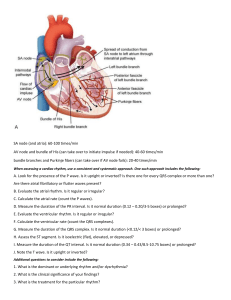
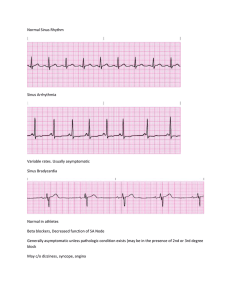
Arrhythmias Cardioversion - “timed” for ventricular depolarization: On the QRS HAS to be synched! Atrial complications Anticoagulation Sedation Voltage varies Take safety: Standard power outlet is 120 – 140 joules; Men with hairy chest —> remove hair takes less electricity Protocol for atrial dysrhythmia: start with 50-100 joules Not going to deliver impulse; will delay until right at QRS AFib/A Flutter: risk of clots - Strokes and pulmonary emboli can result HR high but controlled Still need to be on anticoagulation (warfarin)—> less stress, blood can move more freely Conduction system of the heart: Sinoatrial node depolarizes/contracts by sending electrical impulses to the atrioventricular node via internodal pathways; this is the PR interval (0.12-0.2 seconds → the electrical impulses initiate ventricular contraction (depolarization) by traveling through bundle of His → down the bundle branches → through Purkinje fibers and up the myocardium The electrical impulse quickly travels from the SA node through the atria to the atrioventricular (AV) node; this process is known as conduction. The electrical stimulation of the muscle cells of the atria causes them to contract. The structure of the AV node slows the electrical impulse, giving the atria time to contract and fill the ventricles with blood. This part of atrial contraction is frequently referred to as the atrial kick and accounts for nearly one third of the volume ejected during ventricular contraction. The electrical impulse then travels very quickly through the bundle of His to the right and left bundle branches and the Purkinje fibers, located in the ventricular muscle. The electrical stimulation is called depolarization, and the mechanical contraction is called systole. Electrical relaxation is called repolarization, and mechanical relaxation is called diastole. The process from sinus node electrical impulse generation through ventricular repolarization completes the electromechanical circuit, and the cycle begins again. To calculate HR from ECG, find R that aligns with bold line and count backwards on each line (300, 150, 100, 75, 60, 50) until Atrial Arrhythmias Atrial Flutter: conduction defect in atrium Rhythm: typically sinus Atrial Rate: 280-320 Ventricular rate: 90 No P waves; saw toothed “F waves” QRS shape and duration: usually normal but can also be abnormal or absent PR: many indiscernible P waves cannot confirm PR interval - Remains low because impulse from SA node is blocked at AV node, preventing the conduction of atrial impulses; this would cause ventricular tachycardia Heart’s electrical signals spread through the atria in a fast but regular rhythm instead of irregularly (Afib) “Birds in the attic (atria) are fluttering their wings in sequence and unison” Conduction begins outside SA node in other part of atria Causes 1. Lung Problems (COPD) 2. Cardiac Problems (Pulm. HTN/Left Side HF; fluid backs up in lungs, placing pressure on the heart) (Valvular Disease → ex: mitral stenosis which is a disease of the valve doors) (Thyrotoxicosis/Excess thyroid hormone → hyperthyroidism crisis (thyroid storm) 3. Cardiac Surgery (CABG and birth defect repairs) - Atria are not squeezing properly so less cardiac output → *less oxygen in the body* Signs/Symptoms COLLAPSED: Chest Pain, Oxygen SPO2 Lower, Low BP, Lethargy, Anxiety, Palpitations (racing heart/gallops), SOB, Even HR/rhythm, Dizziness (syncope) Patient Goals 1. Slow the HR and restore normal electrical conduction at the SA node 2. Effective/organized pump in those atria 3. Prevent clots i. Anticoagulants - high risk for bleeding so ensure INR ranges from 2.5-3.5 1. Maintain typical intake of leafy greens that have Vitamin K which blocks the effectiveness of warfarin ii. Beta Blockers - slow HR iii. Cardiac Ablation - burning/freezing erratic atria cells iv. Digoxin- cardiac glycoside that produces deeper contractility (positive inotropic) and decreases HR (negative chronotropic) 1. Hold if apical pulse (fifth intercostal space) is less than 60 bpm 2. Toxicity is 2.0 or more; symptom is seeing green/yellow halos; hypokalemia due to diuretics (furosemide, hydrochlorothiazide) puts the patient at risk for toxicity v. Electro Cardioversion (50-200) joules to reset SA node; usually done after TTE (transthoracic echocardiogram), which is used to rule out presence of blood clots Medical Management - Adenosine: causes sympathetic block and