: *increased fussiness *decreased feeding *upper respiratory issues ie runny nose *low grade fever --Current: *decreased breath sounds *crackles, course breath sounds, rhonchi *harsh cough *labored breathing (dyspnea) -tachypnea (^RR) -nasal flaring -retractions -grunting -stridor *apnea *fever *increased mucous, often thick and copious *lethargic yet fussy *poor feeding Nursing Priorities: A = Airway B = Breathing C = Fluid volume Goals: --Optimize respiratory function --Alleviate symptoms --Facilitate recovery Nursing role: --Assess respiratory function --Support respiratory function --Provide comfort/safety --Promote hydration and nutrition --Implement infection control measures --Educate parents --Collaborate with the healthcare team RSV Case Study Present Problem: Olivia Davis is an 8-month-old female infant who presents to ER with mom in December. Mom reports that Olivia has had a runny nose for several days and today, it has worsened. Mom denies any fever, but says Olivia “feels warm”. Olivia has trouble clearing her nose of mucous, and mom doesn’t like to suction her unless the mucous is excessive. Mom reports that her feedings have been in decline as she works harder to breathe and that she is more irritable and not as active. Mom gives Olivia acetaminophen and ibuprofen for subjective fever and to minimize symptoms. What are relevant issues in present problem and clinical significance of each? (Hint: The relevant issues are in bold print, but what is the clinical significance of each of these?) Personal/Social History: Olivia was a late preterm infant, delivered vaginally at 35 weeks and weighing 2.28 kg. Olivia was discharged home with mom at 48 hours of life. Per mom, Olivia has been a “healthy baby” although she has had 2 ear infections. She has a frequent runny nose. Her immunizations are up-to-date. Current weight is 17.6 POUNDS. Current length is 27 INCHES. Mom is a single mother of two children, Olivia and a 3-year-old male who attends preschool. Mom smokes ½ pack per day of cigarettes. The family is on WIC (Women, Infants, and Children Assistance Program). What are the relevant issues in the history and why is each clinically significant? (Hint: Again, the relevant info is in bold print, so please state why each is significant to know?) What are the first nursing actions? (ASSESSMENT) 1. Vital signs: T: 38.9C/102F temporal (36.5C-37.5C) P: 174 and regular (6-9 mo = 98-168bpm) R: 79 and regular (less than 60) BP: 95/58 (normal…when low, late sign of hypovolemic shock, act fast) SpO2: 89% on room air (95-100%) Which of these vital signs are relevant and must be recognized by the nurse as clinically significant? Which pain scale will you use to assess pain? 2. Physical exam: General appearance: Held on mom’s lap, laying against her chest. Tearful but comforts quickly with mom’s touch. Cheeks are flush. ENT: Rhinorrhea that is clear, thick, copious amounts. No drainage from ears. Mouth moist. No teeth present. Respiratory: Course breath sounds with expiratory wheezes bilaterally. Moderate intercostal retractions, nasal flaring, tachypneic, harsh nonproductive cough Cardiac: Pink, warm, dry. Heart sounds regular with no murmur. Femoral and brachial pulses palpable and strong. Cap refill < 3 sec in UE and LE. Circumoral cyanosis when crying but resolves when quiet. Neuro: Lethargic but responsive. Moves all extremities equally. Neck with full ROM. Makes eye contact. Responds to spoken word. GI: Abdomen soft/nontender. +BS per auscultation in all 4 quadrants. Last bowel movement >24 hours ago. GU: Dark yellow urine in diaper Skin: Skin intact, no rashes. Anterior fontanel slightly sunken, soft. No tenting noted. ***What is the relevant assessment data and why is each clinically significant? ***What labs would you expect to be ordered and drawn? Why would these labs be clinically important? What orders will you anticipate? Why?? *Albuterol 0.1 mg/kg nebulizer Q4h with CPT (chest physical therapy) STAT*Continuous oximeter*Acetaminophen suppository every 4 hours per rectum PRN*CXR*RSV antigen test (rRt-PCR swab) *Covid/flu swab *NPO until RR less than or equal to 60 *NG/OG placement for feeding/decompression *Oxygen 2L NC, titrate FiO2 PRN to keep saturation >93% *Contact/droplet precautions *Lumbar puncture for temp >38C in infants *CBC/CRP/blood culture *IV D5 1/2NS with 20 mEq K+ to run at 100ml/kg/day *Ampicillin 50mg/kg/day divided equally Q8h IV *Cefotaxime 100mg/kg per dose Q6h IV *Methylprednisolone 1.5 mg/kg/day divided equally Q8h IV *Famotidine 0.5 mg/kg per dose Q12 IV *Daily weight *Strict I & O *Vital signs Q4h