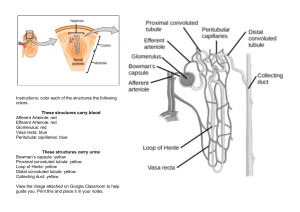
MEDN2001: RENAL PHYSIOLOGY LEARNING OBJECTIVES Produce a diagram showing the structures and major functions of the nephron. Explain the relationship between renal blood flow and glomerular filtration rate. Discuss the role of the sympathetic nervous system in the regulation of renal blood flow. Describe the role of the renin–angiotensin–system as it relates to renal blood flow. List several factors that affect glomerular filtration rate. Briefly explain the process of urine formation. List specific transport mechanisms occurring in different parts of the nephron, including active transport, osmosis, facilitated diffusion, and passive electrochemical gradients Describe the processes which occur in the nephron to regulate fluid and electrolyte balance in the body Identify the electrolytes reabsorbed and secreted by the proximal and distal tubes. Describe the system of urine concentration. Identify hormones activated or secreted by the kidney and describe their actions. THE NEPHRON The nephron is the functional unit of the kidney, having the ability to form urine. The nephron is formed of the outer cortex and inner medullar, however the medulla only gets 2% of the blood flow (only the loop of henle dips below the medulla). From the renal artery we have different arterials feeding into different nephrons. The nephron is a tubule that is convoluted at some parts and consists of 6 main structures. Collecting ducts: collects the urine from multiple functional units. Consists of intercalated and principal cells. Bowman’s capsule: the expand ends of the tubule (C shape part of tubule) which consists of a glomerular membrane across which happens the filtration. There is a basement membrane onto which we have epithelium cells; they also have podocytes with large slits in between allowing for the movement of particles. Under the basement membrane, we have the lining of the capillaries (endothelium cells). The size of slit and fenestrae regulate what can pass through the glomerular membrane. Glomerulus: expanded ends of the tubule with the capillaries, and is surrounded by the bowman’s capsule Proximal convoluted tubule: the first part which is convoluted. The proximal convoluted tubule cells are rich in mitochondria and microvilli which allows the cell to have a very large surface area for transport. This tubule is responsible for reabsorbing substances such as glucose, amino acids and sodium back into the bloodstream. Distal convoluted tubule: second part which is convoluted. The distal convoluted tubule cells have less mitochondria and microvilli than the proximal tubule – as it has the same function but to a lesser extent. This tubule is responsible for regulating the balance of electrocytes in the urine Loop of Henle: it is U shaped between the proximal convoluted tubule and consists of a thin descending part and thick ascending part. It helps concentrate urine by creating a concentration gradient in the kidney. The blood that enters the nephron from the renal artery afferent arteriole is filtered at the Bowman’s capsule; the blood is filtered to remove waste products such as urea. The important nutrients (such as glucose) are reabsorbed back into the blood at the proximal convoluted tubule (can sometimes occur in the distal); the loop of Henle helps concentrate urine by reabsorbing water. Some substances are secreted from the blood to be added to the urine (e.g., excess electrolytes) and this occurs in the distal convoluted tubule. The collecting duct then carries the urine from multiple nephrons and excretes it out of the body; urine excretion rate = filtration – reabsorption rate + secretion rate RENAL BLOOD FLOW AND GLOMERULAR FILTRATION RATE Renal blood flow determines the rate at which blood is filtered through the glomeruli in the kidney; the glomeruli is a network of small blood vessels that are responsible for filtering blood and producing urine. The renal blood flow is the amount of blood that flows through the kidneys per unit time, regulated by local and systemic factors such as blood pressure. The glomerular filtration rate is the amount of blood that is filtered through the glomeruli per unit time, reflecting the ability of the kidneys to remove waste products from the blood. Thus, renal blood flow affects the glomerular filtration rate by regulating the amount of blood that flows through the glomeruli and ultimately the filtration pressure in the glomeruli. An increase in renal blood flow will cause an increase in the glomerular filtration rate, and any decrease in renal blood flow will decrease the glomerular filtration rate. SYMPATHETIC NERVOUS SYSTEM AND RENAL BLOOD FLOW REGULATION The sympathetic nervous system regulates renal blood through a complex interplay of neural, hormonal and local factors; being involved in the control of the constriction and dilation of renal blood vessels. When the sympathetic nervous system is activated, the neurotransmitter norepinephrine is released from the sympathetic nerve terminals, and the renin-angiotensin-aldosterone system (RAAS) is also activated. Norepinephrine acts on alpha-adrenergic receptors on the smooth muscle cells in the renal blood vessels, causing vasoconstriction (constriction of vessels) of the afferent arterioles and reducing renal blood flow; vasoconstriction decreases pressure in the vessels