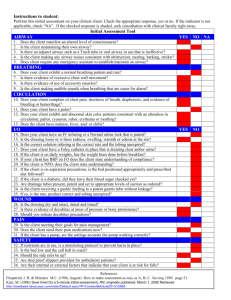
Airway Respiration and Ventilation Upper airway: nasopharynx, oral cavity, mouth, uvula, laryngopharynx, down to larynx; cricoid cartilage: firm ridge forming lower part of the larynx below thyroid cartilage, only complete ring around trachea; epiglottis closes over trachea while swallowing and is at base of oropharynx Lower airway: below vocal cords: trachea (divides at carina), bronchi, -R mainstem bronchi is in direct line with trachea, likely for foreign objects -smaller objects pass more easily beyond carina -R lung has 3 lobes, L lung has 2 lobes Upper airway: flu, sinus infection, croup Lower airway: RSV, bronchiolitis, pneumonia Head Tilt/Chin Lift: heel of one hand on patient’s forehead, firm pressure applied to tilt the patient’s head back; fingertips of alternate hand placed under lower jaw and chin lifted upward -can be used on trauma patient IF jaw thrust fails to open airway -avoid if spinal injury is suspected unless there is no alternative way to open airway If cervical/spinal trauma suspected (even if no obvious signs): jaw thrust maneuver -fingers behind angle of lower jaw, jaw moved upward with index and middle fingers and the thumbs help position the lower jaw -Inline stabilization of cervical spine to ensure no further damage until C Collar Inadequate breathing: adventitious breath sounds, bradypnea, tachypnea (shortness of breath), irregular rhythm, diminished/noisy breath sounds, unequal shallow chest expansion, accessory muscle use, cyanosis, cool moist skin, skin pulling in around the ribs (retractions) Adequate perfusion: normal LOC and good skin color -ventilation can be ok but not necessarily respiration -pulse ox, pink skin, moist mucus membrane are unreliable signs of perfusion (CO poisoning) Innacurate Pulse Ox: -dark/metallic nail polish, dirty fingers -CO poisoning -hypovolemia -severe peripheral vasoconstriction (hypoxia, smoking, hypothermia) -bright ambient light Capillary Refill: good test of circulation in children -under 2-3 seconds -cool proximal extremities reflect poor perfusion and shunting of blood to core Inadequate oxygenation: tachypnea, dyspnea, confusion, lethargy, dizziness, lightheaded, anxiety, irritability, restlessness, headache Hypoxia: -Early: restless, irritable, apprehensive, tachycardic, anxious, tripod position, retractions -Late: altered mental, weak/thready pulse, cyanosis, hypoxia, bradypnea, bradycardia, altered LOC Cyanosis: -chronic bronchitis, hypoxia, hypothermia Anemia: lack of RBCs, appear weak and have pale skin Lung Sounds Stridor: brassy, high-pitched crowing sound heard during inhalation. It suggests a partially occluded airway; upper airway obstruction Wheezing: high-pitched whistling sound; exhalation; bronchi constricted; lower airway constricted (common in asthma, COPD) Rhonchi: low-pitched, noisy sounds that are most prominent on exhalation, suggesting mucus in the lungs, often accompanied by productive cough (COPD, pneumonia, asthma, bronchitis) Crackles/Rales: wet cracking sounds; air passing through fluid in alveoli; CHF, pulmonary edema Gurgling: Fluid in upper airway- requires suction Snoring: upper airway obstruction Vesicular: normal breath sounds Sniffing position: -patient sitting upright with head and chin thrust slightly forward -best for ventilation and intubation -keeps trachea straight and maintains proper spinal alignment -patient on firm surface, small towel under patient’s shoulders and back, stabilize patient forehead to limit rolling during transport Abdominal Thrust (Heimlich): conscious but has a foreign body obstruction -to clear airway obstruction (complete, patient unable to speak or cough) -severe obstruction: weak/absent cough, cyanosis, decreasing LOC -stand behind patient, wrap one arm around make fist with one hand, grasp fist with other hand; place thumb side against patient abdomen just above umbilicus and below xiphoid process; press fist into abdomen in quick inward and upward thrust -Kids: just above umbilicus and well below tip of sternum -If LOC, start CPR and chest compressions -Infants: back blows + chest thrusts 5 back blows between shoulder blades