slowing of conduction through the AV node - Used to end the tachycardia - Ideally used for visualization for dx reasons - Given by rapid IV administration immediately followed by a 20 mL saline flush and elevation of the arm to promote circulation of medicine - Atrial flutter is treated with antithrombotic therapy, rate control, and rhythm control in the same manner as atrial fibrillation - Cardioversion Junctional Rhythm aka idionodal rhythm - - When SA node/pacemaker sites fail, the AV Junction is left with pacemaker responsibility. Sinus node slows or when the impulse can’t be conducted through the AV node → AV node discharges an impulse automatically Originates from the junctional area (mostly AV node, bundle of His, and bundle branches) that will generate a signal to pace the heart when the SA node is not working ECG Characteristics (if rhythm is not caused by complete heart block) - Ventr. rate: 40-60 bpm - Atrial rate: 40-60 bpm if P waves are visible - Heart Rate: 40 - 60 BPM - Ventricle/Atrial rhythm: regular - QRS shape/duration: usually normal but can be abnormal - P wave may be: absent, after/before QRS complex, or inverted especially in lead II - PR: <0.12 seconds; may be inverted, hidden in QRS, or following QRS (retrograde) May produce S/S of reduced cardiac output; tx is then the same as for bradycardia Ventricular Dysrhythmias (Amiodarone is most commonly used for ventricular problems) Ventricular Tachycardia - Three or more consecutive PVCs > 100 bpm Patient is nearly always unresponsive and pulseless Ventricular and atrial rate: ventricular: 100-200 bpm; atrial depends on underlying rhythm (e.g., sinus rhythm) Ventricular and atrial rhythm: ventricular is usually regular and atrial is sometimes regular QRS shape/duration: 0.12 seconds or more; bizarre, abnormal shape - P wave: very difficult to see; atrial rate and rhythm may be indeterminable PR interval: very irregular, if P waves can be seen P:QRS Ratio: difficult to determine but if P waves are present, there are usually more QRS complexes than P waves Medical Management - Initial treatment is determined by: identifying rhythms as either mono/polymorphic, determining existence of prolonged QT interval before TV initiation, any comorbidities, and verifying patient’s heart function (normal/decreased) - Antiarrhythmic medications include: procainamide, amiodarone, sotalol, and lidocaine (based upon type of VT, clinical presentation, and patient comorbidities) - Cardioversion is tx of choice for monophasic VT in a symptomatic patient - Defibrillation is tx of choice for pulseless VT - Patient with VT who is unconscious and pulseless is treated in SAME MANNER as V Fib → immediate defibrillation - EF >35% may be managed with antiarrhythmic medication - EF <35% should be considered for an implantable cardioverter defibrillator Torsades de Pointes - Polymorphic VT preceded by prolonged QT interval (congenital or acquired) Common causes: CNS disease; medications (cipro, erythromycin, haloperidol, lithium, methadone), hypokalemia, hypocalcemia, or hypomagnesemia, congenital QT prolonged interval - - Rhythm is likely to cause the patient to deteriorate and become pulseless; immediate treatment is required, which include: electrolyte correction, IV magnesium, IV isoproterenol, or pacing if bradycardic Hard to regulate, NO PULSE! Treatment CPR first Early defibrillation EPI Magnesium Ventricular Fibrillation - Most common arrhythmia in patients with cardiac arrest Rapid, disorganized ventricular rhythm that causes ineffective quivering of ventricles Always characterized by absence of audible heartbeat, palpable pulse, respirations No coordinated activity → cardiac arrest and death are imminent if not corrected Early defibrillation with immediate CPR until defibrillation is available No atrial activity on ECG Most common cause is coronary artery disease and resulting acute MI Other causes: unsuccessfully treated VT, cardiomyopathy, valvular heart disease, proarrhythmic medications, acid-base and electrolyte imbalances, electrical shock, Brugada syndrome (patient frequently of Asian descent has a normally structured heart, few/no risk factors for coronary artery disease, and family hx of sudden cardiac death Medications: Amiodarone, Epinephrine ECG Characteristics - Ventricular rate is > 300 BPM - Ventricular rhythm: extremely irregular with no specific pattern - QRS shape and duration: irregular, undulating waves with changes amplitudes - *NO recognizable QRS complexes* Idioventricular