and thus decreases glomerular filtration rate (GFR) and urine output. Activation of the renin-angiotensin-aldosterone system (RAAS) also regulates renal blood flow through the action of the hormone Angiotensin II. Angiotensin II acts on angiotensin receptors on the smooth muscle cells of the renal blood vessels, causing moderate vasoconstriction of the efferent arterioles and reducing blood flow. Angiotensin II also stimulates the release of aldosterone, promoting sodium retention and water reabsorption which increases blood volume and pressure, and hence renal blood flow. RENIN-ANGIOTENSIN-SYSTEM The renin-angiotensin-system is a hormonal system that plays an important role in the regulation of blood flow. Receptors in the kidney will detect a decrease in blood pressure or blood volume and as a result will secrete renin. Renin acts on its substrate, angiotensinogen, to cleave it into angiotensin I, which is then converted to angiotensin II when it reaches the lungs by the action of the angiotensin-converting enzyme (ACE). Angiotensin II can directly act on the kidney to constrict vessel walls in the efferent arterioles (vasoconstriction) – these are the blood vessels that carry blood away from the glomeruli. This results in a decrease in glomerular filtration rate and an decrease in renal blood flow. Angiotensin II can also stimulate the secretion of aldosterone from the adrenal glands. Aldosterone promotes sodium retention and water reabsorption, which leads to an increase in blood volume and blood pressure – aldosterone is the king of salt and water retention. Drugs that target the RAAS system, such as ACE inhibitors and angiotensin receptor blockers, work by inhibiting the production/effects of angiotensin II – reducing vasoconstriction and increasing renal blood flow. GLOMERULAR FILTRATION RATE Glomerular filtration rate (GFR) is the rate of filtration against the glomerular membrane, the volume which will be filtered within unit time. The forces across the membrane affects the rate of filtration. GFR = Kf (glomerular hydrostatic pressure + Bowman’s colloidal osmotic pressure) – (Bowman’s hydrostatic pressure + glomerular colloidal osmotic pressure) Factors that can affect the GFR include: Glomerular hydrostatic pressure: this can be effect by the diameter of afferent and efferent arterioles and arterial blood pressure. Glomerular colloidal pressure: increased pressure (e.g., dehydration) decreases GFR, decreased pressure (e.g., hypoproteinemia) increases GFR Bowman’s hydrostatic pressure: e.g., stone in the ureter, increases pressure and decreases GFR Bowman’s colloidal osmotic pressure Ultrafiltration coefficient: permeability of the membrane (increases thickness, reduces Kf and GFR), surface area of membrane (increase surface area, increases Kf and increases GFR) Surface area can be affected by the relaxation of mesangial cells e.g., cAMP and dopamine which will increase surface area. The contraction of mesangial cells e.g., norepinephrine and histamine will reduce surface area. A decrease in the number of glomerular capillaries will decrease surface area. Renal blood flow: an increase in renal blood flow will increase GFR Blood pressure: an increase in blood pressure can lead to an increase in GFR Hormonal factors: hormones such as angiotensin II and aldosterone can affect GFR (through the regulation of renal blood flow and sodium/water reabsorption) URINE FORMATION The process of urine formation takes place in the nephrons of the kidneys. The first process in urine filtration is glomerular filtration, where the blood enters the glomerulus (a network of capillaries in the nephron) through the renal artery afferent arteriole and is filtered through a semi-permeable membrane. The filtrate is filtered in the Bowman’s capsule and contains water, electrolytes and small molecules such as glucose, amino acids and urea – due to the semi-permeable nature of the membrane. The filtrate then moves into the renal tubules, where important nutrients such as glucose and amino acids are reabsorbed into the blood in the proximal convoluted tubule in the processes of tubular reabsorption. Sodium and water are also reabsorbed to maintain fluid balance in the body. Next, tubular secretion occurs in the distal convoluted tubule. Substances, such as hydrogen ions, are secreted into the renal tubules by active transport to be added to the urine (e.g., excess electrolytes) As the filtrate moves through the Loop of Henle, water is reabsorbed to concentrate the urine. The concentrated urine is then collected in the renal pelvis and transported to the bladder for storage and eventual excretion. TRANSPORT MECHANSIMS IN THE NEPHRON The different areas of the nephron use a variety of transport mechanisms in the formation of urine. The mechanisms of tubular transport in the proximal and distal tubule uses active transport and passive transport to achieve their respective functions. Active transport requires energy in the form of ATP and follows the chemical and electrical gradient. There are two types of active transport, and this includes primary active transport and secondary active transport (can be co-transport or counter-transport). Actively transported substances have a tubular transport maximum (Tm) which is the maximum rate at which a substance can be transported by the renal tubules due to the saturation of