using heel of hand, 5 chest thrusts on lower part of sternum using 2 fingers -Pregnant/Obese: chest thrusts in lieu of abdominal thrust For mild/partial airway obstructions: -wheezing, stridor, and coughing are common -provide oxygen, place in position of comfort, and rapidly transport -indicated by patient being able to breath and talk -avoid ventilation, manual attempts to remove object, abdominal thrusts -is obstruction is VISIBLE: use gloved index finger to sweep it forward -encourage patient to cough forcefully -Unresponsive: begin chest compressions -oxygen cylinder is cracked before attaching regulator to remove dust and other particles -wrench rotates valve counterclockwise then clockwise Oxygen cylinders: D: 0.16 E: 0.28 M: 1.56 G: 2.41 H: 3.14 K: 3.14 ● ● ● ● ● ● D-size: 350 L Jumbo D-size: 500 L E-size: 625 L M (MM)-size: 3,000 L G-size: 5,300 L H, A (M4), or K-size: 6,900 L NRB: 10-15 liters per minute -up to 90-95% oxygen when reservoir bag is filled -bag should be fill before mask is placed on patient (place finger over bag outlet) -if oxygen is not flowing, patient exposed to rebreathing exhaled carbon dioxide -for patients with adequate breathing with suspected/confirmed hypoxia -provide ventilations at same rate as patients and slowly adjust to normal BVM: 100% oxygen with filled reservoir bag and supplemental oxygen 10-15 lpm -1 breath every 5-6 seconds for adults; 1 breath every 3-5 seconds for kids -2 person is best: 1 person maintains mask seal with 2 hands, other ventilates with BVM -for patients with signs of inadequate breathing/respiratory distress -if gurgling is heard, remove mask, inspect oropharynx, suction as needed -1200-1600 mL volume capacity (500 mL for peds and 240 for infant) -500-600 mL over 1 second is appropriate tidal volume -overventilation can cause pneumothorax, gastric distention, vomit aspiration -common complications: poor mask seal, poor head position, gastric distention, barotrauma, decreased cardiac output from increased intrathoracic pressure -Hyper-oxygenation: rare complication Hyperventilation: over breathing, reduced arterial CO2 -causes: diabetic ketoacidosis, aspirin overdose, severe infection -result: anxiety, dizziness, numbness/tingling, spasms in hands and feet (respiratory alkalosis) -instruct patient to slow breathing, give supplemental oxygen, provide transport Nasal Cannula: 24-44% oxygen, 1-6 lpm -not appropriate is hypoxia is suspected (NRB should be used) -for patients who don’t require high flow oxygen, can’t tolerate a NRB or have a specific illness (COPD, bronchopulmonary dysplasia) Mouth to mask device: 55% oxygen with supplemental oxygen at 15 lpm Pocket mask -one way valve prevents backflow of secretions, vomitus, gases -supplemental oxygen can be attached to barrier device 55% oxygen at 15 lpm Blow by blow technique -less frightening oxygen for kids -tubing inserted into a small hole into cup or funnel, connected to oxygen source (6 lpm) -cup held 1-2 inches from child’s face CPAP: provides pressure to keep alveoli open/reverse atelectasis from pulmonary edema -indicated for respiratory distress, pulmonary edema, hypoxia, COPD, recent submersion incident, rapid breathing affecting minute volume, pulse ox below 90 -contradicted for: respiratory arrest, hypoventilation, can’t speak or protect airway, hypotension (less than 90 systolic BP), chest trauma, pneumothorax, GI bleed or surgery, can’t sit upright, cant tolerate mask/seal, facial trauma -complications: claustrophobia, gastric distention, hypotension, decreased blood return/preload Venturi Mask: 24, 28, 35, or 40% oxygen depending on adaptor OPA: -to keep tongue from blocking upper airway (will not prevent liquids) -contradicted for intact gag reflex, conscious patients, petroleum ingestion NPA is an option -Peds: measure using length based resuscitation tape (Broselow tape) or place airway next to child’s face with flange at level of central incisors and bite block segment parallel to hard palate, tip should reach angle of the jaw -gently remove by following curvature of the mouth -rough insertion can cause bleeding -after inserted, reassess airway before assisted ventilation or