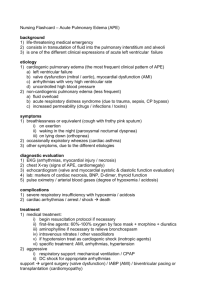
Risk Factors Obesity HTN DM Smoking Illicit drug use PATHOPHYSIOLOLGY MAP (Patient Specific Information) Cues Fatigue Weight gain Elevated HR Hypo- or hypertension SOB Potential complications Pulmonary Edema Dysrhythmias Renal failure Angina MI Death Disease Process: __Chronic Heart Failure____________________ Pathophysiology – include information about your patient Definition: Heart failure is a progressive disease characterized by myocardial cell dysfunction, resulting in the inability of the heart to pump enough cardiac output to meet the demands of the body. Etiology: HF is caused Myocardial cell dysfunction and myocardial muscles become weakened and unable to pump efficiently Chronicity: Heart failure is a chronic progressive disease. Prognosis: HF mortality rates are declining but remain high at about 40% after five years from time of diagnosis. Reference: Hoffman, J. J., & Sullivan, N. J. (2020). Davis advantage for medical-surgical nursing: Making connections to practice. F.A. Davis. Nursing actions-highlight the interventions you implemented Monitor VS (HR, BP, RR, O2, Temp) Auscultate Breath Sounds Assess pt for skin color, peripheral pulses, and capillary refill time Oxygen therapy HOB Elevation Medication Administration (Diuretics, ARB”s) Fluid and Sodium Restriction In your own words, provide the rationales for the interventions you implemented VS can indicate if the pt has increased afterload and low CO2 Crackles can indicate pulmonary congestion S/S of low CO2 are pale/cyanotic skin color, weak peripheral pulses, sluggish capillary refill time. Oxygen therapy to maintain adequate oxygenation HOB Elevation can assist with oxygenation/comfort. Medication can decrease volume, afterload, workload and myocardial oxygen consumption