Rhythm - Ventricles “last call” before things stop Ventricles move more slowly than normal <50 BPM Usually don’t see it unless patient has actively been in cardiac arrest No pulse —> EPI Compressions and EPI will treat Not shockable Atrial Fibrillation Rhythm: irregular Atrial rate: ≥ 350; other rate usually over 100 bpm No PR intervals No P waves, “fib waves” instead; atria is not contracting QRS is normal RR, QRS, and QT intervals are analyzed to verify effectiveness of antiarrhythmics First goal is rate control, then cardioversion Cardizem is commonly used Anticoagulation is needed - AV node blocks most of the rapid misfires from the SA node, protecting the ventricles **Increased risk of HR, MI, and embolic events (e.g. PE, CVA, DVT)** - - - Rapid and irregular ventricular response → reduced time for ventricular filling → lower stroke volume Atria are not squeezing blood out to body → less cardiac output = lower oxygen to the body Atrial kick (last part of diastole & ventricular filling, which accounts for 25-30% of cardiac output) is lost due to absence of AV synchrony Some patients are asymptomatic while other experience palpitations and manifestations of HF, including SOB, hypotension, dyspnea, and fatigue High ventricular rate: greater than 80 bpm - Can lead to mitral valve dysfunction, regurgitation, intraventricular conduction delays, and dilated ventricular cardiomyopathy Pulse deficit (difference between apical and radial pulses) - Shorter diastole → ventricles not adequately filling → less time available for coronary artery perfusion → increases risk of MI with onset of chest pain Promotes thrombi formation, especially in left atrium Most common origin of embolisms that result in a stroke in those with nonvalvular afib (arrhythmia caused by HTN, stress, etc) is the left atrial appendage (LAA) LAAO (left atrial appendage occlusion): Paroxysmal: sudden onset with spontaneous termination or an intervention; lasts ≤7 days and may recur Persistent: continuous, lasting more than 7 days Long-standing persistent: continuous, lasting more than 12 months Permanent: persistent, but decision has been made not to restore or maintain sinus rhythm Nonvalvular: absence of moderate-to-severe mitral stenosis or mechanical heart valve Causes - Recovering from open heart surgery can place stress on the heart HTN adds pressure on the heart Alcohol (Holiday Heart Syndrome) is a full episode of AFib - Hyperthyroidism can increase your metabolism, causing added heart stimulation - Diastole: ventricles are relaxed and filling with blood (relax and refill) Systole: heart contracts and pumps blood out from arteries Assessment/Dx - - - Evaluation should include history and exam that identifies onset, nature, frequency, duration, any precipitating factors, and response to medications Risk Factors: Increasing age, Hypertension, Diabetes, Obesity, Valvular heart disease, Heart failure, Obstructive sleep apnea, Alcohol abuse, Hyperthyroidism, Myocardial infarction, Smoking, Exercise, Cardiothoracic surgery, Increased pulse pressure, European ancestry, Family history 12 lead ECG to confirm the arrhythmia and to identify presence or absence of left ventricular hypertrophy, bundle branch block, prior MI, or other arrhythmias TTE (transesophageal echocardiogram) can identify valvular heart disease, provide info about ventricle size/function, RV pressure to identify pulmonary hypertension, LV hypertrophy, and presence of atrial thrombi Blood tests are used to screen for diseases that are risks for atrial fibrillation (thyroid, renal, hepatic) when it is a recent onset or when ventricular rate is hard to control Signs/Symptoms COLLAPSED: Chest Pain, Oxygen SPO2 Lower, Low BP, Lethargy, Anxiety, Palpitations (racing heart/gallops), SOB, Elevated ventricle or heart rate, Dizziness (syncope) What are the main patient outcome goals? 