further intervention NPA: -indicated for unconscious or semiconscious with intact gag reflex or won't tolerate OPA -contradicted for severe head injury, blood draining from nose, fractured nasal bone -basilar skull fracture: CSF draining from ears -ecchymosis under eyes (racoon eyes), or behind one ear (Battle sign) are severe head injury CO Poisoning: -flu like symptoms, dizziness, fatigue, headache, impaired judgment, confusion, hallucination, syncope, seizure Cyanide: dyspnea, respiratory arrest, tachypnea, flushed skin, tachycardia, altered mental, seizures, coma, cardiac arrest Extended transport or Croup: indication for humidified oxygen ● ● ● ● ● ● Ages 0 to 12 months: 30 to 60 breaths per minute Ages 1 to 3 years: 24 to 40 breaths per minute Ages 4 to 5 years: 22 to 34 breaths per minute Ages 6 to 12 years: 18 to 30 breaths per minute Ages 13 to 18 years: 12 to 16 breaths per minute Ages 18 and up: 12 to 20 breaths per minute Children: -Pediatric Assessment Triangle: Appearance, Work of Breathing, Circulation -Bradycardia: critical hypoxia ischemia -ominous sign of respiratory arrest (below 20 for kids under 6 and below 12 for older) -hypertension not a clinical problem; hypotension definitely hypotensive shock, “normal” value is compensated shock -capillary refill more reliable method of evaluating perfusion in children -tongues larger -trachea smaller, easily obstructed -narrowest part of airway is cricoid ring: inferior to thyroid cartilage, lowest part of larynx, first and only complete ring of trachea -diaphragm more relied on for breathing; abdominal breathing is a normal finding (chest cavity can’t optimally contribute to breathing) -signs of increased work: grunting, wheezing, accessory muscle use, retractions (drawing in intercostal or substernal muscles), head bobbing, nasal flaring, tachypnea, tripod position Rigid Catheter: -should be measured from corner of mouth to tip of earlobe -apply suction only while withdrawing the catheter -prolonged suction (over 10 s) can cause vagal stimulation further hypoxia or bradycardia -insert to depth measured (not to resistance or base of tongue) 1. assemble unit 2. ensure vacuum of more than 300 mmHg 3. turn patients head (if no c spine) 4. open mouth using cross finger or tongue jaw lift 5. insert catheter only as far as can be visualized 6. apply suction in a circular motion during withdrawal -Suctioning: at least 300 mmHg vacuum pressure -turn head to side if no spine injury -no more than 10 seconds -prolonged suctioning can obstruct airway, vagal stimulation -French/whistle tip catheter should be used for stoma, clenched teeth, or nose suctioning -Tonsil tip/Yankauer best for infants and children- large diameter, rigid, will not collapse Log roll: to remove visible foreign bodies To alleviate gastric distention in spinal injury patient: -roll patient to one side and apply pressure to upper abdomen -use spinal motion restriction device to turn patient to one side Supraglottic Airway (King LT, LMA, i-Gel)-Indicated for failed intubation through trachea (endotracheal) -contradicted for intact gag reflex or known esophageal disease or caustic substance ingestion -Supraglottic airway sits above glottis while allowing advanced airway access -Intubation confirmed by attaching end tidal waveform CO2 detector btwn airway and bag used to assist ventilation -presence of bilateral breath sounds and absence of gastric or epigastric sounds help confirm appropriate placement King LT Airway sizes: White: (1) 5-12 kg Yellow: (3) 4-5 ft tall Red: (4) 5-6 ft tall Purple: (5) over 6 ft tall Endotracheal Intubation: BE MAGIC Bag valve mask to pre oxygenate, Evaluate airway, Manipulate patient into proper position, Attempt intubation, GI (use supraglottic airway device if unable to intubate), Confirm placement Shiley: tracheostomy tube placed in stoma Epiglottitis: inflammatory disease of epiglottis, rapid onset of signs and symptoms -bacterial infection -soft tissue above vocal cords -ill, sore throat, high fever, tripod positon Tension pneumothorax: collapsed lung Body temperature: -95-93F: shivering, rapid breathing, constricted blood vessels -92-89F: loss of coord, muscle