specific carrier and enzyme systems involved in active transport (e.g., glucose, PAH). Passive transport requires no energy and moves with the chemical electrical gradient. The moving of a substance from the lumen to the interstitial fluid can be done by transcellular transport (the substance passes through the cell) or paracellular transport through the middle of the cells. For example, sodium is actively transported out of the tubular lumen by the sodium-potassium pump, and when this occurs chlorine CI- can be transported paracellular. Water and urea also be transported paracellular – when other substances are actively transported into the fluid through osmosis. Water and electrolytes are reabsorbed by peritubular capillaries by bulk flow. The kidney reabsorbs filtered glucose through the sodium-glucose cotransporters; essentially cotransport is driven by the active sodium transport out of the cell through the sodium-potassium pump which allows for the glucose uptake following the concentration gradient. 100% of glucose is reabsorbed in the proximal convoluted tubule with sodium. Water reabsorption occurs through the process of osmosis and can be obligatory or facultative. Obligatory reabsorption is independent of ADH and will result in the maximum amount of water excreted if we do not reabsorb more under the effect of ADH – this accounts for 87% of filtered water. Under obligatory reabsorption, the proximal tubule accounts for 65% of reabsorption, 15% of reabsorption occurs in the thin loop of Henle as it is not permeable to any solutes (increases osmolarity), and 5% of reabsorption occurs in the distal tubules. In comparison, facultative reabsorption is dependent on the effects of ADH and accounts for 12.5% of filtered water. The action of ADH relocates more water channels to the membrane to increase the permeability of the membrane to water, which results in an extra 8% reabsorbed from the late distal tubule and cortical collecting duct, and 4.5% more from the medullary collecting duct. Sodium is an important substance in the reabsorption of water, thus 99% or more of filtered sodium ions are reabsorbed along the renal tubule. The thin descending loop of the loop of Henle does not allow for the reabsorption of any ions, including sodium, so the majority of sodium ions (65%) are reabsorbed in the proximal convoluted tubule. Sodium is important for reabsorptions of other substances through secondary active transport, such as glucose and amino acids, which rely on the sodium-potassium pump. Hydrogen relies on the sodium-potassium pump in the mechanism of counter transport; in that for every hydrogen ion secreted, there is one bicarb ion reabsorbed. In the thick ascending loop of Henle, we have a channel that allows one sodium ion and two chloride ions will be reabsorbed secondary to the active reabsorption of sodium. The potassium will leak into the lumen urine to ensure that the channel keeps working; this leaking also creates a positive potential allowing magnesium and calcium to enter the interstitium blood. The distal convoluted tubule is the site of sodium and chloride reabsorption. The collecting duct is the site of the action of epithelial sodium channels, as they have cells which have receptors for the hormone aldosterone. Aldosterone will enter the cell and stimulates the nucleus to form proteins that form the epithelial sodium channels; the availability of these channels makes sodium reabsorption easier. REGULATION OF BODY FLUID AND ELECTROYTE BALANCE Filtration: this occurs in the glomerulus where the blood is filtered through a semipermeable membrane, allowing for the passage of water, electrolytes, and small molecules such as glucose, amino acids, and urea. Reabsorption: this occurs in the proximal convoluted tubule where important nutrients such as glucose, amino acids and electrolytes are transported back into the blood – this can be through active transport, facilitated diffusion and diffusion. Sodium ions are actively transported out of the tubular fluid into the surrounding blood vessels which creates a concentration gradient that drives the pass transport of other solutes, such as glucose and amino acids. Water will follow the solutes through osmosis. Water and electrolytes are also reabsorbed by peritubular capillaries by bulk flow. Secretion: this occurs in the distal convoluted tubule where the nephron secretes certain substances into the tubular fluid through active transport mechanisms. These substances may include excess ions or toxins that need to be eliminated from the body. Regulation: the rate of filtration and reabsorption in the nephron is regulated by hormones such as aldosterone and antidiuretic hormone (ADH). These hormones can alter the permeability of the nephron to water and solutes which change the rate at which they can be reabsorbed or secreted – e.g., aldosterone promotes the reabsorption of sodium ions and water. The Loop of Henle creates a concentration gradient in the medulla which allows for the concentration of the urine; the collecting duct will respond to ADH which allows for the regulation of permeability to water, leading to the reabsorption of water back into the body and produces more concentrated urine. ELECTROCYTLE BALANCE BY PROXIMAL AND DISTAL TUBES Proximal tubule Sodium: the proximal tubules reabsorbs approx. 