1. SLOW the heart rate and RESTORE normal electrical conduction at the SA NODE 2. Effective/organized PUMP in those ATRIA 3. Prevent CLOTS Nursing Interventions A. Anticoagulants (warfarin) to prevent clots but caution for bleeding i. Monitor INR; 2.5-3.5 is therapeutic range ii. Instruct patient to maintain their normal intake of leafy greens; they contain Vitamin K, which blocks warfarin’s effectiveness B. Beta Blockers to slow the heart rate C. Cardiac Ablation: burn/freeze erratic atria cells D. Digoxin (cardiac glycoside) increases contractility (inotropic) & decreases HR (negative chronotropic); slower but more effective movement of the heart i. HOLD if heart rate is <60 bpm; listen to apical pulse in 5th intercostal space ii. Side note: chrono = time → rate iii. Toxic level: ≥ 2 iv. S/S include patient reports of seeing green or yellow halos and hypokalemia from diuretics (hydrochlorothiazide, furosemide) E. Electro Cardioversion (50-200 joules) given to reset SA node; usually done after TTE (used to rule out blood clots in the atria - Defibrillation (200-360 joules) is usually only given with deadly rhythms (VFib, pulseless V Tach) Premature Ventricular Complex (PVC) - Impulse that begins in a ventricle and is conducted through ventricles before the next normal sinus impulse (premature beat of QRS) - Can occur in healthy people, especially those who use nicotine, caffeine, or alcohol - May be caused by cardiac ischemia, infarction, increased workload on heart (HF and tachycardia), digitalis toxicity, hypoxia, acidosis, or electrolyte imbalances (hypokalemia) - Unifocal: PVCs look the same; we can pinpoint where issue is occurring in cardiac cycle - Multifocal: PVCs have at least two different morphologic appearances Bigeminy: every other complex is a PVC Trigeminy: every third complex is a PVC Quadrigeminy: every fourth complex is a PVC - QRS either accelerates/rebounds or widens out - Ventricular/Atrial rate: depends on underlying rhythm - Ventricular/Atrial rhythm: irregular due to early QRS, creating one RR interval that is shorter than the others; the PP interval may be regular, indicating that the PVC did not depolarize the SA node - QRS shape/duration: duration is ≥ 0.12 seconds, shape is bizarre/abnormal; - P wave: visibility depends on timing of PVC; may be absent (hidden in QRS or T wave) or in front of the QRS; if P wave follows the QRS, its shape may be different - Patients feel that their “heart is skipping a beat” - Effect depends on its timing in cardiac cycle and how much blood was in the ventricles when they contracted - Common occurrence and may increase in frequency with age - Initial tx: aimed at correcting the cause Medical Management - PVCs that are frequent and persistent may be treated with amiodarone or beta blockers - Long-term pharmacotherapy is not usually indicated - Association with adverse outcomes: patients may need to be evaluated for underlying causes (ischemic heart disease and LV dysfx) Premature Atrial Contraction - Premature contraction/beat of P wave - Atria did not wait on depolarization after T wave (electrical impulse starts in atrium before next normal impulse of SA node) - QRS look the same - Early P wave - Less likely to be symptomatic - Can be caused by caffeine, alcohol, nicotine, stretched atrial myocardium (hypervolemia), anxiety, hypokalemia, hypermetabolic states (pregnancy), atrial ischemia, injury, or infarction - Often seen with sinus tachycardia - If infrequent, no tx necessary - If frequent (more than 6/min) this may signal a worsening state or onset of more serious arrhythmia (AFib) - Management is directed towards treating underlying state Premature Junctional Contraction - Impulse that starts in AV node area before the next normal sinus impulse reaches the AV node - Less common than PACs - Causes: digitalis toxicity, HF, CAD - P wave may be absent, may follow QRS, or may occur before QRS but with a PR interval of < 0.12 seconds - Rarely produces symptoms Treatment - If infrequent, no tx necessary - If frequent (more than 6/min) this may signal a worsening state or onset of more serious arrhythmia - Management is directed towards treating underlying state Heart Block (1st degree AV block) - Occurs when all atrial impulses are conducted through the AV node into the ventricles at a slower rate - PRI = > 20 seconds - PR interval: > 0.20 seconds; PR interval measurement is consistent Heart Block (2nd Degree Type I AV Block) Winckebacke - - - - Occurs when there is a repeating pattern in which all but one of a series of atrial impulses are conducted through the AV nose into the ventricles (e.g., every ⅘ atrial impulses are conducted) Each atrial impulse takes a longer time for conduction than the one before, until one impulse is fully blocked AV node is not depolarized by the blocked atrial impulse → AV node has time to fully repolarize so that the next atrial impulse can be conducted within the shortest amount of time Ventricular and atrial rate: Depends on the underlying rhythm, but the ventricular rate is lower than the atrial rate Ventricular and atrial rhythm: The PP interval is regular if the