stiffness, slow respiration/pulses, confused, lethargic, sleepy -88-80F: unresponsive, coma, weak pulse, very slow respirations MDI: metered dose inhaler -for acute asthma COPD, bronchitis -6 rights: patient, med, dose, route, time, documentation -needs to be prescribed and medical direction approval needed -contradicted if patient unable to help coordinate depression of trigger Asthma: bronchioles are inflamed and swollen, produce excess mucus -triggered by: upper respiratory infections, exercise, cold air or smoke, emotional stress -wheezing and respiratory distress -treat with Albuterol Acute asthma, COPD, bronchitis -albuterol, ipratropium bromide, levalbuterol, metaproterenol -dilates bronchioles (beta agonist), does not reduce swelling/myocardial oxygen demand/lung moistness Chronic asthma, COPD -beclomethasone, cromolyn, fluticasone, montelukast, salmeterol -anti-inflammatory, reduce swelling COPD: irreversible airway obstruction (emphysema) + significant inflammation (chronic bronchitis) -progressive airflow limitation due to chronic inflammation from noxious gases or particles -chronic inflammation causes narrowing of small airways and decreased elastic recoil of the lung -increased air trapping, progressive airflow limitation -dyspnea, poor exercise tolerance, chronic cough, wheezing, typically have elements of chronic bronchitis and emphysema together -most common cause is smoking -if experiencing hypoxia, high flow oxygen with NRB, and place in fowler position Pneumonia: -fever, tachycardia, hypotension, dyspnea, wheezing/crackles/rhonchi -dehydration, chest pain, weight loss, altered mental Emphysema (type of COPD) -loss of elastic material within alveolar air space -more common than chronic bronchitis -crackles, rhonchi, wheezing -dyspnea, chronic coughing, sputum, long expiration CHF: -damaged ventricular heart muscle can’t keep up with atria blood flow -blood backs up into pulmonary veins lung congestion, pulmonary edema -tachycardia, hypertension, tachypnea, dyspnea alleviated when sitting upright -rales heard -distended neck veins, peripheral edema, cyanotic pale sweaty skin pink frothy sputum Pleural Effusion: -collection of fluid outside lung -causes: Pulmonary embolism, CHF, cancer Intramuscular Epinephrine: -signs of localized allergy: sudden pain, swelling, localized heat, urticaria, redness -signs of anaphylaxis: bronchospasms, wheezing, chest tightness, coughing, dyspnea, hypotension, anxiety, GI complaints Pneumothorax: partial or complete accumulation of air in pleural space -Spontaneous: no identifiable cause, but associated with emphysema, asthma, tall thin men, dyspnea, pleuritic chest pain (sharp, stabbing pain on one side that is worse with inspiration or expiration), absent decreased breath sounds on affected side -Tension: caused by blunt trauma, fractured rib that lacerates lung or bronchus; chest pain, respiratory distress, decreased lung sounds, tachycardia, signs of shock, tracheal deviation -hypotension, hypoxia, absent breath sounds on affected side, tracheal deviation, JVD, tachycardia, tachypnea narrowing pulse pressures: hypoperfusion, tension pneumothorax, cardiac tamponade Pulmonary embolism: blood clot of foreign body/air bubble -commonly formed in a vein in leg or pelvis then break off and travel -no O2/Co2 exchange occurs -cyanosis and dyspnea, tachycardia, tachypnea, chest pain, hemoptysis Nose bleed: pinch nostrils gently while leaning forward Burns: -stop burning, remove clothing -high flow oxygen -cover burns with dry sterile dressing, do not use ointment, lotion, antiseptic, or break blisters -treat for shock: warm blanket to prevent heat loss and hypothermia -transport immediately DVT: blood clot in veins, can lead to pulmonary embolism -sedentary lifestyle, recent injury or surgery, lack of blood flow in legs, stasis -edema in legs and ankles, aching legs, skin discoloration, ulcers Atherosclerosis -buildup of plaque on inside of blood vessels -coronary artery MI NFPA 704 System: diamond shaped symbols with 4 smaller diamonds Red: flammability Blue: health White: special Yellow: reactivity 0-4 (high risk) -used at fixed facilities not transportation