2/3s of filtered sodium through active transport of sodium ions out of the tubular lumen by the sodium-potassium pump – this creates a concentration gradient that drives the reabsorption of other solutes. Chloride: chloride ions are reabsorbed along with sodium through passive transport, when sodium is transported through the sodium-potassium pump Potassium: potassium ions are reabsorbed through a combination of passive transport and active transport mechanisms. This occurs in the thick ascending limb of the loop of Henle, if you are potassium deficient than in the distal tubule you will reabsorb 5% of potassium. Magnesium: magnesium ions are reabsorbed through passive transport mechanisms Calcium: calcium ions are reabsorbed through passive transport mechanisms – will only reabsorb 50% because the other 50% is bound to protein. Distal tubule Sodium: the distal tubule fine-tunes the amount of sodium reabsorbed /secreted depending on the body’s needs Chloride: can be reabsorbed or secreted depending on the body’s needs Potassium: fine-tunes the regulation of the potassium ion balance, can either secrete or reabsorb potassium depending on the body’s needs. If you are high in potassium, then the aldosterone hormone will instead reabsorb sodium and water and secretes potassium Hydrogen: regulation of the acid-base balance in the body is maintained by secreting hydrogen ions to maintain a proper pH balance. H+ ions are secreted in all segments of the renal tubule, except the descending and thin ascending limbs of the loop of Henle. For each H+ secreted, one HCO3- is reabsorbed. SYSTEM OF URINE CONCENTRATION The aim of urine concentration is to produce urine with a high concentration of solutes (such as urea, sodium and potassium) and a low volume of water to conserve water in the body and maintain proper fluid balance. In order to produce concentrated urine, there must be enough ADH which increases the permeability of the late distal convoluted tubule, collecting tubule and medullary duct to water. The main mechanism in the system of urine concentration is the counter current exchange. The blood is first filtered in the glomeruli of the nephron and then water and electrolytes are reabsorbed in the proximal tubules. The function of the loop of Henle in the counter current exchange mechanism is as the counter current multiplier. The loop of Henle consists of one descending limb and one ascending limb, each of which has a distinct permeability to water and solutes – descending limb is highly permeable to water (but impermeable to solutes) while the ascending limb is impermeable to water (but permeable to solutes). As fluid flows through the descending limb water is passively reabsorbed out of the tubule into the surrounding interstitial fluid due to the high concentration of solutes in the interstitial fluid (equilibrate by osmosis). The ascending limb is impermeable to water but can actively transport ions such as sodium and chloride into the interstitial fluid – results in dilute tubular fluid. The interstitial fluid becomes increasingly concentrated as solutes are transported out of the ascending limb establishing a concentrated gradient. As the fluid advances, it creates a gradient where water is passively reabsorbed out of the tubule and into the interstitial fluid – concentrating the urine. The vasa recta then acts as a counter current exchanger which maintains the gradient created by the loop of Henle. In the presence of ADH, urea is also reabsorbed into the interstitium through passive diffusion (from the medullary duct) which helps with the concentration of urine. The antidiuretic hormone (ADH) also plays a role in the concentration of urine. ADH is released from the pituitary gland in response to changes in blood osmolarity, increasing the permeability of the collecting ducts to water through the relocation of more water channels in the membrane. This allows for the reabsorption of water back into the bloodstream and thus makes the urine more concentrated. Counter current mechanism: as urine flows downwards in the collecting tubule, it encounters higher concentrations of solutes in the interstitium and hence loses water due to osmosis. HORMONES OF THE KIDNEY Renin: an enzyme secreted by juxtaglomerular cells and is involved in the regulation of blood pressure by catalysing the conversion of angiotensinogen into angiotensin I. Angiotensin I is then converted into angiotensin II by the action of the enzyme ACE. Angiotensin II causes vasoconstriction, increasing sodium reabsorption in the kidneys and stimulates the release of aldosterone from the adrenal gland which promotes sodium and water retention. Erythropoietin (EPO): a hormone secreted by the kidneys in response to low oxygen levels in the blood. It stimulates the production of red blood cells in bone marrow, increasing oxygen-carrying capacity and improving tissue oxygenation Calcitriol: also known as vitamin D3 which helps to regulate calcium and phosphorus metabolism. It increases calcium and phosphorus absorption in the small intestine and promotes calcium reabsorption in the kidneys. Prostaglandins: group of lipid compounds that play a role in regulating blood pressure by causing vasodilation and inhibiting sodium and water reabsorption in the kidneys. Also aids the regulation of kidney function by modulating blood flow, glomerular filtration rate and electrolyte balance.