patient has an underlying normal sinus rhythm; the RR interval characteristically reflects a pattern of change. Starting from the RR that is the longest, the RR interval gradually shortens until there is another long RR interval “long, longer, longer, DROP” QRS shape and duration: Usually normal, but may be abnormal P wave: In front of the QRS complex; shape depends on underlying rhythm. PR interval: The PR interval becomes longer with each succeeding ECG complex until there is a P wave not followed by a QRS. The changes in the PR interval are repeated between each “dropped” QRS, creating a pattern in the irregular PR interval measurements Heart Blocks (2nd degree Type II AV Block) - - - Occurs when only some of the atrial impulses are conducted through the AV node into the ventricles Generally a little slower than type 1 and patient becomes more symptomatic Random P wave but no QRS with it Ventricular and atrial rate: Depends on the underlying rhythm, but the ventricular rate is lower than the atrial rate Ventricular and atrial rhythm: The PP interval is regular if the patient has an underlying normal sinus rhythm. The RR interval is usually regular but may be irregular, depending on the P:QRS ratio QRS shape and duration: Usually abnormal, but may be normal P wave: In front of the QRS complex; shape depends on underlying rhythm PR interval: The PR interval is constant for those P waves just before QRS complexes P:QRS ratio: 2:1, 3:1, 4:1, 5:1, and so forth - 2, 3, 4… P waves to every Heart Blocks (3rd degree AV Block) - QRS Occurs when no atrial complex is conducted through the AV node into the ventricles Two impulses stimulate the heart: one stimulates the ventricles (QRS complex), and one stimulates the atria (P wave) P wave may be seen, but atrial electrical activity is not conducted down into the ventricles to initiate the QRS complex, the ventricular electrical activity Having two impulses stimulate the heart results in a condition called AV dissociation, which may also occur during VT Ventricular and atrial rate: Depends on the escape rhythm (idionodal or idioventricular) and underlying atrial rhythm, but the ventricular rate is lower than the atrial rate Ventricular and atrial rhythm: The PP interval is regular and the RR interval is regular, but the PP interval is not equal to the RR interval - - - QRS shape and duration: Depends on the escape rhythm; with junctional rhythm, QRS shape and duration are usually normal; with idioventricular rhythm, QRS shape and duration are usually abnormal P wave: Depends on underlying rhythm PR interval: Very irregular Sporadic P waves & sporadic QRS P:QRS ratio: More P waves than QRS complexes P wave is basically firing whenever it wants Atrial rate is typically in the 30s Dizziness, fatigue, palpitations, possible chest discomfort Transcutaneous pacemaking (defibrillation pads applied —> hit “pacer” function on crash cart) Increase pacing by 10 millivolts until desired rate is reached Usually stabilized short-term quickly after pacing atropine makes HR go up (works on SA) but all it will do is increase atrial rate and place patient at risk for MI P and QRS miscommunication Bundle Branch Blocks - QRS is the issue Blockage in heart where impulse will split Widening on would cause ventricular (bad) TX - document; can’t do anything about it Watch every 6 months Chest pain, SOB, syncope episodes Do not use BB MI, cardiomyopathy, advanced heart disease, stimulant abuse Medical Management of Conduction Abnormalities Based on the cause of the AV block and the stability of the patient, treatment is directed toward increasing the heart rate to maintain a normal cardiac output. If the patient is stable and has no symptoms, no treatment may be indicated or it may simply consist of decreasing or eliminating the cause (e.g., withholding the medication or treatment). If the causal medication is necessary for treating other conditions and no effective alternative is available, pacemaker implantation may be indicated. The initial treatment of choice is an IV bolus of atropine, although it is not effective in second-degree AV block, type II, or third-degree AV block. If the patient does not respond to atropine, has advanced AV block, or has had an acute MI, temporary transcutaneous pacing may be started. If the patient has no pulse, treatment is the same as for ventricular asystole (Link et al., 2015; Soar et al., 2018). A permanent pacemaker may be necessary if the block